Abstract
Background
Acetabular version influences joint mechanics and the risk of impingement. Cross-sectional studies have reported an increase in acetabular version during adolescence; however, to our knowledge no longitudinal study has assessed version or how the change in version occurs. Knowing this would be important because characterizing the normal developmental process of the acetabulum would allow for easier recognition of a morphologic abnormality.
Questions/purposes
To determine (1) how acetabular version changes during adolescence, (2) calculate how acetabular coverage of the femoral head changed during this period, and (3) to identify whether demographic factors or hip ROM are associated with acetabular development.
Methods
This retrospective analysis of data from a longitudinal study included 17 volunteers (34 hips) with a mean (± SD) age of 11 ± 2 years; seven were male and 10 were female. The participants underwent a clinical examination of BMI and ROM and MRIs of both hips at recruitment and at follow-up (6 ± 2 years). MR images were assessed to determine maturation of the triradiate cartilage complex, acetabular version, and degree of the anterior, posterior, and superior acetabular sector angles (reflecting degree of femoral head coverage provided by the acetabulum anteriorly, posteriorly and superiorly respectively). An orthopaedic fellow (GG) and a senior orthopaedic resident (PJ) performed all readings in consensus; 20 scans were re-analyzed for intraobserver reliability. Thereafter, a musculoskeletal radiologist (KR) repeated measurements in 10 scans to test interobserver reliability. The intra- and interobserver interclass correlation coefficients for absolute agreement were 0.85 (95% CI 0.76 to 0.91; p < 0.001) and 0.77 (95% CI 0.70 to 0.84), respectively. All volunteers underwent a clinical examination by a senior orthopaedic resident (PJ) to assess their range of internal rotation (in 90° of flexion) in the supine and prone positions using a goniometer. We tested investigated whether the change in anteversion and sector angles differed between genders and whether the changes were correlated with BMI or ROM using Pearson’s coefficient. The triradiate cartilage complex was open (Grade I) at baseline and closed (Grade III) at follow-up in all hips.
Results
The acetabular anteversion increased, moving caudally further away from the roof at both timepoints. The mean (range) anteversion angle increased from 7° ± 4° (0 to 18) at baseline to 12° ± 4° (5 to 22) at the follow-up examination (p < 0.001). The mean (range) anterior sector angle decreased from 72° ± 8° (57 to 87) at baseline to 65° ± 8° (50 to 81) at the final follow-up (p = 0.002). The mean (range) posterior (98° ± 5° [86 to 111] versus 97° ± 5° [89 to 109]; p = 0.8) and superior (121° ± 4° [114 to 129] to 124° ± 5° [111 to 134]; p = 0.07) sector angles remained unchanged. The change in the anterior sector angle correlated with the change in version (rho = 0.5; p = 0.02). The change in version was not associated with any of the tested patient factors (BMI, ROM).
Conclusions
With skeletal maturity, acetabular version increases, especially rostrally. This increase is associated with, and is likely a result of, a reduced anterior acetabular sector angle (that is, less coverage anteriorly, while the degree of coverage posteriorly remained the same). Thus, in patients were the normal developmental process is disturbed, a rim-trim might be an appropriate surgical solution, since the degree of posterior coverage is sufficient and no reorientation osteotomy would be necessary. However, further study on patients with retroversion (of various degrees) is necessary to characterize these observations further. The changes in version were not associated with any of the tested patient factors; however, further study with greater power is needed.
Level of Evidence
Level II, prognostic study.
Introduction
Femoroacetabular impingement (FAI) is a well-described clinical phenomenon [9] that is associated with premature osteoarthritis of the hip [8, 15]. The understanding of the underlying mechanisms leading to FAI continues to evolve; it is evident, however, that femoral (cam, retroversion) and acetabular (pincer, retroversion) anatomy may contribute to the development of FAI [8, 9, 15]. Several studies have described the development of cam deformities as the skeleton matures and the association of these deformities with increased activity during adolescence [5, 11, 21, 22]. However, considerably less is known about the development of the acetabulum and what changes occur during adolescence, which appears to be the key developmental stage[12].
Acetabular development occurs with the confluence of the ilium, ischium, and pubis, which form the triradiate cartilage complex, a Y-shaped structure [20, 25]. The depth of the acetabulum forms via interstitial growth of the triradiate cartilage complex, and acetabular concavity depends on its interaction and articulation with the spherical femoral head [20, 25]. During skeletal maturation, three secondary ossification centers appear: the os acetabuli (epiphysis of the pubis), acetabular epiphysis (epiphysis of the ilium), and epiphysis of the ischium [20, 25, 27]. Subtle variations in acetabular morphology that lead to pincer or acetabular retroversion may be a result of abnormal acetabular development in different regions; for example, acetabular retroversion may be a result of either increased anterior wall coverage and/or posterior wall deficiency or underdevelopment [6]. To better understand what contributes to the development of acetabular morphologic abnormalities, we must first better characterize what changes to the acetabular orientation occur during normal development and how these changes occur.
To date, two retrospective cross-sectional studies derived from CT data (hence missing the cartilaginous portions of the growing skeleton) noted that acetabular version was higher in skeletally mature hips than in skeletally immature hips [10, 19]. The authors noted that the increase in version was secondary to an increase in the size of the bony posterior rim; however, they recognized that this may be owing to CT’s inability to detect the cartilaginous posterior rim in the earlier stages of development [10]. A recent MRI-based study, with MRIs performed at the 1-year interval in patients at various developmental stages, showed that the acetabular version increases during adolescence, but did not identify how this may occur [2].
The current study, a retrospective analysis of a longitudinal study, aimed to determine (1) how acetabular version changes during adolescence, (2) calculate how acetabular coverage of the femoral head changed during this period, and (3) to identify demographic factors associated with acetabular development.
Patients and Methods
This was an institutional review board-approved, retrospective review of a longitudinal study. In 2014, we reported on the etiology of cam deformities by performing a prospective, cross-sectional MRI-based study [5]. In that study, cam deformities were only present in post-physeal closure hips, and none of the pre-physeal closure hips showed a cam deformity [5]. In this study, volunteers who had recovered from minor upper-limb trauma between July and December 2010 were recruited from the fracture clinic at a children’s hospital; all had asymptomatic lower extremities. Exclusion criteria for participation in the study included any previous fracture or vertebral fracture, history of lower-extremity conditions or surgery, known hip disorders, or any known musculoskeletal or rheumatologic or developmental disorders. An a priori power analysis for the primary research question of how acetabular version changed with skeletal maturity showed that with a level of significance set at p < 0.05, a β-error of 20%, and an expected increase from 14° ± 4° (pre-physeal closure) to 19° ± 4° (post-physeal closure) [10], eight hips would be the minimum sample required.
All 23 volunteers from the original report [5] who were at the pre-physeal closure stage were invited to participate in this follow-up study. Two patients were excluded from the study because of loss to follow-up. One patient moved away, and the other patient refused to return for a follow-up appointment; a further four patients had MR images of the hips that could not be retrieved from our archive. Thus, the study’s cohort comprised 17 volunteers (34 hips) who underwent longitudinal MRI of the pelvis. All participants presented for a follow-up clinical examination and underwent MRI of the hips. At the time of both the initial and follow-up clinical examinations, basic demographic data were recorded, including gender, age and BMI. Furthermore, all volunteers underwent a clinical examination by a senior orthopaedic resident (PJ) to assess their range of internal rotation (in 90° of flexion) in the supine and prone positions using a goniometer.
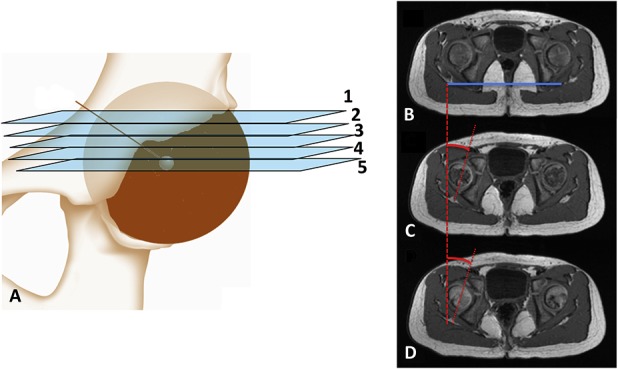
The mean (range) longitudinal follow-up duration was 6 years (2 to 10). The mean age at the initial assessment was 11 ± 1 years (8 to 13), while the mean (range) age at follow-up was 17 ± 1 years (14 to 19). The mean BMI increased from 19 ± 3 kg/m2 (14 to 27) at the initial examination to 24 ± 5 kg/m2 (18 to 37) at the follow-up examination (Table 1). The mean ±SD (range) of internal rotation reduced from 58° ± 14° (45 to 85) to 41° ± 10° (25 to 80) in the supine position and from 58° ± 14° (45 to 85) to 50° ± 11° (29 to 70) in the prone position.
Table 1.
Demographics: pre-physeal versus post-physeal closure
MRI
Each participant underwent MRI of both hips at both examinations using the same imaging protocol for each scan. No sedation or contrast was used. The imaging was performed with a 1.5-T MRI scanner (GE HDxt v15, 1.5 Tesla MRI; GE Healthcare, Milwaukee, WI, USA), with a phased-array surface coil placed anteriorly over the pelvis and spine-phased array coils situated posteriorly. Participants lay supine in the scanner with their feet in the neutral position. The MRI sequence was an axially acquired, 3-D isotropic, T1-weighted spoiled gradient with the following parameters: field of view, 40 cm; slice thickness, 1 mm; acquisition matrix, 384 x 256; and TR/TE/flip angle, 11.4 ms/4.0 ms/205°, 1 average. Multiplanar reformation was performed to generate radial, coronal, and sagittal images using the center of the femoral neck as the axis of rotation, with 2-mm-thick images generated at 30° intervals. All images were sent to out institutional PACS system (Siemens, Erlangen, Germany) for review.
Radiologic Assessments
The same assessments were performed for both the initial and follow-up MRIs. Images were reviewed (GG) to determine the status of the triradiate cartilage complex of the physis using the Oxford system, as originally described by Acheson [1, 23]; Grade 1 corresponds to an open physis, Grade 2 corresponds to a partially ossified physis, and Grade 3 corresponds to a closed physis. At the initial examination, all hips had a Grade I (open) triradiate cartilage complex; at the follow-up examination, all hips had a Grade III (closed) triradiate cartilage complex.
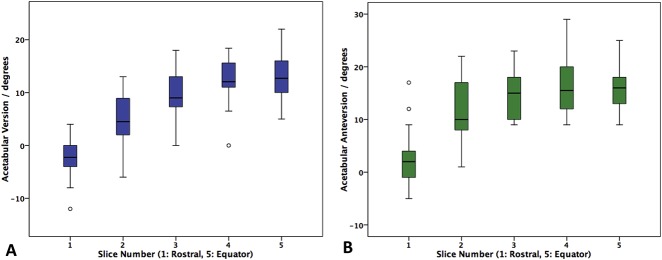
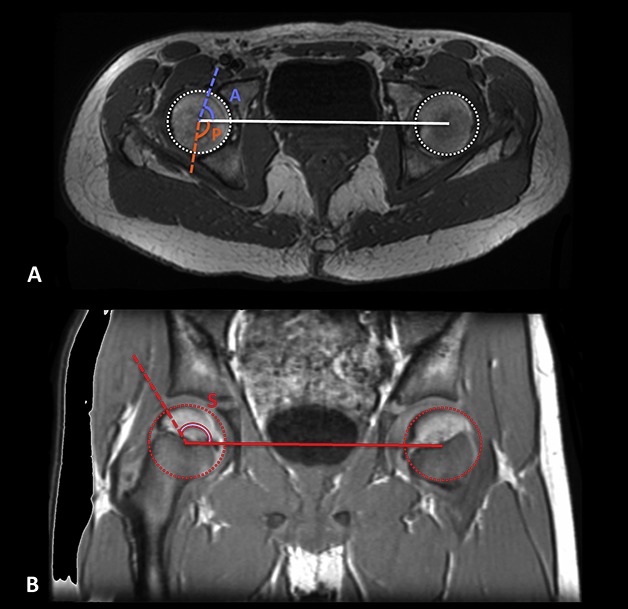
The acetabular version angles were determined in the axial plane by a line connecting the anterior and posterior margins of the cartilaginous acetabulum, correcting for rotation by accounting for the position of the ischial tuberosities (Fig. 1A-D). Acetabular version was measured 2 mm caudal to the roof of the acetabulum (Slice 1), at the equator of the hip (Slice 5), and at three equidistant levels (Slices 2-4) between these two locations. This method has been used for measuring acetabular orientation [16, 18] and is superior to using fixed distance levels (for example, 5 or 10 mm from the roof) because it is independent of acetabular size.
Fig. 1 A-D.
(A) A schematic of the acetabulum is shown. Acetabular version was measured 2 mm caudal to the roof of the acetabulum. (B) In this image, rotation of the pelvis from the ischial tuberosities was determined to determine version (θ) as illustrated in axial images (C) and (D) as the angle between the anterior and posterior rims.
Furthermore, three acetabular sector angles reflecting the degree of femoral head coverage that the acetabulum provides [3, 7, 10] were determined for each hip (Fig. 2A-B). The anterior acetabular sector angle was defined as the angle between a line connecting the center of each femoral head and a line from the center of the femoral head to the anterior margin of the bony acetabulum in the axial plane. The posterior acetabular sector angle was determined by the angle between the same centerline and the posterior margin of the bony acetabulum in the axial plane. Lastly, the superior acetabular sector angle was determined on the coronal reformatted images; it was calculated as the angle between the line connecting the center of the femoral head and a line from the center of the femoral head to the superior-lateral margin of the bony acetabulum.
Fig. 2 A-B.
(A) Axial and (B) coronal MR images illustrate measurement of the acetabular sector angles.
Reliability
All images were reviewed by an orthopaedic hip fellow with a subspecialty interest in hip surgery (GG), a senior orthopaedic resident (PJ), and a board-certified musculoskeletal radiologist (KR) to assess the adequacy of image quality and perform measurements. The fellow and resident performed all of the measurements in consensus. The intra- and inter observer reliability for the Acheson classification was excellent interclass correlation coefficients (ICC) of 1.00 (p < 0.001). To assess the reliability of the acetabular angular measurements, we tested 20 randomly selected hips for intraobserver reliability. Interobserver reliability was tested by the board-certified musculoskeletal radiologist (KR), who performed the measurements for 10 randomly selected hips. The intraobserver and interobserver ICC for absolute agreement were 0.85 (95% CI 0.76 to 0.91; p < 0.001) and 0.77 (95% CI 0.70 to 0.84), respectively.
Outcome Measures
The primary outcome measure was to study how the anteversion changed overall between the two intervals and for each of the five levels. Secondary measures were to determine (1) how the three sector angles changed over time and whether any of the morphological changes were associated with demographic or ROM measured.
Statistical Analysis
The statistical analysis was performed with Statistical Package for the Social Sciences (SPSS) version 23 (IBM Corp, Armonk, NY, USA). Nonparametric tests were used for the analysis. The Mann-Whitney U and Kruskal-Wallis tests were used for scale data, and the chi-square and Fisher’s exact tests were used for categorical data. Spearman’s (ρ) correlation was used to determine whether any correlations existed for scale data. Statistical significance was set at p < 0.05
Results
Determine How the Acetabular Version Changes During Adolescence
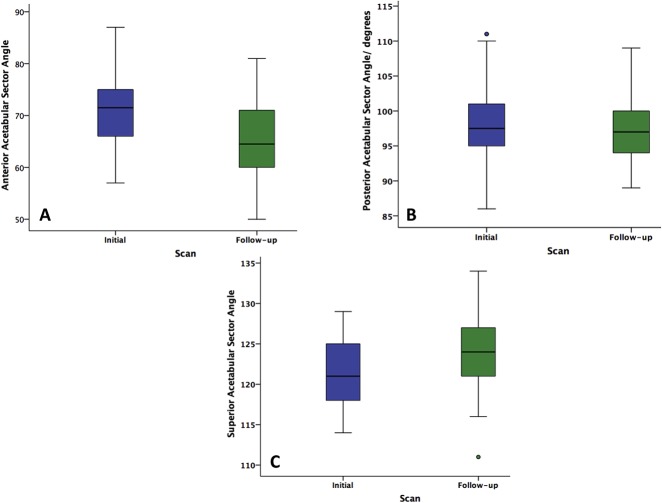
The mean anteversion angle increased from a mean (range) of 7° ± 4° (0 to 18) (initially) to 12° ± 4° (5 to 22) (at follow-up) (p < 0.001). The mean increase in the anteversion angle was 5°± 2° (0 to 9). Acetabular version increased, moving caudally and further away from the roof at both timepoints (Fig. 3A-B). Acetabular version differed at various levels (Table 2). An increase in version occurred, as seen on all MRI slices (range p < 0.001 to 0.003); the greatest increase occurred at the rostral one-fourth of the acetabulum (Slices 1 and 2) (Fig. 4). Eighteen percent of hips (six of 34) had evidence of acetabular retroversion of the rostral one-fourth of the acetabulum at the initial MRI, while none of the hips had retroversion at the follow-up MRI.
Fig. 3 A-B.
These box plots of acetabular version measurements were plotted for the different slice levels at (A) the initial MRI and (B) follow-up MRI.
Table 2.
Acetabular version at various levels along the acetabulum
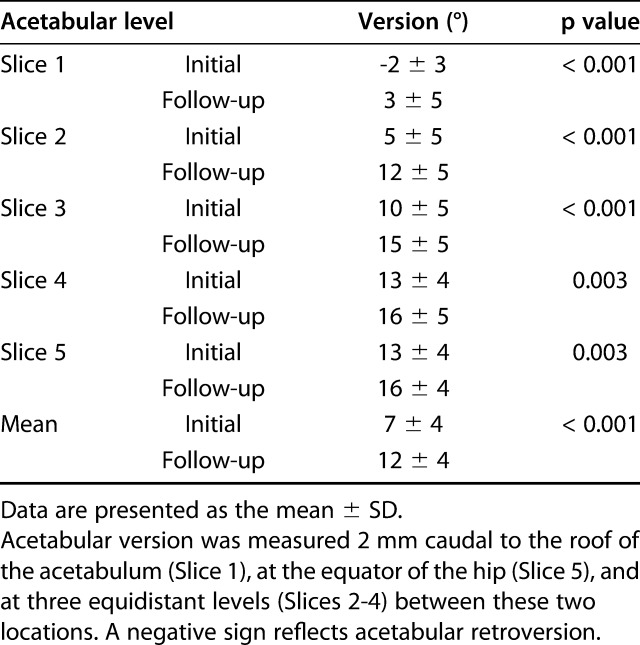
Fig. 4.
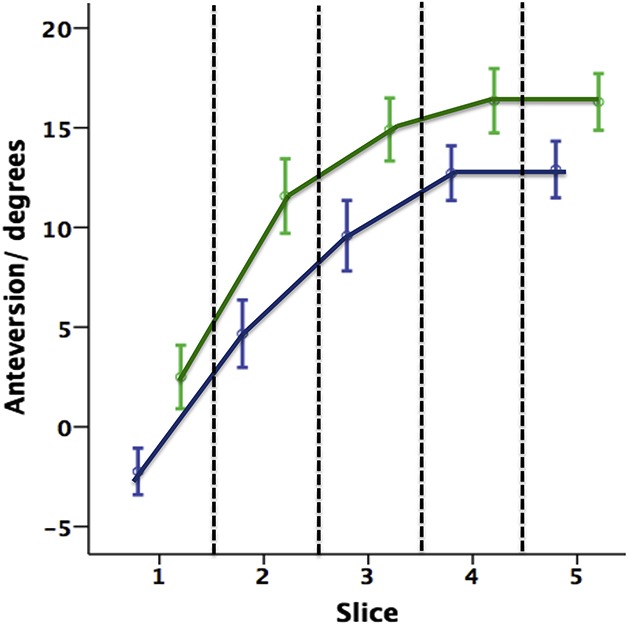
This box and whisker plot of anteversion measurements was plotted for different images of the acetabulum, color-coded per MR image. The initial image is indicated by the blue line; the follow-up image is represented by the green line.
Calculate How Acetabular Coverage of the Femoral Head Changed During the Same Period
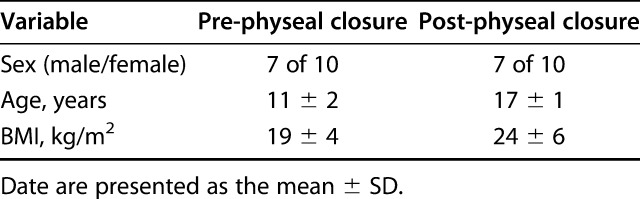
The anterior sector angle decreased from a mean ± SD (range) 72° ± 8° (57 to 87) at the initial MRI to 65° ± 8° (50 to 81) (p = 0.002) at the follow-up MRI (Fig. 5A). The posterior sector angle remained unchanged between the initial (98° ± 5°; 86 to 111) and follow-up MRIs (97° ± 5°; 89 to 109) (p = 0.8) (Fig. 5B). Lastly, with the numbers available, we found no differences in the superior sector angle from initial (121 ± 4°; 114 to 129) to the follow-up (124° ± 5°; 111 to 134) MRI (p = 0.07) (Fig. 5C). The change in the anterior sector angle correlated with the change in version (r = 0.5; p = 0.02).
Fig. 5 A-C.
Box and whisker plots show the (A) anterior, (B) posterior, and (C) superior acetabular sector angle measurements of the initial (blue) and follow-up (green) MR images.
Identify Any Demographic Factors That May Influence Acetabular Development
Female patients had greater mean ± SD (range) anteversion (13° ± 5°; 5 to 22) than did male volunteers (11° ± 2°; 7 to 16; p = 0.04). However, the change that occurred between the two MRIs was not different between male patients (5° ± 2°; 0 to 9) and female patients (5° ± 2°; 2 to 9; p = 0.9). The change in version did not correlate with BMI (ρ = -0.1; p = 0.6), nor with the hip internal rotation in the supine or prone position (ρ = 0.04; p = 0.8).
Discussion
FAI, defined as the abutment of the proximal femur against the acetabulum during physiologic movement, can cause pain [13], and is a precursor of hip osteoarthritis in some patients [8]. Various morphologic abnormalities, including an abnormal femoral head-neck offset and/or version of both the femur and acetabulum, can predispose a hip to FAI and subsequent deformities [8, 15]. Characterizing the normal developmental process of the acetabulum would allow for easier recognition of a morphologic abnormality secondary to “maldevelopment.” With this longitudinal cohort of asymptomatic adolescents, we were able to delineate the changes that occur during acetabular development by imaging the same hips at Stages 1 (open) and 3 (fully closed) development of the triradiate cartilage complex of the physis. The immature acetabulum has overall less version, and retroversion is a common feature rostrally. With maturity, version increased, and the increase was greater over the rostral part than in the remainder of the joint. By measuring the various acetabular sector angles, we were able to show that most of the increase in anteversion was because of a relative reduction in cover by the anterior acetabular wall. This implies that if the normal developmental process were to be disturbed, the resulting (rostral) retroversion would be owing to anterior over-coverage rather than a posterior wall deficiency; this would have implications on whether a corrective osteotomy (indicated for posterior wall insufficiency) or just anterior acetabular rim-trim (for anterior over-coverage) would be the most appropriate surgical treatment option.
This study has a number of limitations. First, this study is limited by selection bias. This cohort was obtained from a fracture clinic in a tertiary hospital and includes a small number of patients overall (although of sufficient to study primary outcome). Second, assessment bias may be present, especially for ROM measurements; the ROM assessments were only performed by a single observer and hence no intra- or interobserver reliability measurements were obtained. However, the assessor was blinded to the outcome of interest in this study. Third, transfer bias may exist as two patients did not present for their follow-up imaging and the MR images were no longer available in four patients of the initial cohort. Fourth, the assessments were performed using MRIs of both hips rather than of the pelvis. Although we attempted to consider pelvic rotation (by considering the position of the ischial tuberosities), accounting for pelvic tilt was not possible because the anterior superior iliac spines were not routinely included in the MRI scan. However, a change in pelvic tilt, which would have increased version, would have been associated with both a reduced anterior sector angle and increased posterior sector angle; that was not seen in this study. Fifth, our inability to find an association between the change in acetabular version and the various patient factors tested may reflect a type β error; the study was sufficiently powered to answer the first two aims of the study but perhaps was insufficiently powered to address the last aim. Lastly, the MRIs did not include data on the rotational profile of the femur. A further study is needed to establish whether an association exists between the reduction in femoral version and increase in acetabular version.
The increase in version seen with skeletal maturity in this study agrees with the findings of other authors. Studies calculating the version changes with both CT data [10, 17, 19] and MRI data [2] showed an increase in acetabular version with skeletal maturity. The above finding is in contrast to the study by Weiner et al. [28], who reported no increase in version with skeletal maturity; however, their study was CT-based and overlooked the cartilaginous portions of the growing skeleton. Additionally, they only measured version using one axial image slice; we hence feel that the approach used in this study is more robust. Furthermore, our finding of a greater increase in version moving caudally in the joint is similar to the observations of two cross-sectional studies using CT data [7, 10] and a similar method of measuring version as used in this study. Further enhancing our current understanding, our longitudinal study design allowed us to compare the relative change in version that occurs in a developing acetabulum. Although version increased at all axial levels with skeletal maturity, the increase was greatest along the rostral part of the joint. As a reflection of this increase, none of the eight hips (24%) that showed rostral retroversion at the initial MRI had evidence of retroversion at follow-up.
By measuring sector angles, we were able to determine the degree of femoral head coverage that the acetabulum provides anteriorly, posteriorly, and superiorly. By measuring the acetabular sector angle, we determined that with skeletal maturity, there was a reduction in the anterior sector angle but no change in the posterior sector angle. Furthermore, the change in the anterior acetabular angle correlated with an increase in acetabular version. Therefore, it appears that version increases because of a reduction of the femoral head coverage anteriorly. This observation is in contrast to a CT-based cross-sectional study by Hingsammer et al. [10], in which the increase in version with skeletal maturity was secondary to an increase in posterior wall coverage. However, the use of CT, rather than MRI-based measurements in the growing skeleton was a limitation of their study because the posterior wall has been shown to be the last part of the acetabulum to ossify and hence appear on CT images. A reduction in coverage of the anterior femoral head by the acetabulum may be secondary to Volkmann-Heuter’s principle of physeal growth [24]. With skeletal maturity, the reduction in femoral version and increase in the alpha angle of the femoral head-neck junction [5] may lead to increased pressure between the femur and anterior wall and result in slowed growth of the anterior acetabular wall. A further study is necessary to support or refute this theory. Acetabular retroversion is a morphologic abnormality predisposing the hip to FAI and can be classified along the spectrum of dysplasia. Therefore, a great variability of deformity exists, with an incidence of up to 15% [4, 14]. However, what extent of acetabular retroversion classifies as pathologic is unknown. Furthermore, debate still exists about whether retroversion is the result of increased anterior coverage, a deficient posterior wall, a rotation abnormality, a low-volume acetabulum, or most likely, a combination of all the above [6, 26]. It is important to determine the underlying morphologic abnormality leading to retroversion because this would guide the surgical management (for example, periacetabular osteotomy or rim-trim). The findings of this study support that if normal developmental changes do not occur during adolescence, the associated rostral retroversion would be related to anterior wall over-coverage rather than a posterior wall deficiency, supporting the observations of Larson et al. [14]. However, the disturbance of the normal developmental process may not be the only way of forming acetabular retroversion, as evident by findings reported in skeletally mature patients [4, 6, 26].
Genetic and environmental factors are important for skeletal development. Although female sex was associated with greater acetabular version, which was consistent with the results of previous reports [16], we found no other patient factors (BMI or ROM of the hip) that were associated with changes in acetabular version. Given that the developmental processes of the proximal femur and acetabulum are considered interlinked [20], a further longitudinal study with greater statistical power to further define this interaction during the developmental process is needed.
The immature acetabulum showed evidence of cranial retroversion in one-fourth of the patients in this cohort. With skeletal maturity during adolescence, acetabular version increases, especially rostrally. This increase in version is associated with, and is likely a result of, a reduced anterior acetabular sector angle, reflecting the degree of femoral head coverage that the anterior wall provides. This indicates that rostral retroversion of the hip seen in the skeletally mature patient is because of anterior over-coverage if the normal developmental process is disturbed. However, further studies on patients with acetabular retroversion (of various degrees) should characterize what proportions of these patients have over-coverage of the anterior acetabular rather than deficiency of the posterior acetabulum. Such information would provide important information on best treatment strategies. The changes in version were not associated with any of the patient factors tested; a further study with greater power is needed to provide further insight into this process.
Acknowledgments
We thank the Canadian Institutes of Health Research for funding the longitudinal study, on which this retrospective chart review is based.
Footnotes
Each author certifies that neither he or she, nor any member of his or her immediate family, has funding or commercial associations (consultancies, stock ownership, equity interest, patent/licensing arrangements, etc.) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research® editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research® neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA approval status, of any drug or device before clinical use.
Each author certifies that his or her institution approved the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
The work was performed at The Ottawa Hospital, Ottawa, ON, Canada.
References
- 1.Acheson RM. The Oxford method of assessing skeletal maturity. Clin Orthop. 1957;10:19-39. [PubMed] [Google Scholar]
- 2.Albers CE, Schwarz A, Hanke MS, Kienle KP, Werlen S, Siebenrock KA. Acetabular version increases after closure of the triradiate cartilage complex. Clin Orthop Relat Res. 2017;475:983-994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Anda S, Svenningsen S, Dale LG, Benum P. The acetabular sector angle of the adult hip determined by computed tomography. Acta Radiol Diagn (Stockh). 1986;27:443-447. [DOI] [PubMed] [Google Scholar]
- 4.Anderson LA, Anderson MB, Erickson JA, Chrastil J, Peters CL. Acetabular wall indices help to distinguish acetabular coverage in asymptomatic adults with varying morphologies. Clin Orthop Relat Res. 2017;475:1027-1033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Carsen S, Moroz PJ, Rakhra K, Ward LM, Dunlap H, Hay JA, Willis RB, Beaule PE. The Otto Aufranc Award. On the etiology of the cam deformity: a cross-sectional pediatric MRI study. Clin Orthop Relat Res. 2014;472:430-436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dandachli W, Islam SU, Liu M, Richards R, Hall-Craggs M, Witt J. Three-dimensional CT analysis to determine acetabular retroversion and the implications for the management of femoro-acetabular impingement. J Bone Joint Surg Br. 2009;91:1031-1036. [DOI] [PubMed] [Google Scholar]
- 7.Fujii M, Nakashima Y, Yamamoto T, Mawatari T, Motomura G, Matsushita A, Matsuda S, Jingushi S, Iwamoto Y. Acetabular retroversion in developmental dysplasia of the hip. J Bone Joint Surg Am. 2010;92:895-903. [DOI] [PubMed] [Google Scholar]
- 8.Ganz R, Leunig M, Leunig-Ganz K, Harris WH. The etiology of osteoarthritis of the hip: an integrated mechanical concept. Clin Orthop Relat Res. 2008;466:264-272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ganz R, Parvizi J, Beck M, Leunig M, Notzli H, Siebenrock KA. Femoroacetabular impingement: a cause for osteoarthritis of the hip. Clin Orthop Relat Res. 2003:112-120. [DOI] [PubMed] [Google Scholar]
- 10.Hingsammer AM, Bixby S, Zurakowski D, Yen YM, Kim YJ. How do acetabular version and femoral head coverage change with skeletal maturity? Clin Orthop Relat Res. 2015;473:1224-1233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kapron AL, Peters CL, Aoki SK, Beckmann JT, Erickson JA, Anderson MB, Pelt CE. The prevalence of radiographic findings of structural hip deformities in female collegiate athletes. Am J Sports Med. 2015;43:1324-1330. [DOI] [PubMed] [Google Scholar]
- 12.Kemper HC. Skeletal development during childhood and adolescence and the effects of physical activity. Pediatr Exerc Sci. 2000;12:198-216. [Google Scholar]
- 13.Khanna V, Caragianis A, Diprimio G, Rakhra K, Beaule PE. Incidence of hip pain in a prospective cohort of asymptomatic volunteers: is the cam deformity a risk factor for hip pain? Am J Sports Med. 2014;42:793-797. [DOI] [PubMed] [Google Scholar]
- 14.Larson CM, Moreau-Gaudry A, Kelly BT, Byrd JW, Tonetti J, Lavallee S, Chabanas L, Barrier G, Bedi A. Are normal hips being labeled as pathologic? A CT-based method for defining normal acetabular coverage. Clin Orthop Relat Res. 2015;473:1247-1254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Leunig M, Beaule PE, Ganz R. The concept of femoroacetabular impingement: current status and future perspectives. Clin Orthop Relat Res. 2009;467:616-622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Merle C, Grammatopoulos G, Waldstein W, Pegg E, Pandit H, Aldinger PR, Gill HS, Murray DW. Comparison of native anatomy with recommended safe component orientation in total hip arthroplasty for primary osteoarthritis. J Bone Joint Surg Am. 2013;95:e172. [DOI] [PubMed] [Google Scholar]
- 17.Monazzam S, Bomar JD, Dwek JR, Hosalkar HS, Pennock AT. Development and prevalence of femoroacetabular impingement-associated morphology in a paediatric and adolescent population: a CT study of 225 patients. Bone Joint J. 2013;95-B:598-604. [DOI] [PubMed] [Google Scholar]
- 18.Murtha PE, Hafez MA, Jaramaz B, DiGioia AM., 3rd Variations in acetabular anatomy with reference to total hip replacement. J Bone Joint Surg Br. 2008;90:308-313. [DOI] [PubMed] [Google Scholar]
- 19.Peterson JB, Doan J, Bomar JD, Wenger DR, Pennock AT, Upasani VV. Sex differences in cartilage topography and orientation of the developing acetabulum: implications for hip preservation surgery. Clin Orthop Relat Res. 2015;473:2489-2494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ponseti IV. Growth and development of the acetabulum in the normal child. Anatomical, histological, and roentgenographic studies. J Bone Joint Surg Am. 1978;60:575-585. [PubMed] [Google Scholar]
- 21.Siebenrock KA, Behning A, Mamisch TC, Schwab JM. Growth plate alteration precedes cam-type deformity in elite basketball players. Clin Orthop Relat Res. 2013;471:1084-1091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Siebenrock KA, Ferner F, Noble PC, Santore RF, Werlen S, Mamisch TC. The cam-type deformity of the proximal femur arises in childhood in response to vigorous sporting activity. Clin Orthop Relat Res. 2011;469:3229-3240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Stasikelis PJ, Sullivan CM, Phillips WA, Polard JA. Slipped capital femoral epiphysis. Prediction of contralateral involvement. J Bone Joint Surg Am. 1996;78:1149-1155. [DOI] [PubMed] [Google Scholar]
- 24.Stokes IA. Mechanical effects on skeletal growth. J Musculoskelet Neuronal Interact. 2002;2:277-280. [PubMed] [Google Scholar]
- 25.Strayer LM., Jr Embryology of he human hip joint. Clin Orthop Relat Res. 1971;74:221-240. [PubMed] [Google Scholar]
- 26.Tannast M, Pfannebecker P, Schwab JM, Albers CE, Siebenrock KA, Buchler L. Pelvic morphology differs in rotation and obliquity between developmental dysplasia of the hip and retroversion. Clin Orthop Relat Res. 2012;470:3297-3305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Watts HG. Fractures of the pelvis in children. Orthop Clin North Am. 1976;7:615-624. [PubMed] [Google Scholar]
- 28.Weiner LS, Kelley MA, Ulin RI, Wallach D. Development of the acetabulum and hip: computed tomography analysis of the axial plane. J Pediatr Orthop. 1993;13:421-425. [DOI] [PubMed] [Google Scholar]