Key Points
Question
Is the retinal elevation observed in eyes with stage 4 retinopathy of prematurity (ROP) retinal detachment or retinoschisis on imaging with optical coherence tomography (OCT)?
Findings
In this study of 21 eyes from 15 preterm infants, more than 50% of eyes with stage 4A ROP diagnosed using indirect ophthalmoscopy exhibited retinoschisis without evidence of retinal detachment using OCT. Optical coherence tomography aided in determination of foveal involvement to distinguish stage 4A ROP from stage 4B ROP.
Meaning
Handheld OCT was useful to assess foveal involvement and differentiating retinal detachment and retinoschisis in stage 4 ROP, and use of preoperative OCT may elucidate whether retinoschisis without retinal detachment portends different prognoses.
This study compares features of eyes with stage 4 retinopathy of prematurity (ROP) using optical coherence tomography (OCT) vs indirect ophthalmoscopy findings and grading of photographs.
Abstract
Importance
Progression of retinopathy of prematurity (ROP) to stage 4 may require surgical intervention. The partial retinal detachment of stage 4 ROP may involve the fovea (stage 4B ROP) or may not (stage 4A ROP). This determination has heretofore been based on indirect ophthalmoscopy and documented with color fundus photography.
Objective
To investigate optical coherence tomography (OCT) features of eyes with stage 4 ROP and compare them with indirect ophthalmoscopy findings and grading of photographs.
Design, Setting, and Participants
In this study, research and clinical medical records of 15 infants with clinically diagnosed stage 4 ROP were retrospectively reviewed. Infants were treated at an academic center from May 2011 to January 2018.
Main Outcomes and Measures
Review of OCT images for the presence and foveal involvement of retinoschisis, retinal detachment, and/or vitreomacular traction masked to indirect ophthalmoscopy findings.
Results
Of the 15 included infants, 9 (60%) were male, the mean (SD) gestational age at birth was 23.9 (1.1) weeks, and the mean (SD) postmenstrual age at surgery was 42.4 (4.9) weeks. A total of 21 eyes were analyzed, of which 19 had adequate OCT imaging. Optical coherence tomography imaging extended to the retinal midperiphery but did not cover the entire region of possible detachment in each eye. Among these eyes, 7 eyes had peripheral retinoschisis without retinal detachment or foveal involvement, 5 eyes had peripheral retinoschisis and retinal detachment without foveal involvement, 7 eyes had either retinoschisis or retinal detachment involving the fovea, and 2 eyes had poor OCT signal owing to high retinal detachment.
Conclusions and Relevance
Handheld OCT imaging is useful in clinical evaluation of stage 4 ROP to determine foveal involvement and differentiate retinal detachment and retinoschisis. Many infants diagnosed as having stage 4A ROP had retinoschisis without OCT evidence of retinal detachment. This group of infants may represent a substage of stage 4A ROP, ie, stage 4A–schisis by OCT. These findings suggest handheld OCT imaging may be useful in the clinical evaluation of stage 4 ROP. Further investigations are needed to determine if this subgroup portends a different prognosis and if this observation should alter future clinical practice.
Introduction
Despite treatment of severe (type 1) retinopathy of prematurity (ROP) with laser ablation of avascular retina and/or intravitreal injection with antivascular endothelial growth factor agents, some preterm infants progress to stage 4 or 5 ROP with retinal detachment. Stage 4 ROP, partial retinal detachment not involving the fovea (stage 4A ROP) or involving the fovea (stage 4B ROP), is determined by experts using indirect ophthalmoscopy.1 While grading widefield digital retinal images for earlier stages of ROP is shown to be highly accurate,2,3 image-based diagnosis of stage 4 and 5 ROP is imperfect owing to hazy media, insufficient retinal coverage, and inability to appreciate retinal elevation.4
The use of handheld optical coherence tomography (OCT) could help address challenges faced when evaluating images of stage 4 ROP, particularly identifying foveal involvement and determining the nature and degree of retinal elevation. In pediatric use, handheld OCT has revealed subclinical structural features in preterm infant retinas that are not obvious on clinical examination, such as cystoid macular edema and changes at the vascular-avascular junction.5,6,7 In advanced ROP, both retinoschisis and retinal detachment have been described at the posterior pole by OCT.8,9,10 Here, we investigate the utility of handheld OCT in evaluating stage 4 ROP at both central and peripheral retina and describe a subgroup of infants with stage 4 ROP in whom OCT revealed only retinoschisis without retinal detachment.
Methods
This study was approved by the Duke University Health System institutional review board and adheres to the Health Insurance Portability and Accountability Act and all tenets of the Declaration of Helsinki. This is a retrospective medical record review of preterm infants with stage 4 ROP as determined by a retina specialist using indirect ophthalmoscopy prior to examination under anesthesia. These infants were either enrolled as part of a prospective study of OCT imaging of infant retina (with written informed consent obtained from the parents or guardians) or had received handheld OCT imaging for standard clinical care (with written informed consent waived due to retrospective analysis), both during examination under anesthesia between May 2011 and January 2018. Imaging included handheld spectral-domain OCT (Leica/Bioptigen Envisu) under a standard protocol obtaining volumes of optic nerve, macula, and the retinal periphery aiming at the area of clinically determined retinal elevation as well as RetCam photography (Natus Medical Incorporated).
Optical coherence tomography images were evaluated for quality and features. Two vitreoretinal specialists (X.C. and C.A.T.) graded OCT images for retinoschisis (splitting of retinal layers), retinal detachment (presence of subretinal fluid), and foveal involvement. Two fellowship-trained pediatric ophthalmologists (S.G.P. and S.F.F.), who both routinely perform ROP screening and have participated in many ROP studies, graded RetCam photographs for zone and stage of ROP, masked to clinical findings. Optical coherence tomography findings were compared with indirect ophthalmoscopy findings and grading of RetCam photographs.
Results
A total of 21 eyes from 15 infants were included in the study. Of the 15 included infants, 9 (60%) were male, the mean (SD) gestational age at birth was 23.9 (1.1) weeks, and the mean (SD) postmenstrual age at surgery was 42.4 (4.9) weeks. Preoperative bedside evaluation by indirect ophthalmoscopy noted 10 eyes with stage 4A ROP, 7 eyes with stage 4B ROP, and 4 eyes with stage 4 ROP but indeterminate foveal involvement. The stage of ROP on masked RetCam photography review for all eyes is summarized in the Table.
Table. Summary of Diagnoses by Clinical Examination, RetCam Photograph Grading, and Optical Coherence Tomography (OCT) in Infants With Stage 4 Retinopathy of Prematurity (ROP).
| Eye, No. | ROP Stage on Indirect Ophthalmoscopy | ROP Stage on Grading Images by ROP Expert | ROP Stage by OCT | OCT Findings | |||||
|---|---|---|---|---|---|---|---|---|---|
| Expert 1 | Expert 2 | Foveal Retinoschisis | Foveal Detachment | Nonfoveal Retinoschisis | Nonfoveal Detachment | Vitreomacular Traction | |||
| 1 | 4A | 4A | 4B | 4A | − | − | + | − | − |
| 2 | 4A | 3 | 4A | 4A | − | − | + | − | − |
| 3 | 4A | 4A | 3 | 4A | − | − | + | − | − |
| 4 | 4A | 3 | 4A | 4A | − | − | + | − | − |
| 5 | 4A | 4B/5 | 4B | 4A | − | − | + | + | − |
| 6 | 4A | 4A | 4A | 4A | − | − | + | + | − |
| 7 | 4A | 4A | 4A | 4A | − | − | + | − | − |
| 8 | 4A | Poor | Poor | 4A | − | − | + | − | + |
| 9 | 4A | 4A | Poor | 4A | Poor | Poor | + | − | + |
| 10 | 4A | 4A | 4B | 4B | + | + | + | + | − |
| 11 | 4A/B | 4A/B | 4B | 4A | − | − | + | + | − |
| 12 | 4A/B | 4B | 4B | 4B | − | + | + | + | − |
| 13 | 4A/B | 4A/B | 4B | 4B | + | + | + | + | − |
| 14 | 4A/B | 5 | 5 | 4B | Poor | + | + | + | − |
| 15 | 4B | 4B | 4B | 4A | − | − | + | + | − |
| 16 | 4B | 4B | 4B | 4A | − | − | + | + | − |
| 17 | 4B | APROP | APROP | 4B | + | + | + | + | − |
| 18 | 4B | 4B | 4B | 4B | − | + | − | + | − |
| 19 | 4B | 4B | 4B | 4B | − | + | + | + | − |
| 20 | 4B | 4A | 5 | U | U | U | U | U | U |
| 21 | 4B | 4B | 5 | U | U | U | U | U | U |
Abbreviations: 4A/B, stage 4 ROP unable to determine foveal involvement; APROP, aggressive posterior retinopathy of prematurity; Poor, poor image quality; U, unable to grade because of high retinal detachment.
Of the 21 eyes, 19 had OCT images of adequate quality; we were unable to obtain adequate OCT images in 2 eyes with high retinal detachment from stage 4B ROP. In 2 eyes with vitreous hemorrhage, image quality was suboptimal, but we were able to grade the macula and midperipheral retina. The OCT images extended to the retinal midperiphery but did not cover the entire area of presumed retinal detachment in most eyes unless a montage was attempted.
On OCT imaging, retinoschisis and/or retinal detachment were distinguishable in areas of retinal elevation in 19 eyes with retinal detachment on clinical examination; retinoschisis without retinal detachment (Figure 1) was present in 7 of 19 eyes, and retinal detachment with or without retinoschisis (Figure 2) was evident in 12 of 19 eyes (Table). Other OCT findings included cystoid macular edema in 6 eyes, foveal single cyst in 5 eyes, intraretinal hyperreflective foci in 18 eyes, subretinal hyperreflective material in 3 eyes, optic disc elevation in 12 of 16 eyes (OCT of 3 eyes did not capture the optic disc), vitreous strands in 18 eyes, and epiretinal membrane in 17 eyes.
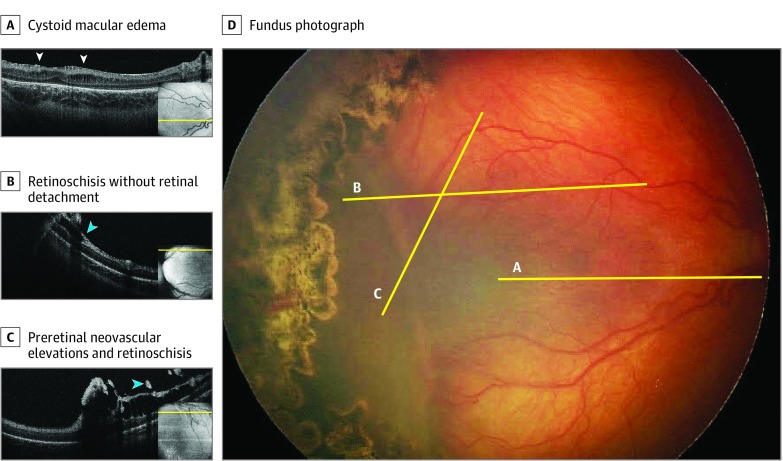
Figure 1. Handheld Optical Coherence Tomography (OCT) Images and Fundus Photograph of a Right Eye With Stage 4A Retinopathy of Prematurity With Retinoschisis Without Retinal Detachment.
A, An OCT B-scan through the fovea shows cystoid macular edema (white arrowheads). B and C, OCT B-scans through the retinal midperiphery in the area of the perceived retinal detachment on indirect ophthalmoscopy shows retinoschisis without retinal detachment (B) as well as preretinal neovascular elevations with retinoschisis (C) (blue arrowheads). The yellow lines mark the approximate location of the OCT B-scans on OCT retina view (insets) and fundus photograph (D).
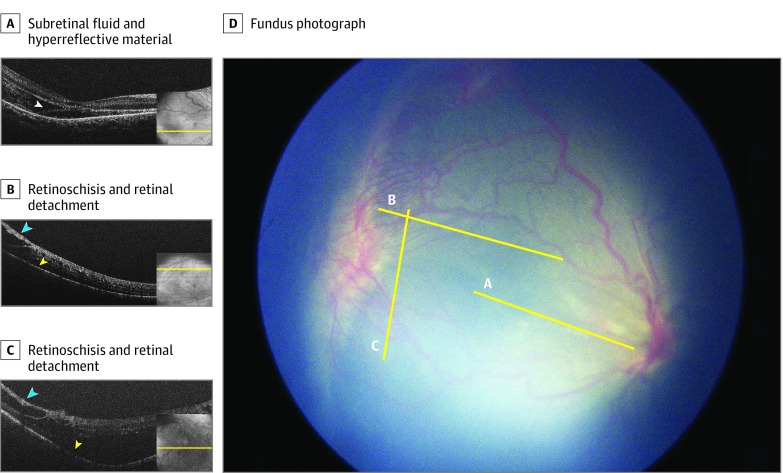
Figure 2. Handheld Optical Coherence Tomography (OCT) Images and Fundus Photograph of a Right Eye With Stage 4B Retinopathy of Prematurity With Both Retinoschisis and Retinal Detachment.
A, An OCT B-scan through the fovea shows subretinal fluid and subretinal hyperreflective material (white arrowhead). B and C, OCT B-scans through the retinal midperiphery in the area of perceived retinal detachment on indirect ophthalmoscopy shows both retinoschisis (blue arrowheads) and retinal detachment (yellow arrowheads). The yellow lines mark the approximate location of the OCT B-scans on OCT retina view (insets) and fundus photograph (D).
On grading RetCam images, the ROP experts agreed with one another on the presence of retinal detachment in 15 of 19 eyes, and each identified 15 of 19 eyes with retinal elevation identified on OCT. In the 2 eyes that the graders marked as having poor image quality, OCT identified severe vitreomacular traction.
Foveal location was distinguishable on OCT in 17 of 19 eyes. In the other 2 eyes, the exact location of the fovea could not be identified, as either the fovea was highly detached or was within areas of atypical severe vitreomacular traction. In the 4 eyes in which ophthalmoscopy noted indeterminant foveal involvement, OCT identified subretinal fluid under the fovea and/or retinoschisis with foveal involvement in 3 eyes and no foveal involvement in 1 eye.
We defined OCT stage 4A ROP as ROP with the fovea not affected by retinoschisis or retinal detachment and OCT stage 4B ROP as ROP with retinoschisis and/or retinal detachment affecting the fovea. Of the 15 eyes with OCT imaging and clinical documentation on the presence or absence of foveal involvement, 3 eyes with the OCT staging of foveal involvement differed from the clinical diagnosis. One eye clinically diagnosed as having stage 4A ROP was changed to OCT stage 4B ROP, and 2 eyes with clinically diagnosed stage 4B ROP was changed to OCT stage 4A ROP. There was 100% agreement between OCT graders for determination of ROP stage by OCT (4A vs 4B) (eTable in the Supplement). Interestingly, 7 of 10 eyes with stage 4A ROP on preoperative clinical examination exhibited retinoschisis alone on OCT (all OCT stage 4A ROP) without evidence of retinal detachment (Table).
Discussion
Over the past decade, multimodal imaging has been incorporated in the evaluation of many vitreoretinal diseases. The advent of handheld OCT provides us with an opportunity to address 2 challenges in the diagnosis of stage 4 ROP: location of the foveal center and appreciation of the degree and nature of retinal elevation. Our study showed that OCT could provide valuable information by addressing these challenges and adds to our armamentarium of tools to evaluate advanced cases of ROP.
We found retinoschisis in almost every eye with stage 4 ROP, presumably because of disease activity and/or increased vitreoretinal traction. Retinoschisis in the setting of advanced ROP has been previously reported at the posterior pole.8,9,10 Our group has also previously identified limited areas of retinoschisis surrounding the neovascular elevation at the vascular-avascular junction in stage 3 ROP.5 Here, we describe that more than half of infants with stage 4A ROP diagnosed using indirect ophthalmoscopy had retinoschisis but no retinal detachment both centrally and at the retinal midperiphery by OCT, denoting a new substage of stage 4A ROP, ie, stage 4A–schisis by OCT. For infants involved in this study, having these OCT images at the time of examination under anesthesia did not change the decision to operate. Additional follow-up studies are needed to determine if this subgroup of infants, compared with the rest of the subgroup (stage 4A ROP with retinal detachment), portends a different prognosis following surgical repair, which may alter future clinical practice.
Limitations
Our current study is limited by the sample size and field of view of the handheld spectral-domain OCT. Larger studies are needed to determine sensitivity, specificity, and predictive value of spectral-domain OCT imaging. Handheld OCT and future advances, such as using swept-source OCT and larger fields of view,11,12,13 may further improve our assessments of infants with ROP.
Conclusions
Handheld OCTs are useful in determining foveal involvement and differentiating retinal detachment and retinoschisis in the evaluation of stage 4 ROP. Many infants with clinical stage 4A ROP exhibit retinoschisis without retinal detachment on OCT imaging. Additional follow-up studies are needed to determine if this subgroup of infants portends a different prognosis following surgical repair.
eTable. OCT grader agreements on OCT features and retinopathy of prematurity (ROP) stage by OCT.
References
- 1.International Committee for the Classification of Retinopathy of Prematurity The International Classification of Retinopathy of Prematurity revisited. Arch Ophthalmol. 2005;123(7):991-999. doi: 10.1001/archopht.123.7.991 [DOI] [PubMed] [Google Scholar]
- 2.Biten H, Redd TK, Moleta C, et al. ; Imaging & Informatics in Retinopathy of Prematurity (ROP) Research Consortium . Diagnostic accuracy of ophthalmoscopy vs telemedicine in examinations for retinopathy of prematurity. JAMA Ophthalmol. 2018;136(5):498-504. doi: 10.1001/jamaophthalmol.2018.0649 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dai S, Chow K, Vincent A. Efficacy of wide-field digital retinal imaging for retinopathy of prematurity screening. Clin Exp Ophthalmol. 2011;39(1):23-29. [DOI] [PubMed] [Google Scholar]
- 4.Patel SN, Singh R, Jonas KE, et al. ; Imaging and Informatics for Retinopathy of Prematurity Research Consortium . Telemedical diagnosis of stage 4 and stage 5 retinopathy of prematurity. Ophthalmol Retina. 2018;2(1):59-64. doi: 10.1016/j.oret.2017.04.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chen X, Mangalesh S, Dandridge A, et al. Spectral-domain OCT findings of retinal vascular-avascular junction in infants with retinopathy of prematurity. Ophthalmol Retina. 2018;2(9):963-971. doi: 10.1016/j.oret.2018.02.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Maldonado RS, O’Connell R, Ascher SB, et al. Spectral-domain optical coherence tomographic assessment of severity of cystoid macular edema in retinopathy of prematurity. Arch Ophthalmol. 2012;130(5):569-578. doi: 10.1001/archopthalmol.2011.1846 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Vajzovic L, Rothman AL, Tran-Viet D, Cabrera MT, Freedman SF, Toth CA. Delay in retinal photoreceptor development in very preterm compared to term infants. Invest Ophthalmol Vis Sci. 2015;56(2):908-913. doi: 10.1167/iovs.14-16021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chavala SH, Farsiu S, Maldonado R, Wallace DK, Freedman SF, Toth CA. Insights into advanced retinopathy of prematurity using handheld spectral domain optical coherence tomography imaging. Ophthalmology. 2009;116(12):2448-2456. doi: 10.1016/j.ophtha.2009.06.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Joshi MM, Trese MT, Capone A Jr. Optical coherence tomography findings in stage 4A retinopathy of prematurity: a theory for visual variability. Ophthalmology. 2006;113(4):657-660. doi: 10.1016/j.ophtha.2006.01.007 [DOI] [PubMed] [Google Scholar]
- 10.Muni RH, Kohly RP, Charonis AC, Lee TC. Retinoschisis detected with handheld spectral-domain optical coherence tomography in neonates with advanced retinopathy of prematurity. Arch Ophthalmol. 2010;128(1):57-62. doi: 10.1001/archophthalmol.2009.361 [DOI] [PubMed] [Google Scholar]
- 11.Campbell JP, Nudleman E, Yang J, et al. Handheld optical coherence tomography angiography and ultra-wide-field optical coherence tomography in retinopathy of prematurity. JAMA Ophthalmol. 2017;135(9):977-981. doi: 10.1001/jamaophthalmol.2017.2481 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Song S, Zhou K, Xu JJ, Zhang Q, Lyu S, Wang R. Development of a clinical prototype of a miniature hand-held optical coherence tomography probe for prematurity and pediatric ophthalmic imaging. Biomed Opt Express. 2019;10(5):2383-2398. doi: 10.1364/BOE.10.002383 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Viehland C, Chen X, Tran-Viet D, et al. Ergonomic handheld OCT angiography probe optimized for pediatric and supine imaging. Biomed Opt Express. 2019;10(5):2623-2638. doi: 10.1364/BOE.10.002623 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable. OCT grader agreements on OCT features and retinopathy of prematurity (ROP) stage by OCT.