This cohort study assesses the association of continuity of hospitalist schedules with outcomes for hospitalized patients.
Key Points
Question
Are hospitalist schedules associated with care outcomes for patients?
Findings
In this cohort study of 3 years of Medicare data from 229 hospitals in Texas, covering 114 777 medical admissions of patients with a 3-day to 6-day length of stay, patients receiving care from hospitalists whose schedules permitted continuity of care had significantly better outcomes, including lower 30-day mortality after discharge, lower readmissions, higher rates of discharge to the home, and $223 lower 30-day postdischarge costs.
Meaning
Hospitalist schedules promoting inpatient continuity of care may be associated with better outcomes of hospitalization.
Abstract
Importance
The working schedules of hospitalists vary widely. Discontinuous schedules, such as 24 hours on and 48 hours off, result in several hospitalists providing care during a patient’s hospital stay. Poor continuity of care during hospitalization may be associated with poor patient outcomes.
Objective
To determine whether admitted patients receiving care from hospitalists with more discontinuous schedules experience worse outcomes.
Design, Setting, and Participants
This retrospective cohort study used conditional models to assess Medicare claims data for 114 777 medical admissions of patients with a 3-day to 6-day length of stay from January 1, 2014, through November 30, 2016, who received all general medical care from hospitalists in 229 hospitals in Texas. Data were analyzed from November 2018 to June 2019.
Exposures
For each admission, the weighted mean of schedule continuity for the treating hospitalists, assessed as the percentage of all their working days in that year that were part of a block of 7 or more consecutive working days, was calculated.
Main Outcomes and Measures
The primary outcome was patient mortality in the 30 days after discharge. Secondary outcomes were readmission rates and Medicare costs in the 30 days after discharge, and discharge destination.
Results
Of the 114 777 patient admissions, the mean (SD) age was 79.9 (8.3) years, and 70 047 (61.0%) were women. For admissions in the lowest quartile for continuity of hospitalist schedules, the hospitalists providing care worked 0% to 30% of their total working days as part of a block of 7 or more consecutive days vs 67% to 100% for hospitalists providing care for patients in the highest quartile for continuity. Patient characteristics were not associated with the continuity of working schedules for the hospitalist(s) providing care. In conditional logistic regression models, admitted patients cared for by hospitalists in the highest quartile of schedule continuity (vs the lowest quartile) had lower 30-day mortality after discharge (adjusted odds ratio [aOR], 0.88; 95% CI, 0.81-0.95), lower readmission rates (aOR, 0.94; 95% CI, 0.90-0.99), higher rates of discharge to the home (aOR, 1.08; 95% CI, 1.03-1.13), and lower 30-day postdischarge costs (−$223; 95% CI, −$441 to −$7). The results were similar across a range of different methods for defining continuity of hospitalist schedules and selecting the cohort.
Conclusions and Relevance
Hospitalist schedules vary widely. Admitted patients receiving care from hospitalists with schedules that promote inpatient continuity of care may experience better outcomes of hospitalization.
Introduction
Continuity of care is recognized as an important aspect of medical care and is associated with fewer hospitalizations, higher quality of life, and other notable health outcomes.1,2,3,4,5,6 A number of studies have found an association of increasing discontinuities of care in different settings with worse patient outcomes.5,6,7,8 This is the case for both ambulatory care and outpatient-to-inpatient transitions. For example, continuity of care across the community-to-hospital trajectory has decreased with the growth in the use of hospitalists and is associated with lower community discharge rates, higher costs, higher readmission rates, and increased mortality after discharge.4,5,6,7
One less-studied aspect of continuity of care involves the medical care provided to hospitalized patients, in particular, inpatient care provided by hospitalists.8,9 Work schedules for hospitalists appear to differ greatly among different hospitals.9,10,11,12,13 We recently used Medicare claims data to characterize hospitalist work schedules.10 We found, for example, that 665 of 2334 (28%) Texas hospitalists had 0 working days in a year that were part of a 7-day or longer block of consecutive working days, whereas 591 of 2334 (25%) hospitalists had more than 54% of their working days as part of 7-day or longer block.10 As expected, hospitalist schedules were strongly associated with the continuity of care experienced by hospitalized patients. For example, for routine medical admissions with a 3-day length of stay, patients receiving care from hospitalists in the highest quartile in terms of consecutive working days in that year were 5.5-fold more likely to receive care from the same hospitalist throughout their hospitalization.10 However, little is known about the outcomes of discontinuities in the care of hospitalized patients.8
We studied the association of hospitalists’ schedules, from those with more consecutive working days to those with more intermittent working days, with mortality and readmissions in the 30 days after discharge, the rate of discharge to the community, and the 30-day postdischarge costs of Medicare enrollees hospitalized with a medical diagnosis. We hypothesized that provision of care from hospitalists with fewer consecutive working days would be associated with worse patient outcomes after discharge.
Methods
Cohorts
We used 100% Texas Medicare data from January 1, 2014, through November 30, 2016, for all analyses. Three sets of cohorts were analyzed: one to identify hospitalist physicians (steps 1-4 in eFigure 1 in the Supplement), another to characterize their work schedules (steps 5-7 in eFigure 1 in the Supplement), and a third to examine the associations of hospitalist schedules with outcomes (eFigure 2 in the Supplement). Each cohort was created separately for each year. The cohort to identify hospitalists comprised all fee-for-service Medicare enrollees with both Parts A and B for the entire year. The cohort to characterize work schedules comprised all inpatient evaluation and management (E&M) claims from all hospitalists in each year. The cohort used in examining outcomes of admissions as a function of the continuity of hospitalist schedules included all medical admissions with a 3-day to 6-day length of stay and a maximum of 1 E&M charge each day from a hospitalist, and without an intensive care unit (ICU) stay and in which all general medical care was provided by hospitalists. We excluded admissions with ICU stays and those with 2 or more E&M charges from hospitalists in a day because both are associated with greater illness severity, which might lead to care from different hospitalists (eg, an ICU physician or an on-call hospitalist at night).
Continuity of Hospitalist Schedules
The distributions of consecutive working days for the hospitalists were highly skewed (eAppendix and eFigures 3-5 in the Supplement). Accordingly, we estimated the continuity of each hospitalist’s schedule as the percentage of working days that were part of a 7-day or longer block of consecutive working days in that year (steps 5-7 in eFigure 1 in the Supplement). In sensitivity analyses, we also used 3, 4, 5, and 6 continuous working days to categorize schedules. We then calculated the average of the schedules of all hospitalists providing care for each admission, weighted by each hospitalist’s number of E&M claims for that admission. In an alternative analysis, we expressed continuity of each hospitalist schedule as the median number of consecutive days worked in a year (eAppendix in the Supplement).
Admission and Hospital Characteristics
The Medicare Denominator File was used to extract information on patient age, sex, and race/ethnicity (non-Hispanic white, non-Hispanic black, Hispanic, and other). Medicaid eligibility was measured using the state buy-in information in the Medicare Denominator File. The percentage of high school graduates in the patient’s zip code area was obtained from the 2015 five-year American Community Survey. Elixhauser comorbidities were assessed based on outpatient, inpatient, and carrier claims in the 12 months prior to the hospital admission.14 Medicare Provider Analysis and Review claims for the hospitalizations were used to determine the length of stay, admitting diagnosis, ICU use, residence prior to hospitalization (community vs nursing facility/institution), and number of hospitalizations in the prior 12 months. We used admitting diagnosis in the analyses rather than diagnosis-related group (DRG) because DRG is determined after the hospital stay and might be affected by the quality of hospitalist care received. We chose the 30 most frequent admission diagnoses as classified by Clinical Classifications Software.15,16 Hospital characteristics included number of beds, location (rural vs urban), profit status (for profit, nonprofit, or government), medical school affiliation (major, limited, graduate program, or none), and patient satisfaction quality rating (1-2 stars, 3 stars, or 4-5 stars).17,18
Outcomes
The main outcome was mortality within 30 days of discharge. Secondary outcomes included discharge location (community vs other), 30-day readmission rate, and Medicare costs within 30 days of discharge. Medicare costs were obtained from inpatient, outpatient, professional, outpatient facility, and medical equipment claims.
Statistical Analysis
Because hospitalist schedules varied widely among hospitals, our main analyses used conditional models, in which the association of hospitalist schedules with outcomes was assessed within each hospital. For the 30-day mortality and discharge to community outcomes, we used conditional logistic regression models19 to determine the association of the quartile of mean weighted hospitalist schedules with outcomes, adjusted for all patient characteristics listed in eTable 1 in the Supplement. For 30-day readmission, we estimated the hazard ratio between quartiles of mean weighted hospitalist schedules using conditional Cox proportional hazard models.20 Death was a competing risk in the survival analysis. In sensitivity analyses, we also expressed continuity of hospitalist schedule as a continuous variable.
We used a 2-level, 2-stage model for 30-day Medicare costs. A 2-level model with gamma distribution was performed for a positive cost, and a 2-level logistic model was performed for a cost of 0.21 We combined the 2 results using the bootstrap method.22
We performed sensitivity analyses using multilevel (admission and hospital) logistic regression analysis to estimate the contribution of the hospital vs admission characteristics to the variation in whether an admitted patient received care from hospitalists whose weighted average schedules were in the top quartile for continuity.23 All analyses were performed using SAS version 9.4 (SAS Institute). We also performed analyses using the median number of consecutive working days in a year as a measure of the continuity of hospitalist schedule, expressed as the weighted average of the median scores of the hospitalists treating each admission (eAppendix in the Supplement). We used χ2 statistics P value to test the associations between categorical covariates and the quartile of weighted average of hospitalist schedules, with a P value less than .05 considered significant. For continuous variables, to test the difference between group means, we used an ANOVA F statistic P value, with a P value less than .05 considered significant. The University of Texas Medical Branch Institutional Review Board reviewed and approved this research and deemed it exempt from requiring patient informed consent owing to the use of deidentified data. We followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guideline.
Results
Using Medicare claims data, from January 1, 2014, to November 30, 2016, there were 114 777 admissions to 229 Texas hospitals. These admissions included only patients with a 3-day to 6-day length of stay and a medical DRG and excluded those with an ICU stay or more than 2 E&M charges from a hospitalist on any 1 day. Patients included in the analysis received all of their inpatient general medical care from 1 or more of 3098 hospitalists.
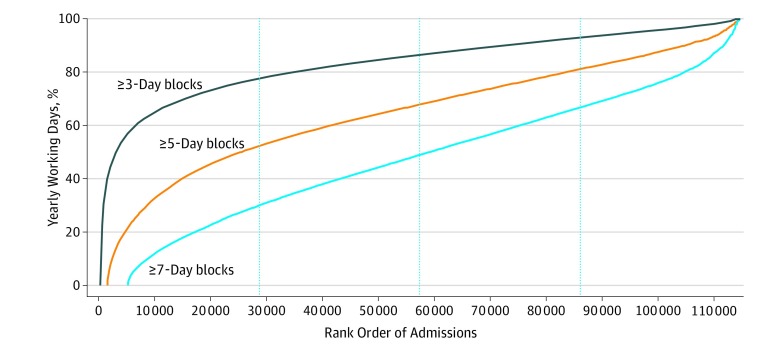
We estimated the continuity of the working schedules for the treating hospitalists by calculating the percentage of their total working days that year that were part of a 3-day, 5-day, or 7-day block of consecutive working days. Then, for each admission, we calculated a measure of continuity as the average percentage of consecutive working days for each treating hospitalist, weighted by their number of E&M charges for that admission. We then ranked all admissions by the weighted mean hospitalist schedules (Figure). Seven-day blocks produced the most separation by quartile. In the lowest quartile of admissions, the weighted mean schedules of the hospitalists providing care had 0% to 30% of working days as part of 7-day or longer blocks, whereas in the highest quartile, the hospitalists’ weighted mean schedules had 67% to 100% of working days as part of 7-day blocks.
Figure. Ranking of 114 777 Patients From 2014 Through 2016 by Weighted Average of Continuity in Hospitalist Schedules .
Dotted vertical lines indicate the 25th, 50th, and 75th percentile of admissions. Schedule continuity was assessed as the percentage of working days for each hospitalist that year that were part of a 3-day, 5-day, or 7-day block of consecutive working days. A weighted average of schedule continuity for each admission was produced as the mean schedule continuity of each hospitalist providing care for an admission, weighted by the number of evaluation and management claims each hospitalist submitted for that admission.
Table 1 presents the characteristics of the admissions by quartile of continuity of the schedules of the hospitalists. Small but significant differences were observed in most admission characteristics among quartiles, with admissions in the highest quartile having slightly higher age, length of stay, DRG weight, and number of prior hospitalizations. As expected, admissions in the highest quartile had fewer hospitalists providing their care. For example, admissions with a 6-day length of stay in the lowest quartile had a mean of 2.11 (95% CI, 2.08-2.14) hospitalists providing care vs 1.64 (95% CI, 1.62-1.67) hospitalists for admissions in the highest quartile.
Table 1. Admission and Hospital Characteristics Associated With the Working Schedules of Hospitalistsa.
| Characteristic | Quartile of Weighted Average of Hospitalist Schedules, % | P Value | |||
|---|---|---|---|---|---|
| Q1 | Q2 | Q3 | Q4 | ||
| Admission Characteristics | |||||
| Patient age, mean (95% CI), y | 79.85 (79.76-79.96) | 79.90 (79.81-80.00) | 80.07 (79.97-80.16) | 79.87 (79.77-79.97) | .008 |
| LOS, mean (95% CI), d | 3.95 (3.94-3.96) | 3.97 (3.96-3.99) | 4.01 (4.00-4.02) | 4.03 (4.02-4.04) | .001 |
| No. of hospitalists, mean (95% CI) | |||||
| 3-d LOS | 1.62 (1.61-1.63) | 1.62 (1.61-1.64) | 1.55 (1.53-1.56) | 1.31 (1.30-1.32) | <.001 |
| 4-d LOS | 1.80 (1.78-1.81) | 1.80 (1.78-1.82) | 1.71 (1.69-1.72) | 1.43 (1.42-1.45) | <.001 |
| 5-d LOS | 1.97 (1.95-2.00) | 1.97 (1.95-1.99) | 1.87 (1.85-1.89) | 1.54 (1.52-1.56) | <.001 |
| 6-d LOS | 2.11 (2.08-2.14) | 2.10 (2.07-2.13) | 1.97 (1.95-2.00) | 1.64 (1.62-1.67) | <.001 |
| No. of comorbidities, mean (95% CI) | 5.35 (5.31-5.39) | 5.49 (5.44-5.53) | 5.54 (5.49-5.58) | 5.66 (5.62-5.70) | <.001 |
| No. of prior hospitalizations, mean (95% CI) | 1.00 (0.98-1.01) | 1.02 (1.01-1.04) | 1.03 (1.01-1.04) | 1.05 (1.04-1.07) | <.001 |
| DRG weights, mean (95% CI) | 1.04 (0.98-1.01) | 1.06 (1.05-1.06) | 1.07 (1.07-1.08) | 1.07 (1.07-1.08) | <.001 |
| Male | 38.90 | 38.76 | 39.06 | 39.18 | .75 |
| Medicaid | 22.31 | 20.74 | 19.54 | 22.20 | <.001 |
| Race | |||||
| White | 74.72 | 74.26 | 75.92 | 73.04 | <.001 |
| Black | 9.54 | 9.52 | 8.77 | 7.82 | |
| Hispanic | 13.64 | 14.32 | 13.30 | 17.19 | |
| Education, mean (95% CI), %b | 82.45 (82.32-82.58) | 82.82 (82.69-82.95) | 83.49 (83.37-83.62) | 81.83 (81.69-81.97) | <.001 |
| Admitted from community | 94.74 | 94.90 | 94.32 | 94.19 | <.001 |
| Emergency hospitalization | 80.37 | 83.69 | 81.01 | 80.62 | <.001 |
| Weekend hospitalization | 30.64 | 31.09 | 30.85 | 30.36 | .28 |
| Hospital Characteristics | |||||
| No. of beds, mean (95% CI) | 451.99 (447.03-456.95) | 508.25 (503.06-513.44) | 535.74 (530.66-540.32) | 536.08 (531.54-540.62) | <.001 |
| Location | |||||
| Rural | 14.86 | 9.12 | 6.56 | 7.31 | <.001 |
| Urban | 85.14 | 90.88 | 93.44 | 92.69 | |
| Type of hospital | |||||
| For profit | 27.81 | 31.80 | 36.56 | 43.01 | <.001 |
| Government | 17.93 | 11.23 | 7.17 | 6.14 | |
| Nonprofit | 54.26 | 56.96 | 56.27 | 50.86 | |
| Medical school affiliation | |||||
| Major | 12.13 | 13.34 | 15.09 | 20.76 | <.001 |
| Limited | 25.71 | 27.90 | 32.70 | 29.96 | |
| Graduate program | 5.70 | 4.46 | 3.19 | 3.93 | |
| None | 56.46 | 54.31 | 49.02 | 45.35 | |
| HCAHPS summary star ratingc | |||||
| 1-2 stars | 12.89 | 13.88 | 10.00 | 13.61 | <.001 |
| 3 stars | 52.09 | 54.22 | 53.64 | 54.17 | |
| 4-5 stars | 35.02 | 31.90 | 36.36 | 32.23 | |
Abbreviations: DRG, diagnosis-related group; HCAHPS, Hospital Consumer Assessment of Healthcare Providers and Systems; LOS, length of stay.
For each admitted patient who received all their generalist care from hospitalists, we determined the continuity score for each hospitalist providing care to that patient and calculated the average continuity score, weighted by the number of days each hospitalist provided care for that patient. These weighted mean continuity scores for each admission were then grouped by quartile, from lowest continuity score to highest continuity score.
Persons 25 years and older in the zip code with a high school education.
Summary star ratings were taken from HCAHPS, a patient satisfaction survey mandated by the Centers for Medicare & Medicaid Services.
Much larger differences were observed among the quartiles in hospital characteristics, with higher percentages of admissions in the highest quartile of hospitalist continuity occurring in larger, urban, nongovernment hospitals and hospitals with a medical school affiliation (Table 1). In a multilevel analysis (admission and hospital) of factors associated with whether a patient received care from hospitalists with schedules in the highest quartile of continuity, the hospital characteristics explained 41.9% of the variation, whereas admission characteristics explained only 0.02% (eTable 2 in the Supplement). Because of the large variation in continuity in hospitalist schedules among hospitals, the main analytic approaches to assessing the association of hospitalist schedules with outcomes used conditional models in which comparisons among working schedules were performed within each hospital, implicitly controlling for differences among hospitals.
Table 2 presents the results of the conditional logistic regression and conditional Cox proportional hazard analyses of the association of the continuity of hospitalist schedules with 30-day mortality, readmissions, and rate of discharge home, controlling for admitting diagnosis, comorbidity, and other patient characteristics. A stepwise association was noted between the quartile of hospitalist schedule continuity and unadjusted and adjusted 30-day mortality. Admissions in the highest quartile for hospitalist schedule continuity had a 6.47% 30-day mortality rate vs a 7.23% 30-day mortality rate for admissions in the lowest quartile (adjusted odds ratio [aOR], 0.88; 95% CI, 0.81-0.95). The hazard of readmission also decreased in the patients cared for by hospitalists in the highest quartile of continuity scores (hazard ratio, 0.94; 95% CI, 0.90-0.99), whereas the rate of patients who were discharged directly home from the hospital increased (aOR, 1.08; 95% CI, 1.03-1.13).
Table 2. Association of Continuity of the Weighted Mean Schedules of Hospitalists Providing Care for Patients With Outcomes of Hospitalization by Quartilea.
| Outcomeb | Quartile of Weighted Average of Hospitalist Schedulesa | |||
|---|---|---|---|---|
| Q1 | Q2 | Q3 | Q4 | |
| Admissions, No. | 29 068 | 28 967 | 28 721 | 28 291 |
| 30-d Mortality | ||||
| Unadjusted rate, No. (%) | 2101 (7.23) | 1965 (6.85) | 1905 (6.63) | 1831 (6.47) |
| aOR (95% CI) | 1 [Reference] | 0.92 (0.85-0.98) | 0.90 (0.83-0.98) | 0.88 (0.81-0.95) |
| 30-d Readmission | ||||
| Unadjusted rate, No. (%) | 4830 (16.62) | 4747 (16.54) | 4746 (16.52) | 4701 (16.61) |
| HR (95% CI) | 1 [Reference] | 0.97 (0.93-1.01) | 0.96 (0.91-1.01) | 0.94 (0.90-0.99) |
| Discharged home | ||||
| Unadjusted rate, No. (%) | 12 778 (43.95) | 12 582 (43.84) | 12 658 (44.07) | 13 154 (46.50) |
| aOR (95% CI) | 1 [Reference] | 1.05 (1.01-1.09) | 1.03 (0.99-1.08) | 1.08 (1.03-1.13) |
Abbreviations: E&M, evaluation and management; HR, hazard ratio; aOR, adjusted odds ratio.
The schedule continuity of hospitalists was categorized as the percentage of their working days in the year of the admission that were part of a block of at least 7 consecutive working days. Each admission was then assigned a weighted mean hospitalist schedule, which was the mean of the continuity of each hospitalist providing care during that admission, weighted by the number of days each hospitalist submitted an E&M claim.
Adjusted odds ratios for 30-day mortality and discharge home were derived from a conditional logistic regression model, and HRs for 30-day readmissions were derived from a conditional Cox proportional hazard model, with death as a competing risk.
Table 3 presents the Medicare costs in the 30 days after hospital discharge as a function of the mean continuity scores for the hospitalists providing care. Both unadjusted and adjusted costs decreased as the continuity score increased. Admissions in the highest quartile of hospitalist schedule continuity had $223 (95% CI, −$441 to −$7) lower cost than those in the first quartile. When stratifying by type of service, costs were lower for additional hospitalization and for skilled nursing facility stays and higher for professional services and home health services.
Table 3. Medicare Costs in the 30 Days After Hospital Discharge, Stratified by the Quartile of Continuity of the Mean Weighted Hospitalist Schedules.
| Costsa | Quartile of Weighted Average of Hospitalist Schedules, $ (95% CI) | |||
|---|---|---|---|---|
| Q1 | Q2 | Q3 | Q4 | |
| Admissions, No. (%) | 29 068 (25.3) | 28 967 (25.0) | 28 721 (25.0) | 28 291 (24.7) |
| Total cost | ||||
| Unadjusted cost | 8667.5 (8533.9 to 8801.0) | 8575.3 (8445.0 to 8705.7) | 8484.6 (8356.4 to 8612.8) | 8206.6 (8074.3 to 8338.9) |
| Adjusted cost | 8366.7 (8149.6 to 8583.8) | 8229.6 (8026.4 to 8432.7) | 8172.0 (7983.1 to 8360.8) | 8143.0 (7954.9 to 8331.1) |
| Difference in adjusted cost from Q1 | 0 [Reference] | −137.1 (−328.4 to 54.2) | −194.7 (−399.6 to 10.2) | −223.7 (−440.8 to −6.6) |
| Inpatient cost | ||||
| Unadjusted cost | 1957.8 (1886.0 to 2029.5) | 1985.6 (1910.8 to 2060.4) | 1947.3 (1873.4 to 2021.1) | 2030.1 (1948.9 to 2111.4) |
| Adjusted cost | 1857.9 (1801.9 to 1913.9) | 1837.1 (1784.3 to 1889.8) | 1765.4 (1717.8 to 1812.9) | 1780.6 (1733.8 to 1827.7) |
| Difference in adjusted cost from Q1 | 0 [Reference] | −20.8 (−70.4 to 28.8) | −92.5 (−144.7 to −40.3) | −77.2 (−133.2 to −21.2) |
| SNF cost | ||||
| Unadjusted cost | 4568.7 (4463.1 to 4674.3) | 4372.2 (4272.3 to 4472.1) | 4314.7 (4216.5 to 4412.9) | 3961.8 (3865.4 to 4058.3) |
| Adjusted cost | 4025.0 (3918.4 to 4131.7) | 3932.6 (3932.0 to 4033.3) | 3991.5 (3894.6 to 4088.3) | 3890.8 (3812.3 to 3969.1) |
| Difference in adjusted cost from Q1 | 0 [Reference] | −44.0 (−138.6 to 50.6) | −82.1 (−182.6 to 18.4) | −134.4 (−241.0 to −27.7) |
| Professional charges cost | ||||
| Unadjusted cost | 962.2 (938.7 to 985.8) | 998.4 (980.1 to 1016.7) | 993.4 (975.8 to 1011.0) | 984.2 (966.6 to 1001.8) |
| Adjusted cost | 859.4 (840.2 to 878.6) | 872.7 (854.6 to 891.1) | 876.2 (859.1 to 893.2) | 885.4 (868.5 to 902.4) |
| Difference in adjusted cost from Q1 | 0 [Reference] | 13.48 (−3.60 to 30.56) | 16.8 (−1.6 to 35.2) | 26.1 (6.9 to 45.2) |
| Home health cost | ||||
| Unadjusted cost | 726.2 (709.0 to 743.3) | 753.8 (736.1 to 771.4) | 771.6 (753.7 to 789.5) | 755.0 (737.2 to 772.8) |
| Adjusted cost | 859.4 (840.2 to 878.6) | 872.9 (854.6 to 891.1) | 876.2 (859.1 to 893.2) | 885.4 (868.5 to 902.4) |
| Difference in adjusted cost from Q1 | 0 [Reference] | 1.3 (−12.1 to 14.7) | 15.3 (1.1 to 29.6) | 16.9 (2.2 to 31.6) |
| Outpatient facility cost | ||||
| Unadjusted cost | 391.2 (376.7 to 405.7) | 398.2 (383.0 to 413.4) | 393.2 (377.7 to 408.7) | 407.7 (391.7 to 423.7) |
| Adjusted cost | 344.9 (332.0 to 357.8) | 354.6 (342.0 to 367.3) | 355.6 (343.8 to 367.4) | 354.27 (342.6 to 366.0) |
| Difference in adjusted cost from Q1 | 0 [Reference] | 9.8 (−1.7 to 21.2) | 10.8 (−1.7 to 23.1) | 9.4 (−3.5 to 22.3) |
| Medical equipment cost | ||||
| Unadjusted cost | 61.4 (56.7 to 66.1) | 67.2 (61.5 to 72.8) | 64.5 (59.6 to 69.3) | 67.7 (62.3 to 73.1) |
| Adjusted cost | 48.4 (46.1 to 50.7) | 48.5 (46.3 to 50.7) | 45.5 (43.6 to 47.4) | 47.4 (45.5 to 49.3) |
| Difference in adjusted cost from Q1 | 0 [Reference] | 0.1 (−1.9 to 2.1) | −2.8 (−5.0 to −0.7) | −0.9 (−3.2 to 1.4) |
Abbreviation: SNF, skilled nursing facility.
The unadjusted costs are the actual mean costs to Medicare in each category. The adjusted costs use a 2-stage multilevel model (admission and hospital) that includes a logistic model for 0 cost and gamma distribution for nonzero cost and is adjusted for all admission characteristics shown in eTable 1 in the Supplement.
We conducted several sensitivity analyses. In one set of analyses, we treated continuity of hospitalist schedules as a continuous variable rather than by quartile (eTable 3 in the Supplement). This did not change the associations between hospitalist schedules and outcomes. In other analyses, we excluded the first hospitalist E&M claim in an admission in determining the treating hospitalists because the first hospitalist to see a patient might be an on-call hospitalist if the patient was admitted during off-hours. The results of these analyses were similar to the main analyses, except that the differences in 30-day readmission rates by quartile of hospitalist continuity were not significant (eTable 4 in the Supplement). To assess whether the association of work schedules with outcomes varied between full-time and part-time hospitalists, we added total hospitalist working days in the year to the analysis and tested for interactions between continuity of hospitalist schedule and total working days. No interactions were observed. Also, adding discharge location to the analysis did not change the association of continuity with outcomes.
We examined the influence of varying the number of consecutive working days in estimating the continuity of the working schedules of the hospitalists by calculating the percentage of each hospitalist’s working days in a year that were part of a 3-day, 4-day, 5-day, 6-day, or 7-day block of continuous working days. eFigure 6 in the Supplement presents aORs for mortality for each 10% increase in continuity of mean weighted hospitalist schedule, calculated by the different methods. The aOR for mortality exhibited almost no change as a function of the number of consecutive days used in estimating continuity of hospitalist schedules (eFigure 6 in the Supplement). In analyses to explore this lack of change, we found that the relative ranking among the hospitalists in schedule continuity changed little as the number of consecutive days used to identify continuity varied (eTable 5 in the Supplement).
Finally, the analyses using the median number of consecutive working days for the treating hospitalists in the year produced results nearly identical to the main analyses (eTable 6 in the Supplement). In a spline analysis, we found that the association of hospitalist median working days and postdischarge mortality was linear between 1 and 14 days (eFigure 7 in the Supplement).
Discussion
In this study, we show that patients receiving care from hospitalists who usually work several days in a row experience better outcomes and lower costs after discharge compared with those cared for by hospitalists with more intermittent schedules. Continuity of care for hospitalized patients may be important for several reasons. It is unlikely that all relevant information communicated by patients and their families to a physician is included in the electronic medical record or transmitted orally during handoffs. Another aspect of continuity of care is trust. Knowledge of patient values and active family involvement are key in medical decision-making and discharge planning. Patients and their families may be less comfortable soliciting and following the advice of a physician they are seeing for the first time, particularly if the issue is value laden, such as end-of-life issues or discharge destination.1,24,25 However, one could also make a case for benefits from discontinuity—a fresh set of eyes might lead to more accurate diagnoses and treatments. The point is, the question of whether continuity of care during hospitalization is associated with patient care outcomes has largely gone unanswered.26,27,28,29,30 A Joint Commission Center for Transforming Healthcare report26 attributed the majority of serious medical errors to miscommunication between physicians during handoffs, but that finding was based on studies of house officers.
We have previously shown that care by hospitalists compared with care by primary care physicians is associated with higher readmission rates, higher costs after discharge, and lower rates of discharge home.7 More recently, Stevens et al5 reported higher 30-day mortality rates and lower rates of discharge home with care by hospitalists compared with care by primary care physicians. Results of the current study suggest that the adverse outcomes associated with hospitalist care might, in part, be because of discontinuities during hospitalization, in addition to the discontinuities experienced in the transitions from community to hospital to community.5,6,7
Much of the discontinuity of care experienced by hospitalized patients receiving care from hospitalists is a function of the working schedules of hospitalists.10 The large variation in hospitalist schedules among hospitals presumably reflects choices between competing priorities, such as preventing physician burnout vs increasing continuity.31 Efforts by hospitals and hospitalist groups to promote working schedules with more continuity could lead to improved postdischarge outcomes in patients receiving hospitalist care.
Limitations
The method of identifying hospitalist schedules in this study has limitations. The method cannot distinguish between, for example, a hospitalist working an 8-hour daily shift for a week from a hospitalist working every other night, in which each 8-hour or 12-hour shift overlaps 2 consecutive calendar days. Both would be categorized as having schedules with a high percentage of working days as part of a 7-day block of continuous working days. However, the association of hospitalists’ schedules with the likelihood of a patient seeing just 1 hospitalist shown in a prior study10 provides internal validation of the method. Also, we excluded admissions with more than 1 hospitalist charge in a day and, in a sensitivity analysis, excluded the initial hospitalist charge, which reduced any contribution from on-call or nocturnist hospitalists. This did not change the results. Another limitation is that hospitalists caring primarily for younger patients or patients who participate in a health-maintenance organization might not generate an E&M charge on a fee-for-service Medicare patient every day that they work, which would bias the estimates of their schedules.
A major challenge in virtually all observational studies is selection bias. At the level of the patients, patients with more complex illnesses might be more likely to see multiple generalist physicians and also may be more likely to experience adverse outcomes, producing a spurious association of discontinuity with adverse outcomes. We addressed this bias in several ways. First, we excluded the patient admissions most likely to exhibit this bias: those with more than 1 E&M charge for generalist care on any day and those with an ICU stay. We also controlled for length of stay, admission diagnosis, and all other available factors associated with the outcomes examined.
Second, the most powerful way of reducing bias takes advantage of the fact that continuity of care of admissions varies greatly by the hospitalists providing the care.10 Thus, these analyses were performed at the level of the hospitalist. We sought to determine whether patients cared for by hospitalists with discontinuous work schedules had worse outcomes, controlling for characteristics of the hospital and the admission. At the hospitalist level, the selection bias outlined above is less plausible; that is, a person would have to postulate that hospitalists with discontinuous work schedules are more likely to care for sicker patients. We found no evidence of this. As summarized in Table 1, patients receiving care from hospitalists in the top quartile of schedule continuity compared with those in the bottom quartile differed only slightly by characteristics of the admission, and most of the differences were associated with a slightly higher risk of adverse outcomes (eTable 1 in the Supplement). Overall, patient characteristics contributed only 0.02% to the variation in continuity of the hospitalist schedules.
Conclusions
Hospitalist schedules vary widely among hospitalists and hospitals. Care provided by hospitalists with more continuous schedules may be associated with better outcomes in hospitalized patients. These findings should be considered in the design of hospitalist schedules.
eAppendix. Expressing schedule continuity by the median number of consecutive days worked in a year.
eFigure 1. Cohort selection for identifying hospitalists (steps 1-4) and hospitalist schedules (steps 4-7).
eFigure 2. Cohort selection for identifying outcomes of hospitalist care.
eFigure 3. This figure presents an analysis of 10 randomly selected hospitalists in 2016, examining the distribution of their blocks of working days.
eFigure 4. Distribution of consecutive days worked for all hospitalists in 2016.
eFigure 5. Distribution of skewness in hospitalist schedules.
eFigure 6. The effect of varying the method of estimating continuity of hospitalist schedule on the association between hospitalist schedule and 30-day mortality.
eFigure 7. Penalized B-splines smoothing curve and 95% confidence band for weighted average of median working days and 30 day mortality.
eTable 1. Odds of 30-day mortality for medical admissions aged 66+ and without an Intensive Care Unit (ICU) stay during hospitalization, by patient characteristics, from a conditional logistic model for 01/01/2014 - 11/30/2016, 100% TX Medicare data.
eTable 2. Intraclass correlation coefficients (ICCs) from multilevel model predicting whether an admission received care from hospitalists who were in the highest quartile in mean weighted schedule continuity.
eTable 3. Association of each 10% increase in weighted mean hospital schedule continuity with 30-day mortality, readmission, and rate of discharge home.
eTable 4. Association of continuity of hospitalist schedule, by quartile, with unadjusted and adjusted 30-day mortality, readmission and rate of discharge home.
eTable 5. Correlation among 3098 hospitalists in their ranking of continuity of their schedules, with continuity of their schedules calculated as the percent of working days that were part of a 3, 4, 5, 6 or 7 day block of continuous working days.
eTable 6. Association of continuity of the schedules of the treating hospitalists, by quartile, with unadjusted and adjusted 30-day mortality, 30-day readmission and rate of discharge home.
eReferences.
References
- 1.Tammes P, Salisbury C. Continuity of primary care matters and should be protected. BMJ. 2017;356:j373. doi: 10.1136/bmj.j373 [DOI] [PubMed] [Google Scholar]
- 2.Nyweide DJ, Anthony DL, Bynum JP, et al. Continuity of care and the risk of preventable hospitalization in older adults. JAMA Intern Med. 2013;173(20):1879-1885. doi: 10.1001/jamainternmed.2013.10059 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Donaldson MS, Yordy KD, Lohr KN, Vaneselow NA, eds; Institute of Medicine (US) Committee on the Future of Primary Care Primary Care: America’s Health in a New Era. Washington, DC: Institute of Medicine, National Academy of Sciences; 1996. [PubMed] [Google Scholar]
- 4.Sharma G, Fletcher KE, Zhang DD, Kuo YF, Freeman JL, Goodwin JS. Continuity of outpatient and inpatient care by primary care physicians for hospitalized older adults. JAMA. 2009;301(16):1671-1680. doi: 10.1001/jama.2009.517 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Stevens JP, Nyweide DJ, Maresh S, Hatfield LA, Howell MD, Landon BE. Comparison of hospital resource use and outcomes among hospitalists, primary care physicians, and other generalists. JAMA Intern Med. 2017;177(12):1781-1787. doi: 10.1001/jamainternmed.2017.5824 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Willett LL, Landefeld CS. The costs and benefits of hospital care by primary physicians: continuity counts. JAMA Intern Med. 2017;177(12):1788-1789. doi: 10.1001/jamainternmed.2017.5833 [DOI] [PubMed] [Google Scholar]
- 7.Kuo YF, Goodwin JS. Association of hospitalist care with medical utilization after discharge: evidence of cost shift from a cohort study. Ann Intern Med. 2011;155(3):152-159. doi: 10.7326/0003-4819-155-3-201108020-00005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fletcher KE, Sharma G, Zhang D, Kuo YF, Goodwin JS. Trends in inpatient continuity of care for a cohort of Medicare patients 1996-2006. J Hosp Med. 2011;6(8):438-444. doi: 10.1002/jhm.916 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wachter RM, Goldman L. Zero to 50,000—the 20th anniversary of the hospitalist. N Engl J Med. 2016;375(11):1009-1011. doi: 10.1056/NEJMp1607958 [DOI] [PubMed] [Google Scholar]
- 10.Goodwin JS, Zhou J, Kuo YF, Nattinger AB. Work schedules of hospitalists and continuity of care during hospital stays of Texas Medicare patients: an observational study. J Gen Intern Med. 2019;34(4):489-491. doi: 10.1007/s11606-018-4777-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dougan BM, Montori VM, Carlson KW. Implementing a hospitalist program in a critical access hospital. J Rural Health. 2018;34(1):109-115. doi: 10.1111/jrh.12190 [DOI] [PubMed] [Google Scholar]
- 12.Simone KG. Hospitalist Recruitment and Retention: Building a Hospital Medicine Program. Hoboken, NJ: Wiley-Blackwell; 2010. [Google Scholar]
- 13.Dwight P, MacArthur C, Friedman JN, Parkin PC. Evaluation of a staff-only hospitalist system in a tertiary care, academic children’s hospital. Pediatrics. 2004;114(6):1545-1549. doi: 10.1542/peds.2004-0077 [DOI] [PubMed] [Google Scholar]
- 14.Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity measures for use with administrative data. Med Care. 1998;36(1):8-27. doi: 10.1097/00005650-199801000-00004 [DOI] [PubMed] [Google Scholar]
- 15.Agency for Healthcare Research and Quality. Clinical Classifications Software (CCS) for ICD-10-PCS (beta version). https://www.hcup-us.ahrq.gov/toolssoftware/ccs10/ccs10.jsp. Accessed October 9, 2019.
- 16.Agency for Healthcare Research and Quality. Clinical Classifications Software (CCS) for ICD-9-CM. https://www.hcup-us.ahrq.gov/toolssoftware/ccs/ccs.jsp. Accessed October 9, 2019.
- 17.Centers for Medicare & Medicaid Services Hospital Compare overall hospital rating. https://www.medicare.gov/hospitalcompare/About/Hospital-overall-ratings.html. Accessed October 9, 2019.
- 18.Centers for Medicare & Medicaid Services 2013. Provider of Services current files. https://www.cms.gov/Research-Statistics-Data-and-Systems/Downloadable-Public-Use-Files/Provider-of-Services/. Updated July 31, 2019. Accessed October 9, 2019.
- 19.Breslow NE, Day NE, Halvorsen KT, Prentice RL, Sabai C. Estimation of multiple relative risk functions in matched case-control studies. Am J Epidemiol. 1978;108(4):299-307. doi: 10.1093/oxfordjournals.aje.a112623 [DOI] [PubMed] [Google Scholar]
- 20.Shinozaki T, Mansournia MA, Matsuyama Y. On hazard ratio estimators by proportional hazards models in matched-pair cohort studies. Emerg Themes Epidemiol. 2017;14(1):6. doi: 10.1186/s12982-017-0060-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Flynn M, Francis LA. More flexible GLMs: zero-inflated models and hybrid models. https://www.casact.org/pubs/forum/09wforum/flynn_francis.pdf. Published 2009. Accessed October 9, 2019.
- 22.Efron B, Tibshirani RJ. An Introduction to the Bootstrap. New York, NY: CRC Press; 1994. [Google Scholar]
- 23.Greenland S. Principles of multilevel modelling. Int J Epidemiol. 2000;29(1):158-167. doi: 10.1093/ije/29.1.158 [DOI] [PubMed] [Google Scholar]
- 24.Sharma G, Freeman JL, Zhang DD, Goodwin JS. Continuity of care and intensive care unit use at the end of life. Arch Intern Med. 2009;169(1):81-86. doi: 10.1001/archinternmed.2008.514 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wray CM, Farnan JM, Arora VM, Meltzer DO. A qualitative analysis of patients’ experience with hospitalist service handovers. J Hosp Med. 2016;11(10):675-681. doi: 10.1002/jhm.2608 [DOI] [PubMed] [Google Scholar]
- 26.Joint Commission Center for Transforming Healthcare releases targeted solutions tool for hand-off communications. Jt Comm Perspect. 2012;32(8):1–, 3.. [PubMed] [Google Scholar]
- 27.Joint Commission Inadequate hand-off communication. Sentinel Event Alert. 2017;58(58):1-6. [PubMed] [Google Scholar]
- 28.Epstein K, Juarez E, Epstein A, Loya K, Singer A. The impact of fragmentation of hospitalist care on length of stay. J Hosp Med. 2010;5(6):335-338. doi: 10.1002/jhm.675 [DOI] [PubMed] [Google Scholar]
- 29.Turner J, Hansen L, Hinami K, et al. The impact of hospitalist discontinuity on hospital cost, readmissions, and patient satisfaction. J Gen Intern Med. 2014;29(7):1004-1008. doi: 10.1007/s11606-013-2754-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.O’Leary KJ, Turner J, Christensen N, et al. The effect of hospitalist discontinuity on adverse events. J Hosp Med. 2015;10(3):147-151. doi: 10.1002/jhm.2308 [DOI] [PubMed] [Google Scholar]
- 31.Ali NA, Hammersley J, Hoffmann SP, et al. ; Midwest Critical Care Consortium . Continuity of care in intensive care units: a cluster-randomized trial of intensivist staffing. Am J Respir Crit Care Med. 2011;184(7):803-808. doi: 10.1164/rccm.201103-0555OC [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eAppendix. Expressing schedule continuity by the median number of consecutive days worked in a year.
eFigure 1. Cohort selection for identifying hospitalists (steps 1-4) and hospitalist schedules (steps 4-7).
eFigure 2. Cohort selection for identifying outcomes of hospitalist care.
eFigure 3. This figure presents an analysis of 10 randomly selected hospitalists in 2016, examining the distribution of their blocks of working days.
eFigure 4. Distribution of consecutive days worked for all hospitalists in 2016.
eFigure 5. Distribution of skewness in hospitalist schedules.
eFigure 6. The effect of varying the method of estimating continuity of hospitalist schedule on the association between hospitalist schedule and 30-day mortality.
eFigure 7. Penalized B-splines smoothing curve and 95% confidence band for weighted average of median working days and 30 day mortality.
eTable 1. Odds of 30-day mortality for medical admissions aged 66+ and without an Intensive Care Unit (ICU) stay during hospitalization, by patient characteristics, from a conditional logistic model for 01/01/2014 - 11/30/2016, 100% TX Medicare data.
eTable 2. Intraclass correlation coefficients (ICCs) from multilevel model predicting whether an admission received care from hospitalists who were in the highest quartile in mean weighted schedule continuity.
eTable 3. Association of each 10% increase in weighted mean hospital schedule continuity with 30-day mortality, readmission, and rate of discharge home.
eTable 4. Association of continuity of hospitalist schedule, by quartile, with unadjusted and adjusted 30-day mortality, readmission and rate of discharge home.
eTable 5. Correlation among 3098 hospitalists in their ranking of continuity of their schedules, with continuity of their schedules calculated as the percent of working days that were part of a 3, 4, 5, 6 or 7 day block of continuous working days.
eTable 6. Association of continuity of the schedules of the treating hospitalists, by quartile, with unadjusted and adjusted 30-day mortality, 30-day readmission and rate of discharge home.
eReferences.