Abstract
Objective
The objective of this study was to explore medical oncology outpatients' perceived experiences of errors in their cancer care.
Methods
A cross-sectional survey was conducted. English-speaking medical oncology outpatients aged 18 years or older were recruited from 9 Australian cancer treatment centers. Participants completed 2 paper-and-pencil questionnaires: an initial survey on demographic, disease and treatment characteristics upon recruitment; and a second survey on their experiences of errors in cancer care 1 month later.
Results
A total of 1818 patients (80%) consented to participate, and of these, 1136 (62%) completed both surveys. One hundred forty-eight participants (13%) perceived that an error had been made in their care, of which one third (n = 46) reported that the error was associated with severe harm. Of those who perceived an error had been made, less than half reported that they had received an explanation for the error (n = 65, 45%) and only one third reported receiving an apology (n = 50, 35%) or being told that steps had been taken to prevent the error from reoccurring (n = 52, 36%). Patients with university or vocational level education (odds ratio [OR] = 1.6 [1.09–2.45], P = 0.0174) and those who received radiotherapy (OR = 1.72 [1.16–2.57]; P = 0.0076) or “other” treatments (OR = 3.23 [1.08–9.63]; P = 0.0356) were significantly more likely to report an error in care.
Conclusions
There is significant scope to improve communication with patients and appropriate responses by the healthcare system after a perceived error in cancer care.
Key Words: patient safety, quality of health care, medical errors, cancer, oncology
From the time of Hippocrates, one of the basic ethical principles underlying health care practice has been to “never do harm.”1 However, medical errors do happen, with the impact on patients ranging from nil to severe.2 It is estimated that the annual cost of medical errors that harm patients in the United States is US $17.1 billion, with 10 types of errors accounting for 69% of this cost.3
The prevalence of errors in cancer care varies according to the population studied4,5 and has been reported in relation to diagnosis,5 labeling of surgical specimens,6 and medication administration.7 Harm resulting from such errors has led to the interest in understanding why errors occur, how professionals and organizations can reduce the chances of errors happening, and mitigating the effect of such incidents when they do occur.8
An appropriate response to an error in care includes the following: (1) an explanation of what occurred, (2) an apology, and (3) a commitment to prevent a recurrence of the error in the future.9,10 Patients confirm that these 3 steps are both desired and expected.11 Although doctors also support disclosure of errors, there is some evidence that this does not always occur.11,12 For example, among a sample of physicians from the United States, 19% reported that they had made a minor error and 4% a major error, which they had not disclosed to the patient.13
Nondisclosure of errors by clinicians may be due to concerns regarding potential litigation, damage to reputation, or the impact the disclosure may have on their relationship with the patient.10,12 However, Mazor et al14 suggest that good communication of medical errors, including explanation and an apology, may actually reduce the chance of litigation and improve patient satisfaction.
Given the negative outcomes that may result from errors, it is important to understand the patient experience of such errors. Despite this, few studies have examined the patient perspective on errors in cancer care. A Swiss study examined perceived errors in chemotherapy treatment among 479 patients recruited from a single hospital.15 The results suggest that 16% perceived that an error had occurred and 11% were very concerned about errors. Our study of 166 Australian patients with hematological cancer found that 26% perceived that an adverse event had occurred in their care.16 A study conducted in the United States explored the experiences of patients with breast and gastrointestinal cancer.17 Only one third of the patients who reported experiencing a problematic event in their cancer care discussed it with a person they perceived was responsible, and only 6% perceived that they received a clear explanation for the event.17 Half of the respondents reported that the clinicians had undertaken helpful actions after the event, but only 13% of the patients formally reported the event. Although these data provide a useful insight into cancer patients' experiences of errors in care, there is a need to explore these issues among a broader sample of patients with cancer.
The current study aimed to explore, among a sample of cancer outpatients, perceptions regarding the following: (1) whether health care providers should inform patients when an error is made and (2) whether an error had been made during their care. For patients who believed an error had been made, the study also assessed patient perceptions of the following: (3) the level of harm associated with the error; (4) how the health care organization responded to the error; (5) who the error was attributable to; and (6) the demographic, disease, and treatment characteristics associated with perceiving that an error had been made.
METHODS
Setting and Design
This research was conducted as part of a large multisite study examining patient psychosocial outcomes in 9 medical oncology treatment centers in Australia. Only the results pertaining to perceived errors in care are reported here. Approval was obtained from the human research ethics committees of the University of Newcastle (H-2010-1324), Cancer Institute New South Wales (2011/10/351), and each participating hospital.
Patient Eligibility Criteria
Patients with a confirmed diagnosis of cancer who were presenting for a medical oncology outpatient appointment, aged 18 years or older, able to read and understand English, and judged by clinic staff to be capable of providing informed consent and completing the questionnaire independently were eligible to participate. Patients who were attending the clinic for the first time were excluded.
Recruitment and Data Collection
A consecutive sample of eligible patients was recruited from each medical oncology clinic. Eligible patients were invited to participate in the study by a research assistant while waiting for their outpatient appointment. Written informed consent was obtained for all participants. The age and sex of nonconsenting patients were collected to assess participation bias. Consenting patients were asked to complete a paper-and-pencil survey including demographic, disease and treatment characteristics, and measures of anxiety, depression, and unmet supportive care needs. The participants were given the option of completing the survey in clinic or taking it home and returning it to the researchers within 1 week using a reply paid envelope. Four weeks after return of the initial survey, the participants were mailed a second survey that included questions about perceptions of errors in cancer care. Up to 2 reminder surveys were sent to nonresponders.
Measures
The following information was collected via patient self-report in the initial survey:
Demographic Characteristics
Age, sex, education, Aboriginal and/or Torres Strait Islander status, marital status, country of birth, post code of residence, living situation, employment, smoking, private health insurance, and concession card status were collected.
Disease and Treatment Characteristics
Cancer type, perceived stage of disease at diagnosis, remission status, time since diagnosis, treatments, and main reason for clinic visit on the day of recruitment were collected.
The following patient perceptions of errors in care were collected in the second survey:
How an Error Should be Dealt With
The participants were asked whether health professionals should be required to tell a patient if a mistake has been made in their care? (yes, always; yes, but only if it will not cause more harm or unnecessary worry; no, they should just fix the mistake).
Whether a Medical Error Occurred
The participants were asked whether the patient experienced a mistake in their cancer care (yes/no) and what the mistake was related to (diagnosis; procedure or surgery; medication type; medication dose; other, please describe).
Harm Related to Medical Error
The level of harm that resulted from the error (none, mild/limited harm, moderate/some harm, severe harm) was noted.
How the Medical Error Was Dealt With
The participants were asked how they found out that an error had been made. Response options included the following: (doctor or other health professionals told me; I noticed something wrong and raised the concern with my doctor; other, please describe). The respondents also indicated whether the cause of the error was explained to them (yes/no), they received an apology (yes/no), or any action had been taken to prevent the error happening again (yes/no/not sure).
Who Was Responsible for the Error
The participants were asked which of the following were, in their opinion, responsible for the error: (my doctor; nurse; other health professional; the hospital/clinic/treatment center; myself; other, please specify).
STATISTICAL ANALYSIS
Frequencies and proportions with 95% confidence intervals (CIs) were calculated for all variables. χ2 tests were used to examine whether demographic, disease, or treatment characteristic variables were associated with the likelihood of reporting an error (see Table 1 for details of the subcategories for each variable). Variables with an association of a P value of less than 0.1 were included in an adjusted logistic regression with reporting an error in cancer care as the outcome. For the logistic regression, a 5% significance level was used. All statistical analyses were conducted using SAS (v9.4; Cary, North Carolina).18
TABLE 1.
Demographic, Disease, and Treatment Characteristics of Participants (N = 1136)*
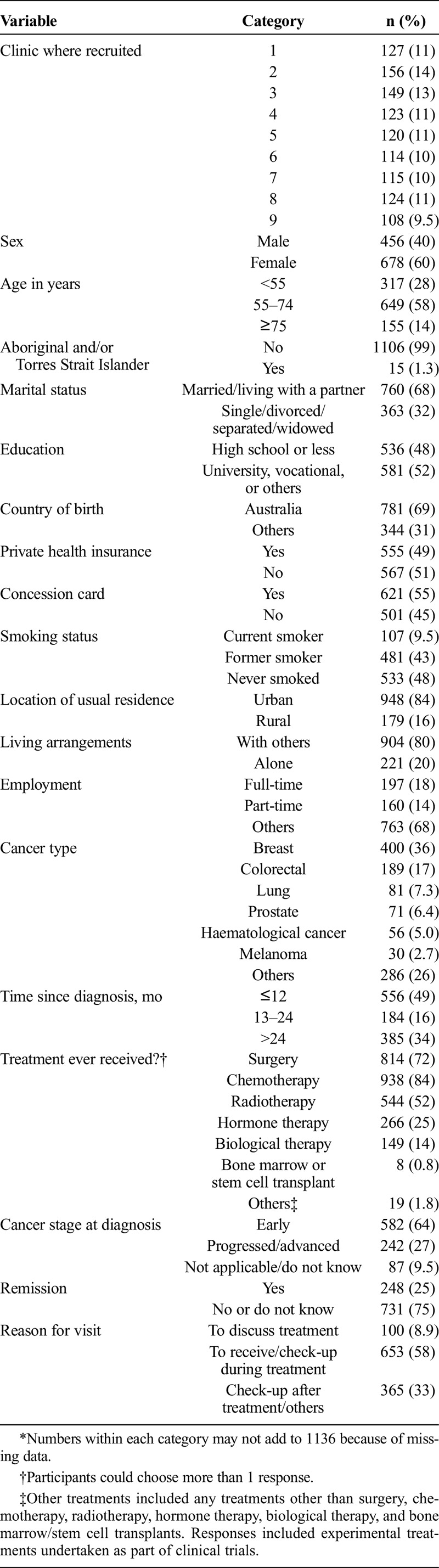
RESULTS
Of the 3906 patients screened for eligibility, 1238 were ineligible because of 1 or more of the following factors: attending the clinic for the first time, no confirmed cancer diagnosis, non-English speaking, too unwell, unable to provide informed consent, or unable to complete the survey independently. A further 392 were not approached to participate because of lack of time before their appointment. Of the remaining 2276 eligible patients, 1818 (80%) provided consent. Of those who consented, 1136 (62%) completed both an initial survey and a second survey and were included in the analyses. The characteristics of participants are shown in Table 1.
How an Error Should be Dealt With
Nine hundred eleven participants (84%; 95% CI = 81.4–85.5) agreed that health care providers should always inform a patient if an error has been made. One hundred fifty-seven participants (14%; 95% CI = 12.3–16.5) thought that patients should only be informed if doing so would not cause more harm or unnecessary worry, while 21 participants (2%; 95% CI = 1.1–2.7) perceived that the health care provider should just fix the error without informing the patient.
Whether a Medical Error Had Occurred
One hundred forty-eight participants (13%; 95% CI = 11.4–15.4) reported that an error had been made in their cancer care, 180 (16%; 95% CI = 14.1–18.5) were not sure, and 777 (70%; 95% CI = 67.6–73.0) reported that no errors had been made.
Harm Related to the Medical Error
Of the participants who experienced an error, 46 reported that the error was associated with severe harm (33%; 95% CI = 25.4–41.3), 36 with moderate/some harm (26%; 95% CI = 18.7–33.5), 30 with mild/limited harm (22%; 95% CI = 14.8–28.7), and 26 with no harm (19%; 95% CI = 12.2–25.4).
How the Medical Error Was Dealt With
Of the participants who experienced an error, 54 (38%; 95% CI = 29.7–45.8) reported that they had identified the error themselves and raised it with their doctor or other health professionals; 49 (34%; 95% CI = 26.4–42.1) reported that their doctor or other health professional had identified the error; and 40 (28%; 95% CI = 20.5–35.4) indicated that the error had been identified by some other means. These “other” responses were classified as follows: identification of error via an adverse event or observable problem (n = 11); unclear or miscellaneous (n = 11); error identified through a subsequent test, investigation, or consultation (n = 8); error identified by patient but not communicated to doctor (n = 5); and identified jointly by the doctor and patient (n = 5).
One hundred forty-four participants provided information regarding the type of error they experienced. Sixty-one participants perceived that an error had been made in relation to diagnosis (42%; 95% CI = 34.1–50.5), 28 participants perceived that an error had occurred during a procedure or surgery (19%; 95% CI = 12.9–26.0), 13 participants perceived that they had been given the wrong dose of medication (9%; 95% CI = 4.3–13.8), and 12 participants perceived that they had been given the wrong type of medication (8%; 95% CI = 3.8–12.9). Thirty participants (21%; 95% CI = 14.1–27.5) perceived that some other type of error had occurred including the following: health service errors (e.g., related to follow-up care or documentation of medical information, n = 12); errors related to the prevention and management of adverse effects (n = 9); treatment errors (e.g., wrong type of treatment, n = 7); and more than 1 type of error (n = 2).
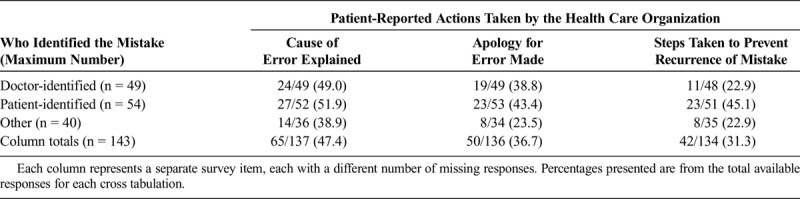
Table 2 shows that a similar proportion of those who reported a doctor- or patient-identified error reported having the cause of the error explained and receiving an apology for the error. A greater proportion of the participants experiencing a patient-identified error received an explanation about steps taken to prevent the error from recurring.
TABLE 2.
Patients' Perceptions of Actions Taken in Response to the Error and How the Error Was Identified
Who Was Responsible for the Error?
Almost two thirds of participants (n = 92, 65%; 95% CI = 56.8–72.7) attributed the error to their doctor, 15 (11%; 95% CI = 5.4–15.7) to a nurse, 17 (12%; 95% CI = 6.6–17.4) to another type of health professional, 24 (17%; 95% CI = 10.7–23.1) to the hospital, clinic, or treatment center, 12 (8.5%; 95% CI = 3.8–13.1) to themselves, and 11 (7.8%; 95% CI = 3.3–12.2) to some other cause.
Factors Associated With a Perceived Error in Care
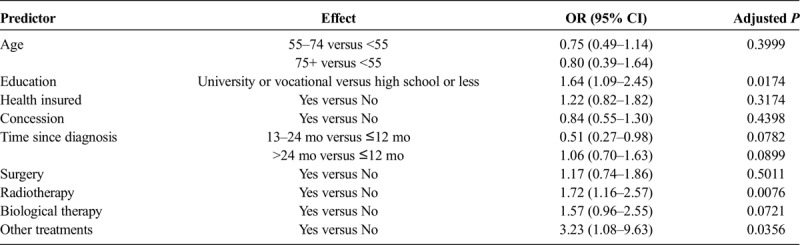
Univariate analysis showed that age, education, private health insurance status, concession card status, time since diagnosis, having surgery, radiotherapy, biological therapy, and “other” treatments for cancer were associated with a reported error in care (P < 0.1). After adjusting for confounders, multiple logistic regression showed that having a university or vocational education increased the odds of reporting an error by 9% to 245% (P = 0.0174), having radiotherapy treatment increased the odds of reporting an error by 16% to 257% (P = 0.0076), while having “other” treatments increased the odds of reporting an error by 8% to 963% (P = 0.0356; Table 3).
TABLE 3.
Factors Associated With Reporting an Error in Care
DISCUSSION
This is one of few large-scale studies to assess oncology patient perceptions of errors in their cancer care. Similar to previous studies,19,20 our results show that most patients with cancer (84%) believe that errors in care should always be disclosed to the patient. In our sample, 1 of 8 participants reported that some type of error has been made in their care, and a third of these perceived that the error was associated with severe harm. The prevalence of errors reported in our study (13%) is similar to that reported by Schwappach and Wernli (16%)15 and lower than that reported by Mazor et al21 (22%) and Bryant et al16 (26%). It should be noted, however, that the results of our study are not directly comparable with these studies because of differences in the samples studied, question framing, and data collection methods.
Most Patients Perceived That the Error Experienced Was Associated With Harm
It is notable that more than half (57%) of the respondents who reported an error perceived that it was associated with moderate to severe harm. This is at odds with other studies that have consistently found that medical errors are usually associated with low levels of harm.4,7,22 This may reflect that our study used patient rather than health professional judgments of level of harm. For example, it is possible that health professionals are not always aware of the level of physical discomfort experienced as a result of an error or that patients take into account considerations such as emotional distress and inconvenience when judging harm. Future work could explore how patient and health professional judgments of harm related to the same error differ. In addition, a limitation of our study was that we did not provide definitions or examples of particular levels of harm. Therefore, it is likely that judgments regarding what constitutes severe harm differed among participants.
How Well Do Patient Experiences of Response to Errors Correspond to Best Practice?
Overall, less than half of the respondents reported that they had received an apology (35%) or an explanation about the cause of the error (45%).
The proportion of patients reporting that an appropriate response to the error was made was lowest among those who identified that the error had been identified by “other” means. A number of errors in this category were identified via a subsequent test, procedure, or consultation. Although we did not collect data on where these tests or services were delivered, it is possible that some of these were performed by another service or doctor, and therefore, the results were not communicated back to the health care providers responsible for the original error. Similarly, in a small number of cases, patients reporting errors identified by “other” means did not notify their health care provider of the error.
Overall, only 36% of patients reporting an error indicated that they had been informed about steps to prevent future errors. As described previously, it is likely that in some cases, this may reflect that the health professionals or services responsible were not aware that an error had occurred. For the remaining cases, it is unclear from our data whether this indicates that no steps were taken or failure to communicate such actions to patients.
Who Is Most Likely to Report an Error?
People with a university or vocational level of education were more likely to report an error in care than those with less education. Because higher levels of education are associated with greater health literacy,23 this finding may reflect greater expectations of care and awareness of errors among such patients, rather than a difference in the rate of errors.
The receipt of radiotherapy or “other” treatment was also associated with higher likelihood of reporting an error in care. Treatment provided for multiple sessions, as well as complex treatments with input from many health professionals, may lend itself to greater opportunity for errors to occur.
IMPLICATIONS
Despite clear policy recommendations regarding the steps that should be taken to respond to errors in care, our data suggest considerable room for improvement in communication after an error.
Our results suggest that a multifaceted approach to improving responses to errors in care is needed. First, given that a sizeable proportion of errors are patient-identified and that not all of these are communicated to the health professional or service responsible, health services may consider ensuring that patients are educated with respected to their rights and responsibilities regarding safe health care. To improve health service awareness of patient-identified errors, discharge planning or other key transition periods could be used to ask some brief questions about whether patients have experienced any concerns or problems with their care. Anonymous patient surveys could also be used to assess patient experiences broadly including the experience of errors.
Given that it is likely that some errors are identified by other services or doctors, it is important that such errors are communicated to the health care providers responsible for the error. This should be performed in a constructive manner to facilitate quality improvement strategies to address problems identified. Finally, development of procedures and training to support staff in communicating with patients regarding errors may also be an important factor in improving care.
LIMITATIONS
Almost all hospitals which participated in this study, were large metropolitan public hospitals. Therefore, it is likely that the current results are not generalizable to the diversity of Australian cancer treatment centers in terms of funding status (public/private) and geographic location (rural/urban). Although the response rate of 62% may seem low, it is comparable with other studies using a 2-step recruitment and data collection process.24,25
The data collected in the current study were self-report and therefore subject to recall bias. There was the option of providing a shorter time frame for recall (e.g., asking respondents about errors experienced in the past 6 months). However, given uncertainty about the prevalence of errors for this time frame, the decision was made to ask about any errors during the patient's cancer care. Although self-report bias suggests caution in interpreting reported error rates, it can be argued that self-report is the most appropriate way of assessing the impact of a perceived error on an individual. Similarly with reported communication after an error, patient self-report is the only way to capture how such communication was perceived and understood.
CONCLUSIONS
One in 8 patients receiving care for cancer perceives that an error has been made in their care. Despite clear recommendations about optimal processes for disclosure after an error, patients report that best practice communication does not occur in most cases. These results highlight the need to redesign health care systems to reduce human error in cancer care and facilitate appropriate responses by the healthcare system when such errors do occur.
ACKNOWLEDGMENTS
The authors thank the participating cancer treatment centers, Rochelle Smits, Alison Zucca, and Hannah Small for research support, Sandra Dowley for data management, and Joseph Hanna, Alessandra Bisquera, and Tiffany Evans for statistical assistance.
Footnotes
This work was supported by a National Health and Medical Research Council Project Grant (ID 1010536), a Strategic Research Partnership Grant (CSR 11-02) from Cancer Council NSW to the Newcastle Cancer Control Collaborative (New-3C), and infrastructure funding from the Hunter Medical Research Institute (HMRI). M.C. is supported by a National Health and Medical Research Council Translating Research into Practice Fellowship (APP1073031). J.B. is supported by an Australian Research Council Post-Doctoral Industry Fellowship. A.W.B. is supported by National Health and Medical Research Council (APP1073317) and Cancer Institute NSW (13/ECF/1-37) Early Career Fellowships.
The authors disclose no conflict of interest.
REFERENCES
- 1.Smith CM. Origin and uses of primum non nocere—above all, do no harm! J Clin Pharmacol. 2005;45:371–377. [DOI] [PubMed] [Google Scholar]
- 2.Kohn LT, Corrigan JM, Donaldson MS. To Err Is Human: Building a Safer Health System. Washington, DC: National Academies Press; 2000. [PubMed] [Google Scholar]
- 3.Van Den Bos J, Rustagi K, Gray T, et al. The $17.1 billion problem: the annual cost of measurable medical errors. Health Aff (Millwood). 2011;30:596–603. [DOI] [PubMed] [Google Scholar]
- 4.Belela AS, Peterlini MA, Pedreira ML. Medication errors reported in a pediatric intensive care unit for oncologic patients. Cancer Nurs. 2011;34:393–400. [DOI] [PubMed] [Google Scholar]
- 5.Singh H, Sethi S, Raber M, et al. Errors in cancer diagnosis: current understanding and future directions. J Clin Oncol. 2007;25:5009–5018. [DOI] [PubMed] [Google Scholar]
- 6.Makary MA, Epstein J, Pronovost PJ, et al. Surgical specimen identification errors: a new measure of quality in surgical care. Surgery. 2007;141:450–455. [DOI] [PubMed] [Google Scholar]
- 7.Walsh KE, Dodd KS, Seetharaman K, et al. Medication errors among adults and children with cancer in the outpatient setting. J Clin Oncol. 2009;27:891–896. [DOI] [PubMed] [Google Scholar]
- 8.Ranchon F, You B, Salles G, et al. Improving cancer patient care with combined medication error reviews and morbidity and mortality conferences. Chemotherapy. 2013;59:330–337. [DOI] [PubMed] [Google Scholar]
- 9.Full Disclosure Working Group. When things go wrong: responding to adverse events: a consensus statement of the Harvard hospitals. Boston, MA: Massachusetts Coalition for the Prevention of Medical Errors; 2006. [Google Scholar]
- 10.Yardley IE, Yardley SJ, Wu AW. How to discuss errors and adverse events with cancer patients. Curr Oncol Rep. 2010;12:253–260. [DOI] [PubMed] [Google Scholar]
- 11.O'Connor E, Coates HM, Yardley IE, et al. Disclosure of patient safety incidents: a comprehensive review. Int J Qual Health Care. 2010;22:371–379. [DOI] [PubMed] [Google Scholar]
- 12.White AA, Gallagher TH, Krauss MJ, et al. The attitudes and experiences of trainees regarding disclosing medical errors to patients. Acad Med. 2008;83:250–256. [DOI] [PubMed] [Google Scholar]
- 13.Kaldjian LC, Jones EW, Wu BJ, et al. Disclosing medical errors to patients: attitudes and practices of physicians and trainees. J Gen Intern Med. 2007;22:988–996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mazor KM, Simon SR, Gurwitz JH. Communicating with patients about medical errors: a review of the literature. Arch Intern Med. 2004;164:1690–1697. [DOI] [PubMed] [Google Scholar]
- 15.Schwappach DL, Wernli M. Chemotherapy patients' perceptions of drug administration safety. J Clin Oncol. 2010;28:2896–2901. [DOI] [PubMed] [Google Scholar]
- 16.Bryant J, Carey M, Sanson-Fisher R, et al. The patients' perspective: haematological cancer patients' experiences of adverse events as part of care. J Patient Saf. 2017. [Epub ahead of print]. [DOI] [PubMed]
- 17.Mazor KM, Roblin DW, Greene SM, et al. Toward patient-centered cancer care: patient perceptions of problematic events, impact, and response. J Clin Oncol. 2012;30:1784–1790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.SAS v9.4. Cary, North Carolina: SAS Institute; 2016. [Google Scholar]
- 19.Gallagher TH, Waterman AD, Ebers AG, et al. Patients' and physicians' attitudes regarding the disclosure of medical errors. JAMA. 2003;289:1001–1007. [DOI] [PubMed] [Google Scholar]
- 20.Hobgood C, Peck CR, Gilbert B, et al. Medical errors—what and when: what do patients want to know? Acad Emerg Med. 2002;9:1156–1161. [DOI] [PubMed] [Google Scholar]
- 21.Mazor KM, Greene SM, Roblin D, et al. More than words: patients' views on apology and disclosure when things go wrong in cancer care. Patient Educ Couns. 2013;90:341–346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Raab SS, Grzybicki DM. Quality in cancer diagnosis. CA Cancer J Clin. 2010;60:139–165. [DOI] [PubMed] [Google Scholar]
- 23.Kutner M, Greenburg E, Jin Y, et al. The Health Literacy of America's Adults: Results from the 2003 National Assessment of Adult Literacy. NCES 2006–483. Washington, DC: National Center for Education Statistics; 2006. [Google Scholar]
- 24.Hall AE, Sanson-Fisher RW, Lynagh MC, et al. Format and readability of an enhanced invitation letter did not affect participation rates in a cancer registry-based study: a randomized controlled trial. J Clin Epidemiol. 2013;66:85–94. [DOI] [PubMed] [Google Scholar]
- 25.Armes J, Crowe M, Colbourne L, et al. Patients' supportive care needs beyond the end of cancer treatment: a prospective, longitudinal survey. J Clin Oncol. 2009;27:6172–6179. [DOI] [PubMed] [Google Scholar]


