Abstract
This study was undertaken to know the incidence and management practices of snakebite envenomation at the First Referral Unit - Sub-District Hospital, Dahanu, Maharashtra, India. Retrospective analysis of snakebite case records (n=145) was carried out for one-year period (January to December 2014). The annual incidence of snakebite was 36 per 100,000 population with case fatality rate of 4.5 per cent. Venomous snakebites were 76 per cent and non-venomous snakebites were 24 per cent. Overall, snakebites were more common in males (52.4%) than females (47.6%). Majority of the snakebites (66%) were in the age group of 18-45 yr. Seasonal variation was observed with highest snakebites in monsoon (58%). Lower extremities were the most common site of bites (63%). Neurotoxic and vasculotoxic envenomation were reported in 19 and 27 per cent snakebite cases, respectively. Anti-snake venom (ASV) was administered at an average dose of 7.5±0.63 vials (range 2-40, median 6). There was no uniform protocol followed for ASV administration as per the National Snakebite Management Protocol of Government of India (2009).
Keywords: Annual incidence, anti-snake venom, envenomation, snakebite, venomous
Every year worldwide, snakebite envenomation leads to more than 100,000 deaths and causes permanent disability or disfigurement in about 400,000 cases1. South Asia is the most affected Region due to snakebite envenomation2,3, and India contributes to 50 per cent of the estimated deaths due to venomous snakebites globally1. In India, highest number of deaths due to snakebites have been reported in Uttar Pradesh, Andhra Pradesh, Bihar, Tamil Nadu, West Bengal and Maharashtra4. Anti-snake venom (ASV) is the only effective specific treatment of snakebite envenoming5. A study conducted in Nepal reported ASV administration within one hour in only 14 per cent and within greater than five hours in 36 per cent of snakebite envenomation6. Delay in ASV administration was associated with high incidence of complications7 and high case fatality rates (CFRs) in snakebite patients6. National Snakebite Management Protocol (2009), Government of India8 and World Health Organization-South East Asia Regional Office guidelines (2010)9 were available to the healthcare providers in India for the management of snakebites before the release of Standard Treatment Guidelines (STG, 2016) on management of snakebite by the Ministry of Health & Family Welfare (MoHFW), Government of India10. Department of Health Research, MoHFW, Government of India, sanctioned a Model Rural Health Research Unit (MRHRU) at Dahanu, district Palghar, Maharashtra in 201411. There was lack of information on incidence and management practices of snakebite envenomation in this tribal block of Dahanu. Therefore, the aim of the present study was to know the annual incidence and management practices of snakebite envenomation at the First Referral Unit (FRU) - Sub-District Hospital (SDH) Dahanu.
The snakebite admission case records and death registers were retrospectively studied from January to December 2014 maintained at SDH, Dahanu. The study was conducted at MRHRU, Dahanu, Maharashtra, and was approved by the Ethics Committee of ICMR-National Institute for Research in Reproductive Health, Mumbai (No. D/ICEC/Sci-108/145/2016). The data were collected on demographic characteristics, circumstances of snakebite, signs and symptoms, first aid, duration (h) between time of snakebite and access to FRU, estimated distance (km) from snakebite locality (based on address mentioned in SDH records) to FRU, ASV administration (test dose, total ASV vials used), duration of stay at FRU (days) and outcomes. The snakebite cases were classified as venomous and non-venomous based on the clinical information and/or data available on species of snakes identified either by the patients or the treating medical officers (MOs) recorded in case record forms. Case records with incomplete or inadequate information were excluded. As per the Census of India (2011)12, total population of Dahanu taluka was 402,095. This was used as reference population for calculation of incidence of snakebites, and CFR.
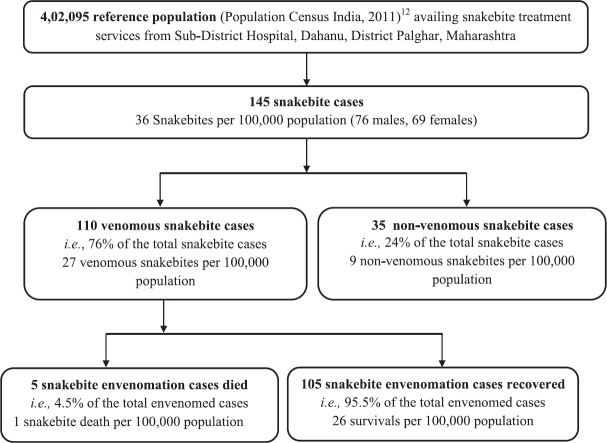
The annual incidence of snakebite was 36 per 100,000 populations which was comparable to Vidarbha region, Maharashtra13, lower than Sri Lanka14, Bangladesh15, Myanmar16 and Chitwan and Nawalparasi districts in Nepal17. Seventy six per cent snakebite cases (n=110) were due to venomous and 24 per cent (n=35) were due to non-venomous snakebites. Five of the 110 venomous snakebites had fatal outcome resulting in 4.5 per cent CFR with an annual incidence of one snakebite death per 100,000 populations. The CFR was comparable with other studies from Maharashtra, India13,18,19 and Myanmar16. The CFR was lower than Nepal6,17 but higher than West Bengal, India20, Bangladesh21 and Sri Lanka22. One hundred and five snakebite cases were recovered with an annual incidence of 26 survivals per 100,000 populations (Fig. 1). The overall distribution of snakebite was higher in males (n=76, 52.4%) than females (n=69, 47.6%). However, the distribution of venomous snakebite was higher in females (53.6%) than males (46.4%) (Fig. 2A). The mean age of snakebite cases was 33.2±1.3 yr [mean ± standard error of mean (SEM), median 32, range 1.6-70 yr]. Majority of the venomous and non-venomous snakebites were higher in the age group of 18-45 yr (Fig. 2B) comparable with other studies from India19,20,23 and Nepal6,17. Ninety per cent of the snakebite cases were admitted during the months of May to November (Fig. 2C). The distribution of snakebites as per the time was reported as eight per cent early morning (0300-0559 h), 25 per cent morning (0600-0959 h), 26 per cent daytime (1000-1659 h), 22 per cent evening (1700-1959 h) and 21 per cent night (2000-0259 h).
Fig. 1.
Flow chart showing population at risk for snakebite, venomous and non-venomous snakebite cases admitted at Sub-District Hospital, Dahanu, Maharashtra, India.
Fig. 2.
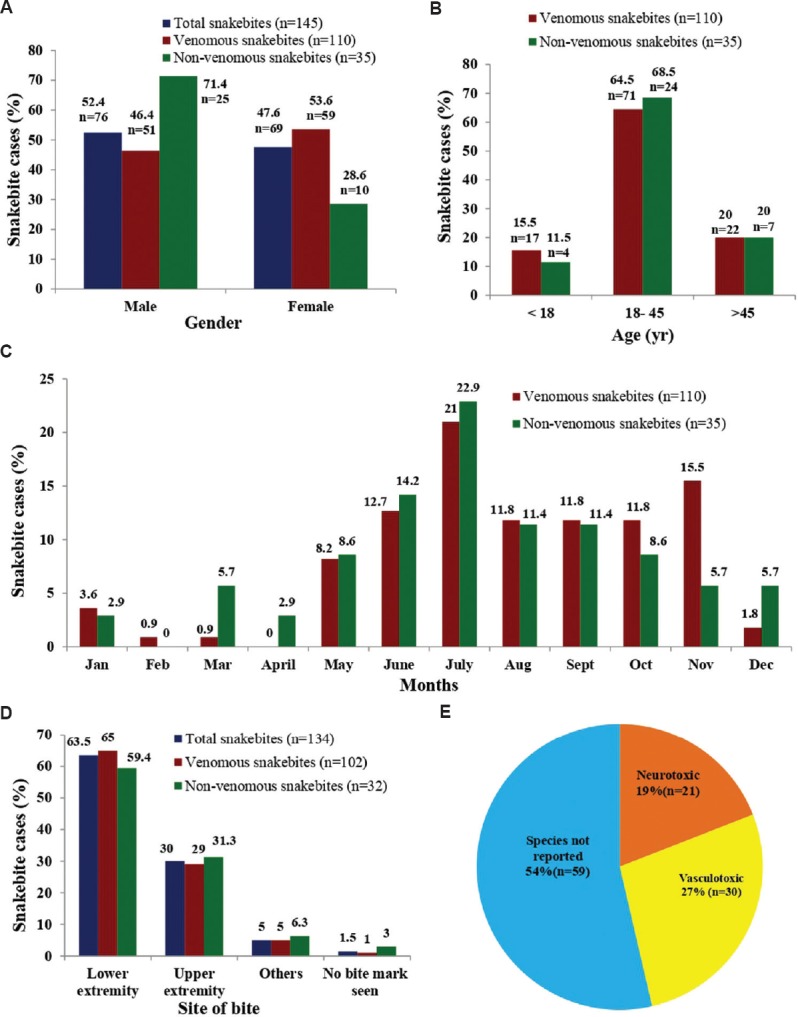
Characteristics of snakebite cases. (A) Gender-based distribution of venomous and non-venomous snakebite cases. (B) Age-wise distribution of venomous and non-venomous snakebite cases. (C) Seasonal variation of snakebite cases. (D) Site of snakebite (Data were available for 134 cases out of 145), n=134. (E) Categorization of snakebite based on signs and symptoms of envenomation.
Majority of snakebites occurred on lower limbs (Fig. 2D). The estimated mean distance between the place of snakebite occurrence and FRU was 19.02±4.28 km. The mean time duration between snakebite and access to FRU was 3.13±0.46. There was no information available related to mode of transport for snakebite case transfer to FRU. The higher mean time duration (with >3 h) between snakebite and admission to FRU could be due to long distance of the place of snakebite occurrence or referral and poor availability of transport facilities, especially during night.
As represented in Figure 2E, 19 per cent showed evidence of neurotoxic envenomation and 27 per cent showed evidence of vasculotoxic envenomation. None of the cases reported evidence of myotoxic envenomation. All snakebite patients received injection tetanus toxoid. The average dose of ASV administered to all venomous snakebite cases was 7.5±0.63 vials (range 2-40, median 6). Seventy snakebite cases received <10 ASV vials, 35 received 10-20 ASV vials and five cases received 21-40 ASV vials. ASV intradermal skin test was reported in 14 non-venomous and three venomous snakebites. No specific record of anaphylactic, pyogenic and serum sickness reactions was maintained at FRU. The average duration of hospital stay was 3.13±0.18 days (median 3, range 1-14 days).
Since there was no awareness and training on the management of snakebites as per the National Snakebite Management Protocol8, there was no uniform protocol followed for the management of snakebite envenomation at FRU. Non-compliance of standard treatment protocol, use of ASV test dose and ASV administration in non-venomous snakebite cases suggest an urgent need of capacity building of public healthcare system on diagnosis and management of snakebites as per the STG10. Lack of detailed information on occupation, activity at time of bite, exact time of ASV administration, anaphylactic reactions to ASV etc., were some of the limitations of this study.
Acknowledgment:
Authors thank Drs V.M. Katoch, Kiran Katoch, Himmatrao Bawaskar, Sanjay Chauhan and S.D. Kholkute for encouragement and support for implementation of this study. Authors sincerely thank Drs Satish Pawar, Archana Patil, Mohan Jadhav, Sanjeev Kamble, Shyam Nimagade, District Health Officer; Civil Surgeon Palghar, Taluka Health Officer, Dahanu, Medical Officers at Sub District Hospital, Dahanu, and Srimati Rachana Dalvi, Dr Dipak Abnave, ICMR-National Institute for Research in Reproductive Health (NIRRH), Mumbai, Maharashtra.
Footnotes
Financial support & sponsorship: This study was funded by the Department of Health Research, Ministry of Health & Family Welfare, Government of India and Tribal Health Research Forum of Indian Council of Medical Research (NIRRH/MS/RA/639/05-2018).
Conflicts of Interest: None.
References
- 1.Gutiérrez JM, Calvete JJ, Habib AG, Harrison RA, Williams DJ, Warrell DA. Snakebite envenoming. Nat Rev Dis Primers. 2017;3:17063. doi: 10.1038/nrdp.2017.63. [DOI] [PubMed] [Google Scholar]
- 2.Chippaux JP. Snake-bites: Appraisal of the global situation. Bull World Health Organ. 1998;76:515–24. [PMC free article] [PubMed] [Google Scholar]
- 3.Kasturiratne A, Wickremasinghe AR, de Silva N, Gunawardena NK, Pathmeswaran A, Premaratna R, et al. The global burden of snakebite: A literature analysis and modelling based on regional estimates of envenoming and deaths. PLoS Med. 2008;5:e218. doi: 10.1371/journal.pmed.0050218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mohapatra B, Warrell DA, Suraweera W, Bhatia P, Dhingra N, Jotkar RM, et al. Snakebite mortality in India: A nationally representative mortality survey. PLoS Negl Trop Dis. 2011;5:e1018. doi: 10.1371/journal.pntd.0001018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.World Health Organization. WHO guidelines for the production, control and regulation of snake antivenom immunoglobulins. WHO. 2018. [accessed on January 31, 2019]. Available from: http://www.who.int/bloodproducts/snake_antivenoms/snakeantivenomguide/en/
- 6.Pandey DP, Vohra R, Stalcup P, Shrestha BR. A season of snakebite envenomation: Presentation patterns, timing of care, anti-venom use, and case fatality rates from a hospital of Southcentral Nepal. J Venom Res. 2016;7:1–9. [PMC free article] [PubMed] [Google Scholar]
- 7.Narvencar K. Correlation between timing of ASV administration and complications in snake bites. J Assoc Physicians India. 2006;54:717–9. [PubMed] [Google Scholar]
- 8.World Health Organization. National snakebite management protocol. India: Directorate General of Health Services, Ministry of Health & Family Welfare, Government of India. 2009 [Google Scholar]
- 9.Warrell DA. New Delhi: World Health Organization Regional Office for South East Asia; 2010. Guidelines for the management of snake-bites. [Google Scholar]
- 10.New Delhi: Ministry of Health & Family Welfare, Government of India; 2017. National Health Mission. Standard Treatment Guidelines: Management of snake bite. [Google Scholar]
- 11.New Delhi: Ministry of Health & Family Welfare, Government of India; 2013. [accessed on December 31, 2018]. Department of Health Research. Establishment of Model Rural Health Research Units (MRHRU) in the States. Available from: https://dhr.gov.in/schemes/establishment-model-rural-health-research-units-states . [Google Scholar]
- 12.New Delhi: Ministry of Home Affairs, Government of India 2011; [accessed on December 20, 2018]. Office of the Registrar General & Census Commissioner, India. District Census HandBook - Maharashtra. Available from: http://censusindia.gov.in/2011census/dchb/DCHB_A/27/2721_PART_A_DCHB_THANE.pdf . [Google Scholar]
- 13.Asawale K, Katre R, Uike PS. Retrospective study of case profile amongst snakebite patients managed at a tertiary care center situated in a tribal district of Maharashtra during a span of three consecutive years. Int J Sci Res. 2018;7:45–7. [Google Scholar]
- 14.Ediriweera DS, Kasturiratne A, Pathmeswaran A, Gunawardena NK, Wijayawickrama BA, Jayamanne SF, et al. Mapping the risk of snakebite in Sri Lanka – A national survey with geospatial analysis. PLoS Negl Trop Dis. 2016;10:e0004813. doi: 10.1371/journal.pntd.0004813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rahman R, Faiz MA, Selim S, Rahman B, Basher A, Jones A, et al. Annual incidence of snake bite in rural Bangladesh. PLoS Negl Trop Dis. 2010;4:e860. doi: 10.1371/journal.pntd.0000860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mahmood MA, Halliday D, Cumming R, Thwin KT, Kyaw MMZ, White J, et al. Snakebite incidence in two townships in Mandalay division, Myanmar. PLoS Negl Trop Dis. 2018;12:e0006643. doi: 10.1371/journal.pntd.0006643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Pandey DP. Epidemiology of snakebite based on hospital survey in Chitwan and Nawalparasi districts, Nepal. J Nepal Health Res Counc. 2006;4:51–7. doi: 10.1007/BF03160933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kirte RC, Wahab SN, Bhathkule PR. Record based study of snake bite cases admitted at Shri Vasantrao Naik government medical college & hospital, Yavatmal (Maharashtra) Indian J Public Health. 2006;50:35–7. [PubMed] [Google Scholar]
- 19.Inamdar IF, Aswar NR, Ubaidulla M, Dalvi SD. Snakebite: Admissions at a tertiary health care centre in Maharashtra, India. S Afr Med J. 2010;100:456–8. doi: 10.7196/samj.3865. [DOI] [PubMed] [Google Scholar]
- 20.Sarkhel S, Ghosh R, Mana K, Gantait K. A hospital based epidemiological study of snakebite in Paschim Medinipur district, West Bengal, India. Toxicol Rep. 2017;4:415–9. doi: 10.1016/j.toxrep.2017.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hossain J, Biswas A, Rahman F, Mashreky SR, Dalal K, Rahman A. Snakebite epidemiology in Bangladesh – A national community based health and injury survey. Health. 2016;8:479–86. [Google Scholar]
- 22.Kasturiratne A, Pathmeswaran A, Fonseka MM, Lalloo DG, Brooker S, de Silva HJ. Estimates of disease burden due to land-snake bite in Sri Lankan hospitals. Southeast Asian J Trop Med Public Health. 2005;36:733–40. [PubMed] [Google Scholar]
- 23.Ghosh R, Mana K, Gantait K, Sarkhel S. A retrospective study of clinico-epidemiological profile of snakebite related deaths at a tertiary care hospital in Midnapore, West Bengal, India. Toxicol Rep. 2018;5:1–5. doi: 10.1016/j.toxrep.2017.11.008. [DOI] [PMC free article] [PubMed] [Google Scholar]