Abstract
We report the case of a 38-year-old male with a previous history of severe cranial trauma and subsequent large subdural and subarachnoid hemorrhage on whom an emergent hematoma evacuation was performed with a good outcome and follow-up. Despite a good clinical evolution, the patient experienced a further intracranial hematoma 18 years after the trauma, with severe aphasia and mild right hemiparesis. After complete etiological study, two cranial pseudoaneurysms were observed in the cerebral angiography. Endovascular treatment was successfully completed, achieving full embolization without complications. No rebleeding was detected during follow-up. The patient had a good clinical outcome at 3 months and achieved complete recovery. Cranial pseudoaneurysm rupture is a rare cause of intracerebral hemorrhage, especially if the trauma occurs years before the bleeding.
Keywords: Cranial pseudoaneurysm, Intracranial hemorrhage, Endovascular treatment
Background
Traumatic cerebral pseudoaneurysm (TCP) is an extremely uncommon cause of intracranial hemorrhage (ICH). Most cases are related to a pseudoaneurysm medium meningeal artery (PMMA) rupture, but other TCP locations have also been reported. Up to 70% of all cases are located in the epidural, subdural, or subarachnoid spaces. Less frequently, an intraparenchymal hemorrhage is associated with a TCP [1, 2, 3, 4].
The association between cranial trauma and a secondary ICH due to a TCP occurs in the first days after trauma onset. Rare cases of delayed rebleeding have been reported [5, 6, 7].
We describe a single case of ICH associated with the presence of TCP 18 years after the cranial trauma.
Case Presentation
A 38-year-old male was admitted to our emergency department with aphasia and mild right hemiparesis 5 h after sudden onset. No vascular risk factors were identified. The anamnesis provided by family members revealed no cranial traumas in the previous weeks; however, they did refer to a history of severe cranial trauma 18 years earlier with ICH and hematoma evacuation through decompressive craniectomy in another country. Neither CT nor cerebral angiography were performed during follow-up. No history of rebleeding was identified during this period, and the patient had an independent functional status, with a mild motor aphasia as the only neurological sequel together with a mild right leg paresis.
Investigations
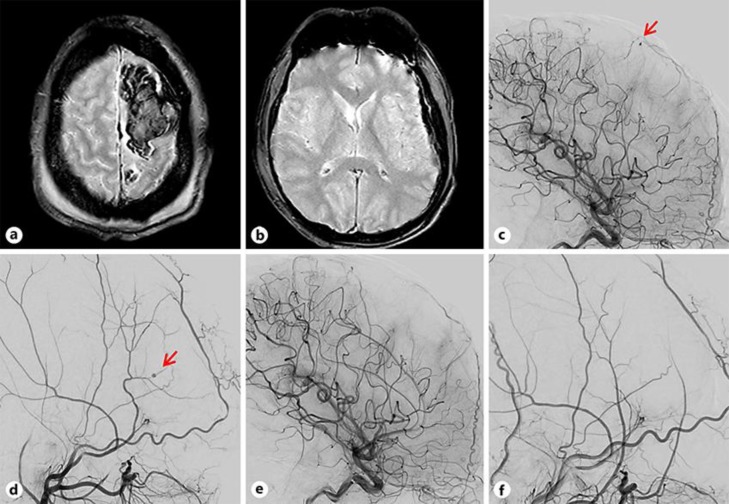
Cranial magnetic resonance imaging was performed in the acute phase. An acute subdural hematoma was observed together with intracerebral and subarachnoid hemorrhages (Fig. 1a, b). No aneurysms or other vascular malformations were identified. No hematoma growth was detected during the computed tomography (CT) follow-up. Finally, a cerebral angiography was carried out to complete the ICH etiology and rule out the presence of any vascular malformation. Two different pseudoaneurysms were detected, located in the left middle meningeal and left callosal marginal arteries (Fig. 1c, d). No arteriovenous malformations of fistulas were detected.
Fig. 1.
a, b A moderate left frontal ICH in a gradient echo sequence, together with subdural and subarachnoid hemorrhage. The diagnostic cerebral angiography shows two cerebral pseudoaneurysms located in the left callosal marginal (c) and medium meningeal arteries (d) (red arrows). e, f Follow-up cerebral angiography showing complete obliteration of both pseudoaneurysms.
Treatment
An emergent endovascular treatment was decided on to avoid new cranial hemorrhages. For the treatment of the first pseudoaneurysm, a microcatheter Magic 1.2 F (Balt, Montmorency, France) was used and navigated through the left callosal marginal to the pseudoaneurysm, which was embolized with Glubran 33% (General Enterprise Marketing, Viareggio, Italy) and Lipiodol Ultra-Fluide (Guerbet, Aulnay-sous-Bois, France).
For the second pseudoaneurysm located in little branches of the left middle meningeal artery, a Sonic 1.2F15 microcatheter balloon (Balt, Montmorency, France) was navigated through the artery to the pseudoaneurysm. The embolization was performed with Squid 18 (Emboflu, Gland, Switzerland).
In the final angiography, complete occlusion of both pseudoaneurysms was achieved, and there were no complications (Fig. 1e, f).
At the 3-month follow-up, the patient presented neurological improvement, remaining with a mild motor aphasia and a mild right leg paresis. The modified Rankin Score was 1. Symptoms and functional outcome improved fully until his previous neurological status was recovered.
Discussion
We describe a single case of ICH associated with the presence of two TCPs 18 years after cranial trauma.
TCP is an extremely uncommon cause of ICH. It occurs after arterial wall rupture by trauma, and the bleeding is confined just by the adventitia and surrounding tissues. TCP is typically located in branches depending on the middle meningeal artery as a consequence of a temporal fracture. The presence of a skull temporal fracture is currently the most important predictive factor associated with PMMA, a correlation that is observed in about 92% of the cases. Another risk factor recorded in the literature that is associated with the appearance of a PMMA is the presence of a small hematoma close to the rim [6, 8, 9, 10, 11].
The association between cranial trauma and a secondary ICH due to a TCP occurs within the first days after trauma onset. If the TCP is not diagnosed by a CT angiography, rebleeding in the acute phase could lead to a worse outcome, including death. Some rare cases of delayed rebleeding between 2 weeks and 11 months after cranial trauma have been reported, but none after the first year has been described [5, 6, 7].
Despite the low frequency of delayed TCP rupture, in patients with ICH and a history of cranial trauma, CT angiography or cerebral angiography is recommended to rule out the presence of TCP because of its potential mortality and morbidity of recurrence of bleeding. Moreover, endovascular therapies for these TCPs have high rates of occlusion and bear a low risk of complications [2, 3, 10, 12].
To the best of our knowledge, this is the first reported case of ICH secondary to a PMMA rupture taking place years after the cranial trauma.
Statement of Ethics
The research was conducted in ethical accordance with the World Medical Association Declaration of Helsinki. The patient gave his written informed consent to publish his case (including publication of images).
Disclosure Statement
The authors have no conflicts of interest to declare.
Funding Sources
This work has not received external funding.
Author Contributions
M.T. performed the diagnostic cerebral angiography, endovascular treatment, and designed the manuscript. S.R. performed the endovascular treatment and reviewed the manuscript. Y.S., S.B., C.C., and J.S. reviewed the manuscript.
Acknowledgement
We thank the patient and his relatives who with their generosity have contributed to this study.
References
- 1.Salazar Flores J, Vaquero J, Garcia Sola R, Rossi E, Martinez R, Martinez P, et al. Traumatic false aneurysms of the middle meningeal artery. Neurosurgery. 1986 Feb;18((2)):200–3. doi: 10.1227/00006123-198602000-00016. [DOI] [PubMed] [Google Scholar]
- 2.Bozzetto-Ambrosi P, Andrade G, Azevedo-Filho H. Traumatic pseudoaneurysm of the middle meningeal artery and cerebral intraparenchymal hematoma: case report. Surg Neurol. 2006;66(Suppl 3):S29–31. doi: 10.1016/j.surneu.2006.08.048. [DOI] [PubMed] [Google Scholar]
- 3.Marvin E, Laws LH, Coppens JR. Ruptured pseudoaneurysm of the middle meningeal artery presenting with a temporal lobe hematoma and a contralateral subdural hematoma. Surg Neurol Int. 2016 Jan;7((3 Suppl 2)):S23–7. doi: 10.4103/2152-7806.173564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wu X, Jin Y, Zhang X. Intraparenchymal hematoma caused by rupture of the traumatic pseudoaneurysm of middle meningeal artery. J Craniofac Surg. 2014;25((2)):e111–3. doi: 10.1097/SCS.0000000000000450. [DOI] [PubMed] [Google Scholar]
- 5.Ko JH, Kim YJ. Traumatic pseudoaneurysm of the middle meningeal artery with an arteriovenous fistula on a non-fractured site. Interv Neuroradiol. 2014 May-Jun;20((3)):352–6. doi: 10.15274/INR-2014-10025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Montanari E, Polonara G, Montalti R, Vivarelli M, Ricciuti RA, Giorgetti R, et al. Delayed Intracerebral Hemorrhage After Pseudoaneurysm of Middle Meningeal Artery Rupture: Case Report, Literature Review, and Forensic Issues. World Neurosurg. 2018 Sep;117:394–410. doi: 10.1016/j.wneu.2018.06.158. [DOI] [PubMed] [Google Scholar]
- 7.Singh M, Ahmad FU, Mahapatra AK. Traumatic middle meningeal artery aneurysm causing intracerebral hematoma: a case report and review of literature. Surg Neurol. 2006 Sep;66((3)):321–3. doi: 10.1016/j.surneu.2005.11.029. [DOI] [PubMed] [Google Scholar]
- 8.Bezircioğlu H, Erşahin Y, Demirçivi F, Yurt I, Dönertaş K, Tektaş S. Nonoperative treatment of acute extradural hematomas: analysis of 80 cases. J Trauma. 1996 Oct;41((4)):696–8. doi: 10.1097/00005373-199610000-00016. [DOI] [PubMed] [Google Scholar]
- 9.Wang CH, Lee HC, Cho DY. Traumatic pseudoaneurysm of the middle meningeal artery: possible indicators for early diagnosis in the computed tomography era. Surg Neurol. 2007 Dec;68((6)):676–81. doi: 10.1016/j.surneu.2006.11.048. [DOI] [PubMed] [Google Scholar]
- 10.Jussen D, Wiener E, Vajkoczy P, Horn P. Traumatic middle meningeal artery pseudoaneurysms: diagnosis and endovascular treatment of two cases and review of the literature. Neuroradiology. 2012 Oct;54((10)):1133–6. doi: 10.1007/s00234-011-1003-7. [DOI] [PubMed] [Google Scholar]
- 11.de Andrade AF, Figueiredo EG, Caldas JG, Paiva WS, De Amorim RL, Puglia P, et al. Intracranial vascular lesions associated with small epidural hematomas. Neurosurgery. 2008 Feb;62((2)):416–20. doi: 10.1227/01.neu.0000316008.11388.f2. [DOI] [PubMed] [Google Scholar]
- 12.Tsutsumi M, Kazekawa K, Tanaka A, Ueno Y, Nomoto Y, Nii K, et al. Traumatic middle meningeal artery pseudoaneurysm and subsequent fistula formation with the cavernous sinus: case report. Surg Neurol. 2002 Nov;58((5)):325–8. doi: 10.1016/s0090-3019(02)00834-0. [DOI] [PubMed] [Google Scholar]