Key Points
Question
What are the health system factors that support or impair the ability of nonphysician health workers to treat noncommunicable diseases in low- and middle-income countries?
Findings
This systematic review and qualitative analysis examined 15 systematic reviews, encompassing 71 studies. These studies consistently demonstrated 6 key lessons of successful care by nonphysician health workers: careful staff recruitment, detailed training, authorization to provide autonomous care, adequate medications and supplies, reliable data systems, and fair, performance-based compensation.
Meaning
Effective, scalable care for noncommunicable diseases led by nonphysicians is feasible in diverse low-resource settings but requires several common, key implementation steps.
This systematic review and qualitative analysis examines the health system barriers to and facilitators of care for noncommunicable diseases by nonphysician health workers in low- and middle-income countries.
Abstract
Importance
Cardiovascular disease, cancer, and other noncommunicable diseases (NCDs) are the leading causes of mortality in low- and middle-income countries. Previous studies show that nonphysician health workers (NPHWs), including nurses and volunteers, can provide effective diagnosis and treatment of NCDs. However, the factors that facilitate and impair these programs are incompletely understood.
Objective
To identify health system barriers to and facilitators of NPHW-led care for NCDs in low- and middle-income countries.
Data Sources
All systematic reviews in PubMed published by May 1, 2018.
Study Selection
The search terms used for this analysis included “task shifting” and “non-physician clinician.” Only reviews of NPHW care that occurred entirely or mostly in low- and middle-income countries and focused entirely or mostly on NCDs were included. All studies cited within each systematic review that cited health system barriers to and facilitators of NPHW care were reviewed.
Data Extraction and Synthesis
Assessment of study eligibility was performed by 1 reviewer and rechecked by another. The 2 reviewers extracted all data. Reviews were performed from November 2017 to July 2018. All analyses were descriptive.
Main Outcomes and Measures
All barriers and facilitators mentioned in all studies were tallied and sorted according to the World Health Organization’s 6 building blocks for health systems.
Results
This systematic review and qualitative analysis identified 15 review articles, which cited 156 studies, of which 71 referenced barriers to and facilitators of care. The results suggest 6 key lessons: (1) select qualified NPHWs embedded within the community they serve; (2) provide detailed, ongoing training and supervision; (3) authorize NPHWs to prescribe medication and render autonomous care; (4) equip NPHWs with reliable systems to track patient data; (5) furnish NPHWs consistently with medications and supplies; and (6) compensate NPHWs adequately commensurate with their roles.
Conclusions and Relevance
Although the health system barriers to NPHW screening, treatment, and control of NCDs and their risk factors are numerous and complex, a diverse set of care models has demonstrated strategies to address nearly all of these challenges. These facilitating approaches—which relate chiefly to strong, consistent NPHW training, guidance, and logistical support—generate a blueprint for the creation and scale-up of such programs adaptable across multiple chronic diseases, including in high-income countries.
Introduction
Noncommunicable diseases (NCDs) are the leading causes of premature death worldwide.1 Noncommunicable diseases are increasingly prevalent in low- and middle-income countries (LMICs), especially their most vulnerable communities,2,3 where human resources for health are severely limited.4 More than one-half of LMICs have fewer than 1 physician per 1000 people,5 which is the minimal threshold advised by the World Health Organization (WHO), and in many LMICs, less than one-quarter of physicians practice in rural areas where one-half of the population lives.6
Fortunately, evidence demonstrates that nonphysician health workers (NPHWs) (ie, persons without a medical doctorate degree who render health care)7,8,9,10 can render multiple aspects of care presumed to require a physician.7,8 Models of care that employ NPHWs—including health professionals (eg, nurses) and laypeople (eg, community health workers [CHWs])—have successfully treated many causes of death and disability, especially maternal-child mortality and HIV/AIDS.7,8,9
Models that successfully leverage NPHWs for NCD control also show promise.10 Pilot studies11,12,13 demonstrate that NPHWs can accurately perform cardiovascular risk screening to identify high-risk patients and counsel them on behavior change. In addition, NPHWs can screen for and treat risk factors associated with cardiovascular disease, such as depression,14,15 diabetes,16 and hypertension,16 including by prescribing medication, and can track and improve patients’ adherence to these therapies. Nonphysician health workers can also screen for cancers17,18 and treat epilepsy19 and asthma,20 among other chronic diseases.
However, the rapid increase of NCDs in LMICs requires the scale-up of these programs into global initiatives,21,22 as recent United Nations summits have demanded.23,24 This demand poses a problem: understanding which elements of health systems (eg, governance and delivery structures) support or hinder NPHWs in the care cascade.10
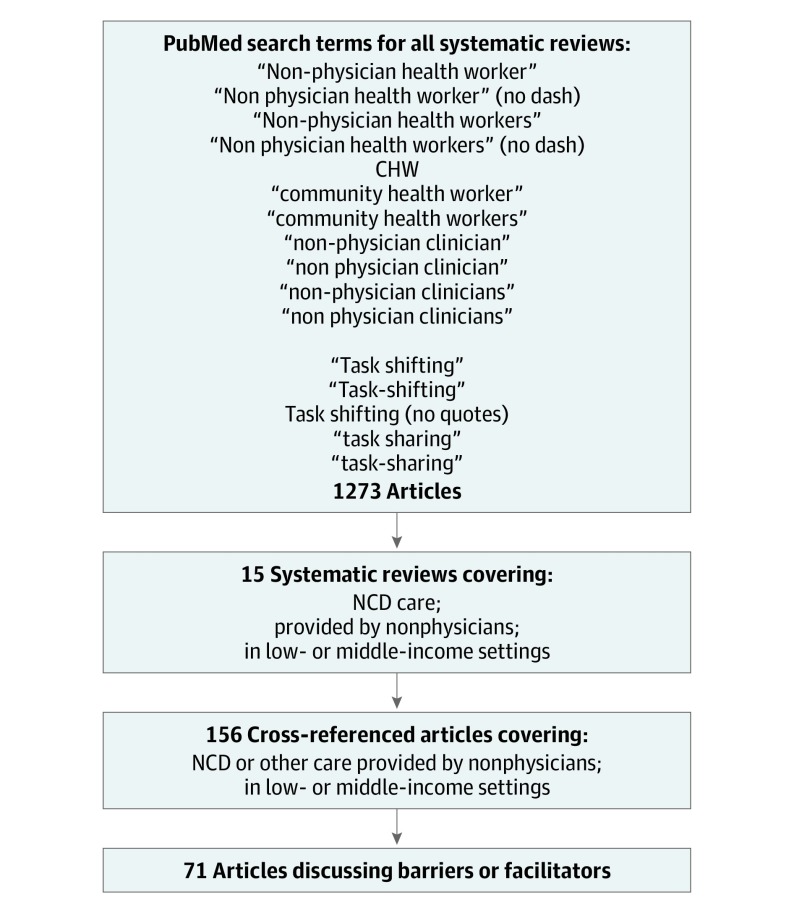
Methods
We undertook a systematic review and qualitative analysis to identify and analyze health system barriers to and facilitators of NPHW-led care for NCDs, as detailed within systematic reviews of these interventions in LMICs. We defined a health system according to the WHO Health Systems Framework’s 6 building blocks25,26: service delivery, health workforce, governance, information systems, medication access, and financing. This descriptive analysis of these heterogeneous interventions did not compile quantitative outcomes, nor did it evaluate a hypothesis. We conducted and reported this review per the Meta-analysis of Observational Studies in Epidemiology (MOOSE) reporting guideline,27 and we display studies identified, screened, reviewed, and included per the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) reporting guideline28 in Figure 1. We did not seek formal review from an institutional review board because we limited our study to published information and did not engage with any human subjects.
Figure 1. Process for Identifying Relevant Articles.
Flowchart shows search terms and criteria used to identify relevant articles for analysis. CHW indicates community health worker; NCD, noncommunicable disease.
Objectives of the Review
We aimed to identify all systematic reviews of initiatives leveraging NPHWs for the treatment of NCDs in LMICs. We defined an NCD as any chronic disease independent of infection, but included long-term conditions caused by infection, such as poststreptococcal rheumatic heart disease.29 We defined LMICs according to 2016 World Bank criteria.30 We considered a study to be leveraging NPHWs if these staff engaged in clinical decision-making for patient care, regardless of physician supervision. This approach includes models for both task-shifting completely from physicians to NPHWs and task-sharing, in which NPHWs assume care under physician oversight.10
Literature Searching
We began our review with 6 systematic reviews already known to us that addressed all of the aforementioned subjects (ie, sentinel reviews). One reviewer (D.J.H.), a clinician-investigator trained in implementation science and public health, searched PubMed from its inception to May 1, 2018, for all systematic reviews that examined NCD care performed by NPHWs in LMICs. Our search terms, developed in consultation with a librarian specializing in advanced search techniques,31 included “non-physician health worker(s),” “task-shifting,” “task-sharing,” “community health worker,” “CHW,” or “non-physician clinician(s)” (Figure 1). We did not expressly search for terms such as “nurse” or “health system,” nor did we exclude them. We excluded all articles that did not focus on NCD care, were not conducted entirely or primarily in LMICs, or were not systematic reviews. A second reviewer (R.J.), a clinician-investigator with expertise in systematic reviews,10 repeated the first reviewer’s search independently. We did not use search software or manual searching, nor did we search databases other than PubMed. Both searches agreed completely and identified all 6 aforementioned reviews, as well as 9 others, all written in English. We quantified the rigor of these 15 reviews using the A Measurement Tool to Assess Systematic Reviews–2 tool, which is designed to evaluate systematic reviews of health care interventions.32
Study Eligibility and Data Extraction
Using review methods derived from Green et al,33 Iwelunmor et al,34 and Popay et al,35 2 coauthors (D.J.H. and A.K., who was then a medical student with public health expertise) reviewed each of these systematic reviews in detail. Each reviewer identified every article referenced within each document that concerned NPHW care for NCDs, referenced barriers to and facilitators of NPHW care (for NCDs or other conditions), was a systematic review, or was referenced in 2 or more systematic reviews. This approach intended to identify any barriers and facilitators of NPHW care relevant to NCD control, but also any systematic reviews that referenced the same but that we had overlooked. The reviewer then examined the abstract of each such article to determine whether it appeared to examine health system issues affecting NPHW-led NCD care. We read each article that explored these issues and identified all concepts related to health systems. We did not contact authors for further details and limited our review to articles published in English. We performed this review from November 2017 to July 2018. Each coauthor who reviewed each article classified the NPHW barriers and facilitators using the WHO’s building block framework,25,26 given its extensive prior use and validation in health systems research. The 2 coauthors (D.J.H. and A.K.) reviewed each other’s classification list for agreement. When they could not reach consensus, they consulted a third coauthor (R.J.) for a final decision.
Categorization of Study Outcomes
After compiling the classification list of health system concepts, we tabulated each documented barrier or facilitator in each reviewed study, as classified by D.J.H. and A.K. Because the study outcomes were heterogeneous, and because our objective was to review qualitative health system factors within these studies rather than those outcomes, we did not perform any meta-analyses or other quantitative analyses, nor did we quantify the quality of these studies apart from the A Measurement Tool to Assess Systematic Reviews calculation.32 After compiling all barriers and facilitators, D.J.H. and A.K. qualitatively reviewed the results for key themes, with feedback from R.J. and the other coauthors. Our goal was to identify actionable elements of an NPHW care intervention (eg, how staff are recruited, supervised, or compensated) that appeared to influence the success or failure of the program in delivering care. We used grounded theory—that is, the iterative review of data to code barriers and facilitators and then sort them into concepts—given that our goal was to describe data rather than test a hypothesis.36 The report follows the Standards for Reporting Qualitative Research (SRQR) reporting guideline.37
Statistical Analysis
We did not undertake any statistical analysis apart from the tally of barriers and facilitators.
Results
Our PubMed search yielded 1273 publications. The search terms are shown in the eAppendix in the Supplement. Among these results, we identified 15 systematic reviews9,10,38,39,40,41,42,43,44,45,46,47,48,49,50 that focused on NCDs and significantly involved LMICs (Table 1). These documents referenced a total of 156 unique articles. Of these, we identified 71 unique articles that met further review criteria defined in the Methods section (Figure 1). We summarize this content in Table 2, organizing content by key measures of health care performance: quality, access, safety, and coverage.51
Table 1. Characteristics of Key Articles Used in Review.
| Study | Type | Disease or Condition Covered | Scope | Studies Included, No. (Total Cited, No.) | WHO Building Blocks Addressed | Types of NPHW Participants | Total Study Participants, No. |
|---|---|---|---|---|---|---|---|
| Mutamba et al,42 2013 | Systematic review | Mental, neurological, and substance abuse disorders | All studies comparing lay community health workers community-level care for these diseases to a control in LMICs | 5 (15) | Service delivery, health workforce | Lay community health workers | 15 039 (7900 intervention; 7139 control) |
| Joshi et al,10 2014 | Systematic review | All NCDs | All peer-reviewed, English language articles up to 2013 that discuss task-shifting of NCDs to NPHWs | 16 (22) | Health workforce, medication access, governance | Nurses or laypersons without medical training | Not provided |
| Ogedegbe et al,45 2014 | Systematic review | CVD | All peer-reviewed, English-language randomized clinical trials up to 2013 to evaluate task-shifting for CVD management in LMICs | 2 (3) | Service delivery, health workforce, information systems, governance | Nonphysician clinicians involved in treatment or risk management | 3002 |
| Khetan et al,40 2017 | Systematic review | CVD | All articles from 1990-2015 involving CHWs for CVD (no other NCDs; no other NPHWs); not limited to randomized clinical trials. | 8 (11) | Service delivery, health workforce | CHWs (persons trained in intervention but without formal health training) | 78 524 |
| Jeet et al,49 2017 | Systematic review | All NCDs (apart from mental health) | All randomized clinical trials from 2000-2015 involving CHWs for NCDs (no other trial types; no other NPHWs) | 5 (16) | NA | CHWs, but these included nurses and “health promoters” among many other NPHWs | 6621 (Diastolic blood pressure); 6782 (systolic blood pressure); 1342 (diabetes) 7302 (tobacco use) inter alia |
| Schneider et al,9 2016 | Scoping review | All diseases | All articles from 2005-2014 that described an LMIC CHW intervention, regardless of condition | 11 (678) | NA | CHWs (lacking formal nursing or medical training) | Not provided |
| Padmanathan et al,41 2013 | Systematic review | Mental illness | All English-language peer-reviewed and gray literature (any study design) on feasibility and acceptability of task-sharing for mental health care in LMICs | 8 (21) | Service delivery, health workforce | Any nonspecialist clinician (including nurses, medical officers, and CHWs) | >1116 (Data incomplete) |
| Abdel-All et al,44 2017 | Systematic review | CVD | All peer-reviewed studies published until December 2016 regarding training of CHWs for prevention or control of CVD (and/or risk factors) in LMICs | 2 (8) | Health workforce | CHWs (from community; usually lack formal training) | 722 |
| Seidman et al,48 2017 | Systematic review | All diseases | All literature regarding the cost-effectiveness of nonphysicians for care provision in LMICs (for NCD and non-NCD care) | 2 (34) | NA | Any less-specialized health worker (including assistant medical officers) | Not provided |
| Chowdhary et al,43 2014 | Systematic review | Perinatal depression | All literature regarding nonspecialist (including generalist physician) perinatal depression care in LMICs | 2 (9) | Service delivery, health workforce | Nonspecialist health workers including nurses, CHWs, mothers | 14 555 (7526 Intervention; 7029 control) |
| Barnett et al,39 2017 | Systematic review | Mental illness | All literature regarding CHW (not other NPHWs) care for mental health care in LMIC and high-income countries | 9 (39) | Service delivery | CHWs (interventionists without mental health training and from community) | 10 199 |
| Hill et al,47 2017 | Systematic review | Diabetes | All literature regarding use of CHWs (not other NPHWs) care for diabetes prevention (not treatment) in LMICs and high-income countries | 1 (30) | NA | Lay CHWs (nonprofessionals recruited usually from community served) | 5834 (Data incomplete) |
| Alaofè et al,50 2017 | Systematic review | Diabetes | All literature regarding use of CHWs (not other NPHWs) care for diabetes prevention and treatment in LMICs | 5 (10) | NA | CHWs (community members without formal health training) | 69 998 |
| Gatuguta et al,38 2017 | Systematic review | Sexual violence, trauma | All literature regarding use of CHWs to treat survivors of sexual violence in LMICs and high-income countries | 2 (7) | Health workforce | CHWs (community members without formal health training) | 961 (Data incomplete) |
| Javadi et al,46 2017 | Systematic review | Mental illness | All literature regarding nonphysician task-shifting for mental health care in LMICs | 23 (30) | NA | Laypersons with minimal mental health training | 701 864 (Data incomplete) |
Abbreviations: CHW, community health worker; CVD, cardiovascular disease; LMIC, low- and middle-income country; NA, not applicable; NCD, noncommunicable disease; NPHW, nonphysician health worker; WHO, World Health Organization.
Table 2. Key Barriers and Facilitators to NPHW Care for Noncommunicable Diseases.
| Building Block | Facilitators | Barriers | Key Themes | Key Conclusions | Care Aspects: Access, Coverage, Quality, Safety |
|---|---|---|---|---|---|
| Service delivery | Home-based or local care; clinician cultural sensitivity; integration of multiple conditions; consistent protocols for patient tracking | Patient education without other care provision; limited patient health literacy; patient transport and safety barriers to accessing care; too few auxiliary and supervisory staff; unclear NPHW roles | Logistics; infrastructure; cultural interaction or stigma | Clinicians benefit from close proximity to the community they serve (home visits or local clinics). Culturally sensitive, locally understandable messages are crucial. Adequate numbers of primary and backup clinicians matter. A clear scope of NPHW care is helpful. Facility-based referral is critical for complex cases and NPHW confidence. | Access: physical and cultural proximity to patients is crucial. Coverage: greater quantity, length, and scope of visits boosts coverage. Quality: protocols for what care is covered, and how patients are tracked, ensure consistency. Safety: patient (and sometimes clinician) safety sometimes at risk in accessing care. |
| Health workforce | Frequent, intensive training; close supervision; specific care delivery algorithms; integration of role with other clinicians | Delays in training; poor staff retention; lack of clear protocols; excessive workload; lack of oversight; limited NPHW literacy | Training; role and expectation; oversight | Clinicians require rigorous, clear, continuous training. Protocol-based workflow that is straightforward and reasonable in expectation. Oversight and backup by other clinicians is crucial. Careful selection and incentive structure may help locate, retain strong clinicians. | Access: poor staff retention impairs patients’ access. Coverage: intensive training boosts breadth of conditions treated. Quality: checklists and algorithms for care boost delivery standards. Safety: close oversight of NPHWs protects patient safety and may prevent errors. |
| Governance | Authorization for NPHWs to prescribe medication; integration with other staff roles; engagement of program with local authorities | Lack of authority to prescribe medication; no policies recognizing NPHW roles; skepticism of NPHW care capacity; political upheaval | Political engagement; codification of NPHW role | Policy makers should recognize the evidence base for NPHW care and define their roles accordingly. NPHWs should have care authority commensurate to the evidence base. Roles of NPHWs and other clinicians should be clearly defined relative to other cadres. Programs should promote stable engagement with communities. | Access: engaging community leaders makes patients aware of available programs. Coverage: ability for NPHWs to give medication improves breadth of conditions treated. Quality: close access to supervisory staff boosts quality of care delivery. Safety: clear roles for NPHWs, other clinicians promote safe scope of practice commensurate with experience. |
| Information systems | Electronic or paper record systems; written patient transfer notes; patient appointment calls or reminder letters; telemedicine consultation mechanisms | Absent data collection infrastructure; difficulty tracking patient records; poor monitoring of disease outcomes | Contact with patients; storage and retention of patient data | Systems to generate and locate patient data are helpful. These systems may aid patients in keeping appointments. | Access: reminder letters, calls, and texts help reach patients. Coverage: telemedicine consults may help NPHWs treat more conditions. Quality: data tracking systems improve care continuity. Safety: patient and disease surveillance may minimize errors. |
| Medication access | Consistent medication availability; supply chain management staff; compensation of supply, transport costs for medication | Medications and supplies out of stock; staff unfamiliarity with medication availability, proper usage | Supply chains or access pathways; NPHW capacity to use or prescribe medication | Consistent medication and supply chains aid care. Donor support for supply chain logistics can boost consistency. Retaining logistical staff to oversee process may also help. | Access: strong supply chains help patients consistently obtain medications. Coverage: broader formulary allows greater breadth of care. Quality: adequate medications, supplies help adhere to latest care guidelines. Safety: reliable suppliers ensure safe medications. |
| Financing | Performance-based compensation; donor awareness of local needs | Lack of monetary performance incentives; low clinician pay; underfinance of patient care infrastructure | Supply-side issues (eg, program funding, NPHW salary); demand-side issues (eg, financing patient access) | Clinicians should be adequately compensated. Pay-for-performance models help. Sufficient investment in care delivery system also key. | Access: stronger care infrastructure (and insurance schemes) help patients reach care. Coverage: donor awareness of local disease burden helps finance relevant care packages. Quality: pay-for-performance boosts level of care provided. Safety: adequate funding ensures safe, functional care infrastructure. |
Abbreviation: NPHW, nonphysician health worker.
Results varied in scope and content across building blocks, and the diseases discussed in the studies were heterogeneous (Table 2; eTable and eReferences in the Supplement). There were a total of 174 barriers and 170 facilitators. Among both barriers and facilitators, service delivery (69 barriers and 54 facilitators) and health workforce (46 barriers and 62 facilitators) factors appeared most commonly, with governance (17 barriers and 23 facilitators), information systems (12 barriers and 19 facilitators), medication access (12 barriers and 7 facilitators), and financing (13 barriers and 8 facilitators) factors arising intermittently. Among the NCDs covered within these 15 articles, cardiovascular conditions and mental illness were the most common (3 studies each); there were 2 studies pertaining to multiple NCDs, 2 pertaining to diabetes, and only 1 pertaining to sexual violence. Most systematic reviews were robust, scoring between 5 and 14 on an A Measurement Tool to Assess Systematic Reviews–2 scale of 13 to 16 items (Table 3). Among the 71 cross-referenced articles, the diseases treated and delivery context were heterogeneous, with neither grossly associated with specific care barriers or facilitators (Table 2; eTable and eReferences in the Supplement).
Table 3. A Measurement Tool to Assess Systematic Reviews–2 Evaluation of Systematic Reviews.
| Source | PICO Use | Protocol A Priori | Study Design Selection | Robust Search Strategy | Duplicate Study Selection | Duplicate Data Extraction | List of Excluded Studies | Detail Given | RoB Assessed | Funders Listed | Sound Meta-analysis Method | RoB Noted in Meta-analysis | RoB Impact Explored | Heterogeneity | Publication Bias | COI | Final Scorea |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mutamba et al,42 2013 | Yes | Yes | Yes | Yes | No | No | Yes | Yes | Yes | No | NA | NA | Yes | Yes | NA | Yes | 10/13 |
| Joshi et al,10 2014 | No | Yes | No | Yes | Yes | Yes | Yes | Yes | No | No | NA | NA | No | Yes | NA | Yes | 7/13 |
| Ogedegbe et al,45 2014 | Yes | Yes | No | Yes | Yes | Yes | Yes | Yes | Yes | No | NA | NA | No | No | NA | Yes | 8/13 |
| Khetan et al,40 2017 | No | Yes | No | Yes | No | No | Yes | Yes | No | No | NA | NA | No | Yes | NA | Yes | 5/13 |
| Jeet et al,49 2017 | Yes | Yes | No | Yes | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | Yes | Yes | 14/16 |
| Schneider et al,9 2016 | No | Yes | Yes | Yes | Yes | Yes | Yes | Yes | No | No | NA | NA | No | No | NA | Yes | 7/13 |
| Padmanathan et al,41 2013 | No | Yes | No | Yes | No | No | Yes | Yes | Yes | No | NA | NA | Yes | No | NA | No | 6/13 |
| Abdel-All et al,44 2017 | No | Yes | No | Yes | Yes | Yes | Yes | Yes | Yes | No | NA | NA | No | No | NA | Yes | 8/13 |
| Seidman et al,48 2017 | No | Yes | No | Yes | Yes | No | Yes | Yes | No | No | NA | NA | Yes | No | NA | Yes | 7/13 |
| Chowdhary et al,43 2014 | Yes | Yes | No | Yes | No | Yes | Yes | Yes | No | No | NA | NA | No | No | NA | No | 6/13 |
| Barnett et al,39 2017 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | No | No | NA | NA | No | Yes | NA | Yes | 10/13 |
| Hill et al,47 2017 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | No | No | NA | NA | No | No | NA | Yes | 9/13 |
| Alaofè et al,50 2017 | No | Yes | No | Yes | Yes | Yes | Yes | Yes | Yes | No | NA | NA | No | Yes | NA | Yes | 8/13 |
| Gatuguta et al,38 2017 | No | Yes | Yes | Yes | No | No | Yes | No | No | No | NA | NA | No | No | NA | Yes | 5/13 |
| Javadi et al,46 2017 | No | Yes | No | Yes | Yes | Yes | Yes | Yes | Yes | No | NA | NA | No | No | NA | Yes | 8/13 |
Abbreviations: COI, conflict of interest; NA, not applicable; PICO, population studied, intervention performed, comparison group, and outcome; RoB, risk of bias.
A Measurement Tool to Assess Systematic Reviews–2 has a scale of 13 to 16 items.
Service Delivery
Three themes emerged among service delivery barriers: logistics, infrastructure, and stigma. Logistical problems included patient difficulty reaching clinics, and, conversely, health worker difficulties reaching patients’ homes.38,39,40,52,53,54,55,56,57 Weak care infrastructure caused crowding and lack of privacy,41,58,59,60 increasing the wait times for care.61 Care delivery barriers included small scale of care,42 difficulty scaling services up,43 limited curative care,62,63 lack of referral systems for care,64 and poor integration across care components.65,66,67 The stigma of seeking care, especially for mental illness and obesity, was a cultural barrier.39,43,44,68 Patient literacy also sometimes hampered care,53,69 as did skepticism of treatment plans56,60,70,71 and gender-related barriers.72
Conversely, delivery facilitators involved creative solutions to logistical barriers and care sensitive to community needs. These strategies included home-based or home-adjacent care,42,43,45,73 integrated care across conditions,72,74,75,76 use of consistent care protocols,77,78 and programs to track and refer patients, including telemedicine.67,79 Nimgaonkar et al70 described a mental health intervention within a village health worker initiative in India and found that integrating these 2 programs facilitated reaching patients and decreased stigma. Culturally applicable health education was also helpful,40,43,45,80 as was community engagement and embeddedness.46,81 Abas et al,82 offering problem-solving therapy for depression in Zimbabwe, found that employing female health workers of the same socioeconomic status as their patients aided care delivery.46
Health Workforce
Workforce barriers comprised gaps between NPHWs’ capacity to perform key tasks and their supervisors’ expectations and support for them to do so. Workers’ skills and training were often insufficient.38,40,46,58,69,83,84,85 Furthermore, supervisors deployed NPHWs ineffectively to use these skills because of unclear job roles,60,86,87 excessive workload,38,60 and weak or adversarial relationships with other workers.10,41,62 Third, weak oversight65,72,73,74,86,87 hampered workers’ ability to meet expectations. Staff turnover also hampered care.8,10,88
Workforce facilitators addressed the aforementioned gaps but also aided in the judicious selection of workers. Nonphysician health workers who were recruited from the community served, or who were aware of its languages and customs, were an asset.39,42,43,46,47,70,82 Also helpful was rigorous, locally relevant training, including care algorithms10,40,44,47,72,76,77,89 and close collaboration with other health workers.10,39,41,45,47,70,77,80,89 Gaziano et al12 evaluated CHWs’ ability to screen for cardiovascular disease risk in Guatemala, Mexico, and Bangladesh and found that careful staff selection, training in local languages, and the use of simple care records facilitated success. Programs for epilepsy care in Kenya77 and postpartum depression in Pakistan89 also praised detailed care protocols and close supervision, respectively.
Governance
Governance barriers pertained to the insufficient authority of NPHWs to treat NCDs resulting from the lack of political will to authorize them and the consequent inability to assume key roles. In addition to weak oversight by supervisors, NPHWs reported poor communication with clinical directors,46 policy makers,90 and other overseers.84 In the absence of implementation science data,8,72 NPHWs faced mistrust regarding new roles, limiting their scope of care.40 These problems were compounded by ambiguity regarding NPHWs’ job roles38,40 and limitations on what care nonphysicians could provide,63 especially regarding prescribing medications.10,41,45 Weak care monitoring64,91 and backup support45 also arose, as did structural political factors, such as deliberate corruption of purpose,62 lack of governmental coordination,90 or active deprioritization by the ministry of health,92 hindering the distribution of personnel and resources.62
However, initiatives providing NPHWs a clear mandate and scope of work integrated within existing health care infrastructure93 aided care delivery,43,46 especially when policy makers and community officials actively assisted the NPHWs’ work and that of their supervisors62,76,86,90,94 and made express commitments to equitable care access.46 An evaluation of CHWs’ effectiveness in treating hypertension and diabetes in Iran94 noted that their impact was substantially greater for diabetes than hypertension because of Iran’s codification of their role in diabetes care.
Information Systems
Information system barriers comprised 2 categories: difficulty tracking patients and storing their data for longitudinal care. Nonphysician health workers struggled to record clinical encounters40,71,73,74; when present, information storage was inefficient.8,40,70 Contacting patients by telephone was also sometimes difficult.58 However, strategies to overcome these barriers were diverse and creative. A hypertension and diabetes program in Cameroon sent reminder letters to patients95; other programs used electronic or telephone systems for patient tracking,46,90 program eligibility and other screening,96,97 and surveillance and intervention planning.8,77,78 Some programs used telemedicine to provide NPHW oversight98 or even remote clinical encounters.79,92
Medication Access
Inconsistent access to medication hampered NPHW care, whereas reliable access promoted it. Many studies8,10,16,46,62,70,71,76,99 noted disruptions in medication or equipment as a challenge. Even when present, medications were sometimes expensive,55 and NPHWs were not always trained on how to use them.100 Interventions that leveraged consistent, inexpensive medication access were invaluable,8,10,46,77,78 but uncommon. Joshi et al,78 in discussing strategies to strengthen nonphysician cardiovascular disease care in rural China, noted that cost-effective drug distribution plans were helpful, as was the use of a single-tablet, multidrug polypill. A nurse-led hypertension treatment program in Cameroon101 also benefited from locally available medication.
Financing
Finance barriers fell into 2 categories: supply-side issues, such as lack of program funding41,46,64 and consequent poor pay for NPHWs,44,88 and mismanagement of resources, including poor performance incentives,74 lack of long-term planning,91 and overuse of out-of-pocket models for reimbursement (instead of insurance subsidies). The latter issue decreased patients’ demand for care102 and encouraged curative care in lieu of preventive medicine.62 Financial facilitators of care, conversely, included not only adequate program and salary funds8,62 but also social protection schemes to encourage patients to access care.97 One study,91 evaluating the integration of mental health care into CHW-led primary care in Kenya, noted that donor awareness of local needs optimized allocation of resources.
Discussion
We undertook a systematic review of health system factors that support or impair NPHW-led interventions to control NCDs in LMICs. Issues involving service delivery, the health workforce, and program governance encompassed the most diverse themes, ranging from logistical matters (eg, the distribution of workers), to structural issues of oversight, to cultural ones (eg, stigma). However, in all 6 domains, most themes pertained to either sufficient quantity of resources (eg, size of clinics or procurement of medications) or their effective stewardship (eg, authorizing NPHWs to use these medicines). Actionable lessons emerged across each block, as outlined here:
Service delivery: Provide protocol-based NPHW care that is community based and culturally sensitive to the community served, with physical infrastructure to allow access and referral based on robust physician backup systems.
Workforce: Select qualified NPHWs responsive to and embedded within communities, and provide rigorous training to workers and support from supervisors.
Governance: Provide detailed, feasible work expectations, with explicit support from clinical leadership and policy makers. Grant authority for NPHWs to perform appropriate clinical duties, including prescribing medication.
Information systems: Furnish electronic systems to allow NPHWs to remotely contact patients, follow their clinical data, and assess their eligibility for health interventions.
Medications: Provide a consistent supply chain of essential drugs, an efficient system for their distribution to patients, and training on appropriate use.
Financing: Provide adequate funds for essential program supplies, pay NPHWs fairly and consistently, and minimize patient out-of-pocket costs.
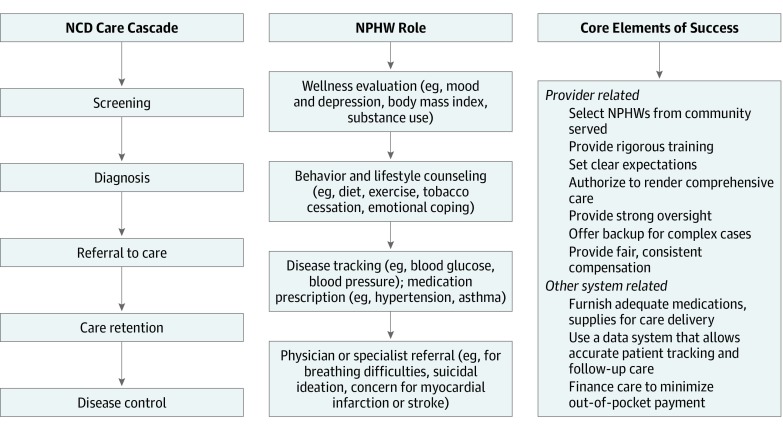
These findings also inform other frameworks specific to the performance of nonphysicians. The US-based CHW Core Consensus Project,103 for example, uses a framework asking how CHWs’ roles have evolved, what roles they currently play, and what skills they need to fill these roles. We found a substantial increase in NPHW-led NCD care models in recent years in all aspects of the NCD care cascade (Figure 2); more broadly, we found that NPHWs should be selected from within the communities served, rigorously trained, and given authority and material support to do their work. Similarly, Palazuelos et al104 designed a 5-point framework to appraise the resources CHWs need in LMIC settings: supervision, partnership, incentives, choice (recruitment), and education. These concepts, too, parallel the need for NPHW oversight, role definition, remuneration, selection, and training, respectively, as described already.
Figure 2. Nonphysician Health Workers (NPHWs) in the Noncommunicable Disease (NCD) Care Cascade.
Chart shows steps and NPHW role in the NCD cascade.
Literature Gaps
Few studies devised or evaluated process measures that could reveal whether and why their interventions operated consistently. For example, tracking how health care workers order key medications, when the medications arrive at clinics, and how often patients actually receive them could address the problem of medications being out of stock. Cost-effectiveness data were also rare,15,58,63,102,104 despite their implications for health policy. Furthermore, studies’ use of novel technologies and governance models raised unanswered questions, such as how best to use mobile telephones for decision support or how to implement performance-based compensation. In addition, although adequate compensation and supervision were crucial to NPHWs’ day-to-day performance, strategies for workers’ retention and promotion did not arise.
Health System Framework Challenges
The WHO’s building block framework did not accommodate all care barriers and facilitators described105,106 because some factors operate outside the health system. For example, some patient access barriers, such as community suspicion of government and inclement weather and roads, derive from factors not directly tied to health but still speak to themes (ie, social dynamics, climate, and built environment) that are instrumental to NPHW-led care. These political and cultural factors also influence the health system proper—for example, through the power dynamics that dictate how policy makers implement a health intervention, or the social values with which communities receive it (ie, the “software” through which the system’s building-block “hardware” renders care).107 This descriptive gap underscores the need for health care frameworks to acknowledge extrasystem barriers and facilitators; integrate health system factors with social, economic, and environmental factors; and use a multidisciplinary approach to NPHW system integration.
Also, some barriers and facilitators fit into multiple blocks.25,26 These included NPHW remuneration (workforce vs financing), NPHW team integration (workforce vs governance), and training on medication use (workforce vs medication). Although we categorized these elements by consensus, as described in the Methods section, the ambiguity highlights the interrelatedness of the building blocks. However, the relevance of the exact categorization is debatable, insofar as the blocks are interconnected,106 with cross-block innovations required to enable effective NPHW care.108
Policy and Program Implications
Our review suggests both practices and policy ideas to optimize NPHW-led NCD care, which some groups have begun to use. Partners in Health’s Mentorship and Enhanced Supervision for Health Care and Quality Improvement initiative,109,110 for example, stipulates that NPHW mentors continuously observe mentees every 4 to 6 weeks using a checklist to ensure quality of care. The Rural Andhra Pradesh Cardiovascular Prevention Study,111 a randomized trial of nonphysician hypertension screening and referral in India, benefited from a simple patient evaluation algorithm. The Nigerian Anti-Hypertensive Trial,112 a randomized trial of nurse-led hypertension treatment, benefited from nurses’ permission to dispense medications. Unfortunately, despite evidence that such interventions are effective12 and culturally acceptable,82 improve outcomes,48 and control costs,70,113,114 few have been scaled into national-level health systems.102
These findings are also applicable to high-income countries such as the United States, where physician assistants, nurses, and pharmacists provide a growing fraction of care.115In addition, nonphysicians are providing care outreach in novel settings, such as high blood pressure counseling and treatment in barber shops116 and churches.117 The Robert Wood Johnson foundation recently convened a task force identifying novel examples of global nonphysician care that can be applied in underserved US communities118; similarly, an intervention in Indiana is leveraging interventions validated in LMICs to reduce infant mortality.119
Limitations
Our review approach had notable limitations. We did not search databases beyond PubMed to identify systematic reviews, nor did we review articles not cited within the systematic reviews we identified, introducing bias both in our selection of studies and inherent within them (Table 3). Furthermore, although 2 reviewers examined all articles, they split the initial review of these articles, with each half reviewed post hoc by the other. Given the ambiguity and overlap of the WHO’s health system building block classification, including many barriers and facilitators not covered within the 6 blocks, it is possible that we missed or incorrectly categorized pertinent findings, potentially altering the results. Although we detailed the care site and disease treated within each study, we did not quantify such trends within these heterogeneous data. Nonetheless, strengths of this work include its detailed, reproducible systematic review protocol, its review of all classifications with a third coauthor, and its codevelopment of approach with a research librarian.
Conclusions
Because NCDs are now the leading cause of premature death and disability in low-income regions where physicians remain scarce, we sought to understand how NPHW-led programs for the control of these diseases are aided or impaired by the health systems they inhabit. This study found a small but growing set of studies describing these health system barriers and facilitators, usually incidentally rather than by the studies’ design, but with frequent and consistent messages regarding each of the WHO’s health system building blocks.
Beyond the training, retention, supervision, and deployment of these workers, furnishing strong support systems (supply chains for medications and equipment) and other infrastructure (telephone patient tracking or electronic patient records), as well as adequate program funding, also may facilitate success. In addition, further implementation research—in which these elements are expressly furnished, delivered, and evaluated for delivery and its care impact—will better illuminate how these elements are associated with care delivery. With these data, the effective scale-up of NPHW programs for the leading cause of morbidity and mortality in LMICs may be feasible.
eAppendix. PubMed Search Terms for Study
eTable. Details of Referenced Studies Citing Barriers and Facilitators to Nonphysician Care
eReferences.
References
- 1.Institute for Health Metrics and Evaluation Global Burden of Disease (GBD) compare tool. https://vizhub.healthdata.org/gbd-compare/. Accessed December 19, 2018.
- 2.Di Cesare M, Khang YH, Asaria P, et al. ; Lancet NCD Action Group . Inequalities in non-communicable diseases and effective responses. Lancet. 2013;381(9866):-. doi: 10.1016/S0140-6736(12)61851-0 [DOI] [PubMed] [Google Scholar]
- 3.Sommer I, Griebler U, Mahlknecht P, et al. . Socioeconomic inequalities in non-communicable diseases and their risk factors: an overview of systematic reviews. BMC Public Health. 2015;15(1):914. doi: 10.1186/s12889-015-2227-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Yoo SGK, Prabhakaran D, Huffman MD. Evaluating and improving cardiovascular health system management in low-and middle-income countries. Circ Cardiovasc Qual Outcomes. 2017;10(11):e004292. doi: 10.1161/CIRCOUTCOMES.117.004292 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.World Health Organization Global Health Observatory (GHO) data: density of physicians per 1,000 population. https://www.who.int/gho/health_workforce/physicians_density/en/. Accessed December 19, 2018.
- 6.Araujo E, Maeda A How to recruit and retain health workers in rural and remote areas in developing countries: a guidance note. https://openknowledge.worldbank.org/handle/10986/16104. Published 2013. Accessed June 10, 2019.
- 7.Callaghan M, Ford N, Schneider H. A systematic review of task-shifting for HIV treatment and care in Africa. Hum Resour Health. 2010;8(1):8. doi: 10.1186/1478-4491-8-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lewin S, Munabi-Babigumira S, Glenton C, et al. . Lay health workers in primary and community health care for maternal and child health and the management of infectious diseases. Cochrane Database Syst Rev. 2010;(3):CD004015. doi: 10.1002/14651858.CD004015.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Schneider H, Okello D, Lehmann U. The global pendulum swing towards community health workers in low- and middle-income countries: a scoping review of trends, geographical distribution and programmatic orientations, 2005 to 2014. Hum Resour Health. 2016;14(1):65. doi: 10.1186/s12960-016-0163-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Joshi R, Alim M, Kengne AP, et al. . Task shifting for non-communicable disease management in low and middle income countries: a systematic review. PLoS One. 2014;9(8):e103754. doi: 10.1371/journal.pone.0103754 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Abegunde DO, Shengelia B, Luyten A, et al. . Can non-physician health-care workers assess and manage cardiovascular risk in primary care? Bull World Health Organ. 2007;85(6):432-440. doi: 10.2471/BLT.06.032177 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gaziano TA, Abrahams-Gessel S, Denman CA, et al. . An assessment of community health workers’ ability to screen for cardiovascular disease risk with a simple, non-invasive risk assessment instrument in Bangladesh, Guatemala, Mexico, and South Africa: an observational study. Lancet Glob Health. 2015;3(9):e556-e563. doi: 10.1016/S2214-109X(15)00143-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Khan M, Lamelas P, Musa H, et al. . Development, testing, and implementation of a training curriculum for nonphysician health workers to reduce cardiovascular disease. Glob Heart. 2018;13(2):93-100. doi: 10.1016/j.gheart.2017.11.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Patel V, Weiss HA, Chowdhary N, et al. . Lay health worker led intervention for depressive and anxiety disorders in India: impact on clinical and disability outcomes over 12 months. Br J Psychiatry. 2011;199(6):459-466. doi: 10.1192/bjp.bp.111.092155 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Weobong B, Weiss HA, McDaid D, et al. . Sustained effectiveness and cost-effectiveness of the Healthy Activity Programme, a brief psychological treatment for depression delivered by lay counsellors in primary care: 12-month follow-up of a randomised controlled trial. PLoS Med. 2017;14(9):e1002385. doi: 10.1371/journal.pmed.1002385 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Labhardt ND, Balo JR, Ndam M, Grimm JJ, Manga E. Task shifting to non-physician clinicians for integrated management of hypertension and diabetes in rural Cameroon: a programme assessment at two years. BMC Health Serv Res. 2010;10(1):339. doi: 10.1186/1472-6963-10-339 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gajalakshmi CK, Krishnamurthi S, Ananth R, Shanta V. Cervical cancer screening in Tamilnadu, India: a feasibility study of training the village health nurse. Cancer Causes Control. 1996;7(5):520-524. doi: 10.1007/BF00051884 [DOI] [PubMed] [Google Scholar]
- 18.Warnakulasuriya KA, Ekanayake AN, Sivayoham S, et al. . Utilization of primary health care workers for early detection of oral cancer and precancer cases in Sri Lanka. Bull World Health Organ. 1984;62(2):243-250. [PMC free article] [PubMed] [Google Scholar]
- 19.Kengne AP, Fezeu L, Awah PK, Sobngwi E, Mbanya JC. Task shifting in the management of epilepsy in resource-poor settings. Epilepsia. 2010;51(5):931-932. doi: 10.1111/j.1528-1167.2009.02414.x [DOI] [PubMed] [Google Scholar]
- 20.Kengne AP, Sobngwi E, Fezeu LL, Awak PK, Dongmo S, Mbanya JC. Nurse-led care for asthma at primary level in rural sub-Saharan Africa: the experience of Bafut in Cameroon. J Asthma. 2008;45(6):437-443. doi: 10.1080/02770900802032933 [DOI] [PubMed] [Google Scholar]
- 21.World Health Organization HEARTS: technical package for cardiovascular disease management in primary health care. https://apps.who.int/iris/bitstream/handle/10665/252661/9789241511377-eng.pdf?sequence=1. Published 2016. Accessed September 19, 2018.
- 22.World Health Organization mhGAP training manuals for the mhGAP intervention guide for mental, neurological and substance use disorders in non-specialized health settings: version 2.0 (for field testing). https://apps.who.int/iris/bitstream/handle/10665/259161/WHO-MSD-MER-17.6-eng.pdf?sequence=1&isAllowed=y. Published 2017. Accessed December 19, 2018.
- 23.United Nations 2011 High level meeting on prevention and control of non-communicable diseases. https://www.un.org/en/ga/ncdmeeting2011/. Published 2011. Accessed December 19, 2018.
- 24.World Health Organization Time to deliver: report of the WHO Independent High Level Commission on Noncommunicable Diseases. https://www.who.int/ncds/management/time-to-deliver/en/. Published June 1, 2018. Accessed December 19, 2018.
- 25.World Health Organization The World Health Report 2003: shaping the future. https://www.who.int/whr/2003/en/whr03_en.pdf. Published 2003. Accessed December 19, 2018.
- 26.World Health Organization Everybody’s business: strengthening health systems to improve health outcomes: WHO’s framework for action. https://www.who.int/healthsystems/strategy/everybodys_business.pdf. Published 2007. Accessed December 19, 2018.
- 27.Stroup DF, Berlin JA, Morton SC, et al. ; Meta-analysis of Observational Studies in Epidemiology (MOOSE) Group . Meta-analysis of observational studies in epidemiology: a proposal for reporting. JAMA. 2000;283(15):2008-2012. doi: 10.1001/jama.283.15.2008 [DOI] [PubMed] [Google Scholar]
- 28.Moher D, Liberati A, Tetzlaff J, Altman DG; PRISMA Group . Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med. 2009;151(4):264-269. doi: 10.7326/0003-4819-151-4-200908180-00135 [DOI] [PubMed] [Google Scholar]
- 29.Bukhman G, Kidder A; Partners in Health The PIH guide to chronic care integration for endemic non-communicable diseases. https://www.pih.org/practitioner-resource/the-pih-guide-to-chronic-care-integration-for-endemic-non-communicable-dise. Published 2011. Accessed December 19, 2018.
- 30.The World Bank Open data: country income. https://data.worldbank.org/income-level/lower-middle-income. Accessed December 19, 2018.
- 31.Roda G, Narula N, Pinotti R, et al. . Systematic review with meta-analysis: proximal disease extension in limited ulcerative colitis. Aliment Pharmacol Ther. 2017;45(12):1481-1492. doi: 10.1111/apt.14063 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Shea BJ, Reeves BC, Wells G, et al. . AMSTAR 2: a critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ. 2017;358:j4008. doi: 10.1136/bmj.j4008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Green BN, Johnson CD, Adams A. Writing narrative literature reviews for peer-reviewed journals: secrets of the trade. J Chiropr Med. 2006;5(3):101-117. doi: 10.1016/S0899-3467(07)60142-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Iwelunmor J, Plange-Rhule J, Airhihenbuwa CO, Ezepue C, Ogedegbe O. A narrative synthesis of the health systems factors influencing optimal hypertension control in sub-Saharan Africa. PLoS One. 2015;10(7):e0130193. doi: 10.1371/journal.pone.0130193 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Popay J, Roberts H, Sowden A, et al. Guidance on the conduct of narrative synthesis in systematic reviews: a product from the ESRC methods Programme. http://citeseerx.ist.psu.edu/viewdoc/download?doi=10.1.1.178.3100&rep=rep1&type=pdf. Published April 1, 2006. Accessed December 19, 2018.
- 36.Corbin JM, Strauss A. Grounded theory research: procedures, canons, and evaluative criteria. Qual Sociol. 1990;13(1):3-21. doi: 10.1007/BF00988593 [DOI] [Google Scholar]
- 37.O’Brien BC, Harris IB, Beckman TJ, Reed DA, Cook DA. Standards for reporting qualitative research: a synthesis of recommendations. Acad Med. 2014;89(9):1245-1251. doi: 10.1097/ACM.0000000000000388 [DOI] [PubMed] [Google Scholar]
- 38.Gatuguta A, Katusiime B, Seeley J, Colombini M, Mwanzo I, Devries K. Should community health workers offer support healthcare services to survivors of sexual violence? a systematic review. BMC Int Health Hum Rights. 2017;17(1):28. doi: 10.1186/s12914-017-0137-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Barnett ML, Gonzalez A, Miranda J, Chavira DA, Lau AS. Mobilizing community health workers to address mental health disparities for underserved populations: a systematic review. Adm Policy Ment Health. 2018;45(2):195-211. doi: 10.1007/s10488-017-0815-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Khetan AK, Purushothaman R, Chami T, et al. . The effectiveness of community health workers in CVD prevention in LMIC. Glob Heart. 2017;12(3):233-243. doi: 10.1016/j.gheart.2016.07.001 [DOI] [PubMed] [Google Scholar]
- 41.Padmanathan P, De Silva MJ. The acceptability and feasibility of task-sharing for mental healthcare in low and middle income countries: a systematic review. Soc Sci Med. 2013;97:82-86. doi: 10.1016/j.socscimed.2013.08.004 [DOI] [PubMed] [Google Scholar]
- 42.Mutamba BB, van Ginneken N, Smith Paintain L, Wandiembe S, Schellenberg D. Roles and effectiveness of lay community health workers in the prevention of mental, neurological and substance use disorders in low and middle income countries: a systematic review. BMC Health Serv Res. 2013;13(1):412. doi: 10.1186/1472-6963-13-412 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Chowdhary N, Sikander S, Atif N, et al. . The content and delivery of psychological interventions for perinatal depression by non-specialist health workers in low and middle income countries: a systematic review. Best Pract Res Clin Obstet Gynecol. 2014;28(1):113-133. doi: 10.1016/j.bpobgyn.2013.08.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Abdel-All M, Putica B, Praveen D, Abimbola S, Joshi R. Effectiveness of community health worker training programmes for cardiovascular disease management in low-income and middle-income countries: a systematic review. BMJ Open. 2017;7(11):e015529. doi: 10.1136/bmjopen-2016-015529 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Ogedegbe G, Gyamfi J, Plange-Rhule J, et al. . Task shifting interventions for cardiovascular risk reduction in low-income and middle-income countries: a systematic review of randomised controlled trials. BMJ Open. 2014;4(10):e005983. doi: 10.1136/bmjopen-2014-005983 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Javadi D, Feldhaus I, Mancuso A, Ghaffar A. Applying systems thinking to task shifting for mental health using lay providers: a review of the evidence. Glob Ment Health (Camb). 2017;4:e14. doi: 10.1017/gmh.2017.15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Hill J, Peer N, Oldenburg B, Kengne AP. Roles, responsibilities and characteristics of lay community health workers involved in diabetes prevention programmes: a systematic review. PLoS One. 2017;12(12):e0189069. doi: 10.1371/journal.pone.0189069 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Seidman G, Atun R. Does task shifting yield cost savings and improve efficiency for health systems? a systematic review of evidence from low-income and middle-income countries. Hum Resour Health. 2017;15(1):29. doi: 10.1186/s12960-017-0200-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Jeet G, Thakur JS, Prinja S, Singh M. Community health workers for non-communicable diseases prevention and control in developing countries: evidence and implications. PLoS One. 2017;12(7):e0180640. doi: 10.1371/journal.pone.0180640 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Alaofè H, Asaolu I, Ehiri J, et al. . Community health workers in diabetes prevention and management in developing countries. Ann Glob Health. 2017;83(3-4):661-675. doi: 10.1016/j.aogh.2017.10.009 [DOI] [PubMed] [Google Scholar]
- 51.Ahluwalia SC, Damberg CL, Silverman M, Motala A, Shekelle PG. What defines a high-performing health care delivery system: a systematic review. Jt Comm J Qual Patient Saf. 2017;43(9):450-459. doi: 10.1016/j.jcjq.2017.03.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Pastakia SD, Ali SM, Kamano JH, et al. . Screening for diabetes and hypertension in a rural low income setting in western Kenya utilizing home-based and community-based strategies. Global Health. 2013;9(1):21. doi: 10.1186/1744-8603-9-21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Balaji M, Chatterjee S, Koschorke M, et al. . The development of a lay health worker delivered collaborative community based intervention for people with schizophrenia in India. BMC Health Serv Res. 2012;12(1):42. doi: 10.1186/1472-6963-12-42 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Chatterjee S, Naik S, John S, et al. . Effectiveness of a community-based intervention for people with schizophrenia and their caregivers in India (COPSI): a randomised controlled trial. Lancet. 2014;383(9926):1385-1394. doi: 10.1016/S0140-6736(13)62629-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Pereira B, Andrew G, Pednekar S, Kirkwood BR, Patel V. The integration of the treatment for common mental disorders in primary care: experiences of health care providers in the MANAS trial in Goa, India. Int J Ment Health Syst. 2011;5(1):26. doi: 10.1186/1752-4458-5-26 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Nadkarni A, Velleman R, Dabholkar H, et al. . The systematic development and pilot randomized evaluation of counselling for alcohol problems, a lay counselor-delivered psychological treatment for harmful drinking in primary care in India: the PREMIUM study. Alcohol Clin Exp Res. 2015;39(3):522-531. doi: 10.1111/acer.12653 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Kohli A, Makambo MT, Ramazani P, et al. . A Congolese community-based health program for survivors of sexual violence. Confl Health. 2012;6(1):6. doi: 10.1186/1752-1505-6-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Mash R, Kroukamp R, Gaziano T, Levitt N. Cost-effectiveness of a diabetes group education program delivered by health promoters with a guiding style in underserved communities in Cape Town, South Africa. Patient Educ Couns. 2015;98(5):622-626. doi: 10.1016/j.pec.2015.01.005 [DOI] [PubMed] [Google Scholar]
- 59.Murray LK, Familiar I, Skavenski S, et al. . An evaluation of trauma focused cognitive behavioral therapy for children in Zambia. Child Abuse Negl. 2013;37(12):1175-1185. doi: 10.1016/j.chiabu.2013.04.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Mendenhall E, De Silva MJ, Hanlon C, et al. . Acceptability and feasibility of using non-specialist health workers to deliver mental health care: stakeholder perceptions from the PRIME district sites in Ethiopia, India, Nepal, South Africa, and Uganda. Soc Sci Med. 2014;118:33-42. doi: 10.1016/j.socscimed.2014.07.057 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Naved RT, Rimi NA, Jahan S, Lindmark G. Paramedic-conducted mental health counselling for abused women in rural Bangladesh: an evaluation from the perspective of participants. J Health Popul Nutr. 2009;27(4):477-491. doi: 10.3329/jhpn.v27i4.3391 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Haines A, Sanders D, Lehmann U, et al. . Achieving child survival goals: potential contribution of community health workers. Lancet. 2007;369(9579):2121-2131. doi: 10.1016/S0140-6736(07)60325-0 [DOI] [PubMed] [Google Scholar]
- 63.Mdege ND, Chindove S, Ali S. The effectiveness and cost implications of task-shifting in the delivery of antiretroviral therapy to HIV-infected patients: a systematic review. Health Policy Plan. 2013;28(3):223-236. doi: 10.1093/heapol/czs058 [DOI] [PubMed] [Google Scholar]
- 64.Abanilla PK, Huang KY, Shinners D, et al. . Cardiovascular disease prevention in Ghana: feasibility of a faith-based organizational approach. Bull World Health Organ. 2011;89(9):648-656. doi: 10.2471/BLT.11.086777 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Jordans MJ, Keen AS, Pradhan H, et al. . Psychosocial counselling in Nepal: perspectives of counsellors and beneficiaries. Int J Adv Couns. 2007;29(1):57-68. doi: 10.1007/s10447-006-9028-z [DOI] [Google Scholar]
- 66.Nishtar S, Badar A, Kamal MU, et al. . The Heartfile Lodhran CVD prevention project: end of project evaluation. Promot Educ. 2007;14(1):17-27. doi: 10.1177/175797590701400103 [DOI] [PubMed] [Google Scholar]
- 67.Lorenzo T, van Pletzen E, Booyens M. Determining the competences of community based workers for disability-inclusive development in rural areas of South Africa, Botswana and Malawi. Rural Remote Health. 2015;15(2):2919. [PubMed] [Google Scholar]
- 68.Ali BS, Rahbar MH, Naeem S, Gul A, Mubeen S, Iqbal A. The effectiveness of counseling on anxiety and depression by minimally trained counselors: a randomized controlled trial. Am J Psychother. 2003;57(3):324-336. doi: 10.1176/appi.psychotherapy.2003.57.3.324 [DOI] [PubMed] [Google Scholar]
- 69.Micikas M, Foster J, Weis A, et al. . A community health worker intervention for diabetes self-management among the Tz’utujil Maya of Guatemala. Health Promot Pract. 2015;16(4):601-608. doi: 10.1177/1524839914557033 [DOI] [PubMed] [Google Scholar]
- 70.Nimgaonkar AU, Menon SD. A task shifting mental health program for an impoverished rural Indian community. Asian J Psychiatr. 2015;16:41-47. doi: 10.1016/j.ajp.2015.05.044 [DOI] [PubMed] [Google Scholar]
- 71.Ndou T, van Zyl G, Hlahane S, Goudge J. A rapid assessment of a community health worker pilot programme to improve the management of hypertension and diabetes in Emfuleni sub-district of Gauteng Province, South Africa. Glob Health Action. 2013;6(1):19228. doi: 10.3402/gha.v6i0.19228 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Abrahams-Gessel S, Denman CA, Montano CM, et al. . The training and fieldwork experiences of community health workers conducting population-based, noninvasive screening for CVD in LMIC. Glob Heart. 2015;10(1):45-54. doi: 10.1016/j.gheart.2014.12.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Chibanda D, Mesu P, Kajawu L, Cowan F, Araya R, Abas MA. Problem-solving therapy for depression and common mental disorders in Zimbabwe: piloting a task-shifting primary mental health care intervention in a population with a high prevalence of people living with HIV. BMC Public Health. 2011;11(1):828. doi: 10.1186/1471-2458-11-828 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Mendis S, Johnston SC, Fan W, Oladapo O, Cameron A, Faramawi MF. Cardiovascular risk management and its impact on hypertension control in primary care in low-resource settings: a cluster-randomized trial. Bull World Health Organ. 2010;88(6):412-419. doi: 10.2471/BLT.08.062364 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Zhong X, Wang Z, Fisher EB, Tanasugarn C. Peer support for diabetes management in primary care and community settings in Anhui Province, China. Ann Fam Med. 2015;13(1)(suppl):S50-S58. doi: 10.1370/afm.1799 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Petersen I, Ssebunnya J, Bhana A, Baillie K; MhaPP Research Programme Consortium . Lessons from case studies of integrating mental health into primary health care in South Africa and Uganda. Int J Ment Health Syst. 2011;5(1):8. doi: 10.1186/1752-4458-5-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Feksi AT, Kaamugisha J, Sander JW, Gatiti S, Shorvon SD; ICBERG (International Community-Based Epilepsy Research Group) . Comprehensive primary health care antiepileptic drug treatment programme in rural and semi-urban Kenya. Lancet. 1991;337(8738):406-409. doi: 10.1016/0140-6736(91)91176-U [DOI] [PubMed] [Google Scholar]
- 78.Joshi R, Jan S, Wu Y, MacMahon S. Global inequalities in access to cardiovascular health care: our greatest challenge. J Am Coll Cardiol. 2008;52(23):1817-1825. doi: 10.1016/j.jacc.2008.08.049 [DOI] [PubMed] [Google Scholar]
- 79.Magidson JF, Lejuez CW, Kamal T, et al. . Adaptation of community health worker-delivered behavioral activation for torture survivors in Kurdistan, Iraq. Glob Ment Health (Camb). 2015;2(Jan):e24. doi: 10.1017/gmh.2015.22 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Bolton P, Bass JK, Zangana GA, et al. . A randomized controlled trial of mental health interventions for survivors of systematic violence in Kurdistan, Northern Iraq. BMC Psychiatry. 2014;14(1):360. doi: 10.1186/s12888-014-0360-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Balagopal P, Kamalamma N, Patel TG, Misra R. A community-based participatory diabetes prevention and management intervention in rural India using community health workers. Diabetes Educ. 2012;38(6):822-834. doi: 10.1177/0145721712459890 [DOI] [PubMed] [Google Scholar]
- 82.Abas M, Bowers T, Manda E, et al. . “Opening up the mind”: problem-solving therapy delivered by female lay health workers to improve access to evidence-based care for depression and other common mental disorders through the Friendship Bench Project in Zimbabwe. Int J Ment Health Syst. 2016;10(1):39. doi: 10.1186/s13033-016-0071-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Pisani P, Parkin DM, Ngelangel C, et al. . Outcome of screening by clinical examination of the breast in a trial in the Philippines. Int J Cancer. 2006;118(1):149-154. doi: 10.1002/ijc.21343 [DOI] [PubMed] [Google Scholar]
- 84.Tsolekile LP, Puoane T, Schneider H, Levitt NS, Steyn K. The roles of community health workers in management of non-communicable diseases in an urban township. Afr J Prim Health Care Fam Med. 2014;6(1):E1-E8. doi: 10.4102/phcfm.v6i1.693 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Murray LK, Dorsey S, Haroz E, et al. . A common elements treatment approach for adult mental health problems in low-and middle-income countries. Cogn Behav Pract. 2014;21(2):111-123. doi: 10.1016/j.cbpra.2013.06.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Agyapong VI, Osei A, Farren CK, McAuliffe E. Factors influencing the career choice and retention of community mental health workers in Ghana. Hum Resour Health. 2015;13(1):56. doi: 10.1186/s12960-015-0050-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Agyapong VI, Osei A, Farren CK, Mcauliffe E. Task shifting of mental health care services in Ghana: ease of referral, perception and concerns of stakeholders about quality of care. Int J Qual Health Care. 2015;27(5):377-383. doi: 10.1093/intqhc/mzv058 [DOI] [PubMed] [Google Scholar]
- 88.Murray LK, Skavenski S, Kane JC, et al. . Effectiveness of trauma-focused cognitive behavioral therapy among trauma-affected children in Lusaka, Zambia: a randomized clinical trial. JAMA Pediatr. 2015;169(8):761-769. doi: 10.1001/jamapediatrics.2015.0580 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Rahman A, Malik A, Sikander S, Roberts C, Creed F. Cognitive behaviour therapy-based intervention by community health workers for mothers with depression and their infants in rural Pakistan: a cluster-randomised controlled trial. Lancet. 2008;372(9642):902-909. doi: 10.1016/S0140-6736(08)61400-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Agyapong VI, Farren C, McAuliffe E. Improving Ghana’s mental healthcare through task-shifting: psychiatrists and health policy directors perceptions about government’s commitment and the role of community mental health workers. Global Health. 2016;12(1):57. doi: 10.1186/s12992-016-0199-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Jenkins R, Kiima D, Okonji M, Njenga F, Kingora J, Lock S. Integration of mental health into primary care and community health working in Kenya: context, rationale, coverage and sustainability. Ment Health Fam Med. 2010;7(1):37-47. [PMC free article] [PubMed] [Google Scholar]
- 92.Pallas SW, Minhas D, Pérez-Escamilla R, Taylor L, Curry L, Bradley EH. Community health workers in low- and middle-income countries: what do we know about scaling up and sustainability? Am J Public Health. 2013;103(7):e74-e82. doi: 10.2105/AJPH.2012.301102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Kok MC, Kane SS, Tulloch O, et al. . How does context influence performance of community health workers in low- and middle-income countries? evidence from the literature. Health Res Policy Syst. 2015;13(1):13. doi: 10.1186/s12961-015-0001-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Farzadfar F, Murray CJ, Gakidou E, et al. . Effectiveness of diabetes and hypertension management by rural primary health-care workers (Behvarz workers) in Iran: a nationally representative observational study. Lancet. 2012;379(9810):47-54. doi: 10.1016/S0140-6736(11)61349-4 [DOI] [PubMed] [Google Scholar]
- 95.Labhardt ND, Balo JR, Ndam M, Manga E, Stoll B. Improved retention rates with low-cost interventions in hypertension and diabetes management in a rural African environment of nurse-led care: a cluster-randomised trial. Trop Med Int Health. 2011;16(10):1276-1284. doi: 10.1111/j.1365-3156.2011.02827.x [DOI] [PubMed] [Google Scholar]
- 96.Hung KJ, Tomlinson M, le Roux IM, Dewing S, Chopra M, Tsai AC. Community-based prenatal screening for postpartum depression in a South African township. Int J Gynaecol Obstet. 2014;126(1):74-77. doi: 10.1016/j.ijgo.2014.01.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Padilla E, Molina J, Kamis D, et al. . The efficacy of targeted health agents education to reduce the duration of untreated psychosis in a rural population. Schizophr Res. 2015;161(2-3):184-187. doi: 10.1016/j.schres.2014.10.039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Tomlinson M, Doherty T, Jackson D, et al. . An effectiveness study of an integrated, community-based package for maternal, newborn, child and HIV care in South Africa: study protocol for a randomized controlled trial. Trials. 2011;12(1):236. doi: 10.1186/1745-6215-12-236 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Adams JL, Almond ML, Ringo EJ, Shangali WH, Sikkema KJ. Feasibility of nurse-led antidepressant medication management of depression in an HIV clinic in Tanzania. Int J Psychiatry Med. 2012;43(2):105-117. doi: 10.2190/PM.43.2.a [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Wright J, Chiwandira C. Building capacity for community mental health care in rural Malawi: findings from a district-wide task-sharing intervention with village-based health workers. Int J Soc Psychiatry. 2016;62(6):589-596. doi: 10.1177/0020764016657112 [DOI] [PubMed] [Google Scholar]
- 101.Kengne AP, Fezeu L, Sobngwi E, et al. . Type 2 diabetes management in nurse-led primary healthcare settings in urban and rural Cameroon. Prim Care Diabetes. 2009;3(3):181-188. doi: 10.1016/j.pcd.2009.08.005 [DOI] [PubMed] [Google Scholar]
- 102.Jafar TH, Islam M, Bux R, et al. . Cost-effectiveness of community-based strategies for blood pressure control in a low-income developing country: findings from a cluster-randomized, factorial-controlled trial. Circulation. 2011;124(15):1615-1625. doi: 10.1161/CIRCULATIONAHA.111.039990 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Rosenthal EL, Rush CH, Allen CG Understanding scope and competencies: a contemporary look at the United States community health worker field—progress report of the community health worker (CHW) core consensus (C3) project. building national consensus on CHW core roles, skills, and qualities. http://chrllc.net/sitebuildercontent/sitebuilderfiles/c3_report_20160810.pdf. Published July 2016. Accessed June 5, 2019.
- 104.Palazuelos D, Ellis K, Im DD, et al. . 5-SPICE: the application of an original framework for community health worker program design, quality improvement and research agenda setting. Glob Health Action. 2013;6(1):19658. doi: 10.3402/gha.v6i0.19658 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Mounier-Jack S, Griffiths UK, Closser S, Burchett H, Marchal B. Measuring the health systems impact of disease control programmes: a critical reflection on the WHO building blocks framework. BMC Public Health. 2014;14(1):278. doi: 10.1186/1471-2458-14-278 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Huff-Rousselle M. Reflections on the frameworks we use to capture complex and dynamic health sector issues. Int J Health Plann Manage. 2013;28(1):95-101. doi: 10.1002/hpm.2161 [DOI] [PubMed] [Google Scholar]
- 107.Sheikh K, Gilson L, Agyepong IA, Hanson K, Ssengooba F, Bennett S. Building the field of health policy and systems research: framing the questions. PLoS Med. 2011;8(8):e1001073. doi: 10.1371/journal.pmed.1001073 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Frenk J. The global health system: strengthening national health systems as the next step for global progress. PLoS Med. 2010;7(1):e1000089. doi: 10.1371/journal.pmed.1000089 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Manzi A, Kirk C, Hirschhorn LR MESH-QI implementation guide: mentorship and enhanced supervision for healthcare and quality improvement. https://www.pih.org/sites/default/files/2017-12/MESH%20QI%20Final%20web%2012.2017.pdf. Published 2017. Accessed October 29, 2019.
- 110.Anatole M, Magge H, Redditt V, et al. . Nurse mentorship to improve the quality of health care delivery in rural Rwanda. Nurs Outlook. 2013;61(3):137-144. doi: 10.1016/j.outlook.2012.10.003 [DOI] [PubMed] [Google Scholar]
- 111.Joshi R, Chow CK, Raju PK, et al. . The Rural Andhra Pradesh Cardiovascular Prevention Study (RAPCAPS): a cluster randomized trial. J Am Coll Cardiol. 2012;59(13):1188-1196. doi: 10.1010/j.jacc.2011.10.901 [DOI] [PubMed] [Google Scholar]
- 112.Adeyemo A, Tayo BO, Luke A, Ogedegbe O, Durazo-Arvizu R, Cooper RS. The Nigerian antihypertensive adherence trial: a community-based randomized trial. J Hypertens. 2013;31(1):201-207. doi: 10.1097/HJH.0b013e32835b0842 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Johnson D, Saavedra P, Sun E, et al. . Community health workers and Medicaid managed care in New Mexico. J Community Health. 2012;37(3):563-571. doi: 10.1007/s10900-011-9484-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Beckham S, Kaahaaina D, Voloch KA, Washburn A. A community-based asthma management program: effects on resource utilization and quality of life. Hawaii Med J. 2004;63(4):121-126. [PubMed] [Google Scholar]
- 115.Cooper RA. Unraveling the physician supply dilemma. JAMA. 2013;310(18):1931-1932. doi: 10.1001/jama.2013.282170 [DOI] [PubMed] [Google Scholar]
- 116.Victor RG, Lynch K, Li N, et al. . A cluster-randomized trial of blood-pressure reduction in black barbershops. N Engl J Med. 2018;378(14):1291-1301. doi: 10.1056/NEJMoa1717250 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Schoenthaler AM, Lancaster KJ, Chaplin W, Butler M, Forsyth J, Ogedegbe G. Cluster Randomized Clinical Trial of FAITH (Faith-Based Approaches in the Treatment of Hypertension) in Blacks. Circ Cardiovasc Qual Outcomes. 2018;11(10):e004691. doi: 10.1161/CIRCOUTCOMES.118.004691 [DOI] [PubMed] [Google Scholar]
- 118.Arnhold Institute for Global Health Task force on global advantage. http://icahn.mssm.edu/research/arnhold/research-development/task-force-global-advantage. Accessed December 28, 2018.
- 119.WeCare Indiana Improving maternal and infant health to reduce infant mortality. https://www.regenstrief.org/projects/wecare-indiana/. Accessed December 28, 2018.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eAppendix. PubMed Search Terms for Study
eTable. Details of Referenced Studies Citing Barriers and Facilitators to Nonphysician Care
eReferences.