Abstract
From the time of diagnosis through either survivorship or end of life, communication between healthcare providers and patients or parents can serve several core functions, including fostering healing relationships, exchanging information, responding to emotions, managing uncertainty, making decisions, and enabling patient/family self-management. We systematically reviewed all studies that focused on communication between clinicians and patients or parents in pediatric oncology, categorizing studies based on which core functions of communication they addressed. After identifying gaps in the literature, we propose a research agenda to further the field.
Keywords: communication, decision making, information sharing, pediatric oncology, physician–patient relationship
1 |. INTRODUCTION
From the time of diagnosis through either survivorship or end of life, communication between healthcare providers and patients or their parents in pediatric oncology serves several core functions. In a project commissioned by the National Cancer Institute in 2007, Epstein and Street proposed six core functions of communication in oncology: fostering healing relationships, exchanging information, responding to emotions, managing uncertainty, making decisions, and enabling patient/family self-management.1 It is currently unknown whether the pediatric literature sufficiently addresses these functions.
Communication in pediatric oncology occurs within the complex relationship between physician, parent, and child, necessitating dedicated communication research in pediatrics. To understand the current state of communication research and identify gaps in the literature, we utilized Epstein and Street’s functions of communication as a framework for analysis of pediatric oncology communication literature. Other recent review articles have focused on specific aspects of communication in pediatric oncology. Two groups focused on educational interventions for patients or physicians.2,3 Another group focused on communication interventions for pediatric patients with cancer.4 Other reviews have focused on specific pediatric cancer subpopulations.5–7 However, these reviews focused primarily on using technology and educational interventions to provide information for adolescent patients, rather than interventions that targeted clinician–patient or clinician–parent interactions.4 Given the relatively small and varied literature on communication in pediatric oncology, we searched the literature for all studies of communication between clinicians and patients or parents, and evaluated whether the literature addresses the six functions of communication. We also summarize major themes and provide guidance for a future research agenda.
2 |. METHODS
We conducted a systematic review following the guidelines provided by Khan et al.8 Although none of the studies reviewed used a randomized clinical trial or intervention design, we followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines for reporting results of reviews insofar as data permitted,9 posing the question: “How does communication between healthcare providers and patients/families in pediatric oncology fulfill the core functions of communication?”
2.1 |. Inclusion and exclusion criteria
This review was inclusive of all research articles presenting original data focused on communication in pediatric oncology between healthcare providers and parents or patients. Exclusion criteria included not focused on healthcare providers, pediatric patients, or parents; topic unrelated to communication interaction between healthcare provider and parent/child; abstract or research communication report; no original data reported; study not available in English. We considered “pediatric” to include all children under 18 years. One author (BS) determined whether studies met inclusion criteria. If studies included children and adults, we included studies but focused on pediatric data.
2.2 |. Search strategy
A medical librarian developed search strategies using adjacency searching, including keywords such as pediatric, child, malignancy, oncology, tumor, neoplasm, communication, disclosure, and interpersonal. These strategies were implemented in Embase 1947-, and OVID Medline 1946- focused on the date range of January 2000 through May 2016. Searches were completed in May 2016 and the results were exported to Endnote. This search strategy was supplemented by snowballing, where additional articles were identified by manual searching through reference lists and review articles.
2.3 |. Data classification
After exclusions, 90 remaining articles were coded based on which core functions of communication each study addressed, using definitions provided in Table 1.1 Reviewers assigned codes for one or more core function to each article, meaning that one study could address multiple communication functions. Reviewers further coded studies regarding perspective captured in interviews or surveys (including child report, parent report, physician report, nurse report, and report of other staff), and content area (including communication of diagnosis, treatment, or side effects/toxicities; fertility preservation; survivorship/late effects other than fertility; research informed consent; communication of prognostic information; and end-of-life discussions). Content area topics were developed inductively while coding. Each study could have multiple perspectives and content area topics. Studies in which communication was observed or recorded, but no surveys or interviews were performed, were not considered to have captured the report of any stakeholders. Coding definitions were developed and agreed upon by all authors. Two authors (BS and JM) independently coded all studies. Agreement was good for all categories of functions and content (mean kappa for agreement by category of communication code = 0.88, range 0.69–1.00; individual kappa scores listed in Table 3). Discrepancies were resolved by consensus between the two coders.
TABLE 1.
Six core functions of clinician–patient/parent communication—adapted from Epstein and Street1
| Function | Description | Example |
|---|---|---|
| Fostering healing relationships | Healing relationships provide emotional support, guidance, and understanding. Such relationships are built on trust, rapport, and mutual understanding of each other’s roles and responsibilities. Physicians can facilitate a healing relationship by engaging in active listening, partnership building, seeking out goals and values of the patient and family, displaying warmth and empathy in communication. | In disclosing a new diagnosis of cancer in a child, the physician listens and speaks in an empathic manner that creates a trusting relationship between the physician and the family. |
| Exchanging information | Patients and their families seek information about the cause, diagnosis, treatment, prognosis, and lasting effects of cancer and its treatment. Fulfilling information needs not only helps families to gain important knowledge about a child’s illness, but also aides the development of a strong clinician–family relationship and supports decision making, among other outcomes. | Prior to enrollment in a clinical trial, the physician describes the risks and benefits of enrollment, as well as the prognosis of the child. |
| Responding to emotions | Patients with cancer can experience a range of emotions, including fear, sadness, anger, anxiety, and depression. When patients or parents express emotions in clinical encounters, the clinician’s task is to recognize the emotional state, ask questions, communicate understanding, and respond with empathy or tangible help. | After a CT scan demonstrates progression of disease, the child’s nurse reflects the parents emotional state and provides emotional support as they process the information. |
| Managing uncertainty | Parents and patients experience many types of uncertainty after a diagnosis of cancer. This uncertainty can pertain to prognosis, side effects, frequency of hospitalization, and long-term effects, among others. Family-centered communication should help to communicate clinical uncertainty when it exists, dispel uncertainty when there is an answer, and help patients and families to manage unavoidable uncertainties. | As a child reaches the end of treatment for cancer, the nurse practitioner sets the families expectations for what is normal versus abnormal after completion of therapy. |
| Making decisions | Effective decision making requires effective communication. Such communication can support decision making in a number of ways: raising the clinician’s awareness of the family’s needs, values, and fears; clarifying clinical reasoning and treatment options; alerting the physician to the family’s preferred role in decision making. | The physician assesses the family’s values and fears, then makes a recommendation regarding whether to pursue fertility preservation for their young daughter with newly diagnosed cancer. |
| Enabling patient self-management | Communication can also help patients to “enhance their ability to solve health-related problems and to take actions to improve their health.” This can encompass recommendation, instruction, and advocacy. | Prior to a family’s first discharge from the hospital, the physician discusses dangerous warning signs that merit evaluation in the emergency department. |
TABLE 3.
Functions and content examined in studies of communication in pediatric oncology (N = 90)
| Functiona | % Yes (n) | References |
|---|---|---|
| Fostering healing relationships (k = 0.74) | 33.3 (30) | 12–25,27,30,31,43,74–77,81,83,84,87,88,92,109,111 |
| Exchanging information (k = 0.84) | 95.6 (86) | 12–24,26,27,29–52,54–59,61–65,67–77,79,80,82,83,86,88–90,92,93,104,107–111 |
| Responding to emotions (k = 0.69) | 25.6 (23) | 12,13,15,16,22–25,31,36,43,57,63,64,75,76,81–87,111 |
| Managing uncertainty (k= 0.92) | 4.4 (4) | 20,26,63,75 |
| Making decisions (k = 0.85) | 35.6 (32) | 12–14,17–19,24,30,33,35–37,42,45,46,53–55,64–66,68,69,72,77,78,86,89–92,106 |
| Enabling patient and family | ||
| Self-management (k = 0.92) | 6.7 (6) | 22,25,63,79,82,93 |
| Content | ||
| Child report (k = 0.87) | 15.6 (14) | 14,16,17,21,37,38,40,53,54,69,70,79,83,110 |
| Parent report (k = 0.90) | 67.8 (61) | 12–21,23–28,34,35,40,42–47,49–54,61,62,65–68,70–75,77–81,85–93,105,107,109 |
| Physician report (k = 0.90) | 32.2 (29) | 18,19,21,25,26,29,31,32,48,52,53,55–58,64,65,68,72,74,78–80,82,86,90,91,104,107 |
| Nurse report (k = 0.96) | 15.6 (14) | 21,22,24,29,31,48,52,53,57,79,82,84,86,108 |
| Report of other staff (k = 0.96) | 5.6 (5) | 48,52,57,79,82 |
| Communication of prognostic disclosure (k = 0.80) | 32.2 (29) | 14,16,18,19,22,26–31,35,44,45,52,57,61,62,71,72,77,80,82,86,88,90,105,107,109 |
| Communication of diagnosis, treatment, toxicity (k = 0.74) | 46.7 (42) | 13,14,16,19,20,22,23,26,28,30–33,35,40,43–47,50–52,60,61,63,66–74,76,79,82,92,105,106,110 |
| Fertility preservation (k = 1.00) | 8.9 (8) | 37,38,40,56,58,65,82,108 |
| End of Life discussion (k = 0.94) | 16.7 (15) | 12,17,19,25,29,41,42,53,57,62,86,90,91,93,104 |
| Research informed consent (k = 0.98) | 17.8 (16) | 13,19,33–36,54,55,59,60,64,68,72,81,89,106 |
| Survivorship/late effects (k = 1.00) | 4.4 (4) | 39,40,49,50 |
For both outcome and content, the total percentage exceeds 100% because studies frequently engaged more than one outcome or content source.
We further classified studies based on the following classifications of psychological research: “descriptive,” “correlational,” or “experimental.” Descriptive studies “create a snapshot of the current state of affairs”; correlational studies “assess the relationships between and among two or more variables”; experimental studies “assess the causal impact of one or more experimental manipulations on a dependent variable.”10 The PRISMA guidelines for a systematic review of Randomized Control Trials and intervention studies recommend that reviews “Specify any assessment of risk of bias that may affect the cumulative evidence (e.g., publication bias, selective reporting within studies).”9 Given the lack of intervention studies in our review, the matter of bias regarding positive findings or selective reporting is not applicable; however, the risk of selectively reporting themes in qualitative and survey research is an unavoidable risk.11
3 |. RESULTS
3.1 |. Description of findings
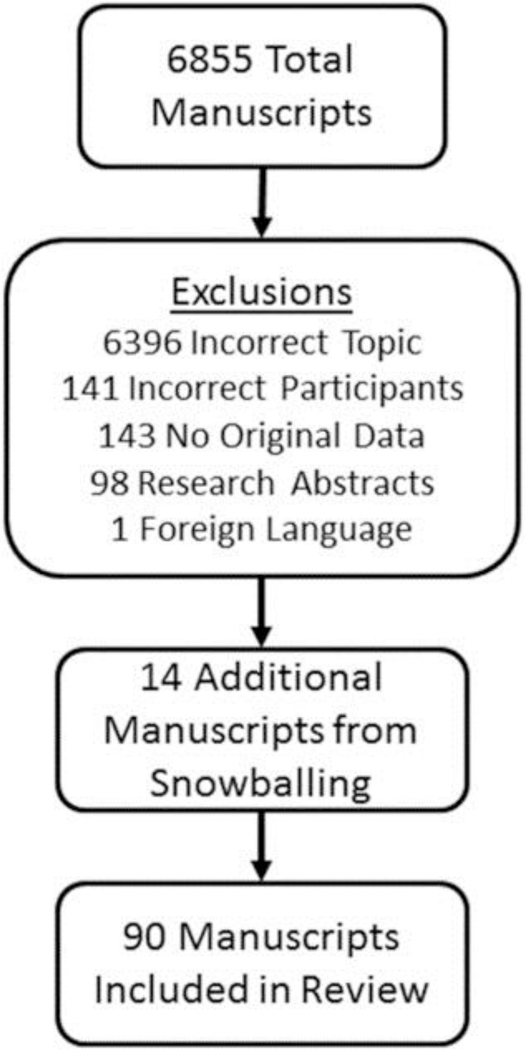
In what follows, we present a general summary of findings followed by a review of findings within individual functions of communication. Our initial search yielded 6,855 unique articles, supplemented by 14 articles from snowballing. Most exclusions addressed a different topic (e.g., intracellular communication rather than interpersonal communication; N = 6,396) or presented no original data (N = 143; Fig. 1). Ninety remaining studies were evaluated, of which most were descriptive studies with small sample sizes (Supplementary Table S1). Seventy seven percent (N = 69/90) of studies were descriptive and 23% (N = 21/90) were correlational. No studies were experimental. Additionally, 90% (N = 81/90) of studies had fewer than 200 participants, and 67% (N = 61/90) had fewer than 100 participants. Most studies included parent report (67%, N = 60/90), compared to 27% (N = 24/90) child report and 39% (N = 35/90) physician report. Most studies took place in the United States (46%, N = 41/90), United Kingdom (10%, N = 9/90), or other areas of Europe (22.2%, N = 20/90; Table 2).
FIGURE 1.
Flow chart for exclusions
TABLE 2.
Summary of nation, population, and sample sizes of communication studies in pediatric oncology (N = 90)
| Variable | % Yes (n) | References |
|---|---|---|
| Nation | ||
| United States | 45.6 (41) | 13,15,18,19,25–29,33–36,41,44,49,53–56,58–60,66,68,72,77,78,80–83,87–90,104–108 |
| United States + Other | 4.4 (4) | 17,30,32,109 |
| United Kingdom | 10.0 (9) | 31,37,38,46,52,70,71,76,110 |
| Europe | 22.2 (20) | 14,16,21,24,39,42,48,50,51,62–65,69,74,75,85,86,91,111 |
| Other | 17.8 (16) | 12,20,22,23,40,43,45,47,57,61,67,73,79,84,92,93 |
| Number of participantsa | ||
| <30 | 30.0 (27) | 13,15,19,20,22,31,35,45,48,53,57,58,63–66,68,69,74,75,79,83–85,87,106,111 |
| 31–100 | 37.8 (34) | 12,14,17,21,28,30,33,36,37,39,42–44,46,49,51,52,54,56,60,61,67,70–73,76,77,86,92,93,107,109,110 |
| 101—200 | 22.2 (20) | 16,18,25–27,34,40,41,47,50,55,59,78,80,81,88–91,108 |
| >200 | 10.0 (9) | 23,24,29,32,38,62,82,104,105 |
| Populationb | ||
| Parents | 66.6 (60) | 12–16,18–21,23–28,30,33–35,40,42–47,49–52,54,59,61–63,65–67,70–78,80,81,85–88,90,92,93,105,107,109,111 |
| Children | 26.7 (24) | 14,16,17,21,30,33,36–41,51,53,54,57,61,63,68–70,79,83,110 |
| Physician | 38.9 (35) | 17,18,21,25,26,28–32,39,48,52,55,56,58,60,63–65,72,74,76–82,88,90–92,104,105 |
| Other healthcare worker | 20.0 (18) | 21,22,24,29–31,45,52,57,63,64,77,79,82,84,91,107,108 |
| Other | 3.3 (3) | 33,59,82 |
For number of participants, we list the number of individual participants or dyads in the case of studies that interviewed, for example, both parents and children together, unless a separate n was provided for each group.
For population, total percentage exceeds 100% because many studies engaged multiple populations.
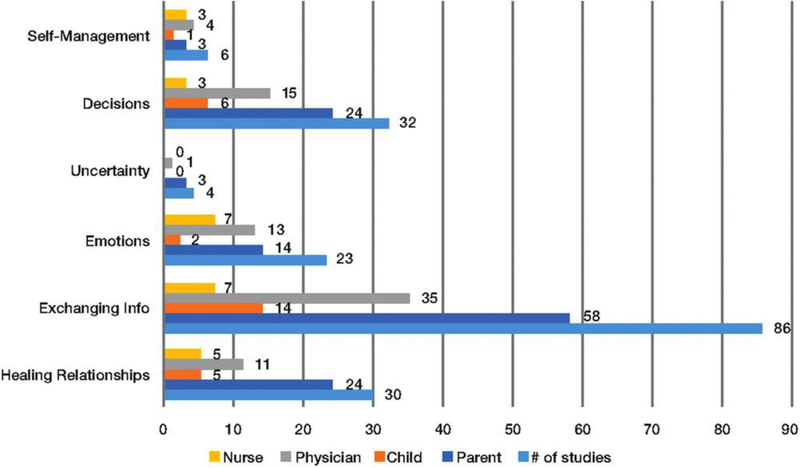
The frequency with which these studies addressed the six functions varied widely from 96% (N = 86/90) for exchanging information to 4% (N = 4/90) for managing uncertainty (Table 3). Additionally, many studies focused on communication of prognosis (32%, N = 29/90) or diagnosis/treatment/toxicity (47%, N = 42/90), yet few studies investigated survivorship/late effects (4%, N = 4/90) or fertility preservation (9%, N = 8/90), as summarized in Figure 2.
FIGURE 2.
Number of studies examining a function and obtaining reports from diverse informants
3.2 |. Fostering healing relationships
Thirty articles addressed “fostering healing relationships,” including 26 descriptive studies and 4 correlational studies. Of the descriptive studies, 20 articles included parental report, 5 child report, 5 physician report, and 5 nursing report. Of the four correlational studies, all included parental report and one additionally included physician report. Overall, three studies included both parent and child report, four parent and physician, and one parent, child, and physician. Three themes were apparent: preferences for communication, barriers to communication, and the use of communication to support aspects of caring.
In articles that elicited preferences from parents and children with cancer, the most common preferences were that clinicians communicate with sensitivity,12,13 honesty,14 and empathy,15,16 that clinicians provide high-quality information12,17 even if it was upsetting,18 and that physicians offer a professional opinion.17,19 Regarding barriers to communication, parents and adolescents were often upset if not provided with sufficient information or if they did not feel they were listened to20 or taken seriously.21 However, parents differed in the amount of information they desired.20 Some nurses reported difficulty in discussing death and poor prognosis with families, especially when they believed parents were not fully informed by their physician.22 Of the studies that highlighted supportive aspects of communication, several articles reinforced that high-quality communication is associated with increased ratings of physician trust,23,24 care,25 sensitivity,25 as well as parental hopefulness26 and peace of mind.27
3.3 |. Exchanging information
“Exchanging information” was addressed in 86 articles, including 70 descriptive studies and 16 correlational studies. Of these 70 descriptive studies, 45 included parental report, 14 child report, 21 physician report, and 5 nursing report. Of the 16 correlational studies, 13 included parental report, 7 physician report, and 2 nursing report. Overall, 6 studies included both parent and child report, 14 parent and physician, and 3 parent, child, and physician. Most “exchanging information” studies focused on providing and receiving information, withholding information, or outcomes of information sharing.
For studies that focused on providing and receiving information, four subthemes were apparent: contents and type of information exchanged, preferences and information needs, how information was processed and understood, and barriers to information exchange. Whether such information exchange took place varied widely depending on the topic (i.e., prognosis,18,28,29 diagnosis and treatment options,15,29–32 trial enrollment,33–36 fertility,37,38 late effects,39,40 and end of life12,17,41,42). Several studies demonstrated that parents have ongoing information needs beginning at diagnosis20,43–48 and carrying through treatment and survivorship49,50; however, parents could also be overwhelmed by large amounts of information.51 Some children reported wanting information directly,52 but some children also expressed discomfort with discussions of death.53 Several studies found that parents want specific54 and clear information,17,19,55 even if the information is upsetting.18
Barriers to information exchange included lack of provider knowledge, experience, or comfort,22,56,57 clinical uncertainty,57 lack of patient/parent comfort or readiness,56,58 unrealistic parental expectations,57 and lack of cultural support.57 Some studies showed that treatment plans were largely understandable,17,35 but several families experienced difficulty absorbing or understanding information regarding fertility,37 research,35,59,60 diagnosis,13,52,61 and poor prognosis.62
Studies that reported on withholding information generally addressed whether children were informed12,25,54,63–67 and whether children should be present during difficult discussions between clinicians and parents.14,16,44,59,68–71 Only one study addressed withholding information from parents.72 Several studies were equivocal regarding preferences for child involvement14,69,70; however, other studies showed parents preferred to hear information about diagnosis and prognosis separate from their children.16,44,71 One study found that most parents thought children should be present during informed consent conferences for research study enrollment59; yet, children in another study were only present at 41% of informed consent conferences.68
Most studies found that provision of high-quality information was associated with desirable outcomes, such as feeling acknowledged,75 comforted,76 hopeful,26,77 having peace of mind,27 and trusting in their physician.23 High-quality information sharing was also associated with parents having their preferred role in decision making78 and being better prepared for self-management.79 However, two studies found the opposite: one found no association between prognostic accuracy and the content of communication or parental information source80; another found more information sharing to be associated with increased anxiety and less control, and unrelated prognostic accuracy.81
3.4 |. Responding to emotions
“Responding to Emotions” was addressed in 23 articles, including 18 descriptive studies and 5 correlational studies. Of the descriptive studies, 10 articles included parental report, 2 child report, 5 physician report, and 7 nursing report. Of the five correlational studies, four included parental report and one physician report. Overall, one study included both parent and child report, and three parent and physician. Three themes were apparent: physician’s role and perceptions, nurse’s role and perceptions, and family’s role and perceptions.
Studies that focused on the physician’s role in emotional support largely found that physicians provide medical information more frequently than they discuss emotions.31,36,82,83 Additionally, physicians were likely to use vague terms57 and withhold sensitive information from children63 when discussing difficult topics such as death. Physicians were also more likely to set boundaries with families than were nurses, and were more likely to defer emotional tasks to nurses. For example, “Doctors explained that an emotional or ‘huggy-buggy’ relationship with parents was inappropriate because doctors were ultimately responsible for the child’s care.”31
Studies that focused on the nurse’s role found that nurses24,84 and families76 largely considered emotional support to be an important aspect of the care that nurses provide. One study found that nurses were more likely to use emotional language than physicians.31 Another study identified that some nurses experienced difficulty when they received negative emotional responses or accusations from families as a result of the child’s poor prognosis.22
Studies that focused on the family’s role and perceptions found that receiving information could elicit positive or negative emotions.13,81,85 One study found that most parents wanted to be engaged in communication and decision making.86 Another found that parents value emotional support.24 When a family’s emotional needs were met with sensitive communication, they reported more trust in the physician23 and higher quality of care.12,25 Several studies identified behaviors and characteristics of communication that provided emotional support: politeness,85 empathy,16,87 compassionate communication and emotional connection,15 honesty and maintaining room for hope,19,87 and staff members showing emotion.15
3.5 |. Managing uncertainty
Only four studies addressed “managing uncertainty,” including three descriptive studies and one correlational study. Of the descriptive studies, two included parental report. The one correlational study included both parental and physician report. In one study, parents felt they were sometimes given too much information, sometimes too little information, and sometimes contradictory or confusing information.20 Another study found that parents and physicians were less likely to agree about prognosis when parents had high levels of confidence in their opinion of prognosis.88 In the third study, parents who felt acknowledged described feeling secure despite uncertainty.75 The fourth study found that many physicians withheld information from adolescents to protect them from uncertainty and anxiety, but this approach was ineffective.63
3.6 |. Making decisions
“Making decisions” was addressed in 32 articles, including 28 descriptive studies and 4 correlational studies. Of the descriptive studies, 20 included parental report, 6 child report, 9 physician report, and 3 nursing report. Of the four correlational studies, all included parental report, and three also included physician report. Overall, 3 studies included parent and child report, 10 parent and physician, and 1 parent, child, and physician. Two themes were apparent: content and characteristics of communication pertaining to decision making, and preferred roles of parents and children.
Families felt their decision making was supported by honesty,14,68 trust,37 being informed,14 being given time to decide,54 and understanding choices.53 Conversations included discussions of risks and benefits,33,37 altruism in trial enrollment,89 prognosis and end of life,12,18,42,77,90 and trial enrollment.17,33,36,54,68,72,89 Some parents reported insufficient discussions of alternatives.35,72
Studies focusing on the preferred roles of stakeholders found that children and adolescents varied in their involvement in decision making. Some studies found children frequently engaged in communication and decision making,65,68 others found limited involvement,36,64,69 and one study found a wide array of roles.66 Parents similarly held a variety of decision-making roles.24,36,46,68,86,91 Though many parents preferred a collaborative role,14,30 participation was sometimes difficult because of their emotional state.13,92 Parents were more likely to fulfill their desired role if communication was deemed to be of “high quality.”78
3.7 |. Enabling patient and family self-management
Only six studies addressed “enabling self-management,” including four descriptive studies and two correlational studies. Of the descriptive studies, one included parental report, one child report, two physician report, three nursing report, and two included report of other staff members. Of the two correlational studies, two included parental and one included physician report. Overall, one study included parent and physician report, and one included parent, child, and physician.
Only one study directly investigated the self-management needs of adolescents, finding that general information about cancer and specific knowledge about treatment options were among the self-management needs of adolescents.79 Other studies focused on aspects of communication that may affect self-management, but did not explicitly link communication with self-management. For example, studies identified physician communication priorities82 and practices63 as well as nursing communication difficulties22 that could limit support for patient and family self-management. Another study found that preparing the parent for circumstances surrounding the child’s death was associated with higher parent rating of physician care.25 Parents were more likely to have received this guidance if a palliative care team was involved in their care.93
4 |. DISCUSSION
This extensive review of provider–parent/patient communication in pediatric oncology has highlighted several important, generalizable lessons for the field. First, children and parents have persistent information needs throughout their illness journeys, but individuals can vary in the amount of information they desire. Uniformly, children and parents prefer communication that is honest, sensitive, empathetic, and hopeful. While parents mostly preferred engagement in communication and decision making, children varied in their desire for inclusion and amount of involvement. Additionally, “high-quality” communication was associated with parental peace of mind, feeling acknowledged and comforted, and greater trust in the physician. Lastly, while many parents reported a desire for physicians to express opinions and emotions, physicians often deferred emotional tasks to nurses. However, many nurses and parents viewed responding to emotions as primarily a nursing task. The current body of literature leaves many unanswered questions about the interaction of communication and emotion. Further study of emotion in communication is especially important given the integral role of emotion in reasoning and decision making.94
The results of this review further support the interconnected model of the functions of communication, as proposed by Epstein and Street.1 In this framework, “the six core functions of patient–clinician communication overlap and interact to produce communication that can affect important health outcomes.”1 In our review of the literature, we found similar characteristics of communication that supported multiple functions. For example, the functions of responding to emotions and fostering healing relationships were both supported by empathy, sensitivity, and compassion. Similarly, the functions of making decisions and fostering healing relationships were both supported by clinician honesty and by parents being well informed. Furthermore, outcomes of communication functions overlapped in many studies, including increased trust in the physician, higher ratings of physician care and sensitivity, and increased parental hopefulness and peace of mind.
Review of this body of literature also reveals striking incongruities in the amount of research dedicated to different functions of communication, content, and populations. While 96% of studies addressed “exchanging information,” only 4% addressed “managing uncertainty” and 7% addressed “enabling patient/family self-management.” Similarly, 68% of studies included parental report and 32% included physician report, but only 16% included the child’s report. Given that children may begin developing autonomous capacity around 10–12 years of age, this lack of research focused on children is concerning.95 Lastly, many studies addressed communication of prognosis, diagnosis, treatment, and toxicity, yet only a small number focused on communication related to survivorship and late effects.
Notably, our search strategy did not identify any studies of interventions focused on improving this communication interaction. While it is possible that our search strategy missed some intervention studies, this is a noticeable deficiency. We do not discount the value of descriptive and correlational studies related to communication. Rather, we see these studies as foundational for the development of future interventions. Importantly, interventions in adult oncology are paving the way for future pediatric interventions. Examples include individualized, real-time communication training sessions,96,97 modifying perspective of clinicians prior to communication interactions,98 and using question prompt lists during interactions.99
Based on this review of the literature, all functions of communication are in need of further study, but different methodologies are needed for different functions. “Exchanging information” has a strong foundation of descriptive and correlational work, and is ripe for innovative experimental studies of interventions. “Fostering healing relationships,” “responding to emotions,” and “making decisions” have a reasonable foundation of descriptive studies but could benefit from further correlational and experimental studies. “Managing uncertainty” and “enabling self-management,” however, have only scarcely been studied and are in great need of foundational work to advance the field. We also propose further emphasis on longitudinal studies that ideally include collaboration across multiple institutions in order to increase sample sizes. Notably, we did not objectively assess quality of evidence and bias for all studies included in this review, therefore we cannot comment specifically on the quality of this body of work. Future systematic reviews should strive to assess all papers prior to publication.
We further recommend attention to the following areas that go beyond functions of communication: integrating children and adolescents into the communication and decision-making process, individualizing communication practices to meet the needs of individual parents and patients at particular time points in their illness journey, development of multidisciplinary communication models that include the roles of physicians, nurses, and other healthcare providers.
In conclusion, communication in pediatric oncology serves several vital functions. Overarching themes in this review included the persistence of information needs over time, the desire for communication that is honest, sensitive, polite, empathetic, and hopeful, and the finding that high-quality communication is associated with parental peace of mind, feeling acknowledged and comforted, and greater trust in the physician. The finding that parents desire honesty while maintaining hope reinforces the concept that hope comes in many forms, of which hope for cure is only one component.100–103 However, research on the communication interaction between healthcare providers and parents or patients is varied in scope and methodology. All studies were descriptive or correlational; none were experimental studies of interventions. Additionally, nearly all studies addressed “exchanging information,” yet few studies addressed “managing uncertainty” or “enabling patient/family self-management.” Future work should address these insufficiently studied functions of communication.
Supplementary Material
ACKNOWLEDGMENTS
The authors would like to thank Lauren Yaeger, MA, MLIS, medical librarian at St. Louis Children’s Hospital for her assistance in developing search criteria and retrieving references. The authors also thank Heidi Walsh, MPH, CHES, for her assistance with reference management.
Funding Information
Grant sponsor: National Center for Advancing Translational Sciences; Grant number: UL1TR000448.
Abbreviation:
- ICU
intensive care unit
- PRISMA
Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines
Footnotes
SUPPORTING INFORMATION
Additional Supporting Information may be found online in the supporting information tab for this article.
CONFLICT OF INTEREST
The authors declare that there is no conflict of interest.
REFERENCES
- 1.Epstein RM, Street RL Jr. Patient-centered communicationin cancer care: promoting healing and reducing suffering. J Nat Cancer Inst. 2007;1:1–222. [Google Scholar]
- 2.Alelwani SM, Ahmed YA. Medical training for communication of bad news: a literature review. J Educ Health Promotion. 2014;3(51):1–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Feraco AM, Brand SR, Mack JW, Kesselheim JC, Block SD, Wolfe J. Communication skills training in pediatric oncology: moving beyond role modeling. Pediatr Blood Cancer. 2016;63(6):966–972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ranmal R, Prictor M, Scott JT. Interventions for improving communication with children and adolescents about their cancer. Cochrane Database Syst Rev. 2008(4):CD002969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.McCarthy MC, Campo M, Drew SE. Pediatric oncology survivorship: conveying risks and communicating information at the right time for the individual. Curr Opin Support Palliat Care. 2013;7(3):289–295. [DOI] [PubMed] [Google Scholar]
- 6.Siembida EJ, Bellizzi KM. The doctor-patient relationship in the adolescent cancer setting: a developmentally focused literature review. J Adoles Young Adult Oncol. 2015;4(3):108–117. [DOI] [PubMed] [Google Scholar]
- 7.Otmani N, Khattab M. Informational support in pediatric oncology: review of the challenges among Arab families. J Cancer Educ. 2016. [DOI] [PubMed] [Google Scholar]
- 8.Khan KS, Kunz R, Kleijnen J, Antes G. Five steps to conducting a systematic review. J R Soc Med. 2003;96(3):118–121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med. 2009;6(7):e1000100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Stangor C Research Methods for the Behavioral Sciences. 4th ed Australia, Belmont, CA: Wadsworth Cengage Learning; 2011. [Google Scholar]
- 11.DuBois JM, Strait M, Walsh H. Is it time to share qualitative research data? Qual Psychol. 2017;Online First Publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Heath J, Clarke N, McCarthy M, Donath S, Anderson V, Wolfe J. Quality of care at the end of life in children with cancer. J Paediatr Child Health. 2009;45(11):656–659. [DOI] [PubMed] [Google Scholar]
- 13.Levi RB, Marsick R, Drotar D, Kodish ED. Diagnosis, disclosure, and informed consent: learning from parents of children with cancer. J Pediatr Hematol Oncol. 2000;22(1):3–12. [DOI] [PubMed] [Google Scholar]
- 14.Zwaanswijk M, Tates K, van Dulmen S, Hoogerbrugge PM, Kamps WA, Bensing JM. Young patients’, parents’, and survivors’ communication preferences in paediatric oncology: results of online focus groups. BMC Pediatr. 2007;7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Snaman JM, Torres C, Duffy B, Levine DR, Gibson DV, Baker JN. Parental perspectives of communication at the end of life at a pediatric oncology institution. J Palliat Med. 2016;19(3):326–332. [DOI] [PubMed] [Google Scholar]
- 16.Zwaanswijk M, Tates K, Van Dulmen S, et al. Communicating with child patients in pediatric oncology consultations: a vignette study on child patients’, parents’, and survivors’ communication preferences. Psychooncology. 2011;20(3):269–277. [DOI] [PubMed] [Google Scholar]
- 17.Hinds PS, Drew D, Oakes LL, et al. End-of-life care preferences of pediatric patients with cancer. J Clin Oncol. 2005;23(36):9146–9154. [DOI] [PubMed] [Google Scholar]
- 18.Mack JW, Wolfe J, Grier HE, Cleary PD, Weeks JC. Communication about prognosis between parents and physicians of children with cancer: parent preferences and the impact of prognostic information. J Clin Oncol. 2006;24(33):5265–5270. [DOI] [PubMed] [Google Scholar]
- 19.Johnson LM, Leek AC, Drotar D, et al. Practical communication guidance to improve phase 1 informed consent conversations and decision-making in pediatric oncology. Cancer. 2015;121(14):2439–2448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Clarke JN, Fletcher P. Communication issues faced by parents who have a child diagnosed with cancer. J Pediatr Oncol Nurs. 2003;20(4):175–191. [DOI] [PubMed] [Google Scholar]
- 21.Essig S, Steiner C, Kuehni CE, Weber H, Kiss A. Improving communication in adolescent cancer care: a multiperspective study. Pediatr Blood Cancer. 2016;63(8):1423–1430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Citak EA, Toruner EK, Gunes NB. Exploring communication difficulties in pediatric hematology: oncology nurses. Asian Pacif J Cancer Prevent. 2013;14(9):5477–5482. [DOI] [PubMed] [Google Scholar]
- 23.El Malla H, Kreicbergs U, Steineck G, Wilderang U, Elborai Yel S, Ylitalo N. Parental trust in health care—a prospective study from the Children’s Cancer Hospital in Egypt. Psychooncology. 2013;22(3):548–554. [DOI] [PubMed] [Google Scholar]
- 24.von Essen L, Enskar K, Skolin I. Important aspects of care and assistance for parents of children, 0–18 years of age, on or off treatment for cancer. Parent and nurse perceptions. Eur J Oncol Nurs. 2001;5(4):254–264. [DOI] [PubMed] [Google Scholar]
- 25.Mack JW, Hilden JM, Watterson J, et al. Parent and physician perspectives on quality of care at the end of life in children with cancer. J Clin Oncol. 2005;23(36):9155–9161. [DOI] [PubMed] [Google Scholar]
- 26.Mack JW, Wolfe J, Cook EF, Grier HE, Cleary PD, Weeks JC. Hope and prognostic disclosure. J Clin Oncol. 2007;25(35):5636–5642. [DOI] [PubMed] [Google Scholar]
- 27.Mack JW, Wolfe J, Cook EF, Grier HE, Cleary PD, Weeks JC. Peace of mind and sense of purpose as core existential issues among parents of children with cancer. Arch Pediatr Adolesc Med. 2009;163(6):519–524. [DOI] [PubMed] [Google Scholar]
- 28.Kamihara J, Nyborn JA, Olcese ME, Nickerson T, Mack JW. Parental hope for children with advanced cancer. Pediatrics. 2015;135(5):868–874. [DOI] [PubMed] [Google Scholar]
- 29.Sanderson A, Hall AM, Wolfe J. Advance care discussions: pediatric clinician preparedness and practices. J Pain Symptom Manage. 2016;51(3):520–528. [DOI] [PubMed] [Google Scholar]
- 30.Bluebond-Langner M, Belasco JB, Goldman A, Belasco C. Understanding parents’ approaches to care and treatment of children with cancer when standard therapy has failed. J Clin Oncol. 2007;25(17):2414–2419. [DOI] [PubMed] [Google Scholar]
- 31.Forsey M, Salmon P, Eden T, Young B. Comparing doctors’ and nurses’ accounts of how they provide emotional care for parents of children with acute lymphoblastic leukaemia. Psychooncology. 2013;22(2):260–267. [DOI] [PubMed] [Google Scholar]
- 32.Parsons SK, Saiki-Craighill S, Mayer DK, et al. Telling children and adolescents about their cancer diagnosis: cross-cultural comparisons between pediatric oncologists in the US and Japan. Psychooncology. 2007;16(1):60–68. [DOI] [PubMed] [Google Scholar]
- 33.Hazen RA, Zyzanski S, Baker JN, Drotar D, Kodish E. Communication about the risks and benefits of phase I pediatric oncology trials. Contemp Clin Trials. 2015;41:139–145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kodish E, Eder M, Noll RB, et al. Communication of randomization in childhood leukemia trials. J Am Med Assoc. 2004;291(4):470–475. [DOI] [PubMed] [Google Scholar]
- 35.Kupst MJ, Patenaude AF, Walco GA, Sterling C. Clinical trials in pediatric cancer: parental perspectives on informed consent. J Pediatr Hematol Oncol. 2003;25(10):787–790. [DOI] [PubMed] [Google Scholar]
- 36.Miller VA, Baker JN, Leek AC, Drotar D, Kodish E. Patient involvement in informed consent for pediatric phase I cancer research. J Pediatr Hematol Oncol. 2014;36(8):635–640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Crawshaw MA, Glaser AW, Hale JP, Sloper P. Male and female experiences of having fertility matters raised alongside a cancer diagnosis during the teenage and young adult years. Eur J Cancer Care. 2009;18(4):381–390. [DOI] [PubMed] [Google Scholar]
- 38.Yeomanson DJ, Morgan S, Pacey AA. Discussing fertility preservation at the time of cancer diagnosis: dissatisfaction of young females. Pediatr Blood Cancer. 2013;60(12):1996–2000. [DOI] [PubMed] [Google Scholar]
- 39.Mellblom AV, Korsvold L, Finset A, Loge J, Ruud E, Lie HC. Providing information about late effects during routine follow-up consultations between pediatric oncologists and adolescent survivors: a video-based, observational study. J Adolesc Young Adult Oncol. 2015;4(4):200–208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Wakefield CE, Butow P, Fleming CA, Daniel G, Cohn RJ. Family information needs at childhood cancer treatment completion. Pediatr Blood Cancer. 2012;58(4):621–626. [DOI] [PubMed] [Google Scholar]
- 41.Bell CJ, Skiles J, Pradhan K, Champion VL. End-of-life experiences in adolescents dying with cancer. Support Care Cancer. 2010;18(7):827–835. [DOI] [PubMed] [Google Scholar]
- 42.Hechler T, Blankenburg M, Friedrichsdorf SJ, et al. Parents’ perspective on symptoms, quality of life, characteristics of death and end-of-life decisions for children dying from cancer. Klin Padiatr. 2008;220(3):166–174. [DOI] [PubMed] [Google Scholar]
- 43.Jackson A, Stewart H, O’Toole M, et al. Pediatric brain tumor patients: their parents’ perceptions of the hospital experience. J Pediatr Oncol Nurs. 2007;24(2):95–105. [DOI] [PubMed] [Google Scholar]
- 44.Kessel RM, Roth M, Moody K, Levy A. Day one talk: parent preferences when learning that their child has cancer. Support Care Cancer. 2013;21(11):2977–2982. [DOI] [PubMed] [Google Scholar]
- 45.Kilicarslan-Toruner E, Akgun-Citak E. Information-seeking behaviours and decision-making process of parents of children with cancer. Eur J Oncol Nurs. 2013;17(2):176–183. [DOI] [PubMed] [Google Scholar]
- 46.McKenna K, Collier J, Hewitt M, Blake H. Parental involvement in paediatric cancer treatment decisions. Eur J Cancer Care. 2010;19(5):621–630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Parker TM, Johnston DL. Parental perceptions of being told their child has cancer. Pediatr Blood Cancer. 2008;51(4):531–534. [DOI] [PubMed] [Google Scholar]
- 48.Ringner A, Jansson L, Graneheim UH. Professional caregivers’ perceptions of providing information to parents of children with cancer. J Pediatr Oncol Nurs. 2011;28(1):34–42. [DOI] [PubMed] [Google Scholar]
- 49.Trask CL, Welch JJ, Manley P, Jelalian E, Schwartz CL. Parental needs for information related to neurocognitive late effects from pediatric cancer and its treatment. Pediatr Blood Cancer. 2009;52(2):273–279. [DOI] [PubMed] [Google Scholar]
- 50.Vetsch J, Rueegg CS, Gianinazzi ME, Bergstrasser E, von der Weid NX, Michel G. Information needs in parents of long-term childhood cancer survivors. Pediatr Blood Cancer. 2015;62(5):859–866. [DOI] [PubMed] [Google Scholar]
- 51.Kastel A, Enskar K, Bjork O. Parents’ views on information in childhood cancer care. Eur J Oncol Nurs. 2011;15(4):290–295. [DOI] [PubMed] [Google Scholar]
- 52.Gibson F, Aldiss S, Bryan G, et al. An exploration of parents’ and professionals’ roles in sharing illness and treatment information with children who have cancer. Arch Dis Child. 2011;96:A83–A84. [Google Scholar]
- 53.Jacobs S, Perez J, Cheng Y, Sill A, Wang J, Lyon M. Adolescent end of life preferences and congruence with their parents’ preferences: results of a survey of adolescents with cancer. Pediatr Blood Cancer. 2015;62(4):710–714. [DOI] [PubMed] [Google Scholar]
- 54.Baker JN, Leek AC, Salas HS, et al. Suggestions from adolescents, young adults, and parents for improving informed consent in phase 1 pediatric oncology trials. Cancer. 2013;119(23):4154–4161. [DOI] [PubMed] [Google Scholar]
- 55.Yap TY, Yamokoski AD, Hizlan S, et al. Informed consent for pediatric phase 1 cancer trials: physicians’ perspectives. Cancer. 2010;116(13):3244–3250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Quinn GP, Vadaparampil ST, King L, et al. Impact of physicians’ personal discomfort and patient prognosis on discussion of fertility preservation with young cancer patients. Patient Educ Couns. 2009;77(3):338–343. [DOI] [PubMed] [Google Scholar]
- 57.Yoshida S, Shimizu K, Kobayashi M, et al. Barriers of healthcare providers against end-of-life discussions with pediatric cancer patients. Jpn J Clin Oncol. 2014;44(8):729–735. 10.1093/jjco/hyu077 [DOI] [PubMed] [Google Scholar]
- 58.Quinn GP, Vadaparampil ST. Fertility preservation and adolescent/young adult cancer patients: physician communication challenges. J Adolesc Health. 2009;44(4):394–400. [DOI] [PubMed] [Google Scholar]
- 59.Cousino MK, Zyzanski SJ, Yamokoski AD, et al. Communicating and understanding the purpose of pediatric phase I cancer trials. J Clin Oncol. 2012;30(35):4367–4372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Koyfman SA, Reddy CA, Hizlan S, Leek AC, Kodish AE, Phase IICRT. Informed consent conversations and documents: a quantitative comparison. Cancer. 2016;122(3):464–469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.O’Shea J, Smith O, O’Marcaigh A, McMahon C, Geoghegan R, Cotter M. Breaking bad news: parents’ experience of learning that their child has leukaemia. Irish Med J. 2007;100(9):588–590. [PubMed] [Google Scholar]
- 62.Lannen P, Wolfe J, MacK J, Onelov E, Nyberg U, Kreicbergs U. Absorbing information about a child’s incurable cancer. Oncology. 2010;78(3–4):259–266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Clemente I Clinicians’ routine use of non-disclosure: prioritizing “protection” over the information needs of adolescents with cancer. Can J Nurs Res. 2007;39(4):19–34. [PMC free article] [PubMed] [Google Scholar]
- 64.de Vries MC, Wit JM, Engberts DP, Kaspers GJL, van Leeuwen E. Pediatric oncologists’ attitudes towards involving adolescents in decision-making concerning research participation. Pediatr Blood Cancer. 2010;55(1):123–128. [DOI] [PubMed] [Google Scholar]
- 65.De Vries M, Bresters D, Engberts D, Wit J, van Leeuwen E. Attitudes of physicians and parents towards discussing infertility risks and semen cryopreservation with male adolescents diagnosed with cancer. Pediatr Blood Cancer. 2009;53(3):386–391. [DOI] [PubMed] [Google Scholar]
- 66.Kelly KP, Pyke-Grimm K, Stewart JL, Hinds PS. Hypothesis generation for childhood cancer communication research: results of a secondary analysis. West J Nurs Res. 2014;36(4):512–533. [DOI] [PubMed] [Google Scholar]
- 67.Watanabe A, Nunes T, de Abreu G. Japanese parents’ perception of disclosing the diagnosis of cancer to their children. Clin Child Psychol Psychiatr. 2014;19(1):125–138. [DOI] [PubMed] [Google Scholar]
- 68.Olechnowicz JQ, Eder M, Simon C, Zyzanski S, Kodish E. Assent observed: children’s involvement in leukemia treatment and research discussions. Pediatrics. 2002;109(5):806–814. [DOI] [PubMed] [Google Scholar]
- 69.Ruhe KM, Badarau DO, Brazzola P, Hengartner H, Elger BS, Wangmo T. Participation in pediatric oncology: views of child and adolescent patients. Psychooncology. 2016;25(9):1036–1042. [DOI] [PubMed] [Google Scholar]
- 70.Young B, Dixon-Woods M, Windridge KC, Heney D. Managing communication with young people who have a potentially life threatening chronic illness: qualitative study of patients and parents. Br Med J. 2003;326(7384):305–308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Young B, Ward J, Salmon P, Gravenhorst K, Hill J, Eden T. Parents’ experiences of their children’s presence in discussions with physicians about Leukemia. Pediatrics. 2011;127(5):e1230–e1238. [DOI] [PubMed] [Google Scholar]
- 72.Miller VA, Cousino M, Leek AC, Kodish ED. Hope and persuasion by physicians during informed consent. J Clin Oncol. 2014;32(29):3229–3235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Arabiat DH, Alqaissi NM, Hamdan-Mansour AM. Children’s knowledge of cancer diagnosis and treatment: Jordanian mothers’ perceptions and satisfaction with the process. Int Nurs Rev. 2011;58(4):443–449. [DOI] [PubMed] [Google Scholar]
- 74.Badarau DO, Wangmo T, Ruhe KM, et al. Parents’ challenges and physicians’ tasks in disclosing cancer to children. A qualitative interview study and reflections on professional duties in pediatric oncology. Pediatr Blood Cancer. 2015;62(12):2177–2182. [DOI] [PubMed] [Google Scholar]
- 75.Ringner A, Jansson L, Graneheim UH. Parental experiences of information within pediatric oncology. J Pediatr Oncol Nurs. 2011;28(4):244–251. [DOI] [PubMed] [Google Scholar]
- 76.Young B, Hill J, Gravenhorst K, Ward J, Eden T, Salmon P. Is communication guidance mistaken qualitative study of parent-oncologist communication in childhood cancer. Br J Cancer. 2013;109(4):836–843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Nyborn JA, Olcese M, Nickerson T, Mack JW. “Don’t try to cover the sky with your hands”: parents’ experiences with prognosis communication about their children with advanced cancer. J Palliat Med. 2016;19(6):626–631. [DOI] [PubMed] [Google Scholar]
- 78.Mack JW, Wolfe J, Cook EF, Grier HE, Cleary PD, Weeks JC. Parents’ roles in decision making for children with cancer in the first year of cancer treatment. J Clin Oncol. 2011;29(15):2085–2090. [DOI] [PubMed] [Google Scholar]
- 79.Stinson JN, Sung L, Gupta A, et al. Disease self-management needs of adolescents with cancer: perspectives of adolescents with cancer and their parents and healthcare providers. J Cancer Surviv. 2012;6(3):278–286. [DOI] [PubMed] [Google Scholar]
- 80.Miller KS, Vannatta K, Vasey M, Yeager N, Compas BE, Gerhardt CA. Health literacy variables related to parents’ understanding of their child’s cancer prognosis. Pediatr Blood Cancer. 2012;59(5):914–918. [DOI] [PubMed] [Google Scholar]
- 81.Miller VA, Drotar D, Burant C, Kodish E. Clinician-parent communication during informed consent for pediatric leukemia trials. J Pediatr Psychol. 2005;30(3):219–229. [DOI] [PubMed] [Google Scholar]
- 82.Bradlyn AS, Kato PM, Beale IL, Cole S. Pediatric oncology professionals’ perceptions of information needs of adolescent patients with cancer. J Pediatr Oncol Nurs. 2004;21(6):335–342. [DOI] [PubMed] [Google Scholar]
- 83.Yingling J Verbal responses of children and their supportive providers in a pediatric oncology unit. J Health Commun. 2000;5(4):371–377. [DOI] [PubMed] [Google Scholar]
- 84.Franca JR, da Costa SF, Lopes ME, da Nobrega MM, de Franca IS. The importance of communication in pediatric oncology palliative care: focus on humanistic nursing theory. Rev Latinoam Enfermagem. 2013;21(3):780–786. [DOI] [PubMed] [Google Scholar]
- 85.Tremolada M, Bonichini S, Pillon M, Schiavo S, Carli M. Eliciting adaptive emotion in conversations with parents of children receiving therapy for leukemia. J Psychosoc Oncol. 2011;29(3):327–346. [DOI] [PubMed] [Google Scholar]
- 86.de Vos MA, Bos AP, Plotz FB, et al. Talking with parents about end-of-life decisions for their children. Pediatrics. 2015;135(2):e465–e476. [DOI] [PubMed] [Google Scholar]
- 87.Orioles A, Miller VA, Kersun LS, Ingram M, Morrison WE. To be a phenomenal doctor you have to be the whole package: physicians’ interpersonal behaviors during difficult conversations in pediatrics. J Palliat Med. 2013;16(8):929–933. [DOI] [PubMed] [Google Scholar]
- 88.Mack JW, Cook EF, Wolfe J, Grier HE, Cleary PD, Weeks JC. Understanding of prognosis among parents of children with cancer: parental optimism and the parent-physician interaction. J Clin Oncol. 2007;25(11):1357–1362. [DOI] [PubMed] [Google Scholar]
- 89.Simon C, Eder M, Kodish E, Siminoff L. Altruistic discourse in the informed consent process for childhood cancer clinical trials. Am J Bioeth. 2006;6(5):40–47. [DOI] [PubMed] [Google Scholar]
- 90.Wolfe J, Klar N, Grier HE, et al. Understanding of prognosis among parents of children who died of cancer: impact on treatment goals and integration of palliative care. J Am Med Assoc. 2000;284(19):2469–2475. [DOI] [PubMed] [Google Scholar]
- 91.de Vos MA, van der Heide A, Maurice-Stam H, et al. The process of end-of-life decision-making in pediatrics: a national survey in the Netherlands. Pediatrics. 2011;127(4):e1004–e1012. [DOI] [PubMed] [Google Scholar]
- 92.Pyke-Grimm KA, Stewart JL, Kelly KP, Degner LF. Parents of children with cancer: factors influencing their treatment decision making roles. J Pediatr Nurs. 2006;21(5):350–361. [DOI] [PubMed] [Google Scholar]
- 93.Kassam A, Skiadaresis J, Alexander S, Wolfe J. Differences in end-of-life communication for children with advanced cancer who were referred to a palliative care team. Pediatr Blood Cancer. 2015;62(8):1409–1413. [DOI] [PubMed] [Google Scholar]
- 94.Haidt J The Righteous Mind: Why Good People are Divided by Politics and Religion. 1st ed New York: Pantheon Books; 2012. [Google Scholar]
- 95.Hein IM, De Vries MC, Troost PW, Meynen G, Van Goudoever JB, Lindauer RJ. Informed consent instead of assent is appropriate in children from the age of twelve: policy implications of new findings on children’s competence to consent to clinical research. BMC Med Ethics. 2015;16(1):76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Wuensch A, Goelz T, Ihorst G, et al. Effect of individualized communication skills training on physicians’ discussion of clinical trials in oncology: results from a randomized controlled trial. BMC Cancer. 2017;17(1):264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Epstein RM, Duberstein PR, Fenton JJ, et al. Effect of a patient-centered communication intervention on oncologist-patient communication, quality of life, and health care utilization in advanced cancer: the VOICE Randomized clinical trial. JAMA Oncol. 2017;3(1):92–100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Gouveia L, Janvier A, Dupuis F, Duval M, Sultan S. Comparing two types of perspective taking as strategies for detecting distress amongst parents of children with cancer: a randomised trial. PLoS One. 2017;12(4):e0175342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Eggly S, Hamel LM, Foster TS, et al. Randomized trial of a question prompt list to increase patient active participation during interactions with black patients and their oncologists. Patient Educ Couns. 2017;100(5):818–826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Feudtner C The breadth of hopes. N Engl J Med. 2009;361(24):2306–2307. [DOI] [PubMed] [Google Scholar]
- 101.Feudtner C Responses from palliative care: hope is like water. Perspect Biol Med. 2014;57(4):555–557. [DOI] [PubMed] [Google Scholar]
- 102.Hill DL, Miller V, Walter JK, et al. Regoaling: a conceptual model of how parents of children with serious illness change medical care goals. BMC Palliat Care. 2014;13(1):9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Rosenberg AR, Feudtner C. What else are you hoping for? Fostering hope in paediatric serious illness. Acta Paediatr. 2016;105(9):1004–1005. [DOI] [PubMed] [Google Scholar]
- 104.Hilden JM, Emanuel EJ, Fairclough DL, et al. Attitudes and practices among pediatric oncologists regarding end-of-life care: results of the 1998 American Society of Clinical Oncology survey. J Clin Oncol. 2001;19(1):205–212. [DOI] [PubMed] [Google Scholar]
- 105.Kaye E, Mack JW. Parent perceptions of the quality of information received about a child’s cancer. Pediatr Blood Cancer. 2013;60(11):1896–1901. [DOI] [PubMed] [Google Scholar]
- 106.Marshall PA, Magtanong RV, Leek AC, Hizlan S, Yamokoski AD, Kodish ED. Negotiating decisions during informed consent for pediatric Phase I oncology trials. J Empirical Res Hum Res Ethics. 2012;7(2):51–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Rosenberg AR, Orellana L, Kang TI, et al. Differences in parent-provider concordance regarding prognosis and goals of care among children with advanced cancer. J Clin Oncol. 2014;32(27):3005–3011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Vadaparampil ST, Clayton H, Quinn GP, King LM, Nieder M, Wilson C. Pediatric oncology nurses’ attitudes related to discussing fertility preservation with pediatric cancer patients and their families. J Pediatr Oncol Nurs. 2007;24(5):255–263. [DOI] [PubMed] [Google Scholar]
- 109.Steele AC, Kaal J, Thompson AL, et al. Bereaved parents and siblings offer advice to health care providers and researchers. J Pediatr Hematol Oncol. 2013;35(4):253–259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Gibson F, Aldiss S, Horstman M, Kumpunen S, Richardson A. Children and young people’s experiences of cancer care: A qualitative research study using participatory methods. International Journal of Nursing Studies 2010;47(11):1397–1407. [DOI] [PubMed] [Google Scholar]
- 111.Scrimin S, Axia G, Tremolada M, Pillon M, Capello F, Zanesco L. Conversational strategies with parents of newly diagnosed leukaemic children: an analysis of 4880 conversational turns. Support Care Cancer. 2005;13(5):287–294. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.