Key Points
Question
What is the association between electronic cigarette (e-cigarette) use and depression?
Findings
In this cross-sectional study of 892 394 participants in the Behavioral Risk Factor Surveillance System from 2016 to 2017, e-cigarette users had higher odds of reporting a history of clinical diagnosis of depression compared with participants who never used e-cigarettes. In addition, increased frequency of e-cigarette use was associated with incrementally higher odds of reporting depression.
Meaning
These findings highlight the need for longitudinal studies to examine the association between e-cigarette use and depression, which may be bidirectional.
This cross-sectional study examines the association between electronic cigarette (e-cigarette) use and depression in a nationally representative sample of the adult population in the United States.
Abstract
Importance
The prevalence of the use of electronic cigarettes (e-cigarettes) in the United States has grown rapidly since their introduction to the market more than a decade ago. While several studies have demonstrated an association between combustible cigarette smoking and depression, the association between e-cigarette use and depression has not been thoroughly studied.
Objective
To examine the association between e-cigarette use and depression in a nationally representative sample of the adult population in the United States.
Design, Setting, and Participants
Cross-sectional study of the Behavioral Risk Factor Surveillance System database, 2016 to 2017. The Behavioral Risk Factor Surveillance System is the largest national telephone-based survey of randomly sampled adults in the United States. A total of 892 394 participants with information on e-cigarette use and depression were included. Data analysis was conducted in May 2019.
Exposures
Electronic cigarette use status defined by self-report as never, former, or current use.
Main Outcomes and Measures
Self-reported history of a clinical diagnosis of depression.
Results
Of the 892 394 participants (414 326 [29.0%] aged ≥60 years; 502 448 [51.3%] women), there were 28 736 (4.4%) current e-cigarette users, of whom 13 071 (62.1%) were aged between 18 and 39 years. Compared with never e-cigarette users, current e-cigarette users were more likely to be single, male, younger than 40 years, and current combustible cigarette smokers (single, 120 797 [24.3%] vs 10 517 [48.4%]; men, 318 970 [46.6%] vs 14 962 [60.1%]; aged 18-39 years, 129 085 [32.2%] vs 13 071 [62.1%]; current combustible cigarette use, 217 895 [7.9%] vs 8823 [51.8%]). In multivariable adjusted models, former e-cigarette users had 1.60-fold (95% CI, 1.54-1.67) higher odds of reporting a history of clinical diagnosis of depression than never users, whereas current e-cigarette users had 2.10 (95% CI, 1.98-2.23) times higher odds. Additionally, higher odds of reporting depression were observed with increased frequency of use among current e-cigarette users compared with never users (daily use: odds ratio, 2.39; 95% CI, 2.19-2.61; occasional use: odds ratio, 1.96; 95% CI, 1.82-2.10). Similar results were seen in subgroup analyses by sex, race/ethnicity, smoking status, and student status.
Conclusions and Relevance
This study found a significant cross-sectional association between e-cigarette use and depression, which highlights the need for prospective studies analyzing the longitudinal risk of depression with e-cigarette use. If confirmed by other study designs, the potential mental health consequences may have regulatory implications for novel tobacco products.
Introduction
Electronic cigarettes (e-cigarettes) were introduced into the US market more than a decade ago as an alternative to combustible cigarettes.1,2,3 They are marketed as less harmful nicotine delivery devices; however, their contents are largely unregulated and vary widely, with nicotine concentrations ranging from 0 to 59 mg/mL.4,5 Many products also contain potentially toxic metals, such as arsenic and lead, as well as propylene glycol. When used, e-cigarettes may generate volatile organic compounds, including acetaldehyde and formaldehyde, especially at high temperatures.4,6
In 2016, 10.8 million adults (4.5%) in the United States reported current e-cigarette use, more than half of whom were younger than 35 years.1 Among current e-cigarette users, 3.6 million (33.5%) reported daily use, with 54.6% also reporting traditional cigarette smoking.1
Among individuals with mental health conditions (MHCs), who make up 36.4% of the US population,7 smoking rates are estimated to be 70% greater than in the general US population,8 with these individuals consuming approximately 56.4% of all cigarettes sold in the United States.7 Cigarette smokers with MHCs also tend to smoke more heavily and find it harder to quit smoking.7,9 The prevalence of depression in the population varies widely, from 6.7% to 16.6%,10,11 and a recent study found that prevalence of current e-cigarette use among those who reported having depression was 9.1%, compared with a prevalence of 4.5% in the general population.1
The popularity of e-cigarettes among the general population and their appeal to those who are susceptible to MHCs, including younger adults, raises a question regarding the association between e-cigarette use and mental health.3,12 To test our hypotheses that e-cigarette users might be more likely to have depression and that depressed individuals might be more likely to use e-cigarettes, we sought to examine the cross-sectional association between the use of e-cigarettes and depression in a large representative sample of adults in the United States.
Methods
Study Population
The Behavioral Risk Factor Surveillance System (BRFSS) is a nationwide, telephone-based survey of randomly sampled US residents older than 18 years, established by the US Centers for Disease Control and Prevention to collect information on health-related risk behaviors, chronic medical conditions, and the use of preventive health services.13 The survey includes participants in all 50 states as well as Washington, DC, and 3 US territories, making it the largest dynamic telephone-based health survey in the world.13
The BRFSS is a publicly available data set containing deidentified data. Thus, based on the code of federal regulations revised common rule,14 our analysis of the data set was exempt from institutional review board review. Each section of this report was prepared using the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guideline.
Inclusion and Exclusion Criteria
To examine the association between e-cigarette use and depression, we pooled data from the 2016 and 2017 BRFSS surveys, which included 936 319 participants. Of the participants in the data set, we excluded participants with missing data on e-cigarette use (n = 39 729 [4.2%]), self-reported history of clinical diagnosis of depression (n = 3818 [0.4%]), and both (n = 378 [0.1%]), leaving a total sample size of 892 394 (95.3%).
Use of e-Cigarettes
Participants were categorized as ever or never e-cigarette users based on their response to the question, “Have you ever used an e-cigarette or other electronic vaping product, even just 1 time, in your entire life?” Those who answered yes were then further classified into occasional or daily users based on their response to the question, “Do you now use e-cigarettes or other vaping products every day, some days, or not at all?” We classified e-cigarette smokers into 4 statuses, as follows: everyday e-cigarette user, some days e-cigarette user, former e-cigarette user, and non–e-cigarette user.
Depression and Mental Health
The dependent variable of interest was depression, defined as a self-reported history of clinical diagnosis if participants answered yes to the question, “Has a physician ever told you have a depressive disorder (including depression, major depression, dysthymia, or minor depression)?”15,16 In separate supporting analyses, subjective poor mental health was explored as an alternative outcome, defined by evaluating participants’ response to the question, “Now thinking about your mental health, which includes stress, depression, and problems with emotions, for how many days during the past 30 days was your mental health not good?”17
Covariate Assessment
Baseline demographic factors, including age, sex, race/ethnicity, marital status, education, and employment status, were self-reported according to BRFSS protocol. Income was defined using federal poverty line cutoffs for each state, taking into account the number of adults and children in the household for each state.18 Data on alcohol and combustible cigarette use were also collected. Heavy alcohol use was defined as more than 14 drinks per week for men and more than 7 drinks per week for women. Combustible cigarette smoking status was categorized as current, former, and never.
Statistical Analysis
The BRFSS uses design weighting and iterative proportional fitting to ensure representativeness of the data.19 These weights were applied in all analyses done with the data set.
Sociodemographic and risk factor characteristics were described according to e-cigarette use categories by applying sampling design elements and using the svy subpop command. Multivariable logistic models were used to assess the association between e-cigarette use and depression, adjusting for age, sex, race/ethnicity, income, marital status, employment, education, heavy alcohol use, and combustible cigarette smoking. The prevalence of depression in the data set was high at 18.9%; thus, supplemental analyses were also performed using Poisson regression models to test the stability of the estimates. Given the known high prevalence of use of e-cigarettes among the younger population as well as among smokers, we performed subgroup analyses among college students and among combustible cigarette users.
Formal effect modification was tested using interaction terms for e-cigarette use and sex, age, race/ethnicity, and cigarette smoking. Stratified analyses were then performed and presented by these variables.
To further test our estimates, subjective mental health was explored as an alternative outcome. We compared those reporting 1 or more days of poor mental health with those reporting no days of poor mental health.
All analyses were conducted using Stata statistical software version 14.2 (StataCorp) with the significance level set at a 2-sided P < .05. Data analysis was conducted in May 2019.
Results
Of 892 394 participants (414 326 [29.0%] aged ≥60 years; 502 448 [51.3%] women), 28 736 (4.4%) were current e-cigarette users, 111 337 (16.5%) were former e-cigarette users, and 752 321 (79.1%) were never e-cigarette users (Table 1). Compared with never e-cigarette users, current e-cigarette users were more likely to be single, men, and younger than 40 years and to concurrently use combustible cigarettes (single, 120 797 [24.3%] vs 10 517 [48.4%]; men, 318 970 [46.6%] vs 14 962 [60.1%]; aged 18-39 years, 129 085 [32.2%] vs 13 071 [62.1%]; current combustible cigarette use, 217 895 [7.9%] vs 8823 [51.8%]) (Table 1). Similar patterns were observed when comparing never e-cigarette users with former e-cigarette users (single, 120 797 [24.3%] vs 38 940 [46.7%]; men, 318 970 [46.6%] vs 55 727 [55.6%]; aged 18-39 years, 129 085 [32.2%] vs 48 808 [60.6%]; current combustible cigarette use, 217 895 [7.9%] vs 27 116 [46.7%]) (Table 1).
Table 1. Demographic and Socioeconomic Characteristics of Individuals in the BRFSS, 2016-2017, by e-Cigarette Use.
| Characteristic | No. (%)a | ||
|---|---|---|---|
| Current e-Cigarette User (n = 28 736) | Former e-Cigarette User (n = 111 337) | Never e-Cigarette User (n = 752 321) | |
| Sex | |||
| Men | 14 962 (60.1) | 55 727 (55.6) | 318 970 (46.6) |
| Women | 13 759 (39.9) | 55 573 (44.4) | 433 116 (53.4) |
| Age, y | |||
| 18-24 | 4817 (27.3) | 15 361 (23.2) | 29 687 (9.7) |
| 25-29 | 2947 (13.4) | 12 445 (14.5) | 27 425 (6.5) |
| 30-34 | 2769 (12.0) | 11 226 (13.3) | 33 531 (8.3) |
| 35-39 | 2538 (9.4) | 9776 (9.6) | 38 442 (7.7) |
| 40-44 | 2016 (8.1) | 7946 (8.0) | 39 998 (8.0) |
| 45-49 | 2280 (6.6) | 8554 (6.5) | 49 351 (7.7) |
| 50-54 | 2693 (7.4) | 10 121 (7.5) | 62 596 (9.4) |
| 55-59 | 2919 (6.1) | 11 255 (6.3) | 76 665 (8.9) |
| ≥60 | 5580 (9.6) | 23 969 (11.0) | 384 777 (33.8) |
| Race/ethnicity | |||
| White | 22 037 (71.9) | 82 726 (66.2) | 572 314(62.7) |
| Black or African American | 1645 (8.6) | 8100 (10.8) | 60 516 (11.9) |
| Hispanic | 1983(11.0) | 9037 (15.0) | 60 529 (17.2) |
| Other | 2598 (8.5) | 9632 (8.1) | 46 013 (8.1) |
| Marital Status | |||
| Married | 10 000 (32.2) | 41 450 (34.4) | 413 777 (55.0) |
| Divorced | 6329 (16.3) | 23 386 (15.7) | 110 882 (12.8) |
| Widowed | 1725 (3.1) | 6979 (3.2) | 102 372 (7.9) |
| Single | 10 517 (48.4) | 38 940 (46.7) | 120 797 (24.3) |
| Education | |||
| <High school | 2776 (14.3) | 10 208 (13.8) | 53 030 (13.4) |
| ≥High school or some college | 20 274 (72.9) | 74 262 (68.9) | 397 440 (56.4) |
| College graduate | 5627 (12.8) | 26 658 (17.4) | 299 448 (30.2) |
| Employment status | |||
| Employed | 15 987 (61.9) | 64 375 (63.1) | 359 362 (55.3) |
| Unemployed | 7815 (23.7) | 26 521 (21.7) | 117 920 (18.1) |
| Student | 1533 (8.9) | 5829 (8.9) | 16 064 (5.1) |
| Retired | 3192 (5.5) | 13 856 (6.4) | 253 949 (21.6) |
| Income, % of poverty line | |||
| <100 | 4507 (17.6) | 16 381 (17.4) | 61 729 (13.3) |
| 100-200 | 6864 (23.3) | 26 066 (23.5) | 142 894 (19.6) |
| >200 | 14 505 (59.1) | 58 940 (59.2) | 500 317 (67.1) |
| Heavy alcohol use | 3183 (11.8) | 12 047 (11.9) | 36 081 (4.8) |
| Combustible cigarette smoking | |||
| Never | 3884 (19.5) | 25 601 (30.5) | 473 736 (67.9) |
| Current | 8823 (51.8) | 27 116 (46.7) | 217 895 (7.9) |
| Former | 15 887 (28.8) | 58 085 (22.8) | 56 486 (24.2) |
| Use of other tobacco productsb | 2062 (8.0) | 7287 (6.6) | 20 720 (2.8) |
| BMI | |||
| <18.5 | 814 (3.1) | 2423 (2.4) | 10 692 (1.8) |
| 18.5 to <25.0 | 9614 (36.5) | 36 541 (36.5) | 216 473 (31.9) |
| 25.0 to <30.0 | 8998 (32.0) | 35 665 (32.9) | 256 803 (35.9) |
| ≥30 | 8206 (28.4) | 31 693 (28.2) | 217 640 (30.4) |
| Any physical activity outside of work in last 30 d | 19 947 (74.5) | 77 806 (74.6) | 548 009 (74.4) |
| Self-reported poor mental health days | |||
| 0 | 13 475 (47.0) | 57 081 (50.4) | 529 450 (68.9) |
| ≥1 | 14 781 (53.0) | 52 557(49.6) | 211 535 (31.1) |
| History of clinical depression | 10 633 (34.1) | 34 197 (27.6) | 124 032 (15.3) |
Abbreviations: BMI, body mass index (calculated as weight in kilograms divided by height in meters squared); BRFSS, Behavioral Risk Factor Surveillance System; e-cigarette, electronic cigarette.
Percentages are weighted to represent the general population.
Defined as current use of chewing tobacco, snuff, or snus every day or some days.
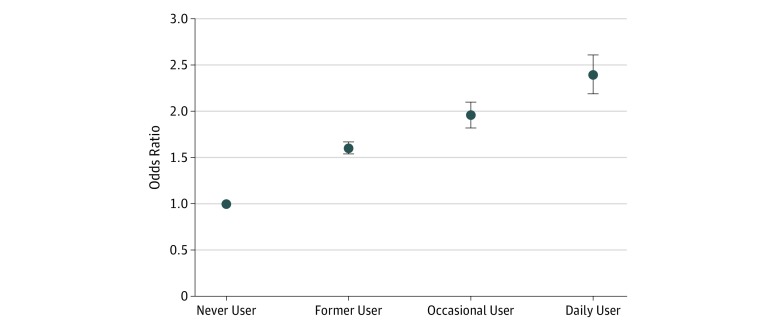
In multivariable-adjusted logistic regression analyses, compared with never users, former e-cigarette users had 1.60-fold (95% CI, 1.54-1.67) higher odds of reporting a history of clinical diagnosis of depression, while current e-cigarette users had 2.10-fold (95% CI, 1.98-2.23) higher odds. Among current e-cigarette users, we found graded higher odds of reporting depression among occasional and daily users compared with never users (occasional use: odds ratio [OR], 1.96; 95% CI, 1.82-2.10; daily use: OR, 2.39; 95% CI, 2.19-2.61) (Table 2 and Figure 1). Similar estimates were observed when multivariable-adjusted Poisson regression models were used to examine the association between e-cigarette use and depression (data not shown).
Table 2. Association Between e-Cigarette Use and History of Clinical Diagnosis of Depression and Subjective Poor Mental Health.
| e-Cigarette Use Status | OR (95% CI) | |||
|---|---|---|---|---|
| Clinical Diagnosis of Depression | Subjective Poor Mental Health | |||
| Unadjusted | Adjusteda | Unadjusted | Adjusteda | |
| Never users | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| Former users | 2.12 (2.06-2.18) | 1.60 (1.54-1.67) | 2.18 (2.13-2.24) | 1.52 (1.47-1.57) |
| Current users | 2.87 (2.74-3.01) | 2.10 (1.98-2.23) | 2.50 (2.39-2.62) | 1.67 (1.58-1.76) |
| Occasional use | 2.73 (2.58-2.89) | 1.96 (1.82-2.10) | 2.64 (2.50-2.80) | 1.73 (1.61-1.85) |
| Daily use | 3.17 (2.94-3.42) | 2.39 (2.19-2.61) | 2.25 (2.09-2.42) | 1.57 (1.44-1.70) |
Abbreviations: e-cigarette, electronic cigarette; OR, odds ratio.
Adjusted for age, sex, race/ethnicity, income, marital status, education, employment, heavy alcohol use, and combustible cigarette use.
Figure 1. Association Between Electronic Cigarette Use and History of Clinical Diagnosis of Depression.
Odds ratios are adjusted for age, sex, race/ethnicity, income, marital status, education, employment, heavy alcohol use, and combustible cigarette use. Point estimates are represented with dots, and 95% CIs represented with upper and lower horizontal bars.
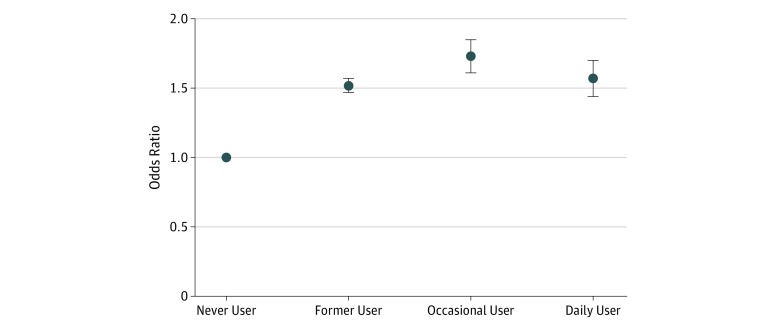
In separate supporting analyses using self-reported days of poor mental health as a binary dependent variable, compared with never users who reported no days of poor mental health, former users had 1.52-fold (95% CI, 1.47-1.57) higher odds of reporting at least 1 day of poor mental health, while current users had 1.67-fold (95% CI, 1.58-1.76) higher odds. Similarly, occasional and daily users were more likely to report at least 1 day of poor mental health compared with never users (occasional use: OR, 1.73; 95% CI, 1.61-1.85; daily use: OR, 1.57; 95% CI 1.44-1.70) (Table 2 and Figure 2).
Figure 2. Association Between Electronic Cigarette Use and Subjective Poor Mental Health.
Odds ratios are adjusted for age, sex, race/ethnicity, income, marital status, education, employment, heavy alcohol use, and combustible cigarette use. Point estimates are represented with dots, and 95% CIs represented with upper and lower horizontal bars.
Among never cigarette smokers, current e-cigarette users were 2.16-fold (95% CI, 1.87-2.49) more likely to report depression compared with never e-cigarette users. These results were similar when comparing dual users to current smokers who never used e-cigarettes (OR, 2.11; 95% CI, 1.94-2.30) (Table 3).
Table 3. Association Between e-Cigarette Use and Depression by Combustible Cigarette Smoking Status.
| e-Cigarette Use Status | OR (95% CI)a | ||
|---|---|---|---|
| Never Smoker (N = 503 221) | Former Smoker (N = 253 834) | Current Smoker (N = 130 458) | |
| Never user | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| Former user | 1.63 (1.52-1.76) | 1.59 (1.48-1.71) | 1.57 (1.48-1.66) |
| Current user | 2.16 (1.87-2.49) | 1.89 (1.71-2.10) | 2.11 (1.94-2.30) |
Abbreviations: e-cigarette, electronic cigarette; OR, odds ratio.
Adjusted for age, sex, race/ethnicity, income, marital status, education, employment, heavy alcohol use.
Both men and women who were current e-cigarette users were twice as likely to report depression compared with never e-cigarette users (men: OR, 2.17; 95% CI 2.00-2.35; women: OR, 2.05; 95% CI, 1.88-2.24) (eTable 1 in the Supplement). Similar results were also observed across strata of age and race, and among students (eg, current users aged 18-24 years: OR, 2.22; 95% CI, 1.92-2.57; current users who are Hispanic: OR, 2.45; 95% CI, 1.99-3.03; current users who are students: OR, 2.01; 95% CI, 1.58-2.56) (eTable 2, eTable 3, and eTable 4 in the Supplement).
In subgroup analyses, we observed statistically significant interactions between e-cigarette use and age (OR per increase in age category, 0.97; 95% CI, 0.96-0.97; P < .001), sex (women vs men: OR, 1.13; 95% CI, 1.08-1.18; P < .001), and race/ethnicity (white individuals vs individuals of other races/ethnicities: OR, 1.07; 95% CI, 1.04-109; P < .001). However, point estimates of the association between e-cigarette use and depression were qualitatively consistent across all subgroups, with a consistently increased odds of depression with former e-cigarette use and an even stronger association with current e-cigarette use. No statistically significant interactions were observed between e-cigarette use and cigarette smoking (OR, 1.03; 95% CI, 1.00-1.10; P = .09).
Discussion
In this cross-sectional analysis of a large nationally representative survey of adults in the United States, we found that former and current e-cigarette users were more likely to report a history of clinical diagnosis of depression compared with never users. In addition, we found a graded association between frequency of use and depression. We further explored subgroups defined by age and race and found no significant differences in the association between e-cigarettes and depression or mental health, suggesting that the association between e-cigarettes and these mental health outcomes was similar across these broad segments of the population.
Our study provides additional evidence to establish an association between e-cigarette use and depression, which could have potentially significant implications for public health, clinical practice, and health policy. Our results are supported by findings from a small longitudinal study by Lechner et al20 conducted among adolescents in Los Angeles, California, which showed that sustained e-cigarette use was associated with an increase in depression symptoms over a 12-month period. While cross-sectional, our sample size was larger, enabling us to conduct important subgroup analyses.
Similar to a study that was conducted in France in 2019,21 we also found that the association between e-cigarettes and depression did not differ significantly by sex or among current and former cigarette smokers. However, while that study found no association between e-cigarettes and depression in nonsmokers, we found that never cigarette smokers who used e-cigarettes had twice the odds of reporting a clinical diagnosis depression compared with those who did not use e-cigarettes, an estimate similar to that found among dual users.
Previous work has shown that college students are more likely to explore new products, including e-cigarettes, and it is not uncommon for this group to be targeted by tobacco companies’ marketing strategies.22,23 Therefore, we explored the association between e-cigarette use and depression in the subpopulation and found that current e-cigarette users also had twice the odds of reporting depression compared with never users in the same category. This highlights the potential susceptibility of e-cigarette users in this group to depression.
Prolonged nicotine exposure has been shown to disrupt the cerebral dopamine pathway, amplify stress sensitivity, and distort the coping mechanisms that buffer against depressive symptoms.20 As many e-cigarettes contain nicotine,4,24 this could explain the graded association seen with increased frequency of use and depression, suggesting a potential dose-response relationship. In addition to nicotine, e-cigarettes contain varying amounts of trace metals including arsenic, aluminum, and lead,25,26,27 many of which are on the priority pollutant list of the Agency for Toxic Substances and Disease registry, with known adverse health effects.26 In particular, lead and aluminum affect the central and peripheral nervous systems and may potentially contribute to the observed association between e-cigarettes and depression.27
Traditional cigarette smoking affects the metabolism of a number of psychiatric medications, mainly via the induction of metabolic enzymes, leading to reduced blood levels and reduced therapeutic effectiveness.28,29 Analyses of e-cigarette contents have shown that they also contain tobacco-specific nitrosamines and some volatile organic compounds, although in less quantity than observed in traditional cigarettes.30,31 This raises further concern about the use of e-cigarettes among individuals with MHCs, as their use might complicate the treatment of psychiatric conditions.
Furthermore, a higher frequency of regular cigarette smoking has been reported among people with major depression compared with individuals who have never had major depression or any psychiatric illness,32,33 and a brief prospective study done in adolescents found smoking to increase the risk of developing an episode of major depressive disorder.34 Among traditional cigarette smokers, patients with depression are less likely to successfully quit smoking, possibly because of worsening depressive symptoms during quitting attempts and poor tolerance of nicotine withdrawal symptoms.21 Smoking has also been shown to be highly predictive of future suicidal behavior, making it particularly concerning in individuals with a history of depression.35 Considering the similarities between e-cigarettes and traditional cigarettes, individuals with depression might be more susceptible to sustained use of e-cigarettes and may find it harder to reduce or quit their e-cigarette use. Furthermore, e-cigarette use might predispose users to developing major depression in the long term.
Consistent evidence of the gateway theory of an association between e-cigarette use and subsequent cigarette smoking initiation has been reported in a meta-analysis done by Soneji et al.36,37,38 This theory, as well as the well-established addictive nature of nicotine,39,40 make the rapid uptake of e-cigarettes among teenagers—described as an epidemic by the US Food and Drug Administration41 and the US Surgeon General42—particularly concerning, especially because our findings show no difference in association between e-cigarette use and depression among younger and older adults.
Our findings, if confirmed in other study designs with longitudinal follow-up, may provide data to inform policies that could protect populations susceptible to depression. For example, the association between e-cigarette use and depression might justify further regulation of advertisements and marketing strategies, appropriate warning labels that highlight the potential risk of depression associated with e-cigarette use, and public health education about the potential effects of e-cigarettes, especially among those with MHCs. This association could also inform clinical practice by providing information that physicians could consider in counselling patients seeking information about the use of e-cigarettes, especially those with depression. At the very least, our findings warrant careful and thorough evaluation of e-cigarette use in both youth and adults with depression. Physicians should consider routine collection of information pertaining to e-cigarette use during clinic visits, especially in patients with depression, and routine counseling for those who use e-cigarettes, offering support to those who express willingness to quit.
Strengths and Limitations
To our knowledge, this study was the first to examine the association between e-cigarette use and depression across several subpopulations in the largest nationally representative database in the United States. However, our study has limitations. It was observational and cross-sectional, and therefore, we can neither infer causality nor ascertain the direction of the association, which we submit might be bidirectional. Furthermore, we lacked granular information on product characteristics, such as the brands of e-cigarettes used, and detailed exposure characterization, including frequency or duration of vaping. We also cannot exclude the possibility of residual confounding. Finally, data on both the exposure and outcome were self-reported, which might lead to nonrandom misclassification.
Conclusions
Our results suggest a strong association between e-cigarette use and depression, and this may have potential implications for regulation of e-cigarettes. Our results also highlighted the need for longitudinal studies to investigate the risk of depression associated with e-cigarette use and the potential bidirectionality of the association between e-cigarette use and depression.
eTable 1. Association Between e-Cigarette Use and Depression, Stratified by Sex
eTable 2. Association Between e-Cigarette Use and Depression, Stratified by Age
eTable 3. Association Between e-Cigarette Use and Depression, Stratified by Race/Ethnicity
eTable 4. Association Between e-Cigarette Use and Depression Among Students
References
- 1.Mirbolouk M, Charkhchi P, Kianoush S, et al. Prevalence and distribution of e-cigarette use among U.S. adults: behavioral risk factor surveillance system, 2016. Ann Intern Med. 2018;169(7):-. doi: 10.7326/M17-3440 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Jaber RM, Mirbolouk M, DeFilippis AP, et al. Electronic cigarette use prevalence, associated factors, and pattern by cigarette smoking status in the United States from NHANES (National Health and Nutrition Examination Survey) 2013-2014. J Am Heart Assoc. 2018;7(14):e008178. doi: 10.1161/JAHA.117.008178 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Menakuru S, Inzamam Ali M. Beliefs and reality of e-cigarette smoking. BMJ Case Rep. 2018;2018:bcr-2018-bcr-225683. doi: 10.1136/bcr-2018-225683 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rom O, Pecorelli A, Valacchi G, Reznick AZ. Are e-cigarettes a safe and good alternative to cigarette smoking? Ann N Y Acad Sci. 2015;1340:65-74. doi: 10.1111/nyas.12609 [DOI] [PubMed] [Google Scholar]
- 5.Jackler RK, Ramamurthi D. Nicotine arms race: JUUL and the high-nicotine product market. Tob Control. 2019. doi: 10.1136/tobaccocontrol-2018-054796 [DOI] [PubMed] [Google Scholar]
- 6.Olmedo P, Goessler W, Tanda S, et al. Metal concentrations in e-cigarette liquid and aerosol samples: the contribution of metallic coils. Environ Health Perspect. 2018;126(2):027010. doi: 10.1289/EHP2175 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Spears CA, Jones DM, Weaver SR, Pechacek TF, Eriksen MP. Use of electronic nicotine delivery systems among adults with mental health conditions, 2015. Int J Environ Res Public Health. 2016;14(1):E10. doi: 10.3390/ijerph14010010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cummins SE, Zhu SH, Tedeschi GJ, Gamst AC, Myers MG. Use of e-cigarettes by individuals with mental health conditions. Tob Control. 2014;23(suppl 3):iii48-iii53. doi: 10.1136/tobaccocontrol-2013-051511 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tidey JWE, Miller ME. Smoking cessation and reduction in people with chronic mental illness. BMJ. 2015;351:h4065. doi: 10.1136/bmj.h4065 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62(6):593-602. doi: 10.1001/archpsyc.62.6.593 [DOI] [PubMed] [Google Scholar]
- 11.Wu B, Cai Q, Sheehan JJ, Benson C, Connolly N, Alphs L. An episode level evaluation of the treatment journey of patients with major depressive disorder and treatment-resistant depression. PLoS One. 2019;14(8):e0220763. doi: 10.1371/journal.pone.0220763 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Murthy VH. e-Cigarette use among youth and young adults: a major public health concern. JAMA Pediatr. 2017;171(3):209-210. doi: 10.1001/jamapediatrics.2016.4662 [DOI] [PubMed] [Google Scholar]
- 13.US Centers for Disease Control and Prevention Behavioral Risk Factor Surveillance System. https://www.cdc.gov/brfss/index.html. Accessed March 30, 2019.
- 14.Electronic Code of Federal Regulations Protection of Human Subjects. https://www.ecfr.gov/cgi-bin/retrieveECFR?gp=&SID=83cd09e1c0f5c6937cd9d7513160fc3f&pitd=20180719&n=pt45.1.46&r=PART&ty=HTML. Accessed September 19, 2019.
- 15.Strine TW, Mokdad AH, Balluz LS, et al. Depression and anxiety in the United States: findings from the 2006 Behavioral Risk Factor Surveillance System. Psychiatr Serv. 2008;59(12):1383-1390. doi: 10.1176/ps.2008.59.12.1383 [DOI] [PubMed] [Google Scholar]
- 16.McClave AK, Dube SR, Strine TW, Kroenke K, Caraballo RS, Mokdad AH. Associations between smoking cessation and anxiety and depression among U.S. adults. Addict Behav. 2009;34(6-7):491-497. doi: 10.1016/j.addbeh.2009.01.005 [DOI] [PubMed] [Google Scholar]
- 17.Chekroud SR, Gueorguieva R, Zheutlin AB, et al. Association between physical exercise and mental health in 1.2 million individuals in the USA between 2011 and 2015: a cross-sectional study. Lancet Psychiatry. 2018;5(9):739-746. doi: 10.1016/S2215-0366(18)30227-X [DOI] [PubMed] [Google Scholar]
- 18.Federal Register Annual Update of the HHS Poverty Guidelines. https://www.federalregister.gov/documents/2017/01/31/2017-02076/annual-update-of-the-hhs-poverty-guidelines. Accessed March 18, 2019.
- 19.US Centers for Disease Control and Prevention Weighting the BRFSS Data. https://www.cdc.gov/brfss/annual_data/2017/pdf/weighting-2017-508.pdf. Accessed March 18, 2019.
- 20.Lechner WV, Janssen T, Kahler CW, Audrain-McGovern J, Leventhal AM. Bi-directional associations of electronic and combustible cigarette use onset patterns with depressive symptoms in adolescents. Prev Med. 2017;96:73-78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wiernik E, Airagnes G, Lequy E, et al. Electronic cigarette use is associated with depressive symptoms among smokers and former smokers: cross-sectional and longitudinal findings from the Constances cohort. Addict Behav. 2019;90:85-91. doi: 10.1016/j.addbeh.2018.10.021 [DOI] [PubMed] [Google Scholar]
- 22.Sutfin EL, McCoy TP, Morrell HER, Hoeppner BB, Wolfson M. Electronic cigarette use by college students. Drug Alcohol Depend. 2013;131(3):214-221. doi: 10.1016/j.drugalcdep.2013.05.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rigotti NA, Lee JE, Wechsler H. US college students’ use of tobacco products: results of a national survey. JAMA. 2000;284(6):699-705. doi: 10.1001/jama.284.6.699 [DOI] [PubMed] [Google Scholar]
- 24.Schroeder MJ, Hoffman AC. Electronic cigarettes and nicotine clinical pharmacology. Tob Control. 2014;23(suppl 2):ii30-ii35. doi: 10.1136/tobaccocontrol-2013-051469 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Zhao J, Nelson J, Dada O, Pyrgiotakis G, Kavouras IG, Demokritou P. Assessing electronic cigarette emissions: linking physico-chemical properties to product brand, e-liquid flavoring additives, operational voltage and user puffing patterns. Inhal Toxicol. 2018;30(2):78-88. doi: 10.1080/08958378.2018.1450462 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Badea M, Luzardo OP, González-Antuña A, et al. Body burden of toxic metals and rare earth elements in non-smokers, cigarette smokers and electronic cigarette users. Environ Res. 2018;166:269-275. doi: 10.1016/j.envres.2018.06.007 [DOI] [PubMed] [Google Scholar]
- 27.Gaur S, Agnihotri R. Health effects of trace metals in electronic cigarette aerosols: a systematic review. Biol Trace Elem Res. 2019;188(2):295-315. doi: 10.1007/s12011-018-1423-x [DOI] [PubMed] [Google Scholar]
- 28.Hall SM, Prochaska JJ. Treatment of smokers with co-occurring disorders: emphasis on integration in mental health and addiction treatment settings. Annu Rev Clin Psychol. 2009;5:409-431. doi: 10.1146/annurev.clinpsy.032408.153614 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Zevin S, Benowitz NL. Drug interactions with tobacco smoking. An update. Clin Pharmacokinet. 1999;36(6):425-438. [DOI] [PubMed] [Google Scholar]
- 30.Goniewicz ML, Knysak J, Gawron M, et al. Levels of selected carcinogens and toxicants in vapour from electronic cigarettes. Tob Control. 2014;23(2):133-139. doi: 10.1136/tobaccocontrol-2012-050859 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Patel D, Davis KC, Cox S, et al. Reasons for current e-cigarette use among U.S. adults. Prev Med. 2016;93:14-20. doi: 10.1016/j.ypmed.2016.09.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Covey LS, Glassman AH, Stetner F. Cigarette smoking and major depression. J Addict Dis. 1998;17(1):35-46. doi: 10.1300/J069v17n01_04 [DOI] [PubMed] [Google Scholar]
- 33.Glassman AH, Helzer JE, Covey LS, et al. Smoking, smoking cessation, and major depression. JAMA. 1990;264(12):1546-1549. [PubMed] [Google Scholar]
- 34.Brown RA, Lewinsohn PM, Seeley JR, Wagner EF. Cigarette smoking, major depression, and other psychiatric disorders among adolescents. J Am Acad Child Adolesc Psychiatry. 1996;35(12):1602-1610. doi: 10.1097/00004583-199612000-00011 [DOI] [PubMed] [Google Scholar]
- 35.Prochaska JJ. Smoking and mental illness: breaking the link. N Engl J Med. 2011;365(3):196-198. doi: 10.1056/NEJMp1105248 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Soneji S, Barrington-Trimis JL, Wills TA, et al. Association between initial use of e-cigarettes and subsequent cigarette smoking among adolescents and young adults: a systematic review and meta-analysis. JAMA Pediatr. 2017;171(8):788-797. doi: 10.1001/jamapediatrics.2017.1488 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Thorndike AN. e-Cigarette use by young adult nonsmokers: next-generation nicotine dependence? Ann Intern Med. 2019;170(1):70-71. doi: 10.7326/M18-2581 [DOI] [PubMed] [Google Scholar]
- 38.Watkins SL, Glantz SA, Chaffee BW. Association of noncigarette tobacco product use with future cigarette smoking among youth in the population assessment of tobacco and health (PATH) study, 2013-2015. JAMA Pediatr. 2018;172(2):181-187. doi: 10.1001/jamapediatrics.2017.4173 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.McManus OB, Werley CA, Dempsey GT. Inhale, exhale: Probing the inside-out mechanism of nicotine addiction using novel fluorescent sensors. J Gen Physiol. 2019;151(6):714-717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Chadi N, Hadland SE, Harris SK. Understanding the implications of the “vaping epidemic” among adolescents and young adults: a call for action. Subst Abus. 2019;40(1):7-10. doi: 10.1080/08897077.2019.1580241 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.US Food and Drug Administration Statement from FDA Commissioner Scott Gottlieb, M.D., on advancing new policies aimed at preventing youth access to, and appeal of, flavored tobacco products, including e-cigarettes and cigars. https://www.fda.gov/news-events/press-announcements/statement-fda-commissioner-scott-gottlieb-md-advancing-new-policies-aimed-preventing-youth-access. Accessed April 17, 2019.
- 42.US Department of Health and Human Services e-Cigarette use among youth and young adults: a report of the Surgeon General. https://e-cigarettes.surgeongeneral.gov/documents/2016_SGR_Full_Report_non-508.pdf. Accessed April 7, 2019.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable 1. Association Between e-Cigarette Use and Depression, Stratified by Sex
eTable 2. Association Between e-Cigarette Use and Depression, Stratified by Age
eTable 3. Association Between e-Cigarette Use and Depression, Stratified by Race/Ethnicity
eTable 4. Association Between e-Cigarette Use and Depression Among Students