Abstract
Polycystic ovary syndrome (PCOS) is a common endocrine disorder predominantly affecting women of reproductive age. Clinical manifestations are diverse including hyperandrogenism, anovulation, infertility and increased risk of metabolic diseases besides psychosocial dysfunction. This review provides information on the problem of PCOS in India, its pathophysiology, genetics and an overview of current management options to instigate further research in this field. Prevalence of PCOS in India ranges from 3.7 to 22.5 per cent depending on the population studied and the criteria used for diagnosis. Abnormalities in leptin-adiponectin (adipocyte biology), oxidative stress and autoimmunity are among the mechanisms studied regarding pathogenesis of PCOS. Many candidate gene studies have shown associations with PCOS in various studies. Studies have consistently demonstrated the relationship between the well-known manifestation of hyperandrogenism among Indian PCOS women and the metabolic morbidities including insulin resistance, glucose intolerance and cardiovascular risk. Management of individual components of PCOS can be achieved by medications or surgical methods, though further clarification regarding pathogenesis of PCOS is needed to sharpen our therapeutic armamentarium.
Keywords: Epidemiology, genetics, India, management, pathogenesis, pathophysiology, polycystic ovary syndrome, prevalence
Introduction
Polycystic ovary syndrome (PCOS) is considered to be a multifaceted disease with a spectrum of manifestations affecting not only women of childbearing age, but also adolescents and postmenopausal women1. PCOS, by the nature of the disease, adversely influences the fertility and reproductive health of the affected women2; moreover, with its association with other lifestyle diseases, it is also the cause of significant cardiovascular and metabolic morbidity3. The exact aetiology and pathogenesis of PCOS are still an area of active research, although multiple hypotheses have been postulated, ranging from genetic susceptibility to environmental exposure, both in utero and in the postnatal life4. Data on the genetics, metabolic parameters and clinical aspects of PCOS in Indian women are available. This article was aimed at reviewing the literature related to the pathogenesis, epidemiology and genetics of PCOS in India, and biochemical and hormonal abnormalities in this disorder besides providing a brief overview of the management options.
Evolution of PCOS as a distinct syndrome - A historical overview
PCOS, discovered by Stein and Leventhal5, earned its name based on the ovarian morphology. The authors described seven women who shared the common features of menstrual disturbances, hirsutism and enlarged ovaries with many small follicles5. They also suspected that bilateral cystic ovaries were the result of abnormal hormonal stimulation, which was confirmed by the later investigators. Medical treatment became the preferred treatment over surgical resection of the ovaries when options such as clomiphene and follicle-stimulating hormone (FSH) became available6. There was a renewed interest in the surgical treatment of PCOS when laparoscopic treatment became popular. Newer technologies such as ultrasound to image ovaries were a breakthrough in the history of PCOS, and the ease of this technique made the diagnosis of PCOS simpler. However, this had the unexpected result that many women were diagnosed with mild or no other features of PCOS, but had polycystic ovaries7. This led to the term of polycystic ovarian morphology, the significance of which is still a subject of debate. It has been argued that the widespread acceptance of the Rotterdam criteria8, which included oligo-anovulatory women with polycystic ovarian morphology without clinical or biochemical evidence of hyperandrogenism, is premature and will lead to unnecessary diagnosis, laboratory evaluation and probably lifelong implications in these women9. Even after so many years of the recognition, the exact aetiology of this syndrome remains elusive and is now considered to be multifactorial, with a strong genetic component. Although insulin resistance (IR) is consistently found in women with PCOS, yet it is not included in any diagnostic criteria.
Clinical features, comorbidities and diagnostic criteria of PCOS
The clinical manifestations of PCOS include oligomenorrhoea, hirsutism, excessive acne and hair loss. In adolescence, it causes significant psychiatric disturbances such as anxiety and depression. PCOS is the leading cause of anovulatory infertility in women. The metabolic consequences include impaired glucose tolerance, type 2 diabetes, obesity and increased risk of cardiovascular diseases. Metabolic complications and increased cardiovascular morbidity were found to be more in the classic PCOS compared to other phenotypes, even after adjustment for obesity10. Clinicians now have these three sets of criteria (Table I) to choose from, though the Rotterdam criteria8 are found to be more preferred. The National Institutes of Health (NIH) Evidence-based Methodology Workshop in 2012 published the final report13 which stated that the following specific phenotypes (Table II) should be reported explicitly in all research studies.
Table I.
Diagnostic criteria of polycystic ovary syndrome (1990-2009)
| PCOS definition | Clinical hyperandrogenism or biochemical hyperandrogenism (elevated total/free testosterone) | Oligomenorrhoea or oligo-anovulation | Polycystic ovaries on ultrasound |
|---|---|---|---|
| NIH (1990)11 | Yes | Yes | Not included |
| ESHRE/ASRM Rotterdam (2003)8 2 of 3 criteria | Yes/no | Yes/no | Yes/no |
| AE-PCOS Society (2006)12 | Yes | Yes/no | Yes/no |
PCOS, polycystic ovary syndrome; AE, androgen excess; NIH, National Institutes of Health; ASRM, American Society for Reproductive Medicine; ESHRE, European Society of Human Reproduction and Embryology
Table II.
Phenotypes of polycystic ovary syndrome as per the Rotterdam criteria8
| Frank or classic polycystic | All the three - chronic anovulation, polycystic ovaries and hyperandrogenism |
| Classic non-cystic | Anovulation, hyperandrogenism with normal ovaries |
| Non-classic ovulatory | Regular menses, polycystic ovaries and hyperandrogenism |
| Non-classic mild or normo-androgenic | Anovulation, polycystic ovaries with normal androgens |
Epidemiology of PCOS in India
Only a few researchers have studied the prevalence of PCOS in India and among those, most of the sampling was convenience based, which might not reflect the true status of PCOS prevalence in the community. A pilot cross-sectional study conducted in Tamil Nadu assessed young adolescent females and found a prevalence of 18 per cent for PCOS14. They also concluded that the proportion of PCOS was higher in urban women in comparison to the rural women. A similar study conducted in Mumbai, which was an urban community-based study, found that the prevalence of PCOS was 22.5 per cent by the Rotterdam criteria and 10.7 per cent by the Androgen Excess Society criteria15. A study conducted among medical students at a private medical college in south India using the modified Cronin questionnaire16, which included 10 items, found that PCOS was a common disorder among the participants and reported a high incidence of mood disorders among them16. A study from Lucknow was published, in which college-going women with menstrual irregularity and hirsutism, in the age range of 18-25 yr, were studied, and it was reported that the calculated prevalence using the NIH criteria, among the participants, was only 3.7 per cent17. Another study from Andhra Pradesh studied young women from a residential college and found that 9.13 per cent of them satisfied the Rotterdam criteria for PCOS18. Vidya Bharathi et al19 showed that the prevalence of PCOS diagnosed by the Rotterdam criteria in community-dwelling women from rural and urban areas of Chennai was 6 per cent. International studies report the prevalence of PCOS to be in the range of 4-10 per cent of women of reproductive age20. As the prevalence of PCOS has been found to be higher or lower depending on the criteria used in these studies, which might be the obvious reason for the discrepancy in the prevalence rates among the studies from India, it is difficult to draw a clear conclusion. Hence, from the limited data available, it can be said that the prevalence of PCOS in India ranges from 3.7 to 22.5 per cent (Table III).
Table III.
Prevalence studies on polycystic ovary syndrome in Indian women/girls
| Study | n | Place/yr | Population/sampling | Prevalence per cent (criteria) |
|---|---|---|---|---|
| Balaji et al14 | 126 | Tamil Nadu/2015 | Young adolescents (12-19 yr) Urban and rural | 18 (Rotterdam)8 |
| Joshi et al15 | 600 | Mumbai/2014 | Adolescents and young adolescents (15-24 yr) Community based | 22.5 (Rotterdam)8 10.7 (AES)12 |
| Joseph et al16 | 441 | Karnataka/2016 | Medical and dental college students (20.4±1.5 yr) with either menstrual irregularity or hirsutism | 9.1 (modified version of Cronin questionnaire)16 |
| Gill et al17 | 1520 | Lucknow/2012 | College girls (18-25 yr) with menstrual irregularity and hirsutism | 3.7 (NIH criteria)11 |
| Nidhi et al18 | 460 | Bengaluru/2011 | College girls (15-18 yr) Oligomenorrhoea and/or hirsutism | 9.13 (Rotterdam)8 |
| Vidya Bharathi et al19 | Chennai/2017 | Random general rural and urban population | 6 (Rotterdam)8 |
AES, Androgen Excess Society
Pathophysiology and genetics of PCOS
PCOS is a disease with a complex multipronged pathogenesis which is still under investigation (Figure). The various pathogenetic mechanisms of PCOS include abnormal gonadotropin-releasing hormone (GnRH) regulation leading to increased luteinizing hormone (LH) and decreased FSH; decreased response of ovarian follicles to FSH; increased anti-Mullerian hormone (AMH); follicular arrest and increased secretion of testosterone, estradiol and dehydroepiandrosterone (DHEA). Obesity, especially abdominal fat deposition, is the major predisposing factor for the expression of IR and metabolic phenotype in PCOS22. Thus, IR at post-receptor level and adipocyte dysfunction are responsible for the metabolic consequences of PCOS21,22,23,24,25. Many other biochemical and hormonal aspects apart from the widely known pathophysiological mechanisms underlying PCOS have been studied by Indian researchers and are reviewed in detail below.
Figure.
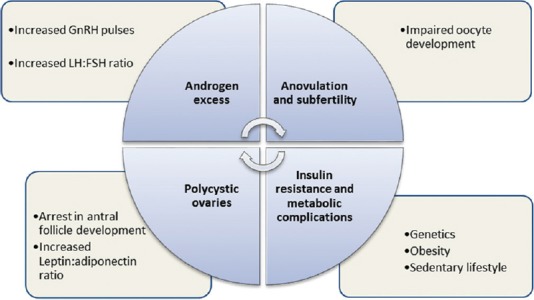
Current concept of pathophysiology of polycystic ovary syndrome. LH, luteinizing hormone; FSH, follicle-stimulating hormone; GnRH, gonadotropin-releasing hormone.
Source: Ref 21.
Studies on PCOS pathogenesis from India
Role of leptin and adiponectin in PCOS pathogenesis
Leptin is a major intermediary between nutritional status and reproductive health of women. High levels of leptin have been found to be associated with the markers of IR in PCOS patients24,26. After adjusting for potential confounders such as obesity status, PCOS women had higher leptin levels as compared to controls and leptin also was positively correlated with the serum testosterone levels27. Another study also demonstrated that high leptin in PCOS women was independent of the obesity status, but this study did not find a significant correlation between leptin levels and serum testosterone27. From these case-control studies, it is difficult to ascertain the cause and effect relationship between leptin levels and hyperandrogenemia or PCOS phenotype, though it is imperative that the complex nature of the same needs further exploration. Singh et al28 in a case-control study demonstrated lower serum adiponectin levels in women with PCOS as compared to controls. The adiponectin levels were lowest in obese women with PCOS and even non-obese PCOS women had low adiponectin, which improved with metformin treatment. Independent of obesity status, hypoadiponectinemia correlated with IR and hyperandrogenemia; this may be because lean PCOS women also may have intra-abdominal fat and thus unhealthy metabolic profile. Reiterating the role of adiponectin in PCOS pathogenesis, animal studies showed that adiponectin treatment reduced androgen synthesis in DHEA-treated PCOS mice in an in vitro study29. In another case-control study, plasma leptin:adiponectin ratio (L:A ratio) seemed to be positively associated with markers of metabolic syndrome and IR, thus reconfirming the lower adiponectin levels to be a potential biomarker of metabolic risk and IR in PCOS women30.
Evidence from proteomics and metabolomics studies
In large case-control study on the proteomics of follicular fluid from women with PCOS and controls undergoing in vitro fertilization (IVF) treatment found altered levels of proteins involved in extracellular matrix remodelling, complement coagulation cascade, fibrinolysis, vasculature development, angiogenesis, lipid transport and metabolism, and the authors postulated that it might reflect the molecular defects in folliculogenesis31. A study of the serum metabolomics of Indian women with PCOS during day 3 to 5 of their menstrual cycle using proton nuclear magnetic resonance and pattern recognition approach showed dysregulation in the expression of various metabolites in the serum of PCOS women, which indicated involvement of multiple pathways in amino acid metabolism, carbohydrate/lipid metabolism, purine and pyrimidine metabolism and protein synthesis32.
Role of oxidative stress and autoimmunity in PCOS pathogenesis
The role of oxidative stress in the pathogenesis of various reproductive diseases and conditions including infertility, recurrent abortions and pre-eclampsia has been postulated, and PCOS is no exception. Plasma amino acid levels were found to be significantly deranged (lower levels of methionine, cystine, isoleucine, phenylalanine, valine, tyrosine, proline, glycine, lysine and histidine and higher arginine and alanine levels) in PCOS women as compared to controls33, and the authors suggested this to be a marker of higher metabolic and oxidative stress in PCOS women. Reduced arginine bioavailability was found in PCOS women, which correlated with low nitric oxide levels, increased oxidative stress and thus lowered regulatory T cells (Treg cells) in patients with PCOS34. Krishna et al35 demonstrated for the first time that the immunosuppressive action of CD4+CD25+CD 127−Treg cells was reduced in PCOS, and this might influence the reproductive function of these women adversely. Sumithra et al36 studied the markers of oxidative stress and high sensitivity C-reactive protein levels (marker of cardiovascular risk), in patients with PCOS compared to controls, and found that both are significantly elevated in the PCOS cases. Deepika et al37 studied genomic instability and cytotoxicity due to oxidative stress, assessed by estimating the frequency of micronucleated cells in epithelial samples and serum malondialdehyde levels, respectively, and found a positive correlation in patients of PCOS as compared to controls, which suggested high oxidative stress in PCOS women. Other investigators have specifically demonstrated elevated oxidative stress markers in lean PCOS patients38. In oral contraceptive pill (OCP)-treated women, plasma intercellular adhesion molecule-1 (ICAM-1) and tumour necrosis factor-α (TNF-α) levels were significantly higher, compared to drug-naïve PCOS women, which suggested a pro-inflammatory state in the OCP-treated women, despite reduced androgen and regularized menstrual cycles39.
PCOS has long been suspected to have a component of autoimmune origin. Arora et al40 from New Delhi found higher prevalence of antithyroglobulin antibodies in PCOS women and suggested a possible role of autoimmunity in the pathogenesis of PCOS. A small case series of patients with both PCOS and Grave's disease also suggested a possible autoimmune aetiology of PCOS41.
Other mechanisms proposed to have a role in PCOS pathogenesis
Some studies have suggested a role of vitamin D deficiency in metabolic abnormalities seen in PCOS women, but many authors have opined that hypovitaminosis D is ubiquitous in India, and this does not seem to alter the metabolic phenotype in women with PCOS42,43. Altered mineral status in the form of hypercalcaemia and very low manganese levels in addition to higher levels of zinc and copper was demonstrated in women with PCOS compared to controls44, which led the authors to propose that altered trace mineral milieu might play a significant role in the pathogenesis of PCOS. The various metabolic, inflammatory and autoimmune components including the obesity-related cytokines and oxidative stress markers evaluated in relation to the pathogenesis of PCOS highlight the multifaceted nature of this disorder and the need for further research to better delineate the contribution of each of these markers and mediators in the final expression of the syndrome of PCOS.
Genetics in PCOS
The evidence that PCOS may be genetically determined initially came from twin studies, where the incidence of PCOS was twice as high in women with an affected twin as compared to the rest of population45. Candidate gene approach worldwide has identified many susceptibility genes including cytochrome P1A1 (CYP1A1), CYP11A, CYP17A1, CYP19, 17β-hydroxysteroid dehydrogenase (HSD17B6), androgen receptor (AR), sex hormone-binding globulin (SHBG), insulin receptor (INSR), insulin receptor substrate 1 (IRS1), peroxisome proliferator-activated receptor gamma (PPAR-γ), follicle stimulating hormone receptor (FSHR), luteinizing hormone/chorionic gonadotropin receptor (LHCGR), anti-Mullerian hormone receptor type 2 (AMHR2), interleukin (IL) IL-1A, IL-1B and IL-645, whereas genome-wide association studies have identified many susceptibility loci including THADA, DENND1A, LHCGR, FSHR, C9orf3, YAP1, GATA4,-NEIL2 and ERBB423,46.
Studies in the genetics of PCOS from India
Diabetes and metabolic syndrome-related genes
In a small study from Hyderabad, 15 single-nucleotide polymorphisms (SNPs) from nine type 2 diabetes-related genes (such as TCF7L2, IGF2BP2, SLC30A8, HHEX, CDKAL1, CDKN2A, IRS1, CAPN10 and PPAR-γ) were studied in PCOS women and controls; no significant association was found; the authors cited studies from other ethnic populations and suggested that the non-association might be universal47. Gly972Arg SNP of IRS1 was found to have a positive association with PCOS in a south Indian study population, whereas INS, IRS2, PPAR-γ and CAPN10 failed to show any association in the same study from Chennai48. Insulin receptor gene polymorphism was studied later49, for its association with IR in Indian women with PCOS; the study suggested that CC genotype (C1085T) might be developed as a marker for IR and metabolic complications in Indian women48. Pro12Ala polymorphism of PPAR-γ showed significant association with reduced susceptibility for PCOS in a study published from Mumbai50. The Calpain-10 (CAPN10) SNPs showed variable association with PCOS in the obese subgroup of patients51; the authors highlighted the importance of this gene in PCOS pathophysiology. The IRS-1 and PPAR-γ gene polymorphisms were found to have a probable protective role against the development of certain specific PCOS sub-phenotypes52. Angiotensin-converting enzyme (ACE) I/D polymorphism was found to be associated with an early age at onset of PCOS symptoms in a case-control study from Hyderabad53. A preliminary study on vitamin D receptor polymorphisms in PCOS patients and controls found no significant association, though some of the SNPs suggested a possible functional significance with regard to PCOS-specific clinical/biochemical traits54. In a study conducted by Yousuf et al55 among Kashmiri women with PCOS and controls, it was found that the ICAM 1 gene polymorphism was not significantly associated with PCOS women compared to controls.
Ovarian function-related gene polymorphisms
In a study to investigate the association of Connexin37/Gap junction alpha 4 gene C1019T SNP with the susceptibility to PCOS among south Indian women56, cases of PCOS were found to be significantly more associated with C/C and C alleles of the C1019T SNP, compared to the controls. Another study57 conducted among two ethnically different PCOS case-control groups has shown that 5,10 methylene tetrahydrofolate reductase (MTHFR) gene 677 CT polymorphism does not affect PCOS susceptibility in Indian women. The LHCGR gene polymorphism rs-2293275 was found to be significantly associated with PCOS compared to controls in a study58 from Hyderabad. Another study from Hyderabad59 suggested that vascular endothelial growth factor +405G/C polymorphism might constitute an inheritable risk factor for PCOS in south Indian women. Insulin-like factor 3 gene polymorphisms were studied among women from Mumbai60, and the authors showed a significant association between rs6523 polymorphism and increased risk of PCOS. Follistatin gene exons were amplified and studied61 for mutations in a large cohort of PCOS women and controls from south India; the authors found no significant role of follistatin gene variants in PCOS susceptibility. Androgen receptor CAG repeat length polymorphism was reported to have no significant association with PCOS in a case-control study62.
Oxidative stress and cytokine-related gene polymorphisms
Two polymorphisms (L55M and Q192R) of paraoxonase 1 (PON1) gene were studied for their association with PCOS susceptibility and related traits in Indian women from Mumbai63, and the authors found that one of those SNPs (L55M) was associated with reduced PCOS susceptibility only in lean women and that it also impacted features such as hyperandrogenemia, lipid parameters and glucose metabolism in these women. This led the authors to suggest that the genetic pathophysiology of PCOS was different in lean and obese women. In another study from south India64, IL 6174 G/C SNP was found to be significantly associated with PCOS risk. A case-control study from south India on the polymorphisms of TNF-α gene and found that the distribution of genotypes for rs1799964 was significantly different between the groups65. IL-β, IL-1Ra and FABP1 gene variants were found to be significantly associated with many metabolic features of PCOS66. Adiponectin and resistin gene polymorphisms were studied in south Indian women67; while it showed no association of the former with PCOS, the authors suggested that resistin gene variants might have a role in PCOS susceptibility. Another study from Hyderabad has shown that carriers of PPAR-γ coactivator 1α (PGC-1α) rs8192678 'Ser’ allele have increased risk of developing PCOS68.
Miscellaneous genes associated with PCOS
In a study from Hyderabad, CYP11A1 microsatellite (tttta)n repeat polymorphism was found to be more common in PCOS patients as compared to controls69, and the authors opined that because this cholesterol side-chain cleavage enzyme-encoding gene was instrumental in the synthesis of sex hormones, this could be a genetic marker of susceptibility to PCOS in the south Indian population studied. Leutinizing hormone β-subunit gene variants were studied among women70 with PCOS from south India; although the ones found to have significant correlation were silent in nature, the authors suggested exploration of other significant polymorphisms in the hypothalamic-pituitary-gonadal axis70. Plasminogen activator inhibitor 1 (PAI-1) 4G/5G polymorphism was found to be associated with risk for recurrent pregnancy loss and implantation failure25. Sagvekar et al71 showed that altered global DNA hypomethylation in peripheral blood lymphocytes and granulosa cells was strongly associated with PCOS and recommended larger studies to shed light on such epigenetic modifications in the PCOS susceptibility.
Candidate gene polymorphism studies involving genes related to diabetes, metabolic syndrome, oxidative stress, cytokines, ovarian function etc., have been conducted in the area of PCOS related genetic research in India. The limitations of candidate gene polymorphism studies in proving the association and the strength of the association need to be acknowledged. Genome-wide studies need to be planned in the future.
Clinical features and co-morbidities of PCOS
A clinical study72 reported that in PCOS subgroups, the phenotype with hyperandrogenism and regular menstrual cycles had higher IR and gonadotropic hormonal abnormalities compared to the subgroup which had patients with irregular menstruation. Another study demonstrated that hyperandrogenism, in the form of high testosterone values, correlated well with obesity and sleep-disordered breathing in PCOS women, and this might be one of the reasons for high cardiovascular morbidity in the PCOS patients73. Hyperandrogenic phenotypes of PCOS were found to be more prone to metabolic complications as compared to the phenotypes with normal androgen levels74.
PCOS occurs in both obese and non-obese women equally, although markers of IR are more common in obese women75. Acanthosis nigricans (AN) was found to be present in more than half of the PCOS women examined in a study conducted at Manipal, south India76. The authors described an association of AN with a family history of diabetes in first-degree relatives in all of these patients. Cardiovascular autonomic function was tested in women with PCOS in a study from south India, which showed an imbalance in the sympathovagal output in patients as compared to controls, and the authors suggested that the altered autonomic function might predispose these patients to cardiovascular morbidity77. The prevalence of abnormal glucose tolerance (AGT) detected by oral glucose tolerance test (OGTT) was found to be high (around 35%) in a large number of young Indian women with PCOS, and it was found that family history of diabetes was not a predictor of AGT in these women78. Thus, studies from India have consistently demonstrated the relationship between the well-known manifestation of hyperandrogenism among Indian PCOS women and the metabolic morbidities including IR, glucose intolerance and cardiovascular risk in this population.
Management of PCOS
The management of PCOS is as complex as the condition itself. The management and treatment of PCOS include a healthy diet, regular physical activity, and medications, which address the associated manifestations and co-morbidities. PCOS management strategies mainly aim at resolving the four major components of PCOS including regularity of menstrual periods, control of hyperandrogenism (acne and hirsutism), management of infertility and IR along with its associated risk factors (type 2 diabetes mellitus, hyperlipidaemia, and obesity). Both non-pharmacological and pharmacological management strategies are important in the overall management of PCOS.
Non-pharmacological measures
Studies on non-pharmacological measures to treat PCOS are very limited in the Indian literature. In a study on reproductive-age women with PCOS, improvement in novel inflammatory cardiac risk markers such as hs-CRP was reported with lifestyle modification, although metformin was also given to the study participants79.
Pharmacological treatment
In a randomized, single-blinded, dose-comparison study, Bhattacharya et al80 reported that OCP containing 20 μg ethinyl estradiol (EE) with drospirenone had similar effects on free androgen index in PCOS women as that containing 30 μg EE with drospirenone. The same authors had earlier studied81 a combination of EE with desogestrel and found significant improvement in hyperandrogenic parameters only during the first six months of treatment and further continuation was useless. A six-month, open-label, randomized trial by Ganie et al82, of low-dose spironolactone and metformin combination than either drug alone, showed the superiority of the former in terms of improved clinical parameters and compliance to treatment. A comparison of metformin and OCP (EE plus drospirenone) was done as a prospective observational study (n=46) over one year by Suvarna et al83, and metformin alone was found to be equally effective in regularizing menstrual cycles and treating hyperandrogenism in Indian women with PCOS. Use of non-hormonal options i.e., metformin and spironolactone, after a period of oral contraceptive use, was retrospectively studied by Kulshreshtha et al84, in a small group of women with PCOS for regularization of their menstrual cycles. They concluded that 75 per cent of women achieved regular cycles with non-hormonal treatment within one year of stopping OCPs. Saini et al85 have tried to develop metformin-loaded cationic nisosomes amalgamated with thermosensitive gel for intravaginal use in PCOS patients.
Treatment of complications
Infertility
Meenakumari et al86 studied the use of metformin in PCOS women with luteal-phase progesterone deficiency and reported improvement in the same after four weeks of treatment with metformin 500 mg thrice a day. A prospective randomized trial was conducted where letrozole and clomiphene citrate (CC) were compared in patients with PCOS and anovulatory infertility. After three cycles of treatment, both letrozole and clomiphene showed comparable ovulation rates, but endometrial response and pregnancy rates were better in the former group87. In a randomized trial comparing metformin and CC, where the primary outcome was live birth rate (LBR), Kar and Sanchita88 reported that the efficacy of metformin was similar to clomiphene in terms of LBR, and their combination gave the highest ovulation rate and LBR. Yanamandra and Gundabattula89 conducted a retrospective study of women who failed ovulation induction for primary infertility and hence underwent diagnostic laparoscopy and hysteroscopy followed by ovarian drilling. They showed an enhanced conception rate (around 50%) with laparoscopic ovarian drilling (LOD). In a small prospective cohort study, the author opined that LOD had no significant effect on AMH levels and thus ovarian reserve90. However, as Mitra et al91 pointed out, use of this treatment in unselected cases of PCOS was not prudent owing to its potential risks such as iatrogenic adhesions and ovarian insufficiency. Moreover, many authorities have questioned92 the utility of LOD in infertility treatment citing lack of significant rates of clinical pregnancy in evidence-based reviews. Considering the adverse effects of LOD, medical treatment with rosiglitazone and CC was compared with LOD and CC in women with PCOS suffering from infertility in a prospective randomized trial93, and the authors concluded that there was no significant difference in ovulation rate or pregnancy rate between the two groups. A retrospective analysis of four-year data at a tertiary care centre in north India was reported by Singh et al94 where PCOS patients undergoing IVF cycle with long GnRH agonist protocol were compared with those on fixed GnRH antagonist protocol, and there was no significant difference in pregnancy rate or incidence of ovarian hyperstimulation syndrome between the two groups.
Obesity, diabetes and other co-morbidities
Kumar and Arora95 reported the results of a randomized controlled trial (RCT) where they studied orlistat versus metformin for weight reduction and ovulation rates in obese PCOS women. Orlistat was equal to metformin in terms of achieving the outcomes of weight reduction and ovulation. They also noted that orlistat had a better side effect profile and was better tolerated than metformin in this trial population. In a retrospective study, the authors96 reported that in women with PCOS with AGT measured by OGTT, six-month therapy with spironolactone and metformin had similar effects in reducing the glucose levels.
Use of unconventional and supplemental pharmacological treatment in PCOS and its complications
Supplementation of vitamin D on insulin sensitivity/resistance parameters in PCOS women was studied by Garg et al97 in a double-blinded RCT, and they concluded that vitamin D at a dose of 4000 IU daily for six months had no significant effect on these parameters.
Conclusion
PCOS is a heterogeneous clinical syndrome with a multifaceted pathogenesis and is associated with lifelong morbidity. The clinical manifestations of PCOS include oligomenorrhoea, hirsutism, excessive acne and hair loss. The estimated prevalence in India ranged from 3.7 to 22.5 per cent. The prevalence of PCOS was found to be higher or lower depending on the criteria used, which might be the obvious reason for the discrepancy in the prevalence rates among the studies. Considering the vast diversity in the population of India, large-scale community-based studies using internationally accepted criteria, in various geographic regions, are necessary to shed light on the actual prevalence of this disorder. The various metabolic, inflammatory and autoimmune components including the obesity-related cytokines and oxidative stress markers in relation to the pathogenesis of PCOS highlight the multifaceted nature of the disorder and the need for further research into the subject to better delineate the contribution of each of these markers and mediators in the final expression of PCOS. Management and treatment of PCOS included healthy diet, regular physical activity, and medications, which address the associated manifestations and co-morbidities. More randomized trials are needed to find the best treatment options for Indian women suffering from this condition.
Footnotes
Financial support & sponsorship: None.
Conflicts of Interest: None.
References
- 1.Azziz R, Dumesic DA, Goodarzi MO. Polycystic ovary syndrome: An ancient disorder? Fertil Steril. 2011;95:1544–8. doi: 10.1016/j.fertnstert.2010.09.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Panda PK, Rane R, Ravichandran R, Singh S, Panchal H. Genetics of PCOS: A systematic bioinformatics approach to unveil the proteins responsible for PCOS. Genom Data. 2016;8:52–60. doi: 10.1016/j.gdata.2016.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Franks S, McCarthy MI, Hardy K. Development of polycystic ovary syndrome: Involvement of genetic and environmental factors. Int J Androl. 2006;29:278–85. doi: 10.1111/j.1365-2605.2005.00623.x. [DOI] [PubMed] [Google Scholar]
- 4.Goodarzi MO, Dumesic DA, Chazenbalk G, Azziz R. Polycystic ovary syndrome: Etiology, pathogenesis and diagnosis. Nat Rev Endocrinol. 2011;7:219–31. doi: 10.1038/nrendo.2010.217. [DOI] [PubMed] [Google Scholar]
- 5.Stein IF, Leventhal ML. Amenorrhea associated with bilateral polycystic ovaries. Am J Obstet Gynecol. 1935;29:181–91. [Google Scholar]
- 6.Wang CF, Gemzell C. The use of human gonadotropins for the induction of ovulation in women with polycystic ovarian disease. Fertil Steril. 1980;33:479–86. doi: 10.1016/s0015-0282(16)44711-4. [DOI] [PubMed] [Google Scholar]
- 7.Swanson M, Sauerbrei EE, Cooperberg PL. Medical implications of ultrasonically detected polycystic ovaries. J Clin Ultrasound. 1981;9:219–22. doi: 10.1002/jcu.1870090504. [DOI] [PubMed] [Google Scholar]
- 8.Rotterdam ESHRE/ASRM-Sponsored PCOS Consensus Workshop Group. Revised 2003 consensus on diagnostic criteria and long-term health risks related to polycystic ovary syndrome. Fertil Steril. 2004;81:19–25. doi: 10.1016/j.fertnstert.2003.10.004. [DOI] [PubMed] [Google Scholar]
- 9.Azziz R. Diagnostic criteria for polycystic ovary syndrome: A reappraisal. Fertil Steril. 2005;83:1343–6. doi: 10.1016/j.fertnstert.2005.01.085. [DOI] [PubMed] [Google Scholar]
- 10.Diamanti-Kandarakis E, Panidis D. Unravelling the phenotypic map of polycystic ovary syndrome (PCOS): A prospective study of 634 women with PCOS. Clin Endocrinol (Oxf) 2007;67:735–42. doi: 10.1111/j.1365-2265.2007.02954.x. [DOI] [PubMed] [Google Scholar]
- 11.Dunaif A, Givens J, Haseltine F, Merriam G. Boston: Blackwell Scientific Publications; 1992. The polycystic ovary syndrome. [Google Scholar]
- 12.Azziz R, Carmina E, Dewailly D, Diamanti-Kandarakis E, Escobar-Morreale HF, Futterweit W, et al. Positions statement: Criteria for defining polycystic ovary syndrome as a predominantly hyperandrogenic syndrome: An Androgen Excess Society guideline. J Clin Endocrinol Metab. 2006;91:4237–45. doi: 10.1210/jc.2006-0178. [DOI] [PubMed] [Google Scholar]
- 13.National Institutes of Health. Evidence-based methodology workshop on polycystic ovary syndrome. Bethesda, Maryland: NIH; 2012. [Google Scholar]
- 14.Balaji S, Amadi C, Prasad S, Bala Kasav J, Upadhyay V, Singh AK, et al. Urban rural comparisons of polycystic ovary syndrome burden among adolescent girls in a hospital setting in India. Biomed Res Int. 2015;2015:158951. doi: 10.1155/2015/158951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Joshi B, Mukherjee S, Patil A, Purandare A, Chauhan S, Vaidya R. A cross-sectional study of polycystic ovarian syndrome among adolescent and young girls in Mumbai, India. Indian J Endocrinol Metab. 2014;18:317–24. doi: 10.4103/2230-8210.131162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Joseph N, Reddy AG, Joy D, Patel V, Santhosh P, Das S, et al. Study on the proportion and determinants of polycystic ovarian syndrome among health sciences students in South India. J Nat Sci Biol Med. 2016;7:166–72. doi: 10.4103/0976-9668.184704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gill H, Tiwari P, Dabadghao P. Prevalence of polycystic ovary syndrome in young women from North India: A community-based study. Indian J Endocrinol Metab. 2012;16:S389–92. doi: 10.4103/2230-8210.104104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Nidhi R, Padmalatha V, Nagarathna R, Amritanshu R. Prevalence of polycystic ovarian syndrome in Indian adolescents. J Pediatr Adolesc Gynecol. 2011;24:223–7. doi: 10.1016/j.jpag.2011.03.002. [DOI] [PubMed] [Google Scholar]
- 19.Vidya Bharathi R, Swetha S, Neerajaa J, Varsha Madhavica J, Janani DM, Rekha SN, et al. An epidemiological survey: Effect of predisposing factors for PCOS in Indian urban and rural population. Middle East Fertil Soc J. 2017;22:313–6. [Google Scholar]
- 20.Azziz R, Woods KS, Reyna R, Key TJ, Knochenhauer ES, Yildiz BO, et al. The prevalence and features of the polycystic ovary syndrome in an unselected population. J Clin Endocrinol Metab. 2004;89:2745–9. doi: 10.1210/jc.2003-032046. [DOI] [PubMed] [Google Scholar]
- 21.Diamanti-Kandarakis E, Dunaif A. Insulin resistance and the polycystic ovary syndrome revisited: An update on mechanisms and implications. Endocr Rev. 2012;33:981–1030. doi: 10.1210/er.2011-1034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Pellatt L, Hanna L, Brincat M, Galea R, Brain H, Whitehead S, et al. Granulosa cell production of anti-Müllerian hormone is increased in polycystic ovaries. J Clin Endocrinol Metab. 2007;92:240–5. doi: 10.1210/jc.2006-1582. [DOI] [PubMed] [Google Scholar]
- 23.Chen ZJ, Zhao H, He L, Shi Y, Qin Y, Shi Y, et al. Genome-wide association study identifies susceptibility loci for polycystic ovary syndrome on chromosome 2p16.3, 2p21 and 9q33.3. Nat Genet. 2011;43:55–9. doi: 10.1038/ng.732. [DOI] [PubMed] [Google Scholar]
- 24.Nasrat H, Patra SK, Goswami B, Jain A, Raghunandan C. Study of association of leptin and insulin resistance markers in patients of PCOS. Indian J Clin Biochem. 2016;31:104–7. doi: 10.1007/s12291-015-0499-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mary MJ, Saravanan L, Deecaraman M, Vijayalakshmi M, Umashankar V, Sailaja J. Polymorphism of the PAI-1gene (4G/5G) may be linked with polycystic ovary syndrome and associated pregnancy disorders in South Indian women. Bioinformation. 2017;13:149–53. doi: 10.6026/97320630013149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Chakrabarti J. Serum leptin level in women with polycystic ovary syndrome: Correlation with adiposity, insulin, and circulating testosterone. Ann Med Health Sci Res. 2013;3:191–6. doi: 10.4103/2141-9248.113660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Pusalkar M, Meherji P, Gokral J, Savardekar L, Chinnaraj S, Maitra A. Obesity and polycystic ovary syndrome: Association with androgens, leptin and its genotypes. Gynecol Endocrinol. 2010;26:874–82. doi: 10.3109/09513590.2010.487586. [DOI] [PubMed] [Google Scholar]
- 28.Singh S, Akhtar N, Ahmad J. Plasma adiponectin levels in women with polycystic ovary syndrome: Impact of metformin treatment in a case-control study. Diabetes Metab Syndr. 2012;6:207–11. doi: 10.1016/j.dsx.2012.05.013. [DOI] [PubMed] [Google Scholar]
- 29.Singh A, Bora P, Krishna A. Direct action of adiponectin ameliorates increased androgen synthesis and reduces insulin receptor expression in the polycystic ovary. Biochem Biophys Res Commun. 2017;488:509–15. doi: 10.1016/j.bbrc.2017.05.076. [DOI] [PubMed] [Google Scholar]
- 30.Gupta V, Mishra S, Mishra S, Gupta VL. A ratio, insulin resistance and metabolic risk in women with polycystic ovarian syndrome. Diabetes Metab Syndr. 2017;11(Suppl 2):S697–701. doi: 10.1016/j.dsx.2017.05.001. [DOI] [PubMed] [Google Scholar]
- 31.Ambekar AS, Kelkar DS, Pinto SM, Sharma R, Hinduja I, Zaveri K, et al. Proteomics of follicular fluid from women with polycystic ovary syndrome suggests molecular defects in follicular development. J Clin Endocrinol Metab. 2015;100:744–53. doi: 10.1210/jc.2014-2086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.RoyChoudhury S, Mishra BP, Khan T, Chattopadhayay R, Lodh I, Datta Ray C. Serum metabolomics of Indian women with polycystic ovary syndrome using 1H NMR coupled with a pattern recognition approach. Mol Biosyst. 2016;12:3407–16. doi: 10.1039/c6mb00420b. [DOI] [PubMed] [Google Scholar]
- 33.Unni SN, Lakshman LR, Vaidyanathan K, Subhakumari KN, Menon NL. Alterations in the levels of plasma amino acids in polycystic ovary syndrome – A pilot study. Indian J Med Res. 2015;142:549–54. doi: 10.4103/0971-5916.171281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Krishna MB, Joseph A, Thomas PL, Dsilva B, Pillai SM, Laloraya M, et al. Impaired arginine metabolism coupled to a defective redox conduit contributes to low plasma nitric oxide in polycystic ovary syndrome. Cell Physiol Biochem. 2017;43:1880–92. doi: 10.1159/000484107. [DOI] [PubMed] [Google Scholar]
- 35.Krishna MB, Joseph A, Subramaniam AG, Gupta A, Pillai SM, Laloraya M. Reduced Tregs in peripheral blood of PCOS patients – A consequence of aberrant il2 signaling. J Clin Endocrinol Metab. 2015;100:282–92. doi: 10.1210/jc.2014-2401. [DOI] [PubMed] [Google Scholar]
- 36.Sumithra NU, Lakshmi RL, Leela Menon N, Subhakumari KN, Sheejamol VS. Evaluation of oxidative stress and hsCRP in polycystic ovarian syndrome in a tertiary care hospital. Indian J Clin Biochem. 2015;30:161–6. doi: 10.1007/s12291-014-0427-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Deepika MLN, Nalini S, Maruthi G, Ramchander V, Ranjith K, Latha KP, et al. Analysis of oxidative stress status through MN test and serum MDA levels in PCOS women. Pak J Biol Sci. 2014;17:574–7. doi: 10.3923/pjbs.2014.574.577. [DOI] [PubMed] [Google Scholar]
- 38.Desai V, Prasad NR, Manohar SM, Sachan A, Narasimha SRPVL, Bitla ARP. Oxidative stress in non-obese women with polycystic ovarian syndrome. J Clin Diagn Res. 2014;8:CC01–3. doi: 10.7860/JCDR/2014/8125.4530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Yousuf SD, Rashid F, Mattoo T, Shekhar C, Mudassar S, Zargar MA, et al. Does the oral contraceptive pill increase plasma intercellular adhesion molecule-1, monocyte chemoattractant protein-1, and tumor necrosis factor-α levels in women with polycystic ovary syndrome: A pilot study. J Pediatr Adolesc Gynecol. 2017;30:58–62. doi: 10.1016/j.jpag.2016.06.010. [DOI] [PubMed] [Google Scholar]
- 40.Arora S, Sinha K, Kolte S, Mandal A. Endocrinal and autoimmune linkage: Evidences from a controlled study of subjects with polycystic ovarian syndrome. J Hum Reprod Sci. 2016;9:18–22. doi: 10.4103/0974-1208.178636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Nisar S, Shah PA, Kuchay MS, Bhat MA, Rashid A, Ahmed S, et al. Association of polycystic ovary syndrome and Graves’ disease: Is autoimmunity the link between the two diseases. Indian J Endocrinol Metab. 2012;16:982–6. doi: 10.4103/2230-8210.103006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Kumar A, Barki S, Raghav V, Chaturvedi A, Kumar KVSH. Correlation of Vitamin D with metabolic parameters in polycystic ovarian syndrome. J Family Med Prim Care. 2017;6:115–9. doi: 10.4103/2249-4863.214985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Ganie MA, Marwaha RK, Nisar S, Farooqi KJ, Jan RA, Wani SA, et al. Impact of hypovitaminosis D on clinical, hormonal and insulin sensitivity parameters in normal body mass index polycystic ovary syndrome women. J Obstet Gynaecol. 2016;36:508–12. doi: 10.3109/01443615.2015.1103715. [DOI] [PubMed] [Google Scholar]
- 44.Chakraborty P, Ghosh S, Goswami SK, Kabir SN, Chakravarty B, Jana K. Altered trace mineral milieu might play an aetiological role in the pathogenesis of polycystic ovary syndrome. Biol Trace Elem Res. 2013;152:9–15. doi: 10.1007/s12011-012-9592-5. [DOI] [PubMed] [Google Scholar]
- 45.Kosova G, Urbanek M. Genetics of the polycystic ovary syndrome. Mol Cell Endocrinol. 2013;373:29–38. doi: 10.1016/j.mce.2012.10.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Hayes MG, Urbanek M, Ehrmann DA, Armstrong LL, Lee JY, Sisk R, et al. Genome-wide association of polycystic ovary syndrome implicates alterations in gonadotropin secretion in European ancestry populations. Nat Commun. 2015;6:7502. doi: 10.1038/ncomms8502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Reddy BM, Kommoju UJ, Dasgupta S, Rayabarapu P. Association of type 2 diabetes mellitus genes in polycystic ovary syndrome aetiology among women from Southern India. Indian J Med Res. 2016;144:400–8. doi: 10.4103/0971-5916.198678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Thangavelu M, Godla UR, Paul Solomon FD, Maddaly R. Single-nucleotide polymorphism of INS, INSR, IRS1, IRS2, PPAR-G and CAPN10 genes in the pathogenesis of polycystic ovary syndrome. J Genet. 2017;96:87–96. doi: 10.1007/s12041-017-0749-z. [DOI] [PubMed] [Google Scholar]
- 49.Gangopadhyay S, Agrawal N, Batra A, Kabi BC, Gupta A. Single-nucleotide polymorphism on exon 17 of insulin receptor gene influences insulin resistance in PCOS: A Pilot study on North Indian women. Biochem Genet. 2016;54:158–68. doi: 10.1007/s10528-015-9708-7. [DOI] [PubMed] [Google Scholar]
- 50.Shaikh N, Mukherjee A, Shah N, Meherji P, Mukherjee S. Peroxisome proliferator activated receptor gamma gene variants influence susceptibility and insulin related traits in Indian women with polycystic ovary syndrome. J Assist Reprod Genet. 2013;30:913–21. doi: 10.1007/s10815-013-0025-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Dasgupta S, Reddy BM. The role of epistasis in the etiology of polycystic ovary syndrome among Indian women: SNP-SNP and SNP-environment interactions. Ann Hum Genet. 2013;77:288–98. doi: 10.1111/ahg.12020. [DOI] [PubMed] [Google Scholar]
- 52.Dasgupta S, Sirisha P, Neelaveni K, Anuradha K, Sudhakar G, Reddy BM. Polymorphisms in the IRS-1 and PPAR-γ genes and their association with polycystic ovary syndrome among South Indian women. Gene. 2012;503:140–6. doi: 10.1016/j.gene.2012.04.060. [DOI] [PubMed] [Google Scholar]
- 53.Deepika MLN, Reddy KR, Rani VU, Balakrishna N, Latha KP, Jahan P. Do ACE I/D gene polymorphism serve as a predictive marker for age at onset in PCOS? J Assist Reprod Genet. 2013;30:125–30. doi: 10.1007/s10815-012-9906-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Dasgupta S, Dutta J, Annamaneni S, Kudugunti N, Battini MR. Association of Vitamin D receptor gene polymorphisms with polycystic ovary syndrome among Indian women. Indian J Med Res. 2015;142:276–85. doi: 10.4103/0971-5916.166587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Yousuf SD, Ganie MA, Zargar MA, Parvez T, Rashid F. The ICAM-1 gly241Arg polymorphism is not associated with polycystic ovary syndrome – results from a case control study in Kashmir, India. Asian Pac J Cancer Prev. 2016;17:1583–8. doi: 10.7314/apjcp.2016.17.3.1583. [DOI] [PubMed] [Google Scholar]
- 56.Guruvaiah P, Govatati S, Reddy TV, Beeram H, Deenadayal M, Shivaji S, et al. Analysis of connexin37 gene C1019T polymorphism and PCOS susceptibility in South Indian population: Case-control study. Eur J Obstet Gynecol Reprod Biol. 2016;196:17–20. doi: 10.1016/j.ejogrb.2015.11.002. [DOI] [PubMed] [Google Scholar]
- 57.Carlus SJ, Sarkar S, Bansal SK, Singh V, Singh K, Jha RK, et al. Is MTHFR 677 C and T polymorphism clinically important in polycystic ovarian syndrome (PCOS). A case-control study, meta-analysis and trial sequential analysis? PLoS One. 2016;11:e0151510. doi: 10.1371/journal.pone.0151510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Thathapudi S, Kodati V, Erukkambattu J, Addepally U, Qurratulain H. Association of luteinizing hormone chorionic gonadotropin receptor gene polymorphism (rs2293275) with polycystic ovarian syndrome. Genet Test Mol Biomarkers. 2015;19:128–32. doi: 10.1089/gtmb.2014.0249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Guruvaiah P, Govatati S, Reddy TV, Lomada D, Deenadayal M, Shivaji S, et al. The VEGF +405 G and C 5’ untranslated region polymorphism and risk of PCOS: A study in the South Indian women. J Assist Reprod Genet. 2014;31:1383–9. doi: 10.1007/s10815-014-0310-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Shaikh N, Dadachanji R, Meherji P, Shah N, Mukherjee S. Polymorphisms and haplotypes of insulin-like factor 3 gene are associated with risk of polycystic ovary syndrome in Indian women. Gene. 2016;577:180–6. doi: 10.1016/j.gene.2015.11.033. [DOI] [PubMed] [Google Scholar]
- 61.Dasgupta S, Pisapati SV, Kudugunti N, Kathragadda A, Godi S, Reddy MB, et al. Does follistatin gene have any direct role in the manifestation of polycystic ovary syndrome in Indian women? J Postgrad Med. 2012;58:190–3. doi: 10.4103/0022-3859.101386. [DOI] [PubMed] [Google Scholar]
- 62.Rajender S, Carlus SJ, Bansal SK, Negi MPS, Sadasivam N, Sadasivam MN, et al. Androgen receptor CAG repeats length polymorphism and the risk of polycystic ovarian syndrome (PCOS) PLoS One. 2013;8:e75709. doi: 10.1371/journal.pone.0075709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Dadachanji R, Shaikh N, Khavale S, Patil A, Shah N, Mukherjee S. PON1 polymorphisms are associated with polycystic ovary syndrome susceptibility, related traits, and PON1 activity in Indian women with the syndrome. Fertil Steril. 2015;104:207–16. doi: 10.1016/j.fertnstert.2015.03.037. [DOI] [PubMed] [Google Scholar]
- 64.Tumu VR, Govatati S, Guruvaiah P, Deenadayal M, Shivaji S, Bhanoori M. An interleukin-6 gene promoter polymorphism is associated with polycystic ovary syndrome in South Indian women. J Assist Reprod Genet. 2013;30:1541–6. doi: 10.1007/s10815-013-0111-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Deepika MLN, Reddy KR, Yashwanth A, Rani VU, Latha KP, Jahan P. TNF-α haplotype association with polycystic ovary syndrome – A South Indian study. J Assist Reprod Genet. 2013;30:1493–503. doi: 10.1007/s10815-013-0080-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Rashid N, Nigam A, Saxena P, Jain SK, Wajid S. Association of IL-1β, IL-1Ra and FABP1 gene polymorphisms with the metabolic features of polycystic ovary syndrome. Inflamm Res. 2017;66:621–36. doi: 10.1007/s00011-017-1045-3. [DOI] [PubMed] [Google Scholar]
- 67.Nambiar V, Vijesh VV, Lakshmanan P, Sukumaran S, Suganthi R. Association of adiponectin and resistin gene polymorphisms in South Indian women with polycystic ovary syndrome. Eur J Obstet Gynecol Reprod Biol. 2016;200:82–8. doi: 10.1016/j.ejogrb.2016.02.031. [DOI] [PubMed] [Google Scholar]
- 68.Reddy TV, Govatati S, Deenadayal M, Shivaji S, Bhanoori M. Polymorphisms in the TFAM and PGC1-α genes and their association with polycystic ovary syndrome among South Indian women. Gene. 2018;641:129–36. doi: 10.1016/j.gene.2017.10.010. [DOI] [PubMed] [Google Scholar]
- 69.Reddy KR, Deepika MLN, Supriya K, Latha KP, Rao SSL, Rani VU, et al. CYP11A1 microsatellite (tttta)n polymorphism in PCOS women from South India. J Assist Reprod Genet. 2014;31:857–63. doi: 10.1007/s10815-014-0236-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Dasgupta S, Sirisha PVS, Neelaveni K, Anuradha K, Sudhakar G, Reddy BM. Role of luteinizing hormone β-subunit gene variants among South Indian women with polycystic ovary syndrome. Gene. 2012;494:51–6. doi: 10.1016/j.gene.2011.11.054. [DOI] [PubMed] [Google Scholar]
- 71.Sagvekar P, Mangoli V, Desai S, Patil A, Mukherjee S. LINE1 CpG-DNA hypomethylation in granulosa cells and blood leukocytes is associated with PCOS and related traits. J Clin Endocrinol Metab. 2017;102:1396–405. doi: 10.1210/jc.2016-2645. [DOI] [PubMed] [Google Scholar]
- 72.Thathapudi S, Kodati V, Erukkambattu J, Katragadda A, Addepally U, Hasan Q. Anthropometric and biochemical characteristics of polycystic ovarian syndrome in South Indian women using AES-2006 criteria. Int J Endocrinol Metab. 2014;12:e12470. doi: 10.5812/ijem.12470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Suri J, Suri JC, Chatterjee B, Mittal P, Adhikari T. Obesity may be the common pathway for sleep-disordered breathing in women with polycystic ovary syndrome. Sleep Med. 2016;24:32–9. doi: 10.1016/j.sleep.2016.02.014. [DOI] [PubMed] [Google Scholar]
- 74.Kar S. Anthropometric, clinical, and metabolic comparisons of the four Rotterdam PCOS phenotypes: A prospective study of PCOS women. J Hum Reprod Sci. 2013;6:194–200. doi: 10.4103/0974-1208.121422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Ramanand SJ, Ghongane BB, Ramanand JB, Patwardhan MH, Ghanghas RR, Jain SS. Clinical characteristics of polycystic ovary syndrome in Indian women. Indian J Endocrinol Metab. 2013;17:138–45. doi: 10.4103/2230-8210.107858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Shivaprakash G, Basu A, Kamath A, Shivaprakash P, Adhikari P, Rathnakar UP, et al. Acanthosis nigricans in PCOS patients and its relation with type 2 diabetes mellitus and body mass at a tertiary care hospital in Southern India. J Clin Diagn Res. 2013;7:317–9. doi: 10.7860/JCDR/2013/4930.2756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Saranya K, Pal GK, Habeebullah S, Pal P. Assessment of cardiovascular autonomic function in patients with polycystic ovary syndrome. J Obstet Gynaecol Res. 2014;40:192–9. doi: 10.1111/jog.12154. [DOI] [PubMed] [Google Scholar]
- 78.Ganie MA, Dhingra A, Nisar S, Sreenivas V, Shah ZA, Rashid A, et al. Oral glucose tolerance test significantly impacts the prevalence of abnormal glucose tolerance among Indian women with polycystic ovary syndrome: Lessons from a large database of two tertiary care centers on the Indian subcontinent. Fertil Steril. 2016;105:194–2010. doi: 10.1016/j.fertnstert.2015.09.005. [DOI] [PubMed] [Google Scholar]
- 79.Rajagopal G, Reddy AP, Venkata Harinarayan C, Suresh V, Bitla A, Rao SPVLN, et al. Effect of lifestyle modification and metformin therapy on emerging cardiovascular risk factors in overweight Indian women with polycystic ovary syndrome. Metab Syndr Relat Disord. 2012;10:273–9. doi: 10.1089/met.2011.0127. [DOI] [PubMed] [Google Scholar]
- 80.Bhattacharya SM, Jha A, DasMukhopadhyay L. Comparison of two contraceptive pills containing drospirenone and 20 μg or 30 μg ethinyl estradiol for polycystic ovary syndrome. Int J Gynaecol Obstet. 2016;132:210–3. doi: 10.1016/j.ijgo.2015.06.065. [DOI] [PubMed] [Google Scholar]
- 81.Bhattacharya SM, Ghosh M, Basu R. Effects of ethinyl estradiol and desogestrel on clinical and metabolic parameters in Indian patients with polycystic ovary syndrome. J Obstet Gynaecol Res. 2012;38:285–90. doi: 10.1111/j.1447-0756.2011.01682.x. [DOI] [PubMed] [Google Scholar]
- 82.Ganie MA, Khurana ML, Nisar S, Shah PA, Shah ZA, Kulshrestha B, et al. Improved efficacy of low-dose spironolactone and metformin combination than either drug alone in the management of women with polycystic ovary syndrome (PCOS): A six-month, open-label randomized study. J Clin Endocrinol Metab. 2013;98:3599–607. doi: 10.1210/jc.2013-1040. [DOI] [PubMed] [Google Scholar]
- 83.Suvarna Y, Maity N, Kalra P, Shivamurthy MC. Comparison of efficacy of metformin and oral contraceptive combination of ethinyl estradiol and drospirenone in polycystic ovary syndrome. J Turk Ger Gynecol Assoc. 2016;17:6–9. doi: 10.5152/jtgga.2016.16129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Kulshreshtha B, Arora A, Pahuja I, Sharma N, Pant S. Menstrual cyclicity post OC withdrawal in PCOS: Use of non-hormonal options. J Obstet Gynaecol. 2016;36:833–8. doi: 10.3109/01443615.2016.1159667. [DOI] [PubMed] [Google Scholar]
- 85.Saini N, Sodhi RK, Bajaj L, Pandey RS, Jain UK, Katare OP, et al. Intravaginal administration of metformin hydrochloride loaded cationic niosomes amalgamated with thermosensitive gel for the treatment of polycystic ovary syndrome: In vitro and in vivo studies. Colloids Surf B Biointerfaces. 2016;144:161–9. doi: 10.1016/j.colsurfb.2016.04.016. [DOI] [PubMed] [Google Scholar]
- 86.Meenakumari KJ, Agarwal S, Krishna A, Pandey LK. Effects of metformin treatment on luteal phase progesterone concentration in polycystic ovary syndrome. Braz J Med Biol Res. 2004;37:1637–44. doi: 10.1590/s0100-879x2004001100007. [DOI] [PubMed] [Google Scholar]
- 87.Roy KK, Baruah J, Singla S, Sharma JB, Singh N, Jain SK, et al. A prospective randomized trial comparing the efficacy of letrozole and clomiphene citrate in induction of ovulation in polycystic ovarian syndrome. J Hum Reprod Sci. 2012;5:20–5. doi: 10.4103/0974-1208.97789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Kar S, Sanchita S. Clomiphene citrate, metformin or a combination of both as the first line ovulation induction drug for Asian Indian women with polycystic ovarian syndrome: A randomized controlled trial. J Hum Reprod Sci. 2015;8:197–201. doi: 10.4103/0974-1208.170373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Yanamandra NK, Gundabattula SR. Outcome of ovarian drilling in women with polycystic ovary syndrome. J Clin Diagn Res. 2015;9:QC01–3. doi: 10.7860/JCDR/2015/8001.5586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Paramu S. Impact of laparoscopic ovarian drilling on serum anti-Mullerian hormone levels in patients with anovulatory polycystic ovarian syndrome. Turk J Obstet Gynecol. 2016;13:203–7. doi: 10.4274/tjod.97523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Mitra S, Nayak PK, Agrawal S. Laparoscopic ovarian drilling: An alternative but not the ultimate in the management of polycystic ovary syndrome. J Nat Sci Biol Med. 2015;6:40–8. doi: 10.4103/0976-9668.149076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Allahbadia GN. Primum non nocere. J Obstet Gynaecol India. 2016;66:71–5. doi: 10.1007/s13224-015-0799-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Roy KK, Baruah J, Sharma A, Sharma JB, Kumar S, Kachava G, et al. A prospective randomized trial comparing the clinical and endocrinological outcome with rosiglitazone versus laparoscopic ovarian drilling in patients with polycystic ovarian disease resistant to ovulation induction with clomiphene citrate. Arch Gynecol Obstet. 2010;281:939–44. doi: 10.1007/s00404-009-1305-8. [DOI] [PubMed] [Google Scholar]
- 94.Singh N, Naha M, Malhotra N, Lata K, Vanamail P, Tiwari A, et al. Comparison of gonadotropin-releasing hormone agonist with GnRH antagonist in polycystic ovary syndrome patients undergoing in vitro fertilization cycle: Retrospective analysis from a tertiary center and review of literature. J Hum Reprod Sci. 2014;7:52–7. doi: 10.4103/0974-1208.130852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Kumar P, Arora S. Orlistat in polycystic ovarian syndrome reduces weight with improvement in lipid profile and pregnancy rates. J Hum Reprod Sci. 2014;7:255–61. doi: 10.4103/0974-1208.147492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Kulshreshtha B, Gupta N, Ganie MA, Ammini AC. Effect of metformin and spironolactone therapy on OGTT in patients with polycystic ovarian syndrome – A retrospective analysis. Gynecol Endocrinol. 2012;28:823–6. doi: 10.3109/09513590.2012.671394. [DOI] [PubMed] [Google Scholar]
- 97.Garg G, Kachhawa G, Ramot R, Khadgawat R, Tandon N, Sreenivas V, et al. Effect of Vitamin D supplementation on insulin kinetics and cardiovascular risk factors in polycystic ovarian syndrome: A pilot study. Endocr Connect. 2015;4:108–16. doi: 10.1530/EC-15-0001. [DOI] [PMC free article] [PubMed] [Google Scholar]


