Abstract
BACKGROUND
Female patients have historically received less aggressive lipid management than male patients. Contemporary care patterns and the potential causes for these differences are unknown.
METHODS
Examining the Patient and Provider Assessment of Lipid Management (PALM) Registry, a nationwide registry of outpatients with or at risk for atherosclerotic cardiovascular disease (ASCVD), we compared the use of statin therapy, guideline-recommended statin dosing, and reasons for under-treatment. We specifically analyzed sex differences in statin treatment and guideline-recommended statin dosing using multivariable logistic regression.
RESULTS
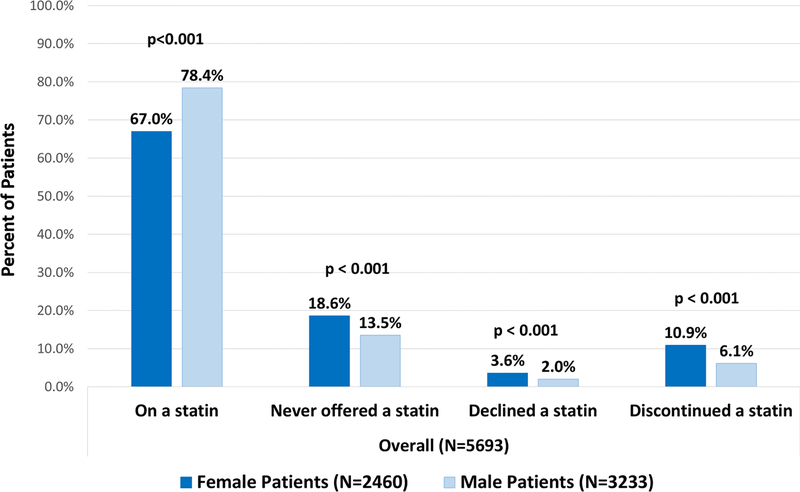
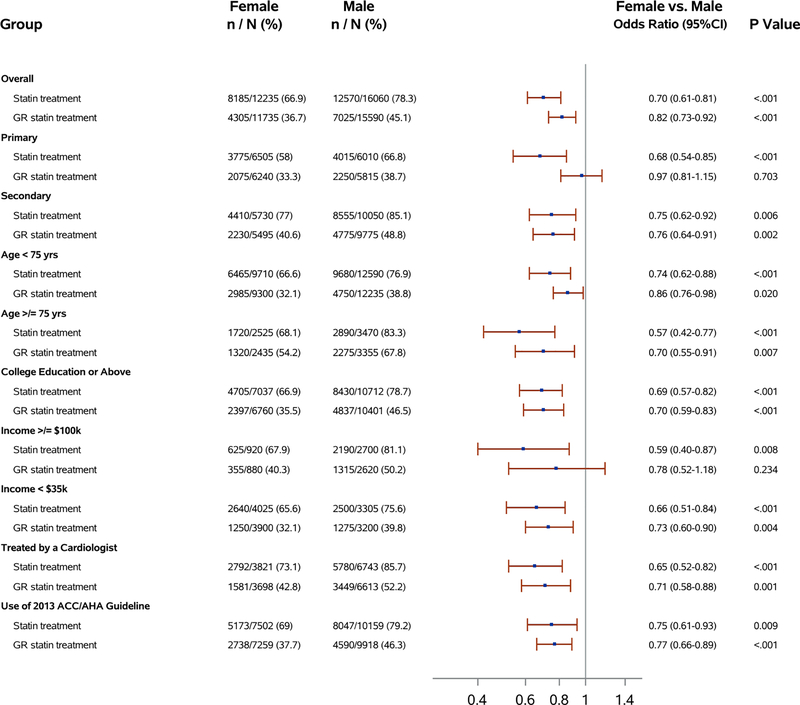
Among 5,693 participants (43% female) eligible for 2013 American College of Cardiology/American Heart Association cholesterol guideline-recommended statin treatment, females were less likely than males to be prescribed any statin therapy (67.0% vs. 78.4%, p<0.001) or to receive a statin at the guideline-recommended intensity (36.7% vs. 45.2%, p<0.001). Females were more likely to report having previously never been offered statin therapy (18.6% vs. 13.5%, p<0.001), declined statin therapy (3.6% vs. 2.0%, p<0.001), or discontinued their statin (10.9% vs. 6.1%, p<0.001). Females were also less likely than males to believe statins were safe (47.9% vs. 55.2%, p<0.001) or effective (68.0% vs. 73.2%, p<0.001) and more likely to report discontinuing their statin due to a side effect (7.9% vs. 3.6%, p<0.001). Sex differences in both overall and guideline-recommended intensity statin use persisted after adjustment for demographics, socioeconomic factors, clinical characteristics, patient beliefs, and provider characteristics (adjusted OR=0.70, 95% CI 0.61–0.81, p<0.001; and OR= 0.82, 95% CI 0.73–0.92, p<0.01, respectively). Sex differences were consistent across primary and secondary prevention indications for statin treatment.
CONCLUSIONS
Females eligible for statin therapy were less likely than males to be treated with any statin or guideline-recommended statin intensity. A combination of females being offered statin therapy less frequently, while declining and discontinuing treatment more frequently, accounted for these sex differences in statin use.
Keywords: statin therapy, sex, women, primary prevention, secondary prevention, treatment differences, Cardiovascular Disease, Women, Primary Prevention, Secondary Prevention, Epidemiology
Statin therapy reduces cardiovascular risk in both females and males.1–4 Nevertheless, sex differences in statin treatment and adherence to guideline-recommended lipid management are well-documented5–9. The reasons underlying lower statin utilization in women remain poorly understood and the degree to which these sex differences may be attributable to differences in patient perceptions, side effects, and differences in physician prescribing patterns, merits further investigation.
The Patient and Provider Assessment of Lipid Management (PALM) Registry is a United States (U.S.) registry of 7,938 individuals with atherosclerotic cardiovascular disease (ASCVD) or at high risk for ASCVD treated at 140 cardiology, primary care, and endocrinology outpatient practices. In addition to clinical, socioeconomic, and lipid data for all enrolled patients, the PALM Registry uniquely captured patient-reported side effects, patient perceptions and beliefs, and provider characteristics—all of which influence treatment use and adherence.10 In this study, we: 1) evaluated whether statin treatment differed between females and males; 2) assessed potential reasons underlying sex differences in statin treatment including side effects, beliefs, and provider characteristics; and 3) identified whether sex differences in guideline-recommended statin treatment persisted after adjustment for demographics, clinical characteristics, socioeconomic status, education, patient beliefs, and provider characteristics.
METHODS
Data Description – The PALM Registry
We set out to investigate sex differences in statin treatment using the PALM registry, a nationwide registry of individuals (n=7938) with ASCVD or at high risk for ASCVD enrolled between May 2015 and November 2015 in 140 U.S. community practices. The design and rationale for the PALM Registry have been described previously.10 Briefly, data regarding sex, socioeconomic status, education level, patient beliefs and perceptions, and statin use were acquired via patient surveys administered on an iPAD in PALM providers’ offices. Providers enrolling patients into the PALM Registry also completed surveys prior to beginning enrollment. Study coordinators at each site abstracted patient clinical data including demographics, medical history, and current statin dosing intensity. Lipid levels were measured in all patients at a core laboratory. Patients who met a guideline-recommendation for statin therapy based on the 2013 American College of Cardiology (ACC)/American Heart Association (AHA) Cholesterol Guideline1 and who completed the survey at enrollment (95.3% response rate) were included (n=5,693). The data, analytic methods, and study materials will not be made available to other researchers for purposes of reproducing the results or replicating the procedure. All study sites obtained institutional review board approval for participation in the PALM Registry and all study participants provided informed consent.
Data Definitions
ASCVD was defined as having a history of coronary artery disease (including prior myocardial infarction, coronary artery disease, coronary artery bypass grafting, and/or percutaneous coronary intervention), cerebrovascular disease (including prior stroke and/or transient ischemic attack), and peripheral artery disease (including prior abdominal aortic aneurysm, peripheral arterial disease, carotid artery stenosis, and/or non-coronary arterial revascularization). Patients were recommended for high-intensity statin therapy if they met one or more of the following criteria: 1) history of ASCVD and aged ≤75 years old; 2) low-density lipoprotein cholesterol (LDL-C) ≥190 mg/dL; or 3) adults aged 40–75 years with diabetes and 10-year ASCVD risk ≥7.5% based on the pooled cohort equation with LDL-C ≥70 mg/dL (if not on a statin) or irrespective of LDL-C if already on a statin at the time of enrollment.1 Patients not meeting criteria for a high-intensity statin qualified for a moderate-intensity statin if they met one or more of the following: 1) history of ASCVD and >75 years old; 2) adults aged 40–75 years without diabetes with ASCVD risk ≥7.5% and LDL-C >70 mg/dL or already on a statin; or 3) adults aged 40–75 years with diabetes and 10-year ASCVD risk <7.5% with LDL-C ≥70mg/dL or already on a statin.
Statistical Analysis
We assessed sex differences in statin treatment patterns including statin use and high-intensity statin use in the overall population, as well as within primary and secondary prevention subgroups. Statin intensity was defined according to definitions from the 2013 ACC/AHA Cholesterol Guideline1. We described sex differences in baseline characteristics, lipid levels, provider characteristics, patient beliefs about statins and cardiovascular disease, patient-reported side effects, and willingness to try statin therapy. We compared females and males by statin treatment overall and guideline-recommended statin intensity, as well as frequency of not being on a statin due to: 1) prior discontinuation; 2) patient preference (i.e., patient declined statin therapy); or 3) never being offered a statin. Categorical variables were presented as frequencies and continuous variables presented as medians with interquartile range. We assessed differences by sex in categorical variables using the Pearson chi-square test and assessed differences by sex in continuous variables using the Wilcoxon rank-sum test. A two-sided p-value less than 0.05 was considered statistically significant.
We evaluated the relationship between sex and statin use (both overall and at guideline- recommended intensity) using logistic regression analysis. We adjusted for the following potential confounders: demographics including age and race; clinical, socioeconomic, and educational factors including prior coronary artery disease, cerebrovascular disease and peripheral arterial disease, diabetes, obesity, smoking, hypertension, heart failure, yearly income, insurance status, education level, patient numeracy, pertinent patient beliefs and perceptions including worry about heart disease, physician trust, patient’s statin beliefs about safety, effectiveness and the link between high cholesterol and heart attack risk; and provider factors including cardiologist vs. non-cardiologist, use of 2013 ACC/AHA guideline, urban vs. rural setting, and provider time in practice. We measured patient numeracy using the subjective numeracy score, a previously validated instrument.11 The generalized estimating equation (GEE) was used to account for clustering of patients within sites. We also evaluated the unadjusted and adjusted odds ratio (OR; 95% confidence interval [CI]) of guideline-recommended statin treatment to examine the sex difference in outcomes in the following subgroups: 1) patients with a primary prevention indication; 2) patients with a secondary prevention indication; 3) patients < or ≥ 75 years old; 4) education college or above; 5) income >$100,000/year; 6) income <$35,000/year; 7) patients treated by cardiologists; and 8) patients treated by a provider who reports using the ACC/AHA guideline. Income was self-reported and missing income data were imputed using 2014 median household income based on patient residence zip code or enrolling site zip code. Multiple imputation was used for all other variables with fully conditional specification approach to impute missing values for covariates with missing data (maximum missing 11.7%) 12. Five imputed datasets were used for multivariable analysis. All analyses were performed using SAS version 9.4 (SAS Institute, Inc., Cary, NC).
RESULTS
Baseline Characteristics
Among 5,693 patients with a 2013 ACC/AHA cholesterol guideline indication for statin treatment, 2,460 (43%) were female. Baseline characteristics differed significantly between female and male patients (Table 1). Compared with males, females were more frequently black, had higher body mass index (BMI), were less likely to have a history of ASCVD, had lower 10- year risk among those without ASCVD, had lower tobacco use, and had higher lipid levels than male patients. Females also more frequently had Medicare and Medicaid with less private insurance, a lower yearly income, and were less likely to be seen by a cardiologist than males (51.9% vs. 65.2%, p<0.001).
Table 1.
Baseline Characteristics by Sex (n=5693)*
| Overall (n=5693) | Primary Prevention (n=2509) | Secondary Prevention (n=3184) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Female Patients (n=2460) | Male Patients (n=3233) | p- value | Female Patients (n=1303) | Male Patients (n=1206) | p-value | Female Patients (n=1157) | Male Patients (n=2027) | p- value | |
| Age (median) | 68.0 (62.0–73.0) | 68.0 (61.0–73.0) | 0.07 | 67.0 (59.0–71.0) | 64.0 (58.0–69.0) | <.001 | 71.0 (64.0–78.0) | 70.0 (63.0–76.0) | 0.005 |
| Race | |||||||||
| White | 1,991 (80.9%) | 2,810 (86.9%) | <.001 | 1,029 (79.0%) | 978 (81.1%) | 0.12 | 962 (83.1%) | 1,832 (90.4%) | <.001 |
| Black | 415 (16.9%) | 349 (10.8%) | 248 (19.0%) | 196 (16.3%) | 167 (14.4%) | 153 (7.5%) | |||
| Other/unknown | 54 (2.2%) | 74 (2.3%) | 26 (2.0%) | 32 (2.7%) | 28 (2.4%) | 42 (2.1%) | |||
| Hispanic | 303 (12.3%) | 323 (10.0%) | 0.006 | 211 (16.2%) | 192 (15.9%) | 0.85 | 92 (8.0%) | 131 (6.5%) | 0.12 |
| 10-year risk (among those w/out ASCVD) | 12.3 (8.4–17.8) | 17.5 (11.6–25.4) | <.001 | 12.3 (8.4–17.8) | 17.5 (11.6–25.4) | <.001 | N/A | N/A | |
| ASCVD | 1,157 (47.0%) | 2,027 (62.7%) | <.001 | N/A | N/A | 1,157 (100.0%) | 2,027 (100.0%) | ||
| Coronary artery disease | 864 (35.1%) | 1,767 (54.7%) | <.001 | N/A | N/A | 864 (74.7%) | 1,767 (87.2%) | <.001 | |
| Cerebrovascular disease | 223 (9.1%) | 260 (8.0%) | 0.17 | N/A | N/A | 223 (19.3%) | 260 (12.8%) | <.001 | |
| Other ASCVD | 404 (16.4%) | 642 (19.9%) | <.001 | N/A | N/A | 404 (34.9%) | 642 (31.7%) | 0.06 | |
| Diabetes | 1,192 (48.5%) | 1,371 (42.4%) | <.001 | 705 (54.1%) | 599 (49.7%) | 0.03 | 487 (42.1%) | 772 (38.1%) | 0.03 |
| Hypertension | 2,010 (81.7%) | 2,632 (81.4%) | 0.78 | 1,013 (77.7%) | 915 (75.9%) | 0.27 | 997 (86.2%) | 1,717 (84.7%) | 0.26 |
| Heart failure | 213 (8.8%) | 344 (10.7%) | 0.02 | 42 (3.3%) | 39 (3.3%) | 0.99 | 171 (15.0%) | 305 (15.2%) | 0.88 |
| History of myopathy | 83 (3.4%) | 135 (4.2%) | 0.12 | 19 (1.5%) | 28 (2.3%) | 0.11 | 64 (5.5%) | 107 (5.3%) | 0.77 |
| Chronic kidney disease | 221 (9.0%) | 362 (11.2%) | 0.006 | 78 (6.0%) | 94 (7.8%) | 0.07 | 143 (12.4%) | 268 (13.2%) | 0.49 |
| Menopausal (if female) | 2,123 (89.8%) | N/A | 1,065 (85.8%) | N/A | 1,058 (94.3%) | N/A | |||
| BMI ≥30 kg/m2 | 1,281 (52.3%) | 1,550 (48.2%) | 0.002 | 741 (57.1%) | 623 (52.1%) | 0.01 | 540 (46.9%) | 927 (45.9%) | 0.60 |
| Smoking status | |||||||||
| Current smoker | 254 (10.5%) | 391 (12.3%) | <.001 | 139 (11.0%) | 166 (14.1%) | <.001 | 115 (10.0%) | 225 (11.2%) | <.001 |
| Quit/former smoker | 881 (36.5%) | 1,589 (49.9%) | 412 (32.5%) | 492 (41.8%) | 469 (41.0%) | 1,097 (54.7%) | |||
| Never smoked | 1,276 (52.9%) | 1,202 (37.8%) | 715 (56.5%) | 520 (44.1%) | 561 (49.0%) | 682 (34.0%) | |||
| College or above | 1,390 (58.1%) | 2,121 (67.0%) | <.001 | 725 (57.9%) | 797 (68.2%) | <.001 | 665 (58.3%) | 1,324 (66.2%) | <.001 |
| Insurance | |||||||||
| Private | 1,326 (55.2%) | 1,981 (62.6%) | <.001 | 719 (56.9%) | 745 (63.7%) | <.001 | 607 (53.3%) | 1,236 (61.9%) | <.001 |
| Medicare | 1,548 (64.5%) | 1,877 (59.3%) | <.001 | 747 (59.2%) | 561 (48.0%) | <.001 | 801 (70.3%) | 1,316 (65.9%) | 0.01 |
| Medicaid | 305 (12.7%) | 306 (9.7%) | <.001 | 160 (12.7%) | 105 (9.0%) | 0.003 | 145 (12.7%) | 201 (10.1%) | 0.02 |
| No insurance | 54 (2.2%) | 68 (2.1%) | 0.80 | 36 (2.9%) | 40 (3.4%) | 0.42 | 18 (1.6%) | 28 (1.4%) | 0.69 |
| Other | 59 (2.5%) | 74 (2.3%) | 0.77 | 24 (1.9%) | 25 (2.1%) | 0.68 | 35 (3.1%) | 49 (2.5%) | 0.30 |
| Income | |||||||||
| <35,000 | 740 (31.4%) | 607 (19.5%) | <.001 | 370 (29.9%) | 228 (19.8%) | <.001 | 370 (33.0%) | 379 (19.3%) | <.001 |
| 35,000–74,999 | 467 (19.8%) | 764 (24.5%) | 278 (22.5%) | 306 (26.6%) | 189 (16.9%) | 458 (23.3%) | |||
| 75,000–99,999 | 135 (5.7%) | 287 (9.2%) | 85 (6.9%) | 111 (9.7%) | 50 (4.5%) | 176 (9.0%) | |||
| ≥100,000 | 178 (7.6%) | 537 (17.2%) | 114 (9.2%) | 217 (18.9%) | 64 (5.7%) | 320 (16.3%) | |||
| Don’t know or refused | 837 (35.5%) | 920 (29.5%) | 390 (31.5%) | 288 (25.0%) | 447 (39.9%) | 632 (32.2%) | |||
| Seen by a cardiologist | 1,248 (51.9%) | 2,070 (65.2%) | <.001 | 366 (29.0%) | 356 (30.3%) | 0.50 | 882 (77.1%) | 1,714 (85.7%) | <.001 |
| Seen by an endocrinologist | 499 (20.7%) | 547 (17.2%) | <.001 | 276 (21.9%) | 226 (19.2%) | 0.11 | 223 (19.5%) | 321 (16.1%) | 0.01 |
| Time in practice (>5 years) | 2,022 (91.3%) | 2,612 (91.6%) | 0.75 | 1,073 (91.8%) | 986 (92.8%) | 0.35 | 949 (90.8%) | 1,626 (90.8%) | 0.98 |
| Provider use of 2013 ACC/AHA Guideline | 1,388 (62.7%) | 1,852 (64.9%) | 0.099 | 677 (57.9%) | 593 (55.8%) | 0.32 | 711 (68.0%) | 1,259 (70.3%) | 0.20 |
| Total cholesterol mg/dL (on treatment) | 171.0 (150.0–196.0) | 151.0 (131.0–175.0) | <.001 | 176.0 (154.0–202.0) | 163.0 (140.0–189.0) | <.001 | 167.0 (145.0–191.0) | 146.0 (128.0–168.0) | <.001 |
| LDL-C mg/dL (on treatment) | 91.0 (73.0–113.0) | 82.0 (66.0–102.0) | <.001 | 96.0 (77.0–117.0) | 92.0 (73.0–114.0) | 0.007 | 88.0 (71.0–108.0) | 78.0 (63.0–96.0) | <.001 |
| LDL-C mg/dL (overall) | 101.0 (80.0–129.0) | 88.0 (69.0–113.0) | <.001 | 109.0 (86.0–135.0) | 101.0 (81.0–126.0) | <.001 | 94.0 (74.0–122.0) | 81.0 (65.0–102.0) | <.001 |
| LDL-C <70 mg/dL (on treatment) | 331 (20.3%) | 767 (30.5%) | <.001 | 127 (16.8%) | 170 (21.1%) | 0.03 | 204 (23.3%) | 597 (35.0%) | <.001 |
| LDL-C <70 mg/dL (overall) | 360 (14.7%) | 807 (25.1%) | <.001 | 134 (10.3%) | 177 (14.7%) | <.001 | 226 (19.8%) | 630 (31.4%) | <.001 |
| HDL-C mg/dL (on statin) | 56.0 (46.0–68.0) | 47.0 (39.0–56.0) | <.001 | 56.0 (47.0–68.0) | 47.0 (40.0–56.0) | <.001 | 56.0 (46.0–67.0) | 47.0 (39.0–55.0) | <.001 |
ACC/AHA indicates American College of Cardiology/American Heart Association; ASCVD, atherosclerotic cardiovascular disease; BMI, body mass index; HDL-C, high- density lipoprotein cholesterol; LDL-C, low-density lipoprotein cholesterol
Data are presented as median [IQR] for continuous variables and n (%) for categorical variables
All percentages calculated as the percent of non-missing values.
Statin Use and Dosing Intensity
Compared with males, females were significantly less likely to be on a statin (67.0% vs. 78.4%, p<0.001) or, if on a statin, were less likely to be on guideline-recommended statin intensity (36.7% vs. 45.2%, p<0.001) (Table 2; Figure 1). Females were more likely to report never having been offered a statin (18.6% vs. 13.5%, p<0.001), previously discontinuing a statin (10.9% vs. 6.1%, p<0.001), or previously declining a statin (3.6% vs. 2.0%, p<0.001) (Figure 1). Trends were similar among patients eligible for statin therapy based on a primary or secondary prevention indication. Sex differences in statin use were identified in three of the four primary statin treatment groups identified in the guideline: individuals with diabetes, those with 10-year ASCVD risk ≥7.5%, and those with ASCVD (eTable 1). We did not observe significant sex differences in statin use in the limited sample of individuals with LDL-C≥190 mg/dL. When considering only untreated patients (33.0% of females, 21.6% of males), the relative distribution of reasons for not being treated were as follows: untreated females reported never being offered therapy less frequently than untreated males (56.2% vs. 62.6%, p=0.01), with similar rates of declining statins (10.9% vs. 9.2%, p=0.25) and discontinuing statins (32.8% vs. 28.2%, p=0.05).
Table 2.
Statin Treatment Characteristics by Sex (N=5693)
| Overall (n=5693) | Primary Prevention (n=2509) | Secondary Prevention (n=3184) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Female Patients (n=2460) | Male Patients (n=3233) | p- value | Female Patients (n=1303) | Male Patients (n=1206) | p- value | Female Patients (n=1157) | Male Patients (n=2027) | p- value | |
| On any statin | 1,647 (67.0%) | 2,535 (78.4%) | <.001 | 757 (58.1%) | 807 (66.9%) | <.001 | 890 (76.9%) | 1,728 (85.2%) | <.001 |
| On guideline-intensity statin | 866 (36.7%) | 1,418 (45.2%) | <.001 | 415 (33.2%) | 453 (38.8%) | 0.004 | 451 (40.6%) | 965 (49.0%) | <.001 |
| Statin intensity at visit | |||||||||
| Not on statin | 813 (34.5%) | 698 (22.2%) | <.001 | 546 (43.7%) | 399 (34.2%) | <.001 | 267 (24.1%) | 299 (15.2%) | <.001 |
| On low-intensity statin | 163 (6.9%) | 193 (6.2%) | 84 (6.7%) | 75 (6.4%) | 79 (7.1%) | 118 (6.0%) | |||
| On moderate-intensity statin | 981 (41.6%) | 1,386 (44.2%) | 489 (39.2%) | 530 (45.4%) | 492 (44.3%) | 856 (43.4%) | |||
| On high-intensity statin | 402 (17.0%) | 861 (27.4%) | 130 (10.4%) | 163 (14.0%) | 272 (24.5%) | 698 (35.4%) | |||
| Previously on statin, discontinued | 267 (10.9%) | 197 (6.1%) | <.001 | 143 (11.0%) | 79 (6.6%) | <.001 | 124 (10.7%) | 118 (5.8%) | <.001 |
| Offered a statin, declined | 89 (3.6%) | 64 (2.0%) | <.001 | 63 (4.8%) | 32 (2.7%) | 0.004 | 26 (2.2%) | 32 (1.6%) | 0.18 |
| Never offered a statin | 457 (18.6%) | 437 (13.5%) | <.001 | 340 (26.1%) | 288 (23.9%) | 0.20 | 117 (10.1%) | 149 (7.4%) | 0.007 |
| On a non-statin lipid-lowering therapy | 639 (26.0%) | 953 (29.5%) | 0.004 | 311 (23.9%) | 315 (26.1%) | 0.19 | 328 (28.3%) | 638 (31.5%) | 0.07 |
All percentages calculated as the percent of non-missing values.
Figure 1. Statin Utilization in Female vs. Male Patients.
This figure displays statin utilization in male and female patients according to percentages on a statin, never offered a statin, declined a statin, and discontinued a statin.
Patient Perceptions and Beliefs
Females and males differed in terms of their beliefs and perceptions surrounding statins and cardiovascular disease (Table 3). Females more frequently stated that they either occasionally or often worry about heart attack or stroke (45.7% vs. 34.4% p<0.001), yet were less likely to believe that people with high cholesterol are more likely to have a heart attack (75.4% vs. 82.1%, p<0.001). Females were less likely than males to agree with the statements that statins are effective (68.0% vs. 73.2%, p<0.001) and statins are safe (47.9% vs. 55.2%, p<0.001). Females were also more likely to report believing that statins can cause diabetes, muscle symptoms, and liver damage (Table 3). Physician trust was similar between female and males (65.9% vs. 64.5%, p=0.29).
Table 3.
Sex Differences in Patient Beliefs and Perceptions about Statins, Cholesterol and Heart Disease in the PALM Registry
| Overall (n=5693) | Primary Prevention (n=2509) | Secondary Prevention (n=3184) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Female Patients | Male Patients | p- value | Female Patients | Male Patients | p- value | Female Patients | Male Patients | p- value | |
| Physician trust and risk perception | |||||||||
| Trust in physician (% completely) | 1,593 (65.9%) | 2,056 (64.5%) | 0.29 | 822 (64.6%) | 711 (60.2%) | 0.02 | 771 (67.3%) | 1,345 (67.1%) | 0.93 |
| Worry about heart attack or stroke (% often or occasionally) | 1,030 (45.7%) | 1,037 (34.4%) | <.001 | 504 (43.0%) | 339 (30.9%) | <.001 | 526 (48.7%) | 698 (36.4%) | <.001 |
| Perceived risk worse than peers | 845 (35.3%) | 1,097 (34.8%) | 0.68 | 400 (31.8%) | 323 (27.8%) | 0.04 | 445 (39.3%) | 774 (38.9%) | 0.81 |
| Believe people w/high cholesterol more likely to have heart attack (% agree to strongly agree) | 1,702 (75.4%) | 2,481 (82.1%) | <.001 | 900 (76.1%) | 898 (81.7%) | 0.001 | 802 (74.5%) | 1,583 (82.3%) | <.001 |
| Don’t need to worry if never had heart attack (% agree to strongly agree) | 201 (9.4%) | 278 (9.6%) | 0.80 | 99 (8.8%) | 103 (9.8%) | 0.46 | 102 (9.9%) | 175 (9.4%) | 0.68 |
| Statin-reported beliefs | |||||||||
| What percentage of patients responded “agree” or “strongly agree” to the following statements? | |||||||||
| Statins are effective in reducing the risk of heart disease and stroke | 1,481 (68.0%) | 2,154 (73.2%) | <.001 | 745 (65.8%) | 721 (67.6%) | 0.38 | 736 (70.4%) | 1,433 (76.4%) | <.001 |
| Statins are safe medications | 1,021 (47.9%) | 1,598 (55.2%) | <.001 | 507 (45.6%) | 552 (52.7%) | <.001 | 514 (50.3%) | 1,046 (56.7%) | 0.001 |
| Statins can cause diabetes | 176 (8.3%) | 183 (6.4%) | 0.01 | 83 (7.5%) | 64 (6.1%) | 0.22 | 93 (9.2%) | 119 (6.5%) | 0.010 |
| Statins can cause muscle aches/pain | 992 (46.3%) | 1,129 (39.1%) | <.001 | 471 (42.2%) | 359 (34.4%) | <.001 | 521 (50.8%) | 770 (41.7%) | <.001 |
| Statins can cause liver damage | 742 (35.0%) | 829 (28.8%) | <.001 | 362 (32.6%) | 279 (26.8%) | 0.003 | 380 (37.5%) | 550 (29.9%) | <.001 |
| Statins can cause memory loss | 295 (13.9%) | 371 (12.9%) | 0.32 | 141 (12.7%) | 117 (11.3%) | 0.31 | 154 (15.2%) | 254 (13.8%) | 0.33 |
Data represent the percentage of subjects who responded “agree” or “strongly agree” on a five point Likert scale to the patient survey question.
All percentages calculated as the percent of non-missing values.
Patient Reported Symptoms and Willingness to Reattempt Statin
Many females (50.1%) and males (43.1%) currently using statins reported some type of adverse symptoms associated with statin use. Relatively few (5.3%) reported stopping their statin due to side effects, but females were more likely to discontinue statin therapy than males (7.9% vs. 3.6%, p<0.001) (Table 4). Among former statin users, females most frequently listed side effects as a reason for stopping (150 out of 267 former users, 56.2%). Among current statin users, those on a high-intensity statins, and former statin users, females were more likely than males to report previously experiencing a side effect when on statins (Table 4). Compared with males, females previously on a statin were less willing to try another statin.
Table 4.
Statin-Related Perceived Side Effects* and Willingness for Therapy
| Overall (n=5693) | |||
|---|---|---|---|
| Female Patients (n=2460) | Male Patients (n=3233) | p-value | |
| Current statin users | n=1647 | n=2535 | |
| Experienced any side effect (among all statin users) | 774 (50.1%) | 1,020 (43.1%) | <.001 |
| Experienced any side effect (among high-intensity statin users) | 201 (52.8%) | 351 (43.6%) | 0.003 |
| Former statin users | n=267 | n=197 | |
| Stopped due to side effect* | 150 (7.9%) | 98 (3.6%) | <.001 |
| Willingness to try another statin | |||
| Not at all or unlikely | 86 (35.2%) | 49 (26.6%) | 0.03 |
| Possibly | 44 (18.0%) | 55 (29.9%) | |
| Very likely or almost certainly | 104 (42.6%) | 74 (40.2%) | |
| Do not know | 10 (4.1%) | 6 (3.3%) | |
% represents the percentage of patients ever on a statin
All percentages calculated as the percent of non-missing values.
Statin Use after Multivariable Adjustment
After adjustment for relevant demographic-, clinical-, socioeconomic-, belief-, and provider- related confounders, females remained less likely to receive any statin (OR 0.70, 95% CI 0.61– 0.81, p<0.001) or a guideline-recommended statin (OR 0.82, 95% CI 0.73–0.92, p<0.001) (Figure 2). Adjusted ORs for all variables included in the final models are provided in the Supplemental Material (eTables 2 and 3). When evaluated within key subgroups, including primary prevention, secondary prevention, age < and ≥75 years, patients with college education or above, income ≥$100,000/year, income <$35,000/year, those treated by cardiologists, and those treated by providers following the ACC/AHA guideline, females remained less likely to be treated with a statin than males in all subgroups (Figure 2). Females were also less likely to receive guideline-recommended statin dosing compared with males in all subgroups on unadjusted analysis, though these trends were no longer statistically significant after adjustment in the primary prevention and high-income (≥$100,000) subgroups (Figure 2).
Figure 2. Multivariable Modelling Results for Statin Utilization in Female vs. Male Patients.
Based on results of a logistic regression model that included age, race, prior ASCVD grouped into CAD, CVD and PAD, diabetes, obesity, smoking, hypertension, heart failure, yearly income, insurance status, education level, patient numeracy, patient beliefs including worry about heart disease, physician trust, statin beliefs about safety, effectiveness and the link between high cholesterol and heart attack risk, cardiologist vs. non-cardiologist, use of 2013 ACC/AHA guideline, urban vs. rural setting, and provider time in practice. In subgroup analyses, the variable that defined the subgroup was not adjusted for except in the secondary prevention group where type of ASCVD was included in the model (CAD vs. CVD vs. PAD).
ACC = American College of Cardiology; AHA = American Heart Association; ASCVD, atherosclerotic cardiovascular disease; CAD = coronary artery disease; CVD = cerebrovascular disease; CI = confidence interval; GR = guideline-recommended; PAD = peripheral vascular disease
DISCUSSION
In a large sample of US adults seen in contemporary community practice, we found that females were less likely than males to receive guideline-recommended statin therapy. There appears to be several reasons for these sex related differences in statin use: Females were less likely to report having been offered statin therapy, more likely to decline statin therapy when offered, and more likely to discontinue statin therapy after starting. These sex differences in statin treatment in PALM were consistent by a number of different subgroups that were analyzed, including indication (primary vs. secondary prevention), education, income, and provider type.
Prior studies have demonstrated similar sex related differences in statin treatment across a variety of study populations.5–7, 13–15 However, these prior studies had not investigated the underlying causes for these care differences. We found that the biggest contributor to sex differences in statin use was the difference in the proportion of patients offered a statin by their physician. Among those recommended for statins, 18.6% of females reported that they had never been offered a statin by their physician vs. 13.5% of males; clinical differences did not explain this gap. Although females patients had less ASCVD and slightly lower 10-year calculated ASCVD risk scores, all of those included in the analysis met guideline indications for statin therapy.1 Furthermore, sex differences in statin utilization persisted even after adjusting for clinical characteristics and when we reanalyzed our results by those with ASCVD vs. not.
Some have suggested that differences in statin use may be explained by insurance status or other socioeconomic factors.13 In the PALM Registry, we found that female patients were less likely to be privately insured, had lower annual household incomes, and were less likely to be seen by a cardiologist than male patients. However, even after adjusting for sociodemographic characteristics such as age, insurance status, education, numeracy, and income, female patients remained significantly less likely to receive statin treatment and ACC/AHA guideline- recommended statin intensity.
The PALM Registry was also unique in its ability to examine the degree to which patient beliefs may have contributed to sex differences in statin utilization. Our findings are consistent with what was found in The Understanding Statin Use in America and Gaps in Patient Education (USAGE) internet-based survey, which found in 2011 that female patients were more likely to report stopping or switching their statin than male patients, frequently due to muscle related complaints15. This work extends the finding of USAGE as it included chart reviews for clinical data, core lab lipid panels, and included patients seen in routine clinical practice. In PALM, we found that females were more likely than males to decline statin therapy. While a small sample size and significant missingness limited our ability to consider patient-reported reasons for declining statin therapy by sex, a recent analysis of the overall PALM population demonstrated that patients declining statin therapy frequently cited worries about side effects (36.8%), preference for diet/exercise (25.0%), and a preference for natural remedies (16.0%) among reasons for declining statins16. When surveyed we also found that females were less likely to believe statins were safe or effective compared with males. Similarly, females were more likely to experience perceived statin-associated side effects and discontinue therapy due to side effects than males. Male patients, both among those patients previously on a statin and among statin naïve patients, were more willing to try a statin. Nonetheless, differences in rates of adults declining statins or discontinuing statins explained only about half of the 11% absolute difference in statin utilization.
Importantly, we examined reasons for lack of statin utilization among all potentially eligible patients, not just those who were untreated. Had we only evaluated patients who were not on a statin, sex-based differences would have appeared artificially attenuated. Among those not on statins, females were less likely to report never being offered a statin than males, with no difference by sex in the relative proportions of untreated males and females who discontinued or declined a statin. However, at a population level, among those eligible for statins, females were more likely than males to report all three reasons for non-treatment (never being offered, discontinued and declining a statin), contributing to large population-level differences in overall statin use.
Since it appears that both provider- and patient factors contribute to sex related differences in statin use, addressing these differences will likely require a multipronged approach. On the provider side, national performance metric systems have been demonstrated to improve the use of evidence-based medications in several conditions. While we found greater statin underuse in females than males, care gaps existed for both. Therefore, we believe that overall quality improvement efforts could bridge these gaps, regardless of patient sex. In addition to provider-directed efforts, our study importantly identified differences in patient beliefs that need to be addressed. For example, women had less belief than men in the safety and effectiveness of statins, which likely contributed to higher rates of patient refusal and/or discontinuation in women. Consequently, focused campaigns that emphasize the risk of ASCVD in women as well as the need for effective prevention could be quite helpful. The AHA “Go Red for Women” campaign represents one past highly successful effort, focusing on cardiovascular disease prevention in female patients.17–19 While the success of this initiative reassures us that progress is possible, the sex differences in statin treatment observed in our study emphasize that more work remains to be done.
Our study had some limitations. First, the PALM Registry was observational in nature; therefore, we cannot determine direct causality based on the associations detected. Second, our study did not capture provider reasoning for statin prescribing (or non-prescribing) in specific patients. Finally, the history of being offered a statin and the reasons for statin discontinuation were based on patient-report and, as a result, could be limited by recall bias. This being said, there are no reasons to believe recall bias should differentially affect women vs. men.
CONCLUSIONS
We observed that sex differences in statin treatment continue to persist in contemporary practice. Females were less likely to receive statins or guideline-recommended statin intensity, even after correcting for demographic, socioeconomic, and clinical confounders. These care differences appear to be due to females reporting being offered a statin by their physician less commonly and females reporting refusing or discontinuing their statin more frequently. Sex related differences in patient beliefs about statins and cholesterol may have further contributed to these care differences. Patients and providers alike must be educated on the safety and efficacy of statin therapy in order to optimize therapeutic efforts.
Supplementary Material
WHAT IS KNOWN
Statin therapy reduces cardiovascular risk in both females and males, but sex differences in statin use are well-documented.
The driving forces underlying sex differences in statin utilization are poorly understood.
WHAT THE STUDY ADDS
Sex differences in statin treatment persist in contemporary practice, with females remaining less likely to receive statins or guideline-recommended statin intensity.
These sex differences in statin use are due to females being offered statins at lower rates by their healthcare providers, while also refusing or discontinuing statins more often.
Variability in patient beliefs about statins and cholesterol may further contribute to the treatment heterogeneity observed.
ACKNOWLEDGMENTS
We thank Erin Campbell, MS, for her editorial contributions to this manuscript. Ms. Campbell did not receive compensation for her contributions, apart from her employment at the institution where this study was conducted.
SOURCES OF FUNDING
This study was supported by Sanofi Pharmaceuticals and Regeneron Pharmaceuticals. Dr. Navar is also funded by NIH K01HL133416-01. Dr. Nanna is also supported by NIH training grant T- 32-HL069749-15.
CONFLICT OF INTEREST DISCLOSURES
TY Wang reports receiving research grants from Amgen, Bristol Myers Squibb, Cryolife, Novartis, Pfizer, and Portola (all modest) and AstraZeneca, Regeneron Pharmaceuticals (both significant), and honoraria from Grifols and Gilead (modest). AC Goldberg reports receiving research grants from Amarin, Amgen, and Pfizer (all modest), and Regeneron, Regeneron/Sanofi, and IONIS (all significant), receiving honoraria from Merck Manual (modest), and is a consultant or advisory board member for Regeneron/Sanofi, Esperion, Novartis, and AKCEA (all modest). JG Robinson reports receiving research grants from Acasti, Amarin, Amgen, Astra-Zeneca, Esai, Merck, Novartis, Pfizer, Regeneron/Sanofi, Takeda (all significant), and is a consultant or advisory board member for Amgen, Merck, Novartis, Novo-Nordisk, Pfizer (all modest), and Sanofi and Regeneron (both significant). SS Virani reports receiving research grants from AHA, ADA, VA (all significant), and honoraria from the American College of Cardiology (significant), Associate Editor for Innovations, acc.org. MJ Louie: reports employment with Regeneron (significant) and ownership interest in Regeneron (modest). A Koren: reports employment with Sanofi (significant). ED Peterson reports receiving research grants from Amgen, Sanofi, Astrazeneca, Merck (all significant), and is a consultant or advisory board member for Amgen (modest), AstraZeneca, Merck, and Sanofi Aventis (all significant). AM Navar: reports receiving research grants from Amarin, Janssen, Amgen, Sanofi, and Regeneron Pharmaceuticals (all significant), and is a consultant or advisory board member for Amarin, Amgen, Novonordisk, AstraZeneca, Sanofi and Regeneron (all significant).
REFERENCES
- 1.Stone NJ, Robinson JG, Lichtenstein AH, Bairey Merz CN, Blum CB, Eckel RH, Goldberg AC, Gordon D, Levy D, Lloyd-Jones DM, McBride P, Schwartz JS, Shero ST, Smith SC Jr.,Watson K, Wilson PW, Eddleman KM, Jarrett NM, LaBresh K, Nevo L, Wnek J, Anderson JL, Halperin JL, Albert NM, Bozkurt B, Brindis RG, Curtis LH, DeMets D, Hochman JS, Kovacs RJ, Ohman EM, Pressler SJ, Sellke FW, Shen WK, Smith SC Jr, Tomaselli GF. 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2014;129:S1–45. [DOI] [PubMed] [Google Scholar]
- 2.Cholesterol Treatment Trialists’ (CTT) Collaborators, Mihaylova B, Emberson J, Blackwell L, Keech A, Simes J, Barnes EH, Voysey M, Gray A, Collins R, Baigent C. The effects of lowering LDL cholesterol with statin therapy in people at low risk of vascular disease: meta-analysis of individual data from 27 randomised trials. Lancet. 2012;380:581–590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Taylor F, Ward K, Moore TH, Burke M, Davey Smith G, Casas JP, Ebrahim S. Statins for the primary prevention of cardiovascular disease. Cochrane Database Syst Rev. 2011:CD004816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cholesterol Treatment Trialists’ (CTT) Collaboration, Fulcher J, O’Connell R, Voysey M, Emberson J, Blackwell L, Mihaylova B, Simes J, Collins R, Kirby A, Colhoun H, Braunwald E, La Rosa J, Pedersen TR, Tonkin A, Davis B, Sleight P, Franzosi MG, Baigent C, Keech A. Efficacy and safety of LDL-lowering therapy among men and women: meta-analysis of individual data from 174,000 participants in 27 randomised trials. Lancet. 2015;385:1397–1405. [DOI] [PubMed] [Google Scholar]
- 5.Writing Group Members, Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, Cushman M, Das SR, de Ferranti S, Despres JP, Fullerton HJ, Howard VJ, Huffman MD, Isasi CR, Jimenez MC, Judd SE, Kissela BM, Lichtman JH, Lisabeth LD, Liu S, Mackey RH, Magid DJ, McGuire DK, Mohler ER 3rd, Moy CS, Muntner P, Mussolino ME, Nasir K, Neumar RW, Nichol G, Palaniappan L, Pandey DK, Reeves MJ, Rodriguez CJ, Rosamond W, Sorlie PD, Stein J, Towfighi A, Turan TN, Virani SS, Woo D, Yeh RW, Turner MB, American Heart Association Statistics Committee; Stroke Statistics Subcommittee. Heart Disease and Stroke Statistics-2016 Update: a report from the American Heart Association. Circulation. 2016;133:e38–360. [DOI] [PubMed] [Google Scholar]
- 6.Salami JA, Warraich H, Valero-Elizondo J, Spatz ES, Desai NR, Rana JS, Virani SS, Blankstein R, Khera A, Blaha MJ, Blumenthal RS, Lloyd-Jones D, Nasir K. National trends in statin use and expenditures in the US adult population from 2002 to 2013: insights from the Medical Expenditure Panel Survey. JAMA Cardiol. 2017;2:56–65. [DOI] [PubMed] [Google Scholar]
- 7.Virani SS, Woodard LD, Ramsey DJ, Urech TH, Akeroyd JM, Shah T, Deswal A, Bozkurt B, Ballantyne CM, Petersen LA. Gender disparities in evidence-based statin therapy in patients with cardiovascular disease. Am J Cardiol. 2015;115:21–26. [DOI] [PubMed] [Google Scholar]
- 8.Peterson ED, Delong ER, Masoudi FA, O’Brien SM, Peterson PN, Rumsfeld JS, Shahian DM, Shaw RE; ACCF/AHA Task Force on Performance Measures, Goff DC Jr, Grady K, Green LA, Jenkins KJ, Loth A, Radford MJ. ACCF/AHA 2010 Position Statement on Composite Measures for Healthcare Performance Assessment: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Performance Measures (Writing Committee to develop a position statement on composite measures). Circulation. 2010;121:1780–1791. [DOI] [PubMed] [Google Scholar]
- 9.Centers for Medicare & Medicaid Services. Measure #438: Statin Therapy for the Prevention and Treatment of Cardiovascular Disease – National Quality Strategy Domain: Effective Clinical Care. Quality Payment Program web site. https://qpp.cms.gov/docs/QPP_quality_measure_specifications/Claims-Registry-Measures/2017_Measure_438_Registry.pdf. Updated December 15, 2016. Accessed October 30, 2018.
- 10.Navar AM, Wang TY, Goldberg AC, Robinson JG, Roger VL, Wilson PF, Virani SS, Elassal J, Lee LV, Webb LE, Peterson E. Design and rationale for the Patient and Provider Assessment of Lipid Management (PALM) Registry. Am Heart J. 2015;170:865–871. [DOI] [PubMed] [Google Scholar]
- 11.Fagerlin A, Zikmund-Fisher BJ, Ubel PA, Jankovic A, Derry HA, Smith DM. Measuring numeracy without a math test: development of the Subjective Numeracy Scale. Med Decis Making. 2007;27:672–80. [DOI] [PubMed] [Google Scholar]
- 12.van Buuren S Multiple imputation of discrete and continuous data by fully conditional specification. Statistical Methods in Medical Research. 2007;16:219–242. [DOI] [PubMed] [Google Scholar]
- 13.Gamboa CM, Colantonio LD, Brown TM, Carson AP, Safford MM. Race-sex differences in statin use and low-density lipoprotein cholesterol control among people with diabetes mellitus in the Reasons for Geographic and Racial Differences in Stroke Study. J Am Heart Assoc. 2017;6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Peters SAE, Colantonio LD, Zhao H, Bittner V, Dai Y, Farkouh ME, Monda KL, Safford MM, Muntner P, Woodward M. Sex differences in high-intensity statin use following myocardial infarction in the United States. J Am Coll Cardiol. 2018;71:1729–1737. [DOI] [PubMed] [Google Scholar]
- 15.Karalis DG, Wild RA, Maki KC, Gaskins R, Jacobson TA, Sponseller CA, Cohen JD. Gender differences in side effects and attitudes regarding statin use in the Understanding Statin Use in America and Gaps in Patient Education (USAGE) study. J Clin Lipidol. 2016;10:833–841. [DOI] [PubMed] [Google Scholar]
- 16.Bradley CK, Wang TY, Li S, Robinson JG, Roger VL, Goldberg AC, Virani SS, Louie MJ, Lee LV, Peterson ED, Navar AM. Patient-Reported Reasons for Declining or Discontinuing Statin Therapy: Insights From the PALM Registry. J Am Heart Assoc. 2019; 8:e011765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mosca L, Benjamin EJ, Berra K, Bezanson JL, Dolor RJ, Lloyd-Jones DM, Newby LK, Pina IL, Roger VL, Shaw LJ, Zhao D, Beckie TM, Bushnell C, D’Armiento J, Kris- Etherton PM, Fang J, Ganiats TG, Gomes AS, Gracia CR, Haan CK, Jackson EA, Judelson DR, Kelepouris E, Lavie CJ, Moore A, Nussmeier NA, Ofili E, Oparil S, Ouyang P, Pinn VW, Sherif K, Smith SC Jr, Sopko G, Chandra-Strobos N, Urbina EM, Vaccarino V, Wenger NK. Effectiveness-based guidelines for the prevention of cardiovascular disease in women−-2011 update: a guideline from the American Heart Association. Circulation. 2011;123:1243–1262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mosca L, Banka CL, Benjamin EJ, Berra K, Bushnell C, Dolor RJ, Ganiats TG, Gomes AS, Gornik HL, Gracia C, Gulati M, Haan CK, Judelson DR, Keenan N, Kelepouris E, Michos ED, Newby LK, Oparil S, Ouyang P, Oz MC, Petitti D, Pinn VW, Redberg RF, Scott R, Sherif K, Smith SC Jr, Sopko G, Steinhorn RH, Stone NJ, Taubert KA, Todd BA, Urbina E, Wenger NK; Expert Panel/Writing Group; American Heart Association; American Academy of Family Physicians; American College of Obstetricians and Gynecologists; American College of Cardiology Foundation; Society of Thoracic Surgeons; American Medical Women’s Association; Centers for Disease Control and Prevention; Office of Research on Women’s Health; Association of Black Cardiologists; American College of Physicians; World Heart Federation; National Heart, Lung, and Blood Institute; American College of Nurse Practitioners. Evidence-based guidelines for cardiovascular disease prevention in women: 2007 update. Circulation. 2007;115:1481–1501.17309915 [Google Scholar]
- 19.Mosca L, Appel LJ, Benjamin EJ, Berra K, Chandra-Strobos N, Fabunmi RP, Grady D, Haan CK, Hayes SN, Judelson DR, Keenan NL, McBride P, Oparil S, Ouyang P, Oz MC, Mendelsohn ME, Pasternak RC, Pinn VW, Robertson RM, Schenck-Gustafsson K, Sila CA, Smith SC Jr., Sopko G, Taylor AL, Walsh BW, Wenger NK, Williams CL, American Heart Association. Evidence-based guidelines for cardiovascular disease prevention in women. Circulation. 2004;109:672–693. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.