Abstract
BACKGROUND:
Language acquisition and child development during the early years of life depend on multiple interacting factors.
AIM:
To explore potential factors that can impact language development in 2 groups of Egyptian children, one with normal language development and the second with delayed development. Also, to explore to what extent can the involvement of impaired motor development potentiate the risk of developmental language delay.
METHODS:
This cross-sectional case-control study involved Egyptian children belonging to the middle socioeconomic class between 18 and 36 months of age. Children were classified according to their performance on language domain of Bayley Scales of Infant and Toddler Development (Bayley-III) into two groups, infants with the average or above score (control group) and those having below-average scores (cases). Motor development was assessed on the same scale. Factors affecting language development were tested, including socio-demographic, obstetric, and maternal medical factors in addition to Infant Feeding Practices.
RESULTS:
The independent factors lowering the language scores were early introduction of complementary food, low family income, history of delivery problems, pregnancy-related diseases of the mother, and maternal education. Impaired motor development appears as a further highly significant risk factor to the previously mentioned factors
CONCLUSION:
In Egyptian children, delayed language development is severely affected by the interaction of medical, social and nutritional factors. Providing adequate maternal health care during pregnancy and childbirth, regular developmental monitoring at each child visit, and screening for such risk factors, can reduce size of the problem and promote child’s social and psychological development.
Keywords: Language development, Motor development, children, Risk factors
Introduction
Language development is an essential part of a child’s overall development. It builds the child’s ability to communicate, express and perceive feelings. It also promotes thinking, problem-solving, and enhancing and maintaining relationships [1]. A child’s early years of language development are crucial for the basis of school readiness, such as literacy skills, social and psychological growth [2].
Children develop receptive and expressive language skills at varying rates. The term Developmental language delay (DLD) or late talker is used to identify children aged 18-36 months who fail to attain the least expressive vocabulary milestones expected for their age and sex [3].
The prevalence of communication disorders in the international literature varies according to the age of affected children and methods of assessment. It was found that 61% of 24-months old children display expressive speech disorders [4], [5]. Developmental language disorder (DLD) comprising the largest disability group in pre-school-aged children. Approximately 7% of the population is expected to have DLD [6]. Egyptian studies concerned with the prevalence of communication disorders are infrequent [7], [8]. Gharib et al. recorded that prevalence of confirmed delayed language development (DLD) in the Egyptian sample was 6.4% [8]. Unnoticed and unmanaged impaired language development can have a significant serious effect on a child’s development, affecting educational, social, and psychological progress [9]. Academic difficulties, learning disabilities [10], shyness and social difficulties, anxiety disorder, behavioural problems [11], [12], [13] and ADHD [14] are common detrimental consequences.
Acquisition of early motor skills is known to enhance the child’s cognitive, language and social development. However, the positive association between motor and language development has been considerably investigated [6], [15], [16]. Libertus and Violi et al., have found that the onset of independent sitting may initiate a developmental cascade that results in increased language learning opportunities [17]. On the other hand, a link between motor impairment and language impairment has been proved [18], [19]. The presence of subtle motor impairment may explain the unresponsiveness of children with language impairment to speech therapy.
Language development is also influenced by other factors. Environmental factors as perinatal problems, poor socioeconomic conditions, lack of parental interaction and improper nutrition may precipitate delay in all developmental domains, including language domain [8]. Speech and language delay may be symptoms of a global developmental disorder such as autistic spectrum disorder, or a genetic disorder as Down syndrome or may be an indicator of hearing impairment. The tendency to speech and language disorders is mostly believed to be multifactorial, involving complex interactions between some common genetic variants and environmental factors [20].
Screening procedures and regular surveillance to recognise factors affecting infant development are crucial for early detection of potential developmental delays and hence, choosing proper management approaches. Therefore, the purposes of the present study were:
- To investigate a group of Egyptian infants for potential risk factors that can influence language development as socioeconomic factors, nutritional factors and perinatal maternal and infant medical conditions.
- To estimate the proportion of infants with subtle motor impairment among a group of infants presented with language impairment and among another matched group with normal language development
- To explore to what extent can the involvement of impaired motor development potentiate the risk of developmental language impairment.
Subjects and Methods
Study design and setting
This cross-sectional case-control study involved male and female Egyptian children aged from 18 to 36 months. They were recruited from Developmental and Behavioral Paediatrics Clinic at the National Research Centre (NRC) and the Pediatrics Outpatient Clinic of Ain Shams University (ASU) in the period from September 2016 to September 2018. A child was enrolled if he belonged to the middle socioeconomic class, the parents’ main complaint was the child’s delayed speech, and if they consented to participate in the study. Children were excluded if they demonstrated any obvious congenital anomalies, features of genetic diseases, or had a history of any metabolic or physical problems.
Sample Size
Previous research had found that delayed motor milestones were documented in about 70% of children with developmental language impairment (LI) and only in 22% of the control children [21].
In this study, it was planned to use two-sided confidence intervals for the difference in proportions to calculate sample size. The used confidence interval method was the Yates chi-square simple asymptotic method with continuity correction (Newcombe, 1998) [22]. The proportion estimates to be used 0.70 for Group 1, and 0.22 for Group 2.
Calculated group sample sizes of 353 (to be rounded to 360) for group 1 and of 293 (To be rounded to 295) for group 2 produce a two-sided 85% confidence interval for the difference in population proportions with a width that is equal to 0.100
Subjects
Enrolled children were classified according to their performance on language domain of Bayley Scales of Infant and Toddler Development (Bayley-III) into two groups: infants having a below-average composite score (impaired development) and those having average or above-average scores (normal development). Three hundred and sixty children with below-average language composite score were recruited as cases, and 295 children of the same age and sex with average and above-average languages composite score served as a control group.
Methods
Socio-demographic assessment: For this special assessment questionnaire was used including questions about maternal age, maternal and paternal education and occupation, marital status, family income, and child order of birth [23]. Family income was classified according to father’s occupation into two categories; lower-middle-income, if the father is unemployed, day-by-day worker, farmer, or manual labourer; upper-middle-income, if the father is employee, professional and employer, or a dealer. Mother education was classified into 3 categories; illiterate to preparatory school, secondary school, and higher education.
Assessment of maternal and prenatal history: This included parity, history of maternal chronic diseases as hypertension, diabetes or hypothyroidism, and diseases acquired during pregnancy as gestational diabetes or preeclampsia. The infant’s data about gestational age, mode of delivery, history of complicated labour such as premature rupture of membranes, fetal asphyxia or umbilical cord prolapse were recorded. History of postnatal problems as cyanosis, jaundice or convulsions and admission to NICU was enquired.
Infant Feeding Practices in the first six months of life: was assessed to identify infants who were predominately breastfed, artificially-fed (who were consuming other milk including fresh, tinned, and powdered milk from cows or other animals) or mixed fed (artificial plus breast milk). The time of introduction of complementary feeding was recorded whether before or after the sixth month of age.
Thorough physical examination and anthropometric measurements: All measurements were made according to techniques described in the Anthropometric Standardization Reference Manual [24]. Physical examination and assessment of growth were performed for cases and control subjects.
Assessment of language and motor development: using the Bayley Scales of Infant and Toddler Development (Bayley-III): These scales were developed by Nancy Bayley [25] to assess the development of infants and toddlers between the age of 1 month to 42 months. Bayley-III consists of 5 subscales, i.e. Cognitive Scale, Language Scale (Receptive Communication and Expressive Communication), Motor Scale (Fine Motor and Gross Motor), Social-Emotional Scale, and Adaptive Behavior Scale. In this study, only the language and motor domains were being measured. The test was administered according to the infant’s age-specific start point. Each correct response is given a score of 1, and the total raw score is then converted into its composite score.
Ethical Considerations: The study complies with the International Ethical Guidelines for Biomedical Research Involving Human Subjects [26]. The Research and Ethical Committee of NRC cleared the study protocol. The ethical approval number was 11020. Informed consent was obtained from the parents of enrolled children.
Confidentiality: Mothers and children were identified by a serial number, and the information at the individual level was kept strictly confidential.
Results
The included children were divided according to the language composite score on Bayley scale into two groups; below-average group (n = 360) who were considered the cases, and average and above-average group (n = 295) who were the controls. Tables 1, 2 and 3 show the results of the univariate analysis of factors affecting language composite score.
Table 1.
The risk of impaired language development according to different feeding practices
| N | Children with impaired language development (Cases) (n = 360) | Children with normal language development (Control) (n = 295) | P | OR (95%CI) | |
|---|---|---|---|---|---|
| Type of feeding | |||||
| Breast fed | 321 | 160 (49.8) | 161 (50.2) | 1 | |
| Bottle fed | 241 | 146 (60.6) | 95 (39.4) | 0.012 | 1.6 (1.1-2.2) |
| Mixed fed | 93 | 54 (58.1) | 39 (41.9) | 0.16 | 1.4 (0.9-2.2) |
| Time to add complementary food | |||||
| Before six months | 201 | 128 (63.7) | 73 (36.3) | 0.003 | 1.7 (1.2-2.4) |
| After six months | 454 | 232 (51.0) | 222 (49.0) |
OR: Odds ratio; CI: Confidence interval.
Table 2.
The risk of impaired language development according to socioeconomic factors
| N | Impaired language development (n = 360) | Normal language development (n = 295) | P | OR (95%CI) | |
|---|---|---|---|---|---|
| Childbirth order | |||||
| > 3 | 213 | 120 (56.3) | 93 (43.7) | 0.623 | 1.1 (0.8-1.5) |
| ≤ 3 | 442 | 240 (54.3) | 202 (45.7) | ||
| Maternal age | |||||
| ≤ 25 years | 241 | 136 (56.4) | 105 (43.6) | 0.564 | 1.1 (0.8-1.5) |
| > 25 years | 414 | 224 (54.1) | 190 (45.9) | ||
| Family Income | |||||
| Lower Middle | 314 | 194 (61.8) | 120 (38.2) | 0.001 | 1.7 (1.3-2.3) |
| Upper Middle | 341 | 166 (48.7) | 175 (51.3) | ||
| Mother education | |||||
| Illiterate to prep | 194 | 124 (63.9) | 70 (36.0) | 0.001 | 1.9 (1.3-2.9) |
| Secondary | 254 | 137 (53.9) | 117 (46.1) | 0.192 | 1.3 (0.9-1.9) |
| High education | 207 | 99 (47.8) | 108 (52.2) | 1 | |
| Occupation | |||||
| House wife | 513 | 278 (54.2) | 235 (45.8) | 0.451 | 0.9 (0.6-1.3) |
| Working | 142 | 82 (57.7) | 60 (42.3) |
Table 3.
The risk of impaired language development according to maternal and child medical history
| N | Children with impaired language development | Children with normal language development | P | OR (95%CI) | |
|---|---|---|---|---|---|
| (n = 360) | (n = 295) | ||||
| Maternal related Factors | |||||
| Chronic diseases | |||||
| Yes | 124 | 74 (59.7) | 50 (40.3) | 0.24 | 1.3 (0.8-1.9) |
| No | 531 | 286 (53.8) | 245 (46.2) | ||
| Pregnancy-related diseases | |||||
| Yes | 89 | 65 (73.0) | 24 (27.0) | < 0.001 | 2.5 (1.5-4.1) |
| No | 566 | 295 (52.1) | 271 (47.9) | ||
| Iron deficiency anaemia | |||||
| Yes | 312 | 163 (52.2) | 149 (47.8) | 0.18 | 0.8 (0.6-1.1) |
| No | 343 | 197 (57.4) | 146 (42.6) | ||
| Nutritional status | |||||
| Malnourished | 529 | 295 (55.8) | 234 (44.2) | 0.39 | 1.2 (0.8-1.8) |
| Normal | 126 | 65 (51.6) | 61 (48.4) | ||
| Infant related Factors | |||||
| Gestational age | |||||
| Preterm | 49 | 32 (65.3) | 17 (34.7) | 0.13 | 1.6 (0.8-2.9) |
| Full term | 606 | 328 (54.1) | 278 (45.9) | ||
| Type of labour | |||||
| Cesarean | 372 | 198 (53.2) | 174 (46.8) | 0.31 | 0.9 (0.6-1.2) |
| Normal | 283 | 162 (57.2) | 121 (42.8) | ||
| Delivery problems | |||||
| Yes | 86 | 76 (88.4) | 10 (11.6) | <0.001 | 7.6 (3.9-15.1) |
| No | 569 | 284 (49.9) | 285 (50.1) | ||
| Weight for age | |||||
| Underweight | 49 | 28(57.1) | 21(42.9) | 0.865 | 1.1(0.6 -1.9) |
| Normal weight | 606 | 332(54.8) | 274(45.2) | ||
| Height for age | |||||
| Stunted | 82 | 47(57.3) | 35(42.7) | 0.734 | 1.1(0.7 -1.8) |
| Normal height | 573 | 313(54.6) | 260(45.4) | ||
OR: Odds ratio; CI: Confidence interval.
Comparison of cases and control groups revealed the independent factors lowering the language composite score and present children who are at more risk of impaired language development. Early introduction of complementary food before the age of six months carries a highly significant risk of impaired language development (OR = 1.7, P = 0.03) Table 1, the lower family income and low maternal education (illiteracy up to preparatory schools vs high education) represent highly significant social risk factors (OR = 1.7, p = 0.001 and OR = 1.9, p = 0.001 respectively) Table 2.
Children subjected to delivery problems are at most risk for impaired language development (OR = 7.6, p < 0.001) and pregnancy-related diseases of the mother increases the risk of impaired language development significantly (OR = 2.5, p < 0.001), weight and height for age expressed without statistically significant difference (Table 3).
The proportion of infants with impaired motor development among cases with language impairment is high (69%) if compared with that (38%) among the control group, as shown in Figure 1.
Figure 1.
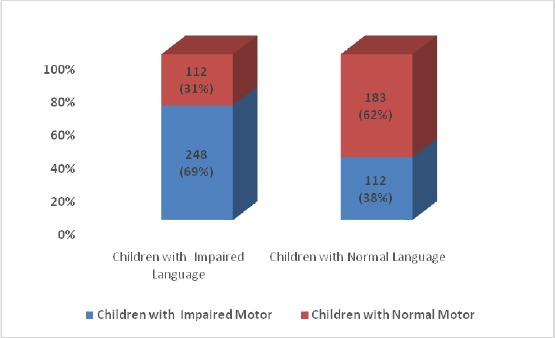
The proportion of children with impaired motor development among cases with impaired language development and controls with normal language development
Table 4 shows the most important predictors of impaired language development in the studied sample. Impaired motor development appears as a further highly significant risk factor to the previously mentioned factors, as shown in logistic regression analysis in Table 4.
Table 4.
Logistic regression of factors affecting language composite score
| B | p | OR | 95%CI of OR | ||
|---|---|---|---|---|---|
| Lower | Upper | ||||
| Early introduction of complementary food | 0.771 | < 0.001 | 2.162 | 1.457 | 3.207 |
| Lower middle family income | 1.176 | 0.002 | 3.242 | 1.719 | 6.115 |
| Delivery problems | 2.484 | < 0.001 | 11.986 | 4.906 | 29.284 |
| Pregnancy related diseases | 2.837 | < 0.001 | 17.070 | 3.869 | 75.312 |
| Mother education (illiteracy vs. high education) | 0.511 | 0.013 | 1.667 | 1.113 | 7.497 |
| Impaired motor development | 1.613 | < 0.001 | 5.016 | 3.068 | 8.199 |
B: Regression co-efficient; OR: Odds ratio; CI: Confidence interval.
Discussion
Child development is influenced by genetic and environmental factors. Environmental issues appear to largely influence young children’s attainment of language skills [27], [28]. In Egypt as a developing country, investigation and consequently, prevention of potential environmental risks is crucial.
This study demonstrated that factors that are independently associated with delayed language development in Egyptian children were early introduction of complementary food before the age of six months, low maternal education, low family income, delivery problems, pregnancy-related diseases of the mother and subtle delayed motor development.
The beneficial effect of breastfeeding on general growth and development of children has long been well recognised [29]. In the current study, history of feeding practices in the first six months of life revealed that bottle feeding and early weaning before the age of six months were associated with a significant risk of DLD. Many studies linked improved cognitive development rather than language development in infancy to breastfeeding. Exclusive breastfeeding was reported to positively affect cognitive development of children in early infancy [30], even after adjustment for other key cofactors [31]. In previous Egyptian studies, exclusive breastfeeding versus bottle-feeding during the first six months of life was correlated with above-average cognitive [32] and socio-emotional development of infants [33].
Few studies tested the link between breastfeeding and the language development of children. Leventakou et al. reported that a longer period of breastfeeding was independently associated with higher scores of language and motor development at 18 months of age [34]. A more recent study confirmed these findings and recommended the promotion of breastfeeding for more than 12 months to attain the maximum benefit in the cognitive and language development of children [35].
Many theories are proposed to explain the effect of feeding on language development. It was proposed that human milk contains a group of nutrients including the characteristic essential fatty acids such as docosahexaenoic acid (DHA) and choline, hormones, and growth factors that stimulate optimal development of brain structure and function [36].
Another theory is, the effect of breastfeeding on immune system function was supposed to influence learning and memory [37]. Also, the act of breastfeeding that enhances mother-infant relationship is thought to be important for cognitive, socio-emotional and language development [38].
Another independent factor that negatively affects language scores in the current study was a low socio-economic status (SES). The socioeconomic standard is usually ruled on the level of parental education, parental occupation and monthly family income [23]. This study showed that lower language composite scores were associated with lower family income and lower mother education. As language is a social act that progresses under social stimuli, it has been shown that children from lower-SES background show slower growth of vocabulary compared to higher-SES children from infancy up to school years [39], [40]. One pathway for explanation of this difference is the availability of learning resources in high-income families whether inside home (as books and toys) or outside home (as high-quality daycare centres or outdoor activities) [41]. Another pathway for this difference is the variation of parents’ speech to their children. Hart and Risley estimated that children from professional families hear an average of 45 million words by age four compared to 13 million words in children from low-income families [42]. Other investigators found that the quality of speech and not the total amount of speech plays a more critical role in language development. In a large sample of low-income families, language development was positively affected by maternal vocabulary input and maternal language and literacy skills [43]. It was found that variation in the quality of nonverbal and verbal interactions were more powerful predictors of language development rather than the number of mothers’ words during the communication with the infant [44], [45]. Mothers’ level of education appeared to have a major effect on early language development not only in normal children but also in children with autism spectrum disorder (ASD) [28]. We thought that maternal education not only can affect language development directly through maternal vocabulary input but also indirectly through choosing appropriate feeding practices [46] and providing a health care and a safe environment for their children [47].
Another important factor affecting language development is the perinatal risk factors. In the current study, pregnancy-related complications (most commonly gestational hypertension, preeclampsia, eclampsia and gestational diabetes) and delivery problems (mostly birth trauma and asphyxia) were the main perinatal risk factors recorded in children with DLD. This could be explained based on placental insufficiency, oxygen deprivation in-utero, birth asphyxia, and neonatal hypoglycaemia which could affect neurocognitive functions and increase the risk of developmental disability [48], [49], [50].
In contrast to our findings, variables as first-minute Apgar scores < 7, mother’s age, emergency caesarean section, maternal haemorrhage, and threatened abortion were significant factors for delayed cognitive and communication skills, while factors such as preeclampsia and premature rupture of the membrane had no significant relationship [51]. Other studies linked developmental disorders to prematurity, low birth weight, maternal difficulties during pregnancy, and congenital malformations [52]. In the current study, variables as maternal malnutrition, maternal chronic diseases, prematurity and caesarean delivery seemed irrelevant to developmental delay. Thus, the relationship between specific perinatal risk factors and subsequent developmental delay has not reached a consensus.
Nutritional deficiencies during infancy are likely to affect cognition, communication, behaviour, and productivity throughout childhood and adulthood [53].
In the current study, though the prevalence of underweight children and that of stunted children were higher in cases than in controls, the differences didn’t reach a significant level (7.8% of cases were underweight vs 7.1% in controls; 13% of cases were stunted vs 11.9% in controls). Thus, malnutrition was not a significant risk factor for DLD in this study. This finding is in agreement with that of Mendes et al., 2012 [54]. However, other studies found that both malnutrition and anaemia early in life might lead to problems in cognitive development and language acquisition [55], [56]. We think that the severity of malnutrition and the association of anaemia are important variables controlling the impact on language development.
Language development depends on other developmental domains. The influence of cognitive and social-emotional domains on language development is completely supported [57]. Some studies support language and motor skills as separate domains, while others suggest that motor skills are a prerequisite for language development [58]. Some research recognised the relationship between motor and cognitive development, and consequently between motor and language development as a sub-domain of cognition. This relationship is a logical consequence in the context of bodily interaction with the physical and social environment [59]. Neuroimaging techniques have shown that areas of the brain implicated in language functions are activated during motor tasks [60], and the activation of motor areas was detected during language tasks [61]. Behavioural studies revealed associations between infant motor maturity and language development [42]. Also, other studies have shown a link between motor performance and between motor performance and language [62], [63].
In the current study, the interrelationship between language and motor development was evident. The percentage of children have got below-average score on Bayley-motor scale, was significantly higher among children with DLD than in normal children (69% vs 38%). Also, delayed motor development appeared as a highly significant predictor of language development in logistic regression analysis. The application of these findings is very important. It denotes the significance of careful evaluation of all developmental domains even the child is presented with DLD only. Non-responding children to intensive speech therapy may benefit if they attend physiotherapy sessions in parallel.
Logistic regression analysis in this study approved the independent predictors of DLD according to their contribution and their level of significance as follows: maternal health problems during pregnancy and child-birth difficulties, followed by impaired motor development, low family income, early introduction of complementary food and the least significant predictor was maternal education.
Limitations: Details of parental-child interaction and whether the child attended childcare centre were not included in the questionnaire. Neither language impairment was not classified into receptive communication disorders and expressive communication disorders, nor was motor impairment not classified into fine motor and gross motor disorders. This is because estimation of composite score of Bayley-scales depends on sum of both functions.
In conclusion, a group of social, medical and nutritional factors are interacting to affect language development in Egyptian children. The most significant risk factors were pregnancy-related diseases and labour-associated problems. This denotes inadequate access of Egyptian mothers to maternal health care during pregnancy and childbirth. Low family income and the level of maternal education were the predominant social risk factors. Child developmental screening should include all developmental domains. Subtle motor impairments common among children with DLD and can potentiate its risk.
Footnotes
Funding: This research did not receive any financial support
Competing Interests: The authors have declared that no competing interests exist
References
- 1.Capone Singleton N, Shulman B. Language Development. Foundations, Processes, and Clinical Applications. 2nd Edition. Baltimore, MD: Jones & Bartlett; 2014. [Google Scholar]
- 2.Conti-Ramsden G, Durkin K, Toseeb U, Botting N, Pickles A. Education and employment outcomes of young adults with a history of developmental language disorder. International Journal of Language & Communication Disorders. 2018;53(2):237–255. doi: 10.1111/1460-6984.12338. https://doi.org/10.1111/1460-6984.12338 PMid:29139196 PMCid:PMC5873379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hawa VV, Spanoudis G. Toddlers with delayed expressive language: an overview of the characteristics, risk factors and language outcomes. Res Dev Disabil. 2014;35(2):400–7. doi: 10.1016/j.ridd.2013.10.027. https://doi.org/10.1016/j.ridd.2013.10.027 PMid:24334229. [DOI] [PubMed] [Google Scholar]
- 4.Buschmann A, Jooss B, Rupp A, Dockter S, Blaschtikowitz H, Heggen I, et al. Children with developmental language delay at 24 months of age: results of a diagnostic work-up. Dev Med Child Neurol. 2008;50(3):223–9. doi: 10.1111/j.1469-8749.2008.02034.x. https://doi.org/10.1111/j.1469-8749.2008.02034.x PMid:18266869. [DOI] [PubMed] [Google Scholar]
- 5.Rosenberg SA, Zhang D, Robinson CC. Prevalence of developmental delays and participation in early intervention services for young children. Paediatrics. 2008;121(6):e1503–9. doi: 10.1542/peds.2007-1680. https://doi.org/10.1542/peds.2007-1680 PMid:18504295. [DOI] [PubMed] [Google Scholar]
- 6.Alcock KJ, Krawczyk K. Individual differences in language development: relationship with motor skill at 21 months. Dev Sci. 2010;13:677–91. doi: 10.1111/j.1467-7687.2009.00924.x. https://doi.org/10.1111/j.1467-7687.2009.00924.x PMid:20712734. [DOI] [PubMed] [Google Scholar]
- 7.Gad-Allah H, Abd-Elraouf S, Abou-Elsaad T. Identification of communication disorders among Egyptian Arabic-speaking nursery schools' children, Mansoura University, Mansoura. Egypt J Ear Nose Throat Allied Sci. 2012;13:83–90. https://doi.org/10.1016/j.ejenta.2012.04.004. [Google Scholar]
- 8.Gharib BA, El Banna MM, Khalil M, Heikal MM. Prevalence and etiology of communication disorders in children attending Alexandria University Children's Hospital, Egypt. Alexandria Journal of Pediatrics. 2017;30(1):17–25. [Google Scholar]
- 9.Skarzynski H, Piotrowska A. Prevention of communication disorders-screening pre-school and school-age children for problems with hearing, vision and speech: European consensus statement. Med Sci Monit. 2012;18(4):SR17–21. doi: 10.12659/MSM.882603. https://doi.org/10.12659/MSM.882603 PMid:22460107 PMCid:PMC3560814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hulme C, Snowling MJ. Children's Reading Comprehension Difficulties. Current Directions in Psychological Science. 2011;20(3):139–142. https://doi.org/10.1177/0963721411408673. [Google Scholar]
- 11.St Clair MC, Pickles A, Durkin K, Conti-Ramsden G. A longitudinal study of behavioral, emotional and social difficulties in individuals with a history of specific language impairment (SLI) Journal of Communication Disorders. 2011;44(2):186–199. doi: 10.1016/j.jcomdis.2010.09.004. https://doi.org/10.1016/j.jcomdis.2010.09.004 PMid:20970811. [DOI] [PubMed] [Google Scholar]
- 12.Bornstein MH, Hahn CS, Suwalsky JT. Language and internalizing and externalizing behavioral adjustment: developmental pathways from childhood to adolescence. Development and Psychopathology. 2013;25(3):857–878. doi: 10.1017/S0954579413000217. https://doi.org/10.1017/S0954579413000217 PMid:23880396 PMCid:PMC4151616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Girard LC, Pingault JB, Doyle O, Falissard B, Tremblay RE. Developmental Associations Between Conduct Problems and Expressive Language in Early Childhood: A Population-Based Study. Journal of Abnormal Child Psychology. 2016;44(6):1033–1043. doi: 10.1007/s10802-015-0094-8. https://doi.org/10.1007/s10802-015-0094-8 PMid:26496905. [DOI] [PubMed] [Google Scholar]
- 14.Petersen IT, Bates JE, Staples AD. The role of language ability and self-regulation in the development of inattentive-hyperactive behavior problems. Development and Psychopathology. 2015;27(1):221–237. doi: 10.1017/S0954579414000698. https://doi.org/10.1017/S0954579414000698 PMid:25025234 PMCid:PMC4294999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.LeBarton ES, Iverson JM. Fine motor skill predicts expressive language in infant siblings of children with autism. Developmental science. 2013;16(6):815–27. doi: 10.1111/desc.12069. https://doi.org/10.1111/desc.12069 PMid:24118709 PMCid:PMC3808875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wang MV, Lekhal R, Aaro LE, Schjolberg S. Co-occurring development of early childhood communication and motor skills: results from a population-based longitudinal study. Child Care Health Dev. 2014;40(1):77–84. doi: 10.1111/cch.12003. https://doi.org/10.1111/cch.12003 PMid:22970997. [DOI] [PubMed] [Google Scholar]
- 17.Libertus K, Violi DA. Sit to talk: relation between motor skills and language development in infancy. Frontiers in psychology. 2016;7:475. doi: 10.3389/fpsyg.2016.00475. https://doi.org/10.3389/fpsyg.2016.00475 PMid:27065934 PMCid:PMC4815289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Owen SE, McKinlay IA. Motor difficulties in children with developmental disorders of speech and language. Child: care, health and development. 1997;23(4):315–25. doi: 10.1046/j.1365-2214.1997.864864.x. https://doi.org/10.1046/j.1365-2214.1997.864864.x. [DOI] [PubMed] [Google Scholar]
- 19.Estil LB, Whiting HT, Sigmundsson H, Ingvaldsen RP. Why might language and motor impairments occur together? Infant and Child Development: An International Journal of Research and Practice. 2003;12(3):253–65. https://doi.org/10.1002/icd.289. [Google Scholar]
- 20.Newbury DF, Monaco AP. Genetic advances in the study of speech and language disorders. Neuron. 2010;68:309–320. doi: 10.1016/j.neuron.2010.10.001. https://doi.org/10.1016/j.neuron.2010.10.001 PMid:20955937 PMCid:PMC2977079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Developmental Medicine & Child Neurology. 2000;42:470–475. doi: 10.1017/s0012162200000876. https://doi.org/10.1017/S0012162200000876 PMid:10972419. [DOI] [PubMed] [Google Scholar]
- 22.Newcombe RG. Improved confidence intervals for the difference between binomial proportions based on paired data. Statistics in medicine. 1998;17(22):2635–50. https://doi.org/10.1002/(SICI)1097-0258(19981130)17:22<2635::AID-SIM954>3.0.CO;2-C. [PubMed] [Google Scholar]
- 23.El-Shakhs A. Social level and the economic scale of the family: the scale manual [Google Scholar]
- 24.Lohman TG, Roche AF, Martorell R. Anthropometric standardization reference manual. Champaign, IL: Human kinetics books; 1988. [Google Scholar]
- 25.Bayley N. Bayley Scales of Infant and Toddler Development. 3rd Edition. Psychological Corporation; 2006. https://doi.org/10.1037/t14978-000. [Google Scholar]
- 26.Council for International Organizations of Medical Sciences, World Health Organization. International ethical guidelines for biomedical research involving human subjects. Geneva: CIOMS; 2002. [PubMed] [Google Scholar]
- 27.Hayiou-Thomas ME. Genetic and environmental influences on early speech, language and literacy development. Journal of communication disorders. 2008;41(5):397–408. doi: 10.1016/j.jcomdis.2008.03.002. https://doi.org/10.1016/j.jcomdis.2008.03.002 PMid:18538338 PMCid:PMC3851292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Grandgeorge M, Hausberger M, Tordjman S, Deleau M, Lazartigues A, Lemonnier E. Environmental factors influence language development in children with autism spectrum disorders. PloS one. 2009;4(4):e4683. doi: 10.1371/journal.pone.0004683. https://doi.org/10.1371/journal.pone.0004683 PMid:19357766 PMCid:PMC2663032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Dieterich CM, Felice JP, O'Sullivan E, Rasmussen KM. Breastfeeding and Health Outcomes for the Mother-Infant Dyad. Pediatr Clin North Am. 2013;60:31–48. doi: 10.1016/j.pcl.2012.09.010. https://doi.org/10.1016/j.pcl.2012.09.010 PMid:23178059 PMCid:PMC3508512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Jedrychowski W, Perera F, Jankowski J, Butscher M, Mroz E, Flak E, et al. Effect of exclusive breastfeeding on the development of children's cognitive function in the krakow prospective birth cohort study. Eur J Pediatr. 2012;171:151–8. doi: 10.1007/s00431-011-1507-5. https://doi.org/10.1007/s00431-011-1507-5 PMid:21660433 PMCid:PMC3747316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Anderson JW, Johnstone BM, Remley DT. Breast-feeding and cognitive development: a meta-analysis. Am J Clin Nutr. 1999;70:525–35. doi: 10.1093/ajcn/70.4.525. https://doi.org/10.1093/ajcn/70.4.525 PMid:10500022. [DOI] [PubMed] [Google Scholar]
- 32.Ebtissam M, Salah El Din, Thanaa M. Rabah, Ammal M. Metwally, Maysa S. Nassar, Mona A Elabd, Ashraf Shalaan, Wafaa Kandeel, Lobna A. El Etreby, Sanaa Y. Shaaban Potential Risk Factors of Developmental Cognitive Delay in the First Two Years of Life Open Access Macedonian. Journal of Medical Sciences. 2019;7(12):2024–2030. doi: 10.3889/oamjms.2019.566. https://doi.org/10.3889/oamjms.2019.566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Metwally AM, El-Din EM, Shehata MA, Shaalan A, El Etreby LA, Kandeel WA, Shaaban SY, Rabah TM. Early Life Predictors of Socio-Emotional Development in a Sample of Egyptian Infants. PloS one. 2016;11(7):e0158086. doi: 10.1371/journal.pone.0158086. https://doi.org/10.1371/journal.pone.0158086 PMid:27379907 PMCid:PMC4933375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Leventakou V, Roumeliotaki T, Koutra K, Vassilaki M, Mantzouranis E, Bitsios P, et al. Breastfeeding duration and cognitive, language and motor development at 18 months of age: Rhea mother-child cohort in Crete, Greece. J Epidemiol Community Health. 2015;69:232–9. doi: 10.1136/jech-2013-202500. https://doi.org/10.1136/jech-2013-202500 PMid:24336236. [DOI] [PubMed] [Google Scholar]
- 35.Iqbal MI, Rafique G, Ali SA. The Effect of Breastfeeding on the Cognitive and Language Development of Children Under 3 Years of Age: Results of Balochistan-Early Childhood Development Project. Journal of General Practice. 2017;5(2):1. https://doi.org/10.4172/2329-9126.1000305. [Google Scholar]
- 36.McCrory C, Murray A. The effect of breastfeeding on neuro-development in infancy. Maternal and child health journal. 2013:1680–1688. doi: 10.1007/s10995-012-1182-9. https://doi.org/10.1007/s10995-012-1182-9 PMid:23135624. [DOI] [PubMed] [Google Scholar]
- 37.Smith JM. Breastfeeding and language outcomes: A review of the literature. J Commun Disord. 2015;57:29–40. doi: 10.1016/j.jcomdis.2015.04.002. https://doi.org/10.1016/j.jcomdis.2015.04.002 PMid:26028604. [DOI] [PubMed] [Google Scholar]
- 38.Reynolds A. Breastfeeding and brain development. PediatrClin North Am. 2001;48(1):159–71. doi: 10.1016/s0031-3955(05)70291-1. https://doi.org/10.1016/S0031-3955(05)70291-1. [DOI] [PubMed] [Google Scholar]
- 39.Morgan PL, Farkas G, Hillemeier MM, Hammer CS, Maczuga S. 24-Month-Old Children With Larger Oral Vocabularies Display Greater Academic and Behavioral Functioning at Kindergarten Entry. Child Dev. 2015;86:1351–70. doi: 10.1111/cdev.12398. https://doi.org/10.1111/cdev.12398 PMid:26283023 PMCid:PMC4567967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Arriaga RI, Fenson L, Cronan T, Pethick SJ. Scores on the MacArthur Communicative Development Inventory of children from lowand middle-income families. Appl Psycholinguist. 1998;19:209–23. https://doi.org/10.1017/S0142716400010043. [Google Scholar]
- 41.Pace A, Luo R, Hirsh-Pasek K, Golinkoff RM. Identifying Pathways between Socioeconomic Status and Language Development. Annu. Rev. Linguist. 2017;3:285–308. https://doi.org/10.1146/annurev-linguistics-011516-034226. [Google Scholar]
- 42.Hart B, Risley TR. Meaningful differences in the everyday experience of young American children. Paul H Brookes Publishing; 1995. [Google Scholar]
- 43.Pan BA, Rowe ML, Singer JD, Snow CE. Maternal correlates of growth in toddler vocabulary production in low-income families. Child Dev. 2005;76:763–82. doi: 10.1111/j.1467-8624.2005.00876.x. https://doi.org/10.1111/j.1467-8624.2005.00876.x PMid:16026495. [DOI] [PubMed] [Google Scholar]
- 44.Hirsh-Pasek K, Adamson LB, Bakeman R, Owen MT, Golinkoff RM, Pace A, et al. The Contribution of Early Communication Quality to Low-Income Children's Language Success. Psychol Sci. 2015;26:1071–83. doi: 10.1177/0956797615581493. https://doi.org/10.1177/0956797615581493 PMid:26048887. [DOI] [PubMed] [Google Scholar]
- 45.Rowe ML, Pan BA, Ayoub C. Predictors of Variation in Maternal Talk to Children: A Longitudinal Study of Low-Income Families. Parenting. 2005;5:259–83. https://doi.org/10.1207/s15327922par0503_3. [Google Scholar]
- 46.Kandeel WA, Rabah TM, Zeid DA, El-Din EM, Metwally AM, Shaalan A, El Etreby LA, Shaaban SY. Determinants of Exclusive Breastfeeding in a Sample of Egyptian Infants. Open access Maced J Medl Sci. 2018;6(10):1818–1823. doi: 10.3889/oamjms.2018.359. https://doi.org/10.3889/oamjms.2018.359 PMid:30455755 PMCid:PMC6236050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Natarajan V, Devaki PR. Does Maternal Education Really Improve Child Health? Journal of Dental and Medical Sciences. 2013;4(4):7–9. https://doi.org/10.9790/0853-0440709. [Google Scholar]
- 48.48 Butalia S, Audibert F, Côté AM, Firoz T, Logan AG, Magee LA, et al. Hypertension Canada's 2018 Guidelines for the Management of Hypertension in Pregnancy. Can J Cardiol. 2018;34(5):526–531. doi: 10.1016/j.cjca.2018.02.021. https://doi.org/10.1016/j.cjca.2018.02.021 PMid:29731014. [DOI] [PubMed] [Google Scholar]
- 49.49 Cai S, Qiu A, Broekman BF, et al. The Influence of Gestational Diabetes on Neurodevelopment of Children in the First Two Years of Life: A Prospective Study. PLoS One. 2016;11(9):e0162113. doi: 10.1371/journal.pone.0162113. https://doi.org/10.1371/journal.pone.0162113 PMid:27603522 PMCid:PMC5014336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Rainaldi MA, Perlman JM. Pathophysiology of Birth Asphyxia. ClinPerinatol. 2016;43(3):409–22. doi: 10.1016/j.clp.2016.04.002. https://doi.org/10.1016/j.clp.2016.04.002 PMid:27524444. [DOI] [PubMed] [Google Scholar]
- 51.Glasson EJ, Petterson B. Perinatal factors and development of autism. Arch Gen Psychiat. 2007;61:618–27. doi: 10.1001/archpsyc.61.6.618. https://doi.org/10.1001/archpsyc.61.6.618 PMid:15184241. [DOI] [PubMed] [Google Scholar]
- 52.Sajedy F, Alizadeh V. The incidence of motor developmental delay in high-risk infants and effective risk factors in developing of it. Q J Rehabil. 2008;5:7. [Google Scholar]
- 53.Prado EL, Dewey KG. Nutrition and brain development in early life. Nutrition reviews. 2014;72(4):267–84. doi: 10.1111/nure.12102. https://doi.org/10.1111/nure.12102 PMid:24684384. [DOI] [PubMed] [Google Scholar]
- 54.Mendes JC, Pandolfi MM, Carabetta C, Júnior, Novo NF, Colombo-Souza P. Factors associated to language disorders in preschool children. Rev Soc Bras Fonoaudiol. 2012;17(2):177–81. https://doi.org/10.1590/S1516-80342012000200013. [Google Scholar]
- 55.Santos JN, Lemos SM, Lamounier JA. Nutritional status and language development in children in a public day care center. Rev Soc Bras Fonoaudiol. 2010;15(4):566–71. https://doi.org/10.1590/S1516-80342010000400015. [Google Scholar]
- 56.Lima LM, Queiroga BA. Phonological acquisition in children with a history of malnutrition. CEFAC. 2007;9(1):13–20. https://doi.org/10.1590/S1516-18462007000100003. [Google Scholar]
- 57.Gleason JB, Ratner NB. The development of language. Boston: Pearson; 2009. [Google Scholar]
- 58.Iverson JM, Braddock BA. Gesture and motor skill in relation to language in children with language impairment. Journal of Speech, Language, and Hearing Research. 2011;54(1):72–86. doi: 10.1044/1092-4388(2010/08-0197). https://doi.org/10.1044/1092-4388(2010/08-0197) [DOI] [PubMed] [Google Scholar]
- 59.Smith JM. Breastfeeding and language outcomes: A review of the literature. J Commun Disord. 2015;57:29–40. doi: 10.1016/j.jcomdis.2015.04.002. https://doi.org/10.1016/j.jcomdis.2015.04.002 PMid:26028604. [DOI] [PubMed] [Google Scholar]
- 60.Morgan PL, Farkas G, Hillemeier MM, Hammer CS, Maczuga S. 24-Month-Old Children With Larger Oral Vocabularies Display Greater Academic and Behavioral Functioning at Kindergarten Entry. Child Dev. 2015;86:1351–70. doi: 10.1111/cdev.12398. https://doi.org/10.1111/cdev.12398 PMid:26283023 PMCid:PMC4567967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Arriaga RI, Fenson L, Cronan T, Pethick SJ. Scores on the MacArthur Communicative Development Inventory of children from lowand middle-income families. Appl Psycholinguist. 1998;19:209–23. https://doi.org/10.1017/S0142716400010043. [Google Scholar]
- 62.Hart B, Risley TR. Meaningful differences in the everyday experience of young American children. Paul H Brookes Publishing; 1995. [Google Scholar]
- 63.Pan BA, Rowe ML, Singer JD, Snow CE. Maternal correlates of growth in toddler vocabulary production in low-income families. Child Dev. 2005;76:763–82. doi: 10.1111/j.1467-8624.2005.00876.x. https://doi.org/10.1111/j.1467-8624.2005.00876.x PMid:16026495. [DOI] [PubMed] [Google Scholar]


