Abstract
Objective
Myositis ossificans is a rare non-neoplastic form of heterotopic ossification most commonly described after trauma or surgery, in the diabetic foot.
Design
We provide a review of the literature including three illustrative cases.
Participants
Individuals presenting to the foot clinic.
Setting
Single centre, tertiary multidisciplinary specialist diabetes foot clinic.
Results
We review the literature surrounding Myositis ossificans, and describe three cases of Myositis ossificans following foot surgery in people with diabetes. All of the imaging was consistent with the descriptions of Myositis ossificans reported elsewhere in large muscle groups. These are the first reports of Myositis ossificans occurring in the feet of people with diabetes.
Conclusions
Myositis ossificans has only very rarely been described in the foot and, as far as we are aware, never in people with diabetes. Given that the prevalence of diabetes is increasing, and the foot problems requiring surgery are also rising, we suggest that clinicians should be more aware of this condition because it may occur more frequently.
Keywords: clinical, diabetes, diagnostics, endocrinology, orthopaedic and trauma surgery, radiology and imaging, surgery
Introduction
We report the first cases (to our knowledge) of myositis ossificans in the ‘diabetic foot’.
Cases
Case 1
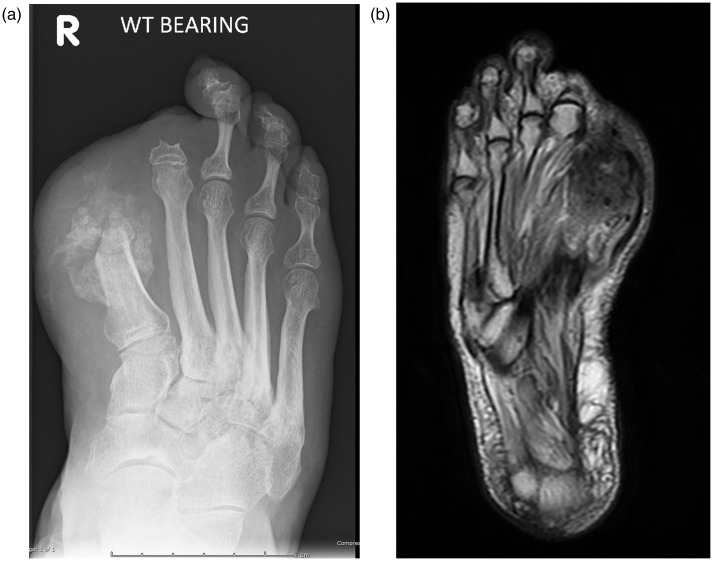
A 54-year-old lady, with a 20-year history of type 1 diabetes mellitus was admitted to our unit with apparent osteomyelitis of her right first metatarsal phalangeal joint. Two weeks prior she had been treated at a local unit with intravenous antibiotics and surgical debridement. She had previously undergone right foot first and second toe amputations, nine and seven years previously, respectively. At presentation to our specialist multidisciplinary foot clinic, her foot was slightly swollen, but there were no other clinical indicators of osteomyelitis. Radiographs of the foot showed exuberant new bone formation adjacent to the hallux metatarsal, reported as being ‘in keeping with osteomyelitis’ (Figure 1(a)). An magnetic resonance imaging scan of her foot was performed to determine the presence and extent of any ongoing bone infection. This showed a soft tissue mass on the plantar and medial aspect of the first metatarsal, corresponding to the area of ossification on the plain radiograph. This was isointense to muscle on T1-weighted sequences and slightly hyperintense on T2-weighted sequences (Figure 1(b)). This was reported as being ‘in keeping with heterotopic ossification and Myositis ossificans’.
Figure 1.
(a) Radiograph of the right foot of Case 1 showing exuberant new bone formation adjacent to the hallux metatarsal and previous first and second toe amputations and (b) T2-weighted sequence magnetic resonance imaging right foot of Case 1 showing a soft tissue mass on the plantar and medial aspect of the first metatarsal.
On the basis of the clinical appearance of the foot and the radiological imaging a management plan was formulated. This meant that patient was initially fitted with specialist insoles for her shoes and scheduled to have an isotope bone scan 12 months later to assess for the ongoing bony activity in her foot. If it had stabilised she would be reviewed for consideration for further surgery and removal of the heterotopic calcification.
Case 2
A 53-year-old man with a 13-year history of Type 2 diabetes mellitus presented to our foot clinic with an ulcer over the plantar aspect of his right second metatarsophalangeal joint and right dorsal second toe. He was known to have a Charcot (neuroarthropathic) foot on the left, diagnosed four years previously. Three months prior to presentation, he had undergone a third metatarsal ray amputation for ulceration and osteomyelitis. On examination, the wound appeared clean and a small piece of bone was removed. Radiographs of the foot showed new bone destruction centred on the neck of the second metatarsal with dislocation of the second metatarsophalangeal joint, in keeping with osteomyelitis (Figure 2(a)). In accordance with our local antibiotic protocol, he was started on a course of oral co-amoxiclav.1 Despite this, an magnetic resonance imaging scan done three weeks later showed extensive osteomyelitis within the second metatarsal with bone fragmentation of the metatarsal head and involvement of the metatarsophalangeal joint. In addition, there was extensive periosseous phlegmon formation around the second metatarsal shaft (Figure 2(b)). Despite these radiological findings, the patient was reluctant to pursue surgical options, opting for another course of broad spectrum antibiotics. Another magnetic resonance imaging scan performed 6 weeks later showed persisting osteomyelitis involving the second metatarsal, with an increasing larger concentric soft tissue mass along the shaft of the second metatarsal associated with bony destruction. However, clinically his foot had no swelling or erythema. Over the subsequent two months he had ongoing debridement and offloading of his foot ulcer. Sequential radiographs showed ongoing exuberant bone formation, bony erosion and periosteal reaction of the right second metatarsal (Figure 2(c)). His ulcer persisted and a further magnetic resonance imaging scan suggested ongoing osteomyelitis in the second metatarsal. Nevertheless, on examination, his foot showed no evidence suggestive of underlying infection. After discussion with the specialist soft tissue radiologist, it was felt that the images of the second metatarsal represented Myositis ossificans with concurrent osteomyelitis.
Figure 2.
(a) Radiograph of the right foot of Case 2 showing new bone destruction centred on the neck of the second metatarsal with dislocation of the second metatarsophalangeal joint, in keeping with osteomyelitis, (b) Magnetic resonance imaging of the right foot of Case 2 showing extensive osteomyelitis within the second metatarsal with bone fragmentation of the metatarsal head and involvement of the metatarsophalangeal joint, as well as extensive periosseous inflammatory phlegmon formation around the second metatarsal shaft and (c) radiograph of the right foot of Case 2 showing ongoing exuberant bone formation, bony erosion and periosteal reaction of the right second metatarsal.
Case 3
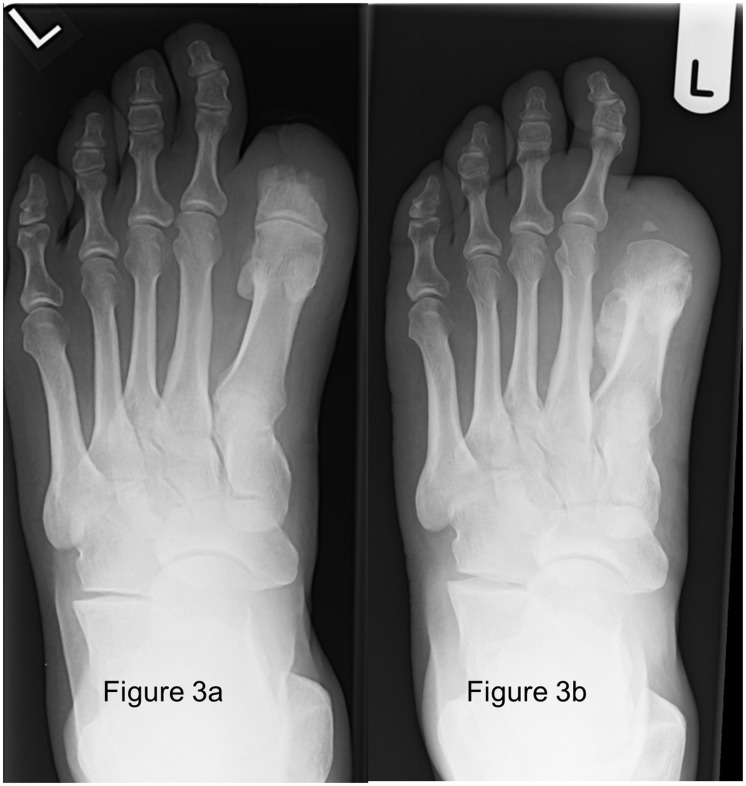
A 43-year-old man with a 12-year history of type 1 diabetes mellitus was referred to the foot team following emergency amputation of his ischaemic and infected left first toe. He was left with a large postoperative wound site which was managed with debridement and broad-spectrum antibiotics. Radiographs of the foot initially showed healthy callus formation, with a radiograph taken four months later showing a new ossification centre at the site of the stump, with remodelling of the residual proximal phalanx of the first toe (Figure 3(a)). Unfortunately, radiographs taken two months later showed lucency in the soft tissue overlying the distal stump and new distal bone resorption. A subsequent magnetic resonance imaging verified the radiograph findings, showing a subcutaneous sinus at the amputation site with diffuse periosseous soft tissue swelling and low grade enhancement in keeping with osteomyelitis. He underwent revision surgery and further amputation at the metatarsophalangeal joint of the first toe. Over the next four months, the wound healed well, but the foot continued to appear swollen. Sequential radiographs and Magnetic resonance imaging of the foot showed new callous formation and periosseous soft tissue swelling at the first metatarsal, with new erosions at the medial aspect and a periosteal reaction at the lateral aspect (Figure 3(b)). More proximally, soft tissue oedema appeared to extend concentrically around the first and second metatarsal shafts, suggesting persistent osteomyelitis. In contrast, clinical examination and blood results indicated no evidence of inflammation or infection. Despite these, and further Magnetic resonance imaging suggesting resolution of infection, his swelling persisted. Because of this discrepancy, all of his imaging was again reviewed by the multidisciplinary foot team and the specialist radiologist. It was concluded that the callous formation at the first amputation site and the periosteal reaction at the lateral aspect of the metatarsal head most likely represented Myositis ossificans, with concurrent osteomyelitis.
Figure 3.
(a) Radiograph of the left foot of Case 3 showing new ossification centre at the site of the stump, with remodelling of the residual proximal phalanx of the first toe and (b) radiograph of the left foot of Case 3 showing new callous formation and periosseous soft tissue swelling at the first metatarsal, with new erosions at the medial aspect and a periosteal reaction at the lateral aspect.
Discussion
Myositis ossificans is a rare non-neoplastic form of heterotopic ossification. Myositis ossificans is an ossifying lesion most commonly described as arising in the large muscle groups of the upper and lower limb, particularly those surrounding bone.2 The clinical presentation of Myositis ossificans is variable, but usually includes a history of repetitive minor trauma or a specific injury leading to a haematoma.2–6 Nevertheless, often no causative reason can be identified. The incidence is approximately 2% in people undergoing hip surgery and 20% in individuals investigated for thigh contusions.6 However, there are very few cases of Myositis ossificans described in the foot, and none occurring in people with diabetes or associated with osteomyelitis.7
Different forms of Myositis ossificans have been described. A classification coined by Noble in 1924 includes: (1) Fibrodysplasia ossificans progressiva, a rare disease of childhood progressively involving all skeletal muscles; (2) traumatic Myositis ossificans which may follow acute or chronic trauma and accounting for 80% of cases described and (3) non-traumatic Myositis ossificans accounting for 20% of cases described and usually associated with paraplegia, clotting disorders or chronic infection. In the literature, Myositis ossificans and heterotropic ossification are often used interchangeably.5 In this case series, we will be focusing on traumatic Myositis ossificans, also known as Myositis ossificans traumatica.
We present an illustrative case series of pedal Myositis ossificans in three individuals with pre-existing diabetes related foot disease. All subjects gave written consent. We suggest that this rare condition may be frequently overlooked in people with diabetes and may occur more frequently as the prevalence of diabetes related foot disease increases.
Myositis ossificans typically forms after single or repeated injury to soft tissue structures surrounding bone.2,5 The pathogenesis is poorly understood, but resultant necrosis or haematoma from these injuries is considered the starting point for the inappropriate, over-exuberant cellular response.4,6
Histology
Histologically, Myositis ossificans follows a characteristic pattern of development with the formation of distinct zonal layers.2,5,8 It forms in a chronological process which reflects various stages of cellular maturation. Initially there is a central proliferating mass made up of immature fibroblastic cells mixed with inflammatory cells.2,3,5 Progressing outwards to the intermediate and outer zones the cells become more condensed and calcified, eventually becoming mature bone. These characteristic layers form gradually and can be appreciated after about three weeks.5 This is clinically relevant because the imaging of these lesions is time dependant. Plain radiographic images may not pick up the lesion early on in their development and they will not be able to demonstrate the zonal pathology described.2,3
Given the rarity of Myositis ossificans there may be diagnostic uncertainty, with differentials including neoplastic bone tumours, other non-neoplastic tumour with bone formation and osteomyelitis.2 Clinically, the condition normally presents as a tender erythematous growth with a gelatinous texture which hardens and becomes well defined over weeks, as it progressively forms into mature lamellar bone.2 The reduction in symptoms as the lesion matures is in contrast to potentially malignant lesions which tend to get worse with time.5
Diagnosis
A diagnosis of Myositis ossificans is most frequently made using a combination of clinical and radiological findings. Depending on timing, a plain radiograph may show nothing, a soft tissue density or an ossified lesion.5 The early stages may also show a periosteal reaction and bone marrow oedema. These can be non-specific on Magnetic resonance imaging, but the mineralisation is visible on CT with a non-ossified centre early on, an osteoid shell and then mature bone.9 Nevertheless, the role of Magnetic resonance imaging in the diagnosis of early Myositis ossificans without calcification or ossification is becoming increasingly recognised.10 Where diagnostic uncertainty remains, a tissue biopsy or excision may be necessary.2,3 Biopsies that preserve the zonal structure will help provide a stronger basis for diagnosis, whereas an aspiration is less likely to demonstrate this. However, in people with diabetes related foot disease this may not be possible. For example, in our centre, bone biopsies are not performed routinely, and after discussion with our radiologists, Magnetic resonance imaging is the preferred imaging modality of choice for diabetes related foot disease rather than computed tomographic imaging. Biopsy would be important if there were a suspicion of any of the other differential diagnoses. These include periosteal or extraosseous osteosarcoma, fibrous histiocytoma or a synovial sarcoma. In our case series, we saw no common pattern of muscle involvement.
Management
Myositis ossificans is a benign and self-limiting condition that usually requires no active treatment if the patient is asymptomatic.2 Myositis ossificans lesions may resolve spontaneously. However, if the patient experiences pain, discomfort or a limited range of motion, previous authors have suggested a combination of initial treatment with rest, ice, compression and elevation.5,11 If symptoms persist then surgical resection has been suggested, but only after the excess bone formation has stopped. This can be picked up by isotope bone scanning.5,9 Even so, invasive surgical resection may compromise local function and lead to local relapse. Because of this, Myositis ossificans has been referred to as a ‘don’t- touch lesion’.12 This suggests that surgical intervention should only be considered if function is impaired, and once the lesion has fully matured.
Some literature exists on the medical prophylaxis of Myositis ossificans. The role of non-steroidal anti-inflammatory drugs in the prophylaxis of Myositis ossificans following hip arthroplasty has been well documented; however, no studies have investigated the role of non steroidal anti-inflammatory drugs in post-traumatic Myositis ossificans.13 Similarly, bisphosphonates have also been found to be effective in the prophylaxis of Myositis ossificans formation in patients with spinal cord injuries. However, they have not been shown to be effective once Myositis ossificans has developed.14
In someone with an ‘at risk’ foot, such as those with diabetes, the excess bone can alter the biomechanics and cause abnormal weight distribution through the foot. Combined with peripheral neuropathy, the risks of developing Charcot disease and diabetic foot disease may warrant further surgical management. Although the prevalence of Myositis ossificans in the diabetic foot is not known, surgical intervention should be considered when the functional impact of altered biomechanics combined with the risk of developing Charcot neuroarthropathy and ulceration outweighs the risks associated with surgery.
In the cases described, all of the patients had diabetes related foot disease and two had been treated with antibiotics for presumed osteomyelitis. The antibiotics failed to improve the symptoms and radiographic findings. This discrepancy between the clinical and the radiographic findings prompted a multidisciplinary review of the cases, concluding that the bony lesions identified were most likely Myositis ossificans.
There are some limitations to these reports that we acknowledge. The radiological images that we have presented are limited mainly to T1-weighted images, and these show periosteal new bone and perhaps some dystrophic bone. These could be described as heterotopic bone and, as mentioned, the terms myositis ossificans and heterotropic ossification are often used interchangeably.5 In addition, because these cases were collected over time; we are unable to go back and obtain adequate T2-weighted fat saturated images to show any inflammation that may be present. Furthermore, while CT imaging may have been more appropriate to detect osteomyelitis as the underlying cause of the Myositis ossificans, more recent data suggest that Magnetic resonance imaging is better for making an early diagnosis of Myositis ossificans.15 We also acknowledge that bone biopsy may have helped clarify the diagnosis, but this procedure is not carried out by our specialist foot and ankle surgeons, podiatrists or radiologists at our institution.
We suggest that these Myositis ossificans lesions developed primarily as a result of trauma and/or surgery (as in Case 1) or may have occurred concurrently or as a result of osteomyelitis (Cases 1–3). To our knowledge, there has only been one report of concomitant Myositis ossificans and osteomyelitis.16 Unlike our cases, where there was no evidence of the Myositis ossificans prior to the patients becoming symptomatic, Mishra et al. reported that their patient had Myositis ossificans six months prior to developing osteomyelitis. We have been unable to find any cases reporting Myositis ossificans occurring as a result of osteomyelitis.
The importance of identifying Myositis ossificans in the diabetes population is two-fold. Firstly, early diagnosis may be confused with malignant conditions such as osteosarcoma or infective conditions such as osteomyelitis. Early identification would potentially prevent unnecessary surgical intervention or prolonged courses of antibiotics. Second, the formation of Myositis ossificans with diabetes related foot disease, combined with peripheral neuropathy, as previously highlighted, may predispose to the development of Charcot neuroarthropathy. Furthermore, altered biomechanics may precipitate the development of pressure ulcers. We suggest that clinicians consider a diagnosis of Myositis ossificans if clinical symptoms do not correlate to radiological evidence of osteomyelitis and/or the formation of heterotopic bone.
Summary and conclusion
We have presented three cases of Myositis ossificans in the diabetic foot. It is important to consider the potential impact of Myositis ossificans in patients with diabetes mellitus because it can change the biomechanics within the foot and potentially worsen functional outcomes. The presented case series highlights the importance of early podiatric care, and the influence of a multidisciplinary foot team, in patients with long-term diabetes. Such an approach may help avoid diabetic and orthopaedic foot complications in such populations.
Because the prevalence of diabetes is increasing, the absolute number of people with foot disease will also increase. A proportion of those will require surgery. Thus, we suggest that it is important for all members of the multidisciplinary foot team to be aware of Myositis ossificans as a possible complication of osteomyelitis or surgery in the diabetic foot. Early identification may prevent unnecessary investigations and interventions.
Acknowledgements
None.
Declarations
Competing Interests
None declared.
Funding
None declared. All of the authors are employees of the UK NHS.
Ethics approval
Not required.
Guarantor
KKD.
Contributorship
VS and DS did the literature search. VS, DS and HD wrote the first drafts of the manuscript. HD and KKD looked after the three illustrative cases. KKD wrote the final version of the manuscript. All authors saw and agreed on the final submitted version.
Provenance
Not commissioned; peer-reviewed by Dhastagir Sheriff.
ORCID iD
Ketan K Dhatariya https://orcid.org/0000-0003-3619-9579
References
- 1.Gooday C, Hallam C, Sieber C, Mtariswa L, Turner J, Schelenz S, et al. An antibiotic formulary for a tertiary care foot clinic: admission avoidance using intramuscular antibiotics for borderline foot infections in people with diabetes. Diabetic Med 2013; 30: 581–589. [DOI] [PubMed] [Google Scholar]
- 2.Goldblum JR, Folpe AL, Weiss SW. Cartilaginous and osseous soft tissue tumors. In: Goldblum JR, Folpe AL, Weiss SW. (eds). Enzinger and Weiss’s soft tissue tumors, Philadelphia, PA: Saunders Elsevier, 2014, pp. 917–946. [Google Scholar]
- 3.Salgado RA, Gielen JL, de Schepper A. Tumor-like soft tissue lesions. In: Pope TL, Bloem H, Beltran J, Morrison WB, Wilson D. (eds). Musculoskeletal imaging, Philadelphia, PA: Elsevier/Saunders, 2015. , pp.996–1015.e1. [Google Scholar]
- 4.Murray BL. Femur and hip. In: Marx JA, Hockberger RS, Walls RM. (eds). Rosen’s emergency medicine: concepts and clinical practice, Philadelphia, PA: Elsevier/Saunders, 2014, pp. 672–697. [Google Scholar]
- 5.Walczak BE, Johnson CN, Howe BM. Myositis ossificans. J Am Acad Orthop Surg 2015; 23: 612–622. [DOI] [PubMed] [Google Scholar]
- 6.McMillan S, Busconi B, Montano M. Hip and thigh contusions and strains. In: Miller MD, Thompson S. (eds). DeLee & Drez’s orthopaedic sports medicine, Philadelphia, PA: Elsevier/Saunders, 2015, pp. 1006–1014. [Google Scholar]
- 7.Al-Timimy QA, Al-Edani MS. Myositis ossificans: a rare location in the foot. Report of a case and review of literature. Int J Surg Case Rep 2016; 26: 84–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kaplan KS, Glaser DL, Hebela N, Shore EM. Heterotopic ossification. J Am Acad Orthop Surg 2004; 12: 116–125. [DOI] [PubMed] [Google Scholar]
- 9.Tyler P, Saifuddin A. The imaging of myositis ossificans. Semin Musculoskelet Radiol 2010; 14: 201–216. [DOI] [PubMed] [Google Scholar]
- 10.Wang C, Mai L, Yang C, Liu D, Sun K, Song W, et al. Reducing major lower extremity amputations after the introduction of a multidisciplinary team in patient with diabetes foot ulcer. BMC Endocr Disord 2016; 16: 38–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jarvinen TA, Jarvinen TL, Kaariainen M, Kalimo H, Jarvinen M. Muscle injuries. Biology and treatment. Am J Sports Med 2005; 33: 745–764. [DOI] [PubMed] [Google Scholar]
- 12.Murphy A and Farooq S. Myositis ossificans, https://radiopaedia.org/articles/myositis-ossificans-1 (2018, accessed 21 June 2019).
- 13.Pavlou G, Kyrkos M, Tsialogiannis E, Korres N, Tsiridis E. Pharmacological treatment of heterotopic ossification following hip surgery: an update. Expert Opin Pharmacother 2012; 13: 619–622. [DOI] [PubMed] [Google Scholar]
- 14.Banovac K, Gonzalez F, Wade N, Bowker JJ. Intravenous disodium etidronate therapy in spinal cord injury patients with heterotopic ossification. Paraplegia 1993; 31: 660–666. [DOI] [PubMed] [Google Scholar]
- 15.Wang H, Nie P, Li Y, Hou F, Dong C, Huang Y, et al. MRI findings of early myositis ossificans without calcification or ossification. BioMed Res Int 2018; 2018: 4186324–4186324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mishra PK, Singhal P, Shukla J, Maravi DS. Osteomyelitis of myositis ossificans in arm – first case report. J Orthop Case Rep 2014; 4: 57–59. [DOI] [PMC free article] [PubMed] [Google Scholar]