Short abstract
The canal of Nuck, caused by the failed closure of the processus vaginalis in the female, is the continued outpouching of parietal peritoneum through the inguinal canal to the labia majora. Disorders of the canal of Nuck include hernia and hydrocele. Some canal of Nuck hernias, especially of the ovary, may result in emergent complications such as incarceration, strangulation, and ovarian torsion. Knowledge of canal of Nuck disorders and prompt diagnosis are important to avoid serious complications. Imaging, especially ultrasound, is essential for timely diagnosis, leading to appropriate management and better patient care.
Keywords: Canal of Nuck, inguinal hernia
Introduction
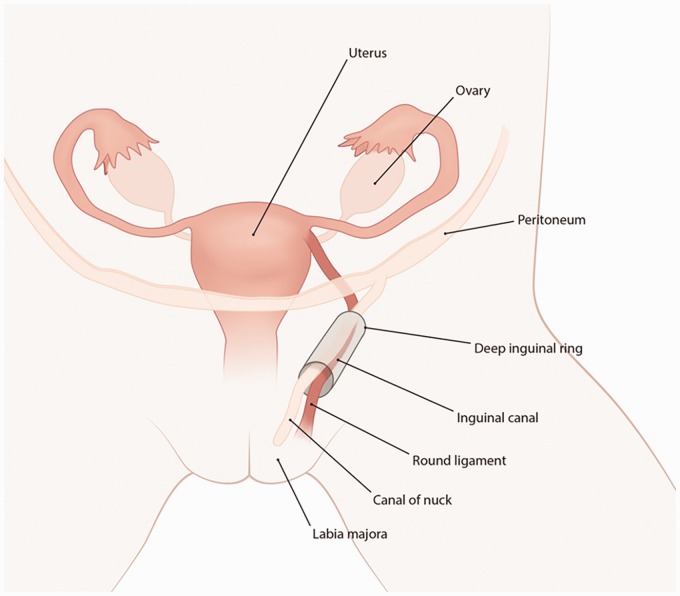
Pediatric inguinal hernias in infants and young children and have a reported incidence in the range of 0.8%–4.4% in the pediatric population (1). They are relatively uncommon in girls, who are affected 6–10 times less frequently compared to boys (1,2). The canal of Nuck represents the continued outpouching of parietal peritoneum through the inguinal canal to the labia majora and may result in an indirect hernia and/or hydrocele as shown in Fig. 1 (3,4). Canal of Nuck hernias often contain bowel and peritoneal fat and are treated with non-urgent, planned surgery (3,4). However, herniation of organs such as ovaries may lead to incarceration, strangulation, and ovarian torsion which are serious complications that require emergent surgery (5). Ultrasound with a high-frequency transducer is the preferred modality for initial imaging (5). Because canal of Nuck hernias are rare but may result in serious complications, it is important to describe the clinical presentation and radiographic findings for prompt diagnosis and management.
Fig. 1.
Illustration of the canal of Nuck.
Cases
Case 1
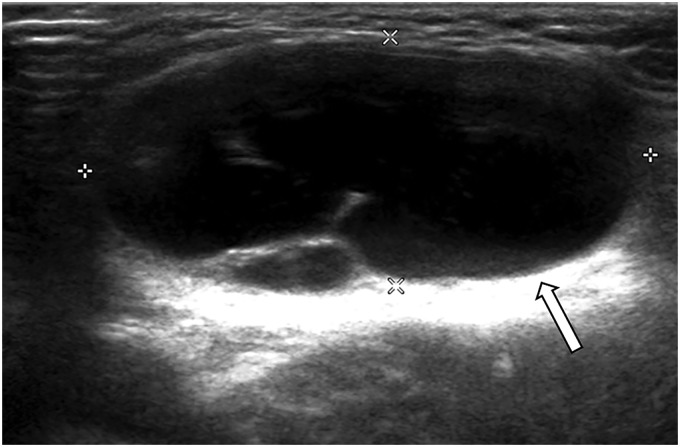
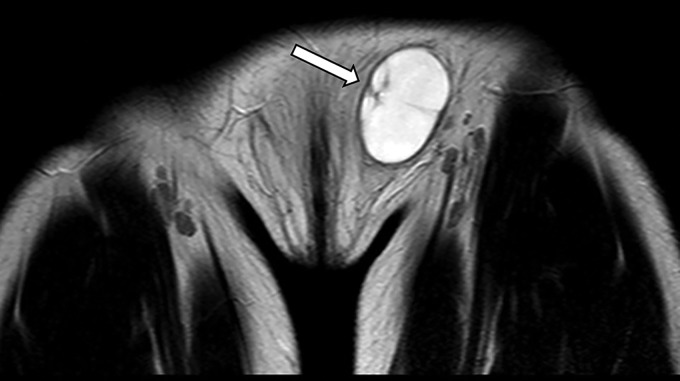
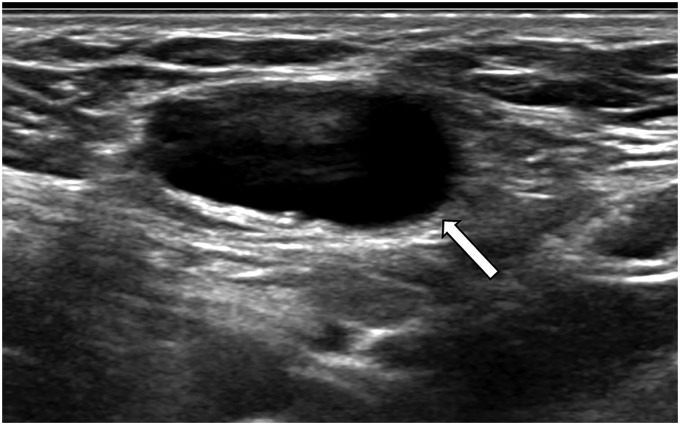
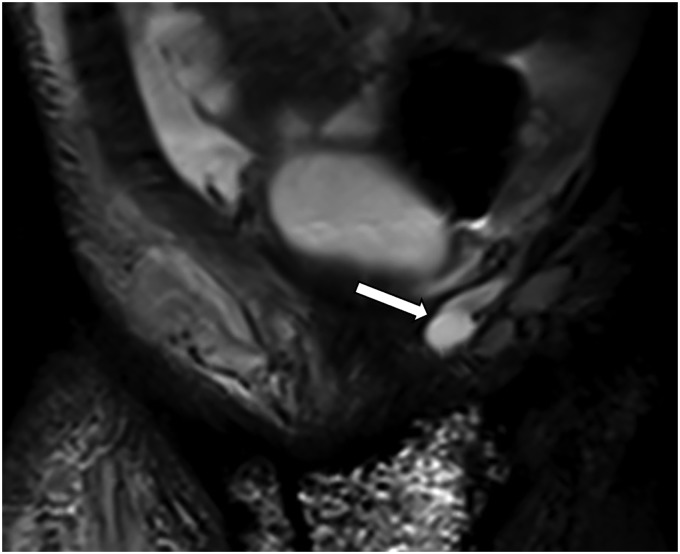
A six-year-old girl presented with minimally tender left groin swelling. Ultrasound demonstrated a well-circumscribed cystic structure in the subcutaneous tissues of the left groin with thin internal septations (Fig. 2). A follow-up MRI (shown is a coronal T2-weighted image of the pelvis) obtained confirmed the diagnosis of canal of Nuck hydrocele (Fig. 3). The protocol utilized to evaluate this groin mass is described in Table 1.
Fig. 2.
Ultrasound of the left groin in a six-year-old girl demonstrates a loculated hydrocele in the canal of Nuck (arrow).
Fig. 3.
Coronal T2-weighted image of the pelvis in a six-year-old girl confirms the left canal of Nuck hydrocele (arrow).
Table 1.
Abbreviated pelvic MRI protocol for canal of Nuck pathology.
| Axial sequences | Coronal sequences |
|---|---|
| STIR | T1-weighted |
| Diffusion-weighted | STIR or T2-weighted |
STIR, short T1 inversion recovery.
Case 2
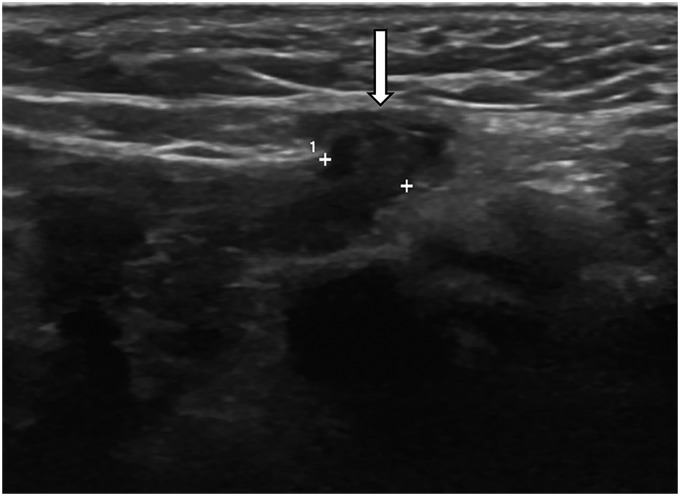
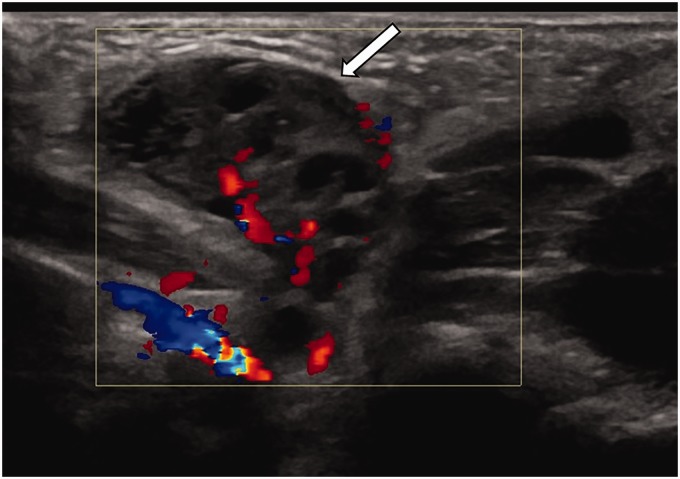
A 51-day-old girl presented with left groin swelling. Ultrasound demonstrated a partial bowel loop protruding through an abdominal wall defect consistent with bowel herniation into the canal of Nuck (Fig. 4).
Fig. 4.
Ultrasound of the left groin in a 51-day-old girl depicts bowel in the canal of Nuck (arrow).
Case 3
A four-year-old girl presented with a transient lump in her right groin. An ultrasound was initially negative, but with Valsalva, a small loop of bowel protruded into the canal of Nuck (Fig. 5).
Fig. 5.
Ultrasound of the right groin in a four-year-old girl during Valsalva shows bowel within the canal of Nuck (arrow).
Case 4
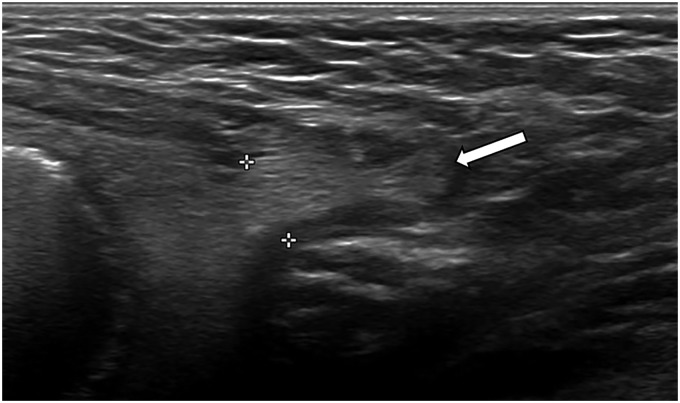
A three-month-old girl was referred for ultrasound evaluation of a left inguinal hernia which was appreciable on physical exam. Ultrasound showed that the uterus and one of the ovaries was visible within the canal of Nuck (Fig. 6).
Fig. 6.
Ultrasound of the left groin in a three-month-old girl reveals the uterus (white arrow) and left ovary (black arrow) in the left canal of Nuck.
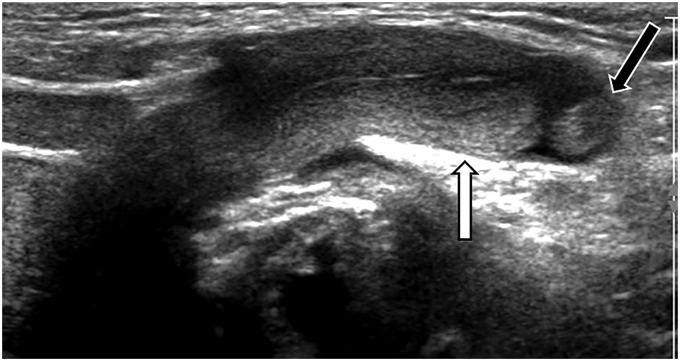
Case 5
A 48-day-old girl who presented with a lump in her left groin underwent ultrasound. The left ovary was present within the left canal of Nuck (Fig. 7).
Fig. 7.
Ultrasound of the left groin in a 48-day-old girl demonstrates an ovary in the left canal of Nuck (arrow).
Case 6
A 13-day-old girl received an ultrasound for a right labial lump. Ultrasound revealed the right ovary within the canal of Nuck (Fig. 8). Ovarian follicles were visible which is typical in the newborn period.
Fig. 8.
Ultrasound of the right groin in a 13-day-old girl depicts the right ovary within the right canal of Nuck (arrow).
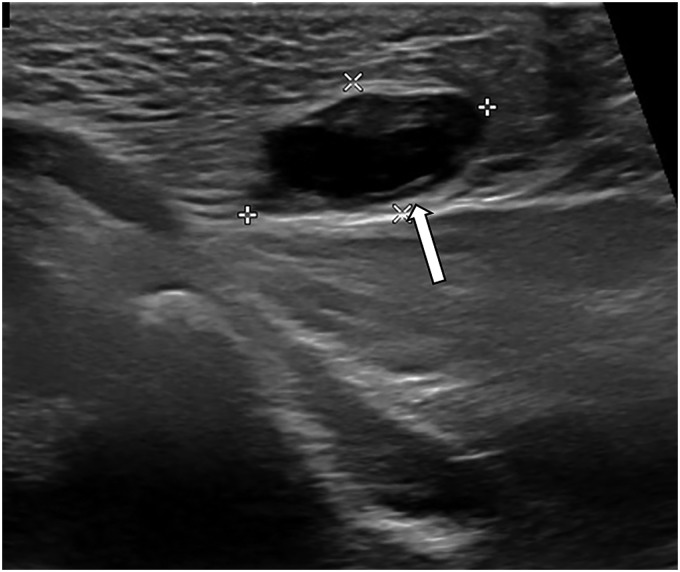
Case 7
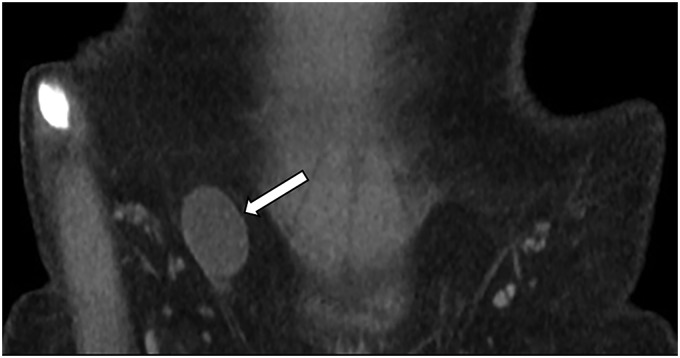
A 12-year-old girl underwent ultrasound for a right groin mass which showed the right ovary within the canal of Nuck (Fig. 9). A coronal reformat of a computed tomography (CT) scan performed subsequently also depicted the right ovary within the canal of Nuck (Fig. 10).
Fig. 9.
Ultrasound of the right groin in a 12-year-old girl shows the right ovary within the right canal of Nuck (arrow).
Fig. 10.
Coronal reformatted image from a CT of the pelvis in a 12-year-old girl confirms the right ovary within the right canal of Nuck (arrow).
Case 8
Magnetic resonance imaging (MRI) of the pelvis was requested for a two-year-old girl with concern for a septic right hip. The MRI revealed a hydrocele in the left canal of Nuck (Fig. 11).
Fig. 11.
Coronal short-T1 inversion recovery MRI of the pelvis reveals a hydrocele in the left canal of Nuck (arrow).
Discussion
Embryologically, the processus vaginalis represents an outpouching of the parietal peritoneum that becomes apparent during the 12th week of gestation. Canal of Nuck abnormalities arise when the processus vaginalis remains patent in girls. Obliteration of the processus vaginalis normally occurs from the seventh month of gestation to one year of age, and canal of Nuck hernias present most often in girls aged < 5 years but have been reported in girls aged as old as 11 years (5,6). Because obliteration of the processus vaginalis begins during gestation, canal of Nuck and other inguinal hernias are associated with prematurity and may occur in 9%–11% of infants born prematurely (7). A study of 92,308 children found that inguinal hernias may be associated with lung disease and mechanical ventilation, which may be explained by the increase in intraabdominal pressure present in these situations (8).
The processus vaginalis normally closes in a craniocaudal direction, starting superiorly and ending inferiorly (6). If only the inferior part of the processus vaginalis remains patent, an encysted hydrocele may form (6). An entirely patent processus vaginalis is referred to as the canal of Nuck and may result in a communicating hydrocele or herniation of organs, most commonly the bowel and ovary (4,6). Based on autopsy data of adults of both sexes, herniation is found in 15%–30% of patients with a patent processus vaginalis (9). As the deep inguinal ring is at the superior end of the canal of Nuck and lateral to the inferior epigastric vessels, the canal of Nuck hernia is classified as an indirect hernia (10).
Herniation of other organs has been less commonly described in the literature. Herniation of the uterus with the ovary has been reported in at least nine pediatric patients, all aged <1 year, with concomitant herniation of the fallopian tube in eight of these nine patients (11–17). While herniation of one ovary and fallopian tube is more common, there have been three reported cases of left-sided herniation of both adnexa (11,12,16). Herniation of the bladder has been described in one adult patient (18).
Inguinal hernias more frequently occur on the right side as the sigmoid colon may help prevent herniation through the left deep inguinal ring (4). Because canal of Nuck hernias are uncommon, no prospective data have been collected. However, in the two retrospective studies consisting solely of canal of Nuck hernias, 31/55 (56%) cases were right-sided, and 2 (4%) cases were bilateral (3,5). Bilateral inguinal hernias are more common in female patients and in patients born prematurely (19,20).
Incarceration, in which the herniated structure is trapped in the canal of Nuck and cannot be readily reduced to its original location, occurs more often when there is herniation of an ovary and in younger patients, though prematurity is not clearly associated with incarceration. Incarceration has been reported in up to 43% of inguinal hernias involving an ovary, perhaps because a herniated edematous ovary is less compressible than herniated bowel (1,21). In a study of 79,794 children, the rate of incarceration decreased as age increased (20). While some studies have reported a positive or negative association between prematurity and incarceration, two studies found no relationship (8,20,22,23).
Canal of Nuck hernias may present with pelvic or groin pain, compressible or non-compressible localized labial swelling, and tenderness without erythema or induration (6). In contrast to a hydrocele, a hernia may be induced and made more appreciable on physical exam when the patient stands up or performs the Valsalva maneuver (24). In children who do not understand the instructions to perform the Valsalva maneuver, they can be induced to cry or instructed to extend their abdomen or exhale to increase intraabdominal pressure (10).
Ultrasound is the preferred modality for initial imaging of canal of Nuck disorders (25). Ultrasound can visualize herniated structures in the canal of Nuck moving anteromedially and inferiorly when the patient stands up or performs the Valsalva maneuver (25). Color Doppler ultrasound detects vascularization and can distinguish between incarceration and strangulation, in which blood flow to the herniated structure is compromised and may lead to necrosis (10). In addition, relevant to the pediatric population, ultrasound does not require the patient to remain still for an extended time as is the case with MRI and does not expose the patient to radiation as in CT. Ultrasound should be performed with a high-frequency transducer to explore the labia and groin. Long- and short-axis views demonstrate the canal of Nuck superficially and medially to the pubic bone (26). When an intra-pelvic structure is identified and localized to the canal of Nuck via ultrasound, no additional differential need be considered, as ultrasound is essentially diagnostic in these cases. MRI is used when ultrasound is inconclusive and may provide more details of the herniated structures (6). When an intrapelvic organ or hydrocele cannot be definitively identified, differential considerations for a soft tissue fluid collection or mass include abscess or lymphadenopathy, though an abscess is likely to exhibit supporting ultrasound features such as regional echogenic fat, and a lymph node is often discernable from an intrapelvic organ by its morphology. CT can detect incidental canal of Nuck hernias but is not recommended as a first line modality for diagnosing canal of Nuck disorders because of radiation exposure (6).
In conclusion, canal of Nuck hernias are uncommon but may lead to emergent conditions such as incarceration, strangulation, or ovarian torsion. Because of these potential complications, knowledge of canal of Nuck disorders and prompt diagnosis are critical. Imaging, especially ultrasound, facilitates prompt diagnosis, leading to appropriate management and improved patient care.
Declaration of conflicting interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iDs
Jeannie K Kwon https://orcid.org/0000-0002-2085-6573
Cory M Pfeifer https://orcid.org/0000-0002-2220-9230
References
- 1.Kapur P, Caty MG, Glick PL. Pediatric hernias and hydroceles. Pediatr Clin North Am 1998; 45:773–789. [DOI] [PubMed] [Google Scholar]
- 2.Lao OB, Fitzgibbons RJ, Cusick RA. Pediatric inguinal hernias, hydroceles, and undescended testicles. Surg Clin N Am 2012; 92:487–504. [DOI] [PubMed] [Google Scholar]
- 3.Jedrzejewski G, Osemlak P, Wieczorek AP, et al. Nuck canal hernias, typical and unusual ultrasound findings. Ultrasound Q 2019; 35:79–81. [DOI] [PubMed] [Google Scholar]
- 4.Nasser H, King M, Rosenberg HK, et al. Anatomy and pathology of the canal of Nuck. Clin Imaging 2018; 51:83–92. [DOI] [PubMed] [Google Scholar]
- 5.Yang DM, Kim HC, Kim SW, et al. Ultrasonographic diagnosis of ovary-containing hernias of the canal of Nuck. Ultrasonography 2014; 33:178–183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rees MA, Squires JE, Tadros S, et al. Canal of Nuck hernia: a multimodality imaging review. Pediatr Radiol 2017; 47:893–898. [DOI] [PubMed] [Google Scholar]
- 7.Grosfeld JL. Current concepts in inguinal hernia in infants and children. World J Surg 1989; 13:506–515. [DOI] [PubMed] [Google Scholar]
- 8.Fu YW, Pan ML, Hsu YJ, et al. A nationwide survey of incidence rates and risk factors of inguinal hernia in preterm children. Pediatr Surg Int 2018; 34:91–95. [DOI] [PubMed] [Google Scholar]
- 9.Rathauser F. Historical overview of the bilateral approach to pediatric inguinal hernias. Am J Surg 1985; 150:527–532. [DOI] [PubMed] [Google Scholar]
- 10.Sameshima YT, Yamanari MG, Silva MA, et al. The challenging sonographic inguinal canal evaluation in neonates and children: an update of differential diagnoses. Pediatr Radiol 2017; 47:461–472. [DOI] [PubMed] [Google Scholar]
- 11.Cascini V, Lisi G, Di Renzo D, et al. Irreducible indirect inguinal hernia containing uterus and bilateral adnexa in a premature female infant: report of an exceptional case and review of the literature. J Pediatr Surg 2013; 48:e17–19. [DOI] [PubMed] [Google Scholar]
- 12.Derinkuyu BE, Affrancheh MR, Sonmez D, et al. Canal of Nuck hernia in a female infant containing uterus, bilateral adnexa and bowel. Balkan Med J 2016; 33:566–568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.George EK, Oudesluys-Murphy AM, Madern GC, et al. Inguinal hernias containing the uterus, fallopian tube, and ovary in premature female infants. J Pediatr 2000; 136:696–698. [DOI] [PubMed] [Google Scholar]
- 14.Jedrzejewski G, Stankiewicz A, Wieczorek AP. Uterus and ovary hernia of the canal of Nuck. Pediatr Radiol 2008; 38:1257–1258. [DOI] [PubMed] [Google Scholar]
- 15.Ming Y-C, Luo C-C, Chao H-C, et al. Inguinal hernia containing uterus and uterine adnexa in female infants: report of two cases. Pediatr Neonatol 2011; 52:103–105. [DOI] [PubMed] [Google Scholar]
- 16.Muthiyal S, Kini V, Kounsal A, et al. Rarity in conspicuity—ultrasound diagnosis of sliding left inguinal hernia through canal of Nuck with uterus, fallopian tubes and ovaries. Eur J Radiol Open 2016; 3:35–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Thomas AK, Teague CT, Jancelewicz T. Canal of Nuck hernia containing pelvic structures presenting as a labial mass. Radiol Case Rep 2018; 13:534–536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Tubbs RS, Loukas M, Shoja MM, et al. Indirect inguinal hernia of the urinary bladder through a persistent canal of Nuck: case report. Hernia 2007; 11:287–288. [DOI] [PubMed] [Google Scholar]
- 19.Burgmeier C, Dreyhaupt J, Schier F. Gender-related differences of inguinal hernia and asymptomatic patent processus vaginalis in term and preterm infants. J Pediatr Surg 2015; 50:478–480. [DOI] [PubMed] [Google Scholar]
- 20.Chang SJ, Chen JY, Hsu CK, et al. The incidence of inguinal hernia and associated risk factors of incarceration in pediatric inguinal hernia: a nation-wide longitudinal population-based study. Hernia 2016; 20:559–563. [DOI] [PubMed] [Google Scholar]
- 21.Bronsther B, Abrams MW, Elboim C. Inguinal hernias in children–a study of 1,000 cases and a review of the literature. J Am Med Womens Assoc (1972) 1972; 27:522–525 passim. [PubMed] [Google Scholar]
- 22.Harper RG, Garcia A, Sia C. Inguinal hernia: a common problem of premature infants weighing 1,000 grams or less at birth. Pediatrics 1975; 56:112–115. [PubMed] [Google Scholar]
- 23.Misra D, Hewitt G, Potts SR, et al. Inguinal herniotomy in young infants, with emphasis on premature neonates. J Pediatr Surg 1994; 29:1496–1498. [DOI] [PubMed] [Google Scholar]
- 24.De Meulder F, Wojciechowski M, Hubens G, et al. Female hydrocele of the canal of Nuck: a case report. Eur J Pediatr 2006; 165:193–194. [DOI] [PubMed] [Google Scholar]
- 25.Revzin MV, Ersahin D, Israel GM, et al. US of the inguinal canal: comprehensive review of pathologic processes with CT and MR imaging correlation. Radiographics 2016; 36:2028–2048. [DOI] [PubMed] [Google Scholar]
- 26.Shadbolt CL, Heinze SBJ, Dietrich RB. Imaging of groin masses: inguinal anatomy and pathologic conditions revisited. Radiographics 2001; 21:S261–S271. [DOI] [PubMed] [Google Scholar]