Abstract
BACKGROUND:
Low back pain is a common presenting symptom among workers in primary health care facilities, including physicians.
AIM:
This study aimed to identify the magnitude, determinants and sequence of the problem of low back pain among physicians working at the King Salman Armed Forces hospital, Tabuk, Saudi Arabia.
METHODS:
A cross-sectional study was carried out among physicians who are working at King Salman Armed Forces Hospital, Tabuk, Saudi Arabia. A previously validated self-administered questionnaire was utilised for data collection including demographic information and data related to low back pain and its characteristics and outcome.
RESULTS:
The study included 254 physicians. Their age ranged between 23 and 66 with a mean ± SD of 36.0 ± 9.3 years. Almost two-thirds (66.9%) were males. Most of the physicians (76.4%) ever had LBP whereas 70.5% had LBP in the last 12 months. The only significant factor associated with LBP in the past 12 months was physicians` speciality as all ophthalmologists and majority of emergency physicians and anaesthesia/intensive care physicians (88.9%) compared to only 14.3% of nephrologists and neurologists expressed LBP in the last 12 months. Overall, the association between physicians’ speciality and a history of LBP in the last 12 months was statistically significant, p = 0.014. Absence from work because of LBP in the last 3 months was mentioned by 15% of physicians.
CONCLUSION:
Low back pain is a very common health problem among physicians working at the King Salman Armed Forces hospital, Saudi Arabia. A considerable proportion of them was absent from work because of LBP.
Keywords: Lower back pain, Physicians, Family Medicine
Introduction
Low back pain (LBP) is one of the most prevalent complaints that require health care. It’s the most common type of musculoskeletal disorder [1]. LBP is defined as a pain that exists below the 12th rib, and above the gluteal folds [2], it’s a symptom of diseases and not considered itself as a disease [3], [4]. LBP is the most common musculoskeletal condition that is frequently causing disability in both developing and developed countries. It was reported that about 70% to 85% of the population worldwide experience LBP at some time in their life [4].
Physicians are susceptible to twisting, bending, maintaining an awkward posture for a long time and lifting heavy loads which is all considered risk factors for musculoskeletal pains [5], several studies revealed that the prevalence of LBP among medical practitioners is higher than any other musculoskeletal symptoms [6], [7], [8]. LBP represents the main type of occupational injury especially in the healthcare field [9], [10], as it is found to be about twice more than other occupations [9]. It was reported that 18.7% of health care workers with chronic LBP were using pain-relief drugs and or analgesia [10]. Several medical specialities were found to be at high risk of LBP such as obstetrics and gynaecology, orthopaedic, nursing, operation theatre staff, and physical therapist [9].
A study was conducted in China showed that the prevalence of LBP among physicians was 44% [11]. In another study conducted in the U K, 19% of ear, nose, and throat consultants had back pain [12]. In Turkey, the lifetime prevalence of LBP among healthcare workers was determined to be 53% [13]. The lifetime prevalence of LBP among the hospital staff in Tunisia 57.7% and the annual prevalence was 51.1% [14]. The prevalence of LBP among primary healthcare professionals worldwide is 56.8%, 36.8%, 72.5%, 46%, 70.9% in Iran [15], India [16], Malaysia [17], Nigeria [18], and Kuwait [19]. In Saudi Arabia, several studies were performed regarding the prevalence of LBP among healthcare workers in different regions of the Kingdom, in Riyadh, the lifetime prevalence of back pain among all the medical practitioners was found to be 83.9% [20]. Prevalence of LBP among healthcare workers in the eastern region of Saudi Arabia was 79% [21]. While in southwestern Saudi Arabia, the prevalence of LBP among health care workers in the past 12 months was 73.9% [1].
LBP problem is associated with occupationally and personal related consequences such as; frequent absenteeism and disability [1]. The societal burden of injuries to physicians such as LBP will be borne through their productivity reducing, cost of treatment, and absence from work [5]. It was reported that LBP could lead to sick leave and activity limitation for more than 50% of health care workers [1]. Hence, this study to assess the prevalence of low back pain and its associated factors among physicians Working at King Salman Armed Forces Hospital, Tabuk, Saudi Arabia.
Methods
Study design, study setting and subjects
This was a cross-sectional questionnaire-based study conducted in Tabuk city in the north of Saudi Arabia which has a population of 910,030 (2017 census) [22]. It includes one military hospital “King Salman Armed Forces hospital” where the study was specifically conducted. It is a tertiary care hospital with 767 beds, belonging to Ministry of Defense and was opened in 1979 [23]. All physicians, from both genders, all specialities and qualifications working at the King Salman Armed Forces hospital (1440-2019) were eligible for the study (n = 512). Those physicians who have been known to have chronic or recurrent back pain were excluded from the study. Also, those who had a trauma in the back, osteoporosis, infection or neoplasm were excluded.
Data collection
A pre-designed valid questionnaire was used for data collection. It has been used previously in a study conducted in Taif by Keriri HM and proved to be valid and reliable in assessing LBP among health care workers [24]. Permission to use the questionnaire was obtained through personal communication with the author. The questionnaire included information regarding demographic data (e.g., age, sex, marital status, speciality), work-related factors (e.g., hours of work per week, type of work, duration of work in hospital etc.) as well as experience of LBP. The validity of the questionnaire scoring system was assured by three consultants in Family medicine, rheumatology and community medicine (content validity). The questionnaires were distributed by the researcher herself hand to hand to recruited physicians during their rest time. Care was taken not to disturb their clinics. They were collected within one week by the researcher also.
Sample size
The margin of error and confidence level were 5% and 99%, respectively. Likewise, the response distribution of the prevalence of back pain was 79% [21]. The minimum recommended size to meet this criterion was 237 participants. The sample was increased to 260 to compensate for drop out. The sample size was calculated using Raosoft, an open-source calculator.
Questionnaire piloting
A pilot study was done on 15 physicians of various specialities working in the same hospital. The pilot study helped to test the understanding of the participants of the questionnaires, select the relevant variables suitable for the used statistical, determine the time needed to answer the questionnaire, and give an actual situation of the main study. As a feedback, the questionnaire was clear and understandable, and tool on average took 15 minutes to be completed by physicians with LBP and less among those without LBP. Their data were included in the final report since there were non-significant changes.
Sampling technique
Stratified random sample technique with proportional allocation was adopted to select physicians from different departments of the hospital proportional to the total number of physicians in each department. Stratification will be done based on working departments.
Data management and analyses
Data were entered to a personal computer and were analysed using Statistical Package for the Social sciences (SPSS, Chicago Illinois) program version 25. Frequency distributions of responses and cross-tabulations of individual, risk job factors were studied in association with a reported prevalence of LBP. Differences and/or associations were further analysed by the chi-square test (χ2). Level of significance was determined at p < 0.05.
Ethical considerations
Approval of the regional research and ethics committee at King Salman Armed Forces hospital was obtained, and permission from the medical director of King Salman Armed Forces hospital was obtained. Written consents from all participating were obtained. All collected data were kept confidential.
Results
Baseline characteristic of participants
Baseline characteristic of participants: The study included 254 physicians. The mean age of participants was 36.0 ± 9.3 years. The males were 170 (66.9%), and the females were 84 (33.1%), (52.0%) were Saudis (Table 1).
Table 1.
Personal characteristics of the participants (n = 254)
| Frequency | Percent | |
|---|---|---|
| Gender | ||
| Male | 170 | 66.9 |
| Female | 84 | 33.1 |
| Nationality | ||
| Saudi | 132 | 52.0 |
| Non-Saudi | 122 | 48.0 |
| Marital status | ||
| Single | 70 | 27.6 |
| Married | 182 | 71.6 |
| Divorced | 2 | 0.8 |
Prevalence of LBP
As displayed from Figure 1, most of the physicians (76.4%) ever had LBP, whereas 70.5% had LBP in the last 12 months, as shown in Figure 2.
Figure 1.
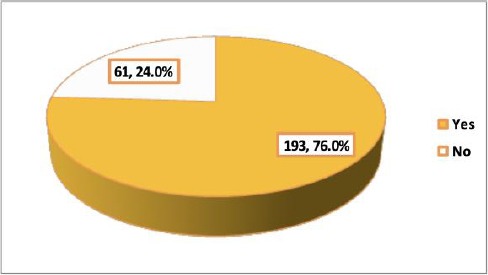
Prevalence of ever back pain among the physicians working at King Salman Armed Forces hospital, Tabuk
Figure 2.
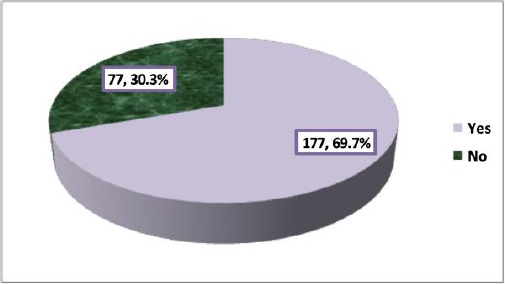
Prevalence of back pain in the last 12 months among the physicians working at King Salman Armed Forces hospital, Tabuk
Characteristics of the low back pain
In this section, responses of 193 physicians who had LBP ever were described as illustrated in Table 2. The first attack of LBP occurred within the last year among 25.9% of the physicians whereas it occurred for more than five years among 27.5% of them. Only 14% and 3.6% of the physicians had numbness and weakness in their lower limbs, respectively. In the last three months, 39.3% of the physicians had more than three attacks of LBP. Duration of the last LBP problem was less than one week among 56.5% of physicians whereas it lasted more than 5 weeks among 6.7% of them.
Table 2.
Characteristics of low back pain among the physicians working at King Salman Armed Forces hospital, Tabuk
| CategoriesFrequency (N = 193) | Percentage | ||
|---|---|---|---|
| Time of the occurrence of the first LBP | Within the last year | 50 | 25.9 |
| 1-5 years | 90 | 46.6 | |
| Since more than 5 years | 53 | 27.5 | |
| Having numbness in the lower limb | Yes | 27 | 14.0 |
| No | 166 | 86.0 | |
| Having weakness in the lower limb | Yes | 7 | 3.6 |
| No | 186 | 96.4 | |
| Frequency of LBP in the last 3 months | None | 30 | 15.5 |
| Once | 33 | 17.1 | |
| Twice | 32 | 16.6 | |
| Three times | 21 | 10.9 | |
| >three times | 77 | 39.9 | |
| Duration of the last LBP problem | 0-<1week | 109 | 56.5 |
| 1-2 weeks | 32 | 16.6 | |
| 3-4 weeks | 26 | 13.5 | |
| 4-5 weeks | 13 | 6.7 | |
| >5 weeks | 13 | 6.7 | |
| Duration of absence from work because of LBP in the last 3 months | 0 days | 164 | 85.0 |
| 1-2 days | 17 | 8.7 | |
| 3-7 days | 9 | 4.7 | |
| >7 days | 3 | 1.6 | |
| Self-rating of pain severity in the last 3 months | 0 (no pain) | 12 | 6.2 |
| 1 | 25 | 13.0 | |
| 2 | 62 | 32.1 | |
| 3 | 70 | 36.3 | |
| 4 | 18 | 9.3 | |
| 5 (very bad pain) Median | 6 | 3.1 | |
| 2 | |||
| Self-rating of experience of pain episodes in the last 3 months | 0 (never) | 21 | 10.9 |
| 1 | 38 | 19.7 | |
| 2 | 72 | 37.2 | |
| 3 | 45 | 23.3 | |
| 4 | 10 | 5.2 | |
| 5 (always) | 7 | 3.6 | |
| Median | 2 | ||
| Modalities of low back pain treatment* | Bed rest | 117 | 60.6 |
| Muscle relaxant | 74 | 38.3 | |
| Pain medication | 96 | 49.7 | |
| Physiotherapy | 30 | 15.5 | |
| Back support | 28 | 14.5 | |
Not mutually exclusive.
Absence from work because of LBP in the last 3 months was mentioned by 15% of physicians. Self-rating pain severity with moderate (median was 2 on a scale ranged between 0 and 5). In the last three months, 10.9% of physicians experience no pain, whereas 3.6% experienced continuous LBP (median was 2 on a scale ranged between 0 and 5). Regarding treatment modalities, bed rest (60.6%) and pain medication (49.7%) were the commonest reported by physicians, followed by muscle relaxants (38.3%). Physiotherapy and back support were reported by 15.5% and 14.5% of the physicians, respectively.
Pain severity among physicians with LBP
Only 10.8% of the physicians with LBP either strongly agreed or agreed that they should not do their normal work with their pain while 40.9% strongly agreed that they could do light work for an hour and 43.5% can walk for an hour. Almost one-third of them (33.7%) strongly agreed that they could do ordinary household chores and 40.3% strongly agreed that they could do the weekly shopping. Less than half of them (43.4%) strongly agreed that they could sleep at night (Table 3).
Table 3.
Response of the physicians with LBP to questions about pain severity
| Frequency | Percentage | |
|---|---|---|
| Should I not do my normal work with my present pain? | ||
| 0 (strongly disagree) | 67 | 34.8 |
| 1 | 57 | 29.5 |
| 2 | 27 | 14 |
| 3 | 21 | 10.9 |
| 4 | 8 | 4.1 |
| 5 (strongly agree) | 13 | 6.7 |
| Median | 1 | |
| Can I do light work for an hour? | ||
| 0 (strongly disagree) | 13 | 6.7 |
| 1 | 17 | 8.8 |
| 2 | 23 | 11.9 |
| 3 | 32 | 16.6 |
| 4 | 29 | 15 |
| 5 (strongly agree) | 79 | 40.9 |
| Median | 4 | |
| Can I walk for an hour? | ||
| 0 (strongly disagree) | 8 | 4.1 |
| 1 | 21 | 10.9 |
| 2 | 22 | 11.4 |
| 3 | 25 | 13 |
| 4 | 33 | 17.1 |
| 5 (strongly agree) | 84 | 43.5 |
| Median | 4 | |
| Can I do ordinary household chores? | ||
| 0 (strongly disagree) | 11 | 5.7 |
| 1 | 22 | 11.4 |
| 2 | 29 | 15 |
| 3 | 34 | 17.6 |
| 4 | 32 | 16.6 |
| 5 (strongly agree) | 65 | 33.7 |
| Median | 4 | |
| Can I do the weekly shopping? | ||
| 0 (strongly disagree) | 9 | 4.7 |
| 1 | 14 | 7.3 |
| 2 | 31 | 16.1 |
| 3 | 28 | 14.5 |
| 4 | 33 | 17.1 |
| 5 (strongly agree) | 78 | 40.3 |
| Median | 4 | |
| Can I sleep at night? | ||
| 0 (strongly disagree) | 10 | 5.2 |
| 1 | 14 | 7.3 |
| 2 | 26 | 13.5 |
| 3 | 22 | 11.4 |
| 4 | 37 | 19.2 |
| 5 (strongly agree) | 84 | 43.4 |
| Median | 4 | |
Pain intensity among physicians with LBP
Table 4 demonstrates that 14.5% of the physicians strongly disagreed that they can tolerate the pain they have without using pain medications and 15% of them strongly agreed that they could manage pain without taking pain medication. Almost one-fifth of them (19.2%) strongly agreed that pain medications provide them complete relief from pain. Only 1.6% of them strongly agreed that pain medication has no effect on relief from pain. Twenty-four physicians with LBP (12.4%) strongly agreed that an increase in pain is an indication that they should stop what they are doing until the pain decreases.
Table 4.
Response of the physicians with LBP to questions about pain intensity
| Frequency | Percentage | |
|---|---|---|
| Can I tolerate the pain I have without having to use pain medication? | ||
| 0 (strongly disagree) | 28 | 14.5 |
| 1 | 29 | 15 |
| 2 | 36 | 18.7 |
| 3 | 20 | 10.4 |
| 4 | 33 | 17 |
| 5 (strongly agree) | 47 | 24.3 |
| Median | 3 | |
| The pain is bad, but I can manage without having to take pain medication? | ||
| 0 (strongly disagree) | 39 | 20.2 |
| 1 | 44 | 22.8 |
| 2 | 31 | 16.1 |
| 3 | 19 | 9.8 |
| 4 | 31 | 16.1 |
| 5 (strongly agree) | 29 | 15 |
| Median | 2 | |
| Pain medication provides me with complete relief from pain? | ||
| 0 (strongly disagree) | 36 | 18.7 |
| 1 | 33 | 17.1 |
| 2 | 41 | 21.2 |
| 3 | 17 | 8.8 |
| 4 | 29 | 15 |
| 5 (strongly agree) | 37 | 19.2 |
| Median | 2 | |
| Pain medication provides me with moderate relief from pain? | ||
| 0 (strongly disagree) | 46 | 23.8 |
| 1 | 44 | 22.8 |
| 2 | 31 | 16.1 |
| 3 | 33 | 17.1 |
| 4 | 27 | 14 |
| 5 (strongly agree) | 12 | 6.2 |
| Median | 2 | |
| Pain medication provides me with little relief from pain? | ||
| 0 (strongly disagree) | 70 | 36.3 |
| 1 | 44 | 22.8 |
| 2 | 40 | 20.7 |
| 3 | 13 | 6.7 |
| 4 | 15 | 7.8 |
| 5 (strongly agree) | 11 | 5.7 |
| Median | 1 | |
| Does pain medication have no effect on relief from pain? | ||
| 0 (strongly disagree) | 125 | 64.8 |
| 1 | 32 | 16.6 |
| 2 | 19 | 9.8 |
| 3 | 13 | 6.7 |
| 4 | 1 | 0.5 |
| 5 (strongly agree) | 3 | 1.6 |
| Median | 0 | |
| An increase in pain is an indication that I should stop what I’m doing until the pain decreases? | ||
| 0 (strongly disagree) | 57 | 29.5 |
| 1 | 27 | 14 |
| 2 | 36 | 18.7 |
| 3 | 29 | 15 |
| 4 | 20 | 10.4 |
| 5 (strongly agree) | 24 | 12.4 |
| Median | 2 | |
Personal factors
As shown in Table 5, none of the studied personal factors (age, gender, nationality, marital status, smoking history and body mass index) was significantly associated with LBP in the last 12 months.
Table 5.
Personal factors associated with LBP among physicians in the last 12 months
| Low back pain | p-value | ||
|---|---|---|---|
| No N=77 N (%) | Yes N=177 N (%) | ||
| Gender | |||
| Male (n=170 | 55 (32.4) | 115 (67.6) | 0.315* |
| Female (n=84) | 22 (26.2) | 62 (73.8) | |
| Nationality | |||
| Saudi (n=132) | 42 (31.8) | 90 (68.2) | 0.588* |
| Non-Saudi (n=122) | 35 (28.7) | 87 (71.3) | |
| Marital status | |||
| Single (n=70) | 21 (30.0) | 49 (70.0) | 0.831* |
| Married (n=182) | 55 (30.2) | 127 (69.8) | |
| Divorced (n=2) | 1 (50.0) | 1 (50.0) | |
| Age (years) | |||
| Mean±SD | 35.3±7.9 | 36.3±9.9 | 0.451** |
| Smoking | |||
| Non-smoker (n=178) | 59 (33.1) | 119 (66.9) | 0.296* |
| Current smoker (n=56) | 14 (25.0) | 42 (75.0) | |
| Ex-smoker (n=20) | 4 (20.0) | 16 (80.0) | |
| Body mass index | |||
| Underweight (n=4) | 1 (25.0) | 3 (75.0) | 0.948* |
| Normal (n=76) | 23 (30.3) | 53 (69.7) | |
| Overweight (n=93) | 30 (32.3) | 63 (67.7) | |
| Obese (n=81) | 23 (28.4) | 58 (71.6) | |
Chi-square test;
Student`s t-test.
Work-related factors
All of ophthalmologists and majority of emergency physicians and anaesthesia / intensive care physicians (88.9%) compared to only 14.3% of nephrologists and neurologists expressed LBP in the last 12 months. Overall, the association between physicians’ speciality and a history of LBP in the last 12 months was statistically significant, p = 0.014. While, the experience of physicians, their number of working days per week and working hours per day was not statistically significant to LBP (Table 6).
Table 6.
Work-related factors associated with LBP among physicians in the last 12 months
| Low back pain | p-value* | ||
|---|---|---|---|
| No N = 77 N (%) | Yes N = 177 N (%) | ||
| Experience as physician (years) | |||
| ≤ 5 (n = 124) | 37 (29.8) | 78 (70.2) | 0.166 |
| 6-10 (n = 44) | 19 (43.2) | 25 (56.8) | |
| 11-15 (n = 33) | 9 (27.3) | 24 (72.7) | |
| > 15 (n = 53) | 12 (22.6) | 41 (77.4) | |
| Working days/week | |||
| ≤5 (n = 177) | 52 (29.4) | 125 (70.6) | 0.623 |
| >5 (n = 77) | 25 (32.5) | 52 (67.5) | |
| Working hours/day | |||
| < 8 (n = 12) | 4 (33.3) | 8 (66.7) | 0.730 |
| 8 (n = 148) | 41 (27.7) | 107 (72.3) | |
| > 8 (n=94) | 32 (34.0) | 62 (66.0) | |
| Specialty | |||
| Family medicine (n = 54) | 11 (20.4) | 43 (79.6) | 0.014 |
| Internal medicine (n = 17) | 5 (29.4) | 12 (70.7) | |
| Pediatrics (n = 25) | 5 (20.0) | 20 (80.0) | |
| General surgery (n = 25) | 9 (36.0) | 16 (64.0) | |
| Obstetrics / Gynecology (n = 25) | 9 (36.0) | 16 (64.0) | |
| Dentistry (n = 10) | 4 (40.0) | 6 (60.0) | |
| Emergency Medicine (n = 9) | 1 (11.1) | 8 (88.9) | |
| Psychiatry (n = 9) | 4 (44.4) | 5 (55.6) | |
| Orthopedics (n = 15) | 6 (40.0) | 9 (60.0) | |
| Ophthalmology (n = 4) | 0 (0.0) | 4 (100) | |
| Neurology (n = 7) | 6 (85.7) | 1 (14.3) | |
| Preventive medicine (n = 7) | 2 (28.6) | 5 (71.4) | |
| Radiology (n = 6) | 2 (33.3) | 4 (66.7) | |
| Nephrology (n = 7) | 6 (85.7) | 1 (14.3) | |
| Oncology (n = 7) | 2 (28.6) | 5 (71.4) | |
| ENT (n = 5) | 1 (20.0) | 4 (80.0) | |
| Anaesthesia/Intensive care (n=9) | 1 (11.1) | 8 (88.9) | |
| Others (n = 13) | 3 (23.1) | 10 (76.9) | |
Chi-square test.
Discussion
Most studies investigating LBP among health care professionals were carried out among nurses with few epidemiological studies have estimated the prevalence and identified associated risk factors of LBP among physicians. This study attempted to estimate the prevalence of LBP and identify its determinants among physicians working at King Salman Armed Forces hospital, Saudi Arabia. Most of the physicians in the current study (76.4%) ever had LBP, whereas 70.5% had LBP in the last 12 months. Comparable figures have been reported in another two Saudi studies carried out recently in the Eastern Region and Riyadh. In the Eastern Region, the prevalence of lifetime LBP was 67.7% among physicians whereas the rate of visiting clinics for LBP was 32.6% [21]. In Riyadh, the lifetime prevalence of LBP was 87.7% [20]. Most of the physicians with LBP (94%) had a minimal disability, 6% had moderate disability, and none of them had a severe disability. Different rates have been reported in international studies. In Turkey, LBP lifetime prevalence was 53.9% among physicians [13]. In Iran, LBP prevalence was 15.1% among physicians [25]. In another study carried out in Iran, the overall prevalence of LBP among resident physicians was 56.8% [15]. In Malaysia, the cumulative prevalence of LBP was 72.5% while the 12-months prevalence was 56.9% [17]. In Kuwait, the 12-month LBP prevalence among physicians was 13.7% [19]. The difference in the prevalence rate between various studies including the present one could be attributed to the difference in demographic and work-related characteristics of the participated nurses in these studies as well as different tools utilised in identifying LBP.
It has been documented that females are more prone to LBP than males as a result of the anatomical, physiological and structural difference between them; also the fact that mechanical disadvantage, sprain and strain, are more common in women than men [26]. However, in the current survey, there was no difference between male and female physicians regarding the prevalence of LBP. This finding agrees with what has been reported by others in Riyadh (KSA) [20], Malaysia [17] and Kuwait [26]. However, in numerous studies [13], [15], [16], [21], [27], females were more likely to have LBP compared to males.
In the present study, the higher rate of LBP was observed among ophthalmologists, emergency physicians and those specialists in anaesthesia and intensive care. This higher prevalence may be due to the greater workload places such as standing for a long time and a lot of movement among those physicians comparing to physicians in other specialities, particularly nephrology and neurology. By what has been reported in a systematic review study, smoking was not a significant predictor for LBP in the present study [22]. In another study conducted in Turkey, smoking was a statistically significant risk factor for LBP [27]. In this study, physicians` body mass index was not a predictor for LBP. In other studies, carried out among healthcare workers (nurses), overweight and obesity were associated with LBP [23], [28]. The exact mechanism underlying the association between obesity and LBP is not fully identified.
Despite the high prevalence of LBP observed in this study, the aetiology and nature of LBP are not yet well understood. Many studies have reported a strong association between musculoskeletal disorders and work-related factors [16] and work pressure [29] among health care workers, including physicians. In the present study, LBP prevalence was not associated with work-related factors, except the physicians` speciality. However, others [27], [30], [31] reported an association between long hours of work and increased risk of back pain among healthcare workers.
In the present study, about 68.4% of the participants who are complaining of pain reported that the score of pain was either 2 or 3 out of a scale of 5. However, about 12.4% reported a score of 4 or 5. Results of another Greek study showed that the pain severity ranged from moderate to intolerable in 38% of the sufferers [32]. Comparison between the two studies is difficult due to using different scales. However, severe pain, in general, affects, for sure the work productivity.
In this study, among physicians who had LBP, 10.8% reported that they could not do their normal work with their pain while 40.9% can do light work for an hour. In another Saudi study carried out in Riyadh [20], a minimal disability was observed among the majority of physicians with LBP, which means that this pain did not prevent them from performing activities of daily living. Therefore, determination of the severity of pain is very essential for those with LBP.
In the present study, 15% of physicians who had LBP reported an absence from work in the last three months because of LBP. Similarly, in a study carried out by AlMalki et al. in Riyadh [20], 13% of those who had back pain had taken days off from work. Also, in Malaysia, 7.3% of physicians reported an absence from work because of LBP [17]. LBP has been identified as one of the main causes of loss of hours and days among the healthcare workers [20]. This finding is very important as it showed that LBP could have consequences on the productivity of the affected physicians, which consequently affect the quality of care delivered to their patients.
In the current study, bed rest and pain medications were the commonest reported treatment modalities for LBP. This finding agrees with what has been reported in Riyadh [20], as most affected physicians did not seek medical help and only used simple analgesics and heat / cold fomentations as mostly LBP is a mechanical procedure. This study includes some important limitations. First of all, results may not be generalised to include physicians in other healthcare settings. Future research might include physicians working in other governmental and private health care sectors and can provide additional information. Moreover, since the design in this study was a cross-sectional, the results should be interpreted with great caution because they express only association and not causation between the risk factors and prevalence of LBP. Lastly, using a self-reported questionnaire as a study tool is subjected to recall bias.
In conclusion, this study revealed that LBP is a very common health problem among physicians working at the King Salman Armed Forces hospital, Saudi Arabia as it affected more than 70% of them in the last 12 months. This problem may negatively impact their health and economy. The possible risk factor of LBP was physicians` speciality as ophthalmologists, emergency physicians and those specialists in anaesthesia or intensive care were more likely to have LBP. This research should be extended to other Saudi hospitals to obtain a broader assessment of the LBP problem among Saudi physicians.
Footnotes
Funding: This research did not receive any financial support
Competing Interests: The authors have declared that no competing interests exist
References
- 1.Alnaami I, Awadalla NM, Alkhairy M, Alburidy S, Alqarni A, Algarni A, Alshehri R, Amrah B, Alasmari M, Mahfouz AA. Prevalence and factors associated with low back pain among health care workers in southwestern Saudi Arabia. BMC Musculoskelet Disord. 2019;20(1):56. doi: 10.1186/s12891-019-2431-5. https://doi.org/10.1186/s12891-019-2431-5 PMid:30736782 PMCid:PMC6368758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Albornoz-Cabello M, Maya-Martín J, Domínguez-Maldonado G, Espejo-Antúnez L, Heredia-Rizo AM. Effect of interferential current therapy on pain perception and disability level in subjects with chronic low back pain: a randomized controlled trial. Clin Rehabil. 2017;31:242–249. doi: 10.1177/0269215516639653. https://doi.org/10.1177/0269215516639653 PMid:26975312. [DOI] [PubMed] [Google Scholar]
- 3.Ehrlich GE. Low back pain. Bull World Health Organ. 2003;81(9):671–6. [PMC free article] [PubMed] [Google Scholar]
- 4.Kebede A, Abebe SM, Woldie H, Yenit MK. Low Back Pain and Associated Factors among Primary School Teachers in Mekele City, North Ethiopia: A Cross-Sectional Study. Occup Ther Int 2019. 2019 doi: 10.1155/2019/3862946. https://doi.org/10.1155/2019/3862946 PMid:31360145 PMCid:PMC6644225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Alsultan A, Alahmed S, Alzahrani A, Alzahrani F, Masuadi E. Comparison of musculoskeletal pain prevalence between medical and surgical specialty residents in a major hospital in Riyadh, Saudi Arabia. J Musculoskeletal Surg Res. 2018;2(4):161–6. https://doi.org/10.4103/jmsr.jmsr_36_18. [Google Scholar]
- 6.Daraiseh NM, Croninb SN, Davis LS, Shell RL, Karwowski W. Low back symptoms among hospital nurses, associations to individual factors and pain in multiple body regions. Int J IndErgon. 2010;40(1):19–24. https://doi.org/10.1016/j.ergon.2009.11.004. [Google Scholar]
- 7.Rugelj D. Low back pain and other work-related musculoskeletal problems among physiotherapists. ApplErgon. 2003;34(6):635–9. doi: 10.1016/S0003-6870(03)00059-0. https://doi.org/10.1016/S0003-6870(03)00059-0. [DOI] [PubMed] [Google Scholar]
- 8.Oude Hengel KM, Visser B, Sluiter VJ. The prevalence and incidence of musculoskeletal symptoms among hospital physicians: a systematic review. Int Arch Occup Environ Health. 2011;84(2):115–9. doi: 10.1007/s00420-010-0565-8. https://doi.org/10.1007/s00420-010-0565-8 PMid:20686782 PMCid:PMC3020318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Alzidani TH, Alturkistani AM, Alzahrani BS, Aljuhani AM, Alzahrani KM. Prevalence and risk factors of low back pain among Taif surgeons. Saudi J Health Sci. 2018;7(3):172–7. https://doi.org/10.4103/sjhs.sjhs_70_18. [Google Scholar]
- 10.Gouveia N, Rodrigues A, Ramiro S, Eusébio M, Machado PM, Canhão H, Branco JC. The Use of Analgesic and Other Pain?Relief Drugs to Manage Chronic Low Back Pain: Results from a National Survey. Pain Pract. 2017;17(3):353–365. doi: 10.1111/papr.12455. https://doi.org/10.1111/papr.12455 PMid:27206719. [DOI] [PubMed] [Google Scholar]
- 11.Smith DR, Wei N, Zhang Y, Wang R. Musculoskeletal complaints and psychosocial risk factors among physicians in mainland China. Int J IndErgon. 2006;36(6):599–603. https://doi.org/10.1016/j.ergon.2006.01.014. [Google Scholar]
- 12.Babar-Craig H, Banfield G, Knight J. Prevalence of back and neck pain amongst ENT consultants: national survey. J LaryngolOtol. 2003;117(12):979–982. doi: 10.1258/002221503322683885. https://doi.org/10.1258/002221503322683885 PMid:14738610. [DOI] [PubMed] [Google Scholar]
- 13.Simsek S, agci N, Senol H. Prevalence and Risk Factors of Low Back Pain among Health-care Workers in Denizli. Agri - J Turkish SocAlgol. 2017;29:71–78. doi: 10.5505/agri.2017.32549. https://doi.org/10.5505/agri.2017.32549 PMid:28895982. [DOI] [PubMed] [Google Scholar]
- 14.Bejia I, Younes M, Jamila HB, Khalfallah T, Salem KB, Touzi M, Akrout M, Bergaoui N. Prevalence and factors associated to low back pain among hospital staff. Joint Bone Spine. 2005;72(3):254–9. doi: 10.1016/j.jbspin.2004.06.001. https://doi.org/10.1016/j.jbspin.2004.06.001 PMid:15850998. [DOI] [PubMed] [Google Scholar]
- 15.SHAMS VAHDATI S, SARKHOSH KHIAVI R, RAJAEI GHAFOURI R, ADIMI I. Evaluation of Prevalence of Low Back Pain Among Residents of Tabriz University of Medical Sciences in Relation with Their Position in Work. Turkish J Emerg Med. 2014;14:125–129. doi: 10.5505/1304.7361.2014.79106. https://doi.org/10.5505/1304.7361.2014.79106 PMid:27331182 PMCid:PMC4909944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Alam A. Prevalence of Low Back Pain and Its Associated Risk Factors among Doctors in Surat. Prevalence of Low Back Pain and Its Associated Risk Factors among Doctors in Surat. European Journal of Preventive Medicine. 2015;3(6):188–192. https://doi.org/10.11648/j.ejpm.20150306.15. [Google Scholar]
- 17.Wong TS, Teo N, Kyaw M. Prevalence and risk factors associated with low back among health care providers in a District Hospital. Malaysian Orthopaedic Journal. 2010;4(2):23–8. https://doi.org/10.5704/MOJ.1007.004. [Google Scholar]
- 18.Omokhodion FO, Umar US, Ogunnowo BE. Prevalence of Low Back Pain among Staff in a Rural Hospital in Nigeria. Occup Med. 2000;50:107–110. doi: 10.1093/occmed/50.2.107. https://doi.org/10.1093/occmed/50.2.107 PMid:10829430. [DOI] [PubMed] [Google Scholar]
- 19.Landry MD, Raman SR, Sulway C, Golightly YM, Hamdan E. Prevalence and Risk Factors Associated With Low Back Pain Among Health Care Providers in a Kuwait Hospital. Spine. 2008;33:539–545. doi: 10.1097/BRS.0b013e3181657df7. https://doi.org/10.1097/BRS.0b013e3181657df7 PMid:18317200. [DOI] [PubMed] [Google Scholar]
- 20.Almalki M, Alkhudhayri M, Batarfi A, Alrumaihi S, Alshehri S, Aleissa S, et al. Prevalence of low back pain among medical practitioners in a tertiary care hospital in Riyadh. Saudi J Sport Med. 2016;16:205. https://doi.org/10.4103/1319-6308.187556. [Google Scholar]
- 21.Al Bahrani A, Al Huwaykim M, Al Kuwaiti A, Alalwi M, Al Dulaim H, Al Mazeedi T, et al. Prevalence of Low Back Pain in Healthcare Workers in Eastern Region in Saudi Arabia. Int J Sci Res. 2015:6. [Google Scholar]
- 22.Leboeuf-Yde C. Smoking and low back pain. A systematic literature review of 41 journal articles reporting 47 epidemiologic studies. Spine. 1999;24:1463–70. doi: 10.1097/00007632-199907150-00012. https://doi.org/10.1097/00007632-199907150-00012 PMid:10423792. [DOI] [PubMed] [Google Scholar]
- 23.El-Najjar A, Hassan A, Abou El-Soud A, El-Fattah N. Prevalence of low back pain in working nurses in Zagazig University Hospitals: an epidemiological study. Egypt Rheumatol Rehabil. 2014;41:109. https://doi.org/10.4103/1110-161X.140525. [Google Scholar]
- 24.Keriri HM. Prevalence and Risk Factors of Low Back Pain Among Nurses in Operating Rooms, Taif, Saudi Arabia. J Med Sci Res. 2013;4:3. https://doi.org/10.5958/j.2321-5798.4.1.001. [Google Scholar]
- 25.Mehrdad R, Dennerlein JT, Morshedizadeh M. Musculoskeletal disorders and ergonomic hazards among Iranian physicians. Arch Iran Med. 2012;15:370–4. [PubMed] [Google Scholar]
- 26.Wáng YXJ, Wáng J-Q, Káplár Z. Increased low back pain prevalence in females than in males after menopause age: evidences based on synthetic literature review. Quant Imaging Med Surg. 2016;6:199–206. doi: 10.21037/qims.2016.04.06. https://doi.org/10.21037/qims.2016.04.06 PMid:27190772 PMCid:PMC4858456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Karahan A, Kav S, Abbasoglu A, Dogan N. Low back pain: prevalence and associated risk factors among hospital staff. J Adv Nurs. 2009;65:516–524. doi: 10.1111/j.1365-2648.2008.04905.x. https://doi.org/10.1111/j.1365-2648.2008.04905.x PMid:19222649. [DOI] [PubMed] [Google Scholar]
- 28.Asadi P, Monsef Kasmaei V, Zia Ziabari SM, Zohrevandi B. The prevalence of low back pain among nurses working in Poursina hospital in Rasht, Iran. J Emerg Pract Trauma. 2015;2:11–15. https://doi.org/10.15171/jept.2015.01. [Google Scholar]
- 29.Ndejjo R, Musinguzi G, Yu X, Buregyeya E, Musoke D, Wang J-S, et al. Occupational Health Hazards among Healthcare Workers in Kampala, Uganda. J Environ Public Health. 2015;2015:1–9. doi: 10.1155/2015/913741. https://doi.org/10.1155/2015/913741 PMid:25802531 PMCid:PMC4329737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Heuch I, Heuch I, Hagen K, Zwart J-A. Physical activity level at work and risk of chronic low back pain: A follow-up in the Nord-Trøndelag Health Study. PLoS One. 2017;12:e0175086. doi: 10.1371/journal.pone.0175086. https://doi.org/10.1371/journal.pone.0175086 PMid:28394896 PMCid:PMC5386240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Trinkoff AM, Le R, Geiger-Brown J, Lipscomb J, Lang G. Longitudinal relationship of work hours, mandatory overtime, and on-call to musculoskeletal problems in nurses. Am J Ind Med. 2006;49:964–971. doi: 10.1002/ajim.20330. https://doi.org/10.1002/ajim.20330 PMid:16691609. [DOI] [PubMed] [Google Scholar]
- 32.Spyropoulos P, Papathanasiou G, Georgoudis G, Chronopoulos E, Koutis H, Koumoutsou F. Prevalence of low back pain in greek public office workers. Pain Physician. 2007;10:651–9. [PubMed] [Google Scholar]


