Description
A 57-year-old retired midwife developed necrotising pneumonia after a recent holiday in India. Her previous medical history was significant only for a pulmonary embolism while pregnant many years ago. Sputum samples had grown Panton-Valentine leukocidin-positive methicillin-resistant Staphylococcus aureus. During around day 38 of her hospital admission, she developed haemoptysis and had an arterial phase CT chest (figure 1) which showed a 13 mm enhancing nodule in the right upper lobe representing a pulmonary artery pseudoaneurysm (PAPA) arising from the posterior segmental branch of the right pulmonary artery. As the patient remained haemodynamically stable and neither the frequency nor the volume of haemoptysis was increasing, a multidisciplinary team of interventional radiologists, critical care and respiratory physicians decided on observation and a repeat CT scan in 3 months showed complete spontaneous resolution of the PAPA (figure 2). The patient fully recovered from the necrotising pneumonia and her haemoptysis completely resolved.
Figure 1.
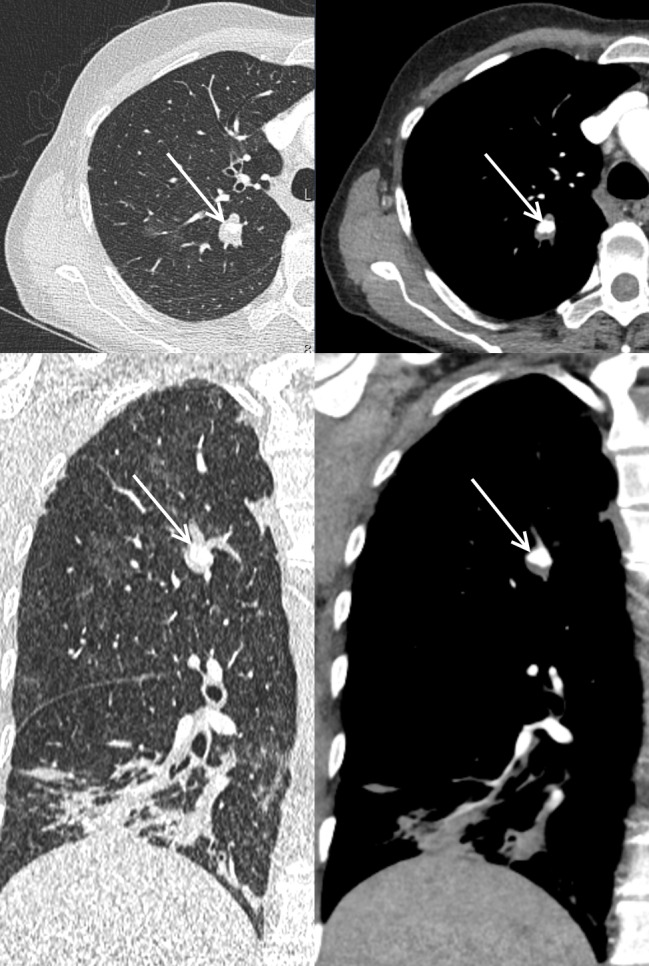
Axial (top) and coronal (bottom) reformats of arterial phase CT chest with soft-tissue (right) and lung windows (left) demonstrating an enhancing nodule (white arrow) in the right upper lobe arising from the posterior segmental branch of the right pulmonary artery. No contrast blush to suggest active bleeding.
Figure 2.
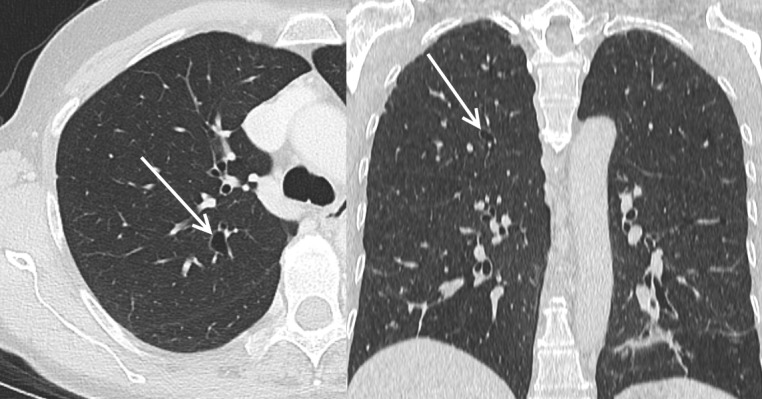
Axial (left) and coronal (right) reformats of a portal venous phase CT chest (lung window) showing an ectatic bronchus (white arrow) in the right upper lobe but no enhancing nodule which was seen on the prior CT.
There are a number of case reports on PAPAs occurring secondary to necrotising pneumonia1–4 but none of these cases opted for observation; the patient either died due to massive haemoptysis3 or the PAPA was treated.1 2 4 When comparing our case, the only two potential factors which differed were severe unremitting haemoptysis3 4 or multi-drug resistant pneumonia,1 neither of which our patient had. Therefore, it may be that these are two potential factors that could play a role in the spontaneous resolution of a PAPA. There is one case series of post-traumatic PAPAs spontaneously resolving5 but to the best of our knowledge, there is no published case report on a self-resolving PAPA due to an underlying infectious or inflammatory cause. To the best of our knowledge, there are currently no established evidence-based guidelines on whether or when PAPAs require intervention or surveillance. This case report highlights that spontaneous resolution could be a part of the natural history of inflammatory as well as post-traumatic PAPAs,5 however more research, with larger patient cohorts, is needed to better understand which factors facilitate spontaneous resolution.
Learning points.
Necrotising pneumonia is a risk factor for pulmonary artery pseudoaneurysm (PAPA) formation.
PAPAs have the potential to spontaneously resolve in certain circumstances.
Footnotes
Contributors: SL wrote the manuscript. AR and CVZ contributed to editing the manuscript. SM contributed to editing the manuscript and came up with an idea for manuscript.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent for publication: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1. Ishimoto S, Sakurai H, Higure R, et al. Pulmonary artery pseudoaneurysm secondary to lung Inf lammation. Ann Thorac Cardiovasc Surg 2018;24:154–6. 10.5761/atcs.cr.17-00172 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Kalina M, Giberson F. Hemoptysis secondary to pulmonary artery pseudoaneurysm after necrotizing pneumonia. Ann Thorac Surg 2007;84:1386–7. 10.1016/j.athoracsur.2007.05.024 [DOI] [PubMed] [Google Scholar]
- 3. Koneru H, Biswas Roy S, Islam M, et al. Pulmonary artery pseudoaneurysm: a rare cause of fatal massive hemoptysis. Case Rep Pulmonol 2018;2018:1–4. 10.1155/2018/8251967 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Smith CB, Patel BN, Smith JP. Pulmonary artery pseudoaneurysm arising secondary to cavitary pneumonia. Radiol Case Rep 2012;7 10.2484/rcr.v7i3.654 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Goel S, Kumar A, Gamanagatti S, et al. Spontaneous resolution of post-traumatic pulmonary artery pseudoaneurysm: report of two cases. Lung India 2013;30:203–5. 10.4103/0970-2113.116262 [DOI] [PMC free article] [PubMed] [Google Scholar]


