Abstract
BACKGROUND:
The number of young depressive patients approaching the primary health care centres in Saudi Arabia for supportive care and treatment has enormously increased, but more cases of depression are not being diagnosed properly at the primary health care level.
AIM:
To assess the prevalence and associated factors of depression among young adult patients attending the primary health centres in Tabuk, Kingdom of Saudi Arabia.
METHODS:
A cross-sectional study was done in selected primary health care centres in Tabuk city from March 2018 to June 2018. Patient Health Questionnaire- PHQ-2 and PHQ-9 and a modified questionnaire were used to collect the necessary information and data were analysed by using SPSS (Version 25.0, SPSS Inc. Chicago, IL, USA).
RESULTS:
The study included 384 patients aged between 20 and 40 years. Most of them (76.6%) were females. The prevalence of depression was 74%; mild among 37.8%, moderate among 20.8% whereas moderately severe to severe among 15.4% of them. Multivariate logistic regression analysis revealed that married patients were at lower risk for depression (Adjusted odds ratio “AOR” was 0.36, 95% confidence interval “CI” was 0.20-0.93), p < 0.001. Patients who reported a lack of social support were more likely to be depressed than those with social support (AOR = 2.05, 95% CI = 1.03-4.07), p = 0.041. Patients who reported disturbed marriage were at almost four-folded risk of depression compared to those without disturbed marriage (AOR = 3.50, 95% CI = 1.23-9.98), p = 0.019. Patients with financial problems were at almost double risk for developing depression compared to those without financial problems (AOR = 2.37, 95% CI = 1.16-4.85), p = 0.019. Those with stressful experience were significantly more likely to have depression compared to those without stressful experience (AOR = 4.75, 95% CI = 2.58-8.71), p < 0.001. Opposed to patients without a family history of depression, those with such history were at higher significant risk for depression (AOR = 2.75, 95% CI = 1.23-6.14), p = 0.014. Also, patients who reported sleep disorders were at nearly double folds of having depression compared to those without such disorders (AOR = 2.24, 95% CI = 1.16-4.30), p = 0.016.
CONCLUSION:
Depression among young adult patients (20-40 years) attending primary healthcare centres in Tabuk is very high. However, it is mostly mild to moderate in its severity. Suicidal thoughts were reported by one-tenth of the participants. Some predictors for depression among them were identified.
Keywords: Depression, Primary health centres Tabuk
Introduction
Mental illnesses are one of the major public health issues across the world, which affects a hundred millions of people. The concepts of westernisation, socialisation and globalisation tremendously altered the lifestyle of the population across the globe and it has become the main reason for the increase in the burden of psychiatric disorders. The mental health problems are anticipated to accounts for 14% of the disease burden worldwide [1].
Depression is one of the most common mental health problems all over the universe that disturb the physical, mental and social well-being of the population [2]. The people with depression always feel unhappy, frustrated and hopeless. Depressed persons don’t have interest in any things, and most importantly, those people have a very low self-esteem level [3]. Around 70% of the depressive patients do have somatic complaints [4].
There are multiple predisposing factors for depression that includes chronic medical condition, stress, chronic pain, family history, female gender, low income, Jobless, substance abuse, low self-esteem, lack of social support, history, being single, divorced or widow, traumatic brain injury and younger age [5]. It is projected that the burden of depression will be more by the year 2020 and it will be the second contributing disease for the global burden as measured by the Disability-adjusted life years (DALY) [6].
According to the world health report 2011 of the world health organisation, 15 % of major depressive patients are more likely to commit suicide [7]. According to 2012 Statistics, one in every twenty persons is likely to have an episode of depression across the globe [2]. In the United States, the prevalence of depression is about 9% among the general population [5], [8], [9] whereas the European countries have the prevalence rate of about 8.5% [10].
The prevalence rate of depression has sharply increased universally during the last 10 years [11], especially in developing countries, the prevalence rate even reached around 44% [12]. The Primary Health Center (PHC) is the first point of contact between the people and the health care delivery system, and the prevalence of depression is high among the patients attending the primary health centres [13]. The prevalence rate of depression among the patients in the primary health centres varies between 15-22% [14], [15].
In Saudi Arabia, the prevalence of depression among the attendees of primary health centres was estimated to be between 30 to 46% in the year 1995 [16] whereas in 2002 the prevalence rate of depression in Saudi Arabia was found to be 18% among the adult population [17]. The prevalence rate of depression among adult patients visiting the primary health centres in the United States ranges from 5 to 13% [18]. It is evident that the prevalence of depression in the kingdom of Saudi Arabia is quite high and also increase in the risk factors which can enhance the depression level such as stress, chronic diseases, sedentary lifestyle, social isolation and social stigmas in terms of psychiatric illnesses [19].
The research studies found that the causes of depression are often undiagnosed in the primary health centres and it showed that one third to one-half of the cases of depression remain undiagnosed at the primary health care level [13], [20]. World Health organisation report says that between 20 and 40 years of age, ie among the young adults the onset of major depression occurs [21]. Therefore, the current study aims to determine the prevalence of depression and its associated factors among young adult patients attending the primary health centres in Tabuk, Kingdom of Saudi Arabia.
Material and Methods
Study design: This is a cross-sectional study.
Study setting: This study was conducted in the selected primary health centres in Tabuk, Saudi Arabia.
Study Period: The study was conducted from Nov 2018 to April 2019.
Sample Size: The sample size was calculated by the Epi Info statistical program. Based on the previously published literature [33] prevalence of depression was 49.9%, at a significance level of 0.05, a design effect of 1 and confidence interval of 95% ended with a minimum sample size equal 384.
Sampling Strategy: Multistage cluster sampling was followed, and the Tabuk city will be divided into East, West, North and South administrations and the number of primary health centres was listed based on these four administrative directions. Three Primary health centres from each administrative direction were selected by using a simple random sampling technique. Patients from the selected primary health centres were enrolled in the study by using the simple random sampling technique.
Ethical permission: Ethical permission was obtained from the Research Ethics Committee, NWAFH, Tabuk, Saudi Arabia.
Inclusion criteria: Patients with the age group between 20 and 40 years at the selected primary health centre on the day of visit and agreed to participate in the study with written informed consent were included.
Exclusion criteria: Patients with special needs and patients < 20 years and > 40 years were excluded.
Potential risk: Nil.
Potential benefit: The participants were benefited by knowing their level of depression and got appropriate medical and social care.
Tools for data collection: Data related to the depression were collected by using standardised questionnaire Patient Health Questionnaire-PHQ-2, and PHQ-9 Arabic version validated questionnaires [34].
PHQ-9 is completed by the participant in a few minutes and is rapidly scored by the researcher [35]. Liu et al., [36] reported that the PHQ-9 had a good internal consistency (α = .80) and test-retest reliability (intra-class correlation coefficient = 0.87).
Scoring of PHQ-9 responses: The PHQ-9 has 9 questions with a score ranging from 0 to 3 for each setting. The following Table describes the provisional diagnoses for scoring classes [37] (Table 1).
Table 1.
Provisional diagnoses for scoring classes [37]
| PHQ-9 score | Provisional diagnosis |
| 0-4 | None |
| 5-9 | Mild depression |
| 10-14 | Moderate depression |
| 15-19 | Moderately severe depression |
| 20-27 | Severe depression |
A self-administered modified questionnaire was developed by conducting an extensive literature search from various databases and the previously published scholarly literature on depression and its risk factors among young adult patients visiting the primary health centres were identified, selected and used to frame the questionnaire.
Each patient was interviewed by using a structured questionnaire which contains information about the socio-demographic characteristics such as nationality, age, marital status, occupation, educational level, family income, type of family, crowding index, and family history of psychiatric disease. The questionnaire was framed in English, translated in Arabic (local language) and back-translated in English to check the translation.
Validity and Reliability:The questionnaire was validated by conducting a pilot study, and test-retest reliability will be done by Alpha (Cronbach’s) test reliability for internal consistency.
Data Analysis: The data analysis was carried out by using SPSS (Version 25.0, SPSS Inc. Chicago, IL, USA).
Frequency tables were used to describe the prevalence rate of depression and Socio-demographic variables. Qualitative data were summarised in percentages, and non-parametric test of significance (Chi-square test) was applied for nominal scale. Multivariate logistic regression analysis was applied to identify predictors of depression among the participants after controlling for confounders. The p-value is two-tailed and statistical significance is set at < 0.05 (Table 2 and 3).
Table 2.
Work Schedule-Gann Chart
| Research Items | Dec 2017 | Jan 2018 | Feb 2018 | Mar 2018 | Apr 2018 | May 2018 | June 2018 |
|---|---|---|---|---|---|---|---|
| Identify Research Areas | |||||||
| Formulate Research Questions | |||||||
| Formulate Research Strategy, Research Design and Research Methods | |||||||
| Literature Search | |||||||
| Write a Research Proposal | |||||||
| Finalise the Research Proposal | |||||||
| Literature Review | |||||||
| Data Collection | |||||||
| Data entry and Data Cleaning | |||||||
| Data Analysis | |||||||
| Report writing | |||||||
| Final Report Submission |
Table 3.
Budget/Funding
| S.No | Budget Items | Numbers | Cost per Item (In SAR) | Total Cost (In SAR) |
|---|---|---|---|---|
| 1 | Man power | 2 | 1000 | 2000 |
| 2 | Instruments (Print out of Questionnaires) | 4X 500 = 2000 | 1 | 2000 |
| 3 | Equipment’s (Laptop) | 1 | 1500 | 1500 |
| 4 | Consumables (Papers, pens, stapler, pins, writing pads etc) | 500 | 500 | |
| 5 | SPSS Software original version | 1 | 2000 | 2000 |
| Total Cost | 8000 |
Management Plan
Utilisation
The study results will be used to give a valid recommendation to the Ministry of health for implementing the systematic screening for depression among the young adult patients attending the primary health centres based on the prevalence rate. It also alarms the primary health care physicians and motivates them to screen the patients for depression and other psychiatric illness. Based on the statistical association between the depression and Socio-demographic variables, the awareness can be created among the patients for minimising the potential risk. The study results will also help the policymakers in proposing a new policy about mental disorders. The study results also serve as baseline data for future researchers.
Results
The study included 384 patients aged between 20 and 40 years, with 46.3% aged between 20 and 25 years. Most of them (76.6%) were females. More than half of the patients (53.1%) were singles whereas 43.2% were married. Majority of them (88.5%) were belonging to nuclear families, at least university graduated (82.8%), employed (78.7%) and having high income (> 8000 SR/month) (73.8%), Table 4.
Table 4.
Socio-demographic characteristics of the participants
| Variables | Categories | Frequency | Percentage |
|---|---|---|---|
| Gender | Male | 90 | 23.4 |
| female | 294 | 76.6 | |
| Age (years) | 20-25 | 178 | 46.3 |
| 26-30 | 64 | 16.7 | |
| 31-35 | 49 | 12.8 | |
| 36-40 | 93 | 24.2 | |
| Marital status | Single | 204 | 53.1 |
| Married | 166 | 43.2 | |
| Divorced/widowed | 14 | 3.7 | |
| Type of family | Nuclear | 340 | 88.5 |
| Joint | 44 | 11.5 | |
| Highest education qualification | High school or lower | 66 | 17.2 |
| College | 292 | 76.0 | |
| Postgraduate | 26 | 6.8 | |
| Employment | Employed | 187 | 78.7 |
| Not employed | 171 | 44.5 | |
| Housewife | 26 | 6.8 | |
| Income (SR / month)* | < 3000 | 8 | 4.3 |
| 3000-5000 | 21 | 11.2 | |
| 5001-8000 | 20 | 10.7 | |
| > 8000 | 138 | 73.8 |
For employed only (n = 187).
Habitual and social characteristics
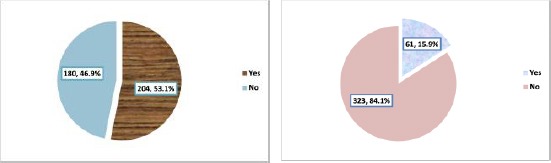
The negative experience of childhood abuse among the participants was mentioned by 28.1% of the participants as illustrated in Figure 1 (left).
Figure 1.
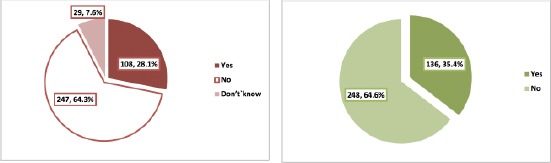
Negative experience of childhood abuse among the participants (left); Facing a lack of social support among the participants (right)
Facing a lack of social support was cited by 35.4% of the participant’s Figure 1 (right).
History of death of near relative among the participants was observed among 47.7% of the patients (Figure 2 left) whereas the history of disturbed marriage life or marital breakdown was reported among 20% of the participants Figure 2 (right).
Figure 2.
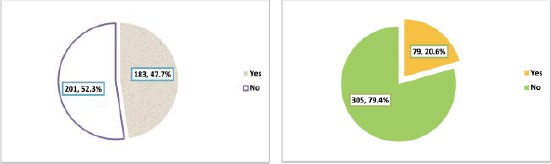
History of death of near relative among the participants (left); History of disturbed marriage life or marital breakdown among the participants (right)
History of family/neighbour quarrel was mentioned by 18.2% of the participants (Figure 3 left) whereas the history of having a financial problem was reported by 31.8% of them as shown in Figure 6)right).
Figure 3.
History of family/neighbour quarrel among the participants (left); History of having a financial problem among the participants (right)
Figure 6.
History of suicidal thoughts among the participants (left); Prevalence of depression among the participants, based on PHQ-9 (right)
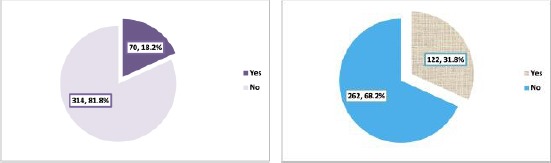
History of stressful experience was mentioned by almost half of the participants (53.1%) as displayed in Figure 4 (left). Prevalence of patients` smoking was 15.9%, Figure 4 (right).
Figure 4.
History of stressful experience among the participants (left); History of smoking among the participants (right)
Medical characteristics
Sleeping disorders were mentioned by almost one-third of the patients (36.2%) as obvious from Figure 5 (left).
Figure 5.
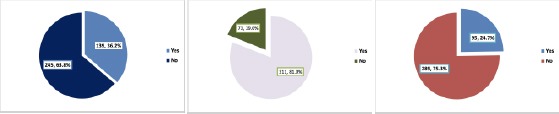
History of having sleep disorders among the participants (left); History of serious illness among the participants (middle); Family history of depression among the participants (right)
History of serious illness was mentioned by 19% of the patient’s Figure 5 (middle).
Nearly one-quarter of the participants (24.7%) had a family history of depression as seen in Figure 5 (right).
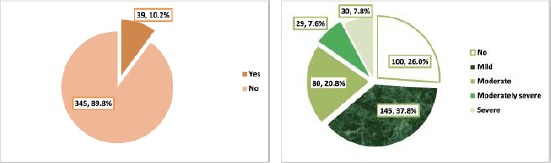
Suicidal thoughts
Suicidal thoughts were reported by 10.2% of the patients as clear from Figure 6 (left).
Prevalence of depression
From Figure 6 (right), it is shown that the prevalence of depression was 74%; mild among 37.8%, moderate among 20.8% whereas moderately severe to severe among 15.4% of them.
Socio-demographic factors
Depression was more reported among single and divorced/widowed than married patients (81.4% and 78.6% versus 64.5%) p = 0.001. Regarding the severity of depression, moderately severe was more observed among divorced/widowed patients (21.4%) compared to singles (5.9%) and married (8.4%) whereas severe depression was more reported among single patients than married (11.3% versus 4.2%), p = 0.001. Depression was significantly more observed among not employed patients compared to both employed and homemakers (81.3% versus 67.9% and 69.2%, respectively), p = 0.013. Patients` gender, age, type of family, highest qualification and income were not significantly associated with depression Table 5.
Table 5.
Socio-demographic factors associated with depression among patients attending primary healthcare centres, Tabuk
| Depression | P1 | P2 | |||||
|---|---|---|---|---|---|---|---|
| No N (%) | Mild N (%) | Moderate N (%) | Moderately severe N (%) | Severe N (%) | |||
| Gender | |||||||
| Male (n = 90) | 30 (33.3) | 33 (36.7) | 17 (18.9) | 6 (6.7) | 4 (4.4) | 0.072 | 0.345 |
| Female (n = 294) | 70 (23.8) | 112 (38.1) | 63 (21.4) | 23 (7.8) | 26 (8.8) | ||
| Age (years) | |||||||
| 20-25 (n = 178) | 46 (25.8) | 74 (41.6) | 37 (20.8) | 9 (5.1) | 12 (6.7) | 0.158 | 0.421 |
| 26-30(n = 64) | 15 (23.4) | 22 (34.4) | 14 (21.9) | 7 (10.9) | 6 (9.4) | ||
| 31-35 (n = 49) | 8 (16.3) | 16 (32.7) | 14 (28.6) | 6 (12.2) | 5 (10.2) | ||
| 36-40 (n = 93) | 31 (33.3) | 33 (35.5) | 15 (16.1) | 7 (7.5) | 7 (7.5) | ||
| Marital status | |||||||
| Single (n = 204) | 38 (18.6) | 80 (39.2) | 51 (25.0) | 12 (5.9) | 23 (11.3) | 0.001 | 0.001 |
| Married (n = 166) | 59 (35.5) | 60 (36.1) | 26 (15.7) | 14 (8.4) | 7 (4.2) | ||
| Divorced/widowed (n = 14) | 3 (21.4) | 5 (35.7) | 3 (21.4) | 3 (21.4) | 0 (0.0) | ||
| Type of family | |||||||
| Nuclear (n = 340) | 88 (25.9) | 125 (36.8) | 75 (22.1) | 25 (7.4) | 27 (7.9) | 0.743 | 0.530 |
| Joint (n = 44) | 12 (27.3) | 20 (45.5) | 5 (11.4) | 4 (9.1) | 3 (6.8) | ||
| Highest qualification | |||||||
| High school or lower (n = 66) | 18 (27.3) | 23 (34.8) | 14 (21.2) | 8 (12.1) | 3 (4.5) | 0.546 | 0.584 |
| College (n = 292) | 73 (25.0) | 113 (38.7) | 63 (21.6) | 18 (6.2) | 25 (8.6) | ||
| Postgraduate (n = 26) | 9 (34.6) | 9 (34.6) | 3 (11.5) | 3 (11.5) | 2 (7.7) | ||
| Employment | |||||||
| Employed (n = 187) | 60 (32.1) | 73 (39.0) | 29 (15.5) | 14 (7.5) | 11 (5.9) | 0.013 | 0.063 |
| Not employed (n = 171) | 32 (18.7) | 66 (38.6) | 44 (25.7) | 13 (7.6) | 16 (9.4) | ||
| House wife (n = 26) | 8 (30.8) | 6 (23.1) | 7 (26.9) | 2 (7.7) | 3 (11.5) | ||
| Income (SR / month)* | |||||||
| < 3000 (n = 8) | 1 (12.5) | 2 (25.0) | 2 (25.0) | 2 (25.0) | 1 (12.5) | 0.495 | 0.334 |
| 3000-5000 (n = 21) | 5 (23.8) | 11 (52.4) | 2 (14.3) | 2 (9.5) | 0 (0.0) | ||
| 5001-8000 (n = 20) | 7 (35.0) | 10 (50.0) | 1 (5.0) | 0 (0.0) | 2 (100) | ||
| > 8000 (n = 138) | 47 (34.1) | 49 (35.5) | 24 (17.4) | 10 (7.2) | 8 (5.8) | ||
For employed only (n = 187); P1: Depression versus non-depression; P2: Severity of depression.
Habitual and social risk factors
Histories of child abuse, lack of social support, disturbed marriage, financial problems and stressful experience were significantly associated with depression and its severity among the participants, p < 0.001. Also, the history of family/neighbour quarrel was significantly associated with depression, p = 0.001. Smoking and death of near relative were not significantly associated with depression or its severity among the participant’s Table 6.
Table 6.
Habitual and social factors associated with depression among patients attending primary healthcare centres, Tabuk
| Depression | P1 | P2 | |||||
|---|---|---|---|---|---|---|---|
| No N (%) | Mild N (%) | Moderate N (%) | Moderately severe N (%) | Severe N (%) | |||
| Smoking | |||||||
| No (n = 323) | 87 (26.9) | 120 (37.2) | 67 (20.7) | 22 (6.8) | 27 (8.4) | 0.543 | 0.359 |
| Yes (n = 61) | 13 (21.3) | 25 (41.0) | 13 (21.3) | 7 (11.5) | 3 (4.9) | ||
| Childhood abuse | |||||||
| No (n = 247) | 85 (34.4) | 103 (41.7) | 38 (15.4) | 14 (5.7) | 7 (2.8) | < 0.001 | < 0.001 |
| Yes (n = 108) | 12 (11.1) | 35 (32.5) | 32 (29.6) | 12 (11.1) | 17 (15.7) | ||
| Don`t know (n = 29) | 3 (10.3) | 7 (24.1) | 10 (34.6) | 3 (10.3) | 6 (20.7) | ||
| Lack of social support | |||||||
| No (n = 248) | 85 (34.3) | 99 (40.0) | 42 (16.9) | 11 (4.4) | 11 (4.4) | < 0.001 | < 0.001 |
| Yes (n = 136) | 15 (11.0) | 46 (33.9) | 38 (27.9) | 18 (13.2) | 19 (14.0) | ||
| Death of near relative | |||||||
| No (n = 201) | 49 (24.4) | 77 (38.3) | 40 (19.9) | 17 (8.5) | 18 (9.0) | 0.436 | 0.769 |
| Yes (n = 183) | 51 (27.9) | 68 (37.2) | 40 (21.9) | 12 (6.6) | 12 (6.6) | ||
| Disturbed marriage | |||||||
| No (n = 305) | 95 (31.1) | 114 (37.4) | 59 (19.3) | 17 (5.6) | 20 (6.6) | < 0.001 | < 0.001 |
| Yes (n = 79) | 5 (6.3) | 31 (39.2) | 21 (26.6) | 12 (15.2) | 10 (12.7) | ||
| Family/neibour quarrel | |||||||
| No (n = 314) | 93 (29.6) | 119 (37.9) | 63 (20.1) | 19 (6.1) | 20 (6.4) | 0.001 | 0.001 |
| Yes (n = 70) | 7 (10.0) | 26 (37.1) | 17 (24.3) | 10 (14.3) | 10 (14.3) | ||
| Financial problems | |||||||
| No (n = 262) | 86 (32.8) | 97 (37.0) | 48 (18.3) | 15 (5.7) | 16 (6.1) | < 0.001 | < 0.001 |
| Yes (n = 122) | 14 (11.5) | 48 (39.3) | 32 (26.2) | 14 (11.5) | 14 (11.5) | ||
| Stressful experience | |||||||
| No (n = 180) | 81 (45.0) | 70 (38.9) | 23 (12.8) | 3 (1.7) | 3 (1.7) | < 0.001 | < 0.001 |
| Yes (n = 204) | 19 (9.3) | 75 (36.8) | 57 (27.9) | 26 (12.7) | 27 (13.2) | ||
P1: Depression versus non-depression; P2: Severity of depression.
Medical risk factors
Sleep disorders and family history of depression were significantly associated with a history of depression among the patients, p < 0.001 while the history of serious illness was not significantly associated with depressions or its severity Table 7.
Table 7.
Medical factors associated with depression among patients attending primary healthcare centres, Tabuk
| Depression | P1 | P2 | |||||
|---|---|---|---|---|---|---|---|
| No N (%) | Mild N (%) | Moderate N (%) | Moderately severe N (%) | Severe N (%) | |||
| Sleep disorders | |||||||
| No (n = 245) | 83 (33.9) | 100 (40.8) | 42 (17.1) | 10 (4.1) | 10 (4.1) | < 0.001 | < 0.001 |
| Yes (n = 139) | 17 (12.2) | 45 (32.4) | 38 (27.3) | 19 (13.7) | 20 (14.4) | ||
| History of serious illness | |||||||
| No (n = 311) | 86 (27.7) | 120 (38.6) | 59 (19.0) | 23 (7.4) | 23 (7.4) | 0.138 | 0.281 |
| Yes (n = 73) | 14 (19.2) | 25 (34.2) | 21 (28.8) | 6 (8.2) | 7 (9.6) | ||
| Family history of depression | |||||||
| No (n = 289) | 91 (31.5) | 104 (36.0) | 59 (20.4) | 16 (5.5) | 19 (6.6) | < 0.001 | < 0.001 |
| Yes (n = 73) | 8 (11.0) | 34 (46.6) | 17 (23.3) | 8 (11.0) | 6 (8.2) | ||
| Don`t know (n = 22) | 1 (4.5) | 7 (31.8) | 4 (18.2) | 5 (22.7) | 5 (22.7) | ||
P1: Depression versus non-depression; P2: Severity of depression.
Suicidal thoughts
Majority of patients who had suicidal thoughts were depressed (97.4%) compared to 71.3%) of those who hadn’t suicidal thoughts, p < 0.001. Also, server depression was more reported among patients who had suicidal thoughts compared to others (43.6% versus 3.8%), p < 0.001 (Table 8).
Table 8.
Association between suicidal thoughts and depression among patients attending primary healthcare centres, Tabuk
| Depression | P1 | P2 | |||||
|---|---|---|---|---|---|---|---|
| No N (%) | Mild N (%) | Moderate N (%) | Moderately severe N (%) | Severe N (%) | |||
| Suicidal tdoughts | 99 (28.7) | 137 (39.7) | |||||
| No (n = 345) | 1 (2.6) | 8 (20.5) | 74 (21.4) | 22 (6.4) | 13 (3.8) | ||
| Yes (n = 39) | 6 (15.4) | 7 (17.9) | 17 (43.6) | < 0.001 | < 0.001 | ||
P1: Depression versus non-depress.
Predictors of depression
Compared to single patients, married patients were at lower risk for depression (Adjusted odds ratio “AOR” was 0.36, 95% confidence interval “CI” was 0.20-0.93), p < 0.001. Patients who reported a lack of social support were more likely to be depressed than those with social support (AOR = 2.05, 95% CI = 1.03-4.07), p = 0.041. Patients who reported disturbed marriage were at almost four-folded risk of depression compared to those without disturbed marriage (AOR = 3.50, 95% CI = 1.23-9.98), p = 0.019. Patients with financial problems were at almost double risk for developing depression compared to those without financial problems (AOR = 2.37, 95% CI = 1.16-4.85), p = 0.019. Those with stressful experience were significantly more likely to have depression compared to those without stressful experience (AOR = 4.75, 95% CI = 2.58-8.71), p < 0.001. Opposed to patients without a family history of depression, those with such history were at higher significant risk for depression (AOR = 2.75, 95% CI = 1.23-6.14), p = 0.014. Also, patients who reported sleep disorders were at nearly double folds of having depression compared to those without such disorders (AOR = 2.24, 95% CI = 1.16-4.30), p = 0.016. Patients` marital status, employment, family/neighbour quarrel, childhood abuse and suicidal thoughts were not significantly associated with depression Table 9.
Table 9.
Predictors of depression among patients attending primary healthcare centres, Tabuk: Results of multivariate logistic regression analysis
| B | SE | AOR | 95% CI | p-value | |
|---|---|---|---|---|---|
| Marital status | |||||
| Single (n = 204)a | 1.0 | --- | --- | ||
| Married (n = 166) | -1.021 | 0.288 | 0.36 | 0.20-0.63 | <0.001 |
| Divorced / widowed (n = 14) | -0.473 | 0.799 | 0.62 | 0.13-2.98 | 0.554 |
| Lack of social support | |||||
| No (n = 248)a | 1.0 | --- | --- | ||
| Yes (n = 136) | 0.716 | 0.351 | 2.05 | 1.03-4.07 | 0.041 |
| Disturbed marriage | |||||
| No (n = 305)a | 1.0 | --- | --- | ||
| Yes (n = 79) | 1.252 | 0.535 | 3.50 | 1.23-9.98 | 0.019 |
| Financial problems | |||||
| No (n = 262)a | 1.0 | --- | --- | ||
| Yes (n = 122) | 0.862 | 0.366 | 2.37 | 1.16-4.85 | 0.019 |
| Stressful experience | |||||
| No (n = 180)a | 1.0 | --- | --- | ||
| Yes (n = 204) | 1.557 | 0.310 | 4.75 | 2.58-8.71 | <0.001 |
| Family history of depression | |||||
| No (n = 289)a | 1.0 | --- | --- | ||
| Yes (n = 73) | 1.012 | 0.410 | 2.75 | 1.23-6.14 | 0.014 |
| Sleep disorders | |||||
| No (n = 245)a | 1.0 | --- | --- | ||
| Yes (n = 139) | 0.805 | 0.333 | 2.24 | 1.16-4.30 | 0.016 |
Reference category;B: Slop; SE: Standard error; AOR: Adjusted odds ratio; CI: Confidence interval.
Terms of employment, family/neighbour quarrel, childhood abuse and suicidal thoughts were removed from the final logistic regression model (not significant).
Discussion
Worldwide, there is growing concern about depression among adult people [38] and Saudi Arabia is not an exception. Additionally, the integration of mental health services at primary care centres in Saudi Arabia is challenging [39]. Thus, there is a need to screen patients attending primary care centres, particularly those of middle age for depression as one of the commonest psychiatric disorders which would help in providing the real situation of psychiatric disorder burden at PHC centres in Saudi Arabia.
Prevalence of depression
In the present study, the prevalence of depression among young adult patients (20-40 years) attending primary healthcare centres in Tabuk was 74%; being mild among 37.8%, moderate among 20.8% whereas moderately severe to severe among 15.4% of them. In a study carried out previously among patients attending primary health care centres in Riyadh [39], a rate of 33.4% has been reported. In a similar study carried out in Northern Province in Sri Lanka [40], the prevalence of mild depression was 13.3% whereas that of major depression was 4.5% in adult patients attending primary care settings.
Many other studies reported various figures. However, they were carried out among the general adult population. Therefore, in comparison with the present study`s figure is not logic as this study included only young adult patients (20-40 years). A systematic review and meta-analysis carried out in Saudi Arabia by Al Ibrahim et al. in 2010 found the prevalence of depression by about 41% [22]. In the pilot study done by El Rufaie et al. in Dammam, the prevalence rate of depression was 17% [23]. A preliminary prevalence study done in the Asir region of Saudi Arabia by Al Qahtani et al. conveyed a 27% prevalence of depression in the year 2008 [24]. A screening on depression was done in a family medicine clinic by Abdul Wahid et al. in southeastern Saudi Arabia relieved 12 % prevalence rate [25]. Studies were done in Riyadh by Becker et al., in primary health, centres stated that the prevalence rate of depression was 20% [26], [27]. In Kuwait, the prevalence of depression was 20.5% [28]. In Qatar, the prevalence rate of depression was 13.5% [29]. Studies conducted in European countries confirmed the prevalence rate of depression ranged between 16.5% and 22.8% [30], [31], [32].
The observed difference in the prevalence rate in various studies, including the present one could be attributed to variation in the demographic characteristics of the studied population, particularly age, variation in the background health status of the participants (healthy or patients), and application of different tools to diagnose depression in various studies as well as cultural variation between different countries.
Predictors of depression
In the present study, patients who reported a lack of social support and those who had disturbed marriage were more likely to be depressed. Other investigators around the world documented the same finding [41], [42], [43].
Patients with financial problems were at more likely to develop depression compared to those without financial problems. Richardson T et al. have documented the same finding., (2017) [44]. Also, Richardson T et al., in 2013 [45] had performed a meta-analysis and reported that 41.7 % of persons with depression were in debt, in comparison to 17.5 % who reported having no debt.
In the current study, patients with stressful experience were significantly more likely to have depression compared to those without stressful experience. In agreement with this finding, Steel Z et al., [46] observed that the population exposed to conflict and displacements were more liable to have mental health problems, particularly depression. Also, in Sri Lanka [47], stressful events after the war were associated with depressive symptoms.
Family history of depression was a significant predictor for depression among young adults in this study. Weissman MM reported that family history of depression doubles the risk for depression [48].
Patients who reported sleep disorders were at higher risk of having depression compared to those without such disorders in the present study. The same has been observed in other studies carried out oversea [49], [50].
In the present study, patients` gender was not a predictor for depression. Other studies reported the same [51], [52]. However, in a systematic review and meta-analysis carried out previously in Saudi Arabia, women were more likely to be depressed when compared to men [22]. Also, El Rufaie et al., in Dammam, observed that depression was higher among females than males [23]. In Kuwait, depression was 20.5 % and highly prevalent among women than men [28]. In Qatar [29], depression was more reported among women than men visiting primary healthcare settings. Studies conducted in European countries confirmed that women were often having mental symptoms more than men [30], [31], [32]. In Sri Lanka [40], women reported higher rates of depression compared to men.
In the present research, most socio-economic indicators such as type of family, qualification, employment status and income were not related to the development of depression. The only significant socio-economic factor associated with depression was the marital status as married adults were less likely to develop depression. In disagreement with our findings, Abdul Wahid et al. in their study in southeastern Saudi Arabia reported that the participants who lived in a flat or an individual villa were 4.8 times less likely to suffer from depression compared to the participants who lived in a room, and working participants were more likely to be depressive than the unemployed participants [25]. In Kuwait, working, highly educated, married individuals and those with three or more children were more depressed [28].
Age was not a predictor for depression in the current study. In a study carried out in Kuwait [28], young people showed a higher rate of depression. On the other hand, in Sri Lanka [40], older individuals showed a higher rate of depression. Also, in other previous studies, older age was a predictor for depression [53], [54]. It is not practical to compare results of the present study with the studies above as we included only young adults aged between 20 and 40 years while in other studies, they included all adults, this could explain the difference between findings.
Strengths and limitations
To our knowledge, this is the first study that evaluated depression among young adult patients attending primary health care setting in Tabuk and even in the whole Kingdom of Saudi Arabia. Also, knowing the magnitude and predictors of depression in such population sought care from primary care settings rather than in the general population would be more beneficial to provide targeted services and to identify those in more need for screening. However, some limitations in the present study should be mentioned. The cross-sectional nature of the study design limits the conclusion of whether risk factors lead to depression or vice-versa. The self–reported measure utilised in this study could increase the likelihood of response bias. Depending only on the PHQ-9 in the diagnosis of depression, despite its proven sensitivity and specificity is not enough, and the final diagnosis needs to be confirmed by a clinical assessment.
In conclusion, depression among young adult patients (20-40 years) attending primary healthcare centres in Tabuk is very high. However, it is mostly mild to moderate in its severity. Suicidal thoughts were reported by one-tenth of the participants. Single marital status, lack of social support, history of disturbed marriage, financial problems, stressful experience, family history of depression and sleep disturbance are predictors for depression among young adults in Tabuk.
Based on the results of the present study and their discussion, the following are recommended:
Conducting screening programs at primary healthcare settings in Tabuk to identify young adults at higher risk for depression earlier to assure better management.
Organizing community-based mental health programmes to increase awareness of the community regarding common psychosocial issues and psychosocial problems.
Training of the primary health care physicians to screen young adults for depression and manage them appropriately and refer severe cases to psychiatrists.
Proposing a new policy about mental disorders by policymakers.
A further longitudinal study is recommended in this regard
Footnotes
Funding: This research did not receive any financial support
Competing Interests: The authors have declared that no competing interests exist
References
- 1.World Health Organization. World Organization of Family Doctors. Integrating mental health into primary care: a global perspective. Geneva: World Health Organization; 2008. [Google Scholar]
- 2.WHO. Depression Fact Sheet No. 369. Geneva, Switzerland: WHO; 2012. [Accessed 23rd January 2018]. Available at: http://www.who.int/mediacentre/factsheets/fs369/en/ [Google Scholar]
- 3.Depression Overview. familydoctor.org.editorial-staff: FamilyDoctor.org. 2011. [Accessed 23rd January 2018]. Available from: http://familydoctor.org/familydoctor/en/diseases-conditions/depression.html .
- 4.Simon GE, VonKorff M, Piccinelli M, Fullerton C, Ormel J. An international study of the relation between somatic symptoms and depression. N Engl J Med. 1999;341(18):1329–1335. doi: 10.1056/NEJM199910283411801. https://doi.org/10.1056/NEJM199910283411801 PMid:10536124. [DOI] [PubMed] [Google Scholar]
- 5.Douglas M, Maurer DM, Carl R. Screening for depression. Am Fam Physician. 2012;85(2):139–144. [PubMed] [Google Scholar]
- 6.Chapman DP, Perry GS. Depression as a major component of public health for older adults. Prev Chronic Dis. 2008;5(1):A22. [PMC free article] [PubMed] [Google Scholar]
- 7.Haden A, Campanini B, editors. WHO: The World Health Report: 2001: Mental health: new understanding, new hope. Geneva: World Health Organization; 2001. p. 30. [Google Scholar]
- 8.Narrow WE, Rae DS, Robins LN, Regier DA. Revised prevalence estimates of mental disorders in the United States: using a clinical significance criterion to reconcile 2 surveys' estimates. Arch Gen Psychiatry. 2002;59(2):115–123. doi: 10.1001/archpsyc.59.2.115. https://doi.org/10.1001/archpsyc.59.2.115 PMid:11825131. [DOI] [PubMed] [Google Scholar]
- 9.Stewart WF, Ricci JA, Chee E, Hahn SR, Morganstein D. Cost of lost productive work time among US workers with depression. JAMA. 2003;289(23):3135–3144. doi: 10.1001/jama.289.23.3135. https://doi.org/10.1001/jama.289.23.3135 PMid:12813119. [DOI] [PubMed] [Google Scholar]
- 10.Ayuso-Mateos JL, Vazquez-Barquero JL, Dowrick C, Lehtinen V, Dalgard OS, Casey P, Wilkinson C, Lasa L, Page H, Dunn G, Wilkinson G. ODIN Group: Depressive disorders in Europe: prevalence figures from the ODIN study. Br J Psychiatry. 2001;179:308–316. doi: 10.1192/bjp.179.4.308. https://doi.org/10.1192/bjp.179.4.308 PMid:11581110. [DOI] [PubMed] [Google Scholar]
- 11.Andersen I, Thielen K, Bech P, Nygaard E, Diderichsen F. Increasing prevalence of depression from 2000 to 2006. Scand J Public Health. 2011;39(8):857–863. doi: 10.1177/1403494811424611. https://doi.org/10.1177/1403494811424611 PMid:21965477. [DOI] [PubMed] [Google Scholar]
- 12.Muhammad Gadit AA, Mugford G. Prevalence of depression among households in three capital cities of Pakistan. need to revise the mental health policy. PLoS One. 2007;2(2):e209. doi: 10.1371/journal.pone.0000209. https://doi.org/10.1371/journal.pone.0000209 PMid:17299589 PMCid:PMC1790700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dowrick C, Buchan I. Twelve month outcome of depression in general practice: does detection or disclosure makes a difference? BMJ. 1995;311:1274–6. doi: 10.1136/bmj.311.7015.1274. https://doi.org/10.1136/bmj.311.7015.1274 PMCid:PMC2551186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Pomerantz JM. Screening for Depression in Primary Care Medscape News. 2005. Available from: http://www.medscape.com/viewarticle/511167 .
- 15.Bethesda: Table 1: prevalence of depressive illness. Health Services/Technology Assessment Text. 3rd edition 2005. [Google Scholar]
- 16.Faris EA, Hamid AA. Hidden and conspicuous psychiatric morbidity in Saudi primary health care. Arab J Psychiatry. 1995;6(2):162–175. [Google Scholar]
- 17.Al-Khathami AD, Ogbeide DO. Prevalence of mental illness among Saudi adult primary-care patients in Central Saudi Arabia. Saudi Med J. 2002;23(6):721–724. [PubMed] [Google Scholar]
- 18.Coyne JC, Fechner-Bates S, Schwenk TL. Prevalence, nature, and comorbidity of depressive disorders in primary care. Gen Hosp Psychiatry. 1994;16(4):267–276. doi: 10.1016/0163-8343(94)90006-x. https://doi.org/10.1016/0163-8343(94)90006-X. [DOI] [PubMed] [Google Scholar]
- 19.Hidaka BH. Depression as a disease of modernity: explanations for increasing prevalence. J Affect Disord. 2012;140(3):205–214. doi: 10.1016/j.jad.2011.12.036. https://doi.org/10.1016/j.jad.2011.12.036 PMid:22244375 PMCid:PMC3330161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Leung KK, Lue BH, Lee MB, Tang LY. Screening of depression in patients with chronic medical diseases in a primary care setting. Fam Pract. 1998;15(1):67–75. doi: 10.1093/fampra/15.1.67. https://doi.org/10.1093/fampra/15.1.67 PMid:9527300. [DOI] [PubMed] [Google Scholar]
- 21.Knandeiwai S. Conquering Depression. New Delhi, India: WHO; 2001. [Google Scholar]
- 22.Alibrahim OA, Al-Sadat N, Elawad NA. Gender and risk of depression in Saudi Arabia, a systematic review and meta-analysis. J Public Health Afr. 2010;1(1):e7. doi: 10.4081/jphia.2010.e7. https://doi.org/10.4081/jphia.2010.e7 PMid:28299041 PMCid:PMC5345398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.El-Rufaie OE, Albar AA, Al-Dabal BK. Identifying anxiety and depressive disorders among primary care patients: a pilot study. Acta Psychiatr Scand. 1988;77(3):280–282. doi: 10.1111/j.1600-0447.1988.tb05121.x. https://doi.org/10.1111/j.1600-0447.1988.tb05121.x PMid:3394530. [DOI] [PubMed] [Google Scholar]
- 24.Alqahtani MM, Salmon P. Prevalence of somatization and minor psychiatric morbidity in primary healthcare in Saudi Arabia: a preliminary study in Asir region. J Family Community Med. 2008;15(1):27–33. [PMC free article] [PubMed] [Google Scholar]
- 25.Abdul Wahid HA, Al-Shahrani SI. Screening of depression among patients in family medicine in Southeastern Saudi Arabia. Saudi Med J. 2011;32(9):948–952. [PubMed] [Google Scholar]
- 26.Becker S, Al Zaid K, Al FE. Screening for somatization and depression in Saudi Arabia: a validation study of the PHQ in primary care. Int J Psychiatry Med. 2002;32(3):271–283. doi: 10.2190/XTDD-8L18-P9E0-JYRV. https://doi.org/10.2190/XTDD-8L18-P9E0-JYRV PMid:12489702. [DOI] [PubMed] [Google Scholar]
- 27.Becker SM. Detection of somatization and depression in primary care in Saudi Arabia. Soc Psychiatry Psychiatr Epidemiol. 2004;39(12):962–966. doi: 10.1007/s00127-004-0835-4. https://doi.org/10.1007/s00127-004-0835-4 PMid:15583903. [DOI] [PubMed] [Google Scholar]
- 28.Al-Otaibi B, Al-Weqayyan A, Taher H, Sarkhou E, Gloom A, Aseeri F, et al. Depressive symptoms among Kuwaiti population attending primary healthcare setting: prevalence and influence of sociodemographic factors. Med Princ Pract. 2007;16(5):384–8. doi: 10.1159/000104813. https://doi.org/10.1159/000104813 PMid:17709928. [DOI] [PubMed] [Google Scholar]
- 29.Bener A, Ghuloum S, Abou-Saleh MT. Prevalence, symptom patterns and comorbidity of anxiety and depressive disorders in primary care in Qatar. Soc Psychiatry Psychaitr Epidemiol. 2012;47(3):349–446. doi: 10.1007/s00127-011-0349-9. https://doi.org/10.1007/s00127-011-0349-9 PMid:21293844. [DOI] [PubMed] [Google Scholar]
- 30.Norton J, de Roquefeuil G, David M, Boulenger JP, Ritchie K, Mann A. Prevalence of psychiatric disorders in French general practice using the patient health questionnaire: comparison with GP case-recognition and psychotropic medication prescription. Encephale. 2009;35(6):560–9. doi: 10.1016/j.encep.2008.06.018. https://doi.org/10.1016/j.encep.2008.06.018 PMid:20004287. [DOI] [PubMed] [Google Scholar]
- 31.Stromberg R, Wernering E, Aberg-Wistedt A, Furhoff A, Johansson S, Backlund L. Screening and diagnosing depression in women visiting GPs' drop in clinic in Primary Health Care. BMC Fam Pract. 2008;9:34–43. doi: 10.1186/1471-2296-9-34. https://doi.org/10.1186/1471-2296-9-34 PMid:18554388 PMCid:PMC2442082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Mergl R, Seidscheck I, Allgaier A, Moller H, Hegerl U, Henkel V. Depressive, anxiety and somatoform disorders in primary care: prevalence and recognition. Depress Anxiety. 2007;24(3):185–95. doi: 10.1002/da.20192. https://doi.org/10.1002/da.20192 PMid:16900465. [DOI] [PubMed] [Google Scholar]
- 33.Al-Qadhi W, Ur Rahman S, Ferwana MS, Abdulmajeed IA. Adult depression screening in Saudi primary care: prevalence, instrument and cost. BMC Psychiatry. 2014;14:190. doi: 10.1186/1471-244X-14-190. https://doi.org/10.1186/1471-244X-14-190 PMid:24992932 PMCid:PMC4227058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Spitzer R, Williams J, Kroenke K. Patient health questionnaire (PHQ) screeners. Pfizer Inc. [Accessed 23rd January 2018]. Available from: http://www.phqscreeners.com .
- 35.Bartlett JE, Kotrlik JW, Higgins CC. Organizational Research: Determining Appropriate Sample Size in Survey Research. Information Technology, Learning, and Performance Journal. 2001;19(1):43–50. https://doi.org/10.5032/jae.2002.03001. [Google Scholar]
- 36.Liu SI, Yeh ZT, Huang HC, Sun FJ, Tjung JJ, Hwang LC, Shih YH, Yeh AW. Validation of Patient Health Questionnaire for depression screening among primary care patients in Taiwan. Compr Psychiatry. 2011;52(1):96–101. doi: 10.1016/j.comppsych.2010.04.013. https://doi.org/10.1016/j.comppsych.2010.04.013 PMid:21111406. [DOI] [PubMed] [Google Scholar]
- 37.Arroll B, Goodyear-Smith F, Crengle S, Gunn J, Kerse N, Fishman T, Falloon K, Hatcher S. Validation of PHQ-2 and PHQ-9 to screen for major depression in the primary care population. Ann Fam Med. 2010;8(4):348–53. doi: 10.1370/afm.1139. https://doi.org/10.1370/afm.1139 PMid:20644190 PMCid:PMC2906530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Al-Shehri SZ, Sabra AA, Taha AZ, Khamis AH, Ahmed S, Hafez AS. Depression and anxiety among males attending primary health care centers, Eastern Saudi Arabia: prevalence and predictors. Life Sci J. 2012;9:128–133. [Google Scholar]
- 39.Alghadeer SM, Alhossan AM, Al-Arifi MN, Alrabiah ZS, Ali SW, Babelghaith SD, et al. Prevalence of mental disorders among patients attending primary health care centers in the capital of Saudi Arabia. Neurosciences. 2018;23(3):238–243. doi: 10.17712/nsj.2018.3.20180058. https://doi.org/10.17712/nsj.2018.3.20180058 PMid:30008000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Senarath U, Wickramage K, Peiris SL. Prevalence of depression and its associated factors among patients attending primary care settings in the post-conflict Northern Province in Sri Lanka: a cross-sectional study. BMC Psychiatry. 2014;14:85. doi: 10.1186/1471-244X-14-85. https://doi.org/10.1186/1471-244X-14-85 PMid:24661436 PMCid:PMC3987835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Choi H, Marks NF. Marital Conflict, Depressive Symptoms, and Functional Impairment. J Marriage Fam. 2008;70(2):377–390. doi: 10.1111/j.1741-3737.2008.00488.x. https://doi.org/10.1111/j.1741-3737.2008.00488.x PMid:18698378 PMCid:PMC2507765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Thomeer MB, Umberson D, Pudrovska T. Marital Processes around Depression: A Gendered and Relational Perspective. Soc Ment Health. 2013;3(3):151–169. doi: 10.1177/2156869313487224. https://doi.org/10.1177/2156869313487224 PMid:25914855 PMCid:PMC4408555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Teo AR, Choi H, Valenstein M. Social Relationships and Depression: Ten-Year Follow-Up from a Nationally Representative Study. PLoS ONE. 2013;8(4):e62396. doi: 10.1371/journal.pone.0062396. https://doi.org/10.1371/journal.pone.0062396 PMid:23646128 PMCid:PMC3640036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Richardson T, Elliott P, Roberts R, Jansen M. A Longitudinal Study of Financial Difficulties and Mental Health in a National Sample of British Undergraduate Students. Community Ment Health J. 2017;53(3):344–352. doi: 10.1007/s10597-016-0052-0. https://doi.org/10.1007/s10597-016-0052-0 PMid:27473685 PMCid:PMC5337246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Richardson T, Elliott P, Roberts R. The relationship between personal unsecured debt and mental and physical health: A systematic review and meta-analysis. Clinical Psychology Review. 2013;33(8):1148–1162. doi: 10.1016/j.cpr.2013.08.009. https://doi.org/10.1016/j.cpr.2013.08.009 PMid:24121465. [DOI] [PubMed] [Google Scholar]
- 46.Steel Z, Chey T, Silove D, Marnane C, Bryant RA, van Ommeren M. Association of torture and other potentially traumatic events with mental health outcomes among populations exposed to mass conflict and displacement: a systematic review and meta-analysis. JAMA. 2009;302(5):537–549. doi: 10.1001/jama.2009.1132. https://doi.org/10.1001/jama.2009.1132 PMid:19654388. [DOI] [PubMed] [Google Scholar]
- 47.Husain F, Anderson M, Lopes Cardozo B, Becknell K, Blanton C, Araki D, Kottegoda Vithana E. Prevalence of war-related mental health conditions and association with displacement status in postwar Jaffna District, Sri Lanka. JAMA. 2011;306(5):522–31. doi: 10.1001/jama.2011.1052. https://doi.org/10.1001/jama.2011.1052 PMid:21813430. [DOI] [PubMed] [Google Scholar]
- 48.Weissman MM, Berry OO, Warner V, Gameroff MJ, Skipper J, Talati A, et al. A 30-Year Study of 3 Generations at High Risk and Low Risk for Depression. JAMA Psychiatry. 2016;73(9):970–7. doi: 10.1001/jamapsychiatry.2016.1586. https://doi.org/10.1001/jamapsychiatry.2016.1586 PMid:27532344 PMCid:PMC5512549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Nutt D, Wilson S, Paterson L. Sleep disorders as core symptoms of depression. Dialogues Clin Neurosci. 2008;10(3):329–336. doi: 10.31887/DCNS.2008.10.3/dnutt. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Franzen PL, Buysse DJ. Sleep disturbances and depression: risk relationships for subsequent depression and therapeutic implications. Dialogues Clin Neurosci. 2008;10(4):473–481. doi: 10.31887/DCNS.2008.10.4/plfranzen. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Siriwardhana C, Adikari A, Pannala G, Siribaddana S, Abas M, Sumathipala A, Stewart R. Prolonged internal displacement and common mental disorders in Sri Lanka: the COMRAID study. PLoS One. 2013;8(5):e64742. doi: 10.1371/journal.pone.0064742. https://doi.org/10.1371/journal.pone.0064742 PMid:23717656 PMCid:PMC3661540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Rosemann T, Backenstrass M, Joest K, Rosemann A, Szecsenyi J, Laux G. Predictors of depression in a sample of 1,021 primary care patients with osteoarthritis. Arthritis Care Res. 2007;57(3):415–422. doi: 10.1002/art.22624. https://doi.org/10.1002/art.22624 PMid:17394226. [DOI] [PubMed] [Google Scholar]
- 53.Djernes JK. Prevalence and predictors of depression in populations of elderly: a review. Acta Psychiatrica Scandinavica. 2006;113(5):372–387. doi: 10.1111/j.1600-0447.2006.00770.x. https://doi.org/10.1111/j.1600-0447.2006.00770.x PMid:16603029. [DOI] [PubMed] [Google Scholar]
- 54.Rosemann T, Backenstrass M, Joest K, Rosemann A, Szecsenyi J, Laux G. Predictors of depression in a sample of 1,021 primary care patients with osteoarthritis. Arthritis Care Res. 2007;57(3):415–422. doi: 10.1002/art.22624. https://doi.org/10.1002/art.22624 PMid:17394226. [DOI] [PubMed] [Google Scholar]


