Abstract
Surgeon wellness is a multidimensional commitment that encompasses occupational, mental, physical, emotional, and social domains. Loss of professional control, autonomy, and flexibility; inefficient processes; disjointed workplace relationships and goals; excessive administrative burdens; poor work–life balance; and frustrations with medical record and order entry systems have all been associated with burnout. Described as a syndrome of emotional exhaustion, depersonalization, and loss of a sense of personal accomplishment, burnout can have myriad untoward consequences. The strong link between surgeons' personal and professional identities can lead to a perfect storm of burnout, depression, compromised patient safety and quality of care, physician job loss and career dissatisfaction, substance abuse, damage to personal relationships, and suicide. The alarming scope of this problem cannot be confined to a single specialty or practice setting and is expected to increase without much needed changes to surgeon work practices and work environments. A heightened focus on wellness in the workplace with attention to improving workflow, scheduling, collaboration, and resource allocation is a welcome step taken by several institutions and championed by professional societies. Much more research is needed to reliably gauge the overall effectiveness of these approaches, further address the nuances of burnout as it applies specifically to surgeons, and ensure that members of the surgical workforce remain at their peak throughout the duration of their careers.
Keywords: burnout, wellness, well-being, practice improvement, surgeon
There is an alarmingly high rate of burnout among surgeons, which, in turn, carries an enormous personal and professional toll and strains the social and financial resources of the U.S. health care system. Available data suggest that more than 50% of practicing surgeons and nearly 70% of general surgery residents meet the posited criteria for burnout. 1 2 3 The notion of burnout and its effects on individuals, institutions, and communities on a larger scale is not new. 4 The specter of burnout for the practicing surgeon, however, is particularly poignant: surgeons are unique in their professional task of treating patients across multiple settings and phases of care, from office, to operating room, to bedside. Patients expect their surgeons to be lifelong learners and to remain at the forefront of the scientific and technical foundation of their practice. Thus, with its negative influence on personal well-being and career satisfaction, burnout threatens both the longevity of surgeons' careers and the safety of those patients to whom they provide care.
In this study, we focus on the history of burnout, the evolution of its definition, and its risk factors, with particular emphasis on the relevance of burnout to the practice of surgery. We offer a summary of reported personal and professional consequences of this increasingly common problem and review contemporary efforts that have helped to identify and potentially mitigate burnout risk factors. This study should by no means be considered exhaustive of the substantial literature that has emerged on this topic. We further direct the interested reader to several excellent reviews on physician burnout 5 6 7 8 to complement this study.
Defining “Burnout”: A History
The first written descriptions of what is commonly understood by “burnout” may date back as far as the Old Testament, in which Moses' father-in-law rebukes, “You will only wear yourselves out. The work is too heavy for you; you cannot handle it alone” (Exodus 18:17–18). 9 The first instance of the verb form “to burn out,” however, may be found in William Shakespeare's The Passionate Pilgrim , written in the 16th century, in which the object of the speaker's affection has “Burned out love, as soon as straw outburneth.” 10 Graham Greene's 1961 novel A Burnt-Out Case tells the story of “a spiritually tormented and disillusioned architect [who] quits his job and withdraws into the African jungle.” 4
“Burnout syndrome” made its first appearance in social psychology during the 1960s and 1970s, initially in the description of probation officers, volunteer staff employed in urban clinics for drug addicts, and lawyers in the service of vulnerable populations. 11 12 13 14 At the turn of the millennium, researchers shifted the focus of burnout away from individuals who seemed to have “unrealistically high altruistic goals” to larger populations not employed in human services or education. 9 Maslach et al described the following three key dimensions of burnout: (1) overwhelming emotional exhaustion (EE), (2) feelings of cynicism and detachment from the job (“depersonalization,” DP), and (3) a sense of ineffectiveness and lack of personal accomplishment (PA). 4 Balch and Shanafelt identified two common burnout symptoms specific to health care: “Treating patients and colleagues as objects rather than human beings, and feeling emotionally depleted.” 15
The Maslach Burnout Inventory (MBI), a 22-item self-administered questionnaire divided into three subscales, emerged in the 1980s as a measure to assess each of the aforementioned dimensions. 16 17 Although other tools such as the Copenhagen Burnout Inventory and Oldenburg Burnout Inventory have been published, the MBI has been the leading methodological component of burnout research. 4 18 19 Criticisms of these tools include a preponderance of negative phrasing, a lack of sufficient dimensionality to address each component of burnout, and a limited ability to assess changes in burnout response to different interventions. 6 20 The Personal Fulfillment Index is one example of a newer assessment that specifically addresses disengagement from patient care and allows reassessment of burnout in individuals across time and circumstance. 20 Nevertheless, nearly three decades since the MBI was conceived and in the midst of a surge in burnout research, Kaschka et al called to attention the dangers of the profligate use of the term “burnout,” the need for the field to develop standardized diagnostic instruments (as opposed to self-evaluation), and the urgency of greater study into the prevalence, incidence, and consequences of this burgeoning epidemic. 9
In the past several years, while much work has contributed to a better understanding of the prevalence of burnout, still there remains an absence of uniform criteria and a standardized, validated diagnostic tool for burnout. A recent editorial on burnout among neurosurgeons described identifying burnout in oneself and among colleagues as similar to finding “the edge of a cliff in the dark.” 21 The relationship between burnout and depression, for example, continues to evolve: some groups argue in favor of a model in which burnout is separate from but may contribute to depression, whereas others insist that burnout and depression are distinguished only by attribution of the former to a specific domain (i.e., the workplace). 5 22 23 24 25 Methodologically, a large and influential study of burnout among U.S. general surgery residents has received criticism for identifying burnout based on individual MBI subscale scores rather than a composite one. 2 26 Thus quantifying and contextualizing burnout remains a challenge.
Burnout and the “Second Victim”
The delivery of health care in the 21st century has been marked by heightened public attention to medical errors, ushered in by an oft-cited report of the Institute of Medicine (IOM) in 2000. 27 Increased public scrutiny, however, has done little to quell the frequently profound effect that adverse patient outcomes have on most physicians and surgeons. In the same year as the IOM report, Wu offered the concept of the physician as the “second victim” of medical errors and untoward outcomes. “Although it is often said that ‘doctors are only human,’” Wu writes, “technological wonders, the apparent precision of laboratory tests, and innovations that present tangible images of illness have in fact created an expectation of perfection.” 28 Scott et al later described a postevent, six-stage trajectory of the second victim comprising 1 chaos and accident response, 2 intrusive reflections, 3 restoring personal integrity, 4 enduring the inquisition, 5 obtaining emotional first aid, and 6 moving on. 29
Second victims are marked by a sense of personal responsibility for the adverse outcome in a given patient, from which there emerges a deep sense of guilt and self-doubt surrounding their knowledge, clinical skills, and career. 29 The consequences of this self-doubt creep into both the personal and professional lives of physicians; a decrease in job satisfaction, collapse in confidence, and heightened concerns over professional reputation become increasingly dominant, as do feelings of anger, embarrassment, and humiliation. 30 Investigations into the incidence of this phenomenon have concluded that anywhere from 10 to 75% of health care professionals will experience second victim syndrome (SVS). 31 We direct the interested reader to recent excellent reviews on this topic. 30 31
The relationship between burnout and SVS deserves attention. Surgeons who experience burnout have reported an increase in the rate of errors committed. 32 As such, burnout has effectively become a risk factor for subsequent SVS and may contribute to a vicious, feed-forward process marked by a turbulent, often unpredictable emotional state that further increases medical errors. 30 For surgeons, the perception of having made a major medical error is associated with a threefold increased risk of suicidal ideation (SI), compounding an otherwise independent association between burnout and SI. 32 33
To manage SVS, it is imperative to address the possibility of underlying burnout. A recent study surveyed 126 surgeons across three teaching hospitals of the same university and identified intraoperative adverse events as occurring anywhere from one (32%) to more than six (9%) times in a given year. 34 In the wake of these events, 84% of respondents reported emotions on a spectrum consistent with SVS and affirmed both a fear of litigation and concern for lack of a standardized reporting system. 34 Given these data and the troubling relationship between burnout and SVS, it is important to appreciate that administrative support following medical errors may not address burnout per se, thereby leaving open the potential for ongoing negative effects on patient outcomes and cost of care.
The Scope of the Problem
In 2001, Campbell et al used the MBI and a study-specific questionnaire to survey a total of 582 actively practicing surgeons, with 32% reporting high levels of EE, 13% reporting DP, and 4% reporting low LP. 35 Building on these findings a decade later, Shanafelt et al produced a landmark cross-sectional study of the American College of Surgeons (ACS), in which nearly 8,000 surgeons responded to surveys comprising the MBI, a depression-screening questionnaire, and a quality of life (QOL) assessment. 36 Forty percent of these respondents met the study criteria for burnout, defined as a high score on either the EE or DP subscales. Furthermore, 30% of respondents screened positive for depression, and 28 and 11% had a significant decrement in the mental and physical QOL scores, respectively, compared with the mean score for the U.S. population.
Among smaller reports, a study examining burnout among colorectal surgeons in the United Kingdom National Health Service (NHS) surveyed a total of 253 respondents and, using the MBI, identified 27% with low PA and 17% with high EE. 37 An MBI-based survey of 259 responding members of the American Society of Transplant Surgeons found 38% of respondents with high EE, 27% with high DP, and 16% with low PA scores. 38 A similar MBI-based survey of 549 members of the Society of Surgical Oncology identified a total of 28% meeting burnout criteria, consistent with a separately reported 36% prevalence on subset analysis of surgical oncologists from the ACS study. 39 40 McCain et al used the Professional Quality of Life Scale V (ProQOL-V) to identify a 37.2% prevalence of burnout in a survey of 168 responding NHS physicians, of whom nearly one-quarter were surgeons. 41 A cross-sectional study of nearly 1,000 U.S. practicing surgeons across multiple specialties responding to a questionnaire identified 26% of respondents at “high risk of physician burnout” based on a Primary Care Posttraumatic Stress Disorder Screen. 42
Data collection by way of self-reporting is inherently vulnerable to selection bias. The respondents to the surveys disseminated in these studies range from 14 to 44%; clearly, there is a large swathe of the surgeon workforce being missed. It would be a mistake to equate the decision to not respond to these questionnaires with the absence of burnout, as published reports have suggested that burnout is associated with a tendency toward introversion and isolation. 37 43
The implications of these data, notwithstanding the methodological weaknesses and biases that attend them, are daunting. Recent data from pioneers in the field suggest that this trend is worsening with time, with one study reporting an overall mean rate of physician burnout as rising from 46 to 54% between 2011 and 2014. 44 By 2025, a projected deficit of between 45,000 to 90,000 physicians will place added burden onto an already strained health care system, and general surgery is among those disciplines that is expected to suffer disproportionately. 45 46 47 Aside from the myriad personal and professional consequences that befall the practicing surgeon, which we will review in greater detail in the sections to follow, neither the medical community nor society on a larger scale can afford the trend toward early retirement or transition away from clinical practice that has been observed among those surgeons reporting burnout. 35 48
Workplace Risk Factors
Workplace risk factors for burnout are remarkably consistent across professions. A recent systematic review and meta-analysis of studies examining the associations between burnout and work environment across a spectrum of jobs and workplaces concluded that high demands, low job control, high workload, low reward, and job insecurity increased the risk of developing EE. 49 Not surprisingly, these associations mirror those that Linzer et al highlighted in their pioneering work on burnout in primary care physicians: workplace emphasis on quality, a sense of cohesiveness, trust among staff, alignment of values between physicians and executives, and a sense of control over the work environment were associated with lower rates of burnout and higher work satisfaction. 50
Campbell et al reported that caseload, practice setting, or percent of patients insured by a health maintenance organization were not associated with burnout in their study; conversely, the perception that the career was unrewarding and there was a lack of autonomy or involvement in decision-making were strongly associated. 35 The ACS study reported that area of surgical specialization (specifically trauma surgeons, urologists, ENT (ear–nose–throat) specialists, vascular surgeons, and general surgeons), greater number of nights on call per week, greater number of hours worked per week, greater number of years in practice, and incentive-based pay were associated with burnout. 36 40 Regardless of subspecialty, those surgeons who worked more than 80 hours a week or had greater than two nights per week on call had the highest reported rates of burnout. 15 The authors further identified an association between a private practice environment and burnout, but they pointed out that common risk factors for burnout within either a private or academic setting included increasing number of hours worked and number of nights on call per week. 40
Substantial data exist to implicate the technologies, administrative requirements, and workplace interactions of the present-day surgical practice in contributing to burnout. In the recent study of NHS physicians described earlier, 82% of respondents attributed burnout not only to a combination of excess workload, poor outcomes, and mistakes, but also to factors such as “constant access to ‘work’” and “the need to bring clinical administrative work home.” 41 These observations have been validated by other groups. Sinsky et al examined the office-day time allocation patterns of 57 physicians in four specialties in four states and identified a 2:1 relationship between time spent on the electronic health record (EHR) (49.2%) and time spent with a patient (27%); physicians spent up to two additional hours postclinic for additional EHR or administrative work. 51 In a separate study of similar design, the authors assessed 142 family medicine physicians and also concluded that time spent on administration and documentation greatly exceeded that spent with patients. 52 A survey-based study of more than 6,000 responding physicians across all specialties in the United States reported that the use of computerized physician order entry systems was associated with a higher risk of burnout. 53
Personal Risk Factors
The reported risk factors for burnout are not only confined to the workplace but also include personal and demographic characteristics of the surgeon. Campbell et al identified younger age and a perceived imbalance between career, family, and personal growth as individual risk factors. 35 Authors of the 2008 ACS study identified younger age, having a spouse employed outside the home as a nonphysician health care professional, and youngest child at home of age <21 years as additional factors (although having children was itself associated with a lower overall risk). 36
Perhaps most strikingly, the very character of those who would become physicians may itself represent a risk factor for the development of burnout. Selflessness, perfectionism, discipline, perseverance, responsibility, and resilience are coveted qualities among medical school admissions committees and residency program directors. Meaningful and longitudinal experiences that speak to an applicants' lifelong commitment to these ideals are essential. An unforeseen, unfortunate, and likely all-too-common outcome, however, is an unhealthy sense of self-sacrifice. In a review on the subject, Balch and Shanafelt write:
Long hours and a lack of control over one's schedule during medical school, residency, and fellowship may also inculcate surgeons (and physicians from other medical specialties) with a set of habits that are counterproductive to achieving a balanced and full life once training is completed … Many physicians seem to believe that they cannot simultaneously have a fulfilling personal and professional life, and may maintain a strategy that puts their personal life on hold until they retire or leave the practice of medicine. 15
As time and energy is poured into the foundation of a surgical career, the same values that drive excellence in medical school and residency can distract surgeons in training and practice from their own individual needs. That we often fail to appreciate the unique relationship between physicians' personal and professional lives is very much the source of our consternation when we hear the age-old adage, “Physician, heal thyself.”
Personal Consequences of Burnout
The studies presented have associated burnout with poor dietary choices, lack of physical activity, and substance abuse, including alcohol, tobacco, and self-prescribed or illicit drugs. 33 37 43 The myriad effects of burnout on physical and mental health are summarized in Fig. 1 . A follow-up report on the 2008 ACS study reported a significant adverse relationship between all three domains of burnout and symptoms of depression and further identified an independent association between burnout and SI that was separate from that of depression and SI. 54 The authors reported a 6.4% rate of SI among surgeons; 60% of those reporting SI expressed reluctance to seek out mental health resources. These findings are in keeping with work from other groups that has suggested that nearly half of physicians may fail to both disclose and seek treatment for mental illness, particularly in the context of maintaining medical licensure. 55 56 A study of SI among surgeons in Italy and Sweden identified a prevalence of 18 and 12%, respectively, and although the authors did not specifically address burnout, they noted a close association between reported SI and endorsement of recent exhaustion, disengagement, and adversarial workplace environments. 57
Fig. 1.
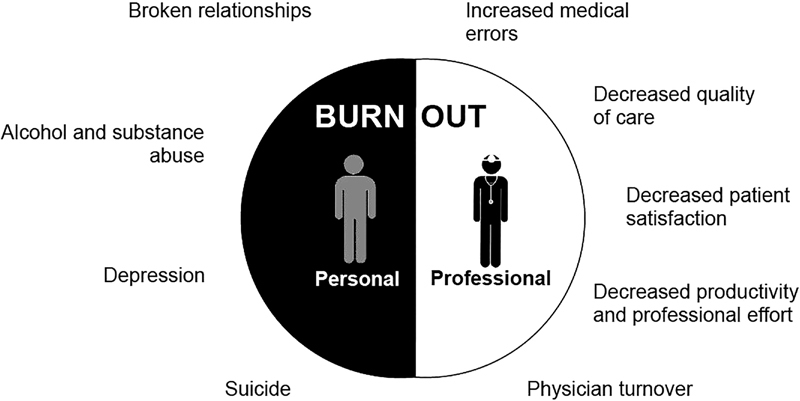
Personal and professional consequences of burnout. (Reproduced with permission of Shanafelt and Noseworthy. 64 )
Data examining the longitudinal effects of burnout on friendships, marriages, and support networks are sparse and often anecdotal. Nevertheless, damage to a surgeon's personal relationships can further contribute to the aforementioned maladaptive behaviors. Data support an association between burnout and increasingly tumultuous family lives. 32 An analysis of self-reported behaviors among surgeons with positive burnout scores suggests a tendency to either keep to oneself or, conversely, lash out at family and friends. 37 Work–home conflicts, defined as the need to perform both work and personal responsibilities simultaneously, not only contribute to burnout but also are also likely to be exacerbated by it. 58 59 Additional work is needed to both corroborate and expand on these findings.
Professional Consequences of Burnout
Surgeon burnout is associated with increased frequency of medical errors and, by extension, can have detrimental effects on the safety and quality of care provided. 32 Though few studies have examined the impact of career distress and job dissatisfaction on surgeons' practices in particular, studies of physicians in nonsurgical specialties have identified associations between these qualities, and medical errors, prescribing practices, malpractice suits, and poor patient satisfaction scores. 42 60 61 62 63 As we have discussed elsewhere, the double impact of burnout in the surgeon who becomes the “second victim” to these errors can create a scenario in which continued practice becomes a liability to both the surgeon and workplace. The professional consequences of burnout are presented in Fig. 1 .
Physicians and surgeons are more likely to seek an exit from clinical practice when they are burned out, be it in the form of early retirement or transition to an entirely nonclinical career. 8 33 35 48 Physician turnover is a costly process, with recent estimates placing the price tag of such an undertaking at more than double a physician's annual salary. 64 It is sobering to consider that those physicians who do not exit practice but continue to work while shouldering burnout are likely to see their productivity suffer. Aside from medical errors, one study identified a dose–response relationship between burnout and decline in full-time work equivalents across 2,000 physicians within the same organization who were surveyed over a 24-month period. 44 Taken together, the costs associated with medical errors, physician and institutional liability, physician turnover, and decreased productivity craft a strong economic argument that should bolster the moral and ethical responsibility to address burnout.
Lessons from the Front Line: Strategies to Reduce Burnout
The data presented hitherto on surgeon burnout can only beg the question: what now? With high stakes for both the individual and institution, the past few years have been witness to a rise in tactics to address and prevent burnout. Collectively, such strategies begin with awareness. The leadership of multiple societies and professional bodies, including the National Academy of Medicine, ACS, and Society for Surgery of the Alimentary Tract, have called attention to the new reality and charged their members to do the same. 65 66 67
While these calls have not gone unanswered, much work remains.
A systematic review and meta-analysis of 15 randomized controlled trials and 37 observational studies identified several individual and organizational interventions that may provide meaningful benefit in preventing and reducing physician burnout. 68 These included mindfulness, self-care, or stress-management programs; duty hour and rotation length restrictions; small group curricula; and communication skills training. While nearly all studies showed a positive effect on reduction of overall burnout and, in particular, EE, the authors highlighted the need to further explore the benefits within individual subgroups of physicians across different specialties and career stages.
Several studies have identified key interventions that deserve mention, as they are likely to provide the groundwork upon which additional measures may be developed and propagated. The opportunity to devote a minimum of 20% of protected time and effort toward an activity that physicians felt was individually meaningful in light of their professional goals had a protective effect against burnout among academic faculty at a single institution. 69 Fassiotto et al recently published encouraging results of a pilot program of career coaching and time-banking, which acknowledges previously undervalued activities of academic medical faculty and strives to minimize work–life conflict. 70
With an eye toward clerical and EHR-related burdens, a small study examined the role of full-time support staff trained and hired to enter orders and conduct previsit planning, and identified a nearly 21% increase in work relative value units, self-reported improvement in focus on patient care, decrease in stress, and decrease in fatigue among internists. 71 A recent study across 11 outpatient surgical clinics demonstrated improved job satisfaction, higher work engagement, and less burnout when “relational coordination” was championed in the workplace. 72 Relational coordination, described as a measure of teamwork in health care, emphasizes shared goals, accountability, mutual respect, teamwork, and open communication, and has been associated with heightened work quality and workplace well-being across diverse professions. 73 Investigators at the Mayo Clinic have embraced a multipronged organizational strategy that focuses on acknowledging and assessing burnout; developing, implementing, and measuring the impact of interventions; cultivating a sense of community built on the principles of relational coordination; and both promoting and enabling work–life balance and self-care. 64
Closing Remarks
Tantamount to the noble efforts of the surgical profession to remain at the forefront of science and service to society is the need to ensure the fitness of surgeons throughout their professional lives. Research into burnout, its causes, and its detrimental effects on patients and physicians alike has breathed new life into the importance of this responsibility, which we cannot ignore any longer. As a group, we must embrace the “quadruple aim,” sharing an obligation to one another's well-being while remaining steadfast in our commitment to quality, safety, and the patient experience. 74 75
Those who embark on a career in surgery do not do so with the expectation that the personal and professional life they inherit will be easy. 76 If anything should be obvious from the literature presented in this study, it is that the solution to surgeon burnout is more complex than to simply have surgeons work less. In any profession, master craftsmanship requires constant exposure. To simply place limits a surgeon's work is not only to take a one-size-fits-all approach to the issue of burnout but also to risk blunting the skill of the surgical workforce. Surgery is a unique profession, with unique challenges and unique relationships. We propose that surgeons take active roles in tailoring solutions that take into account our unique needs as individuals, and the nuances of our profession. Inasmuch as we are responsible to our patients, so too must we be responsible to ourselves and to one another. We must be mindful of factors at the individual, work group, organizational, and national levels that contribute to burnout and not narrow our focus on time or remuneration alone. An iteration of this interplay is provided in Table 1 .
Table 1. Drivers of burnout with examples of individual, work unit, organization, and national factors that influence each driver.
| Drivers of burnout | Examples of influential factors across different levels | |||
|---|---|---|---|---|
| Individual | Work unit | Organizational | National | |
| Workload and job demands | Specialty Practice Location Practice type Work–income relationship |
Expectations Team structure Efficiency Allied health staff |
Productivity targets Pattern of compensation Payer Mix |
Reimbursement structure Medicare/Medicaid Fee-for-service Bundled payments Documentation requirements |
| Efficiency and resources | Experience Personal efficiency Organizational skills Willingness to delegate Ability to say “no” |
Support staff Scribes Team huddles Allied health staff |
EHR Computerized ordering system Interpretation and application of state/federal regulations |
E-prescribing Medication reconciliation requirements Federal mandates for EHR Certification agencies Precertification requirements |
| Meaning in work | Knowing what is personally meaningful Doing what is personally meaningful Shaping career to match interests Doctor-patient relationships Recognizing positive events |
Matching talents and interests Education Research Leadership |
Organizational culture Practice environment Professional development opportunities |
Supervisory role of physicians and potential for less contact with patients Declining funds for education and research Clerical work burden |
| Culture and values | Altruism Moral compass Commitment to an organization |
Behavior of leadership Availability space, rooms Equity/fairness |
Organizational mission Organization values Communication Just culture |
Coverage for uninsured Remuneration structure: what is rewarded? Regulations |
| Control and flexibility | Personality Assertiveness Intentionality |
Control of physician calendars Clinic hours Vacation time Call schedules |
Scheduling systems Referral pattern oversight and restrictions Role and implementation of “practice guidelines” |
Precertification requirements Restrictive insurance networks Practice guidelines |
| Social support | Personality Length of service Relationship-building skills |
Collegiality Physical configuration Social gatherings |
Collegiality Physicians' lounge Community-building strategies, events |
Role of medical specialty societies in building community, championing members |
| Work–life balance | Priorities and values Spouse/partners Children/ dependents Health issues |
Call schedule, including vacations and weekends Expectations Role models |
Vacation policies Sick/medical leave Short-term disability Part-time work Flexible scheduling Role models |
Maintenance of certification Licensure Clerical work burden |
Abbreviation: EHR, electronic health record.
Source: adapted with permission of Shanafelt and Noseworthy. 64
Progress is being made to improve on the status quo within this generation and for the next, not in the least by way of elevating burnout research from a science in its infancy to a fundamental tool with which to continually evaluate and improve the dynamic between the worker and the workplace. As this field develops, longitudinal measures of efforts to address and mitigate the risk factors for burnout will help usher in a period of improved satisfaction and productivity. Above all else, surgery must remain, in the best sense of the word, a human endeavor.
Footnotes
Conflict of Interest None.
References
- 1.Dimou F M, Eckelbarger D, Riall T S. Surgeon burnout: a systematic review. J Am Coll Surg. 2016;222(06):1230–1239. doi: 10.1016/j.jamcollsurg.2016.03.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Elmore L C, Jeffe D B, Jin L, Awad M M, Turnbull I R. National survey of burnout among US general surgery residents. J Am Coll Surg. 2016;223(03):440–451. doi: 10.1016/j.jamcollsurg.2016.05.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Brandt M L. Sustaining a career in surgery. Am J Surg. 2017;214(04):707–714. doi: 10.1016/j.amjsurg.2017.06.022. [DOI] [PubMed] [Google Scholar]
- 4.Maslach C, Schaufeli W B, Leiter M P. Job burnout. Annu Rev Psychol. 2001;52:397–422. doi: 10.1146/annurev.psych.52.1.397. [DOI] [PubMed] [Google Scholar]
- 5.Imo U O. Burnout and psychiatric morbidity among doctors in the UK: a systematic literature review of prevalence and associated factors. BJPsych Bull. 2017;41(04):197–204. doi: 10.1192/pb.bp.116.054247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rothenberger D A. Physician burnout and well-being: a systematic review and framework for action. Dis Colon Rectum. 2017;60(06):567–576. doi: 10.1097/DCR.0000000000000844. [DOI] [PubMed] [Google Scholar]
- 7.DeCaporale-Ryan L, Sakran J V, Grant S B et al. The undiagnosed pandemic: burnout and depression within the surgical community. Curr Probl Surg. 2017;54(09):453–502. doi: 10.1067/j.cpsurg.2017.07.001. [DOI] [PubMed] [Google Scholar]
- 8.Lacy B E, Chan J L. Physician burnout: the hidden health care crisis. Clin Gastroenterol Hepatol. 2018;16(03):311–317. doi: 10.1016/j.cgh.2017.06.043. [DOI] [PubMed] [Google Scholar]
- 9.Kaschka W P, Korczak D, Broich K. Burnout: a fashionable diagnosis. Dtsch Arztebl Int. 2011;108(46):781–787. doi: 10.3238/arztebl.2011.0781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Schaufeli W B, Buunk B P. New York, NY: Wiley; 1996. Professional burnout; pp. 311–46. [Google Scholar]
- 11.Maslach C, Pines A. The burn-out syndrome in the day care setting. Child Care Q. 1977:6100–113. [Google Scholar]
- 12.Freudenberger H J. Staff burn-out. J Soc Issue. 1974;30(01):159. [Google Scholar]
- 13.Pines A, Maslach C. Characteristics of staff burnout in mental health settings. Hosp Community Psychiatry. 1978;29(04):233–237. doi: 10.1176/ps.29.4.233. [DOI] [PubMed] [Google Scholar]
- 14.Bradley H B. Community-based treatment for young adult offenders. Crime Delinq. 1969;15(03):359–370. [Google Scholar]
- 15.Balch C M, Shanafelt T. Combating stress and burnout in surgical practice: a review. Adv Surg. 2010;44(01):29–47. doi: 10.1016/j.yasu.2010.05.018. [DOI] [PubMed] [Google Scholar]
- 16.Iwanicki E F, Schwab R L. A cross validation study of the Maslach Burnout Inventory. Educ Psychol Meas. 1981;41(04):1167–1174. [Google Scholar]
- 17.Maslach C, Jackson S E.The measurement of experienced burnout Journal of Occupational Behaviour 198120299–113.. JSTOR, HYPERLINKhttp://www.jstor.org/stable/3000281 [Google Scholar]
- 18.Demerouti E, Bakker A B. New York, NY: Nova Science Publishers; 2008. The Oldenburg Burnout Inventory: A good alternative to measure burnout and engagement. Handbook of stress and burnout in health care; pp. 65–78. [Google Scholar]
- 19.Kristensen T S, Borritz M, Villadsen E. The Copenhagen Burnout Inventory: a new tool for the assessment of burnout. Work Stress. 2005;19(03):192–207. [Google Scholar]
- 20.Trockel M, Bohman B, Lesure E et al. A brief instrument to assess both burnout and professional fulfillment in physicians: reliability and validity, including correlation with self-reported medical errors, in a sample of resident and practicing physicians. Acad Psychiatry. 2018;42(01):11–24. doi: 10.1007/s40596-017-0849-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Eddleman C S, Aoun S G, Batjer H H. How to identify the edge of a cliff in the dark: burnout and neurosurgery. World Neurosurg. 2013;80(05):e111–e113. doi: 10.1016/j.wneu.2013.01.063. [DOI] [PubMed] [Google Scholar]
- 22.Epstein R M, Privitera M R.Doing something about physician burnout Lancet 2016388(10057):2216–2217. [DOI] [PubMed] [Google Scholar]
- 23.Bianchi R, Schonfeld I S, Laurent E.Burnout or depression: both individual and social issue Lancet 2017390(10091):230. [DOI] [PubMed] [Google Scholar]
- 24.Bianchi R, Schonfeld I S, Laurent E. ‘Burnout syndrome’ - from nosological indeterminacy to epidemiological nonsense. BJPsych Bull. 2017;41(06):367–368. doi: 10.1192/pb.41.6.367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bianchi R, Schonfeld I S, Laurent E. Is it time to consider the “burnout syndrome” a distinct illness? Front Public Health. 2015;3:158. doi: 10.3389/fpubh.2015.00158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Brisson R, Bianchi R. On the inconsistency of burnout conceptualization and measurement. J Am Coll Surg. 2017;224(01):87. doi: 10.1016/j.jamcollsurg.2016.09.006. [DOI] [PubMed] [Google Scholar]
- 27.Kohn K T, Corrigan J M, Donaldson M S, eds;Institute of Medicine Committee on Quality of Health Care in America. To Err Is Human: Building a Safer Health System Washington, DC: National Academies Press; 1999 [PubMed] [Google Scholar]
- 28.Wu A W.Medical error: the second victim. The doctor who makes the mistake needs help too BMJ 2000320(7237):726–727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Scott S D, Hirschinger L E, Cox K R, McCoig M, Brandt J, Hall L W. The natural history of recovery for the healthcare provider “second victim” after adverse patient events. Qual Saf Health Care. 2009;18(05):325–330. doi: 10.1136/qshc.2009.032870. [DOI] [PubMed] [Google Scholar]
- 30.Marmon L M, Heiss K. Improving surgeon wellness: the second victim syndrome and quality of care. Semin Pediatr Surg. 2015;24(06):315–318. doi: 10.1053/j.sempedsurg.2015.08.011. [DOI] [PubMed] [Google Scholar]
- 31.Coughlan B, Powell D, Higgins M F. The second victim: a review. Eur J Obstet Gynecol Reprod Biol. 2017;213:11–16. doi: 10.1016/j.ejogrb.2017.04.002. [DOI] [PubMed] [Google Scholar]
- 32.Shanafelt T D, Balch C M, Bechamps G et al. Burnout and medical errors among American surgeons. Ann Surg. 2010;251(06):995–1000. doi: 10.1097/SLA.0b013e3181bfdab3. [DOI] [PubMed] [Google Scholar]
- 33.Shanafelt T D, Dyrbye L N, West C P, Sinsky C A. Potential impact of burnout on the US physician workforce. Mayo Clin Proc. 2016;91(11):1667–1668. doi: 10.1016/j.mayocp.2016.08.016. [DOI] [PubMed] [Google Scholar]
- 34.Han K, Bohnen J D, Peponis T et al. The surgeon as the second victim? Results of the Boston Intraoperative Adverse Events Surgeons' Attitude (BISA) Study. J Am Coll Surg. 2017;224(06):1048–1056. doi: 10.1016/j.jamcollsurg.2016.12.039. [DOI] [PubMed] [Google Scholar]
- 35.Campbell D A, Jr, Sonnad S S, Eckhauser F E, Campbell K K, Greenfield L J.Burnout among American surgeons Surgery 200113004696–702., discussion 702–705 [DOI] [PubMed] [Google Scholar]
- 36.Shanafelt T D, Balch C M, Bechamps G J et al. Burnout and career satisfaction among American surgeons. Ann Surg. 2009;250(03):463–471. doi: 10.1097/SLA.0b013e3181ac4dfd. [DOI] [PubMed] [Google Scholar]
- 37.Sharma A, Sharp D M, Walker L G, Monson J RT. Stress and burnout among colorectal surgeons and colorectal nurse specialists working in the National Health Service. Colorectal Dis. 2008;10(04):397–406. doi: 10.1111/j.1463-1318.2007.01338.x. [DOI] [PubMed] [Google Scholar]
- 38.Bertges Yost W, Eshelman A, Raoufi M, Abouljoud M S. A national study of burnout among American transplant surgeons. Transplant Proc. 2005;37(02):1399–1401. doi: 10.1016/j.transproceed.2005.01.055. [DOI] [PubMed] [Google Scholar]
- 39.Kuerer H M, Eberlein T J, Pollock R E et al. Career satisfaction, practice patterns and burnout among surgical oncologists: report on the quality of life of members of the Society of Surgical Oncology. Ann Surg Oncol. 2007;14(11):3043–3053. doi: 10.1245/s10434-007-9579-1. [DOI] [PubMed] [Google Scholar]
- 40.Balch C M, Shanafelt T D, Sloan J A, Satele D V, Freischlag J A. Distress and career satisfaction among 14 surgical specialties, comparing academic and private practice settings. Ann Surg. 2011;254(04):558–568. doi: 10.1097/SLA.0b013e318230097e. [DOI] [PubMed] [Google Scholar]
- 41.McCain R S, McKinley N, Dempster M, Campbell W J, Kirk S J.A study of the relationship between resilience, burnout and coping strategies in doctorsPostgrad Med J2017(e-pub ahead of print). Doi: postgradmedj-2016-134683 [DOI] [PubMed]
- 42.Jackson T N, Pearcy C P, Khorgami Z, Agrawal V, Taubman K E, Truitt M S. The physician attrition crisis: a cross-sectional survey of the risk factors for reduced job satisfaction among US surgeons. World J Surg. 2018;42(05):1285–1292. doi: 10.1007/s00268-017-4286-y. [DOI] [PubMed] [Google Scholar]
- 43.Shanafelt T D, Oreskovich M R, Dyrbye L N et al. Avoiding burnout: the personal health habits and wellness practices of US surgeons. Ann Surg. 2012;255(04):625–633. doi: 10.1097/SLA.0b013e31824b2fa0. [DOI] [PubMed] [Google Scholar]
- 44.Shanafelt T D, Mungo M, Schmitgen J et al. Longitudinal study evaluating the association between physician burnout and changes in professional work effort. Mayo Clin Proc. 2016;91(04):422–431. doi: 10.1016/j.mayocp.2016.02.001. [DOI] [PubMed] [Google Scholar]
- 45.Markit I. The Complexities of Physician Supply and Demand: Projections from 2015 to 2030 [2017 Update] https://aamc-black.global.ssl.fastly.net/production/media/filer_public/a5/c3/a5c3d565-14ec-48fb-974b-99fafaeecb00/aamc_projections_update_2017.pdf https://aamc-black.global.ssl.fastly.net/production/media/filer_public/a5/c3/a5c3d565-14ec-48fb-974b-99fafaeecb00/aamc_projections_update_2017.pdf
- 46.Kirch D G, Henderson M K, Dill M J. Physician workforce projections in an era of health care reform. Annu Rev Med. 2012;63:435–445. doi: 10.1146/annurev-med-050310-134634. [DOI] [PubMed] [Google Scholar]
- 47.Association of American Medical Colleges. 2017 State Physician Workforce Data Report. Washington, DC: AAMC; 2017 (4, 65). Available online athttps://store.aamc.org/2017-state-physician-workforce-data-report.html
- 48.Shanafelt T, Sloan J, Satele D, Balch C. Why do surgeons consider leaving practice? J Am Coll Surg. 2011;212(03):421–422. doi: 10.1016/j.jamcollsurg.2010.11.006. [DOI] [PubMed] [Google Scholar]
- 49.Aronsson G, Theorell T, Grape T et al. A systematic review including meta-analysis of work environment and burnout symptoms. BMC Public Health. 2017;17(01):264. doi: 10.1186/s12889-017-4153-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Linzer M, Konrad T R, Douglas J et al. Managed care, time pressure, and physician job satisfaction: results from the physician worklife study. J Gen Intern Med. 2000;15(07):441–450. doi: 10.1046/j.1525-1497.2000.05239.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Sinsky C, Colligan L, Li L et al. Allocation of physician time in ambulatory practice: a time and motion study in 4 specialties. Ann Intern Med. 2016;165(11):753–760. doi: 10.7326/M16-0961. [DOI] [PubMed] [Google Scholar]
- 52.Arndt B G, Beasley J W, Watkinson M D et al. Tethered to the EHR: primary care physician workload assessment using EHR event log data and time-motion observations. Ann Fam Med. 2017;15(05):419–426. doi: 10.1370/afm.2121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Shanafelt T D, Dyrbye L N, Sinsky C et al. Relationship between clerical burden and characteristics of the electronic environment with physician burnout and professional satisfaction. Mayo Clin Proc. 2016;91(07):836–848. doi: 10.1016/j.mayocp.2016.05.007. [DOI] [PubMed] [Google Scholar]
- 54.Shanafelt T D, Balch C M, Dyrbye L et al. Special report: suicidal ideation among American surgeons. Arch Surg. 2011;146(01):54–62. doi: 10.1001/archsurg.2010.292. [DOI] [PubMed] [Google Scholar]
- 55.Dyrbye L N, West C P, Sinsky C A, Goeders L E, Satele D V, Shanafelt T D. Medical licensure questions and physician reluctance to seek care for mental health conditions. Mayo Clin Proc. 2017;92(10):1486–1493. doi: 10.1016/j.mayocp.2017.06.020. [DOI] [PubMed] [Google Scholar]
- 56.Gold K J, Andrew L B, Goldman E B, Schwenk T L. “I would never want to have a mental health diagnosis on my record”: a survey of female physicians on mental health diagnosis, treatment, and reporting. Gen Hosp Psychiatry. 2016;43:51–57. doi: 10.1016/j.genhosppsych.2016.09.004. [DOI] [PubMed] [Google Scholar]
- 57.Wall M, Schenck-Gustafsson K, Minucci D, Sendén M G, Løvseth L T, Fridner A. Suicidal ideation among surgeons in Italy and Sweden - a cross-sectional study. BMC Psychol. 2014;2(01):53. doi: 10.1186/s40359-014-0053-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Dyrbye L N, Shanafelt T D, Balch C M, Satele D, Sloan J, Freischlag J. Relationship between work-home conflicts and burnout among American surgeons: a comparison by sex. Arch Surg. 2011;146(02):211–217. doi: 10.1001/archsurg.2010.310. [DOI] [PubMed] [Google Scholar]
- 59.Dyrbye L N, Sotile W, Boone S et al. A survey of U.S. physicians and their partners regarding the impact of work-home conflict. J Gen Intern Med. 2014;29(01):155–161. doi: 10.1007/s11606-013-2581-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Firth-Cozens J.Predicting stress in general practitioners: 10 year follow up postal survey BMJ 1997315(7099):34–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Shanafelt T D, Bradley K A, Wipf J E, Back A L. Burnout and self-reported patient care in an internal medicine residency program. Ann Intern Med. 2002;136(05):358–367. doi: 10.7326/0003-4819-136-5-200203050-00008. [DOI] [PubMed] [Google Scholar]
- 62.Melville A. Job satisfaction in general practice: implications for prescribing. Soc Sci Med, Med Psychol Med Sociol. 1980;14A(06):495–499. doi: 10.1016/0160-7979(80)90050-8. [DOI] [PubMed] [Google Scholar]
- 63.Grol R, Mokkink H, Smits A et al. Work satisfaction of general practitioners and the quality of patient care. Fam Pract. 1985;2(03):128–135. doi: 10.1093/fampra/2.3.128. [DOI] [PubMed] [Google Scholar]
- 64.Shanafelt T D, Noseworthy J H. Executive leadership and physician well-being: nine organizational strategies to promote engagement and reduce burnout. Mayo Clin Proc. 2017;92(01):129–146. doi: 10.1016/j.mayocp.2016.10.004. [DOI] [PubMed] [Google Scholar]
- 65.Dissanaike S. How to prevent burnout (maybe) Am J Surg. 2016;212(06):1251–1255. doi: 10.1016/j.amjsurg.2016.08.022. [DOI] [PubMed] [Google Scholar]
- 66.Dyrbye L N, Shanafelt T D, Sinky C A, Cipriano P F, Ommaya A, West C Pet al. Burnout among health care professionals: a call to explore and address this underrecognized threat to safe, high-quality care. NAM PerspectivesDiscussion Paper, National Academy of Medicine, Washington, DC,2017
- 67.Soper N J. SSAT Presidential Address 2017 “Passion and the GI Surgeon”. J Gastrointest Surg. 2018;22(01):1–7. doi: 10.1007/s11605-017-3481-3. [DOI] [PubMed] [Google Scholar]
- 68.West C P, Dyrbye L N, Erwin P J, Shanafelt T D.Interventions to prevent and reduce physician burnout: a systematic review and meta-analysis Lancet 2016388(10057):2272–2281. [DOI] [PubMed] [Google Scholar]
- 69.Shanafelt T D, West C P, Sloan J A et al. Career fit and burnout among academic faculty. Arch Intern Med. 2009;169(10):990–995. doi: 10.1001/archinternmed.2009.70. [DOI] [PubMed] [Google Scholar]
- 70.Fassiotto M, Simard C, Sandborg C, Valantine H, Raymond J. An integrated career coaching and time-banking system promoting flexibility, wellness, and success: a pilot program at Stanford University School of Medicine. Acad Med. 2018;93(06):881–887. doi: 10.1097/ACM.0000000000002121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Contratto E, Romp K, Estrada C A, Agne A, Willett L L. Physician order entry clerical support improves physician satisfaction and productivity. South Med J. 2017;110(05):363–368. doi: 10.14423/SMJ.0000000000000645. [DOI] [PubMed] [Google Scholar]
- 72.Gittell J H, Logan C, Cronenwett Jet al. Impact of relational coordination on staff and patient outcomes in outpatient surgical clinics Health Care Manage Rev 2018(e-pub ahead of print). 10.1097/HMR.0000000000000192 [DOI] [PubMed] [Google Scholar]
- 73.Gittell J H, Seidner R, Wimbush J. A relational model of how high-performance work systems work. INFORMS. 2010;21(02):311–591. [Google Scholar]
- 74.Bodenheimer T, Sinsky C. From triple to quadruple aim: care of the patient requires care of the provider. Ann Fam Med. 2014;12(06):573–576. doi: 10.1370/afm.1713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Gergen Barnett K A. In Pursuit of the fourth aim in health care: the joy of practice. Med Clin North Am. 2017;101(05):1031–1040. doi: 10.1016/j.mcna.2017.04.014. [DOI] [PubMed] [Google Scholar]
- 76.Yeo H, Viola K, Berg D et al. Attitudes, training experiences, and professional expectations of US general surgery residents: a national survey. JAMA. 2009;302(12):1301–1308. doi: 10.1001/jama.2009.1386. [DOI] [PubMed] [Google Scholar]


