Abstract
Neglected tropical diseases (NTDs) are a diverse group of infectious conditions that vary in their epidemiology, impact and control. They are among the most common conditions globally, affecting approximately one billion people. Many NTDs have long-term consequences, such as visual and physical impairments. As a result, people with NTDs may have difficulties in carrying out activities or participating in society—in other words, NTDs can cause disabilities. Additionally, NTDs are often strongly linked to stigma and can have mental health consequences. It is therefore important to incorporate rehabilitation within NTD programmes. Rehabilitation can be conceptualized narrowly in terms of the provision of clinical services (e.g. physiotherapy and assistive devices) or, more broadly, including efforts to improve employment, overcome stigma and enhance social participation of people with disabilities. Approximately 15% of the global population has a disability, and this large group must be considered when designing NTD programmes. Improving the inclusion of people with disabilities may require adaptations to NTD programmes, such as making them physically accessible or training staff about disability awareness. Without incorporating disability within NTD programmes, the quality of life of people with NTDs will suffer and global targets for elimination and management of NTDs will not be met.
Keywords: disability, impairment, neglected tropical disease, rehabilitation
Introduction
Neglected tropical diseases (NTDs) are a diverse group of infectious conditions that vary in their distribution, epidemiology, impact and control. Collectively they are among the most common diseases globally,1 with the World Health Organization (WHO) estimating that one billion people are affected by NTDs. NTDs share common features: they are treatable or preventable through relatively simple public health interventions and are concentrated in the poorest countries and among the poorest people. Moreover, they are neglected, meaning that they are reported late and diagnosed and treated late, so NTDs often lead to chronic conditions, although rarely to death. This feature distinguishes NTDs from other high-profile infectious diseases, such as human immunodeficiency virus, malaria and tuberculosis, which are often fatal. Essentially NTDs are common, avoidable and potentially debilitating, which is why prioritizing their control is important. As a result, the last decade has witnessed an extraordinary increase in the attention given to NTDs, including an initiative by the WHO for the control, elimination and eradication of 17 NTDs by 2020.2
There are many overlaps and similarities between NTDs and disability. Like NTDs, disability affects about one billion people and is concentrated among the poorest in the world.3 Disability is also receiving growing international attention, with a high-profile Global Disability Summit arranged by the UK government and convened in London on 24 July 2018 to draw attention to this global issue. The aim of this review is to reflect on the connections between disability and NTDs. The review will put NTDs explicitly within a disability framework to consider which strategies could or should be put in place for NTD control to more holistically meet the needs of patients. It will also discuss the adaptation of NTD control programmes to be inclusive of people with disabilities and what the potential gains are of taking this approach. A formal systematic review was not undertaken, due to the lack of specificity of the search terms for NTDs and disabilities, thus a scoping review of the relevant literature was conducted.
What is disability and why is it important?
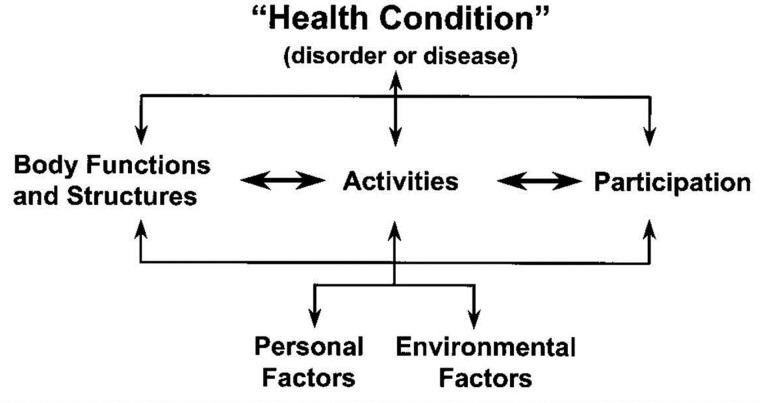
There are many different ways of conceptualizing disability. The most common way of describing disability is through the International Classification of Functioning, Disability and Health (ICF) model of the WHO (Figure 1).4
Figure 1.
International Classification of Functioning, Disability and Health (ICF) model.
Essentially, a health condition can lead to an abnormality in body functions and structures. For instance, repeated infection with Chlamydia trachomatis can, over time, cause trichiasis, where the eyelid rotates and the eyelashes scratch against the eye. Trichiasis can lead to corneal ulceration and ultimately to corneal opacity and blindness. In this example, trachoma infection is the health condition and blindness is the abnormality in body function and structure, that is, the impairment. People who are blind can experience difficulties in performing activities, such as walking independently. These activity limitations can cause participation restrictions, such as difficulties in working or joining in social events. As a consequence, people with disabilities are being left behind, including in terms of schooling, and employment, and they are more likely to be poor.3 The impact of blindness on participation restriction and exclusion is not the same for everyone, but is influenced by personal and environmental factors. For instance, people with positive personal factors, such as high levels of social support or personal wealth, may be enabled to participate in events despite their blindness. Similarly, the provision of mobility devices (e.g. white canes) and an accessible physical environment, will help people to engage in activities.
Using this framework, it is clear that most of the NTDs can cause impairments. As examples, Buruli ulcer starts with a skin infection that can lead to extensive tissue necrosis and ultimately potentially to damage to the eye and amputation and contracture at the knee and ankle joints. Guinea worm infection is initially symptom free, but about 1 y later can cause painful blistering of the skin, vomiting and dizziness, with consequent difficulties in walking. A study of 982 people infected with Guinea worm in Nigeria found that 21% were ‘totally incapacitated’, 20% were ‘seriously disabled’, 44% had ‘mild incapacity’ and only 16% were unaffected.5 Overall, most of the 17 main NTDs can lead directly to impairments: trachoma and onchocerciasis can cause blindness, while leprosy, chikungunya, yaws, lymphatic filariasis, Buruli ulcer, Chagas disease and African trypanosomiasis can lead to physical impairments. NTDs can also cause impairments indirectly. Soil-transmitted helminths and schistosomiasis in childhood can lead to delayed physical and mental development and a predisposition to developmental disabilities. NTDs are also linked to mental health conditions, particularly depression, whether through the direct effects of disease (e.g. neurological sequelae) or as a result of the pain, discomfort and stigma experienced.6
There are many examples of how NTD-related impairments can lead to activity limitations and participation restriction and thus negatively impact on well-being. Schistosomiasis infection may cause abdominal pain, diarrhoea and blood in the stool or urine. In children, it is also linked to poorer learning and memory, as well as lower school attendance and achievement,7,8 which may impact on well-being. For instance, a survey of adults in Cote D’Ivoire showed lower quality of life associated with schistosomiasis infection.9 Sleeping sickness causes pain, amnesia and physical impairments, and a Zambian study showed that infection was linked to loss of productive time, dropping out of school, loss of friends and lower self-esteem.10 Lymphatic filariasis infection can cause lymphedema (swelling in body tissue), scrotal hydrocele (swelling in the scrotum) and rheumatic and respiratory problems. These symptoms can result in difficulties walking, with the added effect of reduced economic productivity.11,12 For instance, a study in Malawi showed that people with lymphatic filariasis earned less than half the amount of unaffected controls per week (cases, $0.70; controls, $1.86) but spent more money on health care (16% vs 22%).13
People with NTDs also often face stigmatizing attitudes and social exclusion,14 and this is often a key concern for those affected. Perhaps the clearest example of stigma is for leprosy.15 Leprosy can cause damage to the eyes, hands and feet, with consequent difficulties in social and economic participation.16 Additionally, stigma is repeatedly shown to be pronounced among people living with leprosy,17,18 perhaps because it causes visible symptoms and there is a great fear of contagion. The Stigma Assessment and Reduction of Impact (SARI) study in Indonesia collected quantitative data and undertook in-depth qualitative interviews (n=49).16 The study showed that 36% of people living with leprosy experienced stigma, specifically related to problems in marriage, difficulties in employment and shame. These quantitative findings are supported by evidence from the in-depth interviews, as described by one source from Indonesia:
‘If he is badly affected and people know that he is affected by leprosy, he will not have any friends’.19
While another stated:
‘People who are affected by leprosy should be banished to the forest [laughs]. They should not live together with other people in the village. Their houses should also be burnt. That was what my parents told me’.
This stigma is so widespread that the term ‘leper’ alone is an insult in many languages, and the expression of feeling ‘like a leper’ is a synonym for social exclusion. Stigma and discrimination is also a common experience for people with other NTDs, for instance, lymphatic filariasis. Symptoms of this condition may be distressing and stigmatizing, with several studies linking it to depression and anxiety12,20,21 and marital and sexual problems.11,22 A study in India found that hydrocele patients were viewed as the ‘last choice’ of a partner to marry.22 Stigma in relation to NTDs is described well by a woman in Uganda reflecting about the lives of people with skin conditions, resulting from onchocerciasis:
‘They are hiding their skin so that people cannot see them. I have not heard of anyone who wants others to know about it. No one will allow them to lead, and many people ignore them. They are considered dangerous. People fear contact with them. I feel sorry for them. Even me, I feared that from staying and meeting them we could get the disease … They find it hard to marry, and marriages can break because of this condition’.15
Stigma related to disabilities and its impacts may vary between men and women. One study on leprosy conducted in Nepal, Indonesia, Nigeria and Brazil found that stigma resulted in more delayed care-seeking in men than in women.23 Moreover, affected men were more concerned about losing their jobs or social status in the community, while affected women worried more about the impact on their domestic roles (e.g. relationship with mother-in-law). Despite these tantalizing findings, data addressing gender differences in stigma resulting from NTD-related disabilities is sparse and does not always show strong gender differences. For instance, a study from Bangladesh showed high levels of stigma among people with leprosy and demonstrated that this impacted negatively on quality of life, but it did not identify clear gender differences in these associations.24
Incorporation of rehabilitation in NTD programmes
The previous section highlighted that NTDs are potentially disabling, with implications in terms of reduced economic productivity, poorer quality of life, social exclusion, negative mental health impacts and high levels of stigma. These impacts are not surprising to NTD researchers and they may question why it is useful to place NTDs within a disability framework. The main reason is to allow us to think in a more structured way about the disabling impacts of NTDs and how they can be alleviated, using the ICF model as a guide.
As an example, a large study was conducted to assess the impact of trichiasis in Ethiopia.25–28 A total of 1000 adults with trichiasis and 200 comparison subjects were recruited and all patients received free trichiasis surgery. The impact of trichiasis in the lives of people was pronounced. At baseline, people with trichiasis were significantly poorer, participated less in economic activities, experienced more difficulties in undertaking activities and needed more assistance as compared with controls without trichiasis.25 Trichiasis was also strongly linked to reduced vision-related and health-related quality of life, even in the absence of visual impairment.26 These data show that trichiasis itself is disabling, even when vision is unaffected. After trichiasis surgery, people reported improved participation in economic activities (e.g. farming, fetching wood), being able to perform activities without assistance (e.g. animal rearing, farming)27 and better quality of life.28 These changes were mostly independent of improvements in visual acuity and were likely driven at least in part by the alleviation of ocular pain resulting from the surgery (ocular pain was experienced by 99% of cases at baseline and 34% after surgery). In other words, trichiasis surgery can help to alleviate disability. Putting an NTD program within a disability framework thus provides additional rationale for investing in NTD treatment, as the programme can alleviate disability as well as prevent specific health conditions or impairments. In the example of trichiasis, surgery does not just prevent blindness, but also can improve quality of life. This is also true for other NTDs; for instance, ivermectin treatment reduces the risk of blindness, but also alleviates symptoms of extreme itchiness among people with onchocerciasis and thus improves well-being.
Another reason why the ICF disability framework is important is because many NTD-related impairments cannot be avoided and there are already millions of people living with disabilities related to NTDs around the world. Turning to the ICF framework, strengthening ‘personal’ and ‘environmental’ factors can help to improve activities and participation, even when the impairment cannot be reduced. In other words, rehabilitation may help to alleviate disability in people with untreatable impairments. The WHO defines rehabilitation as ‘a set of measures that assist individuals, who experience or are likely to experience disability, to achieve and maintain optimum functioning in interaction with their environment.’3 Rehabilitation can be conceptualized narrowly from a clinical perspective, with a focus on services such as physiotherapy, speech and language therapy, psychological support and provision of orthoses, prostheses and assistive devices. Rehabilitation can also be thought of more broadly, including initiatives to overcome stigma and discrimination, improve participation (e.g. in education, employment, social life) and provide social assistance. In either case, the focus of rehabilitation is to improve the functioning of people with disabilities by addressing personal (e.g. wealth, training) and environmental factors (e.g. assistive technologies) and thereby improve their activities, participation and quality of life.
A clear recommendation for NTD programmes is therefore that they should link people with NTD-related impairments to clinical rehabilitation services, as these links are currently often lacking. For instance, an overview of existing programmes for lymphatic filariasis found that only 26 of 81 endemic countries had morbidity programmes in place at all.29 Additionally, programs may consider screening people more regularly for impairments to identify need. Clinical tools, such as to assess the presence of hearing, visual or physical impairments, are broadly available to routinely screen NTD clients,30 including using smartphone tools (e.g. Peek Vision and hearScreen).
Management of physical symptoms alone is insufficient, however, as not all symptoms can be cured, and a major impact of NTDs is in creating stigma, and thereby discrimination. Some NTD programmes, in particular leprosy programmes, have made attempts to implement strategies to reduce stigma,31 often relying on raising awareness about a condition to take away the fear and ignorance, and thus reduce stigma. The SARI trial in Indonesia showed that increasing ‘contact events’ between people with and without leprosy, such as through giving testimonies, developing participatory videos or comics, improved knowledge about leprosy in the general population and reduced negative attitudes.19 Qualitative interviews undertaken as part of the trial also supported the benefits of the intervention. As one community member said,
‘This [contact event] is very good, I understand more. I used to be very afraid to visit someone who has leprosy, but now I am not afraid’.
A study in Nepal showed that women living with leprosy reported high levels of problems in their marital and sexual relationships, including due to fear of leprosy, and thus advocated for education and counselling at the point of diagnosis in order to reduce stigma.18 Anecdotally, in Brazil, parents of children with disabilities related to Zika report experiencing less stigma and more social support than parents of children with other disabilities (e.g. cerebral palsy), presumably because of the high levels of knowledge and awareness about Zika within the general population. NTD programmes should therefore consider implementing specific strategies to raise awareness about the condition and thereby reduce stigma. NTD programmes may also consider strengthening links with mental health services to enhance the well-being of service users.
Some NTD programmes have gone further still and have incorporated more holistic rehabilitation into their control strategy. Onchocerciasis was extremely widespread and a major cause of blindness in Africa before the implementation of the successful African Programme for Onchocerciasis Control. Onchocerciasis is highly clustered geographically and is most common close to rivers (which was why it was called ‘river blindness’), where the land is also the most fertile. Eventually, in some communities, large proportions of the adults became blind and communities began to abandon the most fertile lands available. As a result, Agricultural Rehabilitation of the Blind (ARB) was established for men blinded by onchocerciasis in Ghana and Burkina Faso in the 1970s. Activities included training people in mobility, agricultural and handicraft techniques at residential courses and in the people’s home villages. Over time these programmes became the basis from which community-based rehabilitation (CBR) was developed by the WHO in the 1980s. CBR has a broader scope than the original ARB programmes and tries to address the holistic needs of people with disabilities in terms of health, education, livelihood, social inclusion and empowerment through the development of community-based and community-led projects.32 As an example of a CBR programme for NTDs, Lepra, a leprosy focused charity, offers programmes that focus on both the diagnosis and treatment of leprosy, but also on tackling stigma and discrimination and providing means to improve livelihoods.
Currently, integration of rehabilitation within NTD programmes is lacking, for several reasons. The focus on NTD programmes is mostly to prevent and treat, in the belief that if these are effective, then rehabilitation will not be needed. However, not all cases of NTDs can be avoided, and many people are already disabled as a result of NTDs. Another constraint is that disability and morbidity have not been measured routinely in NTD programmes, and as the adage goes, ‘what isn’t counted doesn’t count’. The lack of data hampers advocacy, as well as planning for interventions, monitoring and evaluating the impact of programmes and identifying funding.33 Different tools are available to collect data on disability in NTD programmes. For instance, the WHO Disability Assessment Schedule (WHODAS), WHO Quality of Life (WHOQOL) and Participation Scale (P-scale) have been used to measure quantitatively the impact of NTDs (and NTD programmes) on quality of life, activities and participation. It is also important to use qualitative tools to capture the broader impact of NTDs through people’s own stories and experiences, as well as to understand barriers to uptake or effectiveness of services. Consensus is needed on which tools should be used in order to scale up comparable data collection.33 Finally, there is a lack of rigorous evidence of what works to alleviate disability among people with NTDs. As one example, a systematic review identified only three studies that assessed the cost-effectiveness of interventions to improve functioning in people with leprosy, and these studies were generally small and of poor quality.34 The literature for other NTDs is likely to be poorer still. A clear recommendation is that more research is needed on the disabling impacts of NTDs and how these can be overcome in order to support the expansion of NTD programmes to incorporate rehabilitation.
Consideration of people with disabilities when designing NTD programmes
People with disabilities make up 15% of the global population.3 On average, therefore, one in seven people targeted by NTD programmes will have disabilities. This proportion could be higher still, as both NTDs and disability are more common among the poorest sectors of society. The upshot is that consideration needs to be given to the inclusion of people with disabilities in mass drug administration and other NTD control programmes. If people with disabilities are not included in programmes, then the global targets for elimination and management of NTDs will not be met.
People with disabilities can face a range of barriers to taking part in NTD programmes. They are not a homogeneous group and include people varying by impairment type, age, gender, religion, and so on, and so the exact barriers faced will vary for different people and in different settings. However, broadly speaking, common barriers facing people with disabilities to inclusion in NTD programmes are physical inaccessibility, communication barriers, stigmatizing attitudes and discrimination, financial constraints and lack of knowledge of health care professionals. Therefore NTD programmes need to identify the most common barriers and put in place mechanisms to overcome these barriers. For instance, programmes may have to tackle physical barriers (e.g. ensuring treatment distribution points are accessible), provide communications in a range of formats (e.g. visual, radio) and include images of people with disabilities in campaign pictures to highlight that the programme is for everyone. These changes will make NTD programmes more accessible to people with disabilities, but will also improve inclusion for other people, such as older people, minority language speakers and people with short-term health conditions, and so improve the overall reach of NTD programmes. People with disabilities must be included in the planning, and potentially the delivery, of NTD programmes, to ensure that the key barriers are identified and appropriately addressed.
Monitoring inclusion is important to check whether these efforts are working. Sightsavers has monitored whether people with disabilities are included in their trichiasis camps within its trachoma programme in Tanzania, using a standardized approach to assessing disability (the Washington Group Short Set35).36 They found that approximately 14% of people undergoing trichiasis surgery had a disability (i.e. reported a lot of difficulty or more in at least one of six domains). This proportion was comparable to the prevalence of disability in a large survey in the general population in Tanzania with similar age groups, indicating that the trichiasis service was inclusive of people with disabilities. The data also helped programme managers consider what other services may be needed for their clients. As the regional NTD coordinator in Tanzania said,
‘We provide eye services but a client could have other issues while for us [previously] we prioritized eyes. We never realized that behind the scene this person has other problems. Knowing the results and getting data about disability has opened our mind on health provision’.
‘The data can be used to improve eye services to the camps … Data can be triangulated and other services provided’.
The Department for International Development and other international agencies are now advocating for the collection of data on disability in programmes to ensure that they are inclusive, and this is also encouraged within the Sustainable Development Goals. More case studies are needed on how this data collection should be achieved. We also need more evidence on what the common barriers are facing people with disabilities in inclusion in NTD programmes and how these may best be overcome.
Conclusions
Many NTDs are potentially disabling. It is therefore important to expand the focus of NTD programmes to incorporate rehabilitation, as this will help improve the quality of life of people living with NTDs. People with disabilities make up 15% of the global population and thus a priority for NTD programmes is to ensure that they are inclusive of people with disabilities so that a greater proportion of the population is reached and NTD targets are more likely to be met. Harnessing the current momentum behind both disability and NTDs will make both sectors stronger and help make sure that no one is left behind as we move towards NTD control.
Author’s contributions: HK conceived the review, conducted the literature search and wrote the article.
Acknowledgments: This review is based on the blog written for the London Centre for Neglected Tropical Disease Research, an innovative research collaboration between Imperial College London, the London School of Hygiene and Tropical Medicine, the Natural History Museum and the Royal Veterinary College.
Funding: Hannah Kuper is supported by the PENDA study, funded by the Department for International Development.
Competing interests: None declared.
Ethical approval: Not required.
References
- 1. Herricks JR, Hotez PJ, Wanga V, et al. . The global burden of disease study 2013: what does it mean for the NTDs? PLoS Negl Trop Dis. 2017;11(8):e0005424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. World Health Organization Accelerating work to overcome the global impact of neglected tropical diseases. A roadmap for implementation. Geneva: World Health Organization; 2012. [Google Scholar]
- 3. World Health Organization World report on disability. Geneva: World Health Organization; 2011. [Google Scholar]
- 4. World Health Organization International Classification of Functioning, Disability and Health. Geneva: W World Health Organization; 2001. [Google Scholar]
- 5. Okoye SN, Onwuliri CO, Anosike JC. A survey of predilection sites and degree of disability associated with guineaworm (Dracunculus medinensis). Int J Parasitol. 1995;25(9):1127–9. [DOI] [PubMed] [Google Scholar]
- 6. Litt E, Baker MC, Molyneux D. Neglected tropical diseases and mental health: a perspective on comorbidity. Trends Parasitol. 2012;28(5):195–201. [DOI] [PubMed] [Google Scholar]
- 7. Pabalan N, Singian E, Tabangay L, et al. . Soil-transmitted helminth infection, loss of education and cognitive impairment in school-aged children: a systematic review and meta-analysis. PLoS Negl Trop Dis. 2018;12(1):e0005523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Ezeamama AE, Bustinduy AL, Nkwata AK, et al. . Cognitive deficits and educational loss in children with schistosome infection—a systematic review and meta-analysis. PLoS Negl Trop Dis. 2018;12(1):e0005524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Furst T, Silue KD, Ouattara M, et al. . Schistosomiasis, soil-transmitted helminthiasis, and sociodemographic factors influence quality of life of adults in Cote d’Ivoire. PLoS Negl Trop Dis. 2012;6(10):e1855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Mwiinde AM, Simuunza M, Namangala B, et al. . Estimating the economic and social consequences for patients diagnosed with human African trypanosomiasis in Muchinga, Lusaka and eastern provinces of Zambia (2004–2014). Infect Dis Poverty. 2017;6(1):150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Wijesinghe RS, Wickremasinghe AR, Ekanayake S, et al. . Physical disability and psychosocial impact due to chronic filarial lymphoedema in Sri Lanka. Filaria J. 2007;6:4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Martindale S, Mkwanda SZ, Smith E, et al. . Quantifying the physical and socio-economic burden of filarial lymphoedema in Chikwawa District, Malawi. Trans R Soc Trop Med Hyg. 2014;108(12):759–67. [DOI] [PubMed] [Google Scholar]
- 13. Stanton MC, Yamauchi M, Mkwanda SZ, et al. . Measuring the physical and economic impact of filarial lymphoedema in Chikwawa district, Malawi: a case-control study. Infect Dis Poverty. 2017;6(1):28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Hofstraat K, van Brakel WH. Social stigma towards neglected tropical diseases: a systematic review. Int Health. 2016;8(Suppl 1):i53–70. [DOI] [PubMed] [Google Scholar]
- 15. Weiss MG. Stigma and the social burden of neglected tropical diseases. PLoS Negl Trop Dis. 2008;2(5):e237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. van Brakel WH, Sihombing B, Djarir H, et al. . Disability in people affected by leprosy: the role of impairment, activity, social participation, stigma and discrimination. Glob Health Action. 2012;5:10.3402/gha.v5i0.18394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Stevelink SA, van Brakel WH, Augustine V. Stigma and social participation in southern India: differences and commonalities among persons affected by leprosy and persons living with HIV/AIDS. Psychol Health Med. 2011;16(6):695–707. [DOI] [PubMed] [Google Scholar]
- 18. van ’t Noordende AT, van Brakel WH, Banstola N, et al. . The impact of leprosy on marital relationships and sexual health among married women in eastern Nepal. J Trop Med. 2016;2016:4230235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Peters RMH, Dadun , Zweekhorst MBM, et al. . A cluster-randomized controlled intervention study to assess the effect of a contact intervention in reducing leprosy-related stigma in Indonesia. PLoS Negl Trop Dis. 2015;9(10):e0004003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Obindo J, Abdulmalik J, Nwefoh E, et al. . Prevalence of depression and associated clinical and socio-demographic factors in people living with lymphatic filariasis in Plateau State, Nigeria. PLoS Negl Trop Dis. 2017;11(6):e0005567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Ton TG, Mackenzie C, Molyneux DH. The burden of mental health in lymphatic filariasis. Infect Dis Poverty. 2015;4:34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Babu BV, Mishra S, Nayak AN. Marriage, sex, and hydrocele: an ethnographic study on the effect of filarial hydrocele on conjugal life and marriageability from Orissa, India. PLoS Negl Trop Dis. 2009;3(4):e414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Varkevisser CM, Lever P, Alubo O, et al. . Gender and leprosy: case studies in Indonesia, Nigeria, Nepal and Brazil. Lepr Rev. 2009;80(1):65–76. [PubMed] [Google Scholar]
- 24. Tsutsumi A, Izutsu T, Islam AM, et al. . The quality of life, mental health, and perceived stigma of leprosy patients in Bangladesh. Soc Sci Med. 2007;64(12):2443–53. [DOI] [PubMed] [Google Scholar]
- 25. Habtamu E, Wondie T, Aweke S, et al. . Trachoma and relative poverty: a case-control study. PLoS Negl Trop Dis. 2015;9(11):e0004228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Habtamu E, Wondie T, Aweke S, et al. . The impact of trachomatous trichiasis on quality of life: a case control study. PLoS Negl Trop Dis. 2015;9(11):e0004254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Habtamu E, Wondie T, Aweke S, et al. . Impact of trichiasis surgery on daily living: a longitudinal study in Ethiopia. Wellcome Open Res. 2017;2:69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Habtamu E, Wondie T, Aweke S, et al. . Impact of trichiasis surgery on quality of life: a longitudinal study in Ethiopia. PLoS Negl Trop Dis. 2016;10(4):e0004627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. World Health Organization WHO global programme to eliminate lymphatic filariasis progress report for 2000–2009 and strategic plan 2010–2020. Geneva: World Health Organization; 2010. [Google Scholar]
- 30. Mactaggart I, Kuper H, Murthy GV, et al. . Measuring disability in population based surveys: the interrelationship between clinical impairments and reported functional limitations in Cameroon and India. PLoS One. 2016;11(10):e0164470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Sermrittirong S, Van Brakel WH, Bunbers-Aelen JF. How to reduce stigma in leprosy—a systematic literature review. Lepr Rev. 2014;85(3):149–57. [PubMed] [Google Scholar]
- 32. World Health Organization Community-based rehabilitation guidelines. Geneva: World Health Organization; 2010. [Google Scholar]
- 33. van ’t Noordende AT, Kuiper H, Ramos AN Jr, et al. . Towards a toolkit for cross-neglected tropical disease morbidity and disability assessment. Int Health. 2016;8(Suppl 1):i71–81. [DOI] [PubMed] [Google Scholar]
- 34. van Veen NH, McNamee P, Richardus JH, et al. . Cost-effectiveness of interventions to prevent disability in leprosy: a systematic review. PLoS One. 2009;4(2):e4548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Washington Group Question sets of the Washington Group 2017 [cited 2017 June 29]. Available from: http://www.washingtongroup-disability.com/washington-group-question-sets/.
- 36. Sightsavers Everybody counts. Disability disaggregation of data pilot projects in India and Tanzania. 2016. Available from: https://www.sightsavers.org/wp-content/uploads/2017/09/everybodycounts_brochure_accessible_web.pdf.