Abstract
Background
Performing mechanical thrombectomy (MT) in patients with basilar artery occlusion (BAO) is currently not evidence-based.
Objective
To compare patients’ outcome, relative merits of achieving recanalization, and predictors of futile recanalization (FR) between BAO and anterior circulation large vessel occlusion (ACLVO) MT.
Methods
In the multicenter BEYOND-SWIFT registry (NCT03496064), univariate and multivariate (displayed as adjusted Odds Ratios, aOR and 95% confidence intervals, 95%-CI) outcome comparisons between BAO (N=165) and ACLVO (N=1574) were performed. The primary outcome was favorable outcome at 90 days (modified Rankin Scale, mRS 0-2). Secondary outcome included mortality, symptomatic intracranial hemorrhage (sICH) and FR. The relative merits of achieving successful recanalization between ACLVO and BAO were evaluated with interaction terms.
Results
MT in BAO was more often technically effective and equally safe in regards to mortality and sICH when compared to ACLVO. When adjusting for baseline differences, there was no significant difference between BAO vs ACLVO regarding rates of favorable outcome (aOR 0.986, 95%-CI 0.553 – 1.758). However, BAO were associated with increased rates of FR (aOR 2.146, 95%-CI 1.267 – 3.633). Predictors for FR were age, stroke severity, maneuver count and intracranial stenting. No significant heterogeneity on the relative merits of achieving successful recanalization on several outcome parameters were observed when comparing BAO and ACLVO.
Conclusions
In selected patients, similar outcomes can be achieved in BAO and ACLVO patients treated with MT. Randomized controlled trials comparing patient selection and interventional strategies seem warranted to avoid FR.
Trial registration number
Keywords: angiography, intervention, stroke, thrombectomy, thrombolysis
Introduction
About 1% of patients with acute ischemic stroke have a basilar artery occlusion (BAO) that is amendable to endovascular treatment.1 2 Such patients present with particularly severe symptoms and have a poor prognosis compared with those with anterior circulation large vessel occlusion (ACLVO).3 4
In patients with BAO and other large vessel occlusions (LVOs) of the posterior circulation (PC), indications for mechanical thrombectomy (MT) lack evidence derived from large pivotal thrombectomy trials.5 6 Intravenous thrombolysis (IVT) is therefore the standard of care in those patients.7 Yet, IVT yields insufficient acute reperfusion rates in patients with BAO.8–13 Therefore, many patients subsequently deteriorate clinically and tend to have poor outcomes if reperfusion is not achieved.8 14
Recanalization rates of MT were reported to be lower than with AC occlusions and procedure time longer.15 Furthermore in BAO, poor outcome despite successful recanalization by MT was reported to occur more frequently—a phenomenon termed futile recanalization (FR) (modified Rankin Scale (mRS) score 4–6 despite complete recanalization).15–18 In this setting, ethics and patient preferences are taken into account when considering the risk of subjecting patients to a treatment that may avoid death but instead creates long-term dependence.19 20 Efforts have been made to identify predictors of FR in BAO—namely, stroke severity on admission, amount of radiological lesion on baseline MRI or CT, respiratory instability, and collateral quality.16–18 21 22 Despite those efforts, the rates of long-term dependence were reported to be around 30%23 after MT in BAO.
Although several studies have reported predictors of outcome after endovascular therapy in patients with BAO, few studies have focused solely on MT. Furthermore, reports were limited by small numbers of patients, non-transparent patient selection, heterogeneous endovascular treatments, and inclusion of patients with more distal occlusions.
The aims of this study were hence to compare patients’ outcome, the relative merits of achieving recanalization, predictors of FR, and procedural safety between BAO and ACLVO MT, and predictors of FR in BAO.
Methods
Details of the BEYOND-SWIFT Registry are in the public domain (NCT03496064) and have been published previously.24 Briefly, the registry is a retrospective, multicenter, non-randomized observational study designed to investigate the safety and efficacy of a Medtronic market-released neurothrombectomy device (applied as the initial device used for interventions) in patients with acute ischemic stroke who do not fulfill treatment eligibility requirements according to the current guidelines. An overview of the patients included in the registry, the follow-up data for each center, and ethical approval procedures can be found in online supplementary table I. Ethical approval was obtained in Bern for pooling and analyses of the registry data (KEK Bern, Bern, Switzerland ID 2018–00766).
neurintsurg-2018-014516supp001.docx (24.4KB, docx)
Most patients included in the registry (n=2046) were treated for large-vessel anterior circulation strokes (n=1832). Of the patients treated for BAO (n=165), 152 (92.1%) had documented 90-day follow-up. Selection criteria for performing MT in BAO were center-specific and are presented in online supplementary table 5.
Variables and image analysis
Local investigators categorized the site of LVO into vertebral artery, basilar artery, or first/second segment of the posterior cerebral artery (P1/P2) occlusions. For the main analysis we compared patients with BAO with those with iICA/carotid-T/M1-occlusions. Either the operator at each center or an independent research fellow rated the postprocedural modified Thrombolysis in Cerebral Infarction (mTICI) score (see online supplementary table I). mTICI 2b was rated as reperfusion of at least 50% of the initially occluded target vessel territory, according to modifications of the TICI scale.25 For clinical outcome evaluation, we assessed 3-month functional outcomes using the mRS score in routinely scheduled clinical visits or standardized telephone interviews organized at each center. FR was defined as successful recanalization in patients with mRS score 4–6 at 90 days.20 Worsening in the National Institutes of Health Stroke Scale (NIHSS) score of ≥4 points between the admission NIHSS score and the score 24 hours later, and not attributable to an intracerebral hemorrhagic event was defined as non-hemorrhagic worsening.26
Statistical analysis
Univariate comparisons between patients with BAO or ACLVO, between patients with favorable outcome (mRS score 0–2) and patients with unfavorable outcome (mRS score 3–6), as well as between patients with futile and non-futile recanalization were made using standard statistical measures (Fisher’s exact test for categorical variables, Mann–Whitney U test for non-normally continuous or ordinally scaled variables, and Welsch’s t-test for independent normally distributed data).
The primary endpoint of this analysis was favorable outcome at 90 days (mRS score 0–2) in BAO versus ACLVO according to multivariate analysis. Secondary outcomes consisted of rate of successful recanalization, FR, all-cause mortality at day 90, overall complication rate, and symptomatic intracerebral hemorrhage (sICH), which was assessed at each center by applying the ECASS II criteria, although they were originally established for AC strokes. The association between BAO versus ACLVO with all of the previously listed outcome parameters was hence assessed using multivariable logistic regression with adjustments for the following confounders: age (continuous), prestroke independence (categorical), NIHSS score on admission (ordinal, adjusted odds ratio (aOR) per point increase), systolic blood pressure (metric, aOR per mm Hg increase), known onset (categorical), risk factor hypertension (categorical), risk factor smoking (categorical), risk factor previous stroke (categorical), risk factor diabetes (categorical), type of admission imaging (CT vs MRI, categorical), IVT (categorical), and time from symptom onset to admission (metric, aOR per minute increase). The adjustments were made according to significant baseline differences in univariate analysis, except for admission glucose levels and history of coronary heart disease since too many data items were missing.
A potential difference in the relative merits of achieving successful recanalization between BAO and ACLVO was evaluated with interaction terms. For this comparison, we assessed the relative effect of successful recanalization on various dichotomizations of functional outcome and safety parameters using multivariable logistic regression with adjustments for the following prespecified confounders: age (continuous), sex (categorical), NIHSS score on admission (ordinal, aOR per point increase) and IVT (categorical). The adjustments for this analysis were made according to a clinical assumption of the main confounders as the restricted number of patients without successful recanalization limited the number of variables that could be included.
Results
Baseline
For baseline differences, the 165 patients with BAO were younger, more often male, more often transferred from other hospitals, had more severe symptoms on admission, higher glucose on admission, less often anticoagulation pretreatment, less often hypertension, less often dyslipidemia, other TOAST etiology, and MRI was less often performed as the initial imaging modality (table 1) as compared with ACLVO. Furthermore, time from symptom onset to groin puncture was longer in BAO than in ACLVO (median 300 min vs 225 min, p<0.001).
Table 1.
Baseline characteristics comparing patients with basilar artery occlusion and patients with large vessel occlusion in the anterior circulation
| Characteristics | BAO (n=165) | ACLVO (intracranial carotid artery, carotid-T, M1) (n=1574) | P value |
| Clinical items | |||
| Age (years) | 70 (59–80), N=165 | 73 (61–82), N=1574 | 0.019 |
| Transfer from another hospital | 80/165 (48.5%) | 561/1572 (35.7%) | 0.002 |
| Sex (female) | 69/165 (41.8%) | 810/1574 (51.5%) | 0.022 |
| NIHSS on admission | 18 (8–30), N=155 | 17 (12–20), N=1558 | 0.046 |
| Prestroke independence | 149/164 (90.9%) | 1446/1556 (92.9%) | 0.341 |
| Blood pressure systolic (mm Hg) | 148 (SD 31), N=86 | 150 (SD 28), N=1141 | 0.413 |
| Blood pressure diastolic (mm Hg) | 78 (SD 16), N=86 | 82 (SD 20), N=1139 | 0.097 |
| Admission glucose (mmol/L) | 7.5 (6.4–9.7), N=93 | 6.6 (5.8–8.1), N=1181 | <0.001 |
| Wake-up stroke | 13/161 (8.1%) | 123/1451 (8.5%) | 1.000 |
| TOAST etiology | 0.008 | ||
| Large artery | 37/163 (22.7%) | 205/1546 (13.3%) | |
| Cardioembolic | 64/163 (39.3%) | 733/1546 (47.4%) | |
| Other specific etiology | 12/163 (7.4%) | 101/1546 (6.5%) | |
| Unknown etiology | 50/163 (30.7%) | 507/1546 (32.8%) | |
| Medication | 0.058 | ||
| Antiplatelet | |||
| Monotherapy | 36/154 (23.4%) | 430/1463 (29.4%) | |
| Dual therapy | 0 (0%) | 26/1463 (1.8%) | |
| Statin | 32/142 (22.5%) | 395/1300 (30.4%) | 0.053 |
| Anticoagulation | 0.014 | ||
| VKA | 10/154 (6.5%) | 180/1464 (12.3%) | |
| NOAC | 2/154 (1.3%) | 64/1464 (4.4%) | |
| Risk factors | |||
| Diabetes | 23/163 (14.1%) | 271/1555 (17.4%) | 0.326 |
| Arterial hypertension | 87/163 (53.4%) | 1046/1553 (67.4%) | <0.001 |
| Dyslipidemia | 60/161 (37.3%) | 788/1547 (50.9%) | 0.001 |
| Smoking | 47/153 (30.7%) | 428/1499 (28.6%) | 0.574 |
| Previous stroke | 17/159 (10.7%) | 209/1565 (13.4%) | 0.389 |
| Coronary artery disease | 17/83 (20.5%) | 235/1131 (20.8%) | 1.000 |
| Type of imaging | 0.010 | ||
| MRI | 42/165 (25.5%) | 994/1544 (64.4%) | |
| CT | 123/165 (74.5%) | 550/1544 (35.6%) | |
| Treatment | |||
| IVT use | 71/165 (43.0%) | 779/1574 (49.5%) | 0.120 |
| Time from onset of symptoms to IVT needle (min) | 165 (113–210), N=39/71 | 120 (83–165), N=437/779 | 0.003 |
| Time from onset of symptoms to admission in stroke center (min) | 228 (IQR 121–369), N=132 | 143 (71–245), N=1380 | <0.001 |
| Time from onset of symptoms to groin puncture (min) | 300 (IQR 211–480), N=133 | 225 (165–315), N=1346 | <0.001 |
ACLVO, anterior circulation large-vessel occlusion; BAO, basilar artery occlusion; IVT, intravenous thrombolysis; NIHSS, National Institutes of Health Stroke Scale; NOAC, non-vitamin K antagonist oral anticoagulants;TOAST, Trial of ORG 10172 in Acute Stroke Treatment; VKA, vitamin K antagonist. Difference in numbers of observations and total numbers of patients in each group due to missing data items.
Technical efficacy
Comparison of MT in patients with BAO and patients with ACLVO showed that the procedure was more often effective in BAO, with achievement of a mTICI 3 recanalization in 61.8% and a mTICI 2b/3 in 90.3% of patients requiring fewer maneuvers (p=0.002). Groin puncture to recanalization intervals in patients with BAO were similar to those in ACLVO (median 45 min vs 47 min, p=0.824). However, more intracranial stents were used in patients with BAO (17.0% vs 2.3%, p<0.001) and longer times from symptom onset to groin-puncture (300 min vs 225 min, p<0.001) were noted, probably because interventions usually required general anesthesia (88.2% vs 54.9%, p<0.001) (table 2). Also on multivariate analysis with adjustments for baseline differences, MT in BAO was associated with higher odds of achieving TICI 3 (aOR=2.004, 95% CI 1.227 to 3.274, p=0.005) and successful recanalization ≥TICI 2b (aOR=2.740, CI 1.145 to 6.554).
Table 2.
Safety and efficacy data comparing patients with basilar artery occlusion and patients with large vessel occlusion in the anterior circulation
| MT of BAO (n=165) | MT of ACLVO (n=1574) | P value | |
| Efficacy | |||
| mTICI 3 | 102/165 (61.8%) | 706/1571 (44.9%) | <0.001 |
| mTICI ≥2b | 149/165 (90.3%) | 1299/1571 (82.7%) | 0.011 |
| Time from groin puncture to recanalization (min) | 45 (30–81), N=153 | 47 (30–75), N=1471 | 0.824 |
| General anesthesia | 142/161 (88.2%) | 792/1442 (54.9%) | <0.001 |
| Additional intra-arterial thrombolytic agents | 18/160 (11.3%) | 112/1443 (7.8%) | 0.127 |
| Maneuver count | 1 (IQR 1–2), N=101 | 2 (1–3), N=1106 | 0.002 |
| Intracranial stenting | 28/165 (17.0%) | 36/1572 (2.3%) | <0.001 |
| Extracranial stenting | 13/165 (7.9%) | 182/1572 (11.6%) | 0.194 |
| Safety | |||
| sICH ECASS II definition | 8/165 (4.8%) | 98/1562 (6.3%) | 0.608 |
| Systemic bleeding | 1/39 (2.6%) | 21/637 (3.3%) | 1.000 |
| Craniectomy | 4/161 (2.5%) | 51/1448 (3.5%) | 0.649 |
| Any interventional complication | 18/165 (10.9%) | 198/1572 (12.6%) | 0.620 |
| Complications |
|
|
ACLVO, anterior circulation large vessel occlusion; BAO, basilar artery occlusion; MT, mechanical thrombectomy; mTICI, modified Thrombolysis in Cerebral Infarction; sICH, symptomatic intracranial hemorrhage according to the European Cooperative Acute Stroke Study II definition. Difference in numbers of observations and total numbers of patients in each group due to missing data items.
Safety
Safety endpoints, including sICH, systemic bleeding, craniectomy, and complication rates, were less frequent in patients with BAO than in patients with ACLVO (table 2), but the difference did not reach statistical significance. Also on multivariate analysis, MT in BAO as compared with ACLVO was not associated with either sICH (aOR=0.773, 95% CI 0.228 to 2.618) or mortality (aOR=1.612, 95% CI 0.891 to 2.918). However, patients with MT in BAO more often had postinterventional non-hemorrhagic worsening (aOR=2.797, CI 1.366 to 5.726) than in ACLVO.
Outcome
Patients with BAO had worse outcomes than patients with ACLVO, as shown by a lower rate of moderate outcome (mRS score 0–3, 46.1% vs 56.7%, p=0.013) and a higher mortality rate (36.2% vs 24.4%, p=0.002), although rates of excellent functional outcome (mRS score 0–1, 25.0% vs 27.3%, p=0.631) and favorable outcome (mRS score 0–2, 36.2% vs 42.9%, p=0.120) were comparable in an unadjusted analysis (online supplementary table 2).
Baseline differences of patients with favorable outcome (mRS score 0–2) and unfavorable outcome (mRS score 3–6) can be found in online supplement table 3 and favoured neither BAO nor ACLVO. After adjusting for baseline differences, there was no significant difference in excellent (aOR=0.893, 95% CI 0.478 to 1.669), favorable (primary outcome, aOR=0.986, 95% CI 0.553 to 1.758, figure 1) and moderate functional outcome at 90 days (aOR=0.692, 95% CI 0.396 to 1.121).
Figure 1.
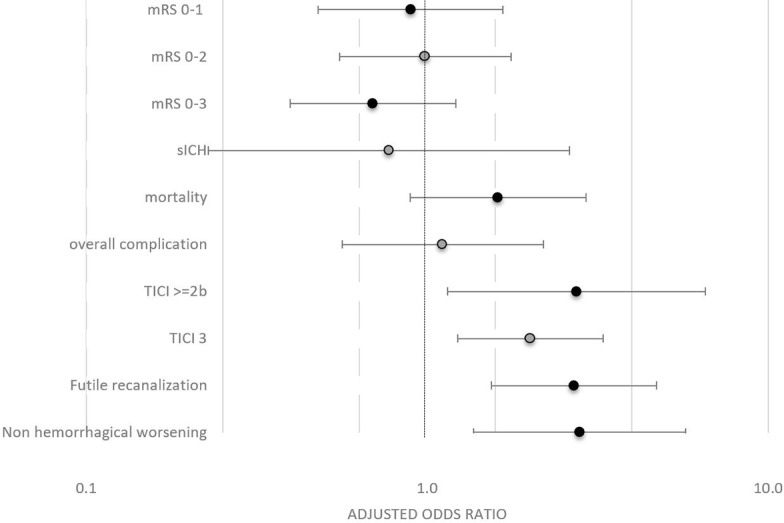
Comparison of outcomes of mechanical thrombectomy (MT) in posterior versus anterior circulation. Adjusted OR of MT in basilar artery occlusion versus anterior circulation large vessel occlusion for outcome parameters in the binary multivariable logistic regression analysis, adjusting for age, National Institutes of Health Stroke Scale score on admission, systolic blood pressure, prestroke independence, known onset, diabetes, arterial hypertension, smoking, previous stroke, imaging type, intravenous thrombolysis, and time from onset to admission. mRS, modified Rankin scale; sICH, symptomatic intracranial hemorrhage; TICI, Thrombolysis in Cerebral Infarction.
In conclusion, patients with BAO had worse outcomes on univariate analysis, but after adjustment for baseline differences, we could observe no significant differences of outcome of MT in BAO vs ACLVO, except an increased occurrence of FR.
FR was found more often in BAO than in ACLVO (aOR=2.146, CI 1.267 to 3.633). Factors associated with FR in univariate analysis were older age, higher stroke severity, coronary artery disease, higher maneuver count, and intracranial stenting (table 3). Prestroke dependence, lower posterior circulation Alberta Stroke Program Early CT Score (pcASPECTS), longer time from groin puncture to recanalization and administration of additional intra-arterial thrombolytic agents showed a trend towards association with FR.
Table 3.
Baseline and interventional differences of patients with futile and non-futile reperfusion
| Futile recanalization (n=70) | Non-futile recanalization (n=79) | P value | |
| Clinical items | |||
| Age (years) | 74 (63–81), N=70 | 67 (57–79), N=79 | 0.025 |
| Transfer from another hospital | 34/70 (48.6%) | 37/79 (46.8%) | 0.870 |
| Sex (female) | 34/70 (48.6%) | 30/79 (38.0%) | 0.246 |
| NIHSS score on admission | 21 (12–36), N=65 | 12 (6–23), N=75 | 0.002 |
| Prestroke independence | 60/70 (85.7%) | 75/79 (94.9%) | 0.089 |
| Blood pressure systolic (mm Hg) | 154 (SD 32), N=41 | 144 (SD 28), N=39 | 0.170 |
| Blood pressure diastolic (mm Hg) | 78 (SD 17), N=41 | 78 (SD 15), N=39 | 0.840 |
| Admission glucose (mmol/L) | 7.6 (6.3–9.3), N=45 | 7.4 (6.4–9.8), N=41 | 0.959 |
| Noticed symptom onset | 50/70 (71.4%) | 62/79 (78.5%) | 0.347 |
| Wake up | 7/70 (10.0%) | 5/77 (6.5%) | 0.551 |
| In-hospital stroke | 2/70 (2.9%) | 0/79 | 0.219 |
| Medication | 0.417 | ||
| Antiplatelet | |||
| Monotherapy | 17/67 (25.4%) | 14/75 (18.7%) | |
| Dual therapy | 0/67 | 0/75 | |
| Statin | 15/63 (23.8%) | 12/69 (17.4%) | 0.394 |
| Anticoagulation | 0.401 | ||
| None | 63/67 (94.0%) | 69/75 (92.0%) | |
| VKA | 4/67 (6.0%) | 4/75 (5.3%) | |
| NOAC | 0/67 | 2/75 (2.7%) | |
| Risk factors | |||
| Diabetes | 10/69 (14.5%) | 9/79 (11.4%) | 0.628 |
| Arterial hypertension | 36/69 (52.2%) | 40/79 (50.6%) | 0.870 |
| Dyslipidemia | 26/67 (38.8%) | 26/79 (32.9%) | 0.491 |
| Smoking | 16/65 (24.6%) | 25/74 (33.8%) | 0.267 |
| Previous stroke | 8/67 (11.9%) | 8/79 (10.1%) | 0.794 |
| Coronary artery disease | 11/35 (31.4%) | 4/40 (10.0%) | 0.040 |
| TOAST etiology |
0.286 | ||
| Large artery | 13/69 (18.8%) | 21/79 (26.6%) | |
| Cardioembolic | 27/69 (39.1%) | 33/79 (41.8%) | |
| Other specific etiology | 4/69 (5.8%) | 7/79 (8.9%) | |
| Unknown etiology | 25/69 (36.2%) | 18/79 (22.8%) | |
| Type of imaging | 1.000 | ||
| MRI | 16/70 (22.9%) | 19/79 (24.1%) | |
| CT | 54/70 (77.1%) | 60/79 (75.9%) | |
| pcASPECTS | 7 (5–9), N=25 | 8 (7–9), N=24 | 0.076 |
| Treatment | |||
| IVT use | 29/70 (41.4%) | 33/79 (41.8%) | 1.000 |
| Time from onset of symptoms to IVT needle (min) | 165 (117–225), N=21/29 | 178 (109–228), N=16/33 | 0.914 |
| Time from onset of symptoms to admission (min) | 240 (122–446), N=55 | 222 (112–335), N=67 | 0.231 |
| Time from onset of symptoms to groin puncture (min) | 305 (211–539), N=55 | 300 (200–450), N=67 | 0.365 |
| Time groin to recanalization (min) | 47 (34–86), N=67 | 41 (28–68), N=76 | 0.096 |
| General anesthesia | 61/70 (87.1%) | 68/77 (88.3%) | 1.000 |
| Additional intra-arterial thrombolytic agents | 11/70 (15.7%) | 4/76 (5.3%) | 0.055 |
| Balloon-guiding catheter | 2/70 (2.9%) | 7/76 (9.2%) | 0.169 |
| Intracranial stent | 17/70 (24.3%) | 7/79 (8.9%) | 0.014 |
| Extracranial stent | 3/70 (4.3%) | 8/79 (10.1%) | 0.219 |
| Any interventional complication | 7/70 (10.0%) | 6/79 (7.6%) | 0.773 |
| Maneuver | 1 (1–2), N=45 | 1 (1–2), N=50 | 0.016* |
| sICH ECASS II | 2/70 (2.9%) | 2/79 (2.5%) | 1.000 |
*Maneuver count higher in futile recanalization.
IVT, intravenous thrombolysis; NIHSS, National Institutes of Health Stroke Scale; NOAC, non-vitamin K antagonist oral anticoagulants; pcASPECTS, posterior circulation Alberta Stroke Program Early CT Score; sICH, symptomatic intracranial hemorrhage according to the European Cooperative Acute Stroke Study II definition; TOAST, Trial of ORG 10172 in Acute Stroke Treatment; VKA, vitamin K antagonist. Difference in numbers of observations and total numbers of patients in each group due to missing data items.
On unadjusted analysis, better outcomes were observed in patients with successful recanalization of BAO (online supplement table 4) as compared with patients without successful recanalization. The relative benefit of achieving successful recanalization for various dichotomizations of the mRS scale, mortality, and sICH were comparable between patients presenting with recanalization of BAO and ACLVO according to multivariable binary logistic regression analysis, adjusting for prespecified confounders outlined in the methods section (figure 2). However, significantly higher rates of independence at 3 months were found only in the cohort of patients presenting with ACLVO.
Figure 2.
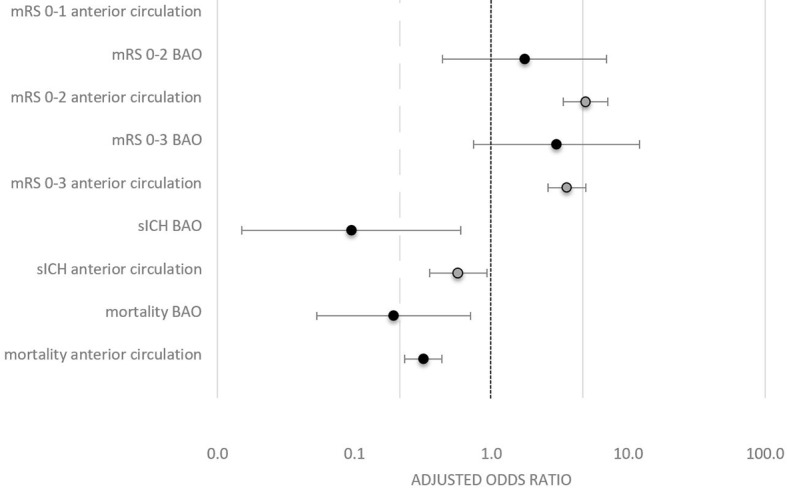
Effect of successful reperfusion on outcomes stratified for posterior versus anterior circulation. Adjusted OR of achieving successful recanalization (modified Thrombolysis in Cerebral Infarction ≥2b/3) for outcome parameters stratified for patients with basilar artery occlusion versus anterior circulation. Notice the broad CIs in the posterior circulation due to the small number of patients in whom recanalization could not be achieved. Numbers indicate the p value for interaction of IV thrombolysis and successful recanalization in the binary multivariable logistic regression analysis, including age, sex, National Institutes of Health Stroke Scale score on admission, and IV thrombolysis. BAO, basilar artery occlusion; mRS, modified Rankin scale; sICH, symptomatic intracranial hemorrhage.
In successfully recanalized BAO patients (TICI ≥2b, n=149), excellent recanalization (TICI 3, n=102) approached significance to increase the odds of a favorable outcome (mRS 0–2) at day 90 (aOR=2.177, 95% CI 0.923 to 5.135) and decreased the odds of all-cause mortality at day 90 (aOR=0.408, 95% CI 0.177 to 0.937).
Discussion
This registry-based retrospective analysis of patients with BAO treated with stent-retriever MT has the following main findings: (1) In comparison with patients presenting with ACLVO, interventional procedures in patients with BAO were more often technically effective and equally safe as regards mortality and sICH. (2) FR occurred more frequently in BAO, and predictors of FR included age, stroke severity, maneuver count, and intracranial stenting. (3) Patients with MT in BAO had worse functional outcome than in ACLVO on univariate analysis, but after multivariable adjustment, this difference was non-significant. (4) Successful recanalization in patients with BAO had similar associations with lower mortality, lower rates of sICH, and functional outcome as seen in ACLVO.
The recanalization rate of 90.3% in BAO from our study is in line with recent MT observational studies,27 although it is slightly higher than in other systematic reviews, which included earlier studies10 17 and recent registries.15 28 Advances in MT technique, operator adjudication,29 use of TICI score in PCLVO30 in our registry, and different patient selection probably best explain the differences observed.
The rate of complications in patients with BAO was 10.9%, which was similar to rates previously reported31 32 and matched the frequency of complications seen in patients presenting with ACLVO.31 Serious complications observed were three artery perforations with one associated death. Patients with unsuccessful recanalization had a higher complication rate (31.3% vs 8.7%, p=0.018).
Irrespective of treatment modalities, patients with BAO more often have a deleterious course than their counterparts presenting with ACLVO.2 33 The mortality rate of 36.2% is in line with the published data.17 In accordance with previous data, we found a higher chance for FR in BAO than in ACLVO (47% vs 34%, p=0.002).15–18 Regarding factors associated with FR, our data confirm previously reported preinterventional factors, including age, baseline NIHSS score and lower pcASPECTS. Contrary to the literature, cardioembolic stroke subtype was no predictor of FR in our study. Importantly, we could identify interventional predictors of FR, mainly higher maneuver count and intracranial stenting. After adjusting for confounders, only age, baseline NIHSS score, and intracranial stenting remained significant prognostic factors for FR in our dataset. Together with a lower mortality rate in successfully recanalized patients, the observation of increased FR suggests that by MT, death was avoided but long-term dependence created. Those finding should be included in the discussion to treat or withhold treatment according to patient preferences.
Corroborating our observations about the beneficial effect of successful recanalization, the meta-analyses by Kumar et al also reported that mortality was bisected in patients in whom successful recanalization (mTICI 2b or mTICI 3) was achieved.10 Although partially present on unadjusted analysis, the higher rates of moderate, favorable, and excellent functional outcome were not statistically significant after adjustment for confounders when recanalization was achieved in BAO, although this could be shown by others.14 28 34 The small number of patients in whom recanalization could not be achieved was associated with broad confidence intervals, which probably explains the lack of statistical significance. More importantly, the effect of achieving successful recanalization with respect to mortality rates and sICH was independent of IVT administration. Sensitivity analysis disclosed no interaction between IVT and recanalization success.
It is noteworthy that excellent recanalization (TICI 3) was more beneficial for all-cause mortality at day 90 compared with successful recanalization (TICI ≥2b), which could be also shown in ACLVO.35–37 Therefore, also in BAO, efforts should be made to improve the quality of recanalization by preventing or treating distal emboli.38
Kumar et al concluded that the significant treatment effect of recanalization, confirmed by observational data and meta-analyses in this severe disease, would make a randomized controlled trial (RCT) to compare MT and the best medication-based treatment unethical.10 However, at least two such RCTs are currently being conducted.39 40 In our opinion, the most relevant question is not whether or not to treat patients with BAO with MT, but rather in which patients recanalization would be futile or cause long-term dependence. Therefore, RCTs comparing patient selection strategies with advanced imaging techniques and concomitant medical therapy are urgently warranted. Possible predictors for good outcome including stroke risk factors, stroke severity (NIHSS score), age, respiratory stability, thrombus length, atherosclerotic stenosis versus embolic occlusion, and collateral status have been published.14 41–52 They should be combined in a study protocol of patient selection in BAO to minimize the incidence of futile recanalization.
Limitations
This is a single-arm multicenter retrospective registry, which has associated limitations. No comparison with patients treated with medical management only was performed, and patient selection for MT was center-specific. Several factors, including final mTICI score and initial pcASPECTS, were not adjudicated by a core laboratory and the exact location of BAO (proximal, middle, distal portion) was unknown. Data quality was incomplete for important predictors of outcome, such as collateral quality and pcASPECTS. Subgroup analyses were generally confined to small cohorts, which introduces a large uncertainty of the presented effects, as indicated by relatively wide confidence intervals.
Conclusion
In selected patients treated with MT, similar outcomes can be achieved in BAO and ACLVO. Patients with BAO in whom recanalization could be achieved, had lower mortality and rate of sICH than those with unsuccessful recanalization, without effect heterogeneity in comparison with ACLVO. The aim of MT should be complete recanalization. RCTs comparing patient selection and interventional strategies to avoid futile interventions seem warranted.
Acknowledgments
We thank Sarah Kendroud (Vallejo, USA) for proofreading the manuscript.
Footnotes
TRM, JK, JG and UF contributed equally.
Contributors: TRM and JK contributed equally to this paper. TRM wrote the statistical analysis plan, cleaned and analysed the data, and drafted and revised the paper. JK designed data collection tools, drafted and revised the paper. PC-I and LPa monitored data collection of the registry. PMo, PJM, PMi, SH, MRi, MRe, CM, BF, VC, AB, LPi, MG, JS, VMP contributed to the design of the registry, and were responsible for clinical data acquisition and provided feedback on the paper. CM revised the manuscript. JG and UF supervised the project and revised the manuscript.
Funding: This work was supported by Medtronic (Dublin, Ireland). Medtronic did not take part in the conception, design or manuscript draft of this study.
Competing interests: UF is a consultant for Medtronic and Stryker and co-principal investigator of the SWIFT DIRECT trial (Medtronic). JG is a global principal investigator of STAR (Solitaire FR Thrombectomy for Acute Revascularisation), clinical event commitee member of the PROMISE study (European Registry on the ACE Reperfusion Catheters and the Penumbra System in the Treatment of Acute Ischemic Stroke; Penumbra), and a principal investigator and consultant for the SWIFT DIRECT study (Medtronic) and receives Swiss National Science Foundation (SNSF) grants for magnetic resonance imaging in stroke. LPi serves as a consultant for Balt, Microvention, and Penumbra. JK has received travel grants from Pfizer and Stryker. MRi serves as a consultant for Medtronic, Stryker, Anaconda, Apta Targets, and Perflow Medical and as a speaker for Neuravi. PMi has received funding for speaker honoraria from Boehringer. He has served on scientific advisory boards also for Boehringer. He has received research grants from Bristol-Myers Squibb, Boehringer, and the Swiss Heart Foundation. VMP is a consultant for Stryker (SC for DAWN trial), Penumbra (SC for PROMISE study), BALT (proctorship of products unrelated to ischemic stroke), Phenox, Rapid Medical, Neurovasc and receives research a grant from Philips. All the other authors have nothing to disclose.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: Available upon reasonable request from the corresponding author after clearance by the ethical committee.
Correction notice: Since this paper was first published online, the author V Costalat has been updated to Vincent Costalat.
Patient consent for publication: Not required.
References
- 1. Smith WS, Lev MH, English JD, et al. Significance of large vessel intracranial occlusion causing acute ischemic stroke and TIA. Stroke 2009;40:3834–40. 10.1161/STROKEAHA.109.561787 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Mattle HP, Arnold M, Lindsberg PJ, et al. Basilar artery occlusion. Lancet Neurol 2011;10:1002–14. 10.1016/S1474-4422(11)70229-0 [DOI] [PubMed] [Google Scholar]
- 3. Merwick Á, Werring D. Posterior circulation ischaemic stroke. BMJ 2014;348:g3175 10.1136/bmj.g3175 [DOI] [PubMed] [Google Scholar]
- 4. Schulz UG, Fischer U. Posterior circulation cerebrovascular syndromes: diagnosis and management. J Neurol Neurosurg Psychiatry 2017;88:45–53. 10.1136/jnnp-2015-311299 [DOI] [PubMed] [Google Scholar]
- 5. Goyal M, Menon BK, van Zwam WH, et al. Endovascular thrombectomy after large-vessel ischaemic stroke: a meta-analysis of individual patient data from five randomised trials. Lancet 2016;387:1723–31. 10.1016/S0140-6736(16)00163-X [DOI] [PubMed] [Google Scholar]
- 6. Powers WJ, Rabinstein AA, Ackerson T, et al. 2018 Guidelines for the early management of patients with acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 2018;49:e46–110. [DOI] [PubMed] [Google Scholar]
- 7. Sarikaya H, Arnold M, Engelter ST, et al. Outcomes of intravenous thrombolysis in posterior versus anterior circulation stroke. Stroke 2011;42:2498–502. 10.1161/STROKEAHA.110.607614 [DOI] [PubMed] [Google Scholar]
- 8. Schonewille WJ, Wijman CA, Michel P, et al. Treatment and outcomes of acute basilar artery occlusion in the Basilar Artery International Cooperation Study (BASICS): a prospective registry study. Lancet Neurol 2009;8:724–30. 10.1016/S1474-4422(09)70173-5 [DOI] [PubMed] [Google Scholar]
- 9. Pagola J, Ribo M, Alvarez-Sabin J, et al. Thrombolysis in anterior versus posterior circulation strokes: timing of recanalization, ischemic tolerance, and other differences. J Neuroimaging 2011;21:108–12. 10.1111/j.1552-6569.2009.00462.x [DOI] [PubMed] [Google Scholar]
- 10. Kumar G, Shahripour RB, Alexandrov AV. Recanalization of acute basilar artery occlusion improves outcomes: a meta-analysis. J Neurointerv Surg 2015;7:868–74. 10.1136/neurintsurg-2014-011418 [DOI] [PubMed] [Google Scholar]
- 11. Lindsberg PJ, Mattle HP. Therapy of basilar artery occlusion: a systematic analysis comparing intra-arterial and intravenous thrombolysis. Stroke 2006;37:922–8. 10.1161/01.STR.0000202582.29510.6b [DOI] [PubMed] [Google Scholar]
- 12. Lindsberg PJ, Soinne L, Tatlisumak T, et al. Long-term outcome after intravenous thrombolysis of basilar artery occlusion. JAMA 2004;292:1862 10.1001/jama.292.15.1862 [DOI] [PubMed] [Google Scholar]
- 13. Ritvonen J, Strbian D, Silvennoinen H, et al. Thrombolysis and adjunct anticoagulation in patients with acute basilar artery occlusion. Eur J Neurol 2019;26:128–35. 10.1111/ene.13781 [DOI] [PubMed] [Google Scholar]
- 14. Bouslama M, Haussen DC, Aghaebrahim A, et al. Predictors of good outcome after endovascular therapy for vertebrobasilar occlusion stroke. Stroke 2017;48:3252–7. 10.1161/STROKEAHA.117.018270 [DOI] [PubMed] [Google Scholar]
- 15. Alonso de Leciñana M, Kawiorski MM, Ximénez-Carrillo Á, et al. Mechanical thrombectomy for basilar artery thrombosis: a comparison of outcomes with anterior circulation occlusions. J Neurointerv Surg 2017;9:1173–8. 10.1136/neurintsurg-2016-012797 [DOI] [PubMed] [Google Scholar]
- 16. Lindsberg PJ, Sairanen T, Nagel S, et al. Recanalization treatments in basilar artery occlusion—systematic analysis. Eur Stroke J 2016;1:41–50. 10.1177/2396987316629889 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Gory B, Eldesouky I, Sivan-Hoffmann R, et al. Outcomes of stent retriever thrombectomy in basilar artery occlusion: an observational study and systematic review. J Neurol Neurosurg Psychiatry 2016;87:520–5. 10.1136/jnnp-2014-310250 [DOI] [PubMed] [Google Scholar]
- 18. Singer OC, Berkefeld J, Nolte CH, et al. Mechanical recanalization in basilar artery occlusion: the ENDOSTROKE study. Ann Neurol 2015;77:415–24. 10.1002/ana.24336 [DOI] [PubMed] [Google Scholar]
- 19. Thiel A, Schmidt H, Prange H, et al. [Treatment of patients with thromboses of the basilar artery and locked-in syndrome. An ethical dilemma]. Nervenarzt 1997;68:653–8. [DOI] [PubMed] [Google Scholar]
- 20. Strbian D, Sairanen T, Silvennoinen H, et al. Thrombolysis of basilar artery occlusion: impact of baseline ischemia and time. Ann Neurol 2013;73:688–94. 10.1002/ana.23904 [DOI] [PubMed] [Google Scholar]
- 21. Nagel S, Herweh C, Köhrmann M, et al. MRI in patients with acute basilar artery occlusion - DWI lesion scoring is an independent predictor of outcome. Int J Stroke 2012;7:282–8. 10.1111/j.1747-4949.2011.00705.x [DOI] [PubMed] [Google Scholar]
- 22. Mokin M, Sonig A, Sivakanthan S, et al. Clinical and procedural predictors of outcomes from the endovascular treatment of posterior circulation strokes. Stroke 2016;47:782–8. 10.1161/STROKEAHA.115.011598 [DOI] [PubMed] [Google Scholar]
- 23. Phan K, Phan S, Huo YR, et al. Outcomes of endovascular treatment of basilar artery occlusion in the stent retriever era: a systematic review and meta-analysis. J Neurointerv Surg 2016;8:1107–15. 10.1136/neurintsurg-2015-012089 [DOI] [PubMed] [Google Scholar]
- 24. Kaesmacher J, Chaloulos-Iakovidis P, Panos L, et al. Clinical effect of successful reperfusion in patients presenting with NIHSS < 8: data from the BEYOND-SWIFT registry. J Neurol 2019;266:598–608. 10.1007/s00415-018-09172-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Higashida RT, Furlan AJ, Roberts H, et al. Trial design and reporting standards for intraarterial cerebral thrombolysis for acute ischemic stroke. J Vasc Interv Radiol 2003;14:E1–31. 10.1016/S1051-0443(07)60431-X [DOI] [PubMed] [Google Scholar]
- 26. Mazya M V, Cooray C, Lees KR, et al. Minor stroke due to large artery occlusion. When is intravenous thrombolysis not enough? Results from the SITS International Stroke Thrombolysis Register. Eur Stroke J 2017;3:239698731774600 10.1177/2396987317746003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Kang DH, Jung C, Yoon W, et al. Endovascular thrombectomy for acute basilar artery occlusion: a multicenter retrospective observational study. J Am Heart Assoc 2018;7:e009419 10.1161/JAHA.118.009419 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Weber R, Minnerup J, Nordmeyer H, et al. Thrombectomy in posterior circulation stroke: differences in procedures and outcome compared to anterior circulation stroke in the prospective multicentre REVASK registry. Eur J Neurol 2019;26:299–305. 10.1111/ene.13809 [DOI] [PubMed] [Google Scholar]
- 29. Zhang G, Treurniet KM, Jansen IGH, et al. Operator versus core lab adjudication of reperfusion after endovascular treatment of acute ischemic stroke. Stroke 2018;49:2376–82. 10.1161/STROKEAHA.118.022031 [DOI] [PubMed] [Google Scholar]
- 30. Jung C, Yoon W, Ahn SJ, et al. The revascularization scales dilemma: is it right to apply the treatment in cerebral ischemia scale in posterior circulation stroke? AJNR Am J Neuroradiol 2016;37:285–9. 10.3174/ajnr.A4529 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Behme D, Gondecki L, Fiethen S, et al. Complications of mechanical thrombectomy for acute ischemic stroke-a retrospective single-center study of 176 consecutive cases. Neuroradiology 2014;56:467–76. 10.1007/s00234-014-1352-0 [DOI] [PubMed] [Google Scholar]
- 32. Lll Y, Holmberg A, Mpotsaris A, et al. Posterior circulation occlusions may be associated with distal emboli during thrombectomy: factors for distal embolization and a review of the literature. Clin Neuroradiol 2018. 10.1007/s00062-018-0679-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Sharma S, Mazya MV, Wahlgren N, et al. IV thrombolysis in very severe and severe ischemic stroke: results from the SITS-ISTR Registry. Neurology 2016;86:2115 10.1212/WNL.0000000000002734 [DOI] [PubMed] [Google Scholar]
- 34. Haussen DC, Dharmadhikari SS, Snelling B, et al. Posterior communicating and vertebral artery configuration and outcome in endovascular treatment of acute basilar artery occlusion. J Neurointerv Surg 2015;7:864–7. 10.1136/neurintsurg-2014-011327 [DOI] [PubMed] [Google Scholar]
- 35. Kleine JF, Wunderlich S, Zimmer C, et al. Time to redefine success? TICI 3 versus TICI 2b recanalization in middle cerebral artery occlusion treated with thrombectomy. J Neurointerv Surg 2017;9:117–21. 10.1136/neurintsurg-2015-012218 [DOI] [PubMed] [Google Scholar]
- 36. Kaesmacher J, Dobrocky T, Heldner MR, et al. Systematic review and meta-analysis on outcome differences among patients with TICI2b versus TICI3 reperfusions: success revisited. J Neurol Neurosurg Psychiatry 2018;89:910–7. 10.1136/jnnp-2017-317602 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Rizvi A, Seyedsaadat SM, Murad MH, et al. Redefining ’success': a systematic review and meta-analysis comparing outcomes between incomplete and complete revascularization. J Neurointerv Surg 2019;11:9–13. 10.1136/neurintsurg-2018-013950 [DOI] [PubMed] [Google Scholar]
- 38. Boeckh-Behrens T, Pree D, Lummel N, et al. Vertebral artery patency and thrombectomy in basilar artery occlusions. Stroke 2019;50:389–95. 10.1161/STROKEAHA.118.022466 [DOI] [PubMed] [Google Scholar]
- 39. Liu X, Xu G, Liu Y, et al. Acute basilar artery occlusion: endovascular interventions versus standard medical treatment (BEST) trial-design and protocol for a randomized, controlled, multicenter study. Int J Stroke 2017;12:779–85. 10.1177/1747493017701153 [DOI] [PubMed] [Google Scholar]
- 40. van der Hoeven EJ, Schonewille WJ, Vos JA, et al. The Basilar Artery International Cooperation Study (BASICS): study protocol for a randomised controlled trial. Trials 2013;14:200 10.1186/1745-6215-14-200 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Alqadri S, Adil MM, Watanabe M, et al. Patterns of collateral formation in basilar artery steno-occlusive diseases. J Vasc Interv Neurol 2013;6:9–13. [PMC free article] [PubMed] [Google Scholar]
- 42. Werner M, Lopez-Rueda A, Zarco F, et al. Mechanical thrombectomy in acute basilar artery occlusion: a safety and efficacy single centre study. Interv Neuroradiol 2016;22:310–7. 10.1177/1591019916631145 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Yoon W, Kim SK, Heo TW, et al. Predictors of good outcome after stent-retriever thrombectomy in acute basilar artery occlusion. Stroke 2015;46:2972–5. 10.1161/STROKEAHA.115.010840 [DOI] [PubMed] [Google Scholar]
- 44. Vergouwen MD, Compter A, Tanne D, et al. Outcomes of basilar artery occlusion in patients aged 75 years or older in the Basilar Artery International Cooperation Study. J Neurol 2012;259:2341–6. 10.1007/s00415-012-6498-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Brandt T, von Kummer R, Müller-Küppers M, et al. Thrombolytic therapy of acute basilar artery occlusion. Variables affecting recanalization and outcome. Stroke 1996;27:875–81. [DOI] [PubMed] [Google Scholar]
- 46. Cross DT, Moran CJ, Akins PT, et al. Collateral circulation and outcome after basilar artery thrombolysis. AJNR Am J Neuroradiol 1998;19:1557-63. [PMC free article] [PubMed] [Google Scholar]
- 47. Gilberti N, Gamba M, Premi E, et al. Endovascular mechanical thrombectomy in basilar artery occlusion: variables affecting recanalization and outcome. J Neurol 2016;263:707–13. 10.1007/s00415-016-8047-x [DOI] [PubMed] [Google Scholar]
- 48. Goyal N, Tsivgoulis G, Nickele C, et al. Posterior circulation CT angiography collaterals predict outcome of endovascular acute ischemic stroke therapy for basilar artery occlusion. J Neurointerv Surg 2016;8:783–6. 10.1136/neurintsurg-2015-011883 [DOI] [PubMed] [Google Scholar]
- 49. Jung S, Mono ML, Fischer U, et al. Three-month and long-term outcomes and their predictors in acute basilar artery occlusion treated with intra-arterial thrombolysis. Stroke 2011;42:1946–51. 10.1161/STROKEAHA.110.606038 [DOI] [PubMed] [Google Scholar]
- 50. Kim YW, Hong JM, Park DG, et al. Effect of intracranial atherosclerotic disease on endovascular treatment for patients with acute vertebrobasilar occlusion. AJNR Am J Neuroradiol 2016;37:2072–8. 10.3174/ajnr.A4844 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Mundiyanapurath S, Möhlenbruch M, Ringleb PA, et al. Posterior circulation acute stroke prognosis early computed tomography score using hypointense vessels on susceptibility weighted imaging independently predicts outcome in patients with basilar artery occlusion. PLoS One 2015;10:e0132587 10.1371/journal.pone.0132587 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Raymond S, Rost NS, Schaefer PW, et al. Patient selection for mechanical thrombectomy in posterior circulation emergent large-vessel occlusion. Interv Neuroradiol 2018;24:309–16. 10.1177/1591019917747253 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
neurintsurg-2018-014516supp001.docx (24.4KB, docx)


