Abstract
Purpose
Based on Q methodology, this study investigated the motivation of orthodontic treatment for patients and their parents. Through investigation, this paper attempts to explore the motivational factors of CLP and NON-CLP children and their parents, which are different or general.
Patients and methods
Q methodology involves 4 phases. (1) Interviews of CLP (N=5), NON-CLP (N=5) patients generated 30 statements (Q-set 1) and CLP (N=5), NON-CLP (N=5) patients’ parents produced 36 statements (Q-set 2) about different reasons to pursue orthodontic care. (2) P-set: recruitment participants. The sample comprised 40 CLP patients (G1) and 40 NON-CLP patients (G2) aged 9–16 years, 40 CLP patients’ parents (G3) and 40 NON-CLP patients’ parents (G4) wanting their children to have orthodontic treatment. (3) Q-sort: 4 groups ranked statements in order of comparative significance using enforced distribution grids (G1, G2 ranked Q-set 1; G3, G4 ranked Q-set 2). (4) Analysis: using the PQMehtod 2.35 vision to analyze data.
Results
Three factors in each group were identified as representing the most widespread views of the majority of the participants, described as G1: (1) aesthetics, (2) preparation for other oral treatments, (3) timely. G2: (1) admiration of others, aesthetics, (2) oral function, (3) oral hygiene and improvement of smile. G3: (1) worrying about the future of children, parents’ responsibilities, children’s feelings; (2) mental health, timely; (3) parents’ responsibilities, ready for treatment. G4: (1) aesthetics, children’s will; (2) future problems, timely; (3) timely, parents’ responsibility and no need to worry about physical problems.
Conclusion
CLP and NON-CLP patients and parents have different orthodontic treatment motives, yet, they still shared 3 global motivation themes, respectively. Consideration of these motives may help clinicians develop their treatment discussions with patients and parents, which could consequently improve their cooperation and may achieve a more satisfactory outcome.
Keywords: cleft lip and/or palate patient, parent, orthodontic, Q methodology, cooperation
Introduction
Cleft lip and/or cleft palate (CLP) is one of the most common craniofacial malformations in the field of oral malformations. The incidence of cleft lip and/or cleft palate is still high in the world. There are 1–2 cleft lip and/or cleft palate in every 1000 live births.1,2 For this situation, orthodontic treatment has gradually become an important part of comprehensive treatment of CLP in children. Clinicians may be undertaken to expand the cleft-affected palatal segment prior to secondary alveolar bone graft surgery, typically when children are 9–11 years old which the maxillary canines are about to erupt.3 Removable or fixed appliance treatment may also be undertaken in adolescence. However, cooperation in the treatment process will directly lead to significant changes in the length of time patients wear orthodontic appliances.4–6 There are many reasons for the lack of patient cooperation, among which the most common reason is lack of corresponding cooperation motivation.7,8 Despite a series of research results on CLP, further research on the motivation of CLP patients to seek orthodontic treatment is still a blank field.
Considering the actual situation, it is not difficult to know that the decisive factor of orthodontic treatment lies in the agreement between doctors and patients and their parents. Previous studies have shown that by combining patients’ treatment motivation with parents’ willingness,9–11 it can be inferred that children lack sufficient cognitive ability to clearly distinguish various motivation structures.12 Social psychology questionnaire is often seemed to be used in those studies such as self-perceived dental aesthetics (Oral Aesthetic Subjective Impact Scale),13 Oral Health-Related Quality of Life (OHRQoL),14–16 State-Trait Anxiety Inventory (STAI),17 the dental aesthetic index (DAI)18 and so on. Most of those investigations were based on a large sample size of the general sample group for analysis, while some specific studies have selected targeted sample to complement, known as the Q methodology.9,11,19 As we all have known, OHRQoL including the items and the response options which are framed by conductor can reflect participants’ subjective point of views to some extent. Nevertheless, the content of the questionnaire in Q-Method was generated by the participants. It is interesting and thought-provoking to make the audience feel and see how the world looks from the diverse perspectives provided by the participants.20 This method was first proposed by William Stephenson in 1935. The main structure of this method is the improvement of Spearman’s factor analysis method.20 Q-method is a traditional methodology that links qualitative and quantitative research.21 It is a fringe enterprise in psychology and still not known by most scholars.
Q-method is often used to innovate and explore the subjective viewpoints of a particular subject. Therefore, this method is usually considered as a method to reveal subjective evaluation, and it has high compatibility and practical value.22 In particular, Davis9 and Prabakaran11 used Q methodology to explore the motivation of patients and their parents from different aspects. Based on the results of previous studies, we can find that these studies have achieved some thought-provoking results, which laid a foundation for the application of Q methodology in motivation research. However, it is worth noting that the motivation of CLP patients is often neglected in the study, and there is no further explanation of these factors on the motivation of CLP patients and their parents and the reality of orthodontic treatment.
Therefore, the main purpose of our study is to compare CLP patients and their parents with the general public sample by Q methodology, so as to preliminarily draw their motivation for orthodontic treatment. Try to figure out whether the difference between CLP groups and NON-CLP groups is greater than the commonness or not. With this purpose as traction, Q-method actually provides us with an effective way to explore the specific motivation of CLP patients and their parents. Common views may provide clinicians with a different perspective. The application of treatment plans for CLP patients and NON-CLP patients will enhance communication to a certain extent and further enhance patient coherence.
Materials and Methods
The research was conducted in the Department of Orthodontics, Shanghai Ninth People’s Hospital, Shanghai Jiao Tong University School of Medicine, Shanghai, China, from 1 June 2018 to 30 December 2018. This research has attained Ethical approval and supported by the health research ethics board at the Shanghai Ninth People’s Hospital, College of Stomatology, Shanghai Jiao Tong University School of Medicine (Ethic: SH9H-2018-T64-1), and a consent form was signed by all participants. This study was supported by the foundation: 2016YFC1000502, 2017YFC0840100, 2017YFC0840110. The participants consisted of 40 CLP patients (i.e., G1) and 40 NON-CLP patients (i.e., G2) who want to undertake orthodontic treatment, 40 CLP patients’ parents (i.e., G3) and 40 NON-CLP patients’ parents (i.e., G4) who want their children to have orthodontic treatment. The sample of G3 and G4 was recruited independently of the G1 and G2 samples to prevent baffling influences among the groups. Ensure there is a sufficiently varied participant group in terms of age, gender and relational background. The following criteria were put forward to be eligible for this research: The patient or parent’s child was between the age of 9 and 16 years. The patient self-identified with CLP or NON-CLP. Patients of G2 were excluded if they were referred for craniofacial syndromes, CLP or orthognathic surgery. Parents of G4 were excluded if their child was involved in the same situation as described above.
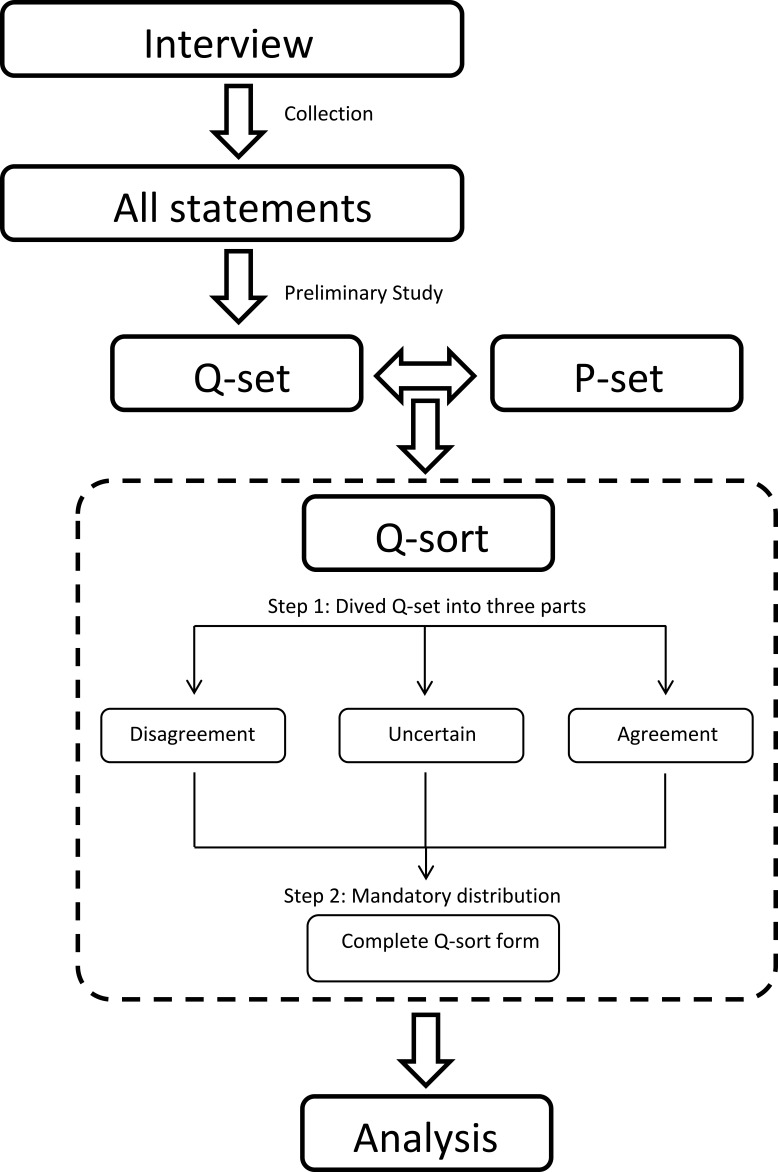
In frequent cases, the focus of the Q methodology is on participants’ first-person views, while the percentage of people with specific views is relatively neglected.23 Similarly, the Q methodology in this paper can be divided into the following four stages: (1) Q-set (concourse): collecting statements on topics. (2) P-set: recruitment participants. (3) Q-sort: ranking statements in a special form. (4) Analysis: data analysis (shown in Figure 1).
Figure 1.
Flow chart of the Q Methodology.
A researcher interviewed participants. Among them, the basic question concerning G1 and G2 was “Why do you wear braces?” (Question 1). In interviews with parents of patients, the question for G3 and G4 was “Why do you want your children to receive orthodontic treatment?” (Question 2).
Phase 1: Q-Set
According to the actual research conditions, the number of Q-sets is usually set between 30 and 140.24 An appropriate Q set covers almost all imaginable viewpoints and viewpoints related to research issues.23 In this article, the main author (Xia T) conducted an open-ended interview with 5 CLP patients and 5 NON-CLP patients (9–16 years old). Based on the results of interviews, this study summarized Question 1 until no new view on the causes of orthodontic treatment emerged.25 By organizing testers’ statements and eliminating repetitive statements, two orthodontists used a preliminary study to test and evaluate the content of statements. This pater 30 colloquial statements were generated as the final set of items, namely, Q-set 1 of G1 and G2. Subsequently, we randomly numbered Q-set 1 and printed them on 30 separate cards. In addition, in the same way, Xia T led another open-ended interview with 5 CLP patient’s parents and 5 NON-CLP patient’s parents, 35 statements were created as Q-set 2 for G3 and G4.
Phase 2: P-Set
According to relevant studies, the number of participants in this paper is suggested to be between 40 and 60.26 In order to ensure that participants’ gender and relationship background are sufficiently different, the last participant group in this study should be fair and balanced from the perspective of demography. Therefore, according to the above selection criteria, we recruited four groups of volunteers with a sample size of 40 in each group.
Phase 3: Q-Sort
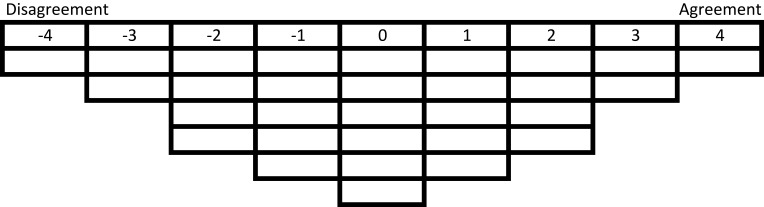
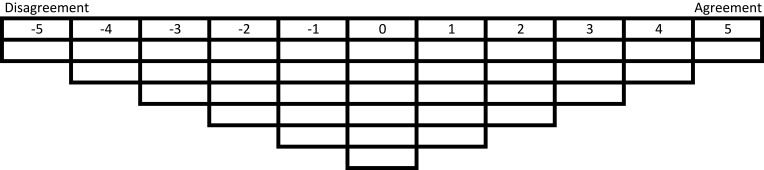
“A participant in a Q study is invited to impose their own personal meanings, or psychological Significance ….”23 The tool used in the experiment of Q methodology is Q-Sort, also known as forced selection distribution. The implication of this distribution is that each statement must be assigned a ranking position by each participant in the form of Q-sort. Based on the above theory, the Q-sort form in this study (shown in Figures 2 and 3) contains 9 or 11 ranking values, rang from 5 or 4 for items that are, say, most agreement, through zero which means uncertain, to −4 or −5 for items that are deemed most disagreement. For instance, participants in G1 and G2 were asked question 1 in a one-to-one interview, and then we asked them to divide 30 statements (Q-set 1) into three parts (i.e. agreement, uncertain and disagreement). In the next step, they were asked to sort the cards in the form of nine columns of mandatory distribution shown in Figure 2. In addition, each bin in Figure 2 must and can only be filled with a card (i.e. statement). Participants can rank statements in order of personal salience and take as much time as they entailed until all cards were placed in the Q-sort form and they were pleased with sorting result. Similar to the above methods, the G3 and G4 groups were tested in the same way. In a test, an interview takes about 25 to 45 mins.
Figure 2.
Nine-column Q sort form for patients.
Figure 3.
Eleven-column Q sort form for parents.
Phase 4: Analysis
The data could be analyzed statistically using centroid method of factor extraction or principal components analysis (PCA) in PQMethod.27 Stephenson believes that the centroid method is used within a dependency factor-analytic framework, with factors rotated at will, which allows to seek explanation and search for meaning within the data.21 Mary M. Brown, however, concluded that there was little difference in which factor analysis was used based on the results of several studies.28 In this study, separate factor analyses were conducted for the four groups by using centroid factor extraction and varimax rotation in PQMethod 2.35.23 Factors were extracted using the following criteria: there were at least three or four defining sorts and the eigenvalues had to be greater than 1.23,25 In addition, factor analysis is carried out for G1, G2, G3 and G4, respectively. According to the analysis results, the corresponding people of each extraction factor in Q methodology are grouped and classified. These people have similar views, perspective or attitudes towards a particular topic.22 This classification can be considered as the motivation of treatment in the context represented by specific factors.
PQMethod can generate a composite Q-sort for each factor in the tables, which reflects the typical profile of participants who loaded on a particular factor. There were distinguishing statements with which a particular factor agreed or disagreed statistically more strongly than other factors. Distinguishing statements that were significant at P<0.05 are indicated with a single asterisk, and those at P<0.01 are indicated with a double asterisk. The factor arrays including the position of each statement and statements about the grounds for seeking orthodontic treatment can assist with interpretation.
Results
Through Q-type analysis of participants, we can find the factor whose eigenvalue is more than 1.0. The cumulative variance of these significant factors and the explanatory variance of the final extracted factors are shown in Tables 1 and 2. In the patients' groups, the average age of the G1 and G2 groups was 12.9 and 13.7 years, respectively, and the corresponding gender distribution (female-to-male ratio) was close to 1:3 and 3:1, respectively. In the parent groups, the ratio of female-to-male was 28:22 in G3 and that in G4 was 30:10. Based on this data result, three factors in the four queues were extracted by using the method of maximum rotation analysis of variables, respectively. Subsequently, according to the extracted factors, all participants can be divided into 12 categories. However, it is important to note that not all participants will map to one of the 12 important factors. Tables 3 and 4 show factor arrays, discriminatory statements of three important factors, and how participants evaluate each statement in G1, G2, G3 and G4.
Table 1.
Motivational Profile for Factors 1 to 3 in G1 (CLP Patients) and G2 (NON-CLP Patients)
| G1(N=36) | G2(N=35) | |||||
|---|---|---|---|---|---|---|
| F1(N=17) | F2(N=9) | F3(N=10) | F1(N=17) | F2(N=7) | F3(N=11) | |
| Explanation variance | 21% | 16% | 18% | 22% | 13% | 18% |
| Eigenvalues | 15.3 | 3.6 | 2.8 | 14.8 | 4.1 | 2.5 |
| Profile | 1. Aesthetics | 2. Preparation for other oral treatments | 3. Timely | 1. Admiration of others, aesthetics | 2. Oral function | 3. Oral hygiene and improvement of smile |
| Agreement | 1. Aesthetics | 1. Preparation for other oral treatments, Happier (S5,S24) | 1. Timely, preparation for other oral treatments (S14,S24) | 1. Admiration of others (S10) | 1. Oral function (S23,S25) | 1. Uneven teeth, oral hygiene(S22,S14) |
| 2. Improve appearance, interpersonal benefit (S11,S16,S9) | 2. Teeth problem, oral function (S15,S26,S23) | 2. Uneven teeth | 2. Improve appearance(S11,S16,S6) | 2. Preparation for other oral treatments | 2. Smile improvement | |
| Disagreement | 1. Just for cool or get more attention (S1,S19) | 1. Just for cool, parent’s will, get attention | 1. Mouth breathing | 1. Preparation for other oral treatment, Get attention | 1. Follow trend (S21,S3) | 1. Be teased, get attention, preparation for other oral treatments (S24,S28) |
| 2. Follow trend (S3,S21) | 2. Admire (S10) | 2. Oral function (S23) | 2. Follow trend, Parent’s will (S2,S21,S3) | 2. Be popular and get attention | 2. Parent’s will | |
Abbreviations: F, factor; N, number; S, statements.
Table 2.
Motivation Profile for Factor 1 to 3 in G3 (CLP Patients’ Parents) and G4 (NON-CLP patients’ Parents)
| G3(N=30) | G4(N=35) | |||||
|---|---|---|---|---|---|---|
| F1(N=13) | F2(N=8) | F3(N=9) | F1(N=11) | F2(N=13) | F3(N=11) | |
| Explanation variance | 22% | 16% | 16% | 14% | 15% | 14% |
| Eigenvalues | 16.9 | 2.5 | 2.1 | 12.5 | 3.7 | 2.8 |
| Profile | 1. Worrying about the future of children, parents’ responsibilities, children’s feelings | 2. Mental health, well-timed | 3. Parents’ responsibilities, ready for treatment | 1. Aesthetics, children’s will | 2. Future problems, well-timed | 3. Well-timed, parents’ responsibility, no need to worry about physical problems |
| Agreement | 1. Children’s feelings | 1.Mental health(S19,S16),timely | 1. Prepare for further treatment(S17) | 1. Children’s will | 1. Growth,well-timed | 1. Well-timed |
| 2. Parents’ responsibilities | 2. Benefits of good teeth.(S21) | 2. Parents’ responsibilities, Children’s confidence, aesthetic of profile (S2,S5,S15) | 2. Aesthetics of teeth and profile(S15,S16) | 2. Future problem(S20,S7) Aesthetics | 2. Parents’ responsibilities, confidence, Aesthetics of teeth (S32,S14) | |
| 3. Be happier, confident and prevent from tease (S4,S5,S6,S19,S23) | 3. Children’s will | 3. Future problems, benefits from good teeth(S21,S26) | ||||
| 4. Oral Function (S33) | 4. Parents’ responsibilities, Mental burn which child has(S19) | |||||
| Disagreement | 1. Self-experience of parents(S28,S11) | 1. Effect by others(S28,S24,S27) | 1. Self-experience of parents(S28) | 1. Self-experience of parents(S11,S28) | 1. Self-experience of parents(S28) | 1. Physical issues which are affected by oral issues.(such as TMJ problems, growth problem) |
| 2. Child’s motive or other’s suggestions(S22,S24,S27) | 2. Oral problem(S30,S36) | 2. Children’ s blame and mental health(S3,S16) | 2. Children’s will or other’s suggestions(S22,S24,S27) | 2. Have an effect on growth | 2. Gummy smile(S18) | |
| 3.teeth injury | ||||||
Abbreviations: F, factor; N, number; S, statements.
Table 3.
Q-Set 1 and Their Corresponding Rank Values for Three Factors G1 (CLP Patients) and G2 (NON-CLP Patients)
| No. | Statement | G1ʹ Factor | G2ʹ Factor | ||||
|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 1 | 2 | 3 | ||
| S1 | It’s cool to have braces. | −4 | −3 | −1* | −2 | −2* | −2 |
| S2 | I do not really want to get braces, but my parents ask for the treatment. | −1 | 0** | −2 | −2 | −1** | −2 |
| S3 | Many friends and classmates around me wear braces which is very trendy. | −3 | −2* | −4 | −2 | −3** | −2 |
| S4 | I do not like the way my teeth look. | 1 | −2** | 1 | 1 | 1 | 0 |
| S5 | Having braces can make me happier. | 0* | 3** | 0* | 0 | 0 | 2** |
| S6 | I want to look better when taking pictures. | 1 | −1** | 1 | 2** | −1** | 0** |
| S7 | I want to have braces. | −2* | −1* | 0** | −1 | −1 | −1 |
| S8 | I want to be more confident. | 2 | 2 | 2 | 2 | 3 | 1* |
| S9 | I want to be more popular. | 2** | −1** | 0** | 1 | −2** | 0 |
| S10 | I admire others with perfect teeth. | 0 | −2** | 1 | 4** | 0 | −1 |
| S11 | I want to look more handsome/beautiful. | 3* | −1** | 2* | 3** | −2** | 2** |
| S12 | Think my teeth get protrusion/cross bite. | 1* | 0 | 1 | 1 | 0** | 2 |
| S13 | To improve my smile. | 2 | 1* | 2 | 2 | 0** | 3 |
| S14 | To make my teeth more even. | 4 | 2* | 4 | 2 | 2 | 4** |
| S15 | Want to close the space between my teeth. | 2* | 3* | 0** | 1 | 2* | 1 |
| S16 | Want to improve my profile. | 3 | 2* | 2 | 3** | 1 | 1 |
| S17 | My friends suggested me to have braces. | −2 | 0** | −1 | −1 | −2 | −1 |
| S18 | Dentist recommended me to have braces. | 0 | 0 | 0 | 0 | 1** | −1 |
| S19 | Get more attention if I have braces. | −3* | −4** | −1** | −4 | −3 | −3 |
| S20 | Childhood is the best time to have braces. | 0 | 0 | 3** | 1 | 2 | 1 |
| S21 | My favorite idol has braces. | −2 | −3* | −3 | −3** | −4** | −1** |
| S22 | It is not easy to clean my teeth. | 1 | 1 | 1 | 0* | 1* | 3** |
| S23 | Chew food difficultly. | 1 | 1 | −2** | 0 | 4** | 0 |
| S24 | Prepare for surgery (alveolar boon graft, orthognathic, etc.). | −1** | 4** | 3** | −3 | 3** | −3 |
| S25 | Front teeth cannot bite well. | −1 | 1** | −1 | −1** | 2 | 2 |
| S26 | Splash saliva when talking. | −1 | 2** | −2 | −1** | 0** | −2** |
| S27 | Sleep with mouth open. | −1** | 1** | −3** | −1** | 0 | 0 |
| S28 | I was teased because of teeth problems. | 0** | −2 | −2 | 0 | −1 | −4** |
| S29 | I want to solve dental problems before going abroad. | −2** | 0 | 0 | −2** | 1 | 1 |
| S30 | Gums uncover/Not enough teeth to show while laughing. | 0 | −1 | −1 | 0 | −1 | 0* |
Notes: Bold type indicates distinguishing statements. Distinguishing statements that were significant at P<0.05 are indicated with a single asterisk, and those at P<0.01 are indicated with a double asterisk.
Abbreviation: S, statements.
Table 4.
Q-Set 2 and Their Corresponding Rank Values for Three Factors G3 (CLP Patients’ Parents) and G4 (NON-CLP patients’ Parents)
| No. | Statement | G3ʹ Factor | G4ʹ Factor | ||||
|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 1 | 2 | 3 | ||
| S1 | I hope my child gets better teeth than me. | −2 | −2 | −1 | 1* | −2** | 0* |
| S2 | It’s my responsibility to take care of my child. | 4 | 1** | 4 | 2 | 1* | 4** |
| S3 | Prevent me from being blamed by my child in the future. | 0 | −1 | −4** | −1* | −2 | −3 |
| S4 | My child is unhappy with uneven teeth. | 2** | −1 | −3 | −1** | −2 | −2 |
| S5 | Want to make my child more confident. | 5 | 1** | 4 | 2 | 2 | 4** |
| S6 | To make my child laugh more. | 3** | 0** | 1** | 0 | 0 | 1 |
| S7 | Do not want my child to be bothered by teeth in the future. | 4 | 3 | 0** | 3 | 3 | 3 |
| S8 | Uneven midline of my child’s front teeth. | 0 | 0 | −2** | −2 | −1 | −3 |
| S9 | My child wants braces. | −2 | 3** | −1 | 5** | −3** | 0** |
| S10 | (Having braces is an essential stage in adolescence.) Having braces is part of growing up. | 0 | 1** | 0 | 0 | 0 | 1 |
| S11 | I had braces myself as well. | −4* | −2* | −5* | −5 | −5 | −2** |
| S12 | I think children should have braces. | 0** | 2 | 2 | 0 | −1 | 2** |
| S13 | Solve tooth problems before my child goes abroad. | −4 | −3 | −4 | −4 | −4 | 0** |
| S14 | Make my child’s teeth perfect. (enhance the beauty of teeth) | 1 | 1 | 2 | 4 | 2** | 3 |
| S15 | Improve the child’s facial appearance. | 2 | 2 | 3 | 4 | 3 | 2 |
| S16 | My child pays too much attention to his/her teeth. (Excessive self-concern my child gets from dental problems) | 1** | 4** | −3** | 1 | −1** | 1 |
| S17 | Preparation for dental restoration in adulthood. | −2** | 2 | 3 | −1** | 1 | 2 |
| S18 | Gummy smile. | −1 | −1 | −2 | −2 | −1** | −3 |
| S19 | (Reduce the mental burden of my child due to teeth.) My child has psychological burden due to teeth problem. | 3 | 5 | 1** | 3** | 2** | 0** |
| S20 | Irregular teeth may affect child’s job search. | 1 | 2 | 1 | 1 | 3** | 1 |
| S21 | I think my child will be more likely to socialize with even teeth. | 1 | 3** | 1 | 3** | 1 | 1 |
| S22 | Recommended to have braces by other dentists. | −3** | −1 | 0 | −2 | 0 | −1 |
| S23 | Prevent my child from teasing due to irregular teeth | 3** | 0 | 0 | 0 | 1 | −2** |
| S24 | My friends’ children have braces. | −3 | −3 | −1** | −3 | −3 | 0** |
| S25 | It’s the best time to have braces. | 2* | 4* | 5** | 2** | 4** | 5** |
| S26 | I think good teeth symbolizes high social status nowadays. | −1 | −2 | −1** | 2** | −3** | 0** |
| S27 | I watched popular science writing about braces. | −3 | −4 | −1* | −2 | −2 | −2 |
| S28 | I realized the value of teeth when I go abroad. | −5 | −5 | −2** | −3 | −4 | −1** |
| S29 | It’s difficult to decay with even teeth. | −1* | 0 | 0 | 1 | 0 | −1** |
| S30 | Braces will help with temporomandibular joint problems. (e.g. jaw) | −1 | −4 | −2 | −3** | −1** | −5** |
| S31 | I am worried about injury to the front teeth. | −1 | 0 | −3** | −1 | 0** | −1 |
| S32 | Want my child to have more even teeth. | 1 | 1 | 2 | 1* | 4 | 3 |
| S33 | Braces will improve my child’s ability to chew and digest. | 2 | −1** | 3 | −1 | 2** | −1 |
| S34 | Facilitates child to clean teeth more easily. | 0* | 0 | −1 | 0 | 1 | 2 |
| S35 | Crossbite/Upper teeth protrusion may affect growth of my child. | 0** | −2** | 2** | −4 | 5** | −4 |
| S36 | Sleep with mouth open. | −2 | −3 | 0 ** | 0 | 0 | −4** |
Notes: Bold type indicates distinguishing statements. Distinguishing statements that were significant at P<0.05 are indicated with a single asterisk, and those at P<0.01 are indicated with a double asterisk.
Abbreviation: S, statements.
Patient Profile (i.e., G1 & G2)
All G1 patients had an alveolar cleft. Thirty-six CLP patients in G1 group had similar views because they sought orthodontic treatment, which was related to one of the three factors. Four CLP patients’ dispersed views could not be loaded into any of the three factors. Among G2 patients, thirty-five NON-CLP patients were identified as one of the three important factors, while the remaining five non-CLP patients were not of any type. Table 1 shows six significant factors of G1 and G2, which are described as G1: (1) aesthetic, (2) prepare for other oral treatments, (3) timely; G2: (1) admire others, aesthetics (2) oral function, (3) oral hygiene and improvement of smile.
Parent Profile (i.e., G3 & G4)
In G3, thirty CLP patients' parents loaded on the three factors while ten participants failed to be categorized as any of them. In G4, thirty-five NON-CLP patients' parents mapped to 1 of 3 significant factors. Table 2 illustrates the six significant factors of G3 and G4, entitled as G3: (1) worrying about the future of child, parents’ responsibilities, children’s feelings; (2) mental health, timely; (3) timely, parents’ responsibilities, ready for treatment. G4: (1) aesthetics, children’s will; (2) future problems, timely; (3) timely, parents’ responsibilities and no need to worry about physical problems.
Comparison of Profiles Between CLP and NON-CLP Groups
For CLP patients (i.e., G1) profile 1 (aesthetics) and NON-CLP patients (i.e.G2) profile 1 (admire of others, aesthetics), aesthetic needs are their main motivation for orthodontic treatment. The improvement of image is the most important problem they consider, and the beauty of appearance in general aesthetics is their most concerned object (S11 and S16). For G1 profile 1, the most satisfactory reason for seeking orthodontic treatment is S14 (they want more even teeth). However, the orthodontic motivation of the G2 patients is due to envy others’ perfect teeth.
For the G1 and G2 groups, it seems that both groups need a pre-orthodontic treatment before undergoing other oral treatments, such as alveolar bone transplantation, dental restoration, orthodontics, etc. G1 profile 2 (ready for other oral treatment) also drives orthodontic treatment because of the desire for personal happiness and closure of dental spaces. While G2 profile 2 (oral function) took chewing problem as the most important reason.
For G1 and G2 profile 3, these patients were motivated by uneven teeth. Additionally, G1 patients in profile 3 thought it is a best time to have orthodontic treatment or prepare for other oral treatment. NON-CLP patients in profile 3 did not suffer from teasing or think tease as a problem, they needed not take orthodontic treatment as a pavement for something either. These patients concerned oral hygiene of their uneven teeth and wanted to have better smiles as well.
CLP patients' parents (i.e., G3) profile 1 (worrying about the future of children, parents’ responsibilities, children’s feelings), these parents have a strong sense of responsibility to take care of their children’s future oral health problems. They hope to increase children’s confidence through orthodontics, so as to avoid dental problems in the future. For parents of NON-CLP (i.e., G4) profile 1 (aesthetics, children’s will), the main driving force is the influence of children’s aesthetics. The child in this profile also desired for treatment.
In G3 profile 2 (mental health, timely), these parents concerned about child’s mental health which may affect by poor teeth. They thought in their children’s age is the best time to undertake orthodontic treatment. This desire “at a right age to do right things” was comparable with G4 profile 2 (future problems, timely) parents. Furthermore, for G4 profile2 parents also concerned about poor teeth may influence the growth.
For both G3 profile 3 (parents’ responsibilities, ready for treatment) and G4 profile 3 (timely, parents’ responsibility, no need to worry about physical problems) parents, they felt a responsibility to pursue treatment and valued the appropriate treatment time to child. However, G3 profile 3 parents did not consider their own oral treatment experience. Additionally, in G4 profile 3 parents, their children had no physical issues which affect by oral issues to worry about.
Discussion
Parents reported greater motivation for their children to have orthodontic treatment than did the children.29 It is easier to obtain cooperation if there are consensus between parents’ and patients’ motives of seeking orthodontic treatment. As we all have known, a better insight into motivation could notify the design of interventions of activity participation in children and influence their adherence.30,31 Blake et al9 deemed that clinicians will improve communication and have better strategies of the treatment plan if they had a better understanding of what influences patients' decision-making. It is vital to have extra information stemmed from patients-based measure rather than depend solely on normative measures of need.32 Thus, in this article, we tried to figure out a part of this underrepresented domain by using Q methodology which was shown as an appropriate technique in the subjective study.9,11
In this study, the causes of orthodontic treatment in four groups (G1, G2, G3, G4) were compared and analyzed. The analysis results show that each participant’s views show rich details, through which we can see that personal experience, vision and social background will have a certain impact on the generation of views. Finally, we identified and categorized three motivational characteristics in each group, in which participants sharing similar motives to seek orthodontic treatment in each profile. These categories demonstrated that differences and similarities coexist between CLP and NON-CLP participants.
Compare G1 (i.e., CLP Patient) with G2 (i.e., NON-CLP patient)
CLP patient profile 1 and NON-CLP patient profile 1 included aesthetics as central motivation. It is consistent with previous findings that aesthetics is preeminent in patients’ motives for treatment.33–36 After all, as we all have known that individuals could benefit from overall esthetic reasons. Acceptable in their social surroundings was exposed to motives by patients regarding treatment.37 However, not all six profiles in these two patient groups have taken aesthetics as the most important motives for treatment. For CLP patients, they may likely be more focus on their nose and lip, especially since these factors may convey important social cues.38 CLP patients in profile 2 and profile 3 took orthodontic treatment as a preparation for other oral treatment (e.g. alveolar bone graft, orthognathic, etc.). In this case, orthodontic treatment becomes the part of the lengthy multidisciplinary treatment. Moreover, CLP patients wanted to be happier by having braces in profile 2. According to the study conducted by Wehby et al that individuals with CLP were unhappy on account of their facial appearance.39 Interestingly, in profile 2, NON-CLP patients would have other oral treatment after orthodontic treatment as well. Additionally, this type of NON-CLP patients suffered with chewing problem, which proved a reasonable explanation that there would be other oral treatment (e.g. tooth restoration) after orthodontic treatment, and a study was revealed that perception of poor chewing function of adolescents is the main desire to undergo treatment, Feldens et al.35 CLP patients in profile 1 and 3, NON-CLP patients in profile 3 had a demand to even teeth. Furthermore, CLP patients in profile 3 had the awareness of the treatment time. They suffered prolonged management of multidisciplinary treatment generally since they were infancy, those experiences may provide more information about oral health care than their normal peers. In addition to the motivation of profile 3 in G2, these NON-CLP patients desire to improve their smile. This finding accords with the study conducted by Christopherson et al that patient desire for braces was significantly correlated with their perception of smile.40 Persons with ideal smiles are considered more intelligent and have a greater chance of finding a job.41
In the present study, patients are generally reluctant to receive additional attention due to orthodontic treatment (S19). Additionally, dentists’ orthodontic treatment advice is only to seek the neutral motivation for the treatment of G1 and G2. The difference between these results and previous studies is that general dentists can influence patients’ treatment intention to some extent. In the United States, more than half of children choose to receive treatment recommendations.40,42 Therefore, it can be preliminarily concluded that people in developing countries are more likely than those in developed countries to lack access to oral health-care services, resulting in a lack of awareness of oral health examination and counseling.
From the results of this study, it can be clearly seen that CLP and NON-CLP patients have similar narratives with global themes in aesthetics, oral function, self-perception and other aspects of treatment preparation. Nevertheless, compared with NON-CLP patients, CLP patients pay more attention to the improvement of interpersonal relationship and life emotion after treatment, while NON-CLP patients pay more attention to the improvement of external expression, such as smile. Previous studies have also shown that CLP patients generally have higher satisfaction with life and there is no significant difference in anxiety between CLP patients and NON-CLP patients.43,44 However, other studies have also exposed problems in race, research design and investigation methods, and there are conflicting differences in the attributes of evidence.45,46
These findings suggest that the initiative shown by the patient at the initial appointment should be brought to the attention of the clinician, which was in accordance with previous studies. After all, children will adopt performance goals if the task is meaningful.47 It is not difficult to find that the understanding of treatment motivation may improve communication among dental professionals, patients and their parents. In summary, CLP patients pay more attention to the benefits of Orthodontics in interpersonal relationships. They hope to get a happy life through treatment. For NON-CLP patients, the focus of this group is on the improvement of the effect of smiling. Nonetheless, they shared three global themes: aesthetic purposes, timely preparation for other treatments in the patient group.
Compare G3 (i.e., CLP Patient’s Parent) with G4 (i.e., NON-CLP Patient’s parent)
Parents of CLP patients in profile 1 and 3, parents of NON-CLP patients in profile 3 considered parental responsibility as the vital motive. Previous study demonstrated that parents felt guilty to their CLP child.48 CLP patients’ parents are more likely to exert parental duty to do the best for their kids in order to reduce the guilty. In addition, aesthetics and “it’s the good time to have braces” were deemed as significant motivating factors in both G3 and G4, which has been echoed by other researches.11,29 In this study, there were more female parents in both G3 and G4 than male parents. It may consider that mothers tend to be more involved in child care, and mothers more frequently realize the need for orthodontic treatment.49,50
However, psychosocial issues are of concern to CLP patients’ parents in profile 2. This was reflected by our analysis significantly which was shown the higher grade of “Agreement” in Table 4 such as “Reduce the mental burden of my child due to teeth” (S19), “My child pays too much attention to his/her teeth” (S16). It may be considered that CLP patients had speech intelligibility disorders, psychosocial issues, facial and dental anomalies, and so on,2,51 and orthodontic treatment would offer social and psychological benefit to patients.52 Parents of NON-CLP patients in profile 1 and profile 2 use their children’s willingness and worries about future problems as motivations for seeking treatment. The statements with significantly higher grade of “Agreement” are shown in Table 4 such as “My child wants braces” (S9), “Irregular teeth may affect child’s job search” (S20), “Crossbite/Upper teeth protrusion may affect growth of my child” (S35). This theme was consistent with the finding in the study of Davis et al.9
Unlikely reported in other countries, almost all of the parents in present study have given up self-experience (S11 and S28) as the desire for treatment.9,11 It may be a reasonable explanation that developing countries as China do not have the resources and conditions to provide dental braces to their parents. Interestingly, worrying about tooth injury also does not have to be taken into account as the important motive by all of the parents. A study showed that the incidence of tooth trauma was reduced by about 11% compared with those who did not receive early orthodontic treatment.53 Parents in this study may seem to be limited by their dental knowledge.54,55 In addition, patients with CLP usually engage in cross-biting and are less likely to be injured than protrusions.
In this research, three profiles of parents in G3 regarded psychosocial concerns as the motivations for their children seeking orthodontic treatment, while parents in G4 referred to the will of the child and concerned about the future of children. Yet, they shared 3 global motives as parental responsibility, well-timed, aesthetic purposes.
Our study was the first research which applies Q methodology to compare CLP and NON-CLP patients and their patients’ motives for undertaking orthodontic treatment. Suffice to say that Q methodology is to comprehend the nature of the shared viewpoints participants have exposed and to a quite advanced qualitative detail. This method has been shown to be sufficiently valid for research23 and investigate in more detail of insights and subjective orthodontic treatment desire. However, the limitation of present research should not be ignored. NON-CLP patients almost from shanghai which may have a better background compared with CLP patients, which could result in selection bias in this study. Moreover, parents and patients were recruited, respectively, with less evidence finding the association. In further research, we tend to cooperate with other hospitals in order to cover participants from different regions.
Conclusion
In this paper, two groups of CLP patients and NON-CLP patients and their respective parents were tested by Q methodology. Through testing, this study explored the motivation of the above population for orthodontic treatment. The results show that the motivation is complex and can be divided into three categories. CLP and NON-CLP patients and parents have different orthodontic treatment motives, yet, they still shared 3 global motivation themes, respectively. The commonness between CLP groups and NON-CLP groups is greater than the difference.
Our findings can establish a good communication mechanism among patients, parents and orthodontists. In addition, Q methodology is an appropriate method to enable us to understand the important factors of subjective topics.
Acknowledgments
Thanks to Simon Watts and Paul Stenner who declaimed that the writing of <Introducing Q methodology: The Inverted Factor Technique> will do little to fawn on their employers or increase their standing and career status, yet still wrote the book, hence inspires and provides an opportunity to the new learners of Q method, like me, having a better way to undertake Q methodology study.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Fan D, Wu S, Liu L, et al. Prevalence of non-syndromic orofacial clefts: based on 15,094,978 Chinese perinatal infants. Oncotarget. 2018;9(17):13981–13990. doi: 10.18632/oncotarget.v9i17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Watkins SE, Meyer RE, Strauss RP, Aylsworth AS Classification, epidemiology, and genetics of orofacial clefts. Clin Plast Surg. 2014;41(2):149–163. doi: 10.1016/j.cps.2013.12.003 [DOI] [PubMed] [Google Scholar]
- 3.Chen ZQ, Qian YF, Wang GM, et al. Sagittal maxillary growth in patients with unoperated isolated cleft palate. Cleft Palate Craniofac J. 2009;46(6):664. doi: 10.1597/08-116.1 [DOI] [PubMed] [Google Scholar]
- 4.Špalj S, Katić V, Vidaković R, et al. History of orthodontic treatment, treatment needs and influencing factors in adolescents in Croatia. Cent Eur J Public Health. 2016;24(2):123–127. doi: 10.21101/cejph.a4117 [DOI] [PubMed] [Google Scholar]
- 5.Skidmore K, Brook K, Thomson W, Harding W Factors influencing treatment time in orthodontic patients. Am J Orthod Dentofacial Orthop. 2006;129(2):230–238. doi: 10.1016/j.ajodo.2005.10.003 [DOI] [PubMed] [Google Scholar]
- 6.Dimitrios M, Athanasiou AE Factors affecting the duration of orthodontic treatment: a systematic review. Eur J Orthod. 2008;30(4):386–395. doi: 10.1093/ejo/cjn018 [DOI] [PubMed] [Google Scholar]
- 7.Brattstr MV, Ingelsson M, Aberg E Treatment co-operation in orthodontic patients. Br J Orthod. 1991;18(1):37–42. doi: 10.1179/bjo.18.1.37 [DOI] [PubMed] [Google Scholar]
- 8.Marshman Z, Eddaiki A, Bekker HL, et al. Development and evaluation of a patient decision aid for young people and parents considering fixed orthodontic appliances. Br J Orthod. 2016;43(4):276–287. doi: 10.1080/14653125.2016.1241943 [DOI] [PubMed] [Google Scholar]
- 9.Davis BB, Bayirli B, Ramsay DS, et al. “Why do you want your child to have braces?” Investigati.ng the motivations of Hispanic/Latino and white parents. Am J Orthod Dentofacial Orthop. 2015;148(5):771–781 doi: 10.1016/j.ajodo.2015.05.023 [DOI] [PubMed] [Google Scholar]
- 10.Barbara WS, Maria S Patient and parent motivation for orthodontic treatment–a questionnaire study. Eur J Orthod. 2010;32(4):447–452. [DOI] [PubMed] [Google Scholar]
- 11.Prabakaran R, Seymour S, Moles DR, et al. Motivation for orthodontic treatment investigated with Q-methodology: patients’ and parents’ perspectives. Am J Orthod Dentofacial Orthop. 2012;142(2):213–220. doi: 10.1016/j.ajodo.2012.03.026 [DOI] [PubMed] [Google Scholar]
- 12.Obradović J, van Dulmen MH, Yates TM, et al. Developmental assessment of competence from early childhood to middle adolescence. J Adolesc. 2006;29(6):857–889. doi: 10.1016/j.adolescence.2006.04.009 [DOI] [PubMed] [Google Scholar]
- 13.Costa ACD, Rodrigues FS, Fonte PPD, et al. Influence of sense of coherence on adolescents’ self-perceived dental aesthetics; a cross-sectional study. BMC Oral Health. 2017;17(1):117. doi: 10.1186/s12903-017-0405-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ferrando-Magraner E, García-Sanz V, Bellot-Arcís C, et al. Oral health-related quality of life of adolescents after orthodontic treatment. A systematic review. J Clin Exp Dent. 2019;11(2):e194–e202. doi: 10.4317/jced.55527 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Thiruvenkadam G, Asokan S, John JB, et al. Oral health-related quality of life of children seeking orthodontic treatment based on child oral health impact profile: a cross-sectional study. Contemp Clin Dent. 2015;6(3):396–400. doi: 10.4103/0976-237X.161899 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dos Santos PR, Meneghim MC, Ambrosano GM, et al. Influence of quality of life, self-perception, and self-esteem on orthodontic treatment need. Am J Orthod Dentofacial Orthop. 2017;151(1):143–147. doi: 10.1016/j.ajodo.2016.06.028 [DOI] [PubMed] [Google Scholar]
- 17.Cioffi I, Michelotti A, Perrotta S, et al. Effect of somatosensory amplification and trait anxiety on experimentally induced orthodontic pain. Eur J Oral Sci. 2016;124(2):127–134. doi: 10.1111/eos.12258 [DOI] [PubMed] [Google Scholar]
- 18.Cristiano M, Alessandro Leite C, Estela Santos GO, et al. Negative self-perception of smile associated with malocclusions among Brazilian adolescents. Eur J Orthod. 2013;35(4):483–490. doi: 10.1093/ejo/cjs022 [DOI] [PubMed] [Google Scholar]
- 19.Tang X, Cai J, Lin B, et al. Motivation of adult female patients seeking orthodontic treatment: an application of Q-methodology. Patient Prefer Adherence. 2015;9(9):249–256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Watts DS, Stenner DP Doing Q methodology: theory, method and interpretation. Qual Res Psychol. 2005;2(1):67–91. doi: 10.1191/1478088705qp022oa [DOI] [Google Scholar]
- 21.Stephenson BW The study of behavior: Q-technique and its methodology. Philos Sci. 1953;22(1):67. [Google Scholar]
- 22.Watts S, Stenner P Q methodology: the inverted factor technique. Ir J Psychol. 2007; 28 (1–2): 63–76. doi: 10.1080/03033910.2007.10446249 [DOI] [Google Scholar]
- 23.Simon W Develop a Q methodological study. Educ Prim Care. 2015;26(6):435–437. doi: 10.1080/14739879.2015.1101855 [DOI] [PubMed] [Google Scholar]
- 24.Xi-ying Y, Yun-lin C Exploration and Analysis of the Q methodology. J Dialectics Nat. 2010;32(5):15–20. [Google Scholar]
- 25.Brown SR Political subjectivity: applications of Q methodology in political science. J Polit. 1980;43(3):217–219. [Google Scholar]
- 26.Shinebourne P Using Q method in qualitative research. Int J Qual Meth. 2009;8(1):93–97. doi: 10.1177/160940690900800109 [DOI] [Google Scholar]
- 27.Schmolck P. PQMethod (version 2.35). 2014. Availabe from: http://schmolck.org/qmethod/index.htm. Accessed November28, 2019.
- 28.Brown M Illuminating Patterns of Perception: an Overview of Q Methodology. 2004:32. [Google Scholar]
- 29.Daniels AS, Seacat JD, Inglehart MR Orthodontic treatment motivation and cooperation: a cross-sectional analysis of adolescent patients’ and parents’ responses. Am J Orthod Dentofacial Orthop. 2009;136(6):780–787. doi: 10.1016/j.ajodo.2007.11.031 [DOI] [PubMed] [Google Scholar]
- 30.Standage M, Duda JL, Ntoumanis N A model of contextual motivation in physical education: using constructs from self-determination and achievement goal theories to predict physical activity intentions. J Educ Psychol. 2003;95(95):97–110. doi: 10.1037/0022-0663.95.1.97 [DOI] [Google Scholar]
- 31.Pannekoek L, Piek JP, Hagger MS Motivation for physical activity in children: a moving matter in need for study. Hum Movement Sci. 2013;32(5):1097–1115. doi: 10.1016/j.humov.2013.08.004 [DOI] [PubMed] [Google Scholar]
- 32.Hamdan AM The relationship between patient, parent and clinician perceived need and normative orthodontic treatment need. Eur J Orthod. 2004;26(3):265–271. doi: 10.1093/ejo/26.3.265 [DOI] [PubMed] [Google Scholar]
- 33.Perillo L, Esposito M, Caprioglio A, et al. Orthodontic treatment need for adolescents in the Campania region: the malocclusion impact on self-concept. Patient Prefer Adherence. 2014;8:353–359. doi: 10.2147/PPA.S58971 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Miguel JAM, Sales HX, Quint OCC, et al. Factors associated with orthodontic treatment seeking by 12-15-year-old children at a state university-funded clinic. Br J Orthod. 2010;37(2):100–106. doi: 10.1179/14653121042957 [DOI] [PubMed] [Google Scholar]
- 35.Feldens CA, Nakamura EK, Tessarollo FR, et al. Desire for orthodontic treatment and associated factors among adolescents in southern Brazil. Angle Orthod. 2015;85(2):224–232. doi: 10.2319/021014-105.1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Stock NM, Zucchelli F, Hudson N, et al. Promoting psychosocial adjustment in individuals born with cleft lip and/or palate and their families: current clinical practice in the United Kingdom. Cleft Palate Craniofac J. 2019:1055665619868331. [DOI] [PubMed] [Google Scholar]
- 37.Pabari S, Moles DR, Cunningham SJ Assessment of motivation and psychological characteristics of adult orthodontic patients. Am J Orthod Dentofacial Orthop. 2011;140(6):e263–e272. doi: 10.1016/j.ajodo.2011.06.022 [DOI] [PubMed] [Google Scholar]
- 38.Gkantidis N, Papamanou DA, Christou P, et al. Aesthetic outcome of cleft lip and palate treatment. Perceptions of patients, families, and health professionals compared to the general public. J Cranio Maxill Surg. 2013;41(7):e105–e110. doi: 10.1016/j.jcms.2012.11.034 [DOI] [PubMed] [Google Scholar]
- 39.Wehby GL, Cassell CH The impact of orofacial clefts on quality of life and healthcare use and costs. Oral Dis. 2010;16(1):3–10. doi: 10.1111/j.1601-0825.2009.01588.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Christopherson EA, Dan B, Inglehart MR Preadolescent orthodontic treatment need: objective and subjective provider assessments and patient self-reports. Am J Orthod Dentofacial Orthop. 2009;135(4):S80–S86. [DOI] [PubMed] [Google Scholar]
- 41.Pithon MM, Nascimento CC, Barbosa GCG, et al. Do dental esthetics have any influence on finding a job? Am J Othord Dentofacial Orthop. 2014;146(4):423–429. doi: 10.1016/j.ajodo.2014.07.001 [DOI] [PubMed] [Google Scholar]
- 42.Gosney MB An investigation into some of the factors influencing the desire for orthodontic treatment. Br J Orthod. 1986;13(2):87–94. doi: 10.1179/bjo.13.2.87 [DOI] [PubMed] [Google Scholar]
- 43.Lansdown R, Polak L A study of the psychological effects of facial deformity in children. Child Care Health Dev. 2010;1(2):85–91. doi: 10.1111/j.1365-2214.1975.tb00001.x [DOI] [PubMed] [Google Scholar]
- 44.Cheung LK, Loh JS, Ho SM Psychological profile of Chinese with cleft lip and palate deformities. Cleft Palate Craniofac J. 2007;44(1):79–86. doi: 10.1597/05-053 [DOI] [PubMed] [Google Scholar]
- 45.Tumer SR, Rumsey N, Sandy JR Psychological aspects of cleft lip and palate. Eur J Orthod. 1998;20(4):407–415. doi: 10.1093/ejo/20.4.407 [DOI] [PubMed] [Google Scholar]
- 46.Hunt O, Burden D, Hepper P, et al. The psychosocial effects of cleft lip and palate: a systematic review. Eur J Orthod. 2005;27(3):274–285. doi: 10.1093/ejo/cji004 [DOI] [PubMed] [Google Scholar]
- 47.Smiley PA, Dweck CS Individual differences in achievement goals among young children. Child Dev. 2010;65(6):1723–1743. doi: 10.2307/1131290 [DOI] [PubMed] [Google Scholar]
- 48.Dölger-Häfner M, Bartsch A, Trimbach G, et al. Parental reactions following the birth of a cleft child. J Orofac Orthop. 1997;58(2):124–133. [PubMed] [Google Scholar]
- 49.Landgfuf JM, Abetz LN Functional status and well-being of children representing three cultural groups: initial self-reports using the chq-cf87. Psychol Health. 1997;12(6):839–854. doi: 10.1080/08870449708406744 [DOI] [Google Scholar]
- 50.Winnier JJ, Nayak UA, Rupesh S, et al. The relationship of two orthodontic indices, with perceptions of aesthetics, function, speech and orthodontic treatment need. Oral Health Prev Dent. 2011;9(2):115–122. [PubMed] [Google Scholar]
- 51.Othman SA, Koay NAA Three-dimensional facial analysis of Chinese children with repaired unilateral cleft lip and palate. Sci Rep. 2016;(6):31335. doi: 10.1038/srep31335 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Henson ST, Lindauer SJ, Graham GW, et al. Influence of dental esthetics on social perceptions of adolescents judged by peers. Am J Orthod Dentofacial Orthop. 2011;140(3): 389–395. doi: 10.1016/j.ajodo.2010.07.026 [DOI] [PubMed] [Google Scholar]
- 53.Batista K, Thiruvenkatachari B, Harrison JE, et al. Orthodontic treatment for prominent upper front teeth (Class II malocclusion) in children and adolescents. Cochrane Db Syst Rev. 2018;3(3):CD003452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Quaranta A, De GO, Coretti C, et al. What do parents know about dental trauma among school-age children? A pilot study. Ann Ig. 2014;26(2):144–147. [DOI] [PubMed] [Google Scholar]
- 55.Maria Letícia RJ, Joana RJ, Isabella MV, et al. Parents’ recognition of dental trauma in their children. Dent Traumatol. 2013;29(4):266–271. doi: 10.1111/edt.12005 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Citations
- Schmolck P. PQMethod (version 2.35). 2014. Availabe from: http://schmolck.org/qmethod/index.htm. Accessed November28, 2019.