Abstract
Smooth muscle hamartomas are benign dermal proliferations of smooth muscle cells. Smooth muscle hamartomas are sub-divided into congenital or acquired; the latter is a rare entity with less than 20 cases being reported in the English literature. Most often asymptomatic, acquired smooth muscle hamartomas follow an indolent course. Treatment in the form of surgical excision can be utilized for symptomatic or cosmetic purposes. Here, we report the first case of an acquired smooth muscle hamartomas of the shin which also uniquely presented with hidrosis. This case highlights the varied clinical spectrum of acquired smooth muscle hamartomas.
Keywords: Hamartoma, general dermatology, smooth muscle
Introduction
Smooth muscle hamartomas (SMHs) are benign dermal proliferations of smooth muscle cells. SMHs are sub-divided into congenital or acquired; the latter is a rare entity with less than 20 cases being reported in the English literature. Here, we report the first case of an acquired smooth muscle hamartoma (ASMH) of the shin which also uniquely presented with hidrosis.
Case report
A 29-year-old female presented to the dermatology clinic for a 6-year history of a painful, sweaty lesion to her left shin. This lesion appeared after minor, incidental trauma to the site. It did not undergo any growth or evolutionary changes. The patient was otherwise healthy and her family history was non-contributory. On examination, she had a 7-cm firm, sclerotic, immobile circular plaque with a central cluster of verrucous skin-coloured papules and a 1-cm border of hyperpigmentation (Figure 1). The lesion exhibited hidrosis and had a negative pseudo-Darier’s sign.
Figure 1.
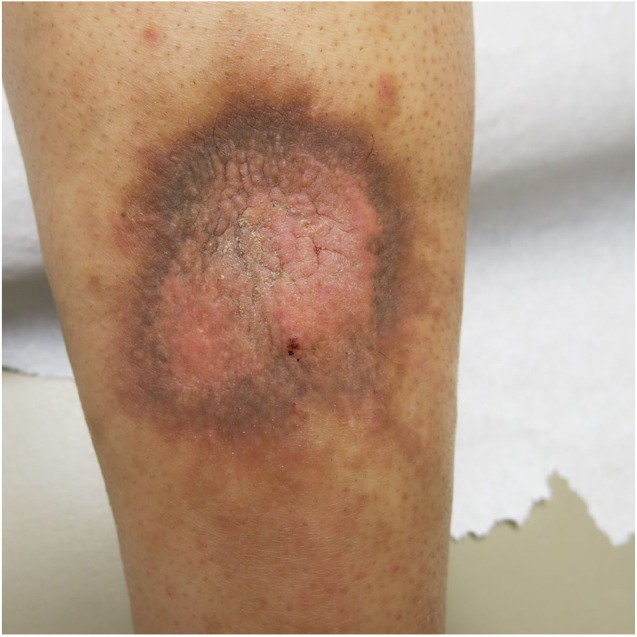
On the left shin, there is a 7-cm firm, sclerotic, immobile circular plaque with a central cluster of verrucous skin-coloured papules and a 1-cm border of hyperpigmentation. Hidrosis is present at the inferior aspect of the lesion.
A punch biopsy demonstrated the following: haphazardly arranged smooth muscle bundles throughout the reticular dermis, sclerotic intervening dermis, small collapsed blood vessels with mild perivascular lymphocytic infiltrate and lack of hair follicles, cytologic atypia, hypercellularity, necrosis or mitoses (Figure 2). The desmin stain was positive, thus confirming a diagnosis of a smooth muscle hamartoma.
Figure 2.

At 2× magnification, histopathological analysis reveals haphazardly arranged smooth muscle bundles throughout the reticular dermis, sclerotic intervening dermis and small collapsed blood vessels with mild perivascular lymphocytic infiltrate.
Discussion
Smooth muscle is an important physiologically active component of the body. It is distributed in the gastrointestinal, genitourinary and respiratory tracts. Within the skin, smooth muscle cells are located in arrector pili muscles, blood vessel walls and genital skin (scrotum, vulva and nipple).1
SMHs are comprised of benign dermal proliferations of smooth muscle cells. SMHs are sub-divided into congenital or acquired. ASMHs are rare with less than 20 cases being reported in the English literature.2
In a review of the published biopsy-proven cases of ASMH, Jain et al.2 found that the age of presentation ranged between 12 and 64 years. In addition, reported sites for ASMH include the scalp, upper extremity (upper arm, forearm and shoulder), chest and genitalia (scrotum, penis and labia majora). Our patient did not align with this trend: while two ASMHs have been previously reported in the foot,3,4 our patient is the first reported case of ASMH in the shin.
ASMH clinically presents as a solitary, often indurated plaque which may have superimposed small papules. Jain et al.2 reported a case of ASMH which presented as multiple lesions on the scalp. As demonstrated by our patient, associated hyperpigmentation and hypertrichosis are not common with ASMH compared with congenital SMH.2 Transient elevation or pilo-erection induced by rubbing is referred to as pseudo-Darier sign; it is a characteristic finding for congenital SMH.1 Pseudo-Darier sign is usually negative in ASMH.2 While most lesions are asymptomatic, pain and pruritus have been reported with ASMH.3,5 To our knowledge, this is the first case of ASMH to be present along with hidrosis.
The histopathologic hallmark of SMH is an increase in well-defined, variably oriented smooth bundles in the dermis.1 There can be extension into the subcutaneous tissue or involve the hair follicles.
Treatment is not necessary, given the benign nature of ASMH.1 However, if desired for symptom control or cosmesis, surgical excision can be utilized.1
This case of ASMH is different from previous reports for two reasons: anatomic location of the lesion (shin) and associated symptom of hidrosis. ASMH is a rare entity and this case adds to its varied clinical spectrum.
Acknowledgments
The authors thank dermatopathologist Dr Amy Thommasen, MD FRCPC for her medical expertise in diagnosis and for providing the above histopathology image.
Footnotes
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship and/or publication of this article.
Informed consent: Consent was obtained from the patient for publication of the images and the case report.
References
- 1. Holst VA, Junkins-Hopkins JM, Elenitsas R. Cutaneous smooth muscle neoplasms: clinical features, histologic findings, and treatment options. J Am Acad Dermatol 2002; 46(4): 477–90; quiz 491. [DOI] [PubMed] [Google Scholar]
- 2. Jain S, Patro S, Darkase B, et al. Multiple acquired smooth muscle hamartomas with thick-walled blood vessels on scalp. J Cutan Pathol 2018; 45(8): 629–632. [DOI] [PubMed] [Google Scholar]
- 3. Lee D, Kim SH, Hong SK, et al. A case of acquired smooth muscle hamartoma on the sole. Ann Dermatol 2009; 21(1): 78–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Desai C, Sheth P, Patil S. Acquired smooth muscle hamartoma of foot: a rare entity. Indian Dermatol Online J 2017; 8(6): 505–507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Kwon KS, Lee CW, Seo KH, et al. Acquired vulvar smooth muscle hamartoma: a case report and review of the literature. J Dermatol 2000; 27(1): 56–59. [DOI] [PubMed] [Google Scholar]


