Abstract
Developing structures and processes for continuous sociotechnical system design is key to sustaining human factors (HF) knowledge in the context of rapid health care changes and technological innovations. Two research studies illustrate how to embed HF in organizational learning processes and structures. We need to develop innovative HF methods for continuous sociotechnical system design.
Keywords: Sociotechnical systems, organizational learning, human factors and systems engineering, continuous implementation, usability of health IT
1. Introduction
There is increasing evidence of the benefits of human factors (HF)-based health IT design for patient safety [1]. We also see how HF-based health IT design can support clinicians’ work and improve clinician outcomes, such as reduced workload [2]. The application of HF methods and design principles to health IT can make a difference for both patients and clinicians. However, we continue to see poorly designed health IT and negative impact on patients (e.g. health IT-related errors with harmful consequences for patients [3]) and clinicians (e.g. burnout [4]). Clearly, our extensive compendium of HF knowledge is not sufficiently applied. Are we providing usable HF knowledge that can be systematically applied to health IT design? Are we addressing emerging problems with health IT (e.g. health IT to support team-based care of chronically ill patients)? Are we developing HF knowledge relevant for evolving health care needs and constraints? In this paper, I focus on challenges posed to our HF community by the constantly evolving world of health care and technological innovations. I will address sustainability of HF knowledge in the context of health IT design, implementation and use.
Given rapid changes in health care and technologies, it may not be judicious to focus on sustainability of specific health IT-based interventions. Instead, we should address how our HF knowledge can be sustained and embedded in organizational learning processes and structures. This approach fits with the concept of continuous technology implementation [5]. The continuous cycle of technology design, implementation and use involves both formal and informal activities where technology users adapt to the technology and adapt the technology [6, 7]. I first review various conceptual approaches of continuous sociotechnical system design, drawing on literature in human factors and ergonomics, organizational psychology and technology adaptation. I then present two research studies that address various aspects of continuous sociotechnical system design. Finally, I compare the two studies and highlight the need for innovative HF methods of continuous sociotechnical system design.
2. Continuous Sociotechnical System Design
Sociotechnical (work) systems are dynamic systems that continuously adapt, evolve and change [6]. In the SEIPS model of work system and patient safety [8, 9], the feedback loops exemplify the dynamic nature of sociotechnical systems as they represent (1) continuous improvement and learning (e.g. data on patient safety outcomes used as input to redesign work system), and (2) adaptation to the work system or adaptation of the work system (e.g. workers learn the new work system and/or adapt system elements over time). This has major implications for sociotechnical system design, including the need to go beyond technology design and initial implementation and consider emergent properties of technology-in-use.
2.1. Sociotechnical system design as a longitudinal extended process
In 2000, Clegg [10] wrote: “Design is an extended social process”. Designing a technology and the rest of the sociotechnical (work) system is not clearly temporally bounded: it does not have a clear beginning or end. Technology design occurs over an extended period of time: before, during, immediately after and long after the technology is in use. Clegg emphasized the HF implications of this sociotechnical principle: “Different people will interpret systems in different ways, and there need to be structures and mechanisms through which views can be aired, recognized and understood”.
Participation of end users and more broadly of stakeholders is key in developing structures and processes for organizational learning that extends over time. Initially, HF experts may accompany end users and other stakeholders in their individual learning, e.g. skills in usability evaluation. Over time, organizational learning and integration of HF in organizational structures and processes will move from external regulation (e.g. HF experts) to internal regulation (e.g. “just-in-case” HF consultants) [11].
2.2. Continuous change and emergent technology-in-use
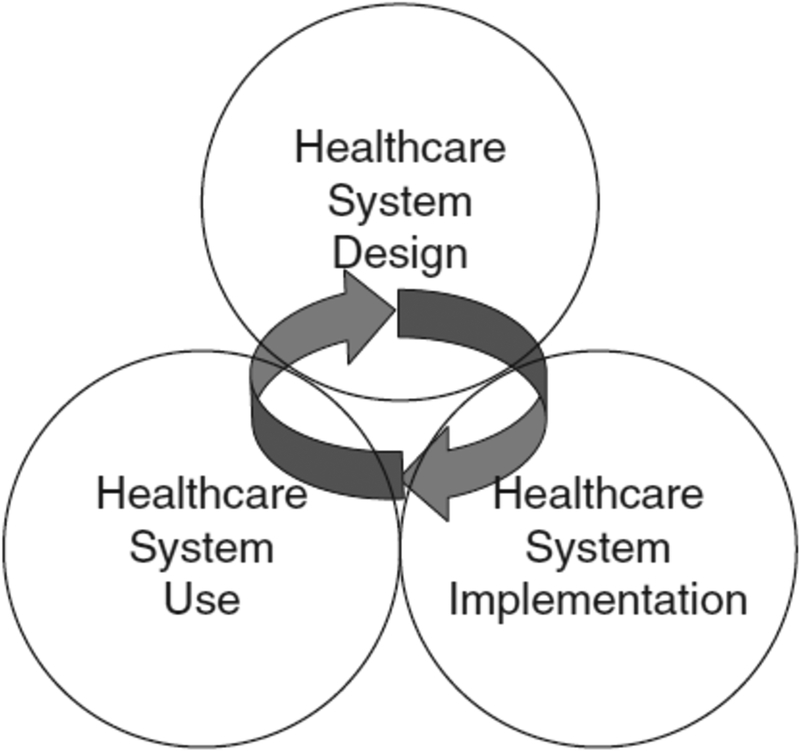
As proposed by Weick and Quinn [12], episodic change is infrequent, discontinuous and intentional. Effective approaches for managing episodic changes, such as implementation of health IT, include planning for the change, change management and use of change agents or champions. In contrast to episodic change, Weick and Quinn propose continuous change, i.e., a series of ongoing, evolving, cumulative, and often uncertain and less predictable activities. Individual and organizational learning are key concepts in effective continuous change. As ongoing changes occur, individuals need to develop new skills and knowledge, and organizations need to develop new modes of functioning. Individual and organizational learning contribute to system adaptation, i.e. feedback loops in SEIPS model [8, 9]. In line with the idea of continuous change, Orlikowski and her colleagues emphasize the need to go beyond the transition phase of technology implementation and to understand technology-in-use and different ways that users adapt to and adapt the technologies [13]. In systems thinking, emergence plays a key role as system elements (including technology) interact and produce outcomes that may not have been anticipated at the stages of design or implementation. Therefore, systems evolve through continuous phases of design, implementation and use, and adapt as users interact with technologies [7] (see Figure 1).
Figure 1.
Continuous adaptation and improvement of healthcare sociotechnical systems [7].
3. Example 1: Continuous Implementation of Smart Infusion Pump Technology
Smart infusion pump technology has helped to reduce medication administration errors, but has not completely eliminated them [14]. In addition, the technology has had multiple usability challenges, e.g. alert fatigue. Whereas HF methods such as proactive risk assessment can identify and mitigate design vulnerabilities [15], these methods are not full-proof and, as suggested above, technology-in-use may bring up emergent issues that were not anticipated at the design stage. In a study on the implementation of smart IV pump technology in an academic hospital, we described what we call “continuous technology implementation” [5]. Using Weick and Quinn’s [12] framework, we identified activities and processes related to both episodic and continuous changes.
Before the smart IV pump technology was implemented, the hospital convened a committee to evaluate various IV pump technologies, conducted an ROI analysis of IV pump technology, performed an FMEA of the IV administration process [15], executed a pilot test of the new IV pump technology on one hospital unit, and conducted extensive just-in-time training for all pump users (e.g. nurses and anesthesiologists). These activities aimed at managing the episodic change, i.e., the implementation of smart IV pump technology in the entire hospital. A few weeks after the IV pump technology was in use, a major safety event occurred; fortunately the event did not produce long-term patient harm [16]. The safety event was followed by multiple activities that fit the concept of continuous change. The hospital had developed capabilities to react quickly to the safety event, as well as an open organizational culture for error detection and correction. The FMEA team was reconstituted as a multidisciplinary (e.g. nursing, anesthesia, medicine, pharmacy, human factors engineering) implementation team, which led the investigation of the pump-related safety event. A small interdisciplinary group was rapidly organized to conduct usability evaluation of the various IV pump technology versions produced by the manufacturer [17]. Both individual and organizational learning occurred in this phase of continuous technology implementation.
4. Example 2: Collaborative Usability Evaluation (CUE) Model for Inpatient EHR Implementation
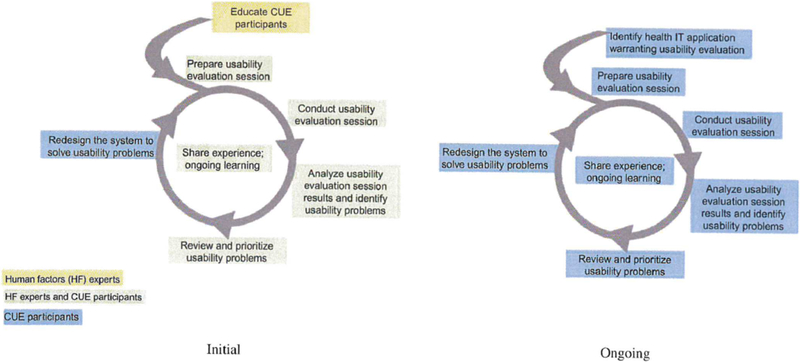
Usability of EHR technology remains a major concern with responsibilities shared by EHR manufacturers, vendors and implementers [18]. In particular, technology design decisions made by health care organizations contribute to (lack of) usability of EHR technology [19]. A challenge is then how to institutionalize usability skills and processes in health care organizations. In collaboration with a large health care organization, we developed a participatory ergonomics model aimed at building a network of individuals trained and proficient at usability evaluation [20]. As shown in Figure 2, the Collaborative Usability Evaluation (CUE) model consists of two phases: an initial phase where HF experts play a significant role in setting up the network and providing training, and an ongoing phase where health IT analysts conduct usability evaluations, implement technology redesigns, and share their experience and learnings. Individual and organizational learning are key to move the CUE program from external regulation (initial phase) to internal regulation (ongoing phase) [11].
Figure 2.
Collaborative Usability Evaluation (CUE) model [20]
In the initial phase, 28 people, including IT analysts and IT leaders from the health care organization and analysts from the EHR vendor, learned and applied usability methods (e.g. heuristic evaluation, user testing, scenario-based evaluation). Over time, the collaborative network of internal usability specialists deepened their impact as they participated in ongoing discussion and application of what they learned in the initial training. In addition, usability evaluations were formally incorporated in the health care organization’s implementation timeline for all new EHR functionality and vendor upgrades.
5. Discussion and Conclusion
The two research studies provide examples of continuous sociotechnical system design and illustrate methods for embedding HF in organizational learning processes and structures. The first study shows how a health care organization reacted to a safety event after the implementation of smart IV pump technology. The second study describes an organizational approach for embedding HF in technology implementation. Table 1 compares the two examples on multiple characteristics of continuous sociotechnical system design, and emphasizes the developmental or constructive perspective to HF, i.e., an approach that focuses on both individual and organizational learning [21]. Participation of end users and stakeholders from various disciplines, units and organizational levels is key to developing and sustaining learning.
Table 1.
Characteristics of continuous sociotechnical system design.
| Characteristics | Continuous implementation of smart IV pump technology | CUE model for organizational health IT usability |
|---|---|---|
| Initial structures & processes | IV pump committee; FMEA team; pilot test; training on new IV pump | Two phases of in-house usability training for 28 CUE participants; shared experience and learning |
| Ongoing structures & processes | Implementation team; multidisciplinary safety investigation; multiple usability evaluation cycles | Usability evaluation embedded in health IT implementation timeline; shared experience and learning |
| User & stakeholder participation | IV pump nurse as liaison; participants in usability evaluation; multidisciplinary teams (FMEA, implementation, event investigation) | 28 CUE participants (including 2 analysts from EHR vendor); participants in usability evaluation; involvement of hospital IT leaders |
| HF methods | FMEA, usability evaluation, safety investigation | Usability evaluation (heuristics, scenario-based) |
| Individual learning | Skills and knowledge in usability evaluation and safety investigation | Skills and knowledge in usability evaluation |
| Organizational learning | Multidisciplinary structures and processes; open organizational culture for error detection and correction | Incorporation of scenario-based usability evaluation in health IT implementation timeline for all new EHR functionality and vendor releases/upgrades |
The two studies provide examples of HF methods for continuous sociotechnical system design (i.e., continuous technology implementation and collaborative usability model), and demonstrate that sustaining HF knowledge cannot be considered as a “one shot” activity. Designing usable health IT is important, but it needs to be embedded in a broader organizational framework to be sustained and have continued impact. In 2004, Bentzi Karsh wrote an important article on “Beyond usability: Designing effective technology implementation systems to promote patient safety” [22]. He argued that we need to not only consider HF technology design (e.g. usability), but also consider HF and organizational methods for implementation and change management. I am proposing to go “beyond-beyond” usability and to not only consider technology design and implementation but also technology-in-use (see Figure 1). Effort should be dedicated to the development of HF methods to support the extended sociotechnical system design process described by Clegg [10]. Because health IT users often collaborate to provide team-based care, we need to develop HF methods through which multiple (team members’) perspectives can be shared and understood. This may, for instance, rely on visual methods such as cognitive mapping [23] or collaborative design approaches [24]. For HF to make deep, sustained impact on health IT and both patient and clinician outcomes, we need to support the continuous process of sociotechnical system design.
Acknowledgments
This research was supported by the Clinical and Translational Science Award (CTSA) program, through the NIH National Center for Advancing Translational Sciences (NCATS), Grant UL1TR000427. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
References
- [1].Russ AL, Zillich AJ, Melton BL, Russell SA, Chen S, Spina JR, et al. , Applying human factors principles to alert design increases efficiency and reduces prescribing errors in a scenario-based simulation, J Am Med Inform Assoc 21 (2014), e287–e96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Mazur LM, Mosaly PR, Moore C, and Marks L, Association of the usability of electronic health records with cognitive workload and performance levels among physicians, JAMA Network Open 2 (2019), e191709–e09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Ratwani RM, Savage E, Will A, Fong A, Karavite D, Muthu N, et al. , Identifying electronic health record usability and safety challenges in pediatric settings, Health Aff 37 (2018), 1752–1759. [DOI] [PubMed] [Google Scholar]
- [4].Gardner RL, Cooper E, Haskell J, Harris DA, Poplau S, Kroth PJ, et al. , Physician stress and burnout: the impact of health information technology, J Am Med Inform Assoc 26 (2018), 106–114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Carayon P, Wetterneck TB, Hundt AS, Rough S, and Schroeder M, Continuous technology implementation in health care: The case of advanced IV infusion pump technology, in: Zink K (Ed.), Corporate Sustainability as a Challenge for Comprehensive Management, Springer, NewYork, 2008,139–151. [Google Scholar]
- [6].Carayon P, Human factors of complex sociotechnical systems, Appl Ergon 37 (2006), 525–535. [DOI] [PubMed] [Google Scholar]
- [7].Carayon P, Bass EJ, Bellandi T, Gurses AP, Hallbeck MS, and Mollo VV. Sociotechnical systems analysis in health care: A research agenda, IIE Transactions on Healthcare Systems Engineering, 1 (2011), 145–160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Carayon P, Hundt AS, Karsh B-T, Gurses AP, Alvarado CJ, Smith M, et al. , Work system design for patient safety: The SEIPS model, Quality & Safety in Health Care 15 (2006), i50–i58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Carayon P, Wetterneck TB, Rivera-Rodriguez AJ, Hundt AS, Hoonakker P, Holden R, et al. , Human factors systems approach to healthcare quality and patient safety, Appl Ergon 45 (2014), 14–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Clegg CW, Sociotechnical principles for system design, Appl Ergon 31 (2000), 463–477. [DOI] [PubMed] [Google Scholar]
- [11].Haims MC and Carayon P, Theory and practice for the implementation of ‘in-house’, continuous improvement participatory ergonomic programs, Appl Ergon 29 (1998), 461–472. [DOI] [PubMed] [Google Scholar]
- [12].Weick KE and Quinn RE, Organizational change and development, Annu Rev Psychol 50 (1999), 361–386. [DOI] [PubMed] [Google Scholar]
- [13].Tyre MJ and Orlikowski WJ, Windows of opportunity: Temporal patterns of technological adaptation in organizations, Organization Science 5 (1994), 98–188. [Google Scholar]
- [14].Ohashi K, Dalleur O, Dykes PC, and Bates DW, Benefits and risks of using smart pumps to reduce medication error rates: A systematic review, Drug Saf 37 (2014), 1011–1020. [DOI] [PubMed] [Google Scholar]
- [15].Wetterneck TB, Skibinski KA, Roberts TL, Kleppin SM, Schroeder ME, Enloe M, et al. , Using failure mode and effects analysis to plan implementation of Smart intravenous pump technology, Am J Health Syst Pharm 63 (2006),1528–1538. [DOI] [PubMed] [Google Scholar]
- [16].Schroeder ME, Wolman RL, Wetterneck TB, and Carayon P, Tubing misload allows free flow event with Smart intravenous infusion pump, Anesthesiology 105 (2006), 434–435. [DOI] [PubMed] [Google Scholar]
- [17].Hundt AS, Carayon P, Wetterneck TB, Schroeder M, and Enloe M, Evaluating design changes of a smart IV pump, in: Tartaglia R, Bagnara S, Bellandi T, Albolino S (Eds), Healthcare Systems Ergonomics and Patient Safety, Taylor & Francis, Florence, Italy, 2005, 239–242. [Google Scholar]
- [18].Sittig DF, Belmont E, and Singh H, Improving the safety of health information technology requires shared responsibility: It is time we all step up, Healthcare 6 (2018), 7–12. [DOI] [PubMed] [Google Scholar]
- [19].Ratwani RM, Savage E, Will A, Arnold R, Khairat S, Miller K, et al. , A usability and safety analysis of electronic health records: a multi-center study, J Am Med Inform Assoc 25 (2018), 1197–1201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Hundt AS, Adams JA, and Carayon P, Collaborative Usability Evaluation (CUE) model for health IT design and implementation, International Journal of Human–Computer Interaction 33 (2016): 287–297. [Google Scholar]
- [21].Falzon P, Constructive Ergonomics, CRC Press, Boca Raton, FL, 2015. [Google Scholar]
- [22].Karsh BT, Beyond usability: Designing effective technology implementation systems to promote patient safety, Quality and Safety in Health Care 13 2004, 388–394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Kjaergaard AL, Jensen TB, Using cognitive mapping to represent and share users’ interpretations of technology, Communications of the Association for Information Systems 34 (2014), 1097–1114. [Google Scholar]
- [24].Détienne F, Collaborative design: Managing task interdependencies and multiple perspectives, Interacting with Computers 18 (2006), 1–20. [Google Scholar]