Abstract
This study assesses the use of spinal anesthesia as the primary anesthetic strategy for operative repair of hip fracture using the National Surgical Quality Improvement Program database.
Hip fractures are a large source of morbidity and mortality, and significant attention has been directed at establishing whether use of spinal anesthesia as an alternative to general anesthesia can improve outcomes.1 Randomized clinical trials are currently under way to investigate this question,2,3 but there has already been sufficient support for this hypothesis that practice guidelines have promoted greater use of spinal anesthesia.4 However, no national analyses have demonstrated whether practice patterns have already shifted in advance of trial data, to our knowledge.
The American College of Surgeons National Surgical Quality Improvement Program (NSQIP) database offers a unique tool for clinical outcomes research because its variables are prospectively collected by a trained clinical reviewer at each participating site, including primary anesthesia type. It is not a comprehensive national database, but it has grown to now include data from 708 participating sites and more than 6.6 million patients. A number of the earlier studies suggesting a benefit of spinal anesthesia used NSQIP.5,6 We sought to examine trends associated with the use of spinal anesthesia as the primary anesthetic strategy for operative repair of hip fracture in this contemporary NSQIP database.
Methods
We used the NSQIP participant user file for January 2007 through December 2017 and identified all patients undergoing open surgical repair of hip fractures by relevant Current Procedural Terminology codes (27244, 27245, 27269, 27236, or 27248). We retained records with a recorded primary anesthesia type of spinal or general anesthesia and excluded those performed under local anesthesia alone, local anesthesia with intravenous sedation, and those with an unknown or missing anesthesia type. Epidural anesthesia was classified with spinal anesthesia. This study was exempt from institutional review board review because it uses deidentified data.
Linear regression was performed to evaluate trends over time using SAS version 9.4 (SAS Institute) with a predetermined 2-sided α of .05 to determine statistical significance. Analysis began in July 2019.
Results
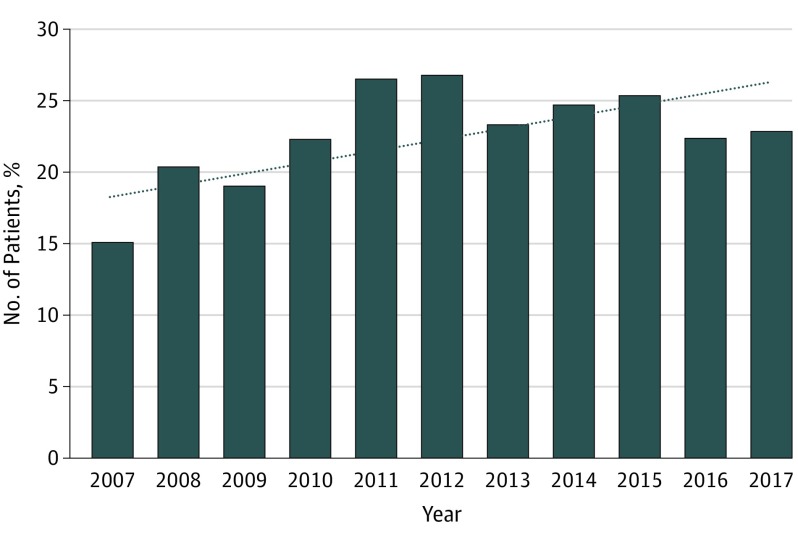
Of 84 067 individuals, the mean (SD) age was 79.17 (11.69) years, and 58 606 (69.7%) were women. Spinal anesthesia was used in 20 085 of 84 016 hip fracture procedures (23.9%) over the entire study period. The proportion of patients treated with spinal anesthesia increased over time (b = 0.0087; P = .03) from 15.1% (26 of 172) in 2007 to 22.9% (4216 of 18 415) in 2017 (Figure 1).
Figure 1. Proportion of Patients Undergoing Hip Fracture Repair Under Spinal Anesthesia.
The dotted line indicates the trend line.
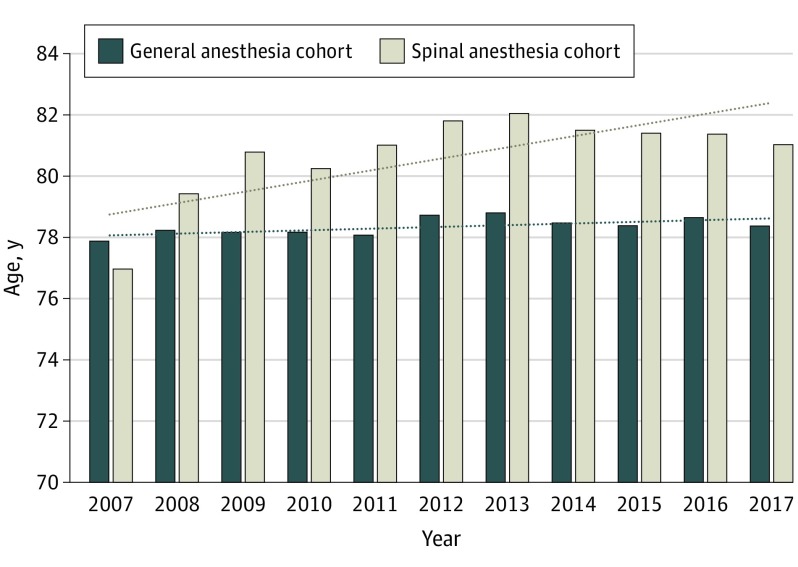
The mean age of the cohort also demonstrated a significantly increasing trend over time (b = 0.6274; P = .01). When divided into cohorts receiving spinal vs general anesthesia, the mean age of the spinal anesthesia cohort demonstrated a similar increasing trend over time (b = 0.3046; P = .02; Figure 2), whereas the mean age of the general anesthesia cohort did not (b = 0.0557; P = .47).
Figure 2. Trend in Age of the Spinal Anesthesia and General Anesthesia Cohorts Over the Study Period.
The dotted lines indicate trend lines for each cohort.
Discussion
This analysis demonstrates increased use of spinal anesthesia for the repair of hip fractures over the study period, 2007 to 2017. This finding may be explained by the observed demographic shift, with increasing age in the spinal anesthesia cohort (but not the general anesthesia cohort) paralleling the rise in use of spinal anesthesia.
Because the purported benefits of spinal anesthesia in patients with hip fractures are associated with the minimization of interventional morbidity in frail, older patients, this analysis supports the notion that use of spinal anesthesia has increased because of growth of this subpopulation, as opposed to the notion that practice patterns have shifted (eg, anesthesiologists using spinal anesthesia with greater frequency overall and/or expanding its use to younger or less frail patient subpopulations).
This analysis has the limitations of any observational study, which by definition cannot demonstrate causation. However, the observed trends are valuable evidence in considering the health care services implications of the noted increase in the use of spinal anesthesia. Results from randomized clinical trials are needed to determine whether increased application of spinal anesthesia to patients beyond the oldest and most frail subgroups is warranted.
References
- 1.Guay J, Parker MJ, Gajendragadkar PR, Kopp S. Anaesthesia for hip fracture surgery in adults. Cochrane Database Syst Rev. 2016;2:CD000521. doi: 10.1002/14651858.CD000521.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kowark A, Adam C, Ahrens J, et al. ; iHOPE study group . Improve hip fracture outcome in the elderly patient (iHOPE): a study protocol for a pragmatic, multicentre randomised controlled trial to test the efficacy of spinal versus general anaesthesia. BMJ Open. 2018;8(10):e023609. doi: 10.1136/bmjopen-2018-023609 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Neuman MD, Ellenberg SS, Sieber FE, Magaziner JS, Feng R, Carson JL; REGAIN Investigators . Regional versus General Anesthesia for Promoting Independence after Hip Fracture (REGAIN): protocol for a pragmatic, international multicentre trial. BMJ Open. 2016;6(11):e013473. doi: 10.1136/bmjopen-2016-013473 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ftouh S, Morga A, Swift C; Guideline Development Group . Management of hip fracture in adults: summary of NICE guidance. BMJ. 2011;342:d3304. doi: 10.1136/bmj.d3304 [DOI] [PubMed] [Google Scholar]
- 5.Fields AC, Dieterich JD, Buterbaugh K, Moucha CS. Short-term complications in hip fracture surgery using spinal versus general anaesthesia. Injury. 2015;46(4):719-723. doi: 10.1016/j.injury.2015.02.002 [DOI] [PubMed] [Google Scholar]
- 6.Basques BA, Bohl DD, Golinvaux NS, Samuel AM, Grauer JG. General versus spinal anaesthesia for patients aged 70 years and older with a fracture of the hip. Bone Joint J. 2015;97-B(5):689-695. doi: 10.1302/0301-620X.97B5.35042 [DOI] [PubMed] [Google Scholar]