Abstract
BACKGROUND:
Egypt is among the world top 10 countries in diabetes prevalence. It is the first country among the MENA region. Healthy lifestyle education and support help people with diabetes to improve health outcomes. Many physical and psychological barriers can hinder patients from following a healthy lifestyle.
AIM:
This study aimed to examine the effect of lifestyle modification educational sessions in helping Egyptian patients to overcome main barriers of diabetes self-management through improving nutritional behaviours, physical activity, medication compliance, and blood glucose monitoring.
METHODS:
A cohort study included 205 patients with type 2 diabetes. Baseline assessment of patients’ lifestyle behaviours and barriers using personal diabetes questionnaire of Louisville University, with both anthropometric and blood glucose assessment. Interventional lifestyle health education was provided weekly through multiple integrated techniques, followed by a post-intervention assessment to evaluate the effect of the health education sessions. Statistical analysis was done to identify any statistically significant difference before and after the health education intervention.
RESULTS:
There was a significant improvement of the post-education mean scores of the studied behaviours when compared with the pre-education scores of the participants’ behaviours (p < 0.001). There was also a significant reduction in the barriers facing patients to diabetes self-management including nutritional barriers (P < 0.001), medication compliance barriers (P < 0.001) with a percent change (43%), physical activity barriers (p < 0.001), and blood glucose monitoring (p < 0.001) with a percent change (44%).There was a statistically significant positive correlation between improvement of medication compliance (P = 0.027), blood glucose monitoring(P = 0.045), and glycated haemoglobin of the study participants
CONCLUSION:
lifestyle modification education of type 2 diabetic patients can overcome the main barriers of following a healthy lifestyle and improve their anthropometric measures and blood glucose level.
Keywords: Lifestyle, Barriers, Type 2 Diabetes, Health education, Egypt
Introduction
According to the International Diabetes Federation and the World Health Organization, Diabetes is recognised as a significant and growing health problem [1]. The global prevalence of diabetes among adults over 18 years of age has risen from 4.7% in 1980 to 8.5% in 2014. In 2013, 382 million adults were diagnosed with diabetes worldwide. This number is expected to grow to 592 million in 2035 [2]. In the MENA region (the Middle East & North Africa), about 40 million have diabetes (18-99 years) which is expected to be 84 million in 2045 [3]. Egypt is among the world top 10 countries with diabetes prevalence (15.6%). Furthermore, reports indicate that further 4.5 million patients are undiagnosed [2], [3]. In Egypt, annual cost analysis estimated that the economic burden of type 2 diabetes was $1.29 billion in 2010. This number excluded the cost associated with prediabetes and the cost associated with loss of productivity. This figure will be doubled by the year 2030 adjusted for inflation [4]. Type 2 diabetes is the result of excess body weight and physical inactivity. Patients with type 2 diabetes constitute around 90%-95% of all diabetic patients worldwide which represent a growing epidemic [5].
Symptoms include polyuria (excessive excretion of urine), thirst (polydipsia), constant hunger, weight loss, vision changes and fatigue [5].
Diabetes is a major cause of many complications including; blindness, kidney failure, heart attacks, stroke and lower limb amputation. In 2012, an estimated 1.5 million deaths were directly caused by diabetes, and another 2.2 million deaths were attributable to high blood glucose. People with diabetes are at increased risk of macrovascular and microvascular complications, as well as early mortality. For instance, patients with diabetes are 2 to 4 times more likely to have fatal or nonfatal coronary events or a stroke. Almost 70%-80% of patients with T2D die from 1 of these two conditions. Almost half of all deaths attributable to high blood glucose occur before the age of 70 years. WHO projects that diabetes will be the 7th leading cause of death in 2030 [2]. Diabetes is a chronic disease that requires the patient to make a multitude of daily self-management decisions and perform complex care activities. Diabetes self-management education and support help people with diabetes to navigate these decisions and activities and has been shown to improve health outcomes and prevent complications. Diabetes self-management education is the process of facilitating the knowledge, skill, and ability necessary for diabetes self-care [6]. Different members of the health care team and community can contribute to this process, it is important for health care providers to have the knowledge, resources, and a systematic referral process to ensure that patients with type 2 diabetes consistently receive their care [6]. In Egypt, although patient education is part of the Ministry of Health (MOH) hospital accreditation scheme, it is not widely implemented or unsatisfactory implemented via brief, uninformative discussions. Moreover, diabetic patients often have difficulty in following healthy lifestyles due to many barriers such as irregular working hours, food cravings, or lack of motivation to exercise. Studies revealed that diabetic patients are also prone to forget their doctor’s advice or possibly ignore it after leaving the clinic. [7]. Easy, understandable, cultural-modified health education messages should be available to the Egyptian patients in good quality to promote their health outcome, prevent complications and counteract any barriers of lifestyle modification.
The objective of this study is to examine the effect of lifestyle modification educational sessions in helping Egyptian patients to overcome main barriers of diabetes self-management through improving nutritional behaviours, physical activity, medication compliance, and blood glucose monitoring.
Study design: A cohort study of Egyptian diabetic patients. Their lifestyle behaviours and barriers were assessed with both anthropometric and blood glucose assessment.
Inclusion criteria: Patients were enrolled if they were adults over 18 years and have type 2 diabetes, belonging to the low socioeconomic village under the study.
Exclusion criteria: Patients were excluded if they are taking insulin or had severe complications.
Study setting: Patients were recruited from low socioeconomic Egyptian village from January 2017 until September 2018.
Sample Size Calculations
Using OpenEpi version 3 [8], two hundred and five adult (18-70 years) diabetic patients with an average age 52.6 years were randomly selected to achieve 95% confidence interval and 5% error with the following equation:
N: Population size
p: prevalence in the population
d: Confidence limits
Taking into consideration that the total adult population is 5000. The prevalence of diabetes is 15.6% with a 5% drop out. The study was started including a total of 205 patients, but there were 8 patients’ dropouts along the intervention period and follow up to be 197 patients at the end of the study.
Methods
Socio-demographic assessment: Updated validated a socioeconomic status scale for health research in Egypt [9] was used to assess age, sex, educational level, occupation for matching the socioeconomic data.
Assessment of nutritional behaviours, physical activity, proper medication use and level of blood glucose monitoring: Standard personal diabetes questionnaire of Louisville University with the standard scoring system [10] to assess three main parts including; the level of proper medication use and level of blood glucose monitoring.
Assessment of glycated haemoglobin and anthropometric measures were used to assess the effect of lifestyle education on the participants’ health.
- Laboratory tools to measure the blood glucose of the participants.
- Anthropometric tools: Calibrated SECA digital scale, HOLTEN stadiometer, a stretch-resistant tape was used to measure weight, height, waist and hip circumference.
Different motivational health education tools were used in this study, and the health education messages were delivered through multiple integrated techniques:
- Appropriate and culturally sensitive educational sessions.
- Written educational materials (diet plans, healthy nutrition booklet).
- Individualised health education sessions to every patient with patient-doctor consultation. Patients’ family and friends were invited to attend these sessions. Problem-solving techniques were taught to help patients to solve their problems with lifestyle modification.
- Peer education: patients who perfectly followed a healthy lifestyle were invited to teach other patients in a simple, easy way.
- Group therapy: patients were encouraged to make small teamwork groups, walk together, ensure medication compliance of each other, and psychologically support each other.
- Community committee involvement in the health education sessions ensures the sustainability of the study.
Health education site: The health education was done in an equipped room with a data show, a microphone, and a sound magnification system.
Health education schedule: The patients were divided into groups. Each group received 48 sessions (one session per week for one year). Each patient selected a regular appointment for an individualised educational session.
Health education topics include the following items:
Contents were adapted from the American Diabetes Association recommendations [11].
Educational materials were translated, simplified, modified to adapt the Egyptian diabetic patients’ culture and economic status. Health education materials were then finally reviewed and then pretested for easiness, clarity, and applicability. The main items for health education included:
- Diabetes: Definition, symptoms, types, causes, complications, and lines of treatment.
- Healthy nutrition for diabetics: The importance of diet regulation in ameliorating symptoms, and preventing complications: including healthy eating principles, and how to put it into practice recommended quantity, quality, and frequency of meals. Diet was prescribed based upon energy requirements, physical activity, and type of anti-hyperglycemic medication.
- Medication compliance: Patients were motivated to take their medication as prescribed regularly by a specialist doctor in diabetes as a part of their self-management strategy. The messages discussed the most common types of oral hypoglycemic drugs, their action in diabetes, their side effects, how to overcome these side effects.
- Blood glucose monitoring: including the importance of blood glucose monitoring compliance, types of blood glucose tests, and target levels.
- Physical activity as a part of treatment: benefits, how much, and what sort of exercise should be incorporated, and maintained. A minimum level of regular walking for 30 minutes at least five days a week was advised.
- Psychological support: how to deal with stress, and anxiety, problem-solving techniques.
- Barriers of lifestyle modification: what are the main barriers of the participants, available solutions to overcome them, how to select the most suitable solution to each patient according to his surroundings.
- Hypoglycemia, Hyperglycemia, Diabetic ketoacidosis: Causes, symptoms, and proper management.
- General health care: for the long-term complications of diabetes on health.
- Foot care: the importance of foot care, and tips to avoid diabetic foot.
- Kidney care: how to avoid diabetic nephropathy, and the importance of urine testing for microalbuminuria once a year.
- Eye care: Frequency of recommended fundus examination.
Health education package was divided so that the patient received one package each visit. The next visit included reinforcement of the previous health education package in addition to the provision of the new package. Reinforcement was performed in the form of questions to assure retention of knowledge each visit. Questions on the new health education package were also asked as a method of the baseline assessment for the patient’s knowledge about the new information covered by the next package. The following visits also covered the same questions to assess retention of knowledge, and to detect changes in attitude and practice.
Data analysis
After data cleaning, the statistical package of social sciences (SPSS-18) was used for data processing [12]. Descriptive statistics were done for data summarisation in the form of frequency, and percentage for qualitative variables, and means ± SD for quantitative variables. Scoring of the patients’ answers was done by using standard scoring of Louisville personal diabetes questionnaire scoring [10]. Inferential statistics were done for comparing the participant groups using Mcnemar test for qualitative variables and paired t-test for parametric quantitative data. With p-value < 0.05 considered significant, and p-value < 0.01 considered highly significant.
Ethical consideration: Informed consents were obtained from all participants. Approval of the research protocol was taken from the ethical committee of the National Research Centre. The research was conducted according to the World Medical Association Declaration of Helsinki [13].
Ethical approval: The Research and Ethical Committee of NRC cleared the study protocol. The number of ethical approvals was 16466
Informed consent: It was obtained from the parents enrolled in the study Confidentiality: Mothers and children were identified by a serial number, and the information at the individual level was kept strictly confidential.
Results
The present study showed that the socio-demographic characteristics of the study population were as follows: The mean age of the study participants was 52.6 years old. About 46.7% of them were men, and 53.2% were women. The majority of the participants were married (80.2%) (Table 1).
Table 1.
Sociodemographic characteristics of the study participants
| Character | Mean | SD |
|---|---|---|
| Age | 52.61 | 10.63 |
| Crowdness Index* | 1.44 | 0.75 |
| Sex | Frequency | Percent (%) |
| Male | 92 | 46.71 |
| Female | 105 | 53.29 |
| Total | 197 | 100 |
| Marital status | ||
| Single | 2 | 1.01 |
| Married | 158 | 80.22 |
| Widow | 32 | 16.24 |
| Divorced | 5 | 2.53 |
| Total | 197 | 100.0 |
| Education | ||
| Illiterate | 80 | 40.63 |
| Read & write | 25 | 12.69 |
| Primary | 17 | 8.62 |
| Preparatory | 16 | 8.12 |
| Secondary | 34 | 17.25 |
| University | 25 | 12.69 |
| Total | 197 | 100.0 |
| Occupation | ||
| Doesn’t work | 100 | 50.76 |
| Unskilled manual worker | 15 | 7.63 |
| Skilled manual worker/farmer | 30 | 15.22 |
| Have trades/ business | 8 | 4.06 |
| Semi-professional/ clerk | 25 | 12.69 |
| Professional | 19 | 9.64 |
| Total | 197 | 100.0 |
| Economic status | ||
| Doesn’t meet necessary expenses (in debt) | 67 | 34.03 |
| Only meet necessary expenses | 114 | 57.86 |
| Meet necessary expenses &emergencies | 13 | 6.59 |
| Meet necessary expenses &able to save/ invest money | 3 | 1.52 |
| Total | 197 | 100.0 |
Crowdedness index: number of individuals living in the house divided by the number of rooms.
There was an overall significant improvement in medication compliance among the study participants (P < 0.001) with a mean pre-education score (2.1 ± 1.5) versus post-education mean score (5 ± 0.15). More than 90% of the study participants seek the doctor for only medication prescription and not for health education.
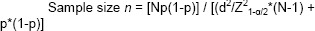
There was an overall significant reduction in barriers of medication non-compliance (< 0.001) with a percent change (43%) in post-education assessment compared to pre-education assessment (Figure 1). The reduction included absence of family support (percent change 57.8%), expensive drugs (11.5%), feeling anxious or stressed (70.8%), being busy (47.5%), feeling discouraged due to lack of results (61.8%), being away from home (25.8%), with the least barrier in reduction was unpleasant side effects with only 1.4% percent change.
Figure 1.
Comparison of pre-intervention and post-intervention score of barriers to medication compliance among the participants
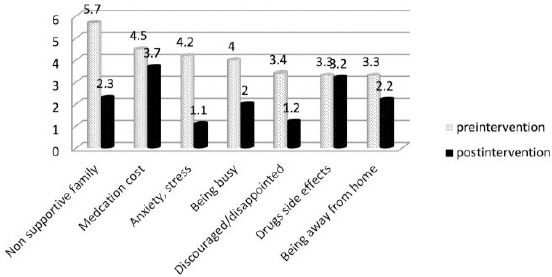
There was a major significant improvement in blood glucose monitoring (p < 0.001). There was an overall significant reduction in barriers of blood glucose monitoring (< 0.001) with a percent change (44%) in post-education assessment compared to pre-education assessment (Figure 2). The reduction includes absence of family support (percent change 67.5%), expensive drugs (15.6%), feeling anxious or stressed (71.7%), being busy (38.2%), feeling discouraged due to lack of results (46.2%), with the least two barriers in reduction were painful test (23.8%), and expensive test with only 15.6% percent change.
Figure 2.
Comparison between pre-education and post-education score of barriers of blood glucose monitoring among the participants
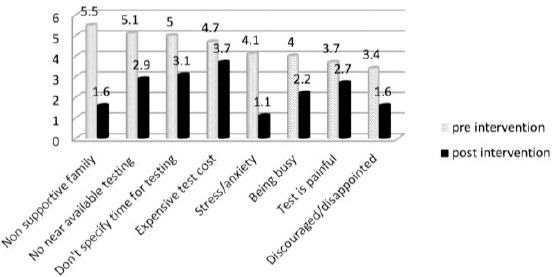
There was an overall statistically significant improvement in the healthy nutritional behaviours’ score (P < 0.001) in post-education assessment compared to pre-education assessment. The behaviour improvement included: increase using information about calories, carbohydrates, fat, using a diet plan, and resist the temptation to eat unhealthy food.
There was an overall statistically significant reduction in barriers of healthy nutritional behaviours’ score (P < 0.001) in post-education assessment compared to pre-education assessment (Figure 3).
Figure 3.
Comparison of pre-education and post-education score of barriers of healthy nutritional behaviours among the participants
There was a statistically significant increase in walking and bicycling among the participants (Table 2).
Table 2.
Comparison between pre-education and post-education physical activities among the participants
| Activity | Pre-education | Post education | P | ||
|---|---|---|---|---|---|
| Yes | No | Yes | No | ||
| Walking | 103 (52.28%) | 94 (47.72%) | 190 (96.44%) | 7 (3.56%) | < 0.001 |
| Bicycling | 5 (2.53%) | 192 (97.46%) | 20 (10.15%) | 177 (89.84) | < 0.01 |
| Going to youth sports center | 9 (4.88%) | 188 (95.12%) | 17 (8.62%) | 180 (91.37%) | 0.17 |
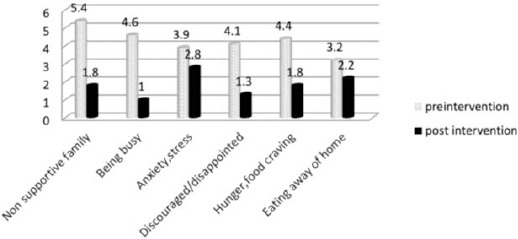
There was an overall statistically significant reduction in barriers to physical activity (Figure 4).
Figure 4.
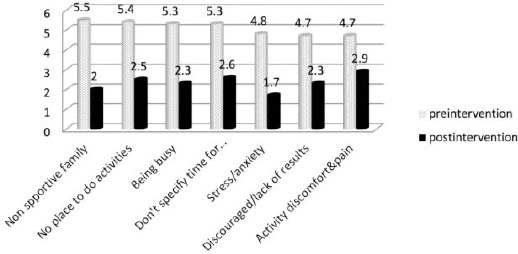
Comparison of Pre education and Post education Score of Physical Activity Barriers among the Study Participants
There was a statistically significant improvement after the lifestyle educational education; the improvement included glycated haemoglobin (HBA1C) of the patients, weight, waist, hip circumference, Waist/Hip Ratio, and BMI of the patients (Table 3).
Table 3.
Comparison between pre-education and post-education indicators (anthropometric measures and HBA1C) among the participants
| Variable | Pre education | Post education | P | Percent change (%) | ||
|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | |||
| HBA1C | 11.33 | 2.02 | 8.45 | 2.46 | < 0.001 | 25.04 |
| Weight | 94.28 | 14.87 | 79.23 | 17.38 | < 0.001 | 13.82 |
| Waist circumference | 115.58 | 12.59 | 103.26 | 21.05 | < 0.001 | 9.03 |
| Hip circumference | 118.56 | 13.96 | 102.30 | 21.58 | < 0.001 | 12.05 |
| Waist/Hip ratio | 1.02 | 0.19 | 0.97 | 0.07 | < 0.001 | 5.49 |
| BMI | 35.13 | 6.69 | 30.35 | 7.32 | < 0.001 | 11.44 |
There was a statistically significant positive correlation between improvement of medication compliance, actual blood glucose monitoring, and glycated haemoglobin of the study participants (Table 4).
Table 4.
Correlation between improvement percent of the studied behaviours and HBA1C improvement percent among the Study Participants
| Healthy nutritional behaviours | Medication compliance | blood glucose monitoring | Physical activity | ||
|---|---|---|---|---|---|
| HBA1C | Correlation coefficient | 0.155 | 0.158 | 0.143 | 0.537 |
| P value | 0.030 | 0.027 | 0.045 | < 0.001 | |
NB: Improvement percent of HBA1C means reduction in its estimated level from basal assessment
Discussion
Shared care defined as care for patients with a chronic condition provided in cooperation between primary and secondary healthcare has been promoted and developed to reduce complications [14]. It was found that 70% of diabetic patients spend 15 minutes or less with their health care providers and more than 90% of office visits of diabetic patients are delivered by health care providers without special training in diabetes management [15].
Research showed that patient-doctor communication is essential for patient compliance and satisfaction with care [16]. In the current study; however, the role of the village physicians in modifying patient’s lifestyle was deficient; their role in prescribing the diabetes medication made the majority of the current study participants seek the doctor for medication prescription which made them feel secure.
Proper compliance to medication refers to the degree or extent of conformity to the recommendations about day-to-day treatment by the provider concerning the timing, dosage, and frequency [17]. There was a significant improvement in medication compliance which is consistent with Ward study [18].
The barriers are defined as the perception of individuals toward the levels of how challenging is the diverse obstacles to the accomplishment of specific behaviour [19]. To manage diabetes effectively, individuals must utilise knowledge and decision-making skills in the context of barriers [20]. There was an overall significant reduction in barriers of medication compliance which is consistent with an American study aimed to assess the impact of medication adherence on diabetes control in Type 2 diabetic patients with the results showed significant improvement among the education group [21].
The barriers in the current study were more prominent than Cheng study which done among type 2 diabetic Chinese patients [22]. This difference may be due to lower accessibility to qualified health care service in the current study, unavailability of a diabetes monitoring program which emphasises on the importance of medication compliance and the fact that many of the study participants had no health insurance coverage.
In the current study, the best barrier in overcoming was anxiety with a significant reduction in medication noncompliance due to anxiety or stress which reflected the good effect of the psychological support delivered to the participants through problem-solving and group therapy sessions. The least barrier in overcoming was drugs’ side effects due to the resistance of the participants to change their medication or add some drugs to reduce the side effects.
The main obstacle to blood glucose monitoring in Egypt is the relatively poor structure and the process of care in government hospitals and primary health care units, as measurement of glycated haemoglobin, blood glucose level, and microalbuminuria is not performed routinely for all patients [23]. Incorporating these processes into the health system and training health care providers in the areas of information, education, and communication should be a vital cornerstone in the control of diabetes in Egypt [24].
In the current study, there was a major significant improvement in blood glucose monitoring after lifestyle educational sessions. This was similar to the results of a Korean study which was conducted to test the effects of diabetic education on blood glucose control among type 2 diabetic patients. The results indicated that patient education improved blood glucose monitoring [25].
As indicated by the prominent theories and extensive reviews, the perceived barriers are the strongest predictors of health behaviours [26], [27], [28]. Situational barriers, which arise from one’s situation in life, can directly or indirectly impede self-management activities [29].
The current study showed that there was an overall significant reduction in barriers of blood glucose monitoring in post-education assessment compared to pre-education assessment. The reduction included barriers such as the absence of family support, expensive drugs, feeling anxious or stressed, being busy, feeling discouraged due to lack of results, painful test and the least barrier in overcoming was the expensive cost of the test.
The results showed higher barriers in the current study than the Cheng study. This difference may be due to the bad socioeconomic status in the current study compared to the participants in Cheng study; they had no extra money to test their blood glucose, they considered it as a luxury among their difficult socioeconomic status.
Regarding the healthy nutritional behaviours such as using information about calories, carbohydrates and fat, there was a statistically significant improvement in mean total post-education score of the healthy nutritional behaviours. The results of the current study showed that the mean total pre-education score was slightly lower than Cheng study which showed that mean total score [19]. This difference may be because the food labels which enables the patients to know information about the food ingredients are uncommon in Egypt especially in the village under study.
Following a healthy diet plan help the patient to manage their diabetes, Ward study assessed the mean score of using a diet plan among the participants after health education sessions [18]. Its score is slightly lower than the score in the current study, which may be due to the condensed multiple integrated nutritional education in this study which provided a healthy diet plan to each participant [30].
With the help of the educational sessions in the current study, the nutritional barriers showed an overall reduction which is consistent with an English study aimed to assess the impact of the nutritional education on diabetes control [31].
There was an overall statistically significant improvement in physical activities as walking and bicycling, which is consistent with an Iranian study showed statistically significant improvement of glycemic control among the education group after lifestyle education [32].
There was no statistically significant improvement in going to the sports centre as the rural culture of the current study participants made it a shame for women and older men to go to the youth sports centre.
The results showed higher barriers in the current study than Cheng study [19]. This difference may be due to the lower degree of education among the current study participants as many of the participants are illiterate who had little idea about the importance of physical activity for control of diabetes.
In the current study, the hardest barrier to overcome was the pain and discomfort associated with physical exercise. This may be due to unavailability of qualified trainers to teach the diabetic patients how to exercise safely, and due to the presence of co-morbidities in diabetic patients which made exercise painful such as early-onset osteoarthritis of the knee, and peripheral neuropathy.
According to the WHO, nearly 70% of adults in Egypt are overweight or obese [33], which is consistent with the current study. There was a statistically significant reduction in the weight and the BMI of the participants after the health education sessions. This improvement may be because health education was afforded to the patients with different ways which make the nutritional information easy and understandable to all the participants.
The health education tools included group sessions, doctor-patient consultation, and written materials. The results of the current study are consistent with the Look ahead study, which proved that intensive lifestyle education for one year resulted in a statistically significant reduction in weight after health education [34].
Glycated haemoglobin (HBA1C) is an indicator that reflects the average plasma glucose level over the past 2 to 3 months. The HBA1C test is relatively stable and has less variability [35]. There was a statistically significant reduction in the post-education measurement than the pre-education assessment which is similar to the results found in an education study carried out on 122 diabetic patients attending diabetes outpatient clinic in Zagazig university, with a statistically significant improvement was found in their levels of glycated hemoglobin (HBA1C) after application of educational messages [36].
In the current study, there was a statistically significant positive correlation (P = 0.03) between improvement of HBA1C (reduction) and improvement of healthy nutritional behaviours. This is consistent with an Australian cohort study which stated that greater healthful food intake reduces HbA1C concentration [37]. This may be because of the effect of nutritional education supporting high fibre low glycemic diet in decreasing glycated haemoglobin and decreasing degree of obesity.
In the current study, there was a statistically significant positive correlation between improvement percent of HBA1C and improvement of medication compliance. This result is consistent with a cross-sectional study conducted in three Malaysian public health clinics, which reported that medication adherence was associated with an improved level of HbA1C [38]. This may be because medication compliance allows the diabetic patient to benefit from its active substances.
The results of the current study are consistent with the Diamond study, which revealed that continuous blood glucose monitoring effectively lowers glycated haemoglobin (HbA1C) in diabetic patients [39]. In the current study, there was a significant positive correlation between blood glucose monitoring and HBA1C which may be due to the alarming effect of health education about continuous blood glucose monitoring which results in more glycemic control.
There was also consistency in the current study with the results of a systematic review study which revealed the effectiveness of physical activity in reducing HbA1c levels [40]. This may be due to the effect of physical activity in reducing insulin resistance.
In the current study, the maximum impact of lifestyle modification education on the glycated haemoglobin was due to the improvement of physical activities, followed by medication compliance, healthy nutritional behaviours then blood glucose monitoring. These results may be due to that physical activity is the most cost-effective lifestyle modification with no specific time, place, or cost. Meanwhile, the other lifestyle modifications need a multifactorial approach to change them.
For example, nutritional modification needs an available budget to buy healthy food, available market, and accessibility to that market. Medication compliance needs the availability of medication cost, accessibility of drugs, and a good memory to remember the time of administration. Blood glucose monitoring also needs accessibility, availability of the test and its kits which is to some extent difficult in the village.
In conclusion, lifestyle education of type 2 diabetes patients counteract the barriers against following healthy nutrition, regular physical activity, medication compliance, and blood glucose monitoring behaviours which appear in the post-education assessment. It is also beneficial in improving their health status, blood glucose level, and body mass index. Health education should be an integral part of diabetes management and should be included in the Standards of Practice (SOP) of diabetes care to be implemented at all levels of health care in Egypt.
Footnotes
Funding: This research did not receive any financial support
Competing Interests: The authors have declared that no competing interests exist
References
- 1.IDF. What is diabetes? 2018. http://www..idf.org/about-diabetes/what-is-diabetes.html .
- 2.WHO. Global report on diabetes. 2016. http://apps.who.int/iris/bitstream/handle/10665/204871/9789241565257_eng.pdf;jsessionid=B62E5691D6F4101CB46AACE8CD109A74?sequence=1 .
- 3.IDF. Diabetes Atlas. 2017. https://www.idf.org/component/attachments/attachments.Html .
- 4.WHO. Diabetes programme. 2018. https://www.who.int/diabetes/en .
- 5.Powers MA, Bardsley J, Cypress M, Duker P, Funnell MM, Fischl AH, Ghandour AA. Out of pocket expenditure on non-communicable diseases among Egyptian patients. The Egyptian Journal of Hospital Medicine. 2015;31(1662):1–8. [Google Scholar]
- 6.Maryniuk MD, Siminerio L, Vivian E. Diabetes self-management education and support in type 2 diabetes: a joint position statement of the American Diabetes Association, the American Association of Diabetes Educators, and the Academy of Nutrition and Dietetics. The Diabetes Educator. 2017;43(1):40–53. doi: 10.1177/0145721716689694. https://doi.org/10.1177/0145721716689694 PMid:28118121. [DOI] [PubMed] [Google Scholar]
- 7.Abaza H, Marschollek M. SMS education for the promotion of diabetes self-management in low & middle income countries: a pilot randomized controlled trial in Egypt. BMC public health. 2017;17(1):962. doi: 10.1186/s12889-017-4973-5. https://doi.org/10.1186/s12889-017-4973-5 PMid:29258499 PMCid:PMC5735794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dean AG, Sullivan KM, Soe MM. OpenEpi: open source epidemiologic statistics for public health, version 3. 2015 [Google Scholar]
- 9.El-Gilany A, El-Wehady A, El-Wasify M. Updating and validation of the socioeconomic status scale for health research in Egypt. Eastern Mediterranean Health Journal. 2012;18:9. doi: 10.26719/2012.18.9.962. https://doi.org/10.26719/2012.18.9.962 PMid:23057390. [DOI] [PubMed] [Google Scholar]
- 10.Stetson B, Schlundt D, Rothschild C, Floyd JE, Rogers W, Mokshagundam SP. Development and validation of The Personal Diabetes Questionnaire (PDQ): a measure of diabetes self-care behaviors, perceptions and barriers. Diabetes research and clinical practice. 2011;91(3):321–32. doi: 10.1016/j.diabres.2010.12.002. https://doi.org/10.1016/j.diabres.2010.12.002 PMid:21215487. [DOI] [PubMed] [Google Scholar]
- 11.American Diabetes Association. 4. Lifestyle management: standards of medical care in diabetes-2018. Diabetes Care. 2018;41(Supplement 1):S38–50. doi: 10.2337/dc18-S004. https://doi.org/10.2337/dc18-S004 PMid:29222375. [DOI] [PubMed] [Google Scholar]
- 12.Carver RH, Nash JG. Doing data analysis with SPSS: version 18.0. Cengage Learning; 2011. [Google Scholar]
- 13.World Medical Association. World Medical Association Declaration of Helsinki. Ethical principles for medical research involving human subjects. Bulletin of the World Health Organization. 2001;79(4):373. [PMC free article] [PubMed] [Google Scholar]
- 14.Van Hateren KJ, Drion I, Kleefstra N, Groenier KH, Houweling ST, van der Meer K, Bilo HJ. A prospective observational study of quality of diabetes care in a shared care setting: trends and age differences (ZODIAC-19) BMJ open. 2012;2(4):e001387. doi: 10.1136/bmjopen-2012-001387. https://doi.org/10.1136/bmjopen-2012-001387 PMid:22936821 PMCid:PMC3432849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hasan ZU, Zia S, Maracy M. Baseline disease knowledge assessment in patients with type 2 diabetes in a rural area of northwest of Pakistan. JOURNAL-PAKISTAN MEDICAL ASSOCIATION. 2004;54(2):67–72. [PubMed] [Google Scholar]
- 16.Burroughs TE, Desikan R, Waterman BM, Gilin D, McGill J. Development and validation of the diabetes quality of life brief clinical inventory. Diabetes Spectrum. 2004;17(1):41–9. https://doi.org/10.2337/diaspect.17.1.41. [Google Scholar]
- 17.Cramer JA, Roy A, Burrell A, Fairchild CJ, Fuldeore MJ, Ollendorf DA, Wong PK. Medication compliance and persistence: terminology and definitions. Value in health. 2008;11(1):44–7. doi: 10.1111/j.1524-4733.2007.00213.x. https://doi.org/10.1111/j.1524-4733.2007.00213.x PMid:18237359. [DOI] [PubMed] [Google Scholar]
- 18.Ward JE. PHD Thesis. USA: Louisville University; 2014. Self-regulation theory and self-monitoring of blood glucose behavior in type 2 diabetes mellitus. [Google Scholar]
- 19.Cheng L, Leung DY, Wu YN, Sit JW, Yang MY, Li XM. Psychometric Properties of the Modified Personal Diabetes Questionnaire Among Chinese Patients With Type 2 Diabetes. Evaluation & the health professions. 2018;41(1):3–24. doi: 10.1177/0163278716664393. https://doi.org/10.1177/0163278716664393 PMid:27649714. [DOI] [PubMed] [Google Scholar]
- 20.Gomersall T, Madill A, Summers LK. A metasynthesis of the self-management of type 2 diabetes. Qualitative health research. 2011;21(6):853–71. doi: 10.1177/1049732311402096. https://doi.org/10.1177/1049732311402096 PMid:21429946. [DOI] [PubMed] [Google Scholar]
- 21.Buysman EK, Anderson A, Bacchus S, Ingham M. Retrospective study on the impact of adherence in achieving glycemic goals in type 2 diabetes mellitus patients receiving canagliflozin. Advances in therapy. 2017;34(4):937–53. doi: 10.1007/s12325-017-0500-4. https://doi.org/10.1007/s12325-017-0500-4 PMid:28251556. [DOI] [PubMed] [Google Scholar]
- 22.Cheng L, Sit JW, Choi KC, Chair SY, Li X, Wu Y, Long J, Tao M. Effectiveness of a patient-centred, empowerment-based intervention programme among patients with poorly controlled type 2 diabetes: A randomised controlled trial. International journal of nursing studies. 2018;79:43–51. doi: 10.1016/j.ijnurstu.2017.10.021. https://doi.org/10.1016/j.ijnurstu.2017.10.021 PMid:29149618. [DOI] [PubMed] [Google Scholar]
- 23.Fatouh NF, El-Din MN. Quality of diabetes care in family health facilities in one health district in alexandria. J Egypt Public Health Assoc. 2009;84(5-6):457–78. [PubMed] [Google Scholar]
- 24.Arafa N, Amin GE. The epidemiology of diabetes mellitus in Egypt: Results of a National Survey. The Egyptian Journal of Community Medicine. 2010;28(3):29–43. [Google Scholar]
- 25.Hyun KS, Kim KM, Jang SH. The effects of tailored diabetes education on blood glucose control and self-care. Journal of Korean Academy of Nursing. 2009;39(5):720–30. doi: 10.4040/jkan.2009.39.5.720. https://doi.org/10.4040/jkan.2009.39.5.720 PMid:19901502. [DOI] [PubMed] [Google Scholar]
- 26.Ahola AJ, Groop PH. Barriers to self?management of diabetes. Diabetic Medicine. 2013;30(4):413–20. doi: 10.1111/dme.12105. https://doi.org/10.1111/dme.12105 PMid:23278342. [DOI] [PubMed] [Google Scholar]
- 27.Nam S, Chesla C, Stotts NA, Kroon L, Janson SL. Barriers to diabetes management: patient and provider factors. Diabetes research and clinical practice. 2011;93(1):1–9. doi: 10.1016/j.diabres.2011.02.002. https://doi.org/10.1016/j.diabres.2011.02.002 PMid:21382643. [DOI] [PubMed] [Google Scholar]
- 28.Kemppainen V, Tossavainen K, Turunen H. Nurses' roles in health promotion practice: an integrative review. Health Promotion International. 2013;28(4):490–501. doi: 10.1093/heapro/das034. https://doi.org/10.1093/heapro/das034 PMid:22888155. [DOI] [PubMed] [Google Scholar]
- 29.Ho AY, Berggren I, Dahlborg-Lyckhage E. Diabetes empowerment related to Pender's Health Promotion Model: A meta?synthesis. Nursing & health sciences. 2010;12(2):259–67. doi: 10.1111/j.1442-2018.2010.00517.x. https://doi.org/10.1111/j.1442-2018.2010.00517.x PMid:20602700. [DOI] [PubMed] [Google Scholar]
- 30.Akohoue SA, Wallston KA, Schlundt DG, Rothman RL. Psychometric evaluation of the short version of the Personal Diabetes Questionnaire to assess dietary behaviors and exercise in patients with type 2 diabetes. Eating behaviors. 2017;26:182–8. doi: 10.1016/j.eatbeh.2017.04.002. https://doi.org/10.1016/j.eatbeh.2017.04.002 PMid:28456108 PMCid:PMC5715467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Palma-Duran SA, Vlassopoulos A, Lean M, Govan L, Combet E. Nutritional intervention and impact of polyphenol on glycohemoglobin (HbA1c) in non-diabetic and type 2 diabetic subjects: Systematic review and meta-analysis. Critical reviews in food science and nutrition. 2017;57(5):975–86. doi: 10.1080/10408398.2014.973932. https://doi.org/10.1080/10408398.2014.973932 PMid:25746842. [DOI] [PubMed] [Google Scholar]
- 32.Najafipour F, Mobasseri M, Yavari A, Nadrian H, Aliasgarzadeh A, Abbasi NM, Niafar M, Gharamaleki JH, Sadra V. Effect of regular exercise training on changes in HbA1c, BMI and VO2max among patients with type 2 diabetes mellitus: an 8-year trial. BMJ Open Diabetes Research and Care. 2017;5(1):e000414. doi: 10.1136/bmjdrc-2017-000414. https://doi.org/10.1136/bmjdrc-2017-000414 PMid:29177050 PMCid:PMC5687538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.WHO. Prevalence of overweight and obesity in Egypt. 2010. https://apps.who.int/infobase/Indicators.aspx .
- 34.Look AHEAD, Research Group. Long term effects of a lifestyle intervention on weight and cardiovascular risk factors in individuals with type 2 diabetes: four year results of the Look AHEAD trial. Archives of internal medicine. 2010;170(17):1566. doi: 10.1001/archinternmed.2010.334. https://doi.org/10.1001/archinternmed.2010.334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Yu Y, Ouyang XJ, Lou QL, Gu LB, Mo YZ, Ko GT, Chow CC, So WY, Ma R, Kong A, Brown N. Validity of glycated hemoglobin in screening and diagnosing type 2 diabetes mellitus in Chinese subjects. The Korean journal of internal medicine. 2012;27(1):41. doi: 10.3904/kjim.2012.27.1.41. https://doi.org/10.3904/kjim.2012.27.1.41 PMid:22403498 PMCid:PMC3295987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Abdo NM, Mohamed ME. Effectiveness of health education program for type 2 diabetes mellitus patients attending Zagazig University Diabetes Clinic, Egypt. J Egypt Public Health Assoc. 2010;85(3-4):113–30. [PubMed] [Google Scholar]
- 37.Carroll SJ, Paquet C, Howard NJ, Coffee NT, Adams RJ, Taylor AW, Niyonsenga T, Daniel M. Local descriptive body weight and dietary norms, food availability, and 10-year change in glycosylated haemoglobin in an Australian population-based biomedical cohort. BMC public health. 2017;17(1):149. doi: 10.1186/s12889-017-4068-3. https://doi.org/10.1186/s12889-017-4068-3 PMid:28148239 PMCid:PMC5289014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Chew BH, Sherina MS, Hassan NH. Association of diabetes-related distress, depression, medication adherence, and health-related quality of life with glycated hemoglobin, blood pressure, and lipids in adult patients with type 2 diabetes: a cross-sectional study. Therapeutics and clinical risk management. 2015;11:669. doi: 10.2147/TCRM.S81623. https://doi.org/10.2147/TCRM.S81623 PMid:25995640 PMCid:PMC4425326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Billings LK, Parkin CG, Price D. Baseline glycated hemoglobin values predict the magnitude of glycemic improvement in patients with type 1 and type 2 diabetes: subgroup analyses from the DIAMOND study program. Diabetes technology & therapeutics. 2018;20(8):561–5. doi: 10.1089/dia.2018.0163. https://doi.org/10.1089/dia.2018.0163 PMid:30044123 PMCid:PMC6080123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Pai LW, Li TC, Hwu YJ, Chang SC, Chen LL, Chang PY. The effectiveness of regular leisure-time physical activities on long-term glycemic control in people with type 2 diabetes: a systematic review and meta-analysis. Diabetes research and clinical practice. 2016;113:77–85. doi: 10.1016/j.diabres.2016.01.011. https://doi.org/10.1016/j.diabres.2016.01.011 PMid:26822261. [DOI] [PubMed] [Google Scholar]


