This nationwide cohort study estimates age- and sex-specific incidence rates and risks of being diagnosed with any mental disorder during childhood and adolescence using Danish population health registers.
Key Points
Question
What are the age- and sex-specific incidence rates and cumulative incidences of the full spectrum of diagnosed mental disorders during childhood and adolescence?
Findings
In this nationwide cohort study of 1.3 million individuals in Denmark, the risk (cumulative incidence) of being diagnosed with a mental disorder before 18 years of age was 14.63% in girls and 15.51% in boys. Distinct age- and sex-specific patterns of occurrence were found across mental disorders in children and adolescents.
Meaning
These findings suggest that precise estimates of rates and risks of all mental disorders during childhood and adolescence are essential for future planning of services and care and for etiological research.
Abstract
Importance
Knowledge about the epidemiology of mental disorders in children and adolescents is essential for research and planning of health services. Surveys can provide prevalence rates, whereas population-based registers are instrumental to obtain precise estimates of incidence rates and risks.
Objective
To estimate age- and sex-specific incidence rates and risks of being diagnosed with any mental disorder during childhood and adolescence.
Design
This cohort study included all individuals born in Denmark from January 1, 1995, through December 31, 2016 (1.3 million), and followed up from birth until December 31, 2016, or the date of death, emigration, disappearance, or diagnosis of 1 of the mental disorders examined (14.4 million person-years of follow-up). Data were analyzed from September 14, 2018, through June 11, 2019.
Exposures
Age and sex.
Main Outcomes and Measures
Incidence rates and cumulative incidences of all mental disorders according to the ICD-10 Classification of Mental and Behavioral Disorders: Diagnostic Criteria for Research, diagnosed before 18 years of age during the study period.
Results
A total of 99 926 individuals (15.01%; 95% CI, 14.98%-15.17%), including 41 350 girls (14.63%; 95% CI, 14.48%-14.77%) and 58 576 boys (15.51%; 95% CI, 15.18%-15.84%), were diagnosed with a mental disorder before 18 years of age. Anxiety disorder was the most common diagnosis in girls (7.85%; 95% CI, 7.74%-7.97%); attention-deficit/hyperactivity disorder (ADHD) was the most common in boys (5.90%; 95% CI, 5.76%-6.03%). Girls had a higher risk than boys of schizophrenia (0.76% [95% CI, 0.72%-0.80%] vs 0.48% [95% CI, 0.39%-0.59%]), obsessive-compulsive disorder (0.96% [95% CI, 0.92%-1.00%] vs 0.63% [95% CI, 0.56%-0.72%]), and mood disorders (2.54% [95% CI, 2.47%-2.61%] vs 1.10% [95% CI, 0.84%-1.21%]). Incidence peaked earlier in boys than girls in ADHD (8 vs 17 years of age), intellectual disability (5 vs 14 years of age), and other developmental disorders (5 vs 16 years of age). The overall risk of being diagnosed with a mental disorder before 6 years of age was 2.13% (95% CI, 2.11%-2.16%) and was higher in boys (2.78% [95% CI, 2.44%-3.15%]) than in girls (1.45% [95% CI, 1.42%-1.49%]).
Conclusions and Relevance
This nationwide population-based cohort study provides a first comprehensive assessment of the incidence and risks of mental disorders in childhood and adolescence. By 18 years of age, 15.01% of children and adolescents in this study were diagnosed with a mental disorder. The incidence of several neurodevelopmental disorders peaked in late adolescence in girls, suggesting possible delayed detection. The distinct signatures of the different mental disorders with respect to sex and age may have important implications for service planning and etiological research.
Introduction
Since 1990, studies on the global burden of disease have continuously ranked mental disorders as some of the most impairing conditions worldwide.1,2 The Global Burden of Disease studies recently reported that in children and adolescents, mental disorders account for the most years lived with disability.3 The World Health Organization emphasized in their Mental Health Action Plan 2013-2020 the strong need for age- and sex-specific data on child mental health.4 The United States and Australia have good survey data, but only 7% of all countries worldwide have such data,5 and in 2013, none of 29 member states in the European Union could provide data on incidence of mental disorders in children or adolescents.6
Knowledge of the age-specific risks of mental disorders forms the backbone for public health decisions, prioritization of resources, evidence-based medicine, and research on risk factors and outcomes. Occurrence of a condition in a population is measured as prevalence (cases at a specific point) or incidence (new cases per unit of time). The cumulative incidence estimates the risk of developing the condition before a specified age, taking into consideration individual follow-up time.7 Estimates of the prevalence of mental health disorders in childhood are often based on information from adolescents or parents and are thus prone to recall, information, and survival biases.
In adults, health registry data have made important contributions to our understanding of the incidence of the full spectrum of mental disorders8 and their risk factors and outcomes.9,10,11,12,13 In children and adolescents, similar methods have been informative about the frequency of a few certain mental disorders14,15,16 and their comorbidities,17 risk factors,18,19,20 and outcomes.21,22,23,24 These findings have been supplemented by prevalence estimates from surveys, most often at a single point25,26,27 and sometimes with repeated assessments.28,29 Hence, surveys estimating prevalence rates and registry studies estimating incidence rates of diagnoses complement each other and each have their own limitations.
Nevertheless, evidence on the incidence of the full spectrum of mental disorders in children and adolescents is lacking. The objective of this study was to estimate the incidence rates and cumulative incidences of any diagnosed mental disorder and 27 specific categories of diagnosed mental disorders during childhood and adolescence, with age- and sex-specific estimates, in a nationwide cohort in Denmark.
Methods
Study Population
The Danish Civil Registration System,30 established in 1968, holds data on the personal identification number, sex, date of birth, and continuously updated information on vital status of all persons in Denmark. This enables accurate linkage of individual-level data across all registers and prevents duplication of prior events. Our study population included all live-born singletons born in Denmark from January 1, 1995, through December 31, 2016. This study was approved by the Danish Data Protection Agency. By Danish law, informed consent is not required for register-based studies. This study followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guideline.
Assessment of Mental Illness
The Danish Psychiatric Central Research Register and the Danish National Patient Register provided data on diagnosed mental disorders for all individuals within the study population.31 These registers include nationwide data on all hospital contacts (inpatient, outpatient, and emergency ward visits) from 1995 onward. In Denmark, hospital treatment is free of charge, all visits are registered, and diagnoses of mental disorders are made according the ICD-10 Classification of Mental and Behavioral Disorders: Diagnostic Criteria for Research (ICD-10-DCR), since 1994.32 The ICD-10-DCR codes of the categories of disorders are shown in Table 1, and observation time, stratified by sex, is presented in eTable 1 in the Supplement. Individuals with more than 1 disorder were included in the numerator for each specific disorder. Age at diagnosis was defined as the first day of the first contact, given the diagnosis of interest.
Table 1. Diagnostic Classification of Mental Disorders According to the ICD-10-DCR and the Number of New Cases During Follow-up of the Cohorta.
| Diagnostic Group | ICD-10-DCR Code | No. of Incident Cases With Mental Disorders During Follow-upb |
|---|---|---|
| Any mental disorder | F00-99 | 99 926 |
| Organic mental disorders | F00-09 | 413 |
| Substance use disorders | F10-19 | 6122 |
| Alcohol abuse | F10 | 3951 |
| Cannabis use | F12 | 1323 |
| Schizophrenia spectrum disorder | F20-29 | 2678 |
| Schizophrenia | F20 | 610 |
| Acute psychoses | F23 | 620 |
| Mood disorders | F30-39 | 7396 |
| Bipolar disorder | F30-31 | 314 |
| Depressive episode | F32-33 | 6940 |
| Anxiety disorders | F40-48 plus F93 | 33 541 |
| OCD | F42 | 4359 |
| Eating disorders | F50 | 5429 |
| Anorexia nervosa | F50.0 | 1649 |
| Bulimia | F50.2 | 291 |
| Personality disorders | F60-69 | 2631 |
| Intellectual disability | F7 | 9236 |
| Other developmental disorders | F80-83 | 15 493 |
| Autism spectrum disorders | F84.x excluding F84.2-F84.4 | 21 602 |
| Childhood autism | F84.0 | 7844 |
| Asperger syndrome | F84.5 | 5074 |
| ADHD | F90.0 plus F98.8 | 30 776 |
| Combined type | F90 | 26 285 |
| Inattentive type | F98.8 | 5973 |
| ODD/CD | F91 plus F90.1 | 6094 |
| Attachment disorders | F94.x excluding F94.0 | 4518 |
| Tic disorders | F95 | 6793 |
Abbreviations: ADHD, attention-deficit/hyperactivity disorder; ICD-10-DCR, ICD-10 Classification of Mental and Behavioral Disorders: Diagnostic Criteria for Research; OCD, obsessive-compulsive disorder; ODD/CD, oppositional defiant disorder/conduct disorder.
Participants were born in Denmark from January 1, 1995, through December 31, 2016, and followed up until 18 years of age or date of death, emigration, or December 31, 2016, whichever came first.
Individuals with more than 1 disorder were included in the numerator for each of the separate disorders.
Study Design
In this nationwide cohort study, all included children were followed up from birth. Follow-up was terminated at the date of the first diagnosis of the disorder (for each disorder separately), death, emigration from Denmark, or December 31, 2016, whichever came first. Ignoring censoring from emigration and/or death would have biased the incidence rates toward underestimation and the cumulative incidences toward overestimation.33 Competing risk is present when the failure event may be one of several distinct failure types, in this case date of onset, death, disappearance, or emigration.
Statistical Analysis
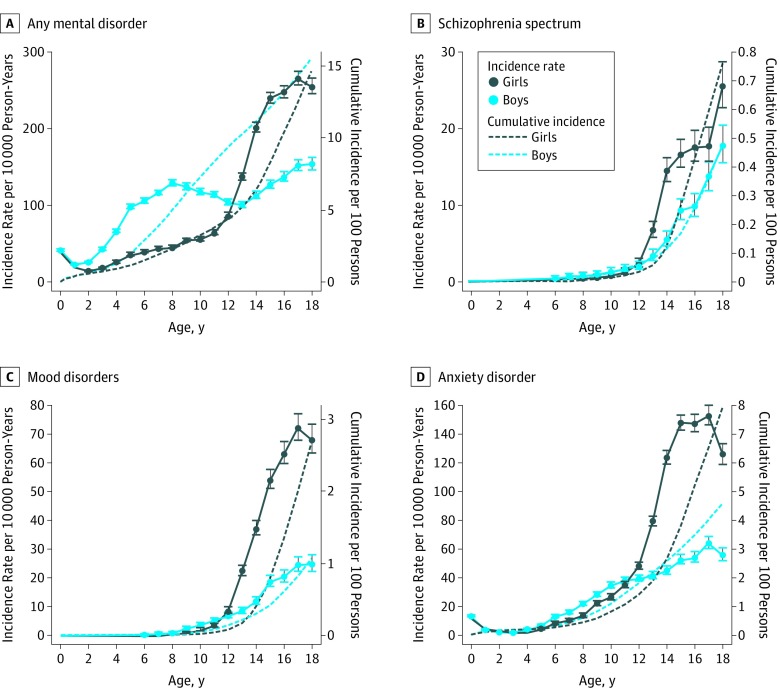
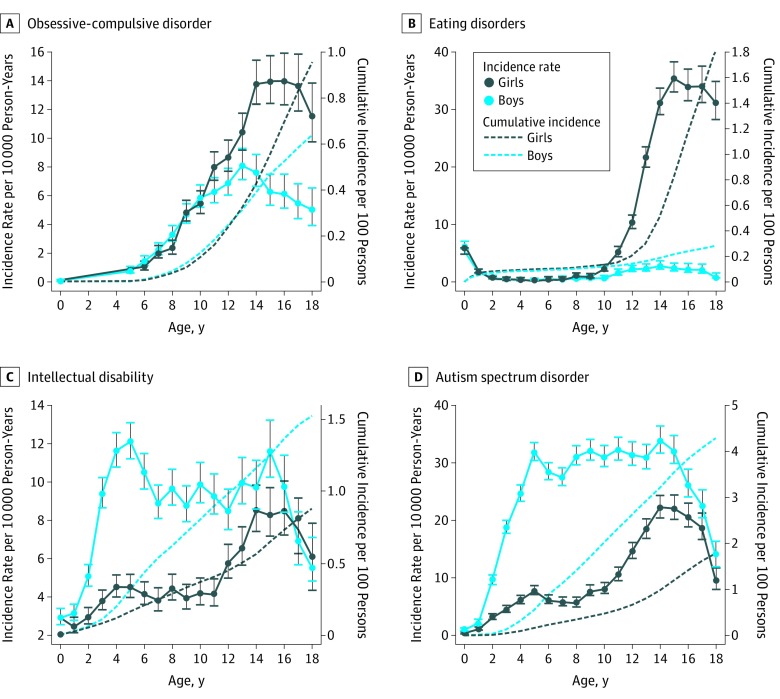
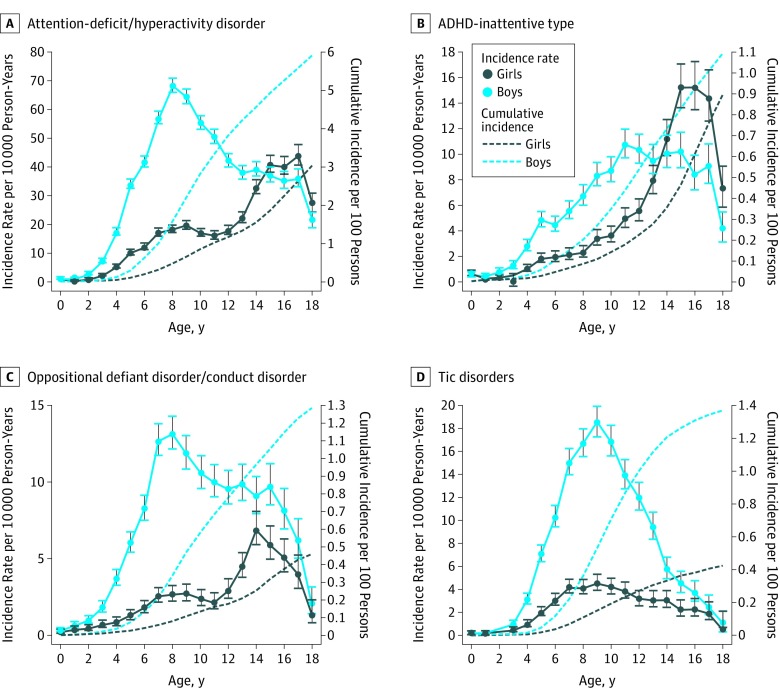
Data were analyzed from September 14, 2018, through June 11, 2019. We estimated sex- and age-specific incidence rates (incident cases per 10 000 person-years) and cumulative incidences (probability per 100 persons in the population diagnosed before a given age) of any psychiatric disorder (ICD-10-DCR codes F00-F99) and each of the separate mental disorders before 6, 13, and 18 years of age. We refer to cumulative incidence as the risk of a disorder. In Figures 1, 2, and 3, incidence rates are shown in 1-year age intervals (or expanded intervals including >10 cases). In a sensitivity analysis, we estimated the cumulative incidences at 13 years of age, including only individuals born from 1995 through 2003 for whom complete follow-up data were available to examine possible cohort effects.34
Figure 1. Sex- and Age-Specific Incidence Rates and Cumulative Incidences for Any Mental Disorder, Schizophrenia Spectrum Disorder, Mood Disorders, and Anxiety Disorder.
Any mental disorder was identified as ICD-10 Classification of Mental and Behavioral Disorders: Diagnostic Criteria for Research (ICD-10-DCR), codes F00 to F99; schizophrenia spectrum disorder, as ICD-10-DCR codes F20 to F29; mood disorders, as ICD-10-DCR codes F30 to F39; and anxiety disorder, as ICD-10-DCR codes F40 to F48 and F93. Error bars show the 95% CIs in designated age ranges. Owing to the large sample size, the 95% CIs for the cumulative incidences are very close to the estimates and are therefore not shown. Because the cumulative incidences are estimated continuously with respect to age and the incidence rates are estimated in 1-year age intervals, the abscissa for the cumulative incidence measures the exact age, whereas the abscissa for the incidence rates measures the lowest cutoff point for the age interval. The y-axis scales differ by disorder to correspond to the range of observed outcomes.
Figure 2. Sex- and Age-Specific Incidence Rates and Cumulative Incidences for Obsessive-Compulsive Disorder, Eating Disorders, Intellectual Disability, and Autism Spectrum Disorders.
Obsessive-compulsive disorder was identified as ICD-10 Classification of Mental and Behavioral Disorders: Diagnostic Criteria for Research (ICD-10-DCR), code F42; eating disorders, as ICD-10-DCR code F50; intellectual disability, as ICD-10-DCR codes F70 to F79; and autism spectrum disorders, as ICD-10-DCR codes F84.x, excluding F84.2 to F84.4. Error bars show the 95% CIs in designated age ranges. Owing to the large sample size, the 95% CIs for the cumulative incidences are very close to the estimates and are therefore not shown. Because the cumulative incidences are estimated continuously with respect to age and the incidence rates are estimated in 1-year age intervals, the abscissa for the cumulative incidence measures the exact age, whereas the abscissa for the incidence rates measures the lowest cutoff point for the age interval. The y-axis scales differ by disorder to correspond to the range of observed outcomes.
Figure 3. Sex- and Age-Specific Incidence Rates and Cumulative Incidences for Attention-Deficit/Hyperactivity Disorder (ADHD), ADHD-Inattentive Type, Oppositional Defiant Disorder/Conduct Disorder, and Tic Disorders.
ADHD was identified as ICD-10 Classification of Mental and Behavioral Disorders: Diagnostic Criteria for Research (ICD-10-DCR), codes F90 and F98.8; ADHD-inattentive type, as ICD-10-DCR code F98.8; oppositional defiant disorder/conduct disorder, as ICD-10-DCR codes F91 plus F90.1; and tic disorders, as ICD-10-DCR code F95. Error bars show the 95% CIs in designated age ranges. Owing to the large sample size, the 95% CIs for the cumulative incidences are very close to the estimates and are therefore not shown. Because the cumulative incidences are estimated continuously with respect to age and the incidence rates are estimated in 1-year age intervals, the abscissa for the cumulative incidence measures the exact age, whereas the abscissa for the incidence rates measures the lowest cutoff point for the age interval. The y-axis scales differ by disorder to correspond to the range of observed outcomes.
We used the GENMOD procedure in SAS software, release 9.4 (SAS Institute, Inc),35 to perform a Poisson regression analysis with the logarithm of person-years as an offset and to produce likelihood ratio–based incidence rates, 95% CIs, and 2-sided P values at a significance level of .05. This level is equivalent to a Cox proportional hazards regression under the assumption of piecewise constant incidence rates. The cumulative incidence was estimated in the presence of competing risk using the SAS-macro comprisk.36
Results
The study population consisted of 1.3 million children born in Denmark from 1995 through 2016 and was followed up until December 31, 2016, resulting in 14 million person-years of observation. In total, 99 926 individuals (41 350 girls and 58 576 boys) had a diagnosis of a mental disorder before 18 years of age. Among the overall study population, 2.7% were censored before the end of follow-up owing to death (n = 4962), disappearance (n = 515), and emigration from Denmark (n = 31 019).
Risks of Mental Disorders by 18 Years of Age
The risk of being diagnosed with any mental disorder before 18 years of age was 15.01% (95% CI, 14.98%-15.17%) in all individuals, 14.63% (95% CI, 14.48%-14.77%) in girls, and 15.51% (95% CI, 15.18%-15.84%) in boys (Table 2). The disorder with the highest cumulative incidence by 18 years of age in girls was anxiety disorder (7.85%; 95% CI, 7.74%-7.97%); in boys, attention-deficit/hyperactivity disorder (ADHD) (5.90%; 95% CI, 5.76%-6.03%). Figures 1 through 3 and eFigures 1 through 4 in the Supplement show the age-specific incidence rates and cumulative incidences for any mental disorder and each of the specific mental disorders investigated for boys and girls separately.
Table 2. Cumulative Incidences of Diagnosed Mental Disorders in Childhood and Adolescence in a Nationwide Cohorta.
| Diagnostic Group | No. of Incident Cases | Cumulative Incidence, % (95% CI)b | ||
|---|---|---|---|---|
| Girls | Boys | Girls | Boys | |
| Any mental disorderc | 41 350 | 58 576 | 14.63 (14.48-14.77) | 15.51 (15.18-15.84) |
| Organic mental disorders | 179 | 234 | 0.07 (0.06-0.08) | 0.07 (0.05-0.11) |
| Substance use disorders | 2897 | 3225 | 1.53 (1.47-1.59) | 1.63 (1.46-1.82) |
| Alcohol abuse | 1874 | 2077 | 1.01 (0.96-1.06) | 1.07 (0.94-1.22) |
| Cannabis use | 558 | 765 | 0.31 (0.28-0.33) | 0.42 (0.35-0.49) |
| Schizophrenia spectrum disorderd | 1569 | 1109 | 0.76 (0.72-0.80) | 0.48 (0.39-0.59) |
| Schizophrenia | 360 | 250 | 0.19 (0.17-0.21) | 0.12 (0.07-0.21) |
| Acute psychoses | 346 | 274 | 0.16 (0.14-0.18) | 0.12 (0.08-0.16) |
| Mood disordersd | 5047 | 2349 | 2.54 (2.47-2.61) | 1.01 (0.84-1.21) |
| Bipolar disorder | 185 | 129 | 0.10 (0.09-0.12) | 0.06 (0.02-0.15) |
| Depressive episoded | 4793 | 2147 | 2.41 (2.34-2.48) | 0.92 (0.76-1.12) |
| Anxiety disordersd | 19 259 | 14 282 | 7.85 (7.74-7.97) | 4.58 (4.33-4.84) |
| OCDd | 2432 | 1927 | 0.96 (0.92-1.00) | 0.63 (0.56-0.72) |
| Eating disordersd | 4297 | 1132 | 1.80 (1.74-1.86) | 0.28 (0.19-0.41) |
| Anorexia nervosad | 1506 | 143 | 0.68 (0.64-0.71) | 0.05 (0.02-0.13) |
| Bulimiad | 282 | 9 | 0.16 (0.14-0.18) | 0.00 (0.00-1.67) |
| Personality disordersd | 1982 | 649 | 1.05 (1.00-1.10) | 0.30 (0.18-0.49) |
| Intellectual disabilityc | 3091 | 6145 | 0.88 (0.85-0.92) | 1.52 (1.46-1.59) |
| Other developmental disordersc | 4545 | 10 948 | 1.41 (1.37-1.46) | 2.74 (2.67-2.81) |
| Autism spectrum disordersc | 5354 | 16 248 | 1.77 (1.72-1.82) | 4.26 (4.16-4.36) |
| Childhood autism | 1600 | 6244 | 0.44 (0.42-0.46) | 1.48 (1.43-1.53) |
| Asperger syndrome | 1260 | 3814 | 0.50 (0.47-0.53) | 1.14 (1.07-1.21) |
| ADHDc | 8815 | 21 961 | 3.04 (2.97-3.11) | 5.90 (5.76-6.03) |
| Combined typec | 6995 | 19 290 | 2.35 (2.29-2.41) | 5.13 (5.00-5.25) |
| Inattentive typec | 2311 | 3662 | 0.89 (0.85-0.93) | 1.09 (1.02-1.15) |
| ODD/CDc | 1393 | 4701 | 0.46 (0.44-0.49) | 1.28 (1.23-1.33) |
| Attachment disordersc | 1705 | 2813 | 0.52 (0.49-0.54) | 0.71 (0.66-0.75) |
| Tic disordersc | 1486 | 5307 | 0.42 (0.40-0.45) | 1.36 (1.32-1.41) |
Abbreviations: ADHD, attention-deficit/hyperactivity disorder; ICD-10-DCR, ICD-10 Classification of Mental and Behavioral Disorders: Diagnostic Criteria for Research; OCD, obsessive-compulsive disorder; ODD/CD, oppositional defiant disorder/conduct disorder.
Participants were born in Denmark from January 1, 1995, through December 31, 2016, and followed up until 18 years of age or date of death, emigration, or December 31, 2016, whichever came first.
Measures the probability of being treated for the disorder before 18 years of age. Individuals with more than 1 disorder were included in the numerator for each of the separate disorders.
Boys had a higher probability of being diagnosed with the disorder by 18 years of age than girls.
Girls had higher probability of being diagnosed with the disorder by 18 years of age than boys.
Sex Differences
The incidence rate of schizophrenia spectrum disorders (Figure 1B) was low before 13 years of age, after which it increased in girls and boys. By 18 years of age, the cumulative incidence was higher in girls (0.76%; 95% CI, 0.72%-0.80%) than in boys (0.48%; 95% CI, 0.39%-0.59%). Similar patterns showing higher risks in girls were found for mood disorders (2.54% [95% CI, 2.47%-2.61%] vs 1.10% [95% CI, 0.84%-1.21%) (Figure 1C), depression (2.41% [95% CI, 2.34%-2.48%] vs 0.92% [95% CI, 0.76%-1.12%]) (Table 2), anxiety disorders (7.85% [95% CI, 7.74%-7.97%] vs 4.58% [95% CI, 4.33%-4.84%]) (Figure 1D), obsessive-compulsive disorder (OCD) (0.96% [95% CI, 0.92%-1.00%] vs 0.63% [95% CI, 0.56%-0.72%]) (Figure 2A), eating disorders (1.80% [95% CI, 1.74%-1.86%] vs 0.28% [95% CI, 0.19%-0.41%]) (Figure 2B), and personality disorders (1.05% [95% CI, 1.00%-1.10%] vs 0.30% [95% CI, 0.18%-0.49%]) (eFigure 3C in the Supplement). In most of these individuals, incidence peaked in late adolescence (approximately at 17-18 years of age).
Compared with girls, boys had higher risks of intellectual disability (1.52% [95% CI, 1.46%-1.59%] vs 0.88% [95% CI, 0.85%-0.92%]), autism spectrum disorders (ASD) (4.26% [95% CI, 4.16%-4.36%] vs 1.77% [95% CI, 1.72%-1.82%]), other developmental disorders (2.74% [95% CI, 2.67%-2.81%] vs 1.41% [95% CI, 1.37%-1.46%]), ADHD (5.90% [95% CI, 5.76%-6.03%] vs 3.04% [95% CI, 2.97%-3.11%]), oppositional defiant disorder/conduct disorder (ODD/CD) (1.28% [95% CI, 1.23%-1.33%] vs 0.46% [95% CI, 0.44%-0.49%]), attachment disorders (0.71% [95% CI, 0.66%-0.75%] vs 0.52% [95% CI, 0.49%-0.54%]), and tic disorders (1.36% [95% CI, 1.32%-1.41%] vs 0.42% [95% CI, 0.40%-0.45%]) (Table 2). For boys, the ASD incidence sharply increased from birth to peak at 4 years of age, after which it was almost constant until 15 years of age, when it declined (Figure 2D). For girls, the ASD incidence was low until 10 years of age, then increased and peaked in early adolescence. In ADHD (Figure 3A), the incidence in boys increased steadily until it peaked at 8 years of age, then steadily declined, whereas the incidence in girls was almost constant from 7 to 12 years of age, after which it increased to peak at 17 years of age, where the incidence of ADHD in girls was higher than in boys. Similar patterns with a late adolescent peak in girls (but not in boys) were seen in ODD/CD (Figure 3C), other developmental disorders (eFigure 3D in the Supplement), and attachment disorders (eFigure 4D in the Supplement).
Risks of Mental Disorders by 6 and 13 Years of Age
The cumulative incidence of any mental disorder before 6 and 13 years of age was higher in boys (2.78% [95% CI, 2.44%-3.15%] and 10.23% [95% CI, 9.90%-10.57%], respectively) than in girls (1.45% [95% CI, 1.42%-1.49%] and 5.17% [95% CI, 5.10%-5.24%], respectively) (eTables 2 and 3 in the Supplement). Risk in total of being diagnosed before 6 years of age was 2.13% (95% CI, 2.11%-2.16%) (eTable 3 in the Supplement). The risk of anxiety disorders by 6 and 13 years of age was higher in boys (0.31% [95% CI, 0.13%-0.67%] and 2.17% [95% CI, 1.93%-2.44%], respectively) than in girls (0.27% [95% CI, 0.26%-0.29%] and 1.88% [95% CI, 1.83%-1.92%], respectively). However, by 18 years of age, the pattern was reversed, with a higher risk of anxiety disorders in girls (7.85%; 95% CI, 7.74%-7.97%) than in boys (4.58%; 95% CI, 4.33%-4.84%).
Sensitivity Analyses
When including only individuals with complete follow-up data available, the estimated cumulative incidence of mental disorders tended to be lower than in our main analyses (eTable 4 in the Supplement). In girls, risks were lower for 8 of the 27 mental disorders investigated; in boys, risks were lower for 5 of the disorders. For girls and boys, the largest difference from our main analyses was seen in the cumulative incidence of childhood autism (sensitivity analysis, 0.20% [95% CI, 0.19%-0.22%] in girls and 0.85% [95% CI, 0.80%-0.89%] in boys; main analysis, 0.44% [95% CI, 0.42-0.46] in girls and 1.48% [95% CI, 1.43%-1.53%] in boys).
Discussion
Worldwide, this nationwide study is the first, to our knowledge, of the incidence of the full spectrum of diagnosed mental disorders in childhood and adolescence. Herein, we will discuss 4 key findings.
Risk of Mental Disorders
We found that 15.01% of all children and adolescents were diagnosed with a mental disorder before reaching 18 years of age, which is consistent with the overall prevalence of 13% to 20% in US surveys26,37,38,39,40 and the estimated worldwide prevalence of mental disorders in young people of 13.4%.41 The prevalence of anxiety disorders in US surveys was 4.4% in girls and 5.0% in boys (7.85% and 4.58%, respectively, in our study).40 Depression was more prevalent in the United States (3.7% in girls and 4.1% in boys)40 compared with our sample (2.41% and 0.92%, respectively), especially in boys. Our study is likely biased toward capture of the more severe cases with depression, whereas surveys in the US studies are often based on retrospective information from the participating parents (potentially leading to misclassification and recall and selection bias), and the methodological aspects may explain some of these differences.
Sex Differences in Peaks in Incidence Rates
Although we obtained statistically significantly different estimates of the risk of any mental disorder in girls and boys, these rates were conceptually identical. Our study is the first, to our knowledge, to report girls having later peaks in the incidence of ASD, ADHD, ODD/CD, other developmental disorders, and attachment disorders compared with boys. Indeed, most girls with neurodevelopmental disorders were diagnosed during late adolescence despite these disorders having an early age of onset. Cumulative incidence of any mental disorders by 13 years of age was also higher in boys than in girls but equal between sexes by 18 years of age. These findings suggest a delayed detection of mental disorders in girls. In support of this possibility, studies of time trends42,43 have found larger increases in the number of girls being diagnosed with ASD and ADHD compared with the increase in the number of boys being diagnosed. Further, compared with boys, girls have been found to be more likely to have undiagnosed ADHD.44
Previous studies on the incidence rates of OCD in children and adolescents have found no differences or mixed sex differences in occurrence45 or higher rates in boys.46,47 We found equal incidence rates before 10 years of age, after which the incidence rate increased more in girls than in boys; by 18 years of age, the risk of OCD was higher in girls than boys. The incidence of OCD peaked in both sexes in early adolescence rather than in late adolescence, contrary to previous reports.45 For eating disorders48,49,50 and mood disorders,51 our findings on age at peak of incidences were consistent with previous studies.
Sex Differences in the Risk of Selected Mental Disorders
We found that girls were more likely to be diagnosed with schizophrenia spectrum disorder (ie, early-onset), mood disorders, anxiety disorders, OCD, eating disorders, and personality disorders, and boys were more likely to be diagnosed with intellectual disability, ASD, other developmental disorders, ADHD, ODD/CD, attachment disorders, and tic disorders. Despite girls having a higher risk of anxiety disorder by 18 years of age, boys had a higher risk of anxiety disorders by 13 years of age compared with girls, which has also, to our knowledge, not previously been reported.
Our finding of the female preponderance of early-onset schizophrenia spectrum disorder is novel. A meta-analysis of incident cases of schizophrenia52 found male preponderance in all age groups, including those with the first diagnosis before 20 years of age. Three other studies examining changes in the incidence of schizophrenia53,54 and early-onset schizophrenia55 over time have pointed toward sex differences similar to those found in our study, with higher incidence rates in girls than in boys in the youngest group. Another study56 has also found the mean age of onset of schizophrenia to be lower in girls compared with boys. Still, the sex difference in risk of early-onset schizophrenia spectrum disorder to date has not previously been estimated as accurately as in our sample.
To our knowledge, the incidences and risks of attachment disorders and personality disorders in children and adolescents have not been previously reported. As in adults,57 we found female preponderance in personality disorders. Very few individuals were diagnosed with personality disorder before 13 years of age, which is in accordance with diagnostic classifications and international clinical guidelines.32,58,59 Finally, we found no sex difference in the risk of substance use disorders before 18 years of age, which contrasts with findings from studies of adults.8
Risk of Mental Disorders in Preschool Children
In preschool children, the overall risk of being diagnosed with a mental disorder was 2.78% in boys and 1.45% in girls (2.13% in total). Apart from a handful of studies related to tic disorders14 and ASD,14,42 our study, to our knowledge, provides the most detailed estimates for the risk of being diagnosed with a broader range of mental disorder in children younger than 6 years of age.
Relevance
We believe the novelty of this report is the comprehensive estimates of risks of diagnosed mental disorders throughout childhood and adolescence in a total nationwide population, and this adds new knowledge to the field of mental health. The existing literature mainly reports prevalence rates in a population alive at a certain point, only obtaining data on surviving individuals, thereby potentially missing data on those with the most severe psychopathologic diagnoses who did not survive until start of the study. Surveys estimating lifetime prevalence rates retrospectively are also prone to recall bias and selection bias, and the occurrence of episodic or remitting disorders may be underestimated in prevalence studies. However, to fully understand the epidemiology of mental disorders in children and adolescents, surveys on prevalence rates and register-based studies on incidence rates are both required.
As such, with unprecedented comprehensiveness (covering an entire nation) examining the broad diagnostic spectrum and reporting detailed sex- and age-specific patterns, our study offers additional new knowledge on the occurrence of mental disorders in children and adolescents. Our estimates of incidence and risks would likely be broadly representative of many high-income nations. Many of the presented findings, including our main finding of 15.01% being diagnosed with a mental disorder at younger than 18 years, concurs with estimates of prevalence rates obtained in the previous surveys using the most rigorous methods. Our findings may also be thought of as important comparisons for studies evaluating prevalence rates of mental disorders in children in low-income countries or living in situations of extreme circumstances, such as war, natural disasters, or other humanitarian emergencies, all of which may influence the occurrence of mental disorders in children.60,61,62
According to the World Health Organization’s most recent Mental Health Atlas from 2017, only 18% of the member states had a plan or strategy for child and adolescent mental health.63 We believe the evidence presented in this study of the patterns of distribution and probabilities of all diagnosed mental disorders across ages and sexes during childhood and adolescence may strengthen advocacy and governance for child and adolescent mental health and form an important platform to guide future policies on access to mental health care, planning of services, prioritizing of resources in public health care, the promotion of human rights of young people with mental disorders, and future research on preventive measures, risk factors, course, and outcome of mental disorders in this age group.
Strengths and Limitations
This study has some strengths. The applied design has previously been used in a study of adults,8 and its main strength lies in the complete and nationwide data coverage during several decades and in the high quality of the diagnostic data, which is based on comprehensive clinical assessments of all mental disorders by cross-disciplinary clinical teams, including child and adolescent psychiatrists. Public health care in Denmark is free of charge, and monetary factors are thus less likely to affect the likelihood of receiving treatment in our study compared with studies performed in other countries.
However, the applied methods also have limitations. Our study was not aimed at examining time trends, and, as in other observational studies, our estimates may be biased by cohort effects.34 Our sensitivity analyses suggest slight overestimation of the risk of a few mental disorders in the main analysis. This overestimation may be related to higher incidence rates in younger cohorts and changes over time in thresholds for referral, attitudes toward mental illness, available resources, and/or environmental risk factors. The risks may also be underestimated because register-based studies are unable to detect mental disorders for which the patients or their families do not seek help (eg, “wait and see”). Further, we did not include individuals with mental disorders diagnosed outside hospital departments (by psychiatrists in private practices). However, in Denmark, most children and adolescents assessed and treated for mental disorders receive such care within public hospital departments. For instance, for ADHD, more than 86% of all cases are assessed in a hospital setting;64 for anxiety and depression, this fraction may be lower. In Denmark, only licensed child and adolescent psychiatrists (not general practitioners) are authorized to initiate pharmacological treatment of mental disorders in individuals younger than 18 years, as stipulated by the Danish health authorities.65,66,67 Finally, although some diagnoses have been validated in Danish registers (eg, schizophrenia, depression, mood disorder, ADHD, and childhood autism),68,69,70,71,72,73,74,75 not all of the diagnostic categories have been validated, especially not in preschool children.
Conclusions
This population-based study provides, to our knowledge, a first comprehensive nationwide assessment of the incidence and risks of all mental disorders in childhood and adolescence. For many mental disorders, we believe we have identified age- and sex-specific patterns of occurrence that, to our knowledge, have not been previously reported. The distinct signatures of the different mental disorders with respect to sex and age may have important implications for service planning and etiological research.
eTable 1. No. of New Cases With Mental Disorders in the Total Cohort and Their Contributing Time of Observation During Follow-up, Stratified by Sex
eTable 2. Cumulative Incidences of Mental Disorders by 13 Years of Age, in a Nationwide Cohort
eTable 3. Cumulative Incidences of Selected Mental Disorders by 6 Years of Age, in a Nationwide Cohort
eTable 4. Sensitivity Analyses of Cumulative Incidences of Mental Disorders by 13 Years of Age, in a Subset of Cohorts Including Only Individuals Born 1995-2003
eFigure 1. Sex- and Age-Specific Incidence Rates and Cumulative Incidences for Organic Mental Disorders, Substance Use Disorders, Alcohol Abuse, and Cannabis Use
eFigure 2. Sex- and Age-Specific Incidence Rates and Cumulative Incidences for Schizophrenia, Acute Psychoses, Bipolar Disorder, and Depressive Episode
eFigure 3. Sex- and Age-Specific Incidence Rates and Cumulative Incidences for Anorexia Nervosa, Bulimia, Personality Disorders, and Other Developmental Disorders
eFigure 4. Sex- and Age-Specific Incidence Rates and Cumulative Incidences for Childhood Autism, Asperger Syndrome, ADHD-Combined Type, and Attachment Disorders
References
- 1.Whiteford HA, Degenhardt L, Rehm J, et al. Global burden of disease attributable to mental and substance use disorders: findings from the Global Burden of Disease Study 2010. Lancet. 2013;382(9904):1575-1586. doi: 10.1016/S0140-6736(13)61611-6 [DOI] [PubMed] [Google Scholar]
- 2.Naghavi M, Abajobir AA, Abbafati C, et al. ; GBD 2016 Causes of Death Collaborators . Global, regional, and national age-sex specific mortality for 264 causes of death, 1980-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet. 2017;390(10100):1151-1210. doi: 10.1016/S0140-6736(17)32152-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Institute for Health Metrics and Evaluation (IHME) GBD Compare Data Visualization. Seattle, WA: IHME, University of Washington; 2017. https://vizhub.healthdata.org/gbd-compare. Accessed June 1, 2018.
- 4.World Health Organization Mental Health Action Plan 2013-2020. Geneva, Switzerland: World Health Organization; 2013. [Google Scholar]
- 5.Erskine HE, Baxter AJ, Patton G, et al. The global coverage of prevalence data for mental disorders in children and adolescents. Epidemiol Psychiatr Sci. 2017;26(4):395-402. doi: 10.1017/S2045796015001158 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.European Profile of Prevention and Promotion of Mental Health (EuroPoPP-MH); Institute of Mental Health. Mental Health Systems in the European Union Member States, Status of Mental Health in Populations and Benefits to be Expected from Investments into Mental Health. Nottingham, UK: Executive Agency for Health and Consumers Tender; July 2013. https://ec.europa.eu/health/sites/health/files/mental_health/docs/europopp_full_en.pdf. Accessed October 24, 2019. [Google Scholar]
- 7.Rothman KJ, Greenland S, Lash TL. Modern Epidemiology. 3rd ed Philidelphia, PA: Lippincott Williams & Wilkins; 2008. [Google Scholar]
- 8.Pedersen CB, Mors O, Bertelsen A, et al. A comprehensive nationwide study of the incidence rate and lifetime risk for treated mental disorders. JAMA Psychiatry. 2014;71(5):573-581. doi: 10.1001/jamapsychiatry.2014.16 [DOI] [PubMed] [Google Scholar]
- 9.McGrath JJ, Petersen L, Agerbo E, Mors O, Mortensen PB, Pedersen CB. A comprehensive assessment of parental age and psychiatric disorders. JAMA Psychiatry. 2014;71(3):301-309. doi: 10.1001/jamapsychiatry.2013.4081 [DOI] [PubMed] [Google Scholar]
- 10.Benros ME, Nielsen PR, Nordentoft M, Eaton WW, Dalton SO, Mortensen PB. Autoimmune diseases and severe infections as risk factors for schizophrenia: a 30-year population-based register study. Am J Psychiatry. 2011;168(12):1303-1310. doi: 10.1176/appi.ajp.2011.11030516 [DOI] [PubMed] [Google Scholar]
- 11.Pedersen CB, Mortensen PB. Evidence of a dose-response relationship between urbanicity during upbringing and schizophrenia risk. Arch Gen Psychiatry. 2001;58(11):1039-1046. doi: 10.1001/archpsyc.58.11.1039 [DOI] [PubMed] [Google Scholar]
- 12.Laursen TM, Nordentoft M, Mortensen PB. Excess early mortality in schizophrenia. Annu Rev Clin Psychol. 2014;10:425-448. doi: 10.1146/annurev-clinpsy-032813-153657 [DOI] [PubMed] [Google Scholar]
- 13.Laursen TM, Munk-Olsen T, Agerbo E, Gasse C, Mortensen PB. Somatic hospital contacts, invasive cardiac procedures, and mortality from heart disease in patients with severe mental disorder. Arch Gen Psychiatry. 2009;66(7):713-720. doi: 10.1001/archgenpsychiatry.2009.61 [DOI] [PubMed] [Google Scholar]
- 14.Atladóttir HO, Parner ET, Schendel D, Dalsgaard S, Thomsen PH, Thorsen P. Time trends in reported diagnoses of childhood neuropsychiatric disorders: a Danish cohort study. Arch Pediatr Adolesc Med. 2007;161(2):193-198. doi: 10.1001/archpedi.161.2.193 [DOI] [PubMed] [Google Scholar]
- 15.Atladottir HO, Gyllenberg D, Langridge A, et al. The increasing prevalence of reported diagnoses of childhood psychiatric disorders: a descriptive multinational comparison. Eur Child Adolesc Psychiatry. 2015;24(2):173-183. doi: 10.1007/s00787-014-0553-8 [DOI] [PubMed] [Google Scholar]
- 16.Steinhausen HC, Jakobsen H. Incidence rates of treated mental disorders in childhood and adolescence in a complete nationwide birth cohort. J Clin Psychiatry. 2019;80(3):17m12012. doi: 10.4088/JCP.17m12012 [DOI] [PubMed] [Google Scholar]
- 17.Ottosen C, Larsen JT, Faraone SV, et al. Sex differences in comorbidity patterns of attention-deficit/hyperactivity disorder. J Am Acad Child Adolesc Psychiatry. 2019;58(4):412-422.e3. doi: 10.1016/j.jaac.2018.07.910 [DOI] [PubMed] [Google Scholar]
- 18.Nielsen PR, Benros ME, Dalsgaard S. Associations between autoimmune diseases and attention-deficit/hyperactivity disorder: a nationwide study. J Am Acad Child Adolesc Psychiatry. 2017;56(3):234-240.e1. doi: 10.1016/j.jaac.2016.12.010 [DOI] [PubMed] [Google Scholar]
- 19.Weisman O, Agerbo E, Carter CS, et al. Oxytocin-augmented labor and risk for autism in males. Behav Brain Res. 2015;284:207-212. doi: 10.1016/j.bbr.2015.02.028 [DOI] [PubMed] [Google Scholar]
- 20.Dalsgaard S, Waltoft BL, Leckman JF, Mortensen PB. Maternal history of autoimmune disease and later development of Tourette syndrome in offspring. J Am Acad Child Adolesc Psychiatry. 2015;54(6):495-501.e1. doi: 10.1016/j.jaac.2015.03.008 [DOI] [PubMed] [Google Scholar]
- 21.Scott JG, Giørtz Pedersen M, Erskine HE, et al. Mortality in individuals with disruptive behavior disorders diagnosed by specialist services: a nationwide cohort study. Psychiatry Res. 2017;251:255-260. doi: 10.1016/j.psychres.2017.02.029 [DOI] [PubMed] [Google Scholar]
- 22.Dalsgaard S, Østergaard SD, Leckman JF, Mortensen PB, Pedersen MG. Mortality in children, adolescents, and adults with attention deficit hyperactivity disorder: a nationwide cohort study. Lancet. 2015;385(9983):2190-2196. doi: 10.1016/S0140-6736(14)61684-6 [DOI] [PubMed] [Google Scholar]
- 23.Dalsgaard S, Mortensen PB, Frydenberg M, Thomsen PH. Conduct problems, gender and adult psychiatric outcome of children with attention-deficit hyperactivity disorder. Br J Psychiatry. 2002;181:416-421. doi: 10.1192/bjp.181.5.416 [DOI] [PubMed] [Google Scholar]
- 24.Meier SM, Uher R, Mors O, et al. Specific anxiety disorders and subsequent risk for bipolar disorder: a nationwide study. World Psychiatry. 2016;15(2):187-188. doi: 10.1002/wps.20314 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Elsabbagh M, Divan G, Koh YJ, et al. Global prevalence of autism and other pervasive developmental disorders. Autism Res. 2012;5(3):160-179. doi: 10.1002/aur.239 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Merikangas KR, Nakamura EF, Kessler RC. Epidemiology of mental disorders in children and adolescents. Dialogues Clin Neurosci. 2009;11(1):7-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kessler RC, Avenevoli S, Costello J, et al. Severity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication Adolescent Supplement. Arch Gen Psychiatry. 2012;69(4):381-389. doi: 10.1001/archgenpsychiatry.2011.1603 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Moffitt TE, Harrington H, Caspi A, et al. Depression and generalized anxiety disorder: cumulative and sequential comorbidity in a birth cohort followed prospectively to age 32 years. Arch Gen Psychiatry. 2007;64(6):651-660. doi: 10.1001/archpsyc.64.6.651 [DOI] [PubMed] [Google Scholar]
- 29.Sayal K, Washbrook E, Propper C. Childhood behavior problems and academic outcomes in adolescence: longitudinal population-based study. J Am Acad Child Adolesc Psychiatry. 2015;54(5):360-368.e2. doi: 10.1016/j.jaac.2015.02.007 [DOI] [PubMed] [Google Scholar]
- 30.Pedersen CB, Gøtzsche H, Møller JØ, Mortensen PB. The Danish Civil Registration System: a cohort of eight million persons. Dan Med Bull. 2006;53(4):441-449. [PubMed] [Google Scholar]
- 31.Mors O, Perto GP, Mortensen PB. The Danish Psychiatric Central Research Register. Scand J Public Health. 2011;39(7)(suppl):54-57. doi: 10.1177/1403494810395825 [DOI] [PubMed] [Google Scholar]
- 32.World Health Organization The ICD-10 Classification of Mental and Behavioural Disorders: Diagnostic Criteria for Research. Geneva, Switzerland: World Health Organization; 1993. [Google Scholar]
- 33.Andersen PK, Geskus RB, de Witte T, Putter H. Competing risks in epidemiology: possibilities and pitfalls. Int J Epidemiol. 2012;41(3):861-870. doi: 10.1093/ije/dyr213 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hansen SN, Overgaard M, Andersen PK, Parner ET. Estimating a population cumulative incidence under calendar time trends. BMC Med Res Methodol. 2017;17(1):7. doi: 10.1186/s12874-016-0280-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.SAS Institute Inc SAS Software (release 9.4). Cary, NC: SAS Institute Inc; 2013. [Google Scholar]
- 36.Gooley TA, Leisenring W, Crowley J, Storer BE. Estimation of failure probabilities in the presence of competing risks: new representations of old estimators. Stat Med. 1999;18(6):695-706. doi: [DOI] [PubMed] [Google Scholar]
- 37.World Health Organization Mental Health: A State of Well-being. Geneva, Switzerland: World Health Organization; 2014. https://www.who.int/features/factfiles/mental_health/en/index.html. Accessed August 26, 2019.
- 38.Merikangas KR, He JP, Burstein M, et al. Lifetime prevalence of mental disorders in US adolescents: results from the National Comorbidity Survey Replication–Adolescent Supplement (NCS-A). J Am Acad Child Adolesc Psychiatry. 2010;49(10):980-989. doi: 10.1016/j.jaac.2010.05.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Merikangas KR, He JP, Brody D, Fisher PW, Bourdon K, Koretz DS. Prevalence and treatment of mental disorders among US children in the 2001-2004 NHANES. Pediatrics. 2010;125(1):75-81. doi: 10.1542/peds.2008-2598 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Perou R, Bitsko RH, Blumberg SJ, et al. ; Centers for Disease Control and Prevention (CDC) . Mental health surveillance among children—United States, 2005-2011. MMWR Suppl. 2013;62(2):1-35. [PubMed] [Google Scholar]
- 41.Polanczyk GV, Salum GA, Sugaya LS, Caye A, Rohde LA. Annual research review: a meta-analysis of the worldwide prevalence of mental disorders in children and adolescents. J Child Psychol Psychiatry. 2015;56(3):345-365. doi: 10.1111/jcpp.12381 [DOI] [PubMed] [Google Scholar]
- 42.Jensen CM, Steinhausen HC, Lauritsen MB. Time trends over 16 years in incidence-rates of autism spectrum disorders across the lifespan based on nationwide Danish Register Data. J Autism Dev Disord. 2014;44(8):1808-1818. doi: 10.1007/s10803-014-2053-6 [DOI] [PubMed] [Google Scholar]
- 43.Mohr Jensen C, Steinhausen HC. Time trends in incidence rates of diagnosed attention-deficit/hyperactivity disorder across 16 years in a nationwide Danish registry study. J Clin Psychiatry. 2015;76(3):e334-e341. doi: 10.4088/JCP.14m09094 [DOI] [PubMed] [Google Scholar]
- 44.Madsen KB, Ravn MH, Arnfred J, Olsen J, Rask CU, Obel C. Characteristics of undiagnosed children with parent-reported ADHD behaviour. Eur Child Adolesc Psychiatry. 2018;27(2):149-158. doi: 10.1007/s00787-017-1029-4 [DOI] [PubMed] [Google Scholar]
- 45.Rintala H, Chudal R, Leppämäki S, Leivonen S, Hinkka-Yli-Salomäki S, Sourander A. Register-based study of the incidence, comorbidities and demographics of obsessive-compulsive disorder in specialist healthcare. BMC Psychiatry. 2017;17(1):64. doi: 10.1186/s12888-017-1224-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Huang LC, Tsai KJ, Wang HK, et al. Prevalence, incidence, and comorbidity of clinically diagnosed obsessive-compulsive disorder in Taiwan: a national population-based study. Psychiatry Res. 2014;220(1-2):335-341. doi: 10.1016/j.psychres.2014.08.011 [DOI] [PubMed] [Google Scholar]
- 47.Thomsen PH. Children and adolescents with obsessive-compulsive disorder: an analysis of sociodemographic background: a case-control study. Psychopathology. 1994;27(6):303-311. doi: 10.1159/000284888 [DOI] [PubMed] [Google Scholar]
- 48.Javaras KN, Runfola CD, Thornton LM, et al. Sex- and age-specific incidence of healthcare-register–recorded eating disorders in the complete Swedish 1979-2001 birth cohort. Int J Eat Disord. 2015;48(8):1070-1081. doi: 10.1002/eat.22467 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Steinhausen HC, Jensen CM. Time trends in lifetime incidence rates of first-time diagnosed anorexia nervosa and bulimia nervosa across 16 years in a Danish nationwide psychiatric registry study. Int J Eat Disord. 2015;48(7):845-850. doi: 10.1002/eat.22402 [DOI] [PubMed] [Google Scholar]
- 50.Zerwas S, Larsen JT, Petersen L, Thornton LM, Mortensen PB, Bulik CM. The incidence of eating disorders in a Danish register study: associations with suicide risk and mortality. J Psychiatr Res. 2015;65:16-22. doi: 10.1016/j.jpsychires.2015.03.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Jensen CM, Steinhausen HC. Time trends in lifetime incidence rates of first-time diagnosed bipolar and depressive disorders across 16 years in Danish psychiatric hospitals: a nationwide study. J Clin Psychiatry. 2016;77(12):e1570-e1575. doi: 10.4088/JCP.15m10276 [DOI] [PubMed] [Google Scholar]
- 52.van der Werf M, Hanssen M, Köhler S, et al. ; RISE Investigators . Systematic review and collaborative recalculation of 133,693 incident cases of schizophrenia. Psychol Med. 2014;44(1):9-16. doi: 10.1017/S0033291712002796 [DOI] [PubMed] [Google Scholar]
- 53.Bray I, Waraich P, Jones W, Slater S, Goldner EM, Somers J. Increase in schizophrenia incidence rates: findings in a Canadian cohort born 1975-1985. Soc Psychiatry Psychiatr Epidemiol. 2006;41(8):611-618. doi: 10.1007/s00127-006-0073-z [DOI] [PubMed] [Google Scholar]
- 54.Kühl JOG, Laursen TM, Thorup A, Nordentoft M. The incidence of schizophrenia and schizophrenia spectrum disorders in Denmark in the period 2000-2012: a register-based study. Schizophr Res. 2016;176(2-3):533-539. doi: 10.1016/j.schres.2016.06.023 [DOI] [PubMed] [Google Scholar]
- 55.Okkels N, Vernal DL, Jensen SO, McGrath JJ, Nielsen RE. Changes in the diagnosed incidence of early onset schizophrenia over four decades. Acta Psychiatr Scand. 2013;127(1):62-68. doi: 10.1111/j.1600-0447.2012.01913.x [DOI] [PubMed] [Google Scholar]
- 56.Køster A, Lajer M, Lindhardt A, Rosenbaum B. Gender differences in first episode psychosis. Soc Psychiatry Psychiatr Epidemiol. 2008;43(12):940-946. doi: 10.1007/s00127-008-0384-3 [DOI] [PubMed] [Google Scholar]
- 57.Pedersen L, Simonsen E. Incidence and prevalence rates of personality disorders in Denmark: a register study. Nord J Psychiatry. 2014;68(8):543-548. doi: 10.3109/08039488.2014.884630 [DOI] [PubMed] [Google Scholar]
- 58.American Psychiatric Association Diagnostic and Statistical Manual of Mental Disorders. 4th ed, text revision Washington, DC: American Psychiatric Association; 2000. [Google Scholar]
- 59.American Psychiatric Association Diagnostic and Statistical Manual of Mental Disorders. 5th ed Arlington, VA: American Psychiatric Publishing; 2013. [Google Scholar]
- 60.Felix E, Hernández LA, Bravo M, Ramirez R, Cabiya J, Canino G. Natural disaster and risk of psychiatric disorders in Puerto Rican children. J Abnorm Child Psychol. 2011;39(4):589-600. doi: 10.1007/s10802-010-9483-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Miller T, el-Masri M, Allodi F, Qouta S. Emotional and behavioural problems and trauma exposure of school-age Palestinian children in Gaza: some preliminary findings. Med Confl Surviv. 1999;15(4):368-378. doi: 10.1080/13623699908409478 [DOI] [PubMed] [Google Scholar]
- 62.Heiervang E, Goodman A, Goodman R. The Nordic advantage in child mental health: separating health differences from reporting style in a cross-cultural comparison of psychopathology. J Child Psychol Psychiatry. 2008;49(6):678-685. doi: 10.1111/j.1469-7610.2008.01882.x [DOI] [PubMed] [Google Scholar]
- 63.World Health Organization Mental Health Atlas 2017. Geneva, Switzerland: World Health Organization; 2018. [Google Scholar]
- 64.Christensen J, Pedersen L, Sun Y, Dreier JW, Brikell I, Dalsgaard S. Association of prenatal exposure to valproate and other antiepileptic drugs with risk for attention-deficit/hyperactivity disorder in offspring. JAMA Netw Open. 2019;2(1):e186606. doi: 10.1001/jamanetworkopen.2018.6606 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.National Board of Health Medical Specialty Report: Child and Adolescent Psychiatry. Copenhagen, Denmark: National Board of Health; 2008. [Google Scholar]
- 66.National Board of Health Clinical Guidelines for Pharmacological Treatment With Antidepressants, Antipsychotics and Stimulant Medications [in Danish]. Copenhagen, Denmark: Ministry of Health; 2000. Publication 11716. [Google Scholar]
- 67.The Danish Health Authority Clinical Guidelines for Pharmacological Treatment of Children and Adolescents With Psychiatric Disorders [in Danish]. Copenhagen, Denmark: Ministry of Health; 2013. Publication 9149. [Google Scholar]
- 68.Kessing L. Validity of diagnoses and other clinical register data in patients with affective disorder. Eur Psychiatry. 1998;13(8):392-398. doi: 10.1016/S0924-9338(99)80685-3 [DOI] [PubMed] [Google Scholar]
- 69.Lauritsen MB, Jørgensen M, Madsen KM, et al. Validity of childhood autism in the Danish Psychiatric Central Register: findings from a cohort sample born 1990-1999. J Autism Dev Disord. 2010;40(2):139-148. doi: 10.1007/s10803-009-0818-0 [DOI] [PubMed] [Google Scholar]
- 70.Linnet KM, Wisborg K, Secher NJ, et al. Coffee consumption during pregnancy and the risk of hyperkinetic disorder and ADHD: a prospective cohort study. Acta Paediatr. 2009;98(1):173-179. doi: 10.1111/j.1651-2227.2008.00980.x [DOI] [PubMed] [Google Scholar]
- 71.Dalsgaard S, Hansen N, Mortensen PB, Damm D, Thomsen PH. Reassessment of ADHD in a historical cohort of children treated with stimulants in the period 1969-1989. Eur Child Adolesc Psychiatry. 2001;10(4):230-239. doi: 10.1007/s007870170012 [DOI] [PubMed] [Google Scholar]
- 72.Mohr-Jensen C, Vinkel Koch S, Briciet Lauritsen M, Steinhausen HC. The validity and reliability of the diagnosis of hyperkinetic disorders in the Danish Psychiatric Central Research Registry. Eur Psychiatry. 2016;35:16-24. doi: 10.1016/j.eurpsy.2016.01.2427 [DOI] [PubMed] [Google Scholar]
- 73.Bock C, Bukh JD, Vinberg M, Gether U, Kessing LV. Validity of the diagnosis of a single depressive episode in a case register. Clin Pract Epidemiol Ment Health. 2009;5:4. doi: 10.1186/1745-0179-5-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Uggerby P, Østergaard SD, Røge R, Correll CU, Nielsen J. The validity of the schizophrenia diagnosis in the Danish Psychiatric Central Research Register is good. Dan Med J. 2013;60(2):A4578. [PubMed] [Google Scholar]
- 75.Jakobsen KD, Frederiksen JN, Hansen T, Jansson LB, Parnas J, Werge T. Reliability of clinical ICD-10 schizophrenia diagnoses. Nord J Psychiatry. 2005;59(3):209-212. doi: 10.1080/08039480510027698 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable 1. No. of New Cases With Mental Disorders in the Total Cohort and Their Contributing Time of Observation During Follow-up, Stratified by Sex
eTable 2. Cumulative Incidences of Mental Disorders by 13 Years of Age, in a Nationwide Cohort
eTable 3. Cumulative Incidences of Selected Mental Disorders by 6 Years of Age, in a Nationwide Cohort
eTable 4. Sensitivity Analyses of Cumulative Incidences of Mental Disorders by 13 Years of Age, in a Subset of Cohorts Including Only Individuals Born 1995-2003
eFigure 1. Sex- and Age-Specific Incidence Rates and Cumulative Incidences for Organic Mental Disorders, Substance Use Disorders, Alcohol Abuse, and Cannabis Use
eFigure 2. Sex- and Age-Specific Incidence Rates and Cumulative Incidences for Schizophrenia, Acute Psychoses, Bipolar Disorder, and Depressive Episode
eFigure 3. Sex- and Age-Specific Incidence Rates and Cumulative Incidences for Anorexia Nervosa, Bulimia, Personality Disorders, and Other Developmental Disorders
eFigure 4. Sex- and Age-Specific Incidence Rates and Cumulative Incidences for Childhood Autism, Asperger Syndrome, ADHD-Combined Type, and Attachment Disorders