Key Points
Question
Is treatment with a single dose of radiotherapy noninferior to multifraction radiotherapy delivered over 5 days among patients with metastatic cancer who have spinal canal compression?
Findings
In a clinical trial of 686 patients, the percentage who were ambulatory at 8 weeks was 69.3% in the single-fraction group vs 72.7% in the multifraction radiotherapy group. The lower CI limit for the risk difference (−11.5%) did not meet the predefined noninferiority margin of −11.0%.
Meaning
Treatment with single-fraction radiotherapy did not meet the criterion for noninferiority compared with multifraction radiotherapy for ambulatory response rate at 8 weeks, but consideration should be given to the extent to which the lower bound of the CI overlapped with the noninferiority margin.
Abstract
Importance
Malignant spinal canal compression, a major complication of metastatic cancer, is managed with radiotherapy to maintain mobility and relieve pain, although there is no standard radiotherapy regimen.
Objective
To evaluate whether single-fraction radiotherapy is noninferior to 5 fractions of radiotherapy.
Design, Setting, and Participants
Multicenter noninferiority randomized clinical trial conducted in 42 UK and 5 Australian radiotherapy centers. Eligible patients (n = 686) had metastatic cancer with spinal cord or cauda equina compression, life expectancy greater than 8 weeks, and no previous radiotherapy to the same area. Patients were recruited between February 2008 and April 2016, with final follow-up in September 2017.
Interventions
Patients were randomized to receive external beam single-fraction 8-Gy radiotherapy (n = 345) or 20 Gy of radiotherapy in 5 fractions over 5 consecutive days (n = 341).
Main Outcomes and Measures
The primary end point was ambulatory status at week 8, based on a 4-point scale and classified as grade 1 (ambulatory without the use of aids and grade 5 of 5 muscle power) or grade 2 (ambulatory using aids or grade 4 of 5 muscle power). The noninferiority margin for the difference in ambulatory status was −11%. Secondary end points included ambulatory status at weeks 1, 4, and 12 and overall survival.
Results
Among 686 randomized patients (median [interquartile range] age, 70 [64-77] years; 503 (73%) men; 44% had prostate cancer, 19% had lung cancer, and 12% had breast cancer), 342 (49.8%) were analyzed for the primary end point (255 patients died before the 8-week assessment). Ambulatory status grade 1 or 2 at week 8 was achieved by 115 of 166 (69.3%) patients in the single-fraction group vs 128 of 176 (72.7%) in the multifraction group (difference, −3.5% [1-sided 95% CI, −11.5% to ∞]; P value for noninferiority = .06). The difference in ambulatory status grade 1 or 2 in the single-fraction vs multifraction group was −0.4% (63.9% vs 64.3%; [1-sided 95% CI, −6.9 to ∞]; P value for noninferiority = .004) at week 1, −0.7% (66.8% vs 67.6%; [1-sided 95% CI, −8.1 to ∞]; P value for noninferiority = .01) at week 4, and 4.1% (71.8% vs 67.7%; [1-sided 95% CI, −4.6 to ∞]; P value for noninferiority = .002) at week 12. Overall survival rates at 12 weeks were 50% in the single-fraction group vs 55% in the multifraction group (stratified hazard ratio, 1.02 [95% CI, 0.74-1.41]). Of the 11 other secondary end points that were analyzed, the between-group differences were not statistically significant or did not meet noninferiority criterion.
Conclusions and Relevance
Among patients with malignant metastatic solid tumors and spinal canal compression, a single radiotherapy dose, compared with a multifraction dose delivered over 5 days, did not meet the criterion for noninferiority for the primary outcome (ambulatory at 8 weeks). However, the extent to which the lower bound of the CI overlapped with the noninferiority margin should be considered when interpreting the clinical importance of this finding.
Trial Registration
ISRCTN Identifiers: ISRCTN97555949 and ISRCTN97108008
This noninferiority randomized clinical trial compared the effect of external beam single-fraction 8-Gy radiotherapy vs 20 Gy of radiotherapy in 5 fractions over 5 days on ambulatory status among patients with spinal canal compression from metastatic prostate, lung, and other cancer.
Introduction
Spinal canal compression is a common complication of metastatic cancer and affected an estimated 4000 patients in the United Kingdom in 2008 and 25 000 in the United States in 2005.1,2 Most patients are treated with radiotherapy, and common practice has been to deliver 20 to 30 Gy in 5 to 10 fractions,3,4 with longer fractionation schedules for patients with a better prognosis. However, the evidence for using single-fraction radiotherapy comes from trials based on patients with bone pain from metastatic disease (eg, pelvis, long bones, skull) after excluding metastatic spinal canal compression at diagnosis.5,6 A systematic review7 on spinal canal compression consisting of only retrospective studies (which tend to be affected by bias and confounding), aside from 1 randomized clinical trial,8 reported similar outcomes between single-fraction and multifraction radiotherapy.
Guidelines from the National Institute of Health and Clinical Excellence in England9 indicate that radiotherapy may be delivered as a single treatment or several consecutive smaller treatments. The American Society for Radiation Oncology guidelines recommend a single 8-Gy radiation dose for patients with painful spinal sites, particularly if they have limited life expectancy, focusing on pain relief.10 The US National Comprehensive Cancer Network guidelines refer to radiotherapy to manage spinal canal compression, but do not indicate or recommend any schedule.11
The objective of this study was to evaluate whether single-fraction radiotherapy was noninferior to multifraction radiotherapy for managing spinal canal compression, using mobility as the clinically relevant outcome for patients.
Methods
Study Oversight and Patients
The single-fraction radiotherapy compared to multifraction radiotherapy (SCORAD) trial was approved in the United Kingdom by a single national ethics review board and in Australia by individual review boards for each institution. All patients gave written informed consent. The protocol and statistical analysis plan can be found in Supplement 1 and Supplement 2.
Eligible patients were aged at least 18 years with an estimated life expectancy greater than 8 weeks and proven diagnosis of spinal canal or cauda equina (C1-S2) compression on magnetic resonance imaging or computed tomographic scan, with single or multiple sites of compression. Histological or cytological confirmation of malignancy was required, but not for patients with clinical evidence of prostate cancer, who had to have a serum prostate-specific antigen level greater than 100 μg/L. Patients were excluded if they were able to undergo surgery or chemotherapy or if they had hematological malignancies or glioma, prophylactic treatment in the absence of radiological spinal canal compression, or previous radiotherapy targeting the spine.
Intervention and Randomization Procedure
Patients were randomized in a 1:1 ratio to receive either 20 Gy of external beam radiotherapy in 5 fractions over 5 consecutive days (daily from Monday to Friday) or 8 Gy of radiotherapy in a single fraction. Randomization was performed centrally by the University College London Cancer Trials Centre using minimization (with a random element), stratified by center, ambulatory status, primary tumor type, and presence or absence of nonskeletal metastases. Megavoltage radiotherapy was delivered to the compression site with a margin of at least 1 vertebral level above and below. The dose was prescribed at cord depth, using magnetic resonance imaging or imaging at simulation. It was mandated that treatment began within 48 hours of a decision to treat based on diagnostic imaging up to 7 days prior to commencement of treatment. Supportive care was given according to local practice, including steroids and analgesics.
End Points
Patients were assessed in clinic at about 1, 4, 8, 12, and 52 weeks after randomization, unless they were unable or unwilling to attend physically, in which case a health professional from the local hospital contacted them by telephone at these time points. Information about whether outcomes were ascertained in person or by telephone was not collected. These assessments included gathering information regarding ambulatory status, adverse events, and additional treatments received. Information about additional therapies and date of death were also obtained from medical records by research staff.
The primary end point was ambulatory response rate in patients alive at 8 weeks, which was considered a clinically meaningful time point in this population by consensus among the clinical investigators. Ambulatory status was assessed on a 4-point scale, consistent with the World Health Organization performance status, based on the validated Medical Research Council muscle power criteria,12 in which 1 indicates ambulatory without the use of walking aids and grade 5 of 5 muscle power in all muscle groups; 2, ambulatory with assistance of walking aids or grade 4 of 5 muscle power in any muscle group; 3, unable to walk with no worse than grade 2 of 5 power in all muscle groups or grade 2 of 5 power in any muscle group; and 4, absence (0/5 muscle power) or flicker (1/5 muscle power) of motor power in any muscle group. The ambulatory response rate was defined as the percentage of patients who achieved ambulatory status grade 1 or 2 at 8 weeks (which could be a result of an improvement from a grade 3 or 4 or maintenance of grade 1 or 2 from baseline) using a window of 49 to 62 days.
A secondary end point was ambulatory status assessed at 1, 4, and 12 weeks after randomization (ie, between 7-13, 21-34, and 70-97 days). Other prespecified secondary end points were (1) time to loss of ambulation among patients with ambulatory status 1 or 2 at baseline, measured from randomization until the first occurrence of grade 3 or 4 ambulatory status (those who did not lose ambulation were censored at their last assessment date); (2) time to recovery of ambulation among patients with ambulatory status 3 or 4 at baseline, measured from randomization until the first reported status of grade 1 or 2 (those without improvement were censored at their last assessment date); (3) overall survival at 12 weeks and 12 months and hazard ratio (HR) measured from randomization to death from any cause, with patients censored at the last date seen alive; (4) adverse events classified according to the Common Terminology Criteria for Adverse Events: Version 4; (5) adverse events of special interest, which were abnormal bladder function, defined as significant urinary incontinence or urinary retention requiring catheterization, or abnormal bowel function, defined as the occurrence of constipation, diarrhea, or incontinence at 1, 4, 8, and 12 weeks; (6) additional therapies after randomization, which included treatments for spinal canal compression (chemotherapy, hormone therapy, radiotherapy, and surgery) and supportive care for spinal canal compression (analgesics, antiemetics, corticosteroids, physiotherapy, and bisphosphonates); and (7) patient-reported quality of life, including pain (an important measure in spinal canal compression and specifically referred to in guidelines), assessed at baseline and week 1, 4, 8, and 12 using the European Organization for Research and Treatment of Cancer (EORTC) Quality of Life Questionnaire-Core Questionnaire (QLQ-C30).13 Each quality of life scale ranges from 0 to 100, with higher scores for global health status and functional scales reflecting better performance, but worse performance for symptom scales. Prespecified secondary end points not reported in this article included place and duration of care. We collected the drug names and doses of the steroids and analgesics used as supportive care therapies, and how these changed from baseline to during follow-up, and these were also not analyzed for this article.
Deterioration-free survival was the only post hoc end point, measured among patients who had ambulatory status grade 1 or 2 at baseline until they worsened to grade 3 or 4 during the trial or died, whichever occurred first. Patients whose ambulatory status did not deteriorate to grade 3 or 4 and did not die were censored at the date last seen alive.
Statistical Analysis
Sample Size
The primary trial objective was to show that ambulatory response rate using a single 8-Gy fraction of radiotherapy was noninferior to a total of 20 Gy of radiotherapy over 5 consecutive days (1 fraction per day) at 8 weeks. Assuming an ambulatory response rate (grade 1 or 2) of 75% of participants in both groups and a noninferiority margin of −11% (defined by consensus among the investigators, approved by the grant funder and the funder’s external reviewers, and similar to or less than noninferiority margins used in other trials),14,15,16 the trial required 386 patients (193 per group) assessable at 8 weeks with 80% power and 1-sided 5% statistical significance. The sample size was inflated to 580 allowing for 33% of participants to die before 8 weeks and later increased to 700 by the independent data monitoring committee because of a higher than anticipated death rate. Investigators remained blinded to the outcomes throughout the study.
Data Analysis
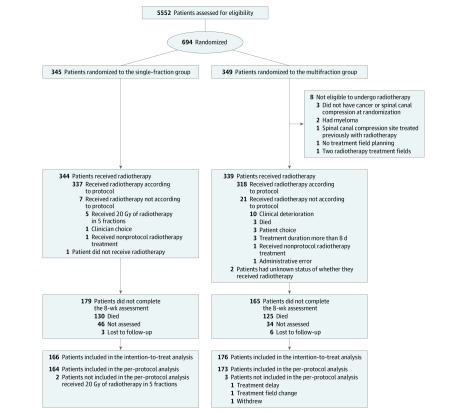
The primary analysis was based on eligible patients who received their randomly assigned treatment and were assessed at 8 weeks. The 8-week ambulatory response rate was compared between groups using the difference in proportions test. A post hoc per-protocol analysis of the primary outcome was done including only patients who received and completed radiotherapy as randomized (Figure 1). A post hoc analysis (logistic regression) of the primary outcome involved adjustment by the randomization factors (baseline ambulatory status, primary tumor, and extent of metastases). Logistic regression was also used to evaluate whether the effect of treatment at 8 weeks varied across subgroups with interaction tests. In this analysis, only baseline ambulatory status, primary tumor type, and extent of metastases were prespecified. Ambulatory response was examined among patients who were alive beyond 48 weeks (long-term survivors) in a post hoc analysis.
Figure 1. Flow of Participants in a Study of the Effect of Single-Fraction vs Multifraction Radiotherapy on Ambulatory Status Among Patients With Spinal Canal Compression From Metastatic Cancer (SCORAD Trial).
A total of 635 patients (93%) started radiotherapy on the day of randomization and all but 1 patient started radiotherapy within 24 hours of randomization.
To evaluate the effect of missing data on the primary analysis, several post hoc sensitivity analyses were performed by (1) extending the definition of the 8-week window from 49 to 62 days to 49 to 69 days by imputing data of patients with a missing assessment at week 8 but with assessments at 1, 4, and 12 weeks; (2) assuming missing data as positive or negative responses; and (3) performing multiple imputation using logistic regression.17,18 Details and assumptions used in these sensitivity analyses are outlined in eTable 4 in Supplement 3.
Other post hoc sensitivity analyses were completed. To evaluate the effect of center (one of the stratification factors), the ambulatory response risk difference CIs were derived from a logistic regression with specified standard errors allowing for intrahospital correlation (clustered sandwich estimator), and to evaluate the effect of individuals who died on the ambulatory response risk difference, we made various assumptions: all assumed to be nonresponders, all assumed to be responders, half were assumed to be responders, or the same response rate was assumed as observed in each group.
Post hoc analyses were performed for the primary end point, overall survival, and impaired bladder and bowel function to address concerns associated with the sensitivity of the bladder to radiation. Patients were classified in the following categories in terms of the location of their spinal cord compression: treatment exclusively directed at the spinal cord (C1 to T12), treatment exclusively directed at the cauda equina (L1 to S2), and treatment directed at both the spinal cord and the cauda equina (T6 to L5).
The analysis of time-to-event outcomes was done using the Kaplan-Meier method and Cox regression. These time-to-event analyses included time to loss of ambulation, time to recovery of ambulation, and overall survival. Stratified Cox regression (stratification factors were center, ambulatory status, primary tumor, and presence or absence of nonskeletal metastases) was carried out and the proportional hazards assumption was tested based on Schoenfeld residuals.
Bowel and bladder function were analyzed using logistic regression. Quality of life assessment scale results, including pain scale results, were analyzed using linear regression and mixed modeling. When SCORAD was designed, there were no recommended or clinically relevant noninferiority margins for the EORTC quality of life measures. A prespecified margin of 0.28 was crudely estimated as what would be a statistically significant difference (at a 1-sided 2.5% level of statistical significance) given a trial of 400 patients.
Post hoc analyses also were conducted to confirm the findings from a large trial of patients with any bone metastases who received single-fraction radiotherapy,19 in which individuals with ambulatory status grade 1 or 2 had improved quality of life compared with individuals with ambulatory status grade 3 or 4.
All comparative effect sizes are for single-fraction vs multifraction radiotherapy. The CIs are 1-sided for the risk difference for ambulatory response and are 2-sided for all other analyses. Noninferiority P values are 1-sided and all other P values are 2-sided. There was no formal statistical adjustment of P values for having multiple secondary outcomes, and therefore these results should be considered exploratory. Data analyses were performed using STATA version 15.1 (StataCorp).
Results
A total of 694 patients were randomized from 42 UK and 5 Australian sites from February 2008 to April 2016, of whom 686 were eligible for inclusion (Figure 1). Baseline characteristics in the total population were balanced (Table 1; eTable 1 in Supplement 3) (median [interquartile range] age, 70 [64-77] years; 503 (73%) men; 304 (44%) had prostate cancer). Thoracic spine only (462 of 686 patients [67%]) and lumbar spine only (137 of 686 patients [20%]) were the most common compression sites, and only 4% of compressions involved the cervical spine. Baseline characteristics among patients who were evaluated at 8 weeks were also well balanced (eTable 2 in Supplement 3). Of the 344 patients who were not evaluated at 8 weeks, 255 (74.1%) died before or during the 8-week assessment and the other 89 (25.9%) only had assessments before or after 8 weeks (eTable 3 in Supplement 3). The date of final follow-up was September 8, 2017.
Table 1. Baseline Characteristics of Participants in a Study of the Effect of Single-Fraction vs Multifraction Radiotherapy on Ambulatory Status Among Patients With Spinal Canal Compression From Metastatic Cancer.
| Characteristic | No. (%) | |
|---|---|---|
| Single-Fraction Radiotherapy Group (n = 345) | Multifraction Radiotherapy Group (n = 341) | |
| Age | ||
| Median (range), y | 70 (23-96) | 70 (33-95) |
| ≥75 y | 106 (31) | 119 (35) |
| Sex | ||
| Men | 255 (74) | 248 (73) |
| Women | 90 (26) | 93 (27) |
| Site of primary cancer | ||
| Prostate | 152 (44) | 152 (45) |
| Lung | 66 (19) | 66 (19) |
| Breast | 39 (11) | 40 (12) |
| Gastrointestinal | 35 (10) | 38 (11) |
| Kidney | 11 (3) | 12 (4) |
| Skin | 9 (3) | 6 (2) |
| Bladder | 7 (2) | 4 (1) |
| Other (ie, gynecologic, head and neck, sarcoma, unspecified) | 26 (8) | 23 (7) |
| Nonskeletal metastases | 159 (46) | 156 (46) |
| No. of spinal cord compression sites | ||
| Single | 303 (88) | 311 (91) |
| Multiple | 42 (12) | 30 (9) |
| Location of spinal metastases | ||
| Thoracic | 232 (67) | 230 (67) |
| Lumbar | 72 (21) | 65 (19) |
| Thoracic and lumbar | 17 (5) | 16 (5) |
| Sacrum (S1 and S2) | 9 (3) | 6 (2) |
| Cervical vertebrae | 7 (2) | 10 (3) |
| Cervical and thoracic | 5 (1) | 8 (2) |
| Lumbar and sacrum | 3 (1) | 4 (1) |
| Not reported | 0 | 2 (1) |
| WHO performance statusa | (n = 343) | (n = 337) |
| 0-1 (Best) | 97 (28) | 94 (28) |
| 2 | 88 (26) | 81 (24) |
| 3 | 114 (33) | 121 (36) |
| 4 (Worst) | 44 (13) | 41 (12) |
| Ambulatory status | ||
| Grade 1 (ambulatory without the use of walking aids) | 76 (22) | 77 (23) |
| Grade 2 (ambulatory with walking aids) | 152 (44) | 146 (43) |
| Grade 3 (unable to walk) | 91 (26) | 90 (26) |
| Grade 4 (absence or flicker of motor power in any muscle group) | 26 (8) | 28 (8) |
| Treatment at baseline | (n = 344) | (n = 341) |
| None | 156 (45) | 141 (41) |
| Hormone therapy within 4 weeks of randomization | 96 (28) | 97 (28) |
| Radiotherapy within 6 mo of randomization | 36 (10) | 39 (11) |
| Chemotherapy within 4 weeks of randomization | 20 (6) | 32 (9) |
| Combination of the above treatments | 36 (10) | 32 (9) |
WHO performance status of 0 indicates able to carry out all normal activity without restriction; 1, restricted in strenuous activity but ambulatory and able to carry out light work; 2, ambulatory and capable of all self-care but unable to carry out any work activities and are up and about for greater than 50% of waking hours; 3, symptomatic and in a chair or in bed for greater than 50% of the day but not bedridden; and 4, completely disabled, cannot carry out any self-care, and totally confined to bed or chair.
Primary End Point
The primary end point (8-week ambulatory response rate) was available for 342 of 686 (49.9%) patients, and was not significantly different between groups (Table 2). At week 8, ambulatory status grade 1 or 2 was achieved by 115 of 166 patients (69.3%) in the single-fraction group vs 128 of 176 (72.7%) in the multifraction group (difference, −3.5% [1-sided 95% CI, −11.5% to ∞]; P value for noninferiority = .06; Table 2 and Figure 2). In the per-protocol analysis, the 8-week ambulatory response rate was 114 of 164 patients (69.5%) in the single-fraction group and 127 of 173 (73.4%) in the multifraction group (difference, −3.9% [1-sided 95% CI, −12.0% to ∞]; P value for noninferiority = .07). Post hoc results adjusted for the randomization stratification factors are shown in eTable 4 in Supplement 3.
Table 2. Ambulatory Response Rate at 8 Weeks of Participants in a Study of the Effect of Single-Fraction vs Multifraction Radiotherapy on Ambulatory Status Among Patients With Spinal Canal Compression From Metastatic Cancer.
| Outcome | No. (%) | Absolute Difference (1-Sided 95% CI)a | 1-Sided P Value for Noninferiority | |
|---|---|---|---|---|
| Single-Fraction Group (n = 345) | Multifraction Group (n = 341) | |||
| 8-Week outcome known | (n = 166) | (n = 176) | ||
| Ambulatory status 1-2 | 115 (69.3) | 128 (72.7) | −3.45 (−11.5 to ∞) | .06 |
| No change in baseline status (grade 1-2)b | 103 (62.1) | 110 (62.5) | ||
| Improved from baseline (3-4 to 1-2) | 12 (7.2) | 18 (10.2) | ||
| No change in baseline status (3-4)b | 22 (13.3) | 26 (14.8) | ||
| Worsened from baseline (1-2 to 3-4) | 29 (17.5) | 22 (12.5) | ||
| 8-Week outcome unknownc | (n = 179) | (n = 165) | ||
| Died before week 8 | 130 | 125 | ||
| 8-Week assessment not availablec | 49 | 40 | ||
1-Sided 95% CI is reported because the noninferiority hypothesis is based on 1-sided α = .05. Single-fraction radiotherapy is not considered noninferior to multifraction radiotherapy if the lower bound of the 1-sided 95% CI is less than −11%.
Patients with either grade 1 or 2 at baseline who remain at grade 1 or 2 at 8 weeks (a patient whose status changed from 1 to 2 or vice versa) or patients with grade 3 to 4 who remain at 3 to 4.
See eTable 3 in Supplement 3 for more information.
Figure 2. Ambulatory Status of Participants in a Study of the Effect of Single-Fraction vs Multifraction Radiotherapy on Ambulatory Status Among Patients With Spinal Canal Compression From Metastatic Cancer.
If the lower boundary of any 1-sided 95% CI is lower than −11% (blue dotted line), single-fraction radiotherapy would not be considered noninferior to multifraction radiotherapy.
Prespecified Secondary Outcomes
The differences in ambulatory response rate between the single-fraction and multifraction groups were −0.4% (63.9% vs 64.3%; [1-sided 95% CI, −6.9% to ∞]; P value for noninferiority = .004) at 1 week, −0.7% (66.8% vs 67.6%; [1-sided 95% CI, −8.1 to ∞]; P value for noninferiority = .01) at 4 weeks, and 4.1% (71.8% vs 67.7%; [1-sided 95% CI, −4.6 to ∞]; P value for noninferiority = .002) at 12 weeks (Figure 2 and eFigure 1 in Supplement 3).
The difference in 8-week ambulatory response rate did not vary across subgroups, including patients who had good or poor WHO performance status at baseline (all interaction P values were not statistically significant P > .05) (eFigure 2 in Supplement 3).
Among patients with ambulatory status 1 or 2 at baseline, there was no statistically significant difference in the time to loss of ambulation between the single-fraction and multifraction group (HR, 1.22 [95% CI, 0.88-1.71]; P = .24; eFigure 3 in Supplement 3). The 8-week loss of ambulation rate was 28% (95% CI, 22%-35%) for the single-fraction group and 23% (95% CI, 17%-29%) for the multifraction group. Among patients with ambulatory status 3 or 4 at baseline, there was also no evidence of a statistically significant between-group difference for time to recovery of ambulation (HR, 1.15 [95% CI, 0.71-1.85]; P = .58; eFigure 4 in Supplement 3). The 8-week recovery of ambulation rate was 41% (95% CI, 31%-53%) in the single-fraction group and 36% (95% CI, 26%-49%) in the multifraction group.
Rates of any additional treatment for cancer within 12 months were not significantly different between the single-fraction and multifraction group (104 of 345 patients [30.1%] in the single-fraction group vs 110 of 341 [32.3%] in the multifraction group; risk difference, −2.1% [95% CI, −9.0% to 4.8%]; P = .55). The additional treatments included chemotherapy in 41 of 345 patients (11.9%) in the single-fraction group vs 47 of 341 (13.8%) in the multifraction group (difference, −1.9% [95% CI, −6.9% to 3.1%]; P = .46), hormone therapy in 44 of 345 patients (12.8%) in the single-fraction group vs 45 of 341 (13.2%) in the multifraction group (difference, −0.4% [95% CI, −5.5% to 4.6%]; P = .86), radiotherapy in 43 of 345 patients (12.5%) in the single-fraction group vs 34 of 341 (10.0%) in the multifraction group (difference, 2.5% [95% CI, −2.2% to 7.2%]; P = .30), and surgical procedure in 7 of 345 patients (2.0%) in the single-fraction group vs 4 of 341 (1.2%) in the multifraction group (difference, 0.9% [95% CI, −1.0% to 2.7%]; P = .37).
The date when supportive care therapies started was collected for 604 patients. The rate of postrandomization supportive care therapies was not significantly different between the single-fraction and multifraction group (210 of 304 patients [69.1%] vs 225 of 300 [75%]; risk difference, −5.9% [95% CI, −13.1% to 1.2%]; P = .11). Supportive care therapies included analgesics in 146 of 304 patients (48.0%) in the single-fraction group vs 153 of 300 (51%) in the multifraction group (difference, −3.0% [95% CI, −10.9% to 5.0%]; P = .47), anti-emetics in 52 of 304 patients (17.1%) in the single-fraction group vs 49 of 300 (16.3%) in the multifraction group (difference, 0.8% [95% CI, −5.2% to 6.7%]; P = .80); corticosteroids in 110 of 304 patients (36.2%) in the single-fraction group vs 116 of 300 (38.7%) in the multifraction group (difference, −2.5% [95% CI, −10.2% to 5.2%]; P = .53), physiotherapy in 76 of 304 patients (25%) in the single-fraction group vs 97 of 300 (32.3%) in the multifraction group (difference, −7.3% [95% CI, −14.5% to −0.1%]; P = .046), and bisphosphonates in 14 of 304 patients (4.6%) in the single-fraction group vs 11 of 300 (3.7%) in the multifraction group (difference, 0.9% [95% CI, −2.2% to 4.1%]; P = .56).
At week 8, the standardized mean differences in the EORTC QLQ-C30 domains (single-fraction scores minus multifraction scores) adjusted for the baseline values were −0.13 ([1-sided 97.5% CI, −0.38 to ∞]; P value for noninferiority = .12) for global health, −0.12 ([1-sided 97.5% CI, −0.35 to ∞]; P value for noninferiority = .09) for physical functioning, and −0.18 ([1-sided 97.5% CI, −0.41 to ∞]; P value for noninferiority = .19) for emotional functioning. Noninferiority was not met using the prespecified margin of −0.28 for the lower limit. Pain improved from baseline in both groups after starting radiotherapy. Pain scores were not significantly different between the single-fraction and multifraction groups at each time point (eFigure 5 in Supplement 3), with a standardized mean difference of 0.12 at week 8 ([1-sided 97.5% CI, ∞ to 0.38]; P value for noninferiority = .11), but noninferiority was not met because the upper limit exceeded the prespecified margin of 0.28.
The median (interquartile range) follow-up was 13.3 (12-50) weeks and the median overall survival was 13.1 weeks, with a total of 529 deaths at the end of follow-up on September 8, 2017 (84.3% were cancer-related deaths; eTable 5 in Supplement 3). The median (interquartile range) survival time was 12.4 (4.6-41.0) weeks in the single-fraction group vs 13.6 (5.9-40.9) weeks in the multifraction group.
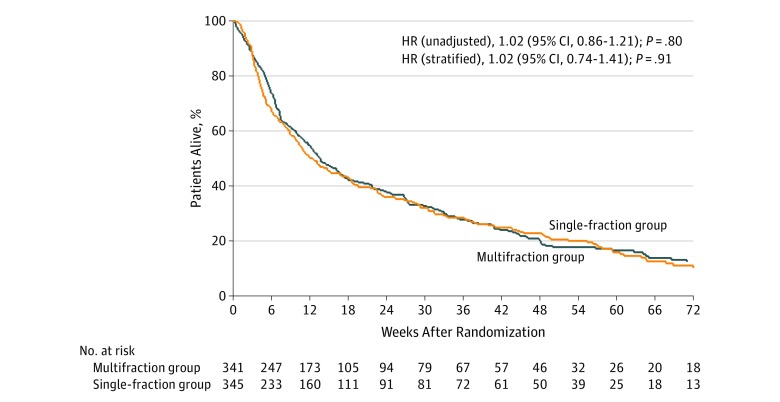
The survival rate was 50% (95% CI, 45%-55%) at 12 weeks and 21% (95% CI, 16%-26%) at 12 months for the single fraction group and 55% (95% CI, 49%-60%) at 12 weeks and 18% (95% CI, 13%-23%) at 12 months for the multifraction group. There was no statistically significant difference in survival between the groups (stratified HR, 1.02 [95% CI, 0.74-1.41]; P = .91; Figure 3). The proportionality hazards assumption was met (P = .35). Also, overall survival was not significantly different across subgroups analyzed (eFigure 6 in Supplement 3).
Figure 3. Overall Survival of Participants in a Study of the Effect of Single-Fraction vs Multifraction Radiotherapy on Ambulatory Status Among Patients With Spinal Canal Compression From Metastatic Cancer.
The median (interquartile range [IQR]) survival time was 12.4 (4.6 to 41.0) weeks in the single-fraction group and 13.6 (5.9-40.9) weeks in the multifraction group. The median (IQR) observation time was 13.7 (12.0-52.7) weeks in the single-fraction group and 12.9 (12 to 48.7) weeks in the multifraction group. The hazard ratio (HR) was stratified on baseline ambulatory status, primary tumor, extension of metastases, and hospital. Shared frailty Cox model HR with hospital as a random effect, 1.02 ([95% CI, 0.86-1.21]; P = .85).
Adverse Events
The percentage of patients with grade 3 or 4 adverse events was 20.6% in the single-fraction group vs 20.5% in the multifraction group, and the percentages were similar between the groups for each of the adverse events (eTable 6 in Supplement 3). The rates of grade 1 or 2 radiation reactions were 11.6% in the single-fraction group vs 19.4% in the multifraction group, and fatigue was reported by 48.7% of patients in the single-fraction group vs 55.4% in the multifraction group.
Impaired bladder function occurred in 42% of patients in the single-fraction group and 34% in the multifraction group (cumulative risk difference, 7.3% [95% CI, −14.8% to 0.2%]; eTable 7 in Supplement 3). At 8 weeks, 47 of 151 patients (31.1%) in the single-fraction group vs 34 of 166 (20.0%) in the multifraction group experienced abnormal bladder function (risk difference, 10.6% [95% CI, 1.0%-20.2%]; unadjusted odds ratio [OR], 1.75 [95% CI, 1.05-2.92]; P = .03) (adjusted OR, 1.78 [95% CI, 0.93-3.39]; P = .08; adjusted for bladder function at baseline, sex, age, baseline ambulatory status, primary tumor, number of spinal canal compression sites, and the extent of metastases at baseline). Impaired bowel function rates were not significantly different between the groups at any time point, and at week 8 the rates were 59 of 151 patients (39%) in the single-fraction group and 61 of 166 (37%) in the multifraction group, with a risk difference of 2.3% (95% CI, −8.4 to 13.0) and unadjusted OR of 1.10 ([95% CI, 0.70-1.74]; P = .67).
Post Hoc Analyses
Across several sensitivity analyses for the primary end point, including multiple imputation, the point estimate for the ambulatory response rate was not significantly different. The differences ranged from −1.50 to −5.80 in the intention-to-treat population and −2.10 to −5.60 in the per-protocol population (eTable 4 in Supplement 3). The risk difference was −3.45 (1-sided 95% CI, −10.3% to ∞) when estimated from logistic regression with standard errors allowing for intrahospital correlation (eTable 4 in Supplement 3).
The primary analysis excluded patients who died before 8 weeks. However, assuming those patients survived to 8 weeks and all were nonresponders, then the response rate was 39% in the single-fraction group and 43% in the multifraction group (risk difference, −3.7% [1-sided 95% CI, −10.3 to ∞]; P value for noninferiority = .03). Assuming that 50% of the patients who died could have been responders had they survived, the difference was −2.3% ([1-sided 95% CI, −8.9% to ∞]; P value for noninferiority = .01), and assuming that the patients who died would have had the same response rate as observed in each group, the difference was −3.5% ([1-sided 95% CI, −9.6% to ∞]; P value for noninferiority = .02).
Deterioration-free survival was not statistically significantly different between the groups (HR, 0.99 [95% CI, 0.80-1.22]; P = .93; eFigure 7 in Supplement 3).
Among the subgroup of patients who were alive after 48 weeks (n = 77), the baseline characteristics were not significantly different between the groups (eTable 8 in Supplement 3). The 8-week ambulatory response rates were 94.9% in the single-fraction group vs 89.5% in the multifraction group (risk difference, 5.4% [1-sided 95% CI, −6.6 to ∞]). After adjusting for baseline characteristics (ambulatory status, the extent of metastases, and primary tumor type), the risk difference was 0.7% (1-sided 95% CI, −10.0 to ∞).
A total of 232 patients (108 in the single-fraction group and 124 in the multifraction group) received treatment exclusively to the spinal cord, defined as C1 to T12, and 88 patients (47 in the single-fraction group and 41 in the multifraction group) received treatment to the cauda equina, defined as L1 to S2. Twenty patients (11 in the single-fraction group and 9 in the multifraction group) received treatment to both the spinal cord and the cauda equina (T6 to L5). There was no statistically significant between-group difference in ambulatory response rate in the treatment location subgroups, although observed ambulatory response rates for patients whose treatment was directed at the cauda equina were 76.6% in the single-fraction group and 85.4% in the multifraction group (difference, −8.8 [95% CI, −25.0% to 7.5%]; P = .30; P value for interaction = 0.65; eTable 9 in Supplement 3). The risk of bladder symptoms in patients receiving radiotherapy to the cauda equina was 34% in the single-dose group vs 10% in the multifraction group (OR, 4.53 [95% CI, 1.4-15.1); P = .014; P value for interaction = 0.15). No significant difference was found in overall median survival between sites of treatment (13 weeks for C1-T12, 16 weeks for L1-L5, and 13 weeks for T6-L5) or between single-fraction and multifraction groups in each category of spinal canal compression site (P value for interaction = .68).
Patients who were ambulatory responders at 4 or 8 weeks had better quality of life than nonresponders (eTable 10 in Supplement 3).19 For the single-fraction group, the mean difference in scores at 4 weeks, adjusted for baseline scores, between ambulant versus nonambulant patients was 15.2 (95% CI, 7.5-22.9) for global health, 29.6 (95% CI, 20.9-38.4) for physical functioning, 25.6 (95% CI, 15.2-36.0) for role functioning, and 16.0 (95% CI, 5.3-26.7) for social functioning (all P values ≤.004). Similar differences in scores were seen in patients in the multifraction radiotherapy group.
Discussion
In this international noninferiority trial involving patients with metastatic spinal canal compression, treatment with single-fraction radiotherapy, compared with multifraction radiotherapy, did not meet the criterion for noninferiority for achieving ambulatory response status grade 1 or 2 at 8 weeks. The lower bound of the CI (−11.5%) overlapped the noninferiority margin of −11%.
However, for all other time points, the CI limits were within the noninferiority margin, and the observed risk differences between single-fraction and multifraction radiotherapy groups in ambulatory status were small and unlikely to be of clinical importance.
This trial evaluated 15 prespecified secondary end points: ambulatory status at 1, 4, and 12 weeks; loss of ambulation; ambulatory recovery; additional treatment; supportive care; quality of life (global, physical, emotional, and pain dimensions); grade 3 or 4 adverse events; bladder and bowel functioning; and overall survival. None of these outcomes were significantly different between treatment groups.
The EORTC QLQ-C30 outcomes also did not meet the prespecified noninferiority margins (0.28), but this margin had no scientific basis when the trial was designed, and it lacked external validity. However, the EORTC later published boundaries of what values constitute a small clinical standardized mean difference (−0.4 for global health, −0.6 for physical functioning, and 0.5 for pain), which can now be used as independently derived noninferiority margins.20
Only 2 other randomized studies have compared single-fraction radiotherapy with multifraction radiotherapy specifically for managing spinal canal compression, and both were small trials. One single-center 3-group randomized trial from Egypt with 285 patients compared single-fraction radiotherapy with 10 or 20 fractions of radiotherapy, but was not designed for noninferiority.8 The other study was designed for noninferiority and compared single-fraction radiotherapy with 5 fractions of radiotherapy, but failed to reach its target accrual.14,15,21 Two trials have shown noninferiority of short-course radiotherapy; 1 trial compared 8 Gy of radiotherapy in 1 fraction with nonstandard 16 Gy of radiotherapy in 2 fractions16 and the other compared 16 Gy in 2 fractions vs 30 Gy in 8 fractions with a split-course schedule.21
The median survival time of 3 months in the current trial is similar to that observed in other studies, specifically studies examining spinal canal compression,9,10,13,16,21 in contrast to the median survival time for individuals with any bone metastases of 7 to 9 months. The findings of the current trial are consistent with observational studies of spinal canal compression7,14,15,16,21 and the ICORG-05-03 trial,14,15 in which 79% of patients who received single-fraction radiotherapy achieved mobility compared with 68% who received multifraction radiotherapy, but with only 38 patients per group. Among longer-surviving patients, mobility was not significantly different between patients who received single-fraction or multifraction radiotherapy, which is consistent with studies of any bone metastases22,23 and in contrast to the proposal that such patients should receive multiple fractions of radiotherapy.24 However, this subgroup was defined using a clinical outcome occurring after randomization, so the results should be interpreted with care.
Use of single-fraction radiotherapy, specifically for patients with spinal canal compression, was low in 2010 (≤18% of clinicians reported using it in an international survey; 8%-11% of US and Canadian clinicians and 17% of European clinicians), which is unlikely to be much higher now.25 A 2013 US study of Surveillance, Epidemiology, and End Results (SEER) Program data and Medicare claims showed a much lower treatment cost per patient for single-fraction radiotherapy ($1873) than for multifraction radiotherapy ($4967) for management of bone metastases from prostate cancer.26
Single-fraction radiotherapy has benefits both in terms of patient convenience and reduced costs. In a patient population that has a median survival time of less than 6 months, the opportunity to reduce treatment burden is particularly relevant for patients who have to make multiple hospital visits and pay for travel or hotel costs. Radiotherapy access is often limited, so reducing the number of fractions allows better allocation of resources.27,28,29 Patients and their caregivers sometimes have to travel significant distances to their nearest radiotherapy center, and travel can be a barrier to radiotherapy adherence.30,31
A greater percentage of patients in this study had bladder problems in the single-fraction group than the multifraction group, but this largely occurred when radiotherapy was given for cauda equina compression, which is likely due to its close proximity to the bladder (bladder and bowel function are regulated by the sacral nerves within the cauda equina). The test for interaction between treatment and location of spinal cord compression and their effect on bladder impairment was not statistically significant, but the trial lacked statistical power for subgroup analyses. Taking into account that patients with metastases in the distal spine or cauda equina receiving single-fraction vs multifraction radiation may have higher rates of bladder toxicity, 5 fractions may be preferred for this subgroup.
Limitations
This study has several limitations. First, ambulatory status was assessed either in the clinic or by telephone when patients were unable or unwilling to attend in-person visits. This approach was intended to minimize missing data and categorized mobility based on a 4-point scale. However, no information about which mode was used to ascertain ambulatory status was recorded and it is conceivable that reporting bias influenced assessment of the primary outcome. Second, a substantial percentage of patients died before the 8-week point, with only half of the randomized patients available for the primary end point assessment at 8 weeks, despite an expected survival of greater than 8 weeks being an inclusion criterion. This higher than expected death rate may have led to a slight reduction in study power. However, this early death rate was similar to the rate in other spinal canal compression trials.16,21 Furthermore, the observed ambulatory response rate (73%) matched the expected rate for the target patient population (75%), so trial participants included in the analysis at 8 weeks are unlikely to be a biased subgroup with regard to the primary end point. Although the death rate was high, there was no significant difference in the secondary outcomes of ambulatory status at either 1 or 4 weeks after randomization, when the majority of patients were still alive. Third, only 12% of patients had breast cancer, suggesting some potential selection bias, with younger patients who had better prognosis being more likely referred for surgery23 or longer fractionation schedules instead of this trial; hence, the generalizability of these findings is limited for these patients. Subgroup analysis by tumor type showed no clear evidence that the treatment effect differed significantly between tumor type, although these analyses were not sufficiently powered. No other overt selection criteria were apparent, with 66% of the population being physically mobile at presentation and WHO performance status 1 or 2. Fourth, the assessments of bladder and bowel function were dichotomized as “normal” and “abnormal,” instead of having a finer grading to indicate severity, and they were not blinded. Fifth, the multifraction group chosen reflects standard practice in the United Kingdom and several other countries, although in the United States and some European countries 30 Gy of radiotherapy in 10 fractions is more often used.4 However, a clinical trial that compared 20 Gy of radiotherapy in 5 fractions with 30 Gy in 10 fractions found no significant difference between them in terms of overall motor response at 1, 3, and 6 months and in overall survivall.32,33
Conclusions
Among patients with metastatic solid tumors causing spinal canal compression, treatment with a single radiotherapy fraction, compared with multifraction radiotherapy delivered over 5 days, did not meet the criterion for noninferiority for the primary outcome of being ambulatory at 8 weeks. However, the extent to which the lower bound of the CI overlapped with the noninferiority margin should be taken into account when interpreting the clinical importance of these findings.
Trial protocol
Statistical analysis plan
eResults
Data sharing statement
References
- 1.Metastatic spinal cord compression in adults: risk assessment, diagnosis and management. Manchester, UK: National Institute for Health and Clinical Excellence ; 2008. https://www.nice.org.uk/guidance/cg75/resources/metastatic-spinal-cord-compression-in-adults-risk-assessment-diagnosis-and-management-pdf-975630102469. Published November 26, 2008. Accessed August 8, 2019. [PubMed]
- 2.Schmidt MH, Klimo P Jr, Vrionis FD. Metastatic spinal cord compression. J Natl Compr Canc Netw. 2005;3(5):711-719. doi: 10.6004/jnccn.2005.0041 [DOI] [PubMed] [Google Scholar]
- 3.Loblaw DA, Laperriere NJ. Emergency treatment of malignant extradural spinal cord compression: an evidence-based guideline. J Clin Oncol. 1998;16(4):1613-1624. doi: 10.1200/JCO.1998.16.4.1613 [DOI] [PubMed] [Google Scholar]
- 4.Loblaw DA, Perry J, Chambers A, Laperriere NJ. Systematic review of the diagnosis and management of malignant extradural spinal cord compression: the Cancer Care Ontario Practice Guidelines Initiative’s Neuro-Oncology Disease Site Group. J Clin Oncol. 2005;23(9):2028-2037. doi: 10.1200/JCO.2005.00.067 [DOI] [PubMed] [Google Scholar]
- 5.Chow E, Harris K, Fan G, Tsao M, Sze WM. Palliative radiotherapy trials for bone metastases: a systematic review. J Clin Oncol. 2007;25(11):1423-1436. doi: 10.1200/JCO.2006.09.5281 [DOI] [PubMed] [Google Scholar]
- 6.Chow E, Zeng L, Salvo N, Dennis K, Tsao M, Lutz S. Update on the systematic review of palliative radiotherapy trials for bone metastases. Clin Oncol (R Coll Radiol). 2012;24(2):112-124. doi: 10.1016/j.clon.2011.11.004 [DOI] [PubMed] [Google Scholar]
- 7.Qu S, Meng HL, Liang ZG, et al. Comparison of short-course radiotherapy versus long-course radiotherapy for treatment of metastatic spinal cord compression: a systematic review and meta-analysis. Medicine (Baltimore). 2015;94(43):e1843. doi: 10.1097/MD.0000000000001843 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Abu-Hegazy M, Wahba HA. Single versus multi-fraction radiation treatment for metastatic spinal cord compression: functional outcome study. Chinese-German J Clin Oncol. 2011;10:535-540. doi: 10.1007/s10330-011-0832-5 [DOI] [Google Scholar]
- 9.National Institute for Health and Care Excellence Metastatic Spinal Cord Compression in Adults: Risk Assessment, Diagnosis, and Management. Manchester, UK: National Collaborating Centre for Cancer; 2008. https://www.nice.org.uk/guidance/cg75/resources/metastatic-spinal-cord-compression-in-adults-risk-assessment-diagnosis-and-management-pdf-975630102469. [Google Scholar]
- 10.Lutz S, Balboni T, Jones J, et al. Palliative radiation therapy for bone metastases: update of an ASTRO evidence-based guideline. Pract Radiat Oncol. 2017;7(1):4-12. doi: 10.1016/j.prro.2016.08.001 [DOI] [PubMed] [Google Scholar]
- 11. National Comprehensive Cancer Network (NCCN) guidelines in oncology. Adult cancer pain. Version 1.2018. January 2018.
- 12.Aids to the Examination of the Peripheral Nervous System: Memorandum No. 45. London, UK: Medical Research Council ; 1976. https://mrc.ukri.org/documents/pdf/aids-to-the-examination-of-the-peripheral-nervous-system-mrc-memorandum-no-45-superseding-war-memorandum-no-7/. Accessed August 8, 2019.
- 13.Aaronson NK, Ahmedzai S, Bergman B, et al. The European Organization for Research and Treatment of Cancer QLQ-C30: a quality-of-life instrument for use in international clinical trials in oncology. J Natl Cancer Inst. 1993;85(5):365-376. doi: 10.1093/jnci/85.5.365 [DOI] [PubMed] [Google Scholar]
- 14.Lee KA, Dunne M, Small C, et al. (ICORG 05-03): prospective randomized non-inferiority phase III trial comparing two radiation schedules in malignant spinal cord compression (not proceeding with surgical decompression); the quality of life analysis. Acta Oncol. 2018;57(7):965-972. doi: 10.1080/0284186X.2018.1433320 [DOI] [PubMed] [Google Scholar]
- 15.Thirion P, O’Sullivan L, Clayton-Lea A, et al. ICORG 05-03: prospective randomized non-inferiority phase 3 trial comparing two radiation schedules in malignant spinal cord compression not proceeding with surgical decompression. Int J Radiat Oncol Biol Phys. 2014;90(5):1263-1264. doi: 10.1016/j.ijrobp.2014.10.036 [DOI] [PubMed] [Google Scholar]
- 16.Maranzano E, Trippa F, Casale M, et al. 8Gy single-dose radiotherapy is effective in metastatic spinal cord compression: results of a phase III randomized multicentre Italian trial. Radiother Oncol. 2009;93(2):174-179. doi: 10.1016/j.radonc.2009.05.012 [DOI] [PubMed] [Google Scholar]
- 17.Raghunathan TE, Lepkowski JM, Van Hoewyk J, Solenberger P. A multivariate technique for multiply imputing missing values using a sequence of regression models. Surv Methodol. 2001;27:85-95. [Google Scholar]
- 18.StataCorp Stata 15 Multiple-imputation Manual. College Station, TX: Stata Press; 2017. [Google Scholar]
- 19.McDonald R, Ding K, Brundage M, et al. Effect of radiotherapy on painful bone metastases: a secondary analysis of the NCIC Clinical Trials Group Symptom Control Trial SC.23. JAMA Oncol. 2017;3(7):953-959. doi: 10.1001/jamaoncol.2016.6770 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cocks K, King MT, Velikova G, Martyn St-James M, Fayers PM, Brown JM. Evidence-based guidelines for determination of sample size and interpretation of the European Organisation for the Research and Treatment of Cancer Quality of Life Questionnaire Core 30. J Clin Oncol. 2011;29(1):89-96. doi: 10.1200/JCO.2010.28.0107 [DOI] [PubMed] [Google Scholar]
- 21.Maranzano E, Bellavita R, Rossi R, et al. Short-course versus split-course radiotherapy in metastatic spinal cord compression: results of a phase III, randomized, multicenter trial. J Clin Oncol. 2005;23(15):3358-3365. doi: 10.1200/JCO.2005.08.193 [DOI] [PubMed] [Google Scholar]
- 22.van der Linden YM, Steenland E, van Houwelingen HC, et al. Patients with a favourable prognosis are equally palliated with single and multiple fraction radiotherapy: results on survival in the Dutch bone metastasis study. Radiother Oncol. 2006;78(3):245-253. doi: 10.1016/j.radonc.2006.02.007 [DOI] [PubMed] [Google Scholar]
- 23.Hartsell WF, Scott CB, Bruner DW, et al. Randomized trial of short- versus long-course radiotherapy for palliation of painful bone metastases. J Natl Cancer Inst. 2005;97(1):798-804. doi: 10.1093/jnci/dji139 [DOI] [PubMed] [Google Scholar]
- 24.Loblaw DA, Mitera G, Ford M, Laperriere NJA. A 2011 updated systematic review and clinical practice guideline for the management of malignant extradural spinal cord compression. Int J Radiat Oncol Biol Phys. 2012;84(2):312-317. doi: 10.1016/j.ijrobp.2012.01.014 [DOI] [PubMed] [Google Scholar]
- 25.Ryu S, Maranzano E, Schild SE, et al. International survey of the treatment of metastatic spinal cord compression. J Radiosurg SBRT. 2015;3(3):237-245. [PMC free article] [PubMed] [Google Scholar]
- 26.Bekelman JE, Epstein AJ, Emanuel EJ. Single- vs multiple-fraction radiotherapy for bone metastases from prostate cancer. JAMA. 2013;310(14):1501-1502. doi: 10.1001/jama.2013.277081 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Borras JM, Dunscombe P, Barton M, et al. Assessing the gap between evidence based indications for radiotherapy and actual practice in European countries. Value Health. 2015;18(7):A481-A482. doi: 10.1016/j.jval.2015.09.1311 [DOI] [Google Scholar]
- 28.Lievens Y, Defourny N, Coffey M, et al. ; HERO Consortium . Radiotherapy staffing in the European countries: final results from the ESTRO-HERO survey. Radiother Oncol. 2014;112(2):178-186. doi: 10.1016/j.radonc.2014.08.034 [DOI] [PubMed] [Google Scholar]
- 29.Borras JM, Lievens Y, Dunscombe P, et al. The optimal utilization proportion of external beam radiotherapy in European countries: an ESTRO-HERO analysis. Radiother Oncol. 2015;116(1):38-44. doi: 10.1016/j.radonc.2015.04.018 [DOI] [PubMed] [Google Scholar]
- 30.Oxford Cancer Intelligence Unit National Cancer Intelligence Network Travel times and distances to radiotherapy centres for head and neck cancer patients in England (2006-2008). http://www.ncin.org.uk/cancer_type_and_topic_specific_work/cancer_type_specific_work/head_and_neck_cancers/head_and_neck_cancer_hub/resources. Published 2012. Accessed November 9, 2018.
- 31.Lin CC, Bruinooge SS, Kirkwood MK, et al. Association between geographic access to cancer care and receipt of radiation therapy for rectal cancer. Int J Radiat Oncol Biol Phys. 2016;94(4):719-728. doi: 10.1016/j.ijrobp.2015.12.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Rades D, Šegedin B, Conde-Moreno AJ, et al. Radiotherapy With 4 Gy × 5 Versus 3 Gy × 10 for metastatic epidural spinal cord compression: final results of the SCORE-2 Trial (ARO 2009/01). J Clin Oncol. 2016;34(6):597-602. doi: 10.1200/JCO.2015.64.0862 [DOI] [PubMed] [Google Scholar]
- 33.Rades D, Conde-Moreno AJ, Cacicedo J, et al. Comparison of two radiotherapy regimens for metastatic spinal cord compression: subgroup analyses from a randomized trial. Anticancer Res. 2018;38(2):1009-1015. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Trial protocol
Statistical analysis plan
eResults
Data sharing statement