Supplemental digital content is available in the text.
Key Words: medical accident, near miss, laparoscopic surgery, thoracoscopic surgery, minimally invasive surgery
Abstract
Objectives
The aim of this study was to clarify the characteristics of adverse events/near misses during laparoscopic/thoracoscopic surgery.
Methods
Using relevant key words for minimally invasive surgeries, 540 records were identified in the database of the Japan Council for Quality Health Care. After data review and the classification of adverse events, 746 events associated with laparoscopic (laparo group) and/or thoracoscopic (thoraco group) surgery were identified. We calculated the frequency of each event, compared the frequency regarding recurrent events, and evaluated the types of event that had resulted in deaths between the 2 groups.
Results
There were 582 events in the laparo group, 159 in the thoraco group, and 5 in those undergoing combined surgery. Overall, injury of other organs (11.4%, 85/746), retention of a foreign body (9.1%, 68/746), breakage/failure of medical equipment or devices (6.2%, 46/746), massive bleeding (5.9%, 44/746), misperception of anatomy (5.6%, 42/746), and vascular injury (4.8%, 36/746) were frequently reported. There were marked differences in the frequency of injury of other organs (laparo group: 13.4%, 78/582; thoraco group: 4.4%, 7/159), massive bleeding (laparo group: 3.4%, 20/582; thoraco group: 14.5%, 23/159), and vascular injury (laparo group: 2.6%, 15/582; thoraco group: 12.6%, 20/159) between the 2 groups. Among the 56 patient-death reports, 132 adverse events were identified. In the thoraco group, bleeding events were frequently observed, whereas in the laparo group, various categories of events were noted.
Conclusions
We observed recurrent incidents and differences in the frequency between the 2 groups. Surgeons should keep in mind these characteristics. Retention of a foreign body and the breakage/malfunctioning of instruments might be reduced by the introduction of specialized checklists.
Since the report “To Err is Human, Building a Safer Health System,”1 health care workers have re-realized that medical accidents are inevitable events during daily clinical practice, and, among medical practices, surgical procedures particularly pose a potential risk to patients, which could result in significant complications.
Recent progress in minimally invasive surgery, such as thoracoscopic/laparoscopic/robotic surgeries, has provided several advantages including reduced pain, less scarring, lower-level blood loss, and an earlier return to normal activities. On the other hand, such progress has made the environment in the operating theater more complex, whereby surgeons have to be familiar with numerous energy devices as well as endoscopic equipment, which is sometimes delicate and fragile. Although magnification by a laparoscope can provide surgeons with a level of anatomic detail that is not possible during open surgery, the haptic feedback and panoramic view are compromised, which might cause medical errors specific to those procedures.
In 2004, to prevent medical adverse events and promote patient safety, the division of adverse event prevention of the Japan Council for Quality Health Care (the JCQHC), a public interest incorporated foundation, started their unique activity of collecting data on medical adverse events/near misses. Since 2010, their data have been available on their Web site, and data on 18,281 medical adverse events and 42,262 near miss events had been made available to the public as of the end of June 2016 (http://www.med-safe.jp/pdf/report_45.pdf). In the present study, we examined the characteristics of medical adverse events/near misses associated with minimally invasive surgeries. Our aim was to clarify the recurrent events and potential backgrounds that should be shared as common knowledge among health care professionals.
METHODS
After institutional review board approval, we searched for medical adverse events/near misses related to laparoscopic/thoracoscopic surgery in the JCQHC open database (http://www.med-safe.jp). At the end of March 2016, 1026 hospitals had participated in medical adverse event collection, 642 hospitals had participated in the collection of details about near misses, and their data had been reported through the JCQHC Web site in a checklist/pull-down list and narrative manner. Regarding medical adverse events, university hospitals, national hospitals, and advanced treatment hospitals have mandatorily participated in this program, and other medical institutions have voluntarily joined it. In terms of near-miss data collection, such data have been voluntarily collected.
In the JCQHC Web site, data on potential events can be exported into Microsoft Excel format using key words. Their data include the discoverer of the incident, personnel in charge of the incident, patient's age (range), sex, details of the incident in a narrative manner, day of the week when the incident occurred, medical field involved, and reporter's assessment regarding the possibility of disabilities remaining. Because their data are in Japanese, Japanese words meaning “laparoscopic surgery,” “thoracoscopic surgery,” “robot-assisted surgery,” and “endoscopic surgery” were used for data extraction. We initiated the present study in April 2014, and our latest search was conducted in June 2016. In the latest search, 934 potential records were extracted. Initially, the first author (T.A.) reviewed all of the reports and then extracted the adverse events described in each report. After the data review, we excluded 394 records from the analysis because of incidents related to procedures other than laparoscopic or thoracoscopic surgery (n = 170), incidents that occurred outside the operating theater (e.g., fall from a bed on the night of surgery, n = 151), incidents associated with diagnostic or therapeutic gastric endoscopy/colon fiber procedures such as endoscopic submucosal dissection (n = 56), incidents with insufficient information (n = 14), reports of events not considered as an incident or near miss (n = 2), and 1 overlapping report. Regarding the allocation of adverse events to the remaining 540 records, we followed the rules described as follows:
Because there were many blanks for the medical field, we allocated the main field related to each report based on the narrative part of the report as well as the original allocation.
We tried to allocate adverse events faithfully according to the description of each report. We sometimes allocated several adverse events, although each event might be closely related, such as anastomotic failure/ileus/peritonitis or vascular injury/massive bleeding.
Regarding the problems related to medical equipment and devices, we considered apparent damage or a part falling off an instrument as “breakage” and malfunction without macroscopic damage as “failure.”
Regarding drain dislocation inside the body, we allocated “problems related to a drainage tube” when immediately realized and “retention of a foreign body” when it was not initially realized and later found as a foreign body.
We allocated “massive bleeding” when (1) description of massive bleeding in the text, (2) blood loss of more than 2000 mL that meant an immediate life-threatening situation and required appropriate management, or (3) bleeding that resulted in death, were found in the reports.
Vascular division or division of the common bile duct because of misperception of the anatomy was counted as “misperception of anatomy” and not vascular injury or injury of the bile duct.
Cases of death due to an unknown cause were recorded as intraoperative death/early postoperative death.
In 146 reports, we allocated multiple events (2 events: n = 104, 3 events: n = 28, 4 events: n = 11, 5 events: n = 2, 6 events: n = 1). Finally, 746 events associated with laparoscopic and/or thoracoscopic surgery were included in the analysis.
Analyses
We firstly gained an overall view of adverse events. Regarding the frequent incidents, we examined their details. Thereafter, we compared the differences in frequent incidents between the laparoscopic/laparoscopy-assisted surgery (laparo group) and thoracoscopic/thoracoscopy-assisted surgery (thoraco group). For the analyses, regarding the 41 events related to robotic surgery (prostate: n = 25, stomach: n = 9, uterus/ovary: n = 4, lung: n = 2, bladder: n = 1), surgeries for abdominal organs were considered as the laparo group and those for the lung as the thoraco group for the analyses. Regarding the 8 events related to esophageal surgery, in which the surgical approach was not described, we treated those as the thoraco group. Lastly, we analyzed the type of adverse event associated with patient deaths.
RESULTS
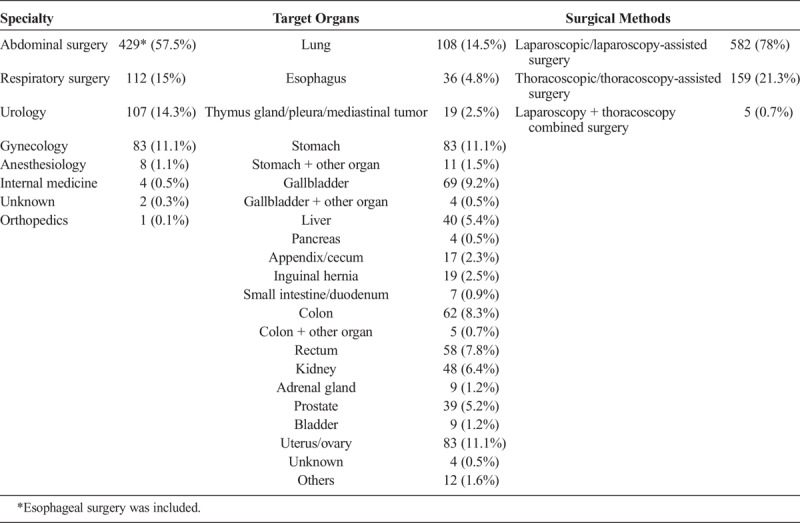
Supplementary Table 1, http://links.lww.com/JPS/A109, summarizes the background information from the 540 records included in the present study. Doctors were the main professionals in charge of incidents (424/540, 78.5%). Fifty-six records (10.4%) described patient deaths, and the reporters described the marked possibility of disabilities remaining in 55 records (10.2%). As described in the “Methods” section, we allocated 746 events to the records. Table 1 summarizes the number of adverse events according to medical fields, target organs, and surgical methods. Of the 746 incidents, 57.5% (429/746) occurred in abdominal surgery, followed by respiratory surgery (15%, 112/746), urology (14.3%, 107/746), and gynecology (11.1%, 83/746). Regarding the surgical approach, 582 events (78%, 582/746) occurred in the laparo group, 159 (21.3%, 159/746) in the thoraco group, and 5 (0.7%, 5/726) in those undergoing combined surgery.
TABLE 1.
Summary of Number of Adverse Events According to Medical Fields, Target Organs, and Surgical Methods
Overall Results
Figure 1 shows the results for all events. The most frequent category was injury of other organs (11.4%, 85/746), followed by the retention of a foreign body (9.1%, 68/746), breakage or failure of medical equipment or devices (6.2%, 46/746), massive bleeding (5.9%, 44/746), misperception of anatomy (5.6%, 42/746), and vascular injury (4.8%, 36/746). Details of miscellaneous events are shown in Supplementary Table 2, http://links.lww.com/JPS/A111.
FIGURE 1.
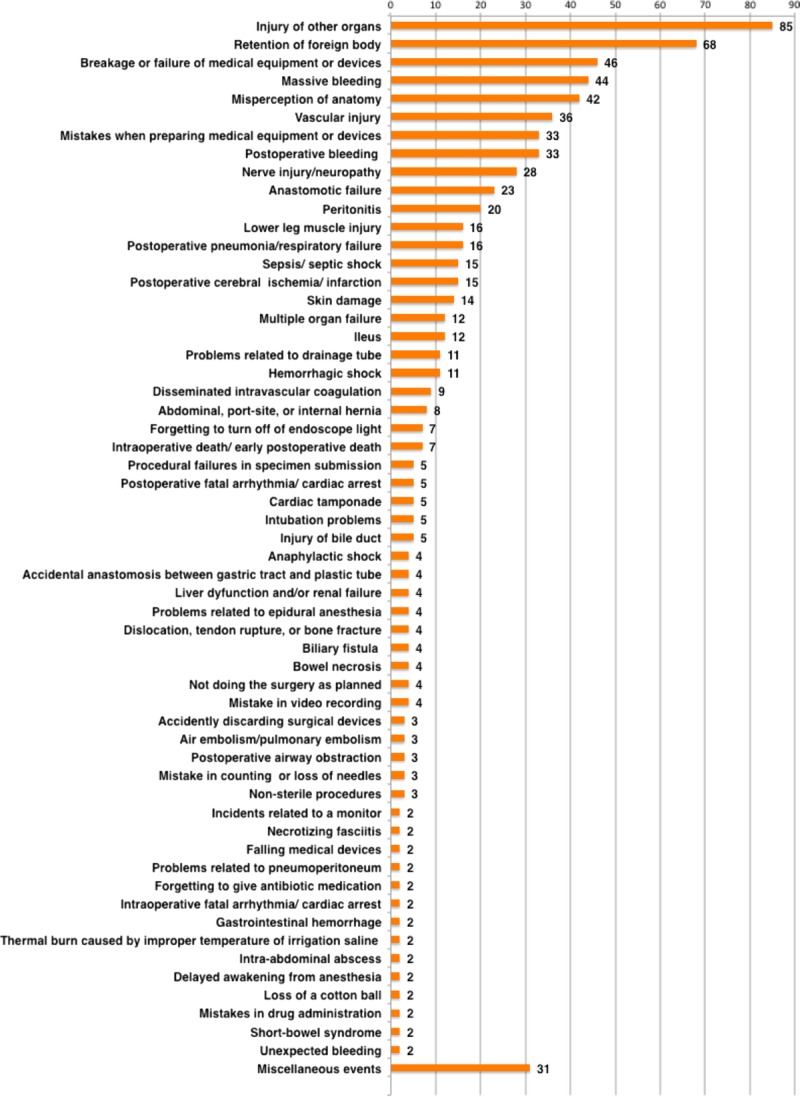
The results for all events. The most frequent category was injury of other organs (11.4%, 85/746), followed by the retention of a foreign body (9.1%, 68/746), breakage or failure of medical equipment or devices (6.2%, 46/746), massive bleeding (5.9%, 44/746), misperception of anatomy (5.6%, 42/746), and vascular injury (4.8%, 36/746).
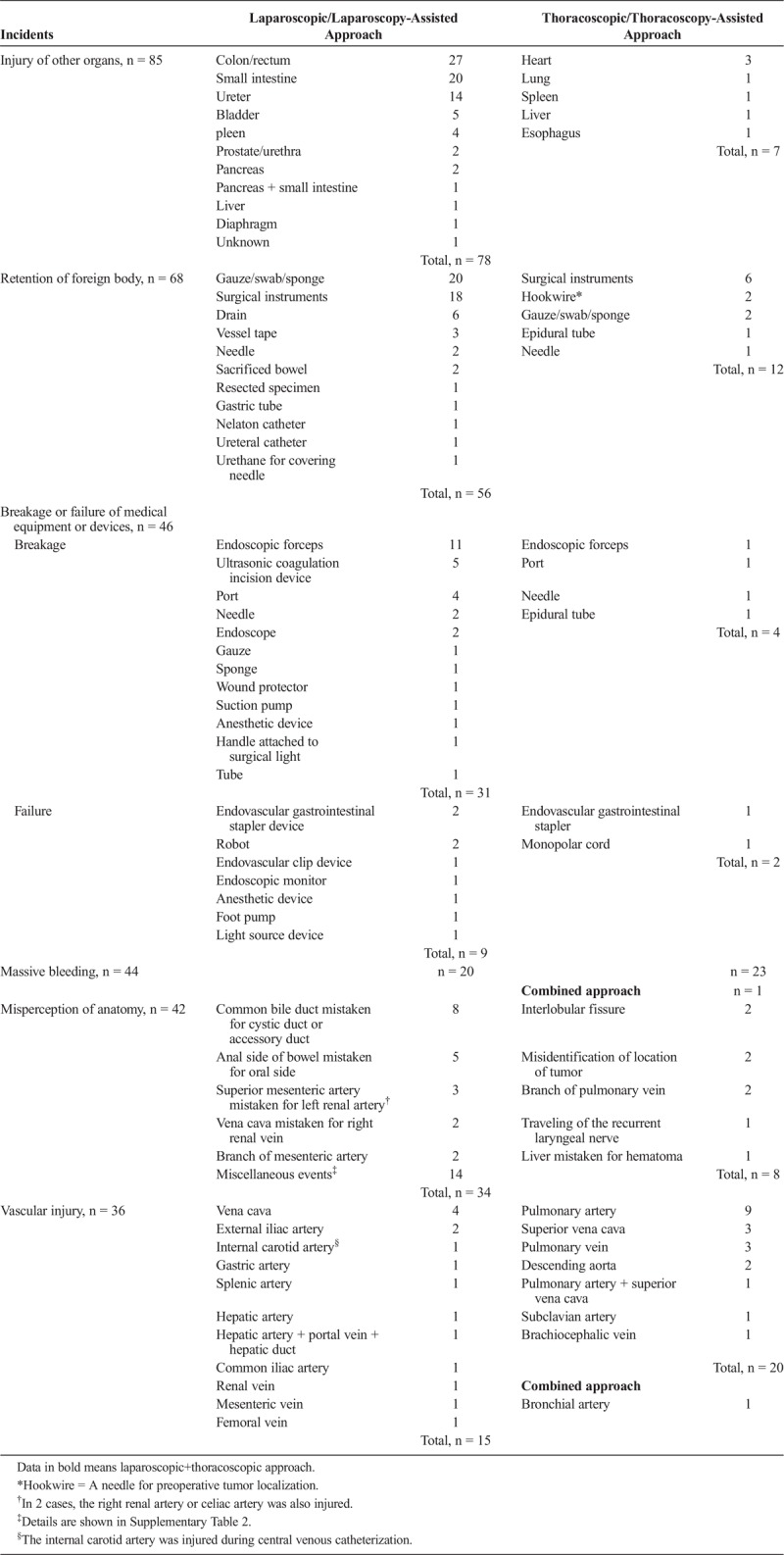
Table 2 summarizes the details of the aforementioned recurrent events in the laparo and thoraco groups. In terms of injury of other organs, bowel injury such as that involving the colon/rectum (n = 27) and small intestine (n = 20) was common, followed by urinary tract injury (ureter: n = 14, bladder: n = 5). Among the 85 injuries, 47.1% (40/85) were detected during the procedures, whereas 52.9% (45/85) were initially missed. In 6 events, injuries were caused by a pneumoperitoneum needle or surgical port placement, and vascular injury simultaneously occurred in 2 of the 6. Regarding the retention of a foreign body, surgical instruments (laparo group: n = 18, thoraco group: n = 6) and a gauze/swab/sponge (laparo group: n = 20, thoraco group: n = 2) were the 2 most common items left in the body. In 14 cases (20.6%, 14/68), retention was incidentally recognized more than 1 year after the operation. Among cases involving the breakage of medical equipment or devices, the breakage of endoscopic forceps was the most frequent (laparo group: n = 11, thoraco group: n = 1), followed by that of an ultrasonic coagulation incision device (laparo group: n = 5) and port (laparo group: n = 4, thoraco group: n = 1). In the 11 cases (endoscopic forceps/ultrasonic coagulation incision device: n = 10, epidural tube: n = 1), breakage events subsequently resulted in the retention of a foreign body. In addition, 2 events of failure of medical equipment or devices caused vascular injures, which resulted in massive bleeding (endovascular gastrointestinal stapler: n = 1, endovascular clip device: n = 1). Regarding misperception of anatomy, the most frequent event was that the common bile duct being mistaken for a cystic or an accessory duct (n = 8). The anal side of the bowel being mistaken for the oral side (n = 5), superior mesenteric artery being mistaken for the left renal artery (n = 3), vena cava being mistaken for the right renal vein (n = 2), misperception of the mesenteric artery branch (n = 2) and interlobular fissure (n = 2), and the misidentification of the location of a tumor (n = 2) or pulmonary vein branch (n = 2) were reported multiple times. Other misperceptions are described in Supplementary Table 3, http://links.lww.com/JPS/A110. In terms of vascular injury, the pulmonary artery was the most frequently injured (n = 9), followed by the superior vena cava (n = 3), pulmonary vein (n = 3), descending aorta (n = 2), and external iliac artery (n = 2). Of the 36 vascular injuries, 75% (27/36) resulted in massive bleeding.
TABLE 2.
Summary of Recurrent Incidents
Comparative Study Between the Laparo and Thoraco Groups
Figure 2 shows a comparative study of the proportion of these 6 categories between the laparo and thoraco groups. There was a marked difference in the rate regarding other organ injury (laparo group: 13.4%, 78/582; thoraco group: 4.4%, 7/159), massive bleeding (laparo group: 3.4%, 20/582; thoraco group: 14.5%, 23/159), and vascular injury (laparo group: 2.6%, 15/582; thoraco group: 12.6%, 20/159) between the 2 groups.
FIGURE 2.
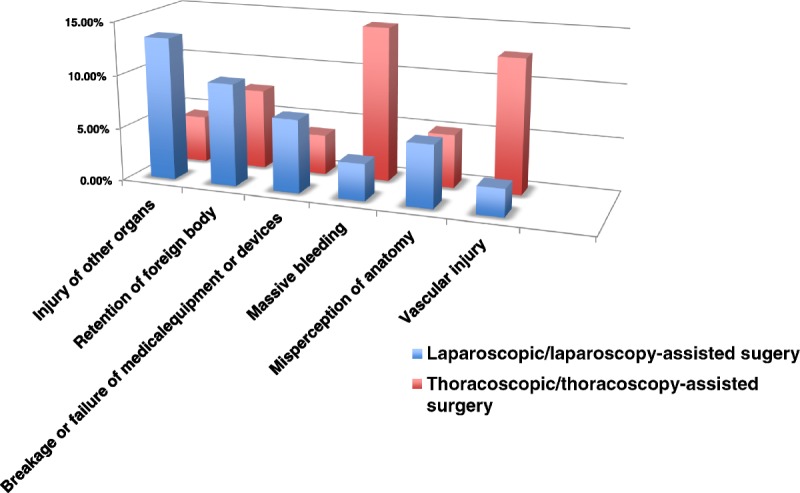
Comparative study of the 6 recurrent categories between laparoscopic/laparoscopy-assisted surgery and thoracoscopic/thoracoscopy-assisted surgery. There was a marked difference in the rate regarding other organ injury (laparo group: 13.4%, 78/582; thoraco group: 4.4%, 7/159), massive bleeding (laparo group: 3.4%, 20/582; thoraco group: 14.5%, 23/159), and vascular injury (laparo group: 2.6%, 15/582; thoraco group: 12.6%, 20/159) between the 2 groups.
Analysis of Death Reports
As described previously, there were 56 patient deaths reported. Target organs were the lung (n = 14), liver (n = 9), esophagus (n = 8), stomach (n = 5), gallbladder (n = 4), colon (n = 3), kidney (n = 3), stomach plus other organs (n = 2), prostate (n = 2), rectum (n = 2), uterus/ovary (n = 1), small intestine/duodenum (n = 1), inguinal hernia (n = 1), and thymus (n = 1). Regarding the adverse events, 132 events were identified. A median of 2 events (range, 1–6) was identified in 1 report. Overall, various adverse events were detected in death cases. A summary of the adverse events associated with patient death divided by target organs is shown in Supplementary Table 4, http://links.lww.com/JPS/A112. Figure 3 shows a summary of adverse events associated with patient death divided by surgical methods. In the thoraco group, bleeding events were frequently observed (massive bleeding, vascular injury, postoperative bleeding, hemorrhagic shock), whereas in the laparo group, various categories of events were observed such as multiple organ failure, postoperative pneumonia/respiratory failure, and anastomotic failure.
FIGURE 3.
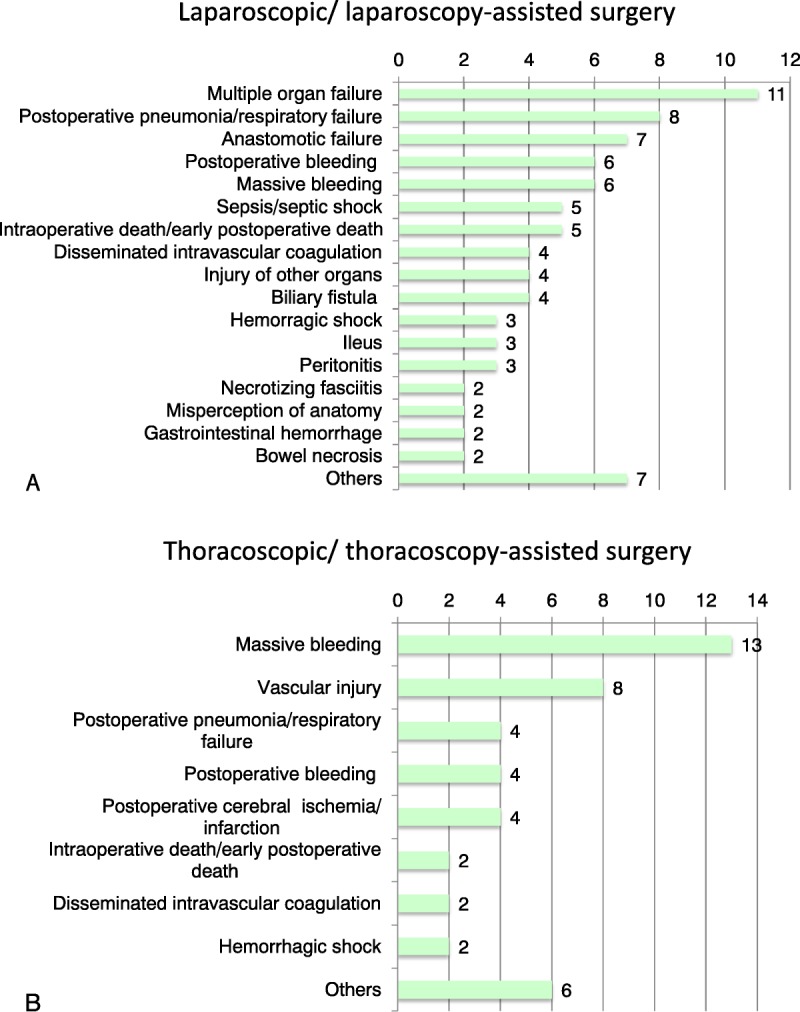
Summary of medical adverse events associated with patient deaths divided by surgical methods. In the thoraco group, bleeding events were frequently observed (massive bleeding, vascular injury, postoperative bleeding, hemorrhagic shock), whereas in the laparo group, various categories of events were observed, such as multiple organ failure, postoperative pneumonia/respiratory failure, and anastomotic failure.
DISCUSSION
The results from the JCQHC open database showed that injury of other organs (11.4%, 85/746), retention of a foreign body (9.1%, 68/746), breakage/failure of medical equipment or devices (6.2%, 46/746), massive bleeding (5.9%, 44/746), misperception of anatomy (5.6%, 42/746), and vascular injury (4.8%, 36/746) were the top 6 medical adverse events/near misses associated with laparoscopic/thoracoscopic surgery. Probably because we focused on the incidents occurring in the operative theater, doctors were the main professionals in charge of incidents in the present study. Injury of other organs was more frequently reported in laparoscopic surgery, whereas in thoracoscopic surgery, massive bleeding and vascular injury were frequent, which were also major causes of patient death in the latter group. Our observation further confirmed the already recognized risks related to minimum invasive surgery that surgeons should refamiliarize themselves with. In addition, our study highlighted novel potential threats inherent in the recently advancing surgery.
Regarding the injured organs, the bowel was the most commonly injured organ, followed by injury of the urinary tract. In the present study, 54% (45/85) of the injuries were initially missed. The previous misadventure data regarding laparoscopic surgery also showed that approximately two-thirds of injuries were initially missed, and, in some cases, that delay caused serious complications, such as peritonitis and sepsis.2 In the 6 reports, injuries were caused by a pneumoperitoneum needle or surgical port placement, and vascular injury simultaneously occurred in 2 of the 6 reports. Injury of other organs or vascular structures at the time of entry is also a well-known complication,3,4 and the reported incidence was around 0.4 to 0.7 per 1000, respectively.3 Regardless of entry procedures such as the open technique (Hasson) and Veress needle technique, surgeons should pay close attention to adjustment structures, especially in patients with a history of surgery. To decrease the incidence of injury of other organs, surgeons should keep in mind that those complications could happen anytime, from trocar insertion to wound closure. The surgeon and assistants should always manipulate the organs gently, be careful during the exchange of devices to prevent organ injuries outside the visual view, and have sufficient knowledge about surgical devices to prevent thermal injuries or a catastrophic situation caused by improper usage. Before terminating procedures, target as well as other organs should be examined carefully to identify previously unrecognized organ injuries. Generally speaking, because surgical experience is associated with the complication rate, novice surgeons should start their laparoscopic surgeries with experienced surgeons.
Regarding foreign body retention, the incidence was estimated to be around 1 per 8000 to 1 per 18,000.5 Although it was an uncommon event, it might cause severe complications, such as bowel perforation, sepsis, or patient death.6 Up to the present, sponges have been considered to be the most common surgical items left in patients. For example, Gawande et al observed that, based on medical malpractice claims and incident reports related to the retention of a surgical instrument or sponge filed between 1985 and 2001 with a large malpractice insurer representing one-third of the physicians in Massachusetts, a total of 61 retained bodies in 54 patients were reported, and, of those, 69% were sponges and 31% were instruments. Thirty-seven patients required a second operation for the removal of the object and management of complications, and their case-control study revealed that emergency surgery, an unplanned change in the operation, and a higher body mass index were significantly correlated with the retention of a foreign body.5 In the present study, surgical instruments and a gauze/swab/sponge were the 2 most frequent items left in the body, and, in 16.2% (11/68) of the events, the breakage of medical devices resulted in retention. Our study revealed a strong association between the breakage of medical instruments and subsequent retention of part of them in laparoscopic/thoracoscopic surgery. Regarding the risk of the breakage of medical instruments, Yasuhara et al7 also reported that, based on incident/near miss–incident reports and the request forms for the repair of broken instruments at the Surgical Center of the University of Tokyo Hospital, instruments for laparoscopy- and thoracoscopy-assisted surgeries were broken more frequently intraoperatively than any other type of instrument (P < 0.01, χ2 test), and they suggested the occult risk of foreign body retention of part of the instruments. Our observation and that of Yasuhara et al revealed the inherent risk of recent sophisticated surgical devices and suggested that physicians and manufacturers must always consider their durability. The limited visual field of a camera would increase the risk of retention, especially when breakage occurs outside the visual field. In the United States, a national surgical patient safety project named “Nothing Left Behind” has been ongoing since 2004 to prevent the retention of surgical items,8 and they also pointed out the growing problem of retained small miscellaneous items named “surgical junk” in the new era of health care.9 Although several researchers reported that a specially designed checklist for laparoscopic procedures in conjunction with a regular briefing protocol was feasible to decrease the number of adverse events,10,11 leaving “surgical junk” might be an unavoidable problem inherent with recent sophisticated and advanced medical devices.
In the present study, we did not observe incidents caused by insulation failure, which is thought to be one of the main causes of electrosurgical complications. Montero et al12 reported in their study, involving 4 major urban hospitals, that of the 226 laparoscopic instruments tested (165 reusable), insulation failure occurred more frequently in reusable (19%, 31/165) than in disposable (3%, 2/61, P < 0.001) instruments. Although the clinical significance of these insulation failures remains unknown, surgeons should recognize the high incidence of insulation failures of surgical instruments, and careful visual inspection of instruments and insulation evaluation with a porosity detector before surgery might reduce the risk of instrument malfunction and thermal injury.
Regarding vascular injury, the injury of the pulmonary artery was the most frequently reported (n = 9), followed by that of the superior vena cava (n = 3), pulmonary vein (n = 3), descending aorta (n = 2), and external iliac artery (n = 2). Because these vasculatures are all major trunks, they do not reflect the true incidence of vascular injury and it is highly likely that many minor vascular injuries, for example, due to endoscopic repair by suturing, hide behind those events. Because of the nature of the JCQHC database, subsequent adverse events after major vascular injury would necessitate the submission of reports by each physician. In fact, we observed high frequencies of massive bleeding and vascular injury, especially in thoraco group death cases. In video-assisted thoracoscopic lung resection, the incidence of vascular injury was reported to be 2.9% to 8.2%,13–15 and the mortality was reported to be 1.4% to 1.5%.13,15,16 Such major vascular injuries might be an unavoidable part of surgery because surgeons take on more challenging cases after the accumulation of experience. To minimize those complications, surgeons should recognize again that (1) vascular injury could occur at the time of entry while inserting a Veress needle or the first trocar; (2) creating a good operative view, not restricted to tunnel vision, is mandatory for safe surgery; and (3) they should learn how to react to unexpected bleeding. As Decaluwe et al13 previously pointed out, it is very important for surgeons to develop the skill to recognize a dangerous situation before bleeding actually occurs and to decide on open conversion before devastating bleeding.
In the present study, 2 events of failure of medical equipment or devices caused vascular injuries that resulted in massive bleeding (endovascular gastrointestinal stapler: n = 1, endovascular clip device: n = 1). In real-world clinical practice, we suggest that there are many similar incidents of malfunction that go unreported. For example, Kwazneski et al17 reported in their survey to the minimally invasive program directors in the United States that most minimally invasive surgeons encountered laparoscopic linear stapler malfunction and 25% caused significant alterations of the planned surgery. Chan et al18 also reported that among 565 laparoscopic nephrectomies, gastrointestinal stapler device malfunction occurred in 10 cases (1.7%), the estimated blood loss ranged from 200 to 1200 mL, and transfusion was required in 3 cases.
In 2014, safety regarding advanced laparoscopic surgery became a major social concern in Japan because a series of postoperative deaths were reported in succession from 2 different hospitals, whereby 8 patients died within 4 months after laparoscopic liver surgery at 1 university hospital (http://www.gunma-u.ac.jp/wp-content/uploads/2015/08/H280730jikocho-saishu-a.pdf) and 11 patients undergoing advanced laparoscopic abdominal surgeries died after a short period of time at another cancer center between 2008 and 2014. Because these patient death events would be recorded in the JCQHC open database (we could not verify this because of the anonymous nature of each report), the number of patient death events might be biased, especially in laparoscopic liver surgery. However, those reports and our present observations reinforce the importance of the “safety-first” principle and transparency when proceeding with cutting-edge surgeries.
There were several limitations of the present study. First, because reporting behavior itself depends on each health care professional, the underreporting of near misses and minor postoperative complications that patients often experience but recover from with appropriate treatments is expected. For example, minor complications such as paralytic ileus after abdominal surgery would happen much more in daily clinical practice. However, we consider that unexpected errors such as foreign body retention or significant misidentification of anatomy, or severe complications, especially those which resulted in patient death, could be largely covered in the present database. Second, as described previously, the first author (T.A.) categorized all of the reports. Although the medical safety manager of our hospital (Y.N.) supervised the present analysis, subjective bias of categorization might still remain. Third, we simply analyzed the number of each incident reported. The risk of each event was unknown, because we did not know the total population for each procedure performed in the participating hospitals. Nevertheless, we consider that several important features of medical errors associated with minimally invasive surgery were demonstrated.
CONCLUSIONS
We observed the frequent incidents such as injury of other organs, retention of a foreign body, breakage or failure of medical equipment or devices, massive bleeding, misperception of anatomy, and vascular injury in minimally invasive surgery that surgeons should refamiliarize themselves with, and differences in the frequency between the laparo and thoraco group. Surgeons should keep in mind these characteristics. In addition, our study suggested novel risks inherent in recent sophisticated surgical instruments, which might cause the retention of tiny parts when breakage occurs outside the visual field, or the malfunctioning of instruments. A specialized checklist might reduce those incidents.
Supplementary Material
ACKNOWLEDGMENT
We appreciate the staff of the Japan Council for Quality Health Care for their continuing great work.
Footnotes
The authors disclose no conflict of interest.
This work was supported by a Grant-in-Aid for Scientific Research (C) (KAKENHI no. 26460853) from the Japan Society for the Promotion of Science.
Supplemental digital contents are available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal’s Web site (www.journalpatientsafety.com).
REFERENCES
- 1.Kohn LT, Corrigan J, Donaldson MS. To Err Is Human: Building a Safer Health System. Washington, DC: National Academy Press; 2000. xxi, 287 p. p. [PubMed] [Google Scholar]
- 2.Ferriman A. Laparoscopic surgery: two thirds of injuries initially missed. BMJ. 2000;321:784. [PMC free article] [PubMed] [Google Scholar]
- 3.Molloy D, Kaloo PD, Cooper M, et al. Laparoscopic entry: a literature review and analysis of techniques and complications of primary port entry. Aust N Z J Obstet Gynaecol. 2002;42:246–254. [DOI] [PubMed] [Google Scholar]
- 4.Munro MG. Laparoscopic access: complications, technologies, and techniques. Curr Opin Obstet Gynecol. 2002;14:365–374. [DOI] [PubMed] [Google Scholar]
- 5.Gawande AA, Studdert DM, Orav EJ, et al. Risk factors for retained instruments and sponges after surgery. N Engl J Med. 2003;348:229–235. [DOI] [PubMed] [Google Scholar]
- 6.Gonzalez-Ojeda A, Rodriguez-Alcantar DA, Arenas-Marquez H, et al. Retained foreign bodies following intra-abdominal surgery. Hepatogastroenterology. 1999;46:808–812. [PubMed] [Google Scholar]
- 7.Yasuhara H, Fukatsu K, Komatsu T, et al. Occult risk of broken instruments for endoscopy-assisted surgery. World J Surg. 2014;38:3015–3022. [DOI] [PubMed] [Google Scholar]
- 8.Gibbs VC. Retained surgical items and minimally invasive surgery. World J Surg. 2011;35:1532–1539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mathias JM. Focus shifts to device fragments, small miscellaneous items in RSIs. OR Manager. 2013;29:1 10–12. [PubMed] [Google Scholar]
- 10.Verdaasdonk EG, Stassen LP, Hoffmann WF, et al. Can a structured checklist prevent problems with laparoscopic equipment? Surg Endosc. 2008;22:2238–2243. [DOI] [PubMed] [Google Scholar]
- 11.Romain B, Chemaly R, Meyer N, et al. Value of a preoperative checklist for laparoscopic appendectomy and cholecystectomy. J Visc Surg. 2012;149:408–411. [DOI] [PubMed] [Google Scholar]
- 12.Montero PN, Robinson TN, Weaver JS, et al. Insulation failure in laparoscopic instruments. Surg Endosc. 2010;24:462–465. [DOI] [PubMed] [Google Scholar]
- 13.Decaluwe H, Petersen RH, Hansen H, et al. Major intraoperative complications during video-assisted thoracoscopic anatomical lung resections: an intention-to-treat analysis. Eur J Cardiothorac Surg. 2015;48:588–598. discussion 99. [DOI] [PubMed] [Google Scholar]
- 14.Mei J, Pu Q, Liao H, et al. A novel method for troubleshooting vascular injury during anatomic thoracoscopic pulmonary resection without conversion to thoracotomy. Surg Endosc. 2013;27:530–537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kawachi R, Tsukada H, Nakazato Y, et al. Morbidity in video-assisted thoracoscopic lobectomy for clinical stage I non-small cell lung cancer: is VATS lobectomy really safe? Thorac Cardiovasc Surg. 2009;57:156–159. [DOI] [PubMed] [Google Scholar]
- 16.Jawitz OK, Wang Z, Boffa DJ, et al. The differential impact of preoperative comorbidity on perioperative outcomes following thoracoscopic and open lobectomies. Eur J Cardiothorac Surg. 2017;51:169–174. [DOI] [PubMed] [Google Scholar]
- 17.Kwazneski D, 2nd, Six C, Stahlfeld K. The unacknowledged incidence of laparoscopic stapler malfunction. Surg Endosc. 2013;27:86–89. [DOI] [PubMed] [Google Scholar]
- 18.Chan D, Bishoff JT, Ratner L, et al. Endovascular gastrointestinal stapler device malfunction during laparoscopic nephrectomy: early recognition and management. J Urol. 2000;164:319–321. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


