Abstract
AIM
To ensure the diagnostic value of computer aided techniques in diabetic retinopathy (DR) detection based on ophthalmic photography (OP).
METHODS
PubMed, EMBASE, Ei village, IEEE Xplore and Cochrane Library database were searched systematically for literatures about computer aided detection (CAD) in DR detection. The methodological quality of included studies was appraised by the Quality Assessment Tool for Diagnostic Accuracy Studies (QUADAS-2). Meta-DiSc was utilized and a random effects model was plotted to summarize data from those included studies. Summary receiver operating characteristic curves were selected to estimate the overall test performance. Subgroup analysis was used to identify the efficiency of CAD in detecting DR, exudates (EXs), microaneurysms (MAs) as well as hemorrhages (HMs), and neovascularizations (NVs). Publication bias was analyzed using STATA.
RESULTS
Fourteen articles were finally included in this Meta-analysis after literature review. Pooled sensitivity and specificity were 90% (95%CI, 85%-94%) and 90% (95%CI, 80%-96%) respectively for CAD in DR detection. With regard to CAD in EXs detecting, pooled sensitivity, specificity were 89% (95%CI, 88%-90%) and 99% (95%CI, 99%-99%) respectively. In aspect of MAs and HMs detection, pooled sensitivity and specificity of CAD were 42% (95%CI, 41%-44%) and 93% (95%CI, 93%-93%) respectively. Besides, pooled sensitivity and specificity were 94% (95%CI, 89%-97%) and 87% (95%CI, 83%-90%) respectively for CAD in NVs detection. No potential publication bias was observed.
CONCLUSION
CAD demonstrates overall high diagnostic accuracy for detecting DR and pathological lesions based on OP. Further prospective clinical trials are needed to prove such effect.
Keywords: Meta-analysis, diabetic retinopathy, computer aided detection
INTRODUCTION
The number of patients with diabetes is increasing worldwide, and this number is estimated to be more than 93 million in 2010[1]. In 2014, there were 96.28 million patients, accounting for about 25% of the global 387 million patients in China. In those diabetic patients, diabetic retinopathy (DR) is one of the most common complications and could possibly results in blindness at its end stage. According to the report from World Health Organization (WHO), the percentage of DR out of total blindness accounts for nearly 16% in U.S and Europe and 7% in China and Mongolia[2], and the latest estimates of global and setting-specific DR prevalence have been updated[3]. About 25% newly diagnosed type 2 diabetic mellitus (DM) patients had DR. DR could be detected by various methods. It's suggested that the retina should be observed at the time of DM being diagnosed and early detection and timely treatment of DR can reduce the risk of blindness. Therefore, it is a urgent task to detect and screen the presence and severity of DR.
Ophthalmic photography (OP) screening is an effective way to detect DR and could be obtained by digital ophthalmic camera, and changes of retinal anatomic structures on the OP could be recorded. In this way, the health status of retinal structure could be evaluated and its morphology could be quantified for research purpose. Taken DR for instance, the retinal arterioles have certain geometric changes and pathological lesions such as microaneurysms (MAs), exudates (EXs), hemorrhage (HM), neovascularization (NV) will appear as the severity of diabetes develops[4]–[8]. Due to the huge amount of diabetic patients, the traditional OP screening performed by experienced ophthalmologists cost a lot of manpower and finances, making regular OP screening difficult. Therefore, automatic DR screening techniques based on OP images were of significance to be developed to improve above situation.
With the advances of computer algorithms on medical image processing, multiple automated DR detection algorithms have been developed, and methods have been proposed to segment lesions on OPs[9]–[11]. The most basic way to segment the normal anatomic structures and lesions from OPs is gray-level thresholding. However, the thresholding results are somehow inconsistent due to uneven illumination of the OP. Instead, edge detection and mixture models was proposed to detect hard EXs, and its classification accuracy was about 95%. Other algorithms including region growing, adaptive region growing, and Bayesian-based approaches were proposed to segment the lesions on OPs with an accuracy rate of 90% for DR detection. The color and shape features extracted from OPs were used to classify MA and HM[12], which was further used to detect normal and abnormal retinal images. Different computer aided detection (CAD) approaches were developed for DR automatic detection based on OPs. Gardner et al[13] detected retinal vessels, EXs and HMs from 179 OPs with back-propagation artificial neural network (BP-ANN) and verified its performance with 278 OPs, the results showed BP-ANN could achieve 88.4% sensitivity and 83.5% specificity. While Goh et al[14] extracted color and textual features from OPs, and they obtained 91% accuracy through their classifiers in 1000 test images. In Priya and Aruna's[15] study, ANN classifier was trained with 250 OPs after geometric features extracted, and achieved over 80% accuracy. In all these methods, the features were firstly extracted from OPs and then classified by different classifiers. Although these algorithms are continually refined and achieving promising results, some state-of-art ones even comparable with human-level performance, the diagnostic values of them are still controversy due to inconsistency of clinical datasets, variance of sample size and difference of DR detection rules. Therefore, our study aims to appraise the diagnostic accuracy of CAD methods in DR detection compared with the accepted gold standard evaluated by experienced or certified readers.
MATERIALS AND METHODS
Search Strategy and Selection Criteria
We searched PubMed, EMBASE, Ei village, IEEE Xplore and Cochrane Library databases for relevant citations on April 2016 and updated the search on December 2018. We used a combination of medical subject headings and search terms indexing DR and CAD. Search terms used were as follows: i) diabetic retinopathy, DR, proliferative diabetic retinopathy, PDR, non-proliferative diabetic retinopathy, NPDR, microaneurysm*, neovascularization, cotton-wool spots, hard exudate*, soft exudate*, haemorrhage, hemorrhage, bleed*, degeneration; ii) computer, algorithm, automat*, machine learning, feature extraction, software; iii) diagnosis, classify*, detect*, specificity, sensitivity, accuracy studies; and iv) fundus, retina*, photo$, image$, ophthalmic. Additional articles not obtained through the electronic searches were identified by examining the reference lists of all relevant articles. The detailed search strategy was available from the authors. We included studies if they used CAD methods to detect the pathological changes such as MAs, EXs, HMs, and NVs, which are believed to be the featured changes in DR patients.
Inclusion criteria
1) Case-control or cohort studies published using different kinds of computer aided methods to detect DR. 2) Determination of DR was made by experienced ophthalmologists based on ophthalmoscopy or OP. 3) Adequate information about the computer methods and the techniques details were available.
Exclusion criteria
1) Comparison between different CAD methods but without gold standard detection results by experts. 2) Insufficient information about baseline characteristics of participants. 3) Insufficient data about image processing and computer detection methods. 4) Insufficient data during data extraction.
Two reviewers (Wu HQ and Shan YX) reviewed the electronic searches independently and obtained full relevant literatures that were likely to meet the predefined selection criteria. If there is any disagreement, a third reviewer was involved for discussion to reach consensus (Dong JC).
Quality Evaluation and Data Extraction
In this study, the Quality Assessment Tool for Diagnostic Accuracy Studies (QUADAS-2) was utilized to evaluate the quality, validity and risk of bias of the included studies[16]. The items including patient selection, index test, reference standards etc. were assessed for potential bias and applicability. The study characteristics were extracted and the quality of included studies was reviewed by two reviewers (Wu HQ and Shan YX) independently. If there is any disagreement, there will be a discussion with a third reviewer (Dong JC) until the consensus.
Data Analysis
For each of the included studies, the raw data regarding the true and false positives, true and false negatives were extracted by two reviewers independently (Shan YX and Wu HQ). Authors would be contacted if the raw data could not be extracted or calculated. The Meta-DiSc (v1.4) software was performed for further statistical analysis[17]. The parameters of diagnostic accuracy such was sensitivity, specificity, positive likelihood ratio (PLR), negative likelihood ratio (NLR), diagnostic odds ratio (DOR) and their corresponding 95% confidence intervals (CI) were computed. For those included studies, heterogeneity induced by threshold effect was calculated by the spearman correlation coefficient and P values between the logit of sensitivity and logit of 1-specificity, while heterogeneity induced by non-threshold effect was assessed using Chi-square or I2. I2<25% means that heterogeneity among studies is low. I2 lies between 25% and 50% means that heterogeneity among studies is moderate. I2>50% means that heterogeneity among studies may produce some impacts[18]. If the significant heterogeneity was detected, the random effects model was used. In addition, the estimate of summary receiver operating characteristics (SROC) curve was plotted and Q* values were calculated from the SROC curve by the point where sensitivity equaled specificity. The area under SROC curve (AUC) was achieved to depict the probability of the correctly ranked diagnostic test values for a random pair of diseased and non-diseased subjects. Potential heterogeneity factors were analyzed by Meta-regressions. If necessary, subgroup analyses were made to distinguish the heterogeneity due to test-related or other potential factors. The statistical significance of statistical tests was defined as P value less than 0.05.
Publication Bias
Publication bias was determined using the Deeks et al[19] test. The bias of publication was assessed using Stata SE 14 software (StataCorp, College Station, TX, USA).
RESULTS
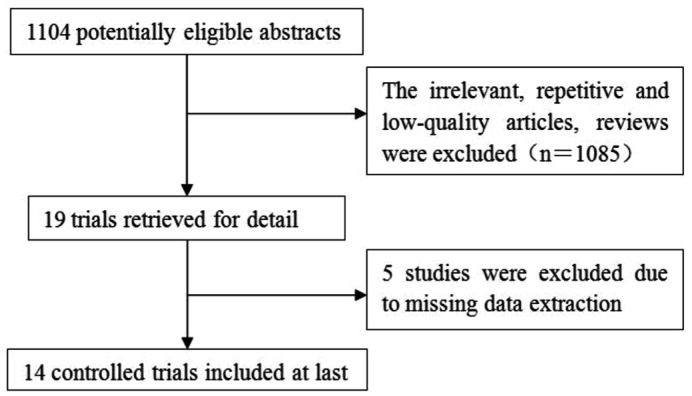
The literature search yielded 1104 references. Figure 1 showed the flowchart of study selection. A total of 19 primary studies were eligible for inclusion, from which five studies were excluded due to missing data during extraction.
Figure 1. Flow chart of study selection.
Summary Characteristics of Included Studies
All studies[20]–[33] recruited subjects regardless who were male or female. Maher et al[29] and Júnior and Welfer[30] recruited subjects with type 1 diabetes. Images with evidence of previous retinal laser treatment were excluded from the study by Goatman et al[22]. In Júnior and Welfer's study[30], the regions with lesions were highlighted manually by four specialists in ophthalmology, who made the analysis individually on each OP. All the images in Jaya et al[24] were graded by trained ophthalmologists. OP images in Torok et al[33] were assessed by two independent ophthalmologists. In Lee et al's[26] study, OP images were taken by TRC-NW6 non-mydriatic camera (Topcon, Tokyo, Japan), similarly, OP images in Nayak et al's[27] study were taken by a TRC-NW200 Topcon non-mydriatic retinal camera. In Niemeijer et al's[28] study, OP images were obtained by different non-mydriatic cameras such as the Topcon NW 100, Topcon NW 200 and Canon CR5-45NM at multiple sites. In Sinthanayothin et al's[31] study, 112 digital OP images were captured using a Topcon TRC-NW5S non-mydriatic camera for those patients attending a DR screening service. Niemeijer et al[28] and Kittipol et al[25] obtained OP images at 45° field of view (FOV). Lee et al[26] and Agurto et al[21] obtained OP images at 50° and 60° FOV, respectively. In the study by Goatman et al[22], 52 OP images were obtained at 45° FOV, and 57 with the common 50° FOV. SujithKumar and Vipula[32], Júnior and Welfer[30], Maher et al[29], Torok et al[33], Jaya et al[24], Kittipol et al[25], Hassan et al[23] all included subjects photographed at one site. Agurto et al[21] and Sinthanayothin et al[31] included subjects photographed at two and three different locations, respectively. Other studies were with no description of the photographed locations. The detailed characteristics of the included studies were summarized in Table 1.
Table 1. Characteristics of the included studies.
| Study ID | Sample size | Imaging modality | Imaging center | Color | Angle of view | CAD methods | Results | Sensitivity (%) | Specificity (%) |
| Acharya (2009) | 331 | FI | NA | RGB | NA | SVM | NPDR, PDR | 82 | 86 |
| Agurto (2012) | 57 | FI | MAC, OD | NA | 60° | Partial least squares | NV | 96 | 83 |
| Goatman (2011) | 109 | FI | NA | Gray | 45°/50° | SVM | NV | 92.1 | 73.2 |
| Hassan (2012) | 313 | ND | OD | Gray | NA | Morphology-based | NV | 63.9 | 89.4 |
| Jaya (2015) | 200 | FI | OD | RGB | NA | SVM | HE | 94.1 | 90 |
| Kittipol (2012) | 2084 | FI | OD | RGB | 45° | FCM | HE | 96.7 | 71.4 |
| Lee (2013) | 130 | FI | NA | Gray | 50° | Multi-model inference | NV | 96.3 | 99.1 |
| Nayak (2008) | 140 | FI | NA | NA | NA | ANN | NPDR PDR | 90.32 | 100 |
| Niemeijer (2007) | 300 | FI | NA | NA | 45° | Probability-based | DR | 95 | 86 |
| 70 | 93 | ||||||||
| 77 | 88 | ||||||||
| Maher (2015) | 130 | FI | MAC | RGB | NA | SVM | MAs | 95.6 | 94.86 |
| Júnior (2013) | 89 | FI | MAC | RGB | NA | ND | MAs, HM | 87.69 | 92.44 |
| Sinthanayothin (2002) | 44 | FI | OD, MAC | RGB | 45° | ANN | HE, MAs, HM | Exudates:88.5 | 99.7 |
| HMA:77.5 | 88.7 | ||||||||
| SujithKumar (2012) | NA | FI | MAC | Gray | NA | Rule-based | No DR; mild DR; moderate DR; severe DR | 89.65; 100; 100; 100 | 100; 88.88; 100; 100 |
| Torok (2015) | 52 | FI | MAC | NA | NA | Naive Bayes | MAs | 93 | 78 |
NA: Not accessible; MAs: Microaneurysms; HM: Hemorrhages; OD: Optic disc; MAC: Macula; HE: Hard exudates; NV: Neovascularization; SVM: Support vector machine; ANN: Artificial neural network; FCM: Fuzzy C-Means; FI: Fundus image; FA: Fluorescein angiogram; PDR: Proliferative DR; NPDR: Non-proliferative DR.
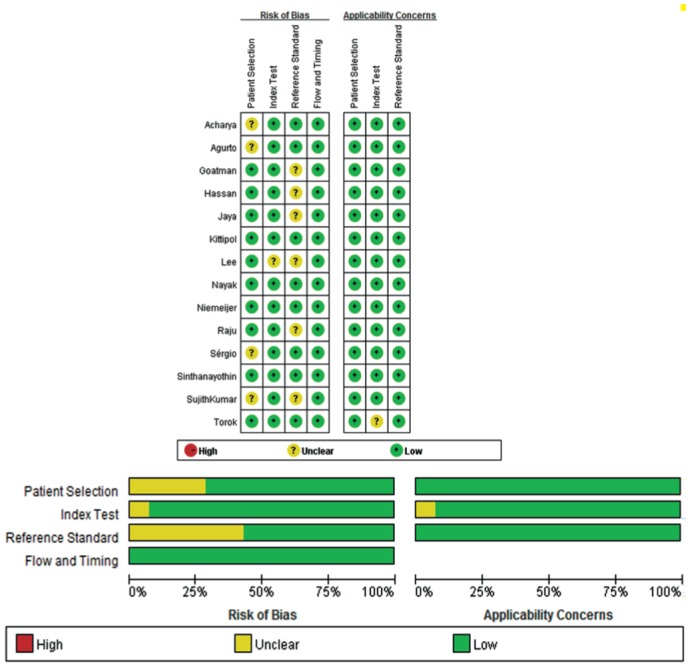
Quality of Included Studies
The methodological qualities of the included studies were illustrated in Figure 2. The overall quality of the included studies was variable. According to QUADAS-2, a good quality study was considered if it had prospective consecutive recruitment, with an adequate description of the study population, the diagnostic test and the reference standard. Besides, the study provided the diagnostic test had a definite reference standard. In this study, the selection of patients had introduced high bias in the study for the subject recruitment. The inclusion and exclusion criteria were clearly defined, with no inappropriate exclusions. The CAD methods for DR were adequately described in all included studies. However, the blindness in the included studies was not reported.
Figure 2. The diagram of the risk of bias, application concerns of each study and their ratio according to QUADAS-2.
Accuracy of Computer Aided Detection in Diabetic Retinopathy Detection
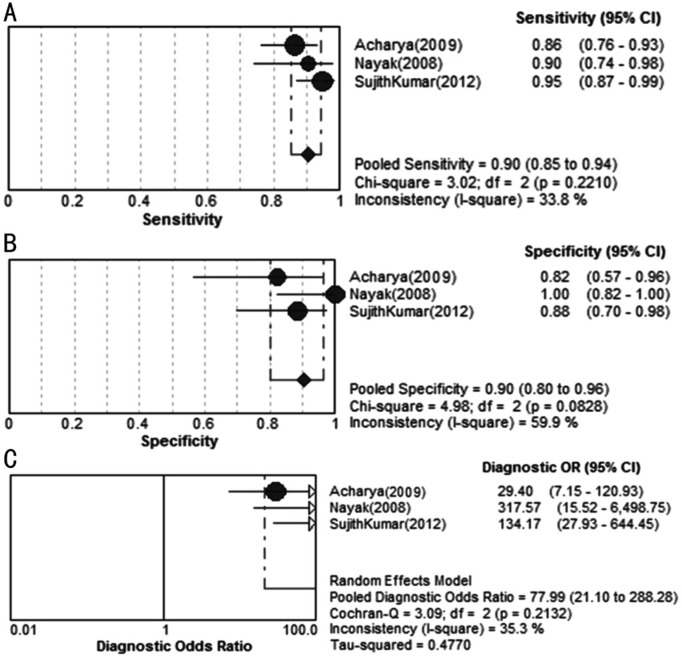
We used random effects model to estimate overall performance of CAD in DR detection (Figure 3).
Figure 3. Forest plots for sensitivity (A), specificity (B) and diagnostic odds ratio (C) of CAD in DR detection.
This figure showed the sensitivity and specificity of each study on the detection of DR. The pooled sensitivity and specificity reach 90% and 90%, respectively. Most of the I2 in sensitivity and specificity forest plots exceeded 50% with P value less than 0.05, indicating the significant heterogeneity among the included studies. The corresponding SROC curves indicated that AUC was 96.07% in the study on the grading of DR, and the pooled diagnostic accuracy (Q*) was greater than 0.9 (Q*=0.9055, SE=0.0384), showing an overall high accuracy of CAD in DR detection (Figure 4).
Figure 4. SROC curves of CAD in DR detection.
AUC: Area under the curve; SE: Standard error.
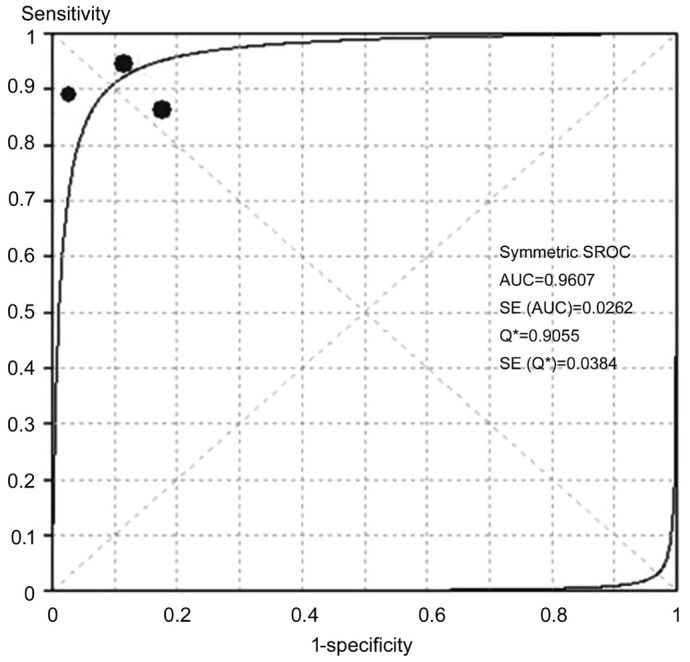
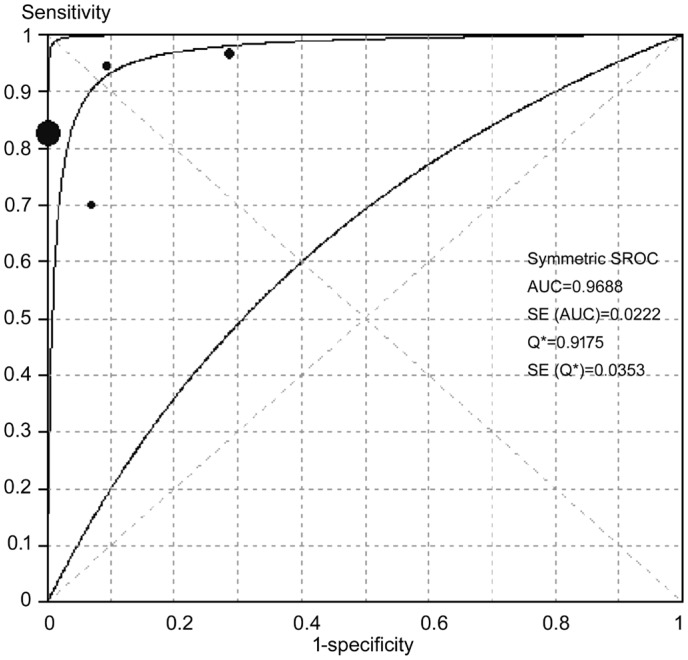
Accuracy of Computer Aided Detection in Exudates Detection
Figure 5 showed the sensitivity and specificity of each CAD study on detecting EXs. The pooled sensitivity and specificity reached 89% and 99%, respectively. Most of the I2 in sensitivity and specificity forest plots exceeded 50% with P value less than 0.05, indicating the significant heterogeneity among the included studies. The corresponding SROC curves showed that AUC was 96.88% in the study on the CAD of EXs detection, and the pooled diagnostic accuracy (Q*) was greater than 0.9 (Q*=0.9175, SE=0.0353), showing an overall high accuracy of CAD in EXs detection (Figure 6).
Figure 5. Forest plots for sensitivity (A), specificity (B) and diagnostic odds ratio (C) of CAD in EXs detection.
Figure 6. SROC curves of CAD in EXs detection.
AUC: Area under the curve; SE: Standard error.
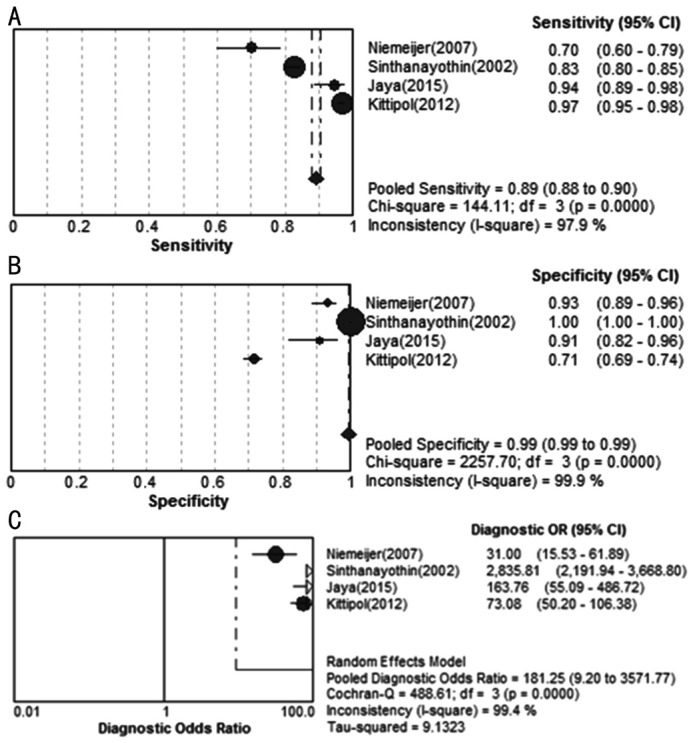
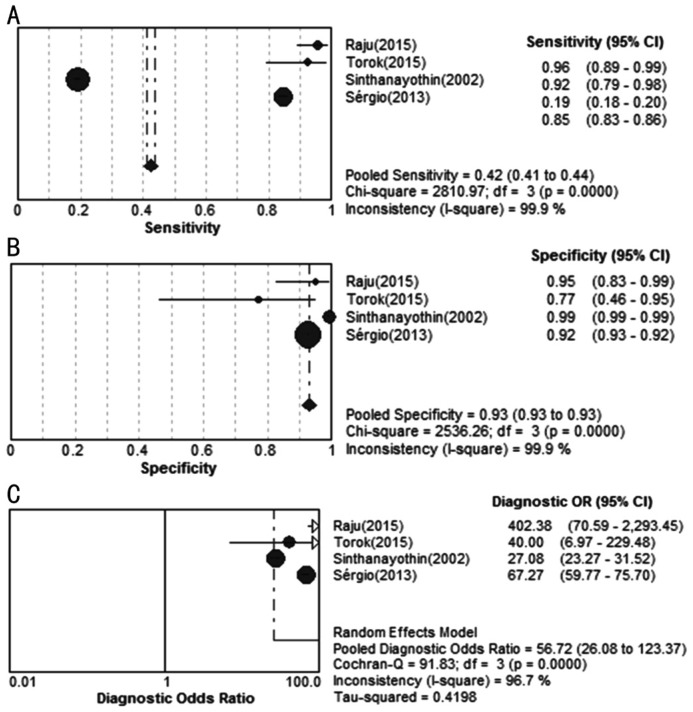
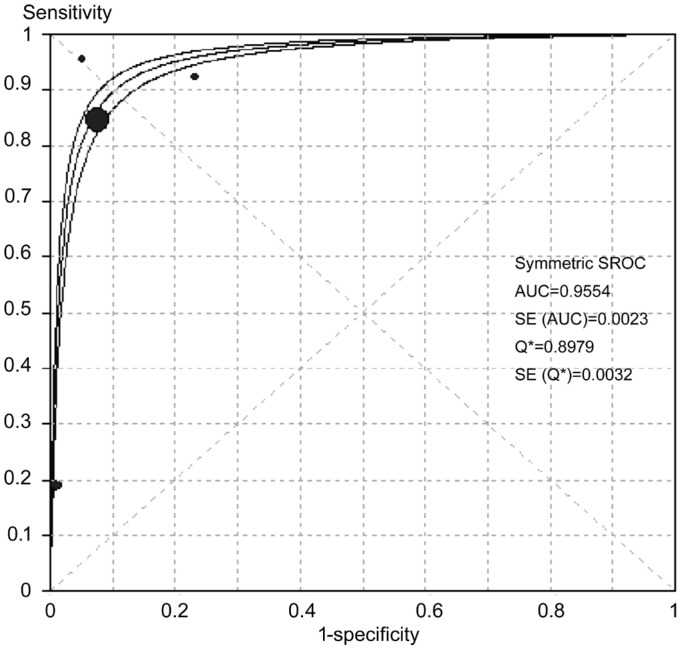
Accuracy of CAD in Microaneurysms and Hemorrhage Detection
Figure 7 showed the sensitivity and specificity of each CAD study on MAs and HM detection. The pooled sensitivity and specificity reach 42% and 93%, respectively. The corresponding SROC curves showed AUC was 95.54% in the study on MAs and HM, and the pooled diagnostic accuracy (Q*) was 0.8979 (SE=0.0032) in MAs and HM detection (Figure 8).
Figure 7. Forest plots for sensitivity (A), specificity (B) and diagnostic odds ratio (C) of CAD studies in detecting MAs and HM.
Figure 8. SROC curves of CAD in MAs and HM detecting AUC: Area under the curve; SE: Standard error.
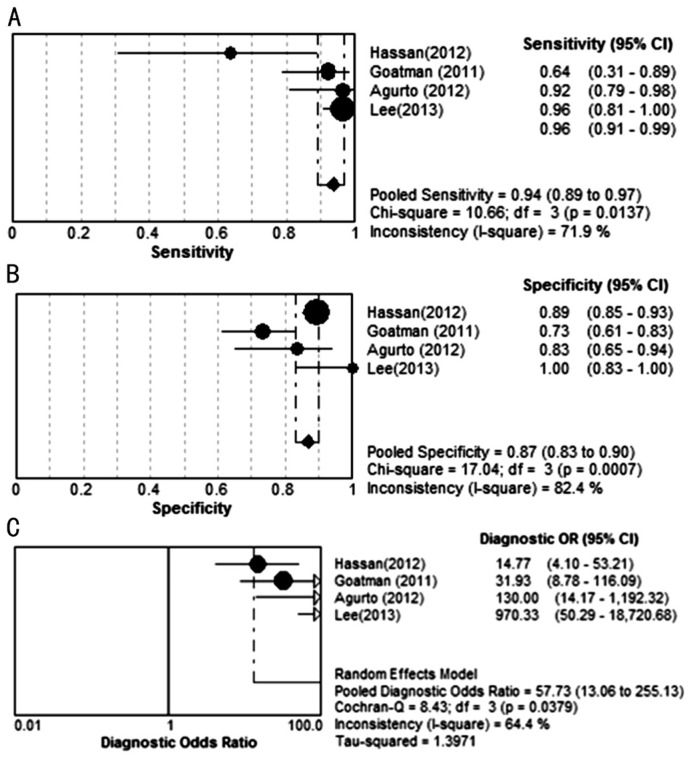
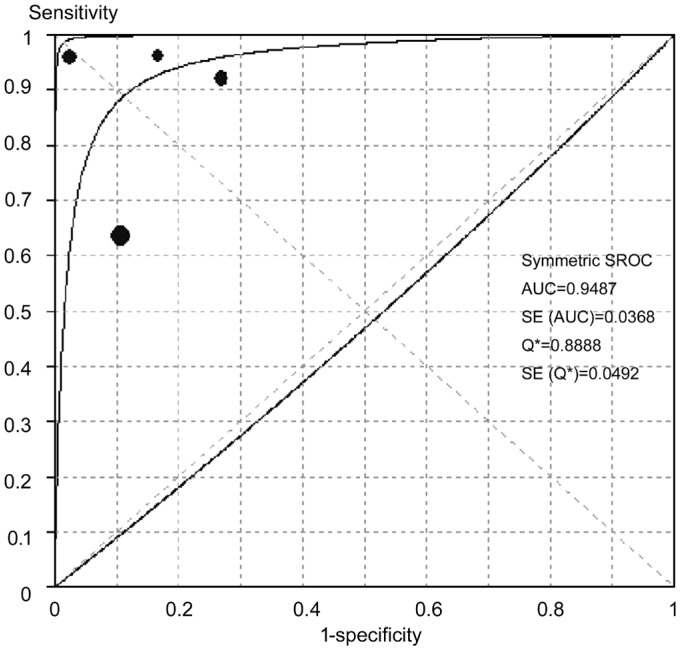
Accuracy of CAD in Neovascularizations Detection
Figure 9 showed the sensitivity and specificity of each study on NVs detection. The pooled sensitivity and specificity reached 94% and 87% respectively. The corresponding SROC curves showed AUC was 94.87% in the study on NV detection, and the pooled diagnostic accuracy (Q*) was greater than 0.9 (Q*=0.8888, SE=0.0492), showing an overall high accuracy of CAD in NV detecting (Figure 10).
Figure 9. Forest plots for sensitivity (A), specificity (B) and diagnostic odds ratio (C) of CAD studies in detecting NV.
Figure 10. SROC curves of varying retinal lesions been detected.
AUC: Area under the curve; SE: Standard error.
The summary of different detection results by CAD were shown in Table 2.
Table 2. Summary of different CAD detection results.
| Parameters | Different detections |
|||
| DR | EXs | MAs & HM | NV | |
| Se (95%CI) | 0.90 (0.85-0.94) | 0.89 (0.88-0.90) | 0.42 (0.41-0.44) | 0.94 (0.89-0.97) |
| Sp (95%CI) | 0.90 (0.80-0.96) | 0.99 (0.99-0.99) | 0.93 (0.93-0.93) | 0.87 (0.83-0.90) |
| PLR (95%CI) | 7.12 (3.40-14.93) | 20.33 (0.89-463.62) | 12.08 (5.30-27.56) | 5.24 (2.87-9.56) |
| NLR (95%CI) | 0.11 (0.06-0.21) | 0.12 (0.05-0.26) | 0.16 (0.03-1.04) | 0.10 (0.03-0.35) |
| DOR (95%CI) | 77.99 (21.10-288.28) | 181.25 (9.20-3571.77) | 56.72 (26.08-123.37) | 57.73 (13.06-255.13) |
MAs: Microaneurysms; EXs: Exudates; HM: Hemorrhage; NV: Neovascularization; DR: Diabetic retinopathy; Se: Sensitivity; Sp: Specificity; PLR: Positive likelihood ratio; NLR: Negative likelihood ratio; DOR: Diagnostic odds ratio.
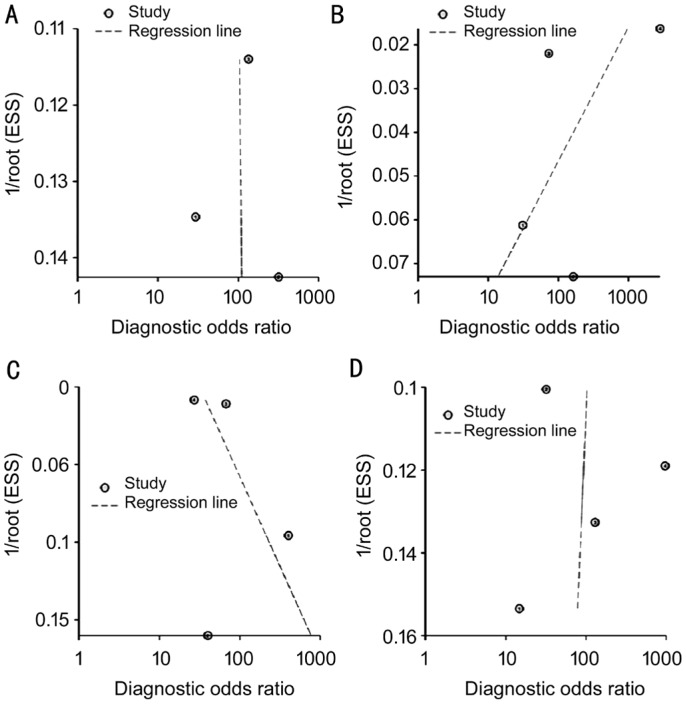
Publication Bias
The raw data of varying detected results was used to detect publication bias. Using Stata software, the Deeks'[19] test was performed to detect publication bias. As shown in Figure 11, there was no statistically significant for the studies of CAD in DR detection (P>0.05), suggesting no potential publication bias.
Figure 11. Test for the assessment of potential publication bias of CAD in DR and lesion detection.
A: DR, P=0.98; B: EXs, P=0.48; C: MAs and HM, P=0.63; D: NV, P=0.94.
DISCUSSION
The advantage of CAD system for DR detection is the ability to detect suspected DR patients from a large population in a short time. However, the reliability of such CAD system to take place of ophthalmologists for DR screening is still doubted. Automatic computer methods for retinal images processing have been developed for over 10y, and different CAD methods have been applied to detect retinal abnormalities. Preliminary studies used digitized OPs or fluorescein angiograms, but their usefulness was limited due to low image resolution[34]. The pre-processed methods such as thresholding, filtering and morphological operators were always utilized to enhance OP image quality before machine classifiers were used for CAD. In one study a BP-ANN was trained to recognize HMs and EXs on the OPs, and the effects of image processing techniques and different network parameters were evaluated. The hybrid forward propagation ANN some preliminary studies to make DR classification, and achieved 88% sensitivity[35], which is consistent with the pooled sensitivity 90% (95%CI: 85%-94%) in CAD detecting DR absence in this analysis.
Besides DR classification, another important function of the screening system is to detect and record abnormal lesions. DR can lead to several abnormalities, e.g. MA, HM, EX, NV, cotton wool spots, vessel geometric changes, and macular edema. Even though a screening system would have to take into account all of these abnormalities, this study majorly analyzed the detection of MA, HM, EX and NV, which all provide clues for DR severity. The components used for feature extraction could be classified as image-level, lesion-specific, and anatomical ones. We included CAD methods on different component classifications in the pool analysis. The pooled sensitivity was 89% (95%CI: 88%-90%) in EXs detecting, 42% (95%CI: 41%-44%) in MAs and HM detecting, 94% (95%CI: 89%-97%) in NV detecting, the specificity was higher than 85% in CAD detecting all kinds of DR lesions. These results suggested that CAD was valuable for DR detecting. The high value of AUC in SROC curves and Q* indicated that the overall high accuracy of CAD in DR detection. For DR lesions detecting, the diagnostic accuracy of CAD was higher in EXs and NV than that in MAs and HM. With respect to imaging center, the OD centered imaging have approximately the same sensitivities as macula centered imaging, suggesting no difference of the CAD performance.
Despite CAD techniques demonstrated overall high diagnostic accuracy for DR detection and the pathological lesions based on OP, there were still some limitations in this analysis. One limitation of this review was the existence of heterogeneity. The results of the Meta analysis with the covariates including aspects of subjects' characteristics, detection measures, and imaging techniques might not provide robust conclusion. Even after subgroup analysis according to different DR pathological changes, the heterogeneity was only partly meliorated. The methods of OP taken from included subjects were varied, which might be a source of heterogeneity too. Ensemble classifiers instead of certain CAD protocol were always utilized in DR classification, making separated classifier analysis difficult. Therefore, the different CAD methods were not pooled analyzed due to discrepancy of these classifiers. Moreover, the efficiencies of these CAD approaches were not validated in the same dataset. Another limitation was that some original data of three included studies unavailable and the data used in this Meta-analysis only from published manuscripts raising the possibility of selection bias. The differences between geographic areas and the changes of the optical means in older groups might compromise the sensitivity of the algorithms used. The modality of OP majorly investigated in this analysis is FI, while other modality like OCT has not been involved. Furthermore, latest CAD techniques of deep learning algorithms[10],[36]–[39] on DR detection or classification have not been included in this study, limiting the generalizability of our findings.
In summary, CAD techniques demonstrate overall high diagnostic accuracy for DR detecting and the pathological lesions based on OP, which can be used widely for DR screening. Prospective clinical trials are needed to prove such effect. Further research should focus on CAD by specific classification technique to and reasonable study design, which can avoid the heterogeneity across studies.
Acknowledgments
Foundations: Supported by National Key R&D Program of China (No.2018YFC1314900; No.2018YFC1314902); Nantong “226 Project”, Excellent Key Teachers in the “Qing Lan Project” of Jiangsu Colleges and Universities, Jiangsu Students' Platform for Innovation and Entrepreneurship Training Program (No.201910304108Y).
Conflicts of Interest: Wu HQ, None; Shan YX, None; Wu H, None; Zhu DR, None; Tao HM, None; Wei HG, None; Shen XY, None; Sang AM, None; Dong JC, None.
REFERENCES
- 1.Yau JW, Rogers SL, Kawasaki R, et al. Global prevalence and major risk factors of diabetic retinopathy. Diabetes Care. 2012;35(3):556–564. doi: 10.2337/dc11-1909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Resnikoff S, Pascolini D, Etya'ale D, Kocur I, Pararajasegaram R, Pokharel GP, Mariotti SP. Global data on visual impairment in the year 2002. Bull World Health Organ. 2004;82(11):844–851. [PMC free article] [PubMed] [Google Scholar]
- 3.Cheloni R, Gandolfi SA, Signorelli C, Odone A. Global prevalence of diabetic retinopathy: protocol for a systematic review and meta-analysis. BMJ Open. 2019;9(3):e022188. doi: 10.1136/bmjopen-2018-022188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Yun WL, Rajendra Acharya U, Venkatesh YV, Chee C, Min LC, Ng EYK. Identification of different stages of diabetic retinopathy using retinal optical images. Inf Sci. 2008;178(1):106–121. [Google Scholar]
- 5.Lim LS, Chee, Cheung CY, Wong TY. Retinal vessel geometry and the incidence and progression of diabetic retinopathy. Invest Ophthalmol Vis Sci. 2017;58(6):BIO200–BIO205. doi: 10.1167/iovs.17-21699. [DOI] [PubMed] [Google Scholar]
- 6.Cheung CY, Sabanayagam C, Law AK, Kumari N, Ting DS, Tan G, Mitchell P, Cheng CY, Wong TY. Retinal vascular geometry and 6 year incidence and progression of diabetic retinopathy. Diabetologia. 2017;60(9):1770–1781. doi: 10.1007/s00125-017-4333-0. [DOI] [PubMed] [Google Scholar]
- 7.Silva PS, El-Rami H, Barham R, Gupta A, Fleming A, van Hemert J, Cavallerano JD, Sun JK, Aiello LP. Hemorrhage and/or microaneurysm severity and count in ultrawide field images and early treatment diabetic retinopathy study photography. Ophthalmology. 2017;124(7):970–976. doi: 10.1016/j.ophtha.2017.02.012. [DOI] [PubMed] [Google Scholar]
- 8.Popovic N, Lipovac M, Radunovic M, Ugarte J, Isusquiza E, Beristain A, Moreno R, Aranjuelo N, Popovic T. Fractal characterization of retinal microvascular network morphology during diabetic retinopathy progression. Microcirculation. 2019:e12531. doi: 10.1111/micc.12531. [DOI] [PubMed] [Google Scholar]
- 9.Lin GM, Chen MJ, Yeh CH, Lin YY, Kuo HY, Lin MH, Chen MC, Lin SD, Gao Y, Ran AR, Cheung CY. Transforming retinal photographs to entropy images in deep learning to improve automated detection for diabetic retinopathy. J Ophthalmol. 2018;2018:2159702. doi: 10.1155/2018/2159702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gulshan V, Peng L, Coram M, Stumpe MC, Wu D, Narayanaswamy A, Venugopalan S, Widner K, Madams T, Cuadros J, Kim R, Raman R, Nelson PC, Mega JL, Webster DR. Development and validation of a deep learning algorithm for detection of diabetic retinopathy in retinal fundus photographs. JAMA. 2016;316(22):2402–2410. doi: 10.1001/jama.2016.17216. [DOI] [PubMed] [Google Scholar]
- 11.Kusakunniran W, Wu Q, Ritthipravat P, Zhang J. Hard exudates segmentation based on learned initial seeds and iterative graph cut. Comput Methods Programs Biomed. 2018;158:173–183. doi: 10.1016/j.cmpb.2018.02.011. [DOI] [PubMed] [Google Scholar]
- 12.Biyani RS, Patre BM. Algorithms for red lesion detection in diabetic retinopathy: a review. Biomedecine Pharmacother. 2018;107:681–688. doi: 10.1016/j.biopha.2018.07.175. [DOI] [PubMed] [Google Scholar]
- 13.Gardner GG, Keating D, Williamson TH, Elliott AT. Automatic detection of diabetic retinopathy using an artificial neural network: a screening tool. Br J Ophthalmol. 1996;80(11):940–944. doi: 10.1136/bjo.80.11.940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Goh J, Tang LL, Saleh G, Turk LA, Fu Y, Browne A. Filtering normal retinal images for diabetic retinopathy screening using multiple classifiers. 2009 9th International Conference on Information Technology and Applications in Biomedicine; November 4-7, 2009; Larnaka, Cyprus. New York, USA: IEEE; 2009. [Google Scholar]
- 15.Priya R, Aruna P. SVM and neural network based diagnosis of diabetic retinopathy. Int J Comput Appl. 2012;41(1):6–12. [Google Scholar]
- 16.Whiting PF, Rutjes AW, Westwood ME, Mallett S, Deeks JJ, Reitsma JB, Leeflang MM, Sterne JA, Bossuyt PM, QUADAS- Group QUADAS-2: a revised tool for the quality assessment of diagnostic accuracy studies. Ann Intern Med. 2011;155(8):529–536. doi: 10.7326/0003-4819-155-8-201110180-00009. [DOI] [PubMed] [Google Scholar]
- 17.Zamora J, Abraira V, Muriel A, Khan K, Coomarasamy A. Meta-DiSc: a software for meta-analysis of test accuracy data. BMC Med Res Methodol. 2006;6:31. doi: 10.1186/1471-2288-6-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327(7414):557–560. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Deeks JJ, Macaskill P, Irwig L. The performance of tests of publication bias and other sample size effects in systematic reviews of diagnostic test accuracy was assessed. J Clin Epidemiol. 2005;58(9):882–893. doi: 10.1016/j.jclinepi.2005.01.016. [DOI] [PubMed] [Google Scholar]
- 20.Acharya UR, Lim CM, Ng EY, Chee C, Tamura T. Computer-based detection of diabetes retinopathy stages using digital fundus images. Proc Inst Mech Eng H. 2009;223(5):545–553. doi: 10.1243/09544119JEIM486. [DOI] [PubMed] [Google Scholar]
- 21.Agurto C, Yu HG, Murray V, Pattichis MS, Barriga S, Bauman W, Soliz P. Detection of neovascularization in the optic disc using an AM-FM representation, granulometry, and vessel segmentation. Conf Proc IEEE Eng Med Biol Soc. 2012;2012:4946–4949. doi: 10.1109/EMBC.2012.6347102. [DOI] [PubMed] [Google Scholar]
- 22.Goatman KA, Fleming AD, Philip S, Williams GJ, Olson JA, Sharp PF. Detection of new vessels on the optic disc using retinal photographs. IEEE Trans Med Imaging. 2011;30(4):972–979. doi: 10.1109/TMI.2010.2099236. [DOI] [PubMed] [Google Scholar]
- 23.Hassan SS, Bong DB, Premsenthil M. Detection of neovascularization in diabetic retinopathy. J Digit Imaging. 2012;25(3):437–444. doi: 10.1007/s10278-011-9418-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Jaya T, Dheeba J, Singh NA. Detection of hard exudates in colour fundus images using fuzzy support vector machine-based expert system. J Digit Imaging. 2015;28(6):761–768. doi: 10.1007/s10278-015-9793-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kittipol W, Nualsawat H, Ekkarat P. Automatic detection of exudates in diabetic retinopathy images. J Comput Sci. 2012;8(8):1304–1313. [Google Scholar]
- 26.Lee J, Zee BC, Li Q. Detection of neovascularization based on fractal and texture analysis with interaction effects in diabetic retinopathy. PLoS One. 2013;8(12):e75699. doi: 10.1371/journal.pone.0075699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Nayak J, Bhat PS, Acharya R, Lim CM, Kagathi M. Automated identification of diabetic retinopathy stages using digital fundus images. J Med Syst. 2008;32(2):107–115. doi: 10.1007/s10916-007-9113-9. [DOI] [PubMed] [Google Scholar]
- 28.Niemeijer M, van Ginneken B, Russell SR, Suttorp-Schulten MS, Abràmoff MD. Automated detection and differentiation of drusen, exudates, and cotton-wool spots in digital color fundus photographs for diabetic retinopathy diagnosis. Invest Ophthalmol Vis Sci. 2007;48(5):2260–2267. doi: 10.1167/iovs.06-0996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Maher R, Kayte S, Panchal D, Bhable SG, Sathe P, Kayte J. Automatic diagnosis of diabetic retinopathy micro aneurysm from low contrast retinal images using mathematical morphology methods. Int J Comput Appl. 2015;130(6):50–56. [Google Scholar]
- 30.Júnior SB, Welfer D. Automatic detection of microaneurysms and hemorrhages in color eye fundus images. Int J Comput Sci Inf Technol. 2013;5(5):21–37. [Google Scholar]
- 31.Sinthanayothin C, Boyce JF, Williamson TH, Cook HL, Mensah E, Lal S, Usher D. Automated detection of diabetic retinopathy on digital fundus images. Diabet Med. 2002;19(2):105–112. doi: 10.1046/j.1464-5491.2002.00613.x. [DOI] [PubMed] [Google Scholar]
- 32.SujithKumar SB, Vipula S. Automatic detection of diabetic retinopathy in non-dilated RGB retinal fundus images. Int J Comput Appl. 2012;47(19):26–32. [Google Scholar]
- 33.Torok Z, Peto T, Csosz E, Tukacs E, Molnar AM, Berta A, Tozser J, Hajdu A, Nagy V, Domokos B, Csutak A. Combined methods for diabetic retinopathy screening, using retina photographs and tear fluid proteomics biomarkers. J Diabetes Res. 2015;2015:623619. doi: 10.1155/2015/623619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Rapkin JS, Rapkin KM, Wilson GW. Digital fundus imaging: a comparison with photographic techniques. Ann Ophthalmol. 1991;23(2):46–53. [PubMed] [Google Scholar]
- 35.Lichode RV, Kulkarni PS. Automatic diagnosis of diabetic retinopathy by hybrid multilayer feed forward neural network. Inter J Sci Engin Tech Res. 2013;2(9):1727–1733. [Google Scholar]
- 36.Eftekhari N, Pourreza HR, Masoudi M, Ghiasi-Shirazi K, Saeedi E. Microaneurysm detection in fundus images using a two-step convolutional neural network. Biomed Eng Online. 2019;18(1):67. doi: 10.1186/s12938-019-0675-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Li F, Chen H, Liu Z, Zhang XD, Wu ZZ. Fully automated detection of retinal disorders by image-based deep learning. Graefes Arch Clin Exp Ophthalmol. 2019;257(3):495–505. doi: 10.1007/s00417-018-04224-8. [DOI] [PubMed] [Google Scholar]
- 38.Lam C, Yu C, Huang L, Rubin D. Retinal lesion detection with deep learning using image patches. Invest Ophthalmol Vis Sci. 2018;59(1):590–596. doi: 10.1167/iovs.17-22721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Saha SK, Fernando B, Xiao D, Tay-Kearney ML, Kanagasingam Y. Deep learning for automatic detection and classification of microaneurysms, hard and soft exudates, and hemorrhages for diabetic retinopathy diagnosis. Invest Ophthalmol Vis Sci. 2016;57(12):5962–5962. [Google Scholar]