Abstract
Purpose
A patient-derived xenograft (PDX) model is an in vivo animal model which provides biological and genomic profiles similar to a primary tumor. The characterization of factors that influence the establishment of PDX is crucial. Furthermore, PDX models can provide a platform for chemosensitivity tests to evaluate the effectiveness of a target agent before applying it in clinical trials.
Methods
We implanted 83 cases of breast cancer into NOD.Cg-Prkdcscid Il2rgtm1Sug/Jic mice, to develop PDX models. Clinicopathological factors of primary tumors were reviewed to identify the factors affecting engraftment success rates. After the establishment of PDX models, we performed olaparib and carboplatin chemosensitivity tests. We used PDX models from triple-negative breast cancer (TNBC) with neoadjuvant chemotherapy and/or germline BRCA1 mutations in chemosensitivity tests.
Results
The univariate analyses (p<0.05) showed factors which were significantly associated with successful engraftment of PDX models include poor histologic grade, presence of BRCA mutation, aggressive diseases, and death. Factors which were independently associated with successful engraftment of PDX models on multivariate analyses include poor histologic grade and aggressive diseases status. In chemosensitivity tests, a PDX model with the BRCA1 L1780P mutation showed partial response to olaparib and complete response to carboplatin.
Conclusions
Successful engraftment of PDX models was significantly associated with aggressive diseases. Patients who have aggressive diseases status, large tumors, and poor histologic grade are ideal candidates for developing successful PDX models. Chemosensitivity tests using the PDX models provide additional information about alternative treatment strategies for residual TNBC after neoadjuvant chemotherapy.
Introduction
Drug development is facilitated by understanding of the interactions between tumors and microenvironments. Preclinical models enhance knowledge of tumor biology and drug development to elucidate drug resistant mechanisms of tumors. Appropriate selection of preclinical models is pivotal to bridge the translational gap between drug development and clinical application.
Triple negative breast cancer (TNBC) tumors lack expression of estrogen receptor (ER), progesterone receptor (PR), and human epithelial growth factor receptor 2 (HER2). Compared to hormone receptor-positive breast cancer, TNBC exhibits aggressive clinical characteristics [1]. Cytotoxic chemotherapy is the only systemic treatment option to manage TNBC, because of a lack of effective target therapy [2].
Pharmaceutical companies have invested in research and development (R&D) to find an effective target therapy. However, many hurdles block the development of new drugs, including the significant cost in terms of money and time. In 2000, the R&D cost per new drug, including the pre-clinical and clinical cost was, on average US 802 million dollars [3]. The mean duration of the clinical and approval phase, from investigational new drug application filing to new drug application submission and approval, was 87.4 months [4]. Although new agents have been discovered, the successful clinical trial process is difficult [5]. A new strategy for successful clinical trial is necessary to overcome these challenges [6].
Drug sensitivity tests can be performed in in vitro models [7] whereby cancer cells are directly exposed to various drug combinations in multiple concentrations. This kind of study is considered a basic experiment before further evaluations of the drug can be tested in clinical trials [8]. However, even well-designed artificial conditions for cancer cell lines do not directly reflect patients’ micro-environments [9, 10].
Mouse models, or in vivo models, use patient-derived cancer cells to induce tumors in mice. Animal models can simulate interaction between tumors and the microenvironment [11, 12]. However, in vivo models which use cultured cancer cells of in vitro studies have the same limitation because they also do not accurately reflect the characteristics of a patient’s primary tumor [13–15].
Patient-derived xenograft (PDX) models which use immune-compromised mice implanted with fresh tumor tissue from patients with cancer have been introduced as new in vivo models for cancer research [16, 17]. In general, tumors in PDX models have shown similar histopathological features as primary tumors [18]. Therefore, theoretically, PDX models can predict drug response of primary tumors better than conventional in vivo or in vitro models [19–21].
Patient-derived xenograft models have been established for several cancer types [22–25] and successful take rates of PDX models vary according to cancer type. Previous studies have reported 10–50% success rates of PDX models in colon, pancreas, lung, prostate, and breast cancer [26]. To enhance successful engraftment and maintenance of PDX models, it is crucial to characterize the factors influencing the establishment of PDX models, but little is known about those factors.
The current study focused on the establishment of PDX models of breast cancer and identifying the influencing factors for successful engraftment of the models. Furthermore, in vivo chemosensitivity tests were performed in the PDX models with TNBC, with and without highly aggressive diseases characteristics, and BRCAness.
Materials and methods
Patients and subtypes
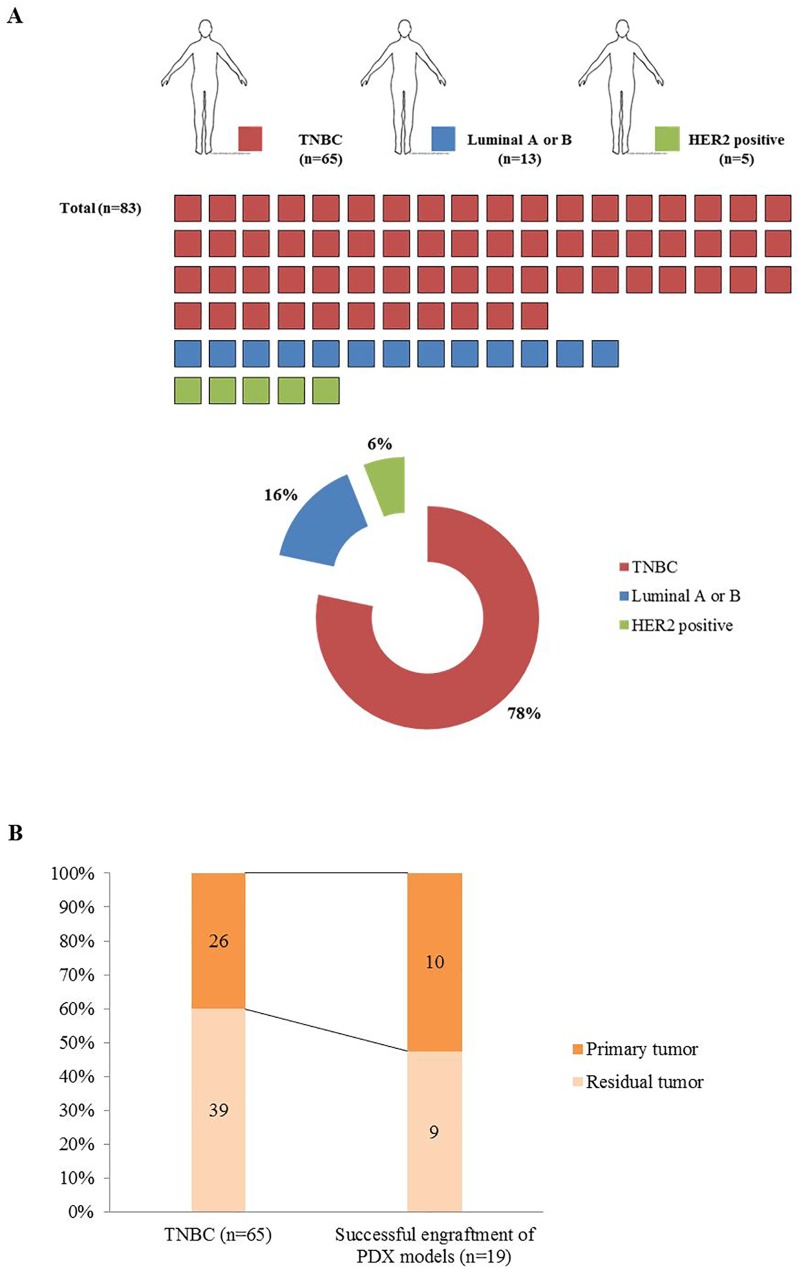
A total of 82 patients with breast cancer were enrolled in this study. One patient who received serial biopsies including a preoperative needle biopsy and surgical resection before (BR30) and after (BR40) neoadjuvant chemotherapy was also included. Thus, a total of 83 malignant tumors of breast were used to develop PDX models in the study. All patients underwent breast surgery or biopsy at Severance Hospital, Seoul, Korea. Fresh tumor tissue was obtained during surgery or biopsy. After removal, tumor tissue was immediately transferred to the animal laboratory (Avison Biomedical Research Center, Seoul, Korea). Cubic tissue of 3mm3 in size was minced and directly implanted into mice without delay. We attempted to establish PDX models from TNBC (n = 65), luminal A or B (n = 13), and HER2 positive (n = 5) breast cancer patients. Among TNBC patients, 39 received neoadjuvant chemotherapy.
PDX models and establishment periods
Tumor tissue was implanted into the subcutaneous or mammary fat pad of 6 to 12-week-old female NOG (NOD.Cg-Prkdcscid Il2rgtm1Sug) mice [27]. Tumor size was measured using calipers once a week, and tumor volume was calculated as 0.5 × Length × Width2[28]. When the tumor volume reached 1500 mm3-, the implanted tumor was harvested from the mice under isoflurane anesthesia [26]. A portion of the tumor (~5mm3) was engrafted in a new generation of mice [29]. The remaining tumor was cut into pieces and stored in liquid nitrogen. The tumor tissue was stored in a solution of 90% fetal bovine serum (FBS) and 10% dimethyl sulfoxide (DMSO) for use in re-engraftment. Some of the tumor tissues were stored frozen for generating sequencing data [30]. Primary tumor was implanted into the first generation of mice, which was defined as F1 mice. The harvested tumor was serially implanted into second- (F2) and third-generation (F3) of mice. When the PDX model had been engrafted into third generation of mice, it was considered a successful PDX model [31].
Establishment periods from F1 to F3 (F1-F3) were measured. The establishment period was divided into establishment periods from F1 to F2 (F1-F2) and F2 to F3 (F2-F3), and compared. Establishment periods from F1 to F3 (F1-F3) was not exceeded 550 days.
Animal care
All animal experiments were performed in a facility accredited by AAALAC International (#001071) in accordance with Guide for the Care and Use of Laboratory Animals 8th edition, NRC (2010). The tumor implanted mice were housed in one cage (maximum five mice). Food was exchanged once a week and water was supplied automatically from the automatic water supply equipment. A facility staff of animal laboratory periodically checked the status of mice. Mice monitoring was performed once a week. After tumor implantation, euthanasia was performed when tumors reached 1500mm3 in volume or became ulcerated, tumors affected physiological functions including gait, posture, ability to eat/drink/urinate/defecate, or when mice lost more than 15% of their first body weight. Mice were euthanized by CO2 gas inhalation in accordance with the humane endpoints which included the above descriptions. And when the mice reached endpoint criteria, we performed euthanasia by CO2 gas inhalation within 2 days. In our study, there were no mice which died before meeting criteria for euthanasia. There are well-trained facility staffs who can help to solve the problem in animal care at our institution. They advised injection methods of drugs (carboplatin/olaparib).
Histopathological confirmation
When a tumor was engrafted to a new mouse, one piece of tumor tissue (~8mm3) was used to construct FFPE (Formalin fixed paraffin embedded) blocks. Immunohistochemistry analysis was performed to confirm the histopathological similarity including ER, PR, and HER2 between primary tumor and those in PDX models. Xylene and serial concentrations of ethanol were used for deparaffinization and hydration of tumor sections. For antigen retrieval and blocking endogenous peroxidases, a solution of 0.4% H2O2 and 10mM sodium citrate buffer (pH6.0) was used. Sections were treated with a peroxidase-conjugated polymer solution (Dako REAL EnVision Detection System, Peroxides/DAB+, antibodies of Rabbit/Mouse). Primary antibodies used for in immunohistochemistry analysis included ERα (clone SP1, 1:100 dilution, LifeSpan BioSciences, Seattle, WA, USA); PR (clone 1E2, 1:100 dilution, ABCAM, Cambridge, CB4 0FL, UK), HER2 (clone EP1045Y, 1:100 dilution, ABCAM, Cambridge, CB4 0FL, UK) and Ki67 (clone EPR3610, 1:500 dilution, ABCAM, Cambridge, CB4 0FL, UK). A pathologist confirmed all stained slides.
Factors relating to success of PDX models
Clinicopathological factors relating to the successful engraftment of PDX models were analyzed. These factors included age, T-stage, nodal status, hormone receptor status, HER2 status, Ki67 level, breast cancer subtype, histologic grade, treatment status, biopsy method (surgery or needle biopsy), engraftment period, mouse type, TNM Classification of Malignant Tumours (TNM) stage, existence/absence of BRCA mutation, and survival status of patient. Disease burden was analyzed. Aggressive diseases were defined as progressive diseases during preoperative or neoadjuvant chemotherapy, recurrent, and metastatic diseases.
Chemosensitivity tests using the PDX models
We performed chemosensitivity tests using three PDX models including a tumor from TNBC with a novel germline pathogenic BRCA1 mutation, c.5339T->C; p.Leu1780Pro; rs80357474 (L1780P), which was introduced in our previous study [32], a tumor from TNBC with a germline BRCA1 deleterious mutation, c.3277delG; p.Val1093SerfsTer16; rs113900085, and a tumor from a TNBC without germline pathogenic BRCA mutation. PDX models were derived from patients who had BRCA1 mutation (n = 2, L1780P and rs113900085) and the wild type of BRCA1 (n = 1). Each model comprised nine mice, which were divided equally into three groups (1 group = 3 mouse, vehicle [PBS], olaparib, and carboplatin.). A total of 27 mice were used in the chemosensitivity tests.
Dosages of olarparib and carboplatin were 50 mg/kg and 25 mg/kg, respectively [33, 34]. Olaparib was administrated via intraperitoneal injection for 28 consecutive days. Carboplatin was administrated via intraperitoneal injection once a week. Duration of the in vivo test was not exceeded 2 months. Tumor volumes were measured using the below equation, Volume = 0.5 × Length × Width2
Sequencing analysis of the PDX model with L1780P
Whole genome sequencing (WGS) and whole exome sequencing (WES) of one PDX model with L1780P mutation were performed in collaboration with the Theragen company (Seoul, Korea). The depth of WGS was 30X in buffy coat, 60X in primary tumor, and 30X in F1, F2, and F3, respectively. WES was only performed in the primary tumor, and the depth of WES was 250X.
Using the TruSeq Nano DNA Sample Preparation Kit from Illumina (San Diego, CA), DNA sequencing libraries of WGS were constructed, according to the manufacturer protocol. Quality of the amplified libraries was confirmed by electrophoresis on Agilent Bioanalyzer High Sensitivity DNA Kit (part # 5067–4626) (Agilent, CA). The libraries were sequenced using Illumina HiSeq2500 and Cluster generation. Then, 2 × 100 cycle sequencing reads, separated by paired-end turnaround, were performed on the instrument using HiSeq Rapid SBS Kit v2 (FC-402-4021) and HiSeq Rapid PE Cluster Kit v2 (PE-402-4002; Illumina, CA).
In the WES, the quality and quantity of purified DNA were assessed by fluorometry (Qubit, Invitrogen) and gel electrophoresis, and the sample was hybridized with RNA probes, SureSelect XT Human All Exon V5 Capture library. The captured targets were then pulled down by biotinylated probe/target hybrids using streptavidin-coated magnetic beads (Dynabeads My One Streptavidine T1; Life Technologies Ltd.). The resulting purified libraries were applied to an Illumina flow cell for cluster generation and sequenced using 100 bp paired-end reads on an Illumina Hiseq2500 sequencer, following the manufacturer's protocols.
The quality of reads in the WGS and WES were confirmed using fastQC (v.0.10.1) [35], which also expounded the basic quality for sequence quality score, GC content, N content, length of distribution, and duplication levels. After examining the read quality, the low-quality bases below Q20 were trimmed using Cutadapt (v.1.8.1) [36].
In order to remove mouse reads in PDX samples, BBMap [37] was applied to the fastq files based on hg19 and Ensembl Release 77 reference genome for human and mouse, respectively. Only reads that were classified as human reads were then analyzed.
Statistics and ethics
The SPSS statistics program version 23 (International Business Machines Crop., Armonk, NY, USA) was used for all analyses. Categorical variables were examined using chi-square test or Fisher’s exact test. Continuous variables were examined using student T-test. Multivariate analyses were examined using binary regression models. Multivariate analyses were adjusted for significant factors in univariate analyses. All statistical analyses were two-sided and p-values of less than 0.05 were considered statistically significant.
All tumor tissue was obtained with the patient’s written consent and the informed written consent was provided by the patients. All procedures were approved by the Institutional Review Board of Yonsei University Health System (IRB No.4-2012-0705). All experiments were approved by the Institutional Animal Care and Use Committee in Yonsei University Hospital System (YUHS-IACUC) and animals were maintained in a facility accredited by AAALAC International (#001071) in accordance with Guide for the Care and Use of Laboratory Animals 8th edition, NRC (2010).
Results
Of the 83 tumor samples, most tumor tissue (65 out of 83 samples) came from TNBC patients (Fig 1A). Only one tumor sample was subcutaneously implanted into mice. 78 tumors were implanted into mammary fat pads. Successful engraftments of PDX models were established in 19 TNBC cases. All successful engraftments of PDX models were implanted into mammary fat pads. We attempted to establish PDX models from residual tumors more than primary tumors (Fig 1B). The overall success rates of PDX models were higher in cases with primary TNBCs than those in residual TNBCs (38.5% for primary TNBC vs. 23.1% for residual TNBCs) (Fig 1B). We established a PDX model with a novel germline pathogenic mutation of BRCA1, L1780P (Patent pending, reference number; DPB172272).
Fig 1. Proportions of successful engraftment of PDX models.
(A) Proportion of breast cancer subtypes. (B) Successful engraftment of PDX models were derived from TNBC patient with or without neoadjuvant chemotherapy.
A total of 21 successful PDX models were derived from TNBC patients. Of those, two cases were classified as developed lymphoma. Except for those two cases, 19 tumors from PDX models coincided with the histopathological characteristics of primary tumors (Fig 2A). Immunohistochemistry revealed Ki67 expression in the PDX models Fig 2B. ER, PR, and HER2 tumor samples were positive controls. (Fig 2C)
Fig 2. Histopathological characteristics of successful engraftment of PDX models and patients.
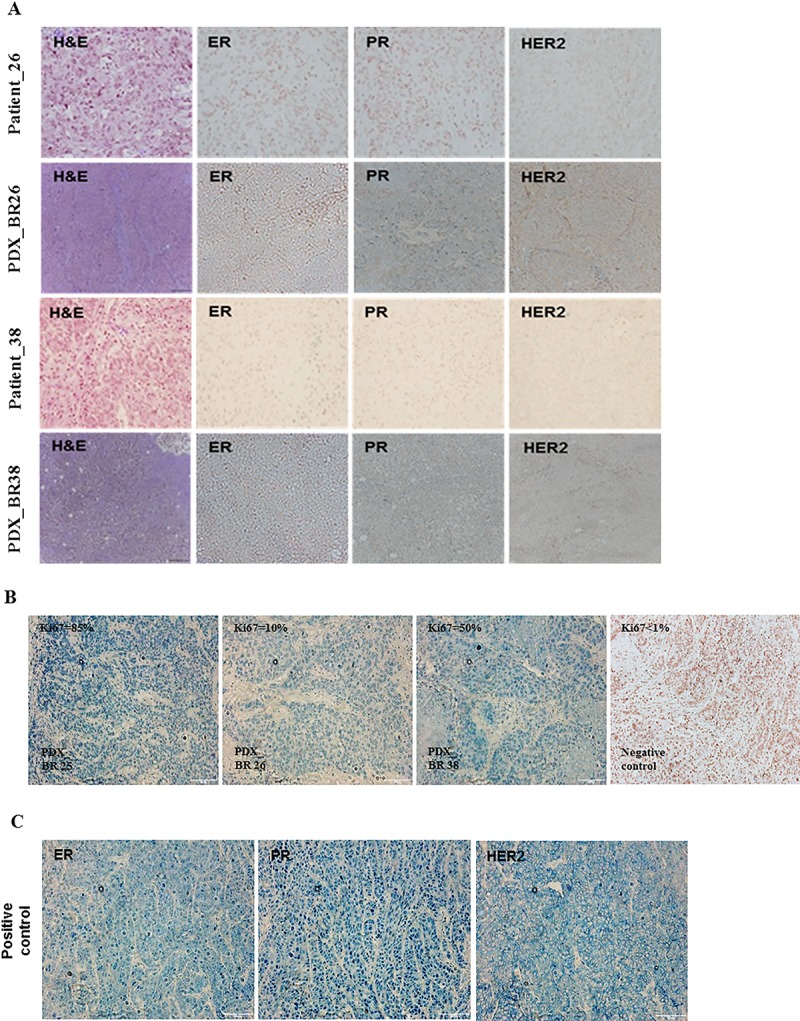
(A) H&E staining and immunohistochemistry of PDX models and primary tumor of patients. (B) Ki67 expression of PDX models. (C) Positive control of ER, PR and HER2 in immunohistochemistry.
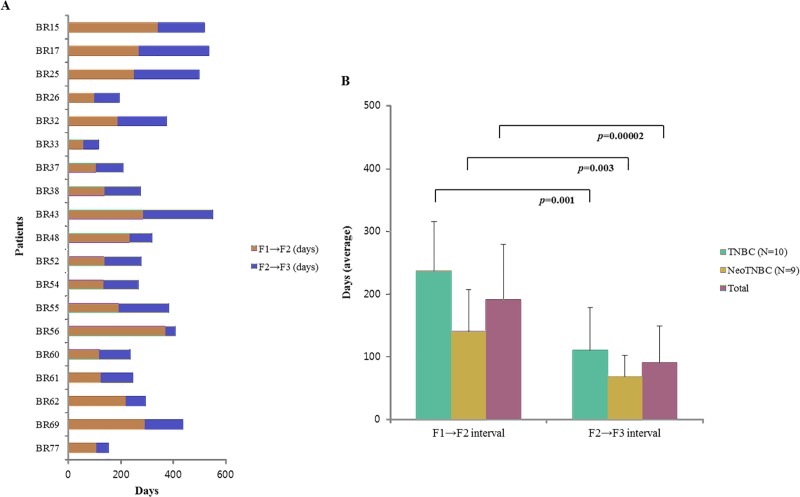
The establishment periods of F1-F3 interval are shown in Fig 3A. The median establishment period from F1 to F3 was 221 days (range 93–550 days). The PDX models of residual TNBC with neoadjuvant chemotherapy (Neo TNBC) showed shorter establishment periods than primary TNBC (p = 0.02; Fig 3B). The F2-F3 interval was significantly shorter than the F1-F2 interval (p = 0.00002; Fig 3B). The shortest interval of establishment period was the F2-F3 interval of Neo TNBC models (median 62 days, range 41–158 days; Fig 3B).
Fig 3. Successful engraftment of F1 to F3 in PDX models.
(A) Establishment periods of all successful PDX models (B) F1-F2 and F1-F3 intervals according to status of neoadjuvant chemotherapy.
In univariate analysis, T-stage, histologic grade, estrogen receptor status, and Ki67 levels were statistically significant (p<0.05) (Table 1). Presence of BRCA mutation, aggressive diseases status, or death were related to successful PDX models (p<0.05). Hormone and HER2 positive cases made up a small portion of total cases (n = 18, 21.7%), and the results were not significant in hormone and HER2 positive cases. All successful PDX models were made from TNBC and Neo TNBC cases.
Table 1. Analysis of factors related to PDX models.
| Factors | PDX status | |||
|---|---|---|---|---|
| Failure (%) | Success (%) | p-value | ||
| Age (years) | <60 | 43 (67.2%) | 14 (73.7%) | 0.592 |
| ≥60 | 21 (32.8%) | 5 (26.3%) | ||
| T stage | -T1 | 34 (56.7%) | 5 (26.3%) | 0.038 |
| T2 | 22 (36.7%) | 10 (52.6%) | ||
| T3-T4 | 4 (6.7%) | 4 (21.1%) | ||
| Nodal status | Negative | 40 (65.6%) | 8 (47.1%) | 0.165 |
| Positive | 21 (34.4%) | 9 (52.9%) | ||
| Histologic grade | I/II | 33 (56.9%) | 3 (15.8%) | 0.002 |
| III | 25 (43.1%) | 16 (84.2%) | ||
| ER | Negative | 51 (79.7%) | 19 (100.0%) | 0.032 |
| Positive | 13 (20.3%) | 0 (0.0%) | ||
| PR | Negative | 55 (85.9%) | 19 (100.0%) | 0.083 |
| Positive | 9 (14.1%) | 0 (0.0%) | ||
| HER2 | Negative | 56 (87.5%) | 19 (100.0%) | 0.105 |
| Positive | 8 (12.5%) | 0 (0.0%) | ||
| Ki67 (%, n = 79) | <39 (n = 41) | 38 (62.3%) | 3 (16.7%) | 0.001 |
| ≥39 (n = 38) | 23 (37.7%) | 15 (83.3%) | ||
| BRCA mutation | Absent | 61(96.9%) | 15(78.9%) | 0.005 |
| Present | 2(3.1%) | 4(21.1%) | ||
| Survival status | Live | 62(96.9%) | 15(78.9%) | 0.008 |
| Death | 2(3.1%) | 4(21.1%) | ||
| Aggressive diseases* | Absent | 54 (87.5%) | 10 (63.2%) | 0.004 |
| Present | 10 (12.5%) | 9 (36.8%) | ||
ER, estrogen receptor; PR, progesterone receptor; HER2, human epidermal growth factor receptor; Ki67: cell proliferation index
* Aggressive diseases were considered to be progressive diseases during neoadjuvant chemotherapy, recurrent, and metastatic disease
In 65 TNBC cases, histologic grade, Ki67 level, presence of BRCA mutation, aggressive diseases status, and death were statistically significant on univariate analysis (p<0.05; Table 2).
Table 2. Analysis of factors related to TNBC PDX models.
| Factors | PDX status | |||
|---|---|---|---|---|
| Failure (%) | Success (%) | p-value | ||
| Age(years) | <60 | 29 (63.0%) | 14 (73.7%) | 0.410 |
| ≥60 | 17 (37.0%) | 5 (26.3%) | ||
| T stage | -T1 | 24 (54.5%) | 5 (26.3%) | 0.070 |
| T2 | 17 (38.6%) | 10 (52.6%) | ||
| T3-T4 | 3 (6.8%) | 4 (21.1%) | ||
| Nodal status | Negative | 28 (63.6%) | 8 (47.1%) | 0.238 |
| Positive | 16 (36.4%) | 9 (52.9%) | ||
| Histologic grade | I/II | 19 (45.2%) | 3 (15.8%) | 0.027 |
| III | 23 (54.8%) | 16 (84.2%) | ||
| Ki67 (%, n = 79) | <39 (n = 41) | 23 (52.3%) | 3 (16.7%) | 0.010 |
| ≥39 (n = 38) | 21 (47.7%) | 15 (83.3%) | ||
| BRCA mutation | Absent | 43(93.5%) | 14(73.7%) | 0.027 |
| Present | 3(6.5%) | 5(26.3%) | ||
| Survival status | Live | 44(95.7%) | 15(78.9%) | 0.034 |
| Death | 2(4.3%) | 4(21.1%) | ||
| Aggressive diseases* | Absent | 37 (80.4%) | 10 (52.6%) | 0.023 |
| Present | 9 (19.6%) | 9 (47.4%) | ||
ER, estrogen receptor; PR, progesterone receptor; HER2, human epidermal growth factor receptor; Ki67: cell proliferation index
* Aggressive diseases were considered to be progressive diseases during neoadjuvant chemotherapy, recurrent, and metastatic disease
Tumor size was not significant in TNBC cases (p>0.05). In TNBC cases with neoadjuvant chemotherapy, histologic grade, presence of BRCA mutation, aggressive diseases status, and death were statistically significant (p<0.05) (Table 3). Information of the chemotherapy regimens is presented in S1 Table.
Table 3. Analysis of factors related to TNBC PDX models with neoadjuvant chemotherapy.
| Factors | PDX status | |||
|---|---|---|---|---|
| Failure (%) | Success (%) | p-value | ||
| Age(years) | <60 | 22 (73.3%) | 8 (88.9%) | 0.331 |
| ≥60 | 8 (26.7%) | 1 (11.1%) | ||
| T stage | -T1 | 13 (44.8%) | 2 (22.2%) | 0.066 |
| T2 | 13 (44.8%) | 3 (33.3%) | ||
| T3-T4 | 3 (10.3%) | 4 (44.4%) | ||
| Nodal status | Negative | 16 (55.2%) | 2 (25.0%) | 0.131 |
| Positive | 13 (44.8%) | 6 (75.0%) | ||
| Histologic grade | I/II | 16 (59.3%) | 1 (11.1%) | 0.012 |
| III | 11 (40.7%) | 8 (88.9%) | ||
| Ki67 (%, n = 79) | <39 (n = 41) | 17 (58.6%) | 2 (22.2%) | 0.056 |
| ≥39 (n = 38) | 12 (41.4%) | 7 (77.8%) | ||
| BRCA mutation | Absent | 28(93.3%) | 6(66.7%) | 0.036 |
| Present | 2(6.7%) | 3(33.3%) | ||
| Survival status | Live | 28(93.3%) | 6(66.7%) | 0.036 |
| Death | 2(6.7%) | 3(33.3%) | ||
| Aggressive diseases* | Absent | 23 (76.7%) | 2 (22.2%) | 0.003 |
| Present | 7 (23.3%) | 7(77.8%) | ||
ER, estrogen receptor; PR, progesterone receptor; HER2, human epidermal growth factor receptor; Ki67: cell proliferation index
* Aggressive diseases were considered to be progressive diseases during neoadjuvant chemotherapy, recurrent, and metastatic disease
Multivariate analyses showed poor histologic grade and aggressive diseases status were independently associated with the successful engraftment of PDX models (p<0.05; Table 4), and presence of BRCA mutation and death event were marginally associated with successful engraftment of PDX models (p = 0.05; Table 4).
Table 4. Multivariate analysis of factors relating to successful engraftment of PDX models.
| Factors | p-value | OR | 95% C.I. | |
|---|---|---|---|---|
|
All cases (n = 83) |
Histologic grade (I/II vs. III) | 0.004 | 7.040 | 1.847–26.836 |
| BRCA mutation (absent vs. present) | 0.012 | 7.262 | 1.549–34.034 | |
| Survival status (live vs. Death) | 0.021 | 8.247 | 1.382–49.444 | |
| Aggressive diseases (absent vs. present) | 0.006 | 4.860 | 1.577–14.974 | |
|
TNBC cases (n = 65) |
Histologic grade (I/II vs. III) | 0.034 | 4.406 | 1.114–17.420 |
| BRCA mutation (absent vs. present) | 0.039 | 5.119 | 1.083–24.196 | |
| Survival status (live vs. Death) | 0.053 | 5.867 | 0.974–35.339 | |
| Aggressive diseases (absent vs. present) | 0.027 | 3.700 | 1.162–11.783 | |
|
Neo TNBC cases (n = 39) |
Histologic grade (I/II vs. III) | 0.030 | 11.636 | 1.269–106.719 |
| BRCA mutation (absent vs. present) | 0.056 | 7.000 | 0.952–51.448 | |
| Survival status (live vs. Death) | 0.056 | 7.000 | 0.952-51-448 | |
| Aggressive diseases (absent vs. present) | 0.007 | 11.500 | 1.930–68.518 |
In the chemosensitivity tests, there were no significant differences in the average tumor volume of the three treatment arms in PDX models with wild type BRCA1 and the deleterious BRCA1 mutation. However, nearly complete remission in the carboplatin arm and partial remission in the olaparib arm were attained in the PDX model with the novel L1780P BRCA1 mutation (Fig 4A–4E).
Fig 4. Scheme and results of chemosensitivity tests using PDX models.
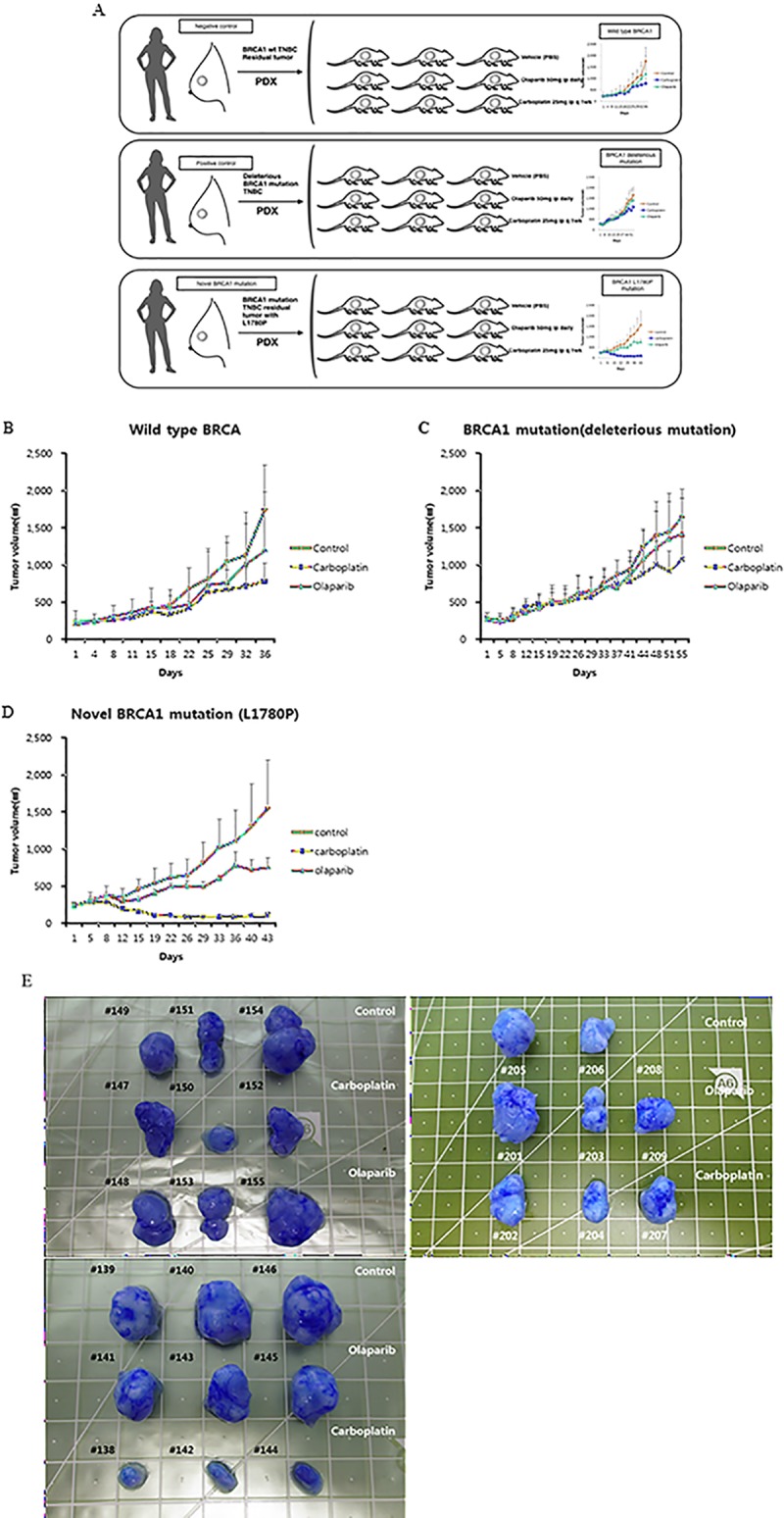
(A) PDX models were derived from patients who had BRCA1 mutation (n = 2) or wild-type BRCA1 (n = 1). Each model comprise nine mice, which were divided into three groups (1 group = 3 mouse, two single treatment groups and one vehicle group). (B-E) When implanted tumor reached an average size of 200–250 mm3 (Volume = 0.5×Length×Width^2), the chemosensitivity test was performed. Olaparib (50mg/kg, once a daily) and carboplatin (25mg/kg, once a weekly) were administered by an intra-peritoneal (i.p.) route. Phosphate buffered saline was used to as a vehicle.
In WGS, c.5339T>C, L1780P in BRCA1 was continuously detected in buffy coat, primary tumor, F1, F2, and F3 tumors. However, variant allele frequency (VAF) was increased in late passage. (Normal = 0.53, F0 = 0.63, F1 = 0.9, F2 = 1.0, F3 = 1.0). There was no pathogenic germline mutation in buffy coat, primary tumor and PDX models, other than in L1780P in WGS. In TCGA data, there was no c.5339T>C, L1780P variant among in BRCA1 mutations.[38] When we investigated the L1780P mutation in a Korean database reported in a previous study, there was no L1780P mutation in the normal population. [32]
Discussion
We demonstrated that the successful establishment of PDX models from TNBC patients is related to poor clinicopathologic factors including large tumor size, poor histologic grade, and aggressive diseases status at the time of tissue sampling. Aggressive diseases, including progressive diseases during neoadjuvant chemotherapy, recurrent disease, and metastatic disease at presentation, were associated with the establishment of successful PDX models on multivariate analysis. A previous study reported that TNBC patients with progressive disease during neoadjuvant chemotherapy had higher xenograft take rate than those with stable diseases or partial response after neoadjuvant chemotherapy (6 of 7 patients, 85.7% vs. 5 of 17 patients, 29.4%) [39]. These findings were similar to our findings. Therefore, tumor tissue from patients with TNBC with aggressive features may be the best candidate for establishing PDX models.
Large tumor size and poor histologic grade were significantly related to stable take rates in successful PDX models. A previous study reported that large tumor size and grade were associated with successful engraftment of PDX in bladder cancer [40]. Similar results have also been reported in pancreatic cancer where large tumor size (≥T3) was shown to be related to successful engraftment of PDX [41]. These studies suggested that large tumor size and poor histologic grade are predictors of successful engraftment of PDX, and this is concordant with our results. The analysis of factors related to the successful engraftment of PDX is crucial because considerable time and funds are consumed making successful PDX models. When developing PDX models, the more suitable the patients enrolled are, the less time and funds are required in order to achieve engraftment. The results of this study will be helpful to improve pre-clinical research. Furthermore, genomic research and drug tests in successful PDX models are necessary to improve the performance of PDX models.
In the current study, the mean F1-F2 interval was longer than the mean F2-F3 interval. In concordance with our results, a previous publication also demonstrated that the F1-F2 interval was longer than the F2-F3 interval in successful breast cancer PDX models [39].
In this study, Neo TNBC PDX models had shorter establishment period intervals than TNBC PDX models. These results suggested that shorter establishment period may be due to the aggressive nature of residual tumors after neoadjuvant chemotherapy, compared to primary tumors [42]. Aggressiveness of tumors has been shown to affect the successful establishment of PDX models and the rapid formation of tumor and tumor growth in the immune-deficient mouse [43, 44]. It was concordant with our study. Thus, in terms of establishment periods for establishing PDX models, residual TNBC after neoadjuvant chemotherapy may be more suitable than primary tumor of TNBC.
Chemosensitivity tests using PDX models were introduced by previous studies [45–47]. However, only a few studies reported chemosensitivity tests using PDX models from residual breast cancer after chemotherapy [48]. It has been suggested that BRCA mutations or BRCAness are potential targets of PARP inhibitors and platinum agents [33, 49]. Thus, we performed in vivo chemosensitivity tests of PARP inhibitor, olaparib and platinum agent, carboplatin, for PDX models with residual TNBC with/without BRCA1 mutation. A potential benefit from olaparib and carboplatin was evident in the PDX model with the L1780P mutation, but not in the other models. The establishment periods of PDX models remains a major challenge to applying them as in vivo chemosensitivity tests or the baseline study of N-of-1 trials. To overcome this hurdle, appropriate selection criteria for enrollment of patients for the PDX models should be considered. In this study, the median establishment period was 8 months. A limitation of this study is that chemosensitivity tests of the PDX models with L1780P mutation were performed in a single PDX model of one patient. Because the current study was conducted as an initial step of proof-of-concept study of N-of-1 trial, the results provide additional information about the potential application of chemosensitivity tests using PDX models. More chemosensitivity tests of PDX models for a larger number of L1780P mutation cases may strengthen the implications of further investigations of BRCA1 L1780P mutation olaparib and carboplatin drug-sensitivity.
In the current study, histopathological characteristics of tumors in successful PDX models were concordant with primary tumors. Interestingly, the sequencing analyses for the PDX model with L1780P mutation showed the VAF of the mutation was different among passages. This suggests that genetic alteration may occur throughout the passages. However, full genomic analyses were not performed in either primary tumors or successful PDX models—which was a limitation of this study. One of the advantages of PDX models is their ability to reflect patients’ genomic and clinicopathologic characteristics. Therefore, sequencing data from patients and PDX models is essential to examine the similarity of the genomic landscape between the two [48, 50, 51].
PDX models often utilize immune deficient mouse to avoid rejection of the human tumor graft by the mouse immune system. For this reason, PDX models using immune deficient mouse cannot reflect crosstalk of the immune system and human tumors. A previous study introduced a PDX model using humanized mice that was developed by injection of human hematopoietic cells into the mice to overcome this limitation of PDX models using immune deficient mice. [52, 53]
In further studies, it will be necessary to perform genomic sequencing and analysis of sequencing data in all successful PDX models. Additional experiments are necessary for the two suspected lymphoma to evaluate the mechanism of formation of lymphoma in PDX models [54].
Conclusions
The current study showed the feasibility of establishing PDX models using residual TNBC after neoadjuvant chemotherapy. Patients who have aggressive diseases status, large tumors, and poor histologic grade are ideal candidates for developing successful PDX models. This study also showed the potential usefulness of in vivo chemosensitivity tests for tumors with targetable biomarkers, particularly tumors with a novel pathologic mutation, L1780P. Further genomic analyses of the PDX models may shed light on tumor progression and drug resistant mechanisms in TNBC.
Supporting information
(XLSX)
Acknowledgments
A part of the abstract of the study was presented in the poster session at the Global Academic Programs (Gap) conference, 2018, Stockholm, Sweden.
Data Availability
All relevant data are within the paper.
Funding Statement
This work was supported by a Faculty Research Grant of Yonsei University College of Medicine grant no. 6-2017-0072 to HSP, a Severance Surgeon's Alumni Research Grant grant no. 2016-01 to HSP, National Research Foundation of Korea grant 2018R1A2A2A15019814 to SIK, Korea Health Industry Development Institute grant HI14C1324 to JHS, National Research Foundation of Korea grant 2016R1D1A1B03934564 to HSP, and a Faculty Research Grant of Yonsei University College of Medicine grant no. 6-2010-0002 to SIK. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Ovcaricek T, Frkovic SG, Matos E, Mozina B, Borstnar S. Triple negative breast cancer—prognostic factors and survival. Radiol Oncol. 2011;45(1):46–52. 10.2478/v10019-010-0054-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Isakoff SJ. Triple-negative breast cancer: role of specific chemotherapy agents. Cancer J. 2010;16(1):53–61. 10.1097/PPO.0b013e3181d24ff7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.DiMasi JA, Hansen RW, Grabowski HG. The price of innovation: new estimates of drug development costs. J Health Econ. 2003;22(2):151–85. 10.1016/S0167-6296(02)00126-1 . [DOI] [PubMed] [Google Scholar]
- 4.Kaitin KI, Healy EM. The new drug approvals of 1996, 1997, and 1998: Drug development trends in the user fee era. Drug Inf J. 2000;34(1):1–14. WOS:000085436000001. [Google Scholar]
- 5.Adams CP, Brantner VV. Estimating the cost of new drug development: is it really 802 million dollars? Health Aff (Millwood). 2006;25(2):420–8. 10.1377/hlthaff.25.2.420 . [DOI] [PubMed] [Google Scholar]
- 6.Dickersin K, Rennie D. Registering clinical trials. JAMA. 2003;290(4):516–23. 10.1001/jama.290.4.516 . [DOI] [PubMed] [Google Scholar]
- 7.Allen DD, Caviedes R, Cardenas AM, Shimahara T, Segura-Aguilar J, Caviedes PA. Cell lines as in vitro models for drug screening and toxicity studies. Drug Dev Ind Pharm. 2005;31(8):757–68. 10.1080/03639040500216246 . [DOI] [PubMed] [Google Scholar]
- 8.Astashkina A, Mann B, Grainger DW. A critical evaluation of in vitro cell culture models for high-throughput drug screening and toxicity. Pharmacol Ther. 2012;134(1):82–106. 10.1016/j.pharmthera.2012.01.001 . [DOI] [PubMed] [Google Scholar]
- 9.Siolas D, Hannon GJ. Patient-derived tumor xenografts: transforming clinical samples into mouse models. Cancer Res. 2013;73(17):5315–9. 10.1158/0008-5472.CAN-13-1069 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hidalgo M, Amant F, Biankin AV, Budinska E, Byrne AT, Caldas C, et al. Patient-derived xenograft models: an emerging platform for translational cancer research. Cancer Discov. 2014;4(9):998–1013. 10.1158/2159-8290.CD-14-0001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Clarke R. Human breast cancer cell line xenografts as models of breast cancer. The immunobiologies of recipient mice and the characteristics of several tumorigenic cell lines. Breast Cancer Res Treat. 1996;39(1):69–86. 10.1007/bf01806079 . [DOI] [PubMed] [Google Scholar]
- 12.Sausville EA, Burger AM. Contributions of human tumor xenografts to anticancer drug development. Cancer Res. 2006;66(7):3351–4, discussion 4. 10.1158/0008-5472.CAN-05-3627 . [DOI] [PubMed] [Google Scholar]
- 13.Daniel VC, Marchionni L, Hierman JS, Rhodes JT, Devereux WL, Rudin CM, et al. A primary xenograft model of small-cell lung cancer reveals irreversible changes in gene expression imposed by culture in vitro. Cancer Res. 2009;69(8):3364–73. 10.1158/0008-5472.CAN-08-4210 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dangles-Marie V, Pocard M, Richon S, Weiswald LB, Assayag F, Saulnier P, et al. Establishment of human colon cancer cell lines from fresh tumors versus xenografts: comparison of success rate and cell line features. Cancer Res. 2007;67(1):398–407. 10.1158/0008-5472.CAN-06-0594 . [DOI] [PubMed] [Google Scholar]
- 15.Gagos S, Iliopoulos D, Tseleni-Balafouta S, Agapitos M, Antachopoulos C, Kostakis A, et al. Cell senescence and a mechanism of clonal evolution leading to continuous cell proliferation, loss of heterozygosity, and tumor heterogeneity: studies on two immortal colon cancer cell lines. Cancer Genet Cytogenet. 1996;90(2):157–65. 10.1016/s0165-4608(96)00049-0 . [DOI] [PubMed] [Google Scholar]
- 16.Manning HC, Buck JR, Cook RS. Mouse Models of Breast Cancer: Platforms for Discovering Precision Imaging Diagnostics and Future Cancer Medicine. J Nucl Med. 2016;57 Suppl 1:60S–8S. 10.2967/jnumed.115.157917 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chijiwa T, Kawai K, Noguchi A, Sato H, Hayashi A, Cho H, et al. Establishment of patient-derived cancer xenografts in immunodeficient NOG mice. Int J Oncol. 2015;47(1):61–70. 10.3892/ijo.2015.2997 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kawaguchi T, Foster BA, Young J, Takabe K. Current Update of Patient-Derived Xenograft Model for Translational Breast Cancer Research. J Mammary Gland Biol Neoplasia. 2017;22(2):131–9. 10.1007/s10911-017-9378-7 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cho SY, Kang W, Han JY, Min S, Kang J, Lee A, et al. An Integrative Approach to Precision Cancer Medicine Using Patient-Derived Xenografts. Mol Cells. 2016;39(2):77–86. 10.14348/molcells.2016.2350 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Byrne AT, Alferez DG, Amant F, Annibali D, Arribas J, Biankin AV, et al. Interrogating open issues in cancer precision medicine with patient-derived xenografts. Nat Rev Cancer. 2017;17(4):254–68. 10.1038/nrc.2016.140 . [DOI] [PubMed] [Google Scholar]
- 21.Gao H, Korn JM, Ferretti S, Monahan JE, Wang Y, Singh M, et al. High-throughput screening using patient-derived tumor xenografts to predict clinical trial drug response. Nat Med. 2015;21(11):1318–25. 10.1038/nm.3954 . [DOI] [PubMed] [Google Scholar]
- 22.Wu L, Allo G, John T, Li M, Tagawa T, Opitz I, et al. Patient-Derived Xenograft Establishment from Human Malignant Pleural Mesothelioma. Clin Cancer Res. 2017;23(4):1060–7. 10.1158/1078-0432.CCR-16-0844 . [DOI] [PubMed] [Google Scholar]
- 23.Peng S, Creighton CJ, Zhang Y, Sen B, Mazumdar T, Myers JN, et al. Tumor grafts derived from patients with head and neck squamous carcinoma authentically maintain the molecular and histologic characteristics of human cancers. J Transl Med. 2013;11:198 10.1186/1479-5876-11-198 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lee HW, Lee JI, Lee SJ, Cho HJ, Song HJ, Jeong DE, et al. Patient-derived xenografts from non-small cell lung cancer brain metastases are valuable translational platforms for the development of personalized targeted therapy. Clin Cancer Res. 2015;21(5):1172–82. 10.1158/1078-0432.CCR-14-1589 . [DOI] [PubMed] [Google Scholar]
- 25.Dong R, Qiang W, Guo H, Xu X, Kim JJ, Mazar A, et al. Histologic and molecular analysis of patient derived xenografts of high-grade serous ovarian carcinoma. J Hematol Oncol. 2016;9(1):92 10.1186/s13045-016-0318-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Tentler JJ, Tan AC, Weekes CD, Jimeno A, Leong S, Pitts TM, et al. Patient-derived tumour xenografts as models for oncology drug development. Nat Rev Clin Oncol. 2012;9(6):338–50. 10.1038/nrclinonc.2012.61 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kato C, Fujii E, Chen YJ, Endaya BB, Matsubara K, Suzuki M, et al. Spontaneous thymic lymphomas in the non-obese diabetic/Shi-scid, IL-2R gamma (null) mouse. Lab Anim. 2009;43(4):402–4. 10.1258/la.2009.009012 . [DOI] [PubMed] [Google Scholar]
- 28.Paez-Ribes M, Man S, Xu P, Kerbel RS. Development of Patient Derived Xenograft Models of Overt Spontaneous Breast Cancer Metastasis: A Cautionary Note. PLoS One. 2016;11(6):e0158034 10.1371/journal.pone.0158034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Morton CL, Houghton PJ. Establishment of human tumor xenografts in immunodeficient mice. Nat Protoc. 2007;2(2):247–50. 10.1038/nprot.2007.25 . [DOI] [PubMed] [Google Scholar]
- 30.DeRose YS, Wang G, Lin YC, Bernard PS, Buys SS, Ebbert MT, et al. Tumor grafts derived from women with breast cancer authentically reflect tumor pathology, growth, metastasis and disease outcomes. Nat Med. 2011;17(11):1514–20. 10.1038/nm.2454 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Zhang X, Claerhout S, Prat A, Dobrolecki LE, Petrovic I, Lai Q, et al. A renewable tissue resource of phenotypically stable, biologically and ethnically diverse, patient-derived human breast cancer xenograft models. Cancer Res. 2013;73(15):4885–97. 10.1158/0008-5472.CAN-12-4081 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Park JS, Nam EJ, Park HS, Han JW, Lee JY, Kim J, et al. Identification of a Novel BRCA1 Pathogenic Mutation in Korean Patients Following Reclassification of BRCA1 and BRCA2 Variants According to the ACMG Standards and Guidelines Using Relevant Ethnic Controls. Cancer Res Treat. 2017;49(4):1012–21. 10.4143/crt.2016.433 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Rottenberg S, Jaspers JE, Kersbergen A, van der Burg E, Nygren AO, Zander SA, et al. High sensitivity of BRCA1-deficient mammary tumors to the PARP inhibitor AZD2281 alone and in combination with platinum drugs. Proc Natl Acad Sci U S A. 2008;105(44):17079–84. 10.1073/pnas.0806092105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Erriquez J, Olivero M, Mittica G, Scalzo MS, Vaira M, De Simone M, et al. Xenopatients show the need for precision medicine approach to chemotherapy in ovarian cancer. Oncotarget. 2016;7(18):26181–91. 10.18632/oncotarget.8325 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.S A. FastQC: a quality control tool for high throughput sequence data. 2010. Available from: http://www.bioinformatics.babraham.ac.uk/projects/fastqc.
- 36.Martin M. Cutadapt removes adapter sequences from high-throughput sequencing reads. 2011. 2011;17(1). 10.14806/ej.17.1.200 pp. 10–12. [DOI] [Google Scholar]
- 37.Bushnell B. BBMap: A Fast, Accurate, Splice-Aware Aligner. 2014 LBNL-7065E.
- 38.Cancer Genome Atlas N. [cited 2019 30, August]. Available from: https://portal.gdc.cancer.gov/genes/ENSG00000012048.
- 39.McAuliffe PF, Evans KW, Akcakanat A, Chen K, Zheng X, Zhao H, et al. Ability to Generate Patient-Derived Breast Cancer Xenografts Is Enhanced in Chemoresistant Disease and Predicts Poor Patient Outcomes. PLoS One. 2015;10(9):e0136851 10.1371/journal.pone.0136851 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Park B, Jeong BC, Choi YL, Kwon GY, Lim JE, Seo SI, et al. Development and characterization of a bladder cancer xenograft model using patient-derived tumor tissue. Cancer Sci. 2013;104(5):631–8. 10.1111/cas.12123 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Jun E, Jung J, Jeong SY, Choi EK, Kim MB, Lee JS, et al. Surgical and Oncological Factors Affecting the Successful Engraftment of Patient-derived Xenografts in Pancreatic Ductal Adenocarcinoma. Anticancer Res. 2016;36(2):517–21. . [PubMed] [Google Scholar]
- 42.Creighton CJ, Li X, Landis M, Dixon JM, Neumeister VM, Sjolund A, et al. Residual breast cancers after conventional therapy display mesenchymal as well as tumor-initiating features. Proc Natl Acad Sci U S A. 2009;106(33):13820–5. 10.1073/pnas.0905718106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Landis MD, Lehmann BD, Pietenpol JA, Chang JC. Patient-derived breast tumor xenografts facilitating personalized cancer therapy. Breast Cancer Res. 2013;15(1):201 10.1186/bcr3355 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Moon HG, Oh K, Lee J, Lee M, Kim JY, Yoo TK, et al. Prognostic and functional importance of the engraftment-associated genes in the patient-derived xenograft models of triple-negative breast cancers. Breast Cancer Res Treat. 2015;154(1):13–22. 10.1007/s10549-015-3585-y . [DOI] [PubMed] [Google Scholar]
- 45.Assayag F, Nicolas A, Vacher S, Dehainault C, Bieche I, Meseure D, et al. Combination of Carboplatin and Bevacizumab Is an Efficient Therapeutic Approach in Retinoblastoma Patient-Derived Xenografts. Invest Ophthalmol Vis Sci. 2016;57(11):4916–26. 10.1167/iovs.15-18725 . [DOI] [PubMed] [Google Scholar]
- 46.Ibrahim YH, Garcia-Garcia C, Serra V, He L, Torres-Lockhart K, Prat A, et al. PI3K inhibition impairs BRCA1/2 expression and sensitizes BRCA-proficient triple-negative breast cancer to PARP inhibition. Cancer Discov. 2012;2(11):1036–47. 10.1158/2159-8290.CD-11-0348 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Juvekar A, Burga LN, Hu H, Lunsford EP, Ibrahim YH, Balmana J, et al. Combining a PI3K inhibitor with a PARP inhibitor provides an effective therapy for BRCA1-related breast cancer. Cancer Discov. 2012;2(11):1048–63. 10.1158/2159-8290.CD-11-0336 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Goetz MP, Kalari KR, Suman VJ, Moyer AM, Yu J, Visscher DW, et al. Tumor Sequencing and Patient-Derived Xenografts in the Neoadjuvant Treatment of Breast Cancer. J Natl Cancer Inst. 2017;109(7). 10.1093/jnci/djw306 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Robson M, Im SA, Senkus E, Xu B, Domchek SM, Masuda N, et al. Olaparib for Metastatic Breast Cancer in Patients with a Germline BRCA Mutation. N Engl J Med. 2017;377(6):523–33. 10.1056/NEJMoa1706450 . [DOI] [PubMed] [Google Scholar]
- 50.Guan Z, Lan H, Chen X, Jiang X, Wang X, Jin K. Individualized drug screening based on next generation sequencing and patient derived xenograft model for pancreatic cancer with bone metastasis. Mol Med Rep. 2017;16(4):4784–90. 10.3892/mmr.2017.7213 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Xie T, Musteanu M, Lopez-Casas PP, Shields DJ, Olson P, Rejto PA, et al. Whole Exome Sequencing of Rapid Autopsy Tumors and Xenograft Models Reveals Possible Driver Mutations Underlying Tumor Progression. PLoS One. 2015;10(11):e0142631 10.1371/journal.pone.0142631 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Morton JJ, Bird G, Keysar SB, Astling DP, Lyons TR, Anderson RT, et al. XactMice: humanizing mouse bone marrow enables microenvironment reconstitution in a patient-derived xenograft model of head and neck cancer. Oncogene. 2016;35(3):290–300. 10.1038/onc.2015.94 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Morton JJ, Bird G, Refaeli Y, Jimeno A. Humanized Mouse Xenograft Models: Narrowing the Tumor-Microenvironment Gap. Cancer Res. 2016;76(21):6153–8. 10.1158/0008-5472.CAN-16-1260 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Choi YY, Lee JE, Kim H, Sim MH, Kim KK, Lee G, et al. Establishment and characterisation of patient-derived xenografts as paraclinical models for gastric cancer. Sci Rep. 2016;6:22172 10.1038/srep22172 [DOI] [PMC free article] [PubMed] [Google Scholar]