Key Points
Question
Is there an association between recovery time and location of injury in unilateral vocal fold paralysis?
Findings
This case series of 1264 patients with unilateral vocal fold paralysis revealed that as the distance between the vocal fold and injury location increased, the maximum recovery time increased but did not exceed 1 year. Of the 208 patients who eventually recovered vocal fold motion, the patients with injury at the thyroid level recovered within 6 months, whereas recovery duration was longer for patients with injury distant from the vocal fold.
Meaning
These findings suggest that injury-based counseling is warranted for optimal timing of permanent treatment for patients with unilateral vocal fold paralysis.
Abstract
Importance
Permanent surgical treatment for unilateral vocal fold paralysis (UVFP) should be performed when further neural recovery is improbable. Conservative delay of the surgical procedure may cause unnecessary deterioration of the patient’s quality of life. Knowledge of the natural course of UVFP is important for better management and counseling.
Objective
To evaluate the natural course of UVFP, focusing on the recovery time according to the injury level to assess the optimal timing for permanent surgical intervention.
Design, Setting, and Participants
This retrospective case series enrolled 1264 patients with UVFP who visited the voice clinic of Seoul National University Hospital, Seoul, Korea, from November 1, 2005, through December 31, 2016. Medical records and stroboscopic video images were reviewed to obtain data on demographic characteristics, vocal fold movement, onset and recovery time, follow-up duration, and cause. Cases of UVFP were classified into 5 groups based on the location of injury: distal to the thyroid level, thyroid level, esophagus and mediastinum level, heart and lung level, and proximal to the thorax level. Data analysis was performed from January 23, 2018, to May 21, 2018.
Main Outcomes and Measures
Recovery of vocal fold movement defined as more than vocal fold twitching confirmed by stroboscopy video images, estimated injury level, and start time of recovery. The recovery time was analyzed according to age, sex, paralytic side, and 5 injury levels.
Results
Of 1264 eligible patients with UVFP (655 [51.8%] male; median age, 56 years [range, 1-90 years]), 208 had evidence of recovery with the recovery time relatively accurate. The maximum recovery time for the group with distal to the thyroid–level injury was 120 days; the group with thyroid-level injury, 157 days; the group with esophagus and mediastinum-level injury, 244 days; the group with heart and lung-level injury, 328 days; and the group with proximal to the thorax-level injury, 333 days with the exception of 1 outlier value (482 days). Recovery time did not differ according to age, sex, or paralytic side. As distance between the vocal fold and injury level increased, the maximum recovery time increased, plateauing at 1 year. Among the patients who showed recovery of the vocal fold movement, most patients with injuries distal to or at the level of the thyroid recovered within 6 months, whereas those with injury more distant from the vocal fold recovered within approximately 1 year.
Conclusions and Relevance
A linear association between injury level and maximum recovery time was observed. The findings suggest that the decision to proceed with permanent phonosurgical treatment should be based on the level of injury associated with UVFP.
This case series assesses the association of injury level causing unilateral vocal cord paralysis with maximum recovery time to evaluate the optimal timing of permanent phonosurgical treatment.
Introduction
Permanent surgical treatment for unilateral vocal fold paralysis (UVFP) should be performed when further neural recovery is improbable. During this process, it is important to estimate prognosis and understand nerve damage and healing.
Laryngeal electromyography is commonly used to assess the outcomes of vocal fold paralysis, but it provides limited prognostic information. Poor electromyography results do not necessarily determine a persistent vocal fold immobility because of the low negative predictive value of the test.1 Therefore, surgeons tend to delay a permanent phonosurgical treatment for a sufficient period until they feel confident that there will be no further neural regeneration. There are only a few studies2 that have aimed to determine the optimal observation period before intervention.
In a systematic review of 20 reports2 regarding the outcome of unilateral idiopathic vocal fold paralysis, most of the 717 cases of idiopathic UVFP analyzed appeared to recover within 1 year with the exception of 3 markedly delayed recoveries of 26 months, 3 years, and 4 years. However, there is little information about the difference in recovery pattern according to different causes of paralysis in the literature. We hypothesized that recovery patterns are different depending on the distance between the innervated muscle and the site of injury based on the Wallerian degeneration or axonal regeneration involved in the recovery process.
In the present study, we analyzed the natural course of UVFP, focusing on the onset-to-recovery time according to the various estimated injury levels causing vocal fold paralysis.
Methods
Study Population
This study was a retrospective case series of the electronic medical records of 1365 patients diagnosed with UVFP who visited the voice clinic of Seoul National University Hospital, Seoul, Korea, from November 1, 2005, through December 31, 2016. Data analysis was performed from January 23, 2018, to May 21, 2018. Diagnoses were made by a single experienced laryngologist (T-K. K.) under examination with rigid or flexible laryngoscopy or stroboscopy. Of the 1365 patients, 101 patients with incomplete clinical data or follow-up, lack of vocal fold paralysis, or vague onset or recovery time were excluded. The remaining 1264 patients were eligible for this study. The study protocol was approved by the institutional review board of Seoul National University Hospital, Seoul, Korea, and patient consent was waived because the study was a retrospective database review.
Variables and Definitions
Complete medical histories were taken, and all patient information was recorded including age, sex, paralytic side, time of onset, follow-up duration, and cause, from which we estimated the level of injury. One experienced laryngologist (T.-K.K.) evaluated vocal fold movement using stroboscopy or laryngoscopy when stroboscopy was unavailable. For most patients, stroboscopic examination was performed and recorded at every visit. The regular follow-up protocol involved 1 visit every month until 3 months from onset and then every 2 to 3 months. However, we accounted for different intervals between patients owing to the patient’s personal circumstances, surgical management of vocal fold paralysis, and treatment plan for comorbidities.
Onset of Paralysis
The onset of paralysis was defined as (1) the time of dramatic symptom changes, such as hoarseness, voice change, aspiration, dysphagia, dyspnea, and throat discomfort, or (2) the day of the surgical procedure in surgical cases. Among patients who had surgery, the date of the surgical procedure was considered as the onset of paralysis by confirmation of normal vocal fold movement before or the start of symptoms immediately after the surgical procedure. If the onset date was unclear, we excluded the case from the study because the estimation of the recovery time would not be accurate.
Recovery Time of Vocal Fold Movement
Our study focused on primary outcomes including both partial and complete recovery of vocal fold movement but not on the recovery of vocal function.3 For patients in whom vocal fold movement improved, the start time of recovery was analyzed but not the completion time. The recovery time was defined as the interval between the onset of the paralysis and the first sign of vocal fold movement, including vocal fold twitching followed by hypomobility.4 Passive vocal fold movement caused by nonparalyzed contralateral vocal fold muscle activities was excluded.
The stroboscopy video images recorded sequentially at each patient’s follow-up were reviewed to confirm signs of vocal fold movement and that the movement was continuously observed thereafter. Among the patients without stroboscopic video images, we included only those with a clear description of vocal fold movement in the electronic medical records.
Level of Injury
We divided the patients into 5 groups according to the estimated injury level as described in the Table, including (1) distal to the thyroid level, (2) thyroid level, (3) esophagus and mediastinum level, (4) heart and lung level, and (5) proximal to the thorax level. The 5 groups were categorized in the order of the distance from the vocal fold to the estimated location of injury along the recurrent laryngeal and vagus nerve pathway. The group with injuries distal to the thyroid included cases of direct injury very near the vocal fold after procedures such as intubation or esophagogastroduodenoscopy.5,6,7 The thyroid-level group included patients who underwent a thyroid surgical procedure with or without central neck dissection or nonsurgical procedures such as radiofrequency ablation. The esophagus and mediastinum-level group included patients who underwent esophageal surgical procedures such as Ivor Lewis esophagectomy and mediastinal mass or lymph node excision performed by thoracic surgeons. The heart and lung–level group included patients who underwent coronary artery bypass graft, heart valve repair or replacement, aortic artery repair or replacement, and pulmonary lobectomy via video-assisted thoracoscopic surgery. The group with injury proximal to the thorax level included patients who underwent neck dissection, spinal surgery, or brain surgery; experienced a stroke; had a history of viral infection such as upper respiratory infection (URI); or had an idiopathic etiology. Patients with a history of URI and idiopathic cases were classified in the proximal to the thorax-level group because these conditions are commonly presumed to involve postviral neuropathy.8 Patients were classified as having post-URI or idiopathic cause after confirming that there were no lesions in the vagus or recurrent laryngeal nerve on computed tomography.
Table. Grouping of the Recovered Patients by Injury Level.
| Level of Injurya | Cause of Vocal Fold Paralysis | Total, No. (%) (n = 208) | Recovery Time, d | |
|---|---|---|---|---|
| Maximum | Median (range) | |||
| Distal to the thyroid | After intubation, prolonged intubation, or after EGD procedure | 16 (7.7) | 120 | 49.5 (14-120) |
| Thyroid | Thyroidectomy with or without central neck dissection or thyroid radiofrequency ablation | 21 (10.1) | 157 | 70 (14-157) |
| Esophagus and mediastinum | Ivor Lewis esophagectomy, mediastinal mass excision, or mediastinal lymph node dissection | 42 (20.2) | 244 | 113.5 (8-244) |
| Heart and lung | CABG, heart valve surgery, aortic artery replacement, or pulmonary lobectomy via video-assisted thoracoscopic surgery | 43 (20.7) | 328 | 61 (2-328) |
| Proximal to the thorax | Neck dissection, spine surgery, brain surgery, stroke, postviral upper respiratory infection, or idiopathic cause | 86 (41.3) | 333 | 75.5 (5-333)b |
Abbreviations: CABG, coronary artery bypass graft; EGD, esophagogastroduodenoscopy.
Patients were categorized into 5 groups in the order of the distance between the vocal fold and the estimated level of injury along the recurrent laryngeal and vagus nerve pathway.
Outlier at 482.
For surgical cases, all medical records were reviewed to accurately estimate the damaged site. Patients with 2 or more presumptive injury levels were classified in the group of the most distant injury from the vocal fold. For example, patients who underwent thyroid surgical procedures with neck dissection were classified in the proximal to the thorax–level group if there was no documented injury of the recurrent laryngeal nerve on operation record. Because the purpose of our study was to assess the timing for permanent intervention, it was reasonable to wait for the longest possible recovery time. We hypothesized that the farther the injury level was from the vocal fold, the longer the recovery time would be.9,10,11
Statistical Analysis
Median differences and 95% CIs were used to assess the difference in recovery time according to sex and paralytic side. Spearman correlation analysis was used to assess the correlation between age and recovery time. All statistical analyses were performed using SPSS, version 22.0 (IBM Corporation).
Results
Patient Characteristics
The 1264 eligible patients with UVFP included 655 males (51.8%) and 609 females (48.2%), with a median age of 56 years (range, 1-90 years). Initial examination revealed 404 cases (32.0%) of right vocal fold paralysis and 860 cases (68.0%) of left vocal fold paralysis. Among the 1264 patients, 66 (5.2%) were classified in the distal to the thyroid–level group, 236 (18.7%) in the thyroid-level group, 110 (8.7%) in the esophagus and mediastinum–level group, 195 (15.4%) in the heart and lung–level group, and 657 (52.0%) in the proximal to the thorax–level group. The median follow-up of all patients from the onset of paralysis was 385 days (range, 1-21 449 days).
In this study, 208 patients had evidence of motion recovery and an accurate assessment of recovery time. The median follow-up of these patients was 168 days (range, 9-2106 days), and the median recovery time was 75 days (range, 2-482 days) (Table).
Recovery Time According to Age, Sex, and Paralytic Side
Of the 208 patients with recovery, 117 (56.2%) were male, with a median age of 57 years (range, 1-90 years); 71 (34.1%) had right and 137 (65.9%) had left vocal fold paralysis. There was no statistically significant difference in recovery time according to age (Spearman correlation coefficient ρ, 0.130; 95% CI, –0.007 to 0.262), sex (median recovery time, 92 days [men] vs 70 days [women]; median difference, 14; 95% CI, –4 to 32), or paralytic side (median recovery time, 59 days [right] vs 92 days [left]; median difference, –18; 95% CI, –39 to 0).
Recovery Time According to Level of Injury
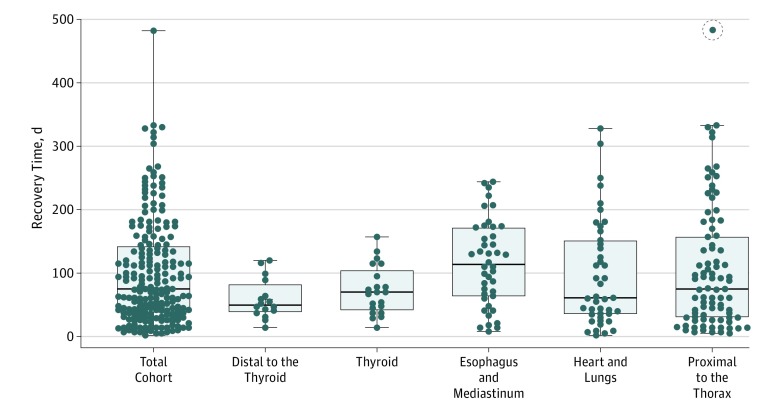
Of the 208 patients who eventually recovered vocal fold motion, the median recovery time for each level of injury was 49.5 days in the distal to the thyroid–level group, 70.0 days in the thyroid-level group, 113.5 days in the esophagus and mediastinum–level group, 61.0 days in the heart and lung–level group, and 75.5 days in the proximal to the thorax–level group. The maximum interval until recovery for each level of injury was 120 days for distal to the thyroid–level injuries, 157 days for thyroid-level injuries, 244 days for esophagus and mediastinum–level injuries, 328 days for heart and lung–level injuries, and 333 days for proximal to the thorax–level injuries (Table). As the distance from the vocal fold to the injury level increased, maximum recovery time increased and plateaued at 1 year; the plateau was observed at the heart and lung level, as well as the proximal to the thorax level except in 1 patient whose estimated recovery time ranged from 364 to 482 days (Figure).
Figure. Recovery Time in 208 Patients With Unilateral Vocal Fold Paralysis According to the Level of Injury.
Every dot of the bee swarm plot represents recovery time of each patient. The upper bar of the whisker diagram represents the maximum value of recovery time belonging to each group; the horizontal bar inside the box indicates the median. As the distance from the vocal fold to the injury level increased, maximum recovery time increased and plateaued at 1 year with 1 exception (circled dot) whose estimated recovery time was from 364 to 482 days.
Discussion
After neuronal damage, new regenerative neurons begin to grow along the nerve pathway from the point of injury to where the nerve function can be restored. The regeneration rate of a nerve is approximately 2.54 cm per month (0.85 mm/d). Unlike sensory neurons, it is difficult to expect regeneration of damaged motor neurons after a certain period. Hypotheses to explain the limited recovery time in damaged motor neurons include the following: (1) Wallerian-degenerated nerve endings may interfere with axonal regeneration, or (2) neuronal regrowth may be useless after irreversible muscle fiber atrophy and fibrosis.11,12
When the peripheral nerve is damaged, it recovers by 2 mechanisms: collateral branching of intact axons or regeneration of the injured axon.13 Collateral branching, which occurs when 20% to 30% of the axons are damaged, starts within 4 days after an injury occurs and progresses for 3 to 6 months. If more than 90% of the axons are damaged, axons are regenerated by the steps of Wallerian degeneration of the distal axon, followed by axonal regeneration and end-organ reinnervation. The known rate of regeneration is 2 to 3 mm per day in proximal segments and 1 to 2 mm per day in distal segments.11 For this reason, the estimated time of regeneration of a paralyzed vocal fold could vary depending on the distance between the vocal fold and injury site. However, it is difficult to find widely accepted studies regarding the recovery pattern according to injury level.
Previous studies2,3,14,15,16 on vocal fold paralysis have shown varying recovery times. In 2018, Rubin and colleagues14 reported that, in a cohort of 100 patients with idiopathic UVFP, 42 patients showed recovery of vocal fold movement, with 93% showing recovery within 2 years. They observed no cases of recovery after 51 months, suggesting a regular follow-up of at least 3 years.14 In the same year, Husain and colleagues3 reported that the mean (SD) voice recovery time of 22 patients with idiopathic vocal fold paralysis was 152.8 (109.3) days, with two-thirds of the patients recovering within 6 months, whereas the possibility of recovery decreased over time. In addition, 5 of 22 patients who experienced voice recovery also showed recovery of vocal fold movement. Mau and colleagues15 recently reported recovery times ranging from 2 to 52 weeks among 727 cases of UVFP, and their model predicted that 86% of patients with recoverable UVFP would improve within 6 months, with 98.9% recovering within 12 months. There are many other reports2,16, but none, to our knowledge, describe how recovery time differs according to the levels of injury.
Because the criteria for the recovery of vocal fold paralysis varies in the literature,2 caution should be taken when comparing the results. For example, both partial and complete recovery of either the voice or vocal fold movement are reported as recovery in different studies.2 In the present study, we defined the sign of vocal fold movement as recovery. The purpose of this study was not to identify when the patients had improved vocal function but to assess the minimum waiting time deemed to be appropriate to perform permanent surgical procedures. To complete this task, we analyzed as much objective data as possible. However, it was impossible to perform an objective voice function test during every follow-up visit for all patients. The subjective report by patients was not suitable for the purpose of this study because it varied according to the occupation, vocal demand, and daily condition of patients.
We hypothesized that the maximum healing duration for recovery is shorter when the injury level is closer to the vocal fold. Our analysis was consistent with this association, showing that the maximum recovery time increased as the injury level was farther from the vocal fold but did not exceed 1 year. The number of recovered patients in the proximal to the thorax-level group (86 [41.3%]) was larger than those in the other groups; therefore, the range of recovery time was likely to increase probabilistically compared with a group with a small number of cases. However, the maximum recovery time in injuries proximal to the thorax level did not increase further with the exception of 1 case. This is consistent with previous reports that state that recovery of vocal fold paralysis rarely occurs after 1 year.2,15
Thyroidectomy is the leading cause of surgery-related UVFP.8 Unilateral vocal fold paralysis can affect quality of life because of deteriorating voice and can increase the risk of aspiration pneumonia. Until recently, a widely accepted treatment policy for UVFP was to delay permanent intervention until 12 months after a surgical procedure, including thyroidectomy.17 On the basis of our findings, if the injury level is close to the vocal fold such as after a thyroidectomy, it is unlikely that the nerve function will return 6 months after surgery. This suggests that withholding permanent treatment for UVFP after undergoing thyroid surgery for 12 months may be associated with unnecessary deterioration of quality of life. We believe that a level of injury-based counseling be given for optimal timing of permanent treatment in patients with UVFP.
We observed 1 delayed recovery case involving a female patient in her 70s with left-sided vocal fold paralysis, which occurred during fasting before undergoing esophagogastroduodenoscopy. No signs of recovery were observed on examination 364 days after onset; however, evidence of recovery was noted at the next examination 482 days after onset. Permanent treatment was not performed because the patient had diminished symptoms and electromyography showed improvement during follow-up.
The rate of recovery from vocal fold paralysis is a topic of interest for laryngologists. The rate of motion recovery from vocal fold paralysis has been reported to vary from 14.7% to 83.0%.2,3,16 Our data were not suitable to calculate the recovery rates. First, we excluded patients whose objective evidence of motion recovery was not available and those who had long follow-up intervals. These exclusions may have underestimated the recovery rate. Second, 35.1% of the cohort did not attend follow-up visits. We assumed that some patients did not return to the hospital because their symptoms were improved and some patients had other serious compounding illnesses preventing them from visiting the hospital. In addition, patients who visit a tertiary hospital may include those who have not recovered at the primary medical facility and are not in good general condition because of severe illnesses; this can also introduce a bias in the calculated recovery rate.
There were a number of difficult issues when analyzing the recovery of vocal fold paralysis. First, in some cases, vocal fold paralysis was diagnosed at another hospital, whereas on initial examination of the larynx at our hospital, signs of recovery were reported. In these cases, the first examination was considered to be the time of recovery. In addition, the exact time of vocal fold paralysis recovery among patients with long follow-up intervals was difficult to determine. Thus, cases for which we were unable to accurately estimate recovery time because of long follow-up intervals were excluded. However, in this study, we did not exclude patients showing a delayed recovery.
Estimating the level of injury and grouping were also difficult. Because the mechanism of idiopathic or URI-related paralysis is not known, locating the part of the nerve that is affected remains challenging. The purpose of this study was not to predict when the patients with vocal fold paralysis would experience improvement but to estimate the minimum waiting time before deciding to perform a permanent surgical procedure. Because we could not exclude the possibility of proximal injury among patients with idiopathic or URI-related paralysis, we chose to classify those patients in the most proximal injury group. However, not all cases of idiopathic or URI-related paralysis manifest with proximal injury. The same classification principle was applied to cases that required surgical procedures at multiple sites at the same time. We analyzed the maximum value of recovery time, not the median value of recovery time. The median recovery time may not necessarily increase when the distance between the vocal fold and injury level increases. We did not observe an increase in the median value of recovery time according to the distance between injury level and vocal fold.
Limitations
The present study has several limitations, including those inherent to retrospective analysis. First, because we did not write every electronic medical record with the study in mind, the onset of paralysis was sometimes unclear or the description of laryngoscopic examination was insufficient to judge improvement. Second, although we tried to exclude patients with lengthy follow-up, the duration of immobility may have been estimated to be longer than the actual healing time. To alleviate this problem, a prospective and controlled study is needed. Third, in some cases, subjective factors confounded the existence of vocal fold movement. If all patients had laryngoscopic or stroboscopic video images or aerodynamic data, we could evaluate the vocal fold movement on a more objective basis. Fourth, there was a misclassification bias because we did not know exactly where the injury occurred, especially in idiopathic and URI-related cases and surgical cases of multiple sites. This bias could affect the analysis of the median value of recovery time. In addition, the degree of injury and the general condition heterogeneity in each group may be confounding factors in the analysis of the median value of recovery time. However, these factors were estimated to be less problematic in the analysis of the maximum value.
Conclusions
Our study results suggest that the expected maximum start time of vocal fold paralysis recovery differed depending on the injury level. The longest recovery time for patients with thyroid-level injury was 157 days. This finding suggests that if UVFP has not begun to recover within 6 months after a thyroid surgical procedure, permanent surgical intervention may be considered because recovery is otherwise unlikely. For patients with UVFP secondary to esophageal and mediastinal surgery, heart and lung surgery, vagus nerve injury, brain surgery, or idiopathic cause, the findings suggest that permanent surgical intervention may be considered 1 year after the initial onset. A treatment policy for the optimal timing of permanent intervention may be associated with reduced unnecessary deterioration of quality of life among patients with UVFP.
References
- 1.Pardo-Maza A, García-Lopez I, Santiago-Pérez S, Gavilán J. Laryngeal electromyography for prognosis of vocal fold paralysis. J Voice. 2017;31(1):90-93. doi: 10.1016/j.jvoice.2016.02.018 [DOI] [PubMed] [Google Scholar]
- 2.Sulica L. The natural history of idiopathic unilateral vocal fold paralysis: evidence and problems. Laryngoscope. 2008;118(7):1303-1307. doi: 10.1097/MLG.0b013e31816f27ee [DOI] [PubMed] [Google Scholar]
- 3.Husain S, Sadoughi B, Mor N, Levin AM, Sulica L. Time course of recovery of idiopathic vocal fold paralysis. Laryngoscope. 2018;128(1):148-152. doi: 10.1002/lary.26762 [DOI] [PubMed] [Google Scholar]
- 4.Peitersen E. Bell’s palsy: the spontaneous course of 2,500 peripheral facial nerve palsies of different etiologies. Acta Otolaryngol Suppl. 2002;(549):4-30. doi: 10.1080/000164802760370736 [DOI] [PubMed] [Google Scholar]
- 5.Ellis PD, Pallister WK. Recurrent laryngeal nerve palsy and endotracheal intubation. J Laryngol Otol. 1975;89(8):823-826. doi: 10.1017/S0022215100081068 [DOI] [PubMed] [Google Scholar]
- 6.Cavo JW., Jr True vocal cord paralysis following intubation. Laryngoscope. 1985;95(11):1352-1359. doi: 10.1288/00005537-198511000-00012 [DOI] [PubMed] [Google Scholar]
- 7.Goto T, Nito T, Ueha R, Yamauchi A, Sato T, Yamasoba T. Unilateral vocal fold adductor paralysis after tracheal intubation. Auris Nasus Larynx. 2018;45(1):178-181. doi: 10.1016/j.anl.2016.12.008 [DOI] [PubMed] [Google Scholar]
- 8.Spataro EA, Grindler DJ, Paniello RC. Etiology and time to presentation of unilateral vocal fold paralysis. Otolaryngol Head Neck Surg. 2014;151(2):286-293. doi: 10.1177/0194599814531733 [DOI] [PubMed] [Google Scholar]
- 9.Gutmann E, Guttmann L, Medawar PB, Young JZ. The rate of regeneration of nerve. J Exp Biol. 1942;19(1):14-44. [Google Scholar]
- 10.Seddon HJ, Medawar PB, Smith H. Rate of regeneration of peripheral nerves in man. J Physiol. 1943;102(2):191-215. doi: 10.1113/jphysiol.1943.sp004027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Menorca RM, Fussell TS, Elfar JC. Nerve physiology: mechanisms of injury and recovery. Hand Clin. 2013;29(3):317-330. doi: 10.1016/j.hcl.2013.04.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Burnett MG, Zager EL. Pathophysiology of peripheral nerve injury: a brief review. Neurosurg Focus. 2004;16(5):E1. doi: 10.3171/foc.2004.16.5.2 [DOI] [PubMed] [Google Scholar]
- 13.Aguayo AJ, Peyronnard JM, Bray GM. A quantitative ultrastructural study of regeneration from isolated proximal stumps of transected unmyelinated nerves. J Neuropathol Exp Neurol. 1973;32(2):256-270. doi: 10.1097/00005072-197304000-00006 [DOI] [PubMed] [Google Scholar]
- 14.Rubin F, Villeneuve A, Alciato L, Slaïm L, Bonfils P, Laccourreye O. Idiopathic unilateral vocal-fold paralysis in the adult. Eur Ann Otorhinolaryngol Head Neck Dis. 2018;135(3):171-174. doi: 10.1016/j.anorl.2018.01.004 [DOI] [PubMed] [Google Scholar]
- 15.Mau T, Pan HM, Childs LF. The natural history of recoverable vocal fold paralysis: implications for kinetics of reinnervation. Laryngoscope. 2017;127(11):2585-2590. doi: 10.1002/lary.26734 [DOI] [PubMed] [Google Scholar]
- 16.Husain S, Sadoughi B, Mor N, Sulica L. Time course of recovery of iatrogenic vocal fold paralysis. Laryngoscope. 2019;129(5):1159-1163. doi: 10.1002/lary.27572 [DOI] [PubMed] [Google Scholar]
- 17.Hartl DM, Travagli JP, Leboulleux S, Baudin E, Brasnu DF, Schlumberger M. Clinical review: current concepts in the management of unilateral recurrent laryngeal nerve paralysis after thyroid surgery. J Clin Endocrinol Metab. 2005;90(5):3084-3088. doi: 10.1210/jc.2004-2533 [DOI] [PubMed] [Google Scholar]