Abstract
Purpose of Review
Update the state of evidence on the effectiveness of retail food environment interventions in influencing diet and explore the underlying role of public policy, through a systematic review of population-level interventions to promote health in the retail food environment, including community and consumer environments. Diet-related outcomes included purchasing, dietary intakes, diet quality, and health including weight. We coded studies for enabling public policy levers underpinning the intervention, using two widely used conceptual frameworks.
Recent Findings
Of 86 articles (1974–2018), the majority (58 articles, 67%) showed at least one positive effect on diet. Thirteen articles (15%) discussed natural experiments, 27 articles (31%) used a design involving comparison groups including 23 articles (27%) specifically describing randomized controlled trials, and 46 (53%) were quasi-experimental (cross-sectional) evaluations. Across the “4Ps” of marketing (product, promotion, placement, and price), promotion comprised the greatest proportion of intervention strategies, especially in earlier literature (pre-2008). Few studies combined geographic access interventions with 4P strategies, and few used robust dietary intake assessments. Behavior change communication remains an intervention mainstay, but recent work has also incorporated environmental and social planning, and fiscal strategies. More recent interventions were multi-component.
Summary
The retail food environment intervention literature continues to grow and has become more robust overall, with clearer evidence of the effect of interventions on diet-related outcomes, including consumer purchasing, dietary intakes, and health. There is still much scope for development in the field. Attention to enabling public policy could help to strengthen intervention implementation and evaluation in the retail food environment.
Keywords: Community food environment, Consumer food environment, Retail food environment, Intervention, Review, Diet, Consumer purchasing, Noncommunicable diseases, Health behavior, Public policy, Policy context
Introduction
Dietary factors are the leading modifiable risk for global morbidity and mortality [1, 2] and a problem of serious policy concern [3]. Growing epidemiological research has investigated how the food choice environment in communities contributes to diet [4, 5]. Retail food stores are the main community food source for many populations, central to food distribution in both advanced and developing economies [6]. Spatial analysis of the retail food environment shows mixed associations between geographic access to stores, diet, and health [5], and an important explanation is the multidimensional character of retail exposures [7], including the complex ways in which humans move and behave in their food environments. Theoretical frameworks distinguish the community food environment (distribution of stores in an area, and how shoppers encounter them through daily mobility) and the consumer food environment (attributes experienced by shoppers in-store, influences usually categorized by the 4Ps of marketing: product, promotion, placement, and price) [8]. Variation among retailers in consumer environment features, such as product availability and price [9, 10], can modify associations between the community food environment and diet [4, 5].
Background: a Brief Review of Retail Intervention Reviews
Within this context, growing attention has been paid to intervention strategies to reduce population dietary risk related to retail food environment exposures [11, 12]. Table 1 describes existing systematic reviews of interventions in community and consumer retail food environments to shape diet and health.
Table 1.
Summary of recent systematic reviews on the effectiveness of retail food environment interventions in community and consumer environments, 2012-2018
| 1st author | Year | N | Settings and interventions included | Main outcome | Dates included |
|---|---|---|---|---|---|
| Reviews specifically focused on retail food environment interventions (direct evidence) | |||||
| Adam [13] | 2016 | 42 | Physical retail food store interventions related to obesity and to increase the consumption of healthy foods, including price, information, and access/availability | Sale/purchase of healthy foods | 2003 to 2015 |
| Cameron [14•] | 2016 | 49 | Supermarket-based interventions, including product, promotion, and placement | Food purchasing, dietary intake, and weight | Database inception to December 2015 |
| Escaron [15] | 2013 | 58 | Supermarket and grocery store-based interventions, including point-of-purchase information, price, availability, promotion, and advertising | Consumer awareness, use, knowledge and beliefs, preferences, sales, and process measures | Late 1940s to July 2012 |
| Gittelsohn [16] | 2012 | 16* | Small store (< 10 employees and < 1,000 sq ft) interventions to influence food access and consumption | Process measures, store impact, consumer psychosocial and behavioral impact, consumer health | 1990 to September 2010 |
| Glanz [17] | 2012 | 125 | Food marketing confronted by consumers in grocery stores, including product, placement, price, and promotion; lab experiments, observational, and field interventions included | Food purchases and/or consumption | 1995 to 2010 |
| Hartmann-Boyce [18] | 2018 | 55 | Settings and interventions included: Supermarket and convenience store interventions including simulations, including price or rewards, placement, promotion, information, and swaps, randomized controlled trials only | Consumer purchasing | No date limit (search carried out June 2017) |
| Hasanthi-Abeykoon [19] | 2017 | 11 | Newly opened grocery stores, with or without added in-store intervention components | Physical or psychological health, psychological factors, food security, dietary intake, food purchasing, other food behavior | 1995 to November 2015 |
| Liberato [20] | 2014 | 32 | Nutrition interventions at the point-of-sale, including availability, affordability, or nutrition education/promotion | Food purchasing or dietary intake | No date limit (article published September 2014) |
| Pinard [21] | 2016 | 19 | Retail food environment research in small food stores, including observational studies as well as interventions, and focus on rural | No limits | May 2005 to May 2015 |
| van’t Riet [22] | 2012 | 16 | Product health information presented at the point-of-purchase | Food sales or purchasing | 1980 to 2010 |
| Woodruff [23] | 2017 | 23 | Initiatives to increase spatial access to food retailers | Fruit and vegetable consumption among adults | Database inception to November 2015 |
| Reviews on population health policies with influences in retail store settings (indirect evidence) | |||||
| Afshin [24] | 2015 | N/R | Broad range of policy interventions (mass media, labels, school procurement, worksite wellness, community built environment, fiscal, marketing) directed towards healthier dietary behavior and diet-related risk factors for cardiovascular disease | Dietary intake, adiposity, blood pressure, and blood lipids | 1980 to N/R (article published September 2015) |
| Allender [25•] | 2012 | N/R | Quantitative primary evidence of the relationship between nine policy areas intended to improve environments for healthy eating and physical activity at the local government level; and nutrition, physical activity, or weight | Summary of evidence was not reported; was used as the basis for qualitative research with informants | N/R; some sub-searches were limited to within last 10 years |
| Thow [26] | 2014 | 43 | Fiscal policies to encourage healthy diets (sugar-sweetened beverage, fat, and calorie-based taxes; nutrient profiling taxes; and healthy food subsidies). Only 4/43 papers assessed an actual tax or subsidy vs. model/hypothetical | Consumption including purchasing and dietary intake | January 2009–March 2012 |
N = number of included papers
N/R not reported
*This review used grey literature as well as peer-reviewed academic literature, and reported n as number of trials
These reviews have demonstrated the substantial heterogeneity among interventions [20], but also show collectively that methodologies for evaluating interventions have strengthened over time, with corresponding clearer effects on food selection behavior, especially purchasing. The 2016 review of supermarket interventions by Cameron et al. [14•] in this journal found that 70% of interventions reported a positive (healthy) effect on food purchasing. The magnitude of effect differed widely, however, and some (generally weaker) studies demonstrated no effect.
Intervention strategies for smaller (i.e., convenience) versus larger (i.e., supermarkets) stores have tended to be assessed separately [14•], although important commonalities emerge when the literature is grouped. Escaron et al. [15] and Gittelsohn et al. [16] both concluded that the evidence for altering the retail choice architecture through multi-component interventions was stronger than for single component interventions, such as changing prices alone, or education/labeling alone.
Within systematic reviews to date, an understudied feature is the public policy context in which interventions are implemented [16]. Realizing the full implementation and impact of population health interventions in community settings requires enabling public policies led by government, a core principle of healthy public policy [27]. Three reviews have assessed public policy related to retail food environment interventions, summarized in Table 1. Allender et al. [25•] started with a review of health evidence but did not report it in the article, focusing instead on acceptability and feasibility of interventions as well as other policy and political considerations, through a local jurisdictional case. Allender et al. [25•] noted that their paper was addressing a key gap in population health literature that articulates intermediary, but necessary steps for policy change, where changes are appraised within a legal architecture and policy process. Afshin et al. [24] and Thow et al. [26] took a more macro approach, focusing specifically on systems-level policy interventions that might have an effect in the community built environment and retail stores, such as food subsidies/taxes.
No review of retail food environment interventions to date has assessed directly how the evidence of effectiveness of interventions is linked to their policy salience. Yet we would argue that this is essential to advance our understanding of how policy can enable successful interventions [11]. For instance, it is widely accepted that retail food environments in publicly funded institutions (e.g., schools, hospitals, recreation facilities) should be governed by supportive government policies that set the conditions for successful retail implementation and consumer uptake of healthier food options. Nutrition researchers are also increasingly examining how upstream regulatory approaches targeting food manufacturers can be used to accomplish public health goals. Only a highly limited range of healthy public policy proposals have been proposed to date for the domain of the private sector retail store, such as zoning. So as a starting point for greater research attention to the diverse policy instruments that might be used, in the current review, we were interested in expanding our understanding of the policy assumptions underlying the body of research on retail interventions designed to shift population diets. Like Allender, our aim is to connect interventions in a more direct way to government policy structures. This is especially important for the retail food environment, where a breadth of policy levers, government authorities, diverse private sector actors, and the governance and relational features among them make up the linking steps to a healthier population diet.
The objective of this paper was thus two-pronged: (a) update the state of the evidence on effectiveness of community and consumer food environment interventions in influencing diet (3 years has passed since the end date of literature captured in Cameron’s review [14•], which also focused solely on supermarkets, and did not include fiscal interventions) and (b) begin to explore the underlying role of public policy in these interventions.
Methods
Search Strategy
Working with an academic librarian at our institution, a systematic search of published peer-reviewed research literature was conducted in PubMed, Scopus, and CINAHL, published from the beginning of each database through to November 2018. The same forwards search was used for each database (* = truncation Boolean operator):
Retail food outlet: food environment OR food retail OR grocer* OR food store OR convenience store OR food market OR supermarket* OR gas station
Intervention foci: price OR pricing OR promotion OR intervention* OR program* OR initiative* OR evaluat* OR marketing
Outcomes:nutrition OR diet OR health* OR chronic disease OR food choice OR food purchasing OR obes* OR overweight OR body weight
Reference lists from seven of the existing systematic reviews [14•, 15, 16, 19–21, 28] were then hand-searched to identify any articles that may have been missed (backwards search).
Inclusion Criteria
We included original peer-reviewed articles in English, with full-text available. Articles were eligible if the intervention aimed to promote health in the retail environment at the population-level. Interventions had to be implemented within real-world retail outlets, defined as fixed location commercial establishments with the main purpose of the business being the sale of a product line(s) of food and non-alcoholic beverages, including grocery stores, supermarkets, convenience stores, and gas stations. A field experiment involving nutrition labels affixed to supermarket shelves was eligible [29]; experiments conducted in purpose-built mock store laboratories were not. The retail literature does not use the terms “grocery stores” and “supermarkets” interchangeably, so we accepted each term as presented by the author(s). Interventions could be evaluated with or without a comparison group and could use a quantitative, qualitative, or mixed methods approach. Interventions could include changing the availability or mix of retailers in a geographic area (community food environment) or the “4Ps” in-store, including product, pricing, placement, or promotion of food and non-alcoholic beverages (consumer food environment). Interventions could be interactive (e.g., dietitian consultations) or non-interactive (e.g., shelf labels).
Price interventions were included in the review as long as the general population of shoppers entering the store was eligible for having the intervention applied. For example, a study restricting participation to shoppers meeting a body mass index (BMI) criterion [30] was excluded. Other pricing interventions relied on cohort enrolment prior to allocation, involving a store loyalty card system to receive discounts [31, 32]; we considered these ineligible, as they targeted members rather than the general population. All dietary outcomes were eligible, including subjective or objective measures, and encompassing purchasing, dietary intake, diet quality, or diet-related health including weight. We did not place any restrictions by administrative jurisdiction or geography. Explicit reference to enabling public policy was not a factor for inclusion or exclusion, but explicit references were coded for in the policy analysis of included articles.
Exclusion Criteria
Interventions were excluded if they were implemented in organizational or foodservices environments (e.g., restaurants, fast-food outlets, vending machines, schools, workplaces). Although the distinction between store and foodservices business models is increasingly blurred (e.g., grab-and-go café outlets selling own product lines; supermarkets that offer ready-to-eat items including dine-in), it is still reasonable to exclude foodservices from this study. Foodservices outlets’ main objective is serving of food for immediate consumption, versus sale of food per se. This is reflected in government licensing arrangements for foodservices outlets which are typically a different category from stores and may entail different enforcement requirements. Food product reformulation without a clear retail component was also excluded [33], as were price interventions external to the retail environment such as mass media-distributed store vouchers. We excluded mobile and online shopping, farmers markets, and primarily non-food retailers such as pharmacies. Formative evaluations, protocols, preliminary planning documents, opinion pieces, and systematic reviews were excluded. As noted above, experiments conducted “in vitro” in lab or web purchasing simulations [34] were also excluded.
Study Selection
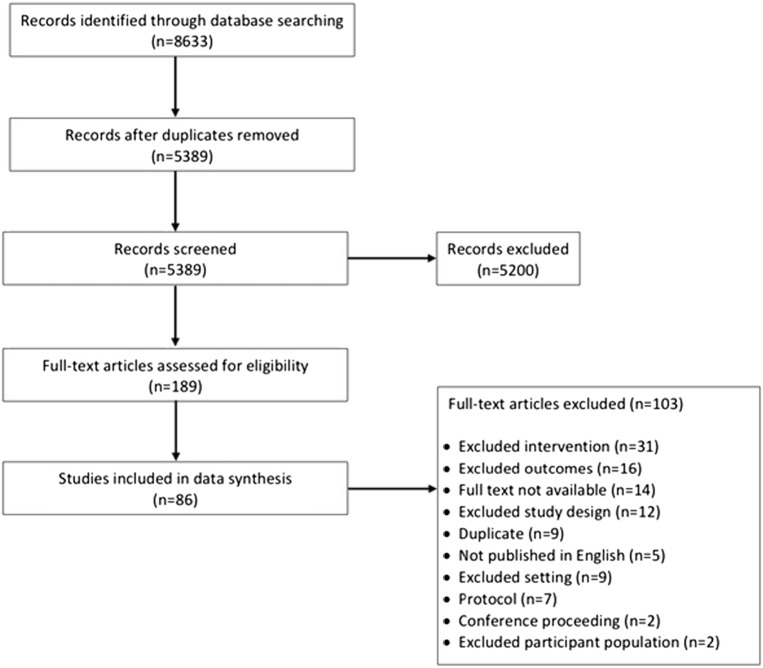
Studies extracted from the databases were uploaded to the Covidence web application, which removed the vast majority of duplicates. Other duplicates were hand-searched and manually removed. Using Covidence, six reviewers independently screened 5,389 articles by title and abstract, with each decision to include or not requiring agreement between at least two reviewers. Studies then underwent full-text screen, with decisions again requiring two reviewers. Reviewers met by phone to discuss conflicts, and if necessary, a third reviewer was consulted to resolve the conflict. For the backwards search, each team member reviewed the reference list of one of the reviews and assessed papers for eligibility; titles of the references were initially screened, then full-text for eligible references were compiled and reviewed for inclusion. Where an article included from the backwards search had been previously excluded through the forwards search, two reviewers resolved the discrepancy (Fig. 1).
Fig. 1.
PRISMA flow diagram, review of retail food environment interventions in community and consumer environments, 1974–2018
Data Extraction
Three coders co-designed the extraction tool and independently extracted study data, one coder per article. To attend to rigour in data extraction and coding, the same three researchers who completed data extraction also completed policy coding. Although each article had a single coder, we integrated an iterative process of peer debriefing to arrive at findings. Coders deliberated throughout extraction and writing: (a) once to refine and finalize the extraction tool based on extracting at least one article each; (b) twice to further calibrate use of the tool; and (c) iteratively through the remainder of extraction, interpretation, and writing. Conflicts were resolved through consensus discussion.
In addition to basic extraction of study features, each article was coded deductively using two public policy frameworks. The Behavior Change Wheel [35, 36] was used to code for the behavioral mechanisms underpinning each intervention and associated types of enabling policies. The Behavior Change Wheel is a widely adopted conceptual framework for health intervention research that notably synthesizes 19 other theory-informed frameworks and goes beyond an exclusive focus on social cognitive or social ecological theory [35]. The Behavior Change Wheel has seven policy types (communications/marketing, guidelines, fiscal measures, regulation, legislation, environmental/social planning, and service provision) that map from “functions,” or how the intervention changes behavior. For example, fiscal policies (e.g., price subsidies on healthier foods) map five functions: incentivization, coercion, training, environmental restructuring, and enablement. The World Cancer Research Fund NOURISHING framework was then used to code for 10 types of public policies within three domains—food systems, food environments, and behavior change communication [12]. The NOURISHING framework is a widely used typology for governments to assemble a coherent suite of policies to support healthier diets [12]. Interventions could map to more than one policy type. We also coded for level of jurisdiction of policy levers, in terms of order of government likely responsible: local/municipal, provincial/regional/state/territorial, and national/federal, acknowledging interjurisdictional differences in authority. We followed a broadly Anglo-American federal political tradition where public policy levers such as urban planning would be local and packaged food labeling (related to the criminal law power) would be national. Corporate (organizational/store) policy was not analyzed in this review. An initial exploration of quality of the included articles was conducted using parameters of the Effective Public Health Practice Project quality assessment tool [37]; studies were ultimately not evaluated for quality, and not included or excluded based on quality, due to wide variation in methods limiting meaningful quality comparisons.
Results
Features of the Included Articles
We included n = 86 articles in the final review, covering 80 interventions. Most (69%) studies were from the USA. The remainder were from (descending order of proportion) Netherlands (6%) [38–42], UK (6%) [43, 44, 45••, 46–47], Australia (5%) [48–51], Canada (5%) [52–55], Denmark (3%) [56–58], Finland (2%) [59, 60], Sweden (1%), Belgium (1%) [61], Japan (1%) [62], and Norway (1%) [63].
The vast majority of articles (88%) reported on interventions in supermarkets (59 articles), grocery stores (14 articles), or a combination of these (3 articles). The remainder were in convenience stores (8 articles), convenience with supermarkets (1 article), and convenience with grocery (1 article). Thirteen articles (15%) discussed natural experiments. Twenty-seven studies (31%) used a design involving comparison groups (indicated as “RCT+” in Table 2): for synthesis purposes, we included in this category two articles using quasi-experimental designs with matched groups of stores allocated to intervention or comparison, one trial with comparison groups that did not mention randomization, and randomized controlled trials (24 articles, 27%). Forty-five (52%) articles were on quasi-experimental (cross-sectional) evaluations without comparison groups, including post-test only or repeat cross-sections. Only two of the convenience store studies used comparison groups, and they were among the more recent.
Table 2.
Summary of strategies, effect on diet, and policy levers of retail food environment interventions in community and consumer environments, 1974–2018
| 1st author | Year | Effect | Geog | Price | Prod | Prom | Place | Study design | Intervention length | Outcome(s) | BCW policy levers | Jurisdiction |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Curhan [64] | 1974 | Mixed^^ | R | R | R | QE | 7 months | $ | Guidelines | National | ||
| Jeffery [65] | 1982 | Null | R | RCT+ | 6 months | $ | Guidelines, communication/marketing | Multilevel | ||||
| Levy [66] | 1985 | Positive | R | RCT+ | 2 years | $ | Guidelines | State | ||||
| Ernst [67] | 1986 | Null | R | QE | 1 year | $ | Guidelines, communication/marketing | National | ||||
| Russo [68] | 1986 | Mixed^^ | R | QE | 33 weeks | $ | Communication/marketing | National | ||||
| Achabal [69] | 1987 | Null | R | QE | 12 weeks | $ | Guidelines | National | ||||
| Dougherty [70] | 1990 | Null | R | QE | 6 weeks | $ | Guidelines, Communication/marketing | National | ||||
| Scott [50] | 1991 | Positive | R | R | QE | 15 weeks | D | Communication/marketing, environmental/social planning | Local | |||
|
Winett [71] *Winett 1991b, Winett 1997 |
1991a | Positive | R | RCT+ | 10–36 min | $ | Communication/marketing | National | ||||
|
Winett [72] *Winett 1991a, Winett 1997 |
1991b | Positive | R | RCT+ | 8–32 min | $ | Communication/marketing | National | ||||
| Patterson [73] | 1992 | Null | R | RCT+ | 2 years | $ | Guidelines, communication/marketing | State | ||||
| Crawford [52] | 1993 | Positive | R | QE | 1.5 h | $ | Communication/marketing | State | ||||
| Rodgers [74] | 1994 | Mixed^ | R | QE | 2 years | $, D | Communication/marketing | National | ||||
| Paine-Andrews [75] | 1996 | Positive | R | R | QE | 9.5 h | $ | Guidelines, communication/marketing | Local | |||
| Anderson [76] | 1997 | Positive | R | R | RCT+ | 10 weeks | $ | Fiscal measures | Multilevel | |||
| Kristal [77] | 1997 | Null | R | R | RCT+ | 8 months | Q | Fiscal measures, communication/marketing | Local | |||
| Teisl [78] | 1997 | Positive | R | QE | 3 years | $ | Guidelines, communication/marketing | National | ||||
|
Winett [79] *Winett 1991a, Winett 1991b |
1997 | Positive | R | R | RCT+ | 30–50 min | $ | Communication/marketing | National | |||
| Narhinen [60] *Narhinen 2000 | 1999 | Null | R | QE | 12 weeks | $ | Guidelines, communication/marketing | Local | ||||
| Narhinen [59] *Narhinen 1999 | 2000 | Positive | R | R | QE | 12 weeks | $ | Guidelines, communication/marketing | Local | |||
| Connell [80] | 2001 | Positive | R | RCT+ | 4 weeks | D | Communication/marketing | National | ||||
| Weinehall [81] | 2001 | Positive | R | N | 10 years | $ | Guidelines | National | ||||
| Wrigley [46] | 2003 | Positive | R | N | 1 year | D | Environmental/social planning | Local | ||||
| Steenhuis [40] | 2004 | Null | R | RCT+ | 6 months | D | Guidelines, communication/marketing | Multilevel | ||||
| Wang [82] | 2007 | Null | R | N | 6 months | D | Environmental/social planning | Multilevel | ||||
| Cummins [44] *Cummins 2008b | 2008a | Null | R | N | 1 year | $ | Environmental/social planning | Local | ||||
| Cummins [45•] *Cummins 2008a | 2008b | Null | R | QE | 1 year | D, H | Environmental/social planning | Local | ||||
| Song [83] | 2009 | Positive | R | R | QE | 10 months | $ | Guidelines, fiscal measures, communication/marketing | Local | |||
| Freedman [84] | 2010 | Null | R | QE | 5 weeks | $ | Guidelines, communication/marketing | National | ||||
| Berning [29] | 2010 | Negative | R | RCT+ | 4 weeks | $ | Legislation | National | ||||
| Gittelsohn [85] | 2010a | Mixed^^ | W | R | QE | 9–11 months | D | Service provision | Local | |||
| Gittelsohn [86] | 2010b | Positive | R | W | R | QE | 10 weeks | D | Service provision, fiscal measures, communication/marketing | Local | ||
| Jetter [87] | 2010 | Positive | R,W | QE | 7 months | $ | Service provision | Local | ||||
| Sutherland [88] | 2010 | Positive | R | N | 2 year | $ | Guidelines, communication/marketing | National | ||||
| Ogawa [62] | 2011 | Positive | R | RCT+ | 60 days | $ | Guidelines, communication/marketing | Multilevel | ||||
| Sigurdsson [63] | 2011 | Positive | R | R | 2–4 days | $ | Legislation | National | ||||
| Dannefer [89] | 2012 | Null | R | R | R | QE | 5 months | $ | Guidelines, service provision, regulation, communication/marketing, environmental/social planning | Local | ||
| Holmes [90] | 2012 | Mixed^ | R | QE | 12 weeks | $ | Guidelines | Multilevel | ||||
| Milliron [91] | 2012 | Null | R | RCT+ | 4 months | $, Q, H | Guidelines, communication/marketing | National | ||||
| Ayala [92] | 2013 | Null | R | R | QE | 2 months | D, H | Guidelines, service provision, communication/marketing | Local | |||
| Geliebter [93] | 2013 | Positive | R | RCT+ | 8 weeks | $, D, H | Fiscal measures | State | ||||
| Gittelsohn [94] | 2013 | Mixed^^ | R | R | RCT+ | 14 months | Q, H | Service provision, communication/marketing | State | |||
| Sadler [95] | 2013 | Null | R | N | 1 year | $ | Environmental/social planning | Multilevel | ||||
| Waterlander [41] | 2013 | Mixed^^ | R | R | RCT+ | 6 months | $ | Fiscal measures, communication/marketing | National | |||
| Bangia [96] *Bangia 2017 | 2014 | Negative | R | QE | 4 months (???) | $ | Communication/marketing | Local | ||||
| Cawley [97] | 2014 | Mixed^^ | R | QE | 2 years | $ | Communication/marketing | National | ||||
| Cummins [98] | 2014 | Null | R | QE | 6-9 months | D, H | Guidelines, service provision, communication/marketing, environmental/social planning | Multilevel | ||||
| Foster [99] | 2014 | Positive | R | R | R | RCT+ | 6 months | $ | Guidelines, communication/marketing | Multilevel | ||
| Gill [47] | 2014 | Positive | R | N | 1 year | D | Environmental/social planning | Local | ||||
| Paek [100] | 2014 | Positive | R | R | QE | 6 months | D | Guidelines, service provision, communication/marketing, environmental/social planning | Local | |||
| Papies [39] | 2014 | Positive | R | QE | Mean = 15 min | $ | Guidelines, communication/marketing | Local | ||||
| Dubowitz [101] | 2015 | Mixed^^^ | R | RCT+ | 1 year | $, D, Q, H | Environmental/social planning | Multilevel | ||||
|
Elbel [102] *Elbel 2017 |
2015 | Null | R | RCT+ | 1 year | $, D, H | Environmental/social planning | Local | ||||
| Fuller [54] | 2015 | Positive | R | QE | 1 year | $ | Environmental/social planning | Local | ||||
| Nikolova [103] | 2015 | Positive | R | N | 6 months | $ | Guidelines | State | ||||
| Payne [104] | 2015 | Positive | R | RCT+ | 28 days | $ | Communication/marketing | State | ||||
| Salmon [42] | 2015 | Positive | R | QE | 4 days | $ | Communication/marketing | Local | ||||
| Taillie [105] | 2015 | Null | W | R | N | 2 years | $ | Guidelines, regulation | National | |||
| Adam [57] | 2016 | Null | R | QE | 5 weeks | $ | Guidelines, fiscal measures, environmental/social planning | Multilevel | ||||
| Ortega [106] | 2016 | Null | R | R | R | RCT+ | 2 years | $, E | Guidelines, communication/marketing | Local | ||
| Payne [107] | 2016 | Positive | R | RCT+ | 2 weeks | $ | Communication/marketing | State | ||||
| Schultz [108] | 2016 | Positive | R | QE | 4 months | D | Communication/marketing, environmental/social planning | Local | ||||
| Surkan [109] | 2016 | Positive | R | R | R | QE | 3 months | $ | Guidelines, fiscal measures, communication/marketing | Local | ||
| de Wijk [38] | 2016 | Null | R | QE | 8 weeks | $ | Environmental/social planning | Local | ||||
| Winkler [56] | 2016 | Mixed^^ | R | R | N | 4 weeks | $ | Communication/marketing, environmental/social planning | Local | |||
| Adjoian [110] | 2017 | Mixed^ | R | R | R | QE | 2 weeks | $ | Guidelines | National | ||
| Albert [111] | 2017 | Null | R | R | R | R | QE | 3.5 years | $, D | Legislation, regulation, environmental/social planning | Multilevel | |
| Bangia [112] *Bangia 2014 | 2017 | Positive | R | QE | 22 min | $ | Communication/marketing | Local | ||||
| Brimblecombe [49] | 2017 | Positive | R | R | RCT+ | 6 months | $ | Fiscal measures | National | |||
| Budd [113•] | 2017 | Mixed^^ | R,W | R | R,W | RCT+ | 6 months | $ | Guidelines, regulation, fiscal measures | Multilevel | ||
|
Elbel [114] *Elbel 2015 |
2017 | Null | R | QE | 17 months | $, D | Fiscal measures, environmental/social planning | Local | ||||
| Ferguson [51] | 2017 | Null | R,W | R | N | 1 year | $ | Fiscal measures, communication/marketing | National | |||
| Gittelsohn [115] | 2017 | Mixed^^ | W | R | RCT+ | 2 years | $, Q | Service provision, communication/marketing | Local | |||
| Hobin [53] | 2017 | Positive | R,W | N | 6 months | $ | Guidelines | National | ||||
| Liu [116] | 2017 | Positive | R | R | R | QE | 4 months | D | Guidelines, fiscal measures, communication/marketing, environmental/social planning | Multilevel | ||
| Minaker [55] | 2017 | Positive | R | W | R | R | QE | 8 months | $ | Environmental/social planning | Local | |
| Rushakoff [117] | 2017 | Positive | R | R | QE | 18 months | $, D | Communication/marketing, environmental/social planning | Local | |||
| Toft [58] | 2017 | Mixed^^ | R | R | R | QE | 3 months | $ | Fiscal measures, environmental/social planning | National | ||
| Vandenbroele [61] | 2017 | Positive | R | QE | 1 month | $ | Guidelines | National | ||||
| Blake [48] | 2018 | Positive | R | R | QE | 17 weeks | $ | Legislation, service provision, fiscal measures | Multilevel | |||
| Franckle [118] | 2018 | Positive | R | R | RCT+ | 5 months | D | Guidelines, fiscal measures, communication/marketing, Environmental/social planning | Multilevel | |||
| Jilcott Pitts [119] | 2018 | Null | R | QE | 1 month | D, H | Environmental/social planning | Local | ||||
| Payne [120] | 2018 | Positive | R | R | QE | 1 month | $ | Communication/marketing, environmental/social planning | Local | |||
| Polascek [121] | 2018 | Positive | R | RCT+ | 4 months | $ | Legislation, service provision, fiscal measures | Multilevel | ||||
| Rogus [122] | 2018 | Mixed^ | R | R | QE | 17 months | D | Fiscal measures | Multilevel | |||
| Walmsley [43] | 2018 | Positive | R | N | 2 years | $ | Environmental/social planning | Local |
Effect: specific combinations of mixed effects are indicated by ^ = positive + negative; ^^ = positive + null; ^^^ = positive + null + negative
Geog, geographic access; Price, price; Prod, product; Prom, promotion; Place, placement. The latter four represent the 4Ps of marketing
R, W: responsibility for implementing intervention changes; R = retailer and W = wholesaler/distributor
Study design: QE = quasi-experimental; RCT+ = randomized controlled trial or other design with comparison groups; N = natural experiment
Outcome(s): $ = sales or purchasing; D = dietary intakes; Q = diet quality; H = other health measures
BCW behavior change wheel
*Articles reporting on same intervention are listed with asterisks for cross-referencing
Effectiveness of the Interventions in Influencing Diet-Related Outcomes
Table 2 provides an overview of the 86 included articles, including the focus of the intervention (geographic access and 4Ps), direction of effect on diet-related outcomes, and associated policy levers according to the Behavior Change Wheel. The table is organized by date of article publication in order to highlight the evolution in the literature over time.
The earliest included paper was published in 1974 [64], and the field has expanded rapidly in the last decade: 61 articles were published from 2008 to 2018. We noted a few thematic and temporal trends. The bulk of studies used promotion-based intervention strategies (sole marketing “P”). Promotion interventions have declined in relative prominence over time, with a greater proportion of studies from 2008 onward based on two or more Ps, as part of a multipronged retail intervention strategy. The literature dealing with community food environments (e.g., store openings to improve geographic access in an underserved community) remains relatively distinct from 4P interventions, with only a handful of studies combining both spatial and in-store strategies. Recent literature has incorporated food system elements, with wholesalers/suppliers as part of interventions, including responsibility for implementing changes.
Consumer purchasing, using an objective measure such as sales data, was a dietary outcome assessed in a majority of studies (52 articles, 60%) (not shown in table). Only 24 articles (28%) assessed dietary intake. Of these, five articles used a 24-h diet recall [85, 93, 101, 102, 114]; two used a 7-day food record [46, 47]; two used full food frequency questionnaires [94, 98]; and the remainder used a brief diet screener, or other brief module as part of a consumer survey.
The majority of articles (58 articles, 67%) described at least one positive effect on diet. Very few articles reported a negative effect (6 articles, of which 4 also reported a positive effect on another dietary outcome). Almost half of articles (43%) described at least one null effect.
Fifteen articles reported mixed effects: 4 articles, positive + negative; 10 articles, positive + null; and 1 article, positive, null, and negative). Note that in all instances of mixed effects, at least one positive effect of the intervention was reported. The mixed effects demonstrate the complexity of purchasing decisions, such as combined “healthy” and “unhealthy” purchases, substitution effects, and the inability to distinguish residual variation in purchasing from environmental versus individual factors. For example, Adjoian et al. [110] assessed purchasing in response to a “healthy checkout” intervention, part of a municipal government supermarket program. They found that a greater proportion of customers bought healthy snacks when using the healthy checkout versus the standard checkout. They also found that a lesser proportion of customers purchased unhealthy snacks from the healthy checkout versus the standard. It is easy to assume from these results that the environmental intervention largely “worked” and that residual unhealthy purchasing would be due to individual factors in a given checkout line. However, the team also found that over a third of items paid for at the healthy checkout were unhealthy items selected from the standard checkout.
Eleven of the 14 articles (79%) describing geographic access interventions reported a mixed or null effect. Not including the two articles using marketing strategies plus geographic access components, when considering 4P (product, promotion, placement, and price) interventions only, a comparable proportion of multi-component interventions tended to have mixed and null effects (15 of 32 articles, or 47% mixed/null), as compared to single component interventions (17 of 40 articles mixed/null, 43%, and 2/40 negative, 5%) (see Table 2).
Policy Levers Underpinning the Interventions
The policy assumptions underpinning interventions have evolved over time. Our policy analysis was intended to unearth what policies the authors expected governments to adopt on the basis of a “successful” intervention, or to detect where authors were attentive to the existing policy context governing stores, and tailored their intervention or evaluation accordingly. As displayed in Table 2, the earlier intervention literature generally emphasized more individualized behavioral assumptions about how policy should support nutrition promotion (e.g., communications/social marketing policies). In contrast, the relative proportion of interventions with a focus on environmental and social planning modifications, and fiscal policies, has increased in the last decade.
Coding based on the NOURISHING framework (not shown in table) also showed the relative emphasis on information-based (rational actor assumptions), in contrast to environmental- and incentive-based policy levers (boundedly rational assumptions). Policy domain “S” (set incentives) in the NOURISHING framework, for instance, is explicitly about incentives and rules to support healthier retail and foodservices environments; 32 (37%) of the articles provided evidence that could be used to inform this type of policy. In contrast, the second “I” (inform people) (35%) and “G” (give nutrition education) (21%) were together even more prominent. For example, one intervention implemented an information kiosk based on a US dietary guideline campaign in-store for 12 weeks [90]. Evidence from this study could reasonably inform public policy tools for nutrition education and dietary guideline implementation, but would be unlikely to inform any government guidance for healthier retailer practices, despite being situated in the setting of the store. Economic policy instruments “U” (use economic tools) featured in just 14 articles. Only 11 articles discussed improving the quality of the food supply (first “I” of the framework), such as the need to address stores’ distributor base [86].
Thirty-four articles (40%) focused on enabling policy conditions that could be adopted through local levers; these were often interventions to address geographic access, such as economic development/urban planning. Twenty-five articles (29%) focused on national level changes, typically large-scale labeling or information initiatives by supermarkets.
The majority of papers (54 articles, 63%) did not mention any specific enabling policies or policy recommendations. Those that did (32 articles, 37%) described options such as
Targeting business interests with locally appropriate pricing structures, marketing, branding, and stocking policy [98];
Municipal economic development initiatives [46, 114]; including microfinancing [89] and attending to local socio-cultural context in retailing [92];
Shelf labeling requirements or incentives [29, 53, 109, 123].
Discussion
The retail food environment intervention literature continues to grow and has become more robust overall, with clearer evidence of the effect of interventions on diet-related outcomes, including consumer purchasing, dietary intakes, and health. There is still much scope for development in the field to improve our understanding of the complex relationship between components of interventions and specific dietary behavior.
Retail intervention strategies have received occasional blanket criticism for a lack of effectiveness [106]. Caution has been directed especially to addressing spatial gaps in store access [98, 114, 124], and in our review, a high proportion of these interventions had mixed or null effects on diet. The combination of geographic access and in-store strategies has had minimal uptake, and we would echo others in recommending that is an area ripe for elaboration [45••, 98, 102], given the ample evidence that despite the potentially positive effects of introducing new stores in terms of food access, that merchandising activities within them can continue to represent an unhealthy influence on dietary behavior.
Confirming earlier systematic reviews, the majority of interventions showed at least one positive effect on a diet-related outcome, particularly among 4P strategies. Among 4P studies, a comparable proportion of articles reporting on multi-component strategies and single component strategies had mixed and null effects. That said, many of the multi-component studies are increasingly attempting to both intervene in and evaluate more than one dietary outcome. This is a development that has strengthened the literature but may also explain mixed outcomes. Continued engagement with multipronged interventions may offer further insights into implementation, and to improving measurement of linking steps in the impact on diet-related behavior. For example, Gittelsohn et al. evaluated the effect of a combined product availability and promotion initiative working in partnership on the Navajo Nation with stores in those communities, to assess the impact on psychosocial predictors of food selection and self-reported food purchasing practices in addition to weight [94]. This randomized controlled trial had a null result in bivariate analyses comparing intervention and comparison groups at follow-up, but found a positive effect on study outcomes mediated by exposure to the intervention.
The widespread use of proximal outcome metrics measured from sales data has benefitted the quality of the literature. The use of purchasing data linked to individuals/households (e.g., loyalty cards) is a particularly strong option. Sales/purchasing data offers researchers confidence to communicate objective study outcomes to policymakers as well as to retail business stakeholders who are interested in the direct and indirect impact of interventions on store revenue and economic viability. A continued research gap, however, is the robustness with which dietary intakes are examined. Kirkpatrick et al. [125], in a systematic review of dietary assessment in food environments research (articles from 2007 to 2012, predominantly cross-sectional assessments), cautioned that the predominance of brief dietary assessment instruments was a limitation, and contributor to measurement bias. Our review suggests that this issue persists and may have led to null or mixed effects in some cases, as well as a lack of generalizability and reproducibility. Indeed, the heterogeneity in dietary assessment, as well as other outcome measures in this review, contributed to our inability to meaningfully compare magnitude of effect among the diverse studies included. Although brief diet assessment tools are less resource-intensive—and may be adequate for focused assessment of one component of diet, the case for some interventions—on the whole, where the intent is to capture intervention effects on total diet in the short term, a 24-h recall would be less prone to systematic error [125]. Another benefit of the 24-h recall specifically in retail interventions would be to capture contextual attributes around food selection, to further unpack how the intervention response occurs in the community. For example, the 24-h recall may better reflect dietary patterns in relation to food supply given that it is not restricted to a pre-specified food lists, offering the potential to assess dietary substitutions in response to an intervention, and details of location of eating or purchase can be readily collected alongside intakes.
Behavior Change Communication
The results of this review indicate that behavior change communication approaches are still a mainstay of retail food environment interventions for changing diets. This may be a reflection of the overall development of the field, which is still relatively new, and has drawn from disciplinary insights in marketing and consumer cognition. Another consideration is that behavior change communication strategies may be more acceptable and feasible for retailer partners to implement. Environmental and social restructuring, and fiscal interventions have become more important within the rapid expansion of retail food environment research in the last decade, likely due to the influence of behavioral economics, social epidemiology, spatial and economic geography.
From a policy standpoint, we would also argue the possibility that influencing food choices in store environments continues to be viewed as a form of “downstream” behavioral health promotion and that “upstream” public policies work separately. It is possible that researchers assessing diet-related interventions in-store see these strategies as unique from—if complementary to—the enabling public policy levers that create broader transformative change in consumption patterns at the population level. This would explain, in part, the distinctiveness of many fiscal interventions that could not be captured within our review inclusion criteria. For example, promotion strategies directed at a few products may not need to wait for a specific policy decision to implement the change widely, as long as buy-in is secured from retailer partners. In contrast, substantive adoption of successful pricing strategies may rely on longer term structural changes and public budget commitments, including adoption of development subsidies, coordination of the supplier base, tax expenditures, or other shifts in tax structures, to motivate corporations to act. This has health equity implications, where the low-hanging fruit of promotion strategies may be used more widely through targeted efforts at dietary improvement, resulting in uneven implementation at the population level.
Policies Enabling Interventions
The studies included in our review indicate that there has been limited attention to enabling policies, or the system-wide policy context where interventions are designed and delivered. In part, this may have been an artefact of publication conventions, where contemplating policy implications that seem to stray from specific outcomes is discouraged. Studies that commented on enabling factors acknowledged that aligning with local context was important [92], which includes attending to how policies structure the behavior of actors well beyond eaters, and beyond the health sector [25•, 126, 127]. Enabling policies could encompass structures affecting store capacity and viability—such as trade pacts, labor market policies, social protections, and other forces that underpin household purchasing power. These, too, are part of the agenda-setting calculus and policy trade-offs to address diet-related risk [114]. There is a limited basis for assessing how these types of policies can link up with store-level interventions within the papers in this review. An enabling policy environment may be an important contextual feature to isolate for measurement or otherwise take into account, to assess its interaction with intervention design, implementation and outcomes [128, 129]. Adding context may have advantages for understanding why interventions succeed or fail, and how they can be adapted or translated across settings.
Most of the interventions included in this review were led by public health (including researchers and/or municipal agencies) and targeted at consumers. Very few studies targeted retailers themselves as a policy actor whose behavior could be changed in a healthier direction. The distinctive perspective of the retailer [17] has become increasingly important in measuring and attempting to modify retail food environment features to become more health-promoting. Only recently has observational research on food stores begun to focus on retailers’ role and indeed agency in shaping food access within the food system [130–133], and few interventions have been retailer-led [48, 134, 135]. Milio has argued that to make the “healthy choice the easy choice” there is a two-part health promotion imperative to direct behavior change incentives towards consumers as well as corporations [136, 137]. Although interventions are being delivered in a growing variety of community settings, the bulk of the retail evidence still comes from a body of work that largely assumes a theory of change relying on the consumer as its focus.
There are notable exceptions: Budd et al.’s article on the B’More Healthy: Retail Rewards intervention is part of a long trajectory of research programs examining multipronged small store interventions in that US jurisdiction [113•]. They focused on retailer outcomes, and considered a full spectrum of behavior change mechanisms for both retailers and consumers in producing the dietary outcome.
In the last decade, the literature has increasingly emphasized evaluating interventions within the ecosystem of the retail food environment [11, 45••], which aligns with a healthy public policy approach. Our review indicated that area-based versus in-store interventions seem to focus on a fundamentally different vision of the role of policy in healthier community environments. And this may be related to the clearer imperative for area-based interventions to situate stores relationally in the retail ecosystem. Although supermarket interventions have been carried out in various forms of cooperation with retailers over the course of the intervention literature [53, 67], we may be continuing to miss an important policy opportunity to target those retailers in more holistic health promotion efforts. The growing literature targeting wholesalers and supply chain pressures for small stores in interventions is an integrative development that may help expand our understanding of enabling policies for the retail ecosystem [51, 53, 55, 85–87, 105, 113•, 115].
Limitations
Our review had a number of limitations. Our aim was to capture a full scope of retail food environment interventions, so unlike some past reviews, we combined geographic access and in-store approaches. Although this met our objectives, the resulting methodological complexity meant that we were unable to capture fully how multipronged interventions may have had explanations for mixed or null effects in comparison to narrower interventions that did not account for store ecosystems. This complexity and heterogeneity also limited our ability to assess and meaningfully compare effect sizes among interventions. As such, we chose to focus on reporting direction of effect, and how this differed among study types. Further analyses might consider developing meta-analysis methods isolating a subgroup of interventions with greater comparability of measures, such as the store sales data studies. Another limitation of this review was our criterion that included interventions should target a general population of shoppers, which resulted in the exclusion of a number of price-based intervention studies that have been based on membership in a cohort [31, 32]. This means that the full scope of fiscal policy discussion in the literature is missing. We excluded studies that had no dietary outcome; paradoxically, this meant that we could not capture some retailer studies that may have offered relevant insights into policy levers. Dunaway et al.’s study [138], for example, was excluded but is one of the few studies beginning to measure retailer characteristics in detail, conducting an in-depth financial analysis alongside evaluating the effect of an infrastructure project on stocking of fruits and vegetables.
Conclusion
Retail food environments are one of the main sources of diet-related risk, but also hold health promotion policy possibility [126]. Retail stores are private corporations, but can also be considered a health promotion setting: [139, 140] a place-based organizational interface between the complex food system and eaters [141]. This review provides an update on the growing array of health promotion interventions taking place in the store environment, and their effectiveness in influencing diet-related outcomes. Retail stores are physical, social, economic, and cultural spaces that shape our dietary behaviors and where structural barriers to nutritional health such as the power over and ownership of food sources are manifest. Our review attempts to expand how we think about public policies that can support and enable effective interventions in these spaces.
Acknowledgments
Our thanks to Mary Myketyn-Driscoll and Emily Taylor who provided research assistance at earlier stages in the review.
Funding
CM is supported by the Canada Research Chairs program and the Canadian Institutes of Health Research (CIHR FRN KAL 139697), RH is supported by the Canadian Institutes of Health Research (Doctoral Award), NT and GL each by a Nova Scotia Graduate Scholarship from the Government of Nova Scotia.
Compliance with Ethical Standards
Ethics
This review did not require institutional ethics review board approval.
Conflict of Interest
Catherine L. Mah, Gabriella Luongo, Rebecca Hasdell, Nathan Taylor, and Brian Lo declare they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Footnotes
This article is part of the Topical Collection on Cardiovascular Disease
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Catherine L. Mah, Email: catherine.mah@dal.ca
Gabriella Luongo, Email: g.luongo@mail.utoronto.ca.
Rebecca Hasdell, Email: rebecca.hasdell@dal.ca.
Nathan G. A. Taylor, Email: nathan.taylor@dal.ca
Brian K. Lo, Email: bl592@cornell.edu
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
- 1.Afshin Ashkan, Sur Patrick John, Fay Kairsten A., Cornaby Leslie, Ferrara Giannina, Salama Joseph S, Mullany Erin C, Abate Kalkidan Hassen, Abbafati Cristiana, Abebe Zegeye, Afarideh Mohsen, Aggarwal Anju, Agrawal Sutapa, Akinyemiju Tomi, Alahdab Fares, Bacha Umar, Bachman Victoria F, Badali Hamid, Badawi Alaa, Bensenor Isabela M, Bernabe Eduardo, Biadgilign Sibhatu Kassa K, Biryukov Stan H, Cahill Leah E, Carrero Juan J, Cercy Kelly M., Dandona Lalit, Dandona Rakhi, Dang Anh Kim, Degefa Meaza Girma, El Sayed Zaki Maysaa, Esteghamati Alireza, Esteghamati Sadaf, Fanzo Jessica, Farinha Carla Sofia e Sá, Farvid Maryam S, Farzadfar Farshad, Feigin Valery L., Fernandes Joao C, Flor Luisa Sorio, Foigt Nataliya A., Forouzanfar Mohammad H, Ganji Morsaleh, Geleijnse Johanna M., Gillum Richard F, Goulart Alessandra C, Grosso Giuseppe, Guessous Idris, Hamidi Samer, Hankey Graeme J., Harikrishnan Sivadasanpillai, Hassen Hamid Yimam, Hay Simon I., Hoang Chi Linh, Horino Masako, Islami Farhad, Jackson Maria D., James Spencer L., Johansson Lars, Jonas Jost B., Kasaeian Amir, Khader Yousef Saleh, Khalil Ibrahim A., Khang Young-Ho, Kimokoti Ruth W, Kokubo Yoshihiro, Kumar G Anil, Lallukka Tea, Lopez Alan D, Lorkowski Stefan, Lotufo Paulo A., Lozano Rafael, Malekzadeh Reza, März Winfried, Meier Toni, Melaku Yohannes A, Mendoza Walter, Mensink Gert B.M., Micha Renata, Miller Ted R, Mirarefin Mojde, Mohan Viswanathan, Mokdad Ali H, Mozaffarian Dariush, Nagel Gabriele, Naghavi Mohsen, Nguyen Cuong Tat, Nixon Molly R, Ong Kanyin L, Pereira David M., Poustchi Hossein, Qorbani Mostafa, Rai Rajesh Kumar, Razo-García Christian, Rehm Colin D, Rivera Juan A, Rodríguez-Ramírez Sonia, Roshandel Gholamreza, Roth Gregory A, Sanabria Juan, Sánchez-Pimienta Tania G, Sartorius Benn, Schmidhuber Josef, Schutte Aletta Elisabeth, Sepanlou Sadaf G., Shin Min-Jeong, Sorensen Reed J.D., Springmann Marco, Szponar Lucjan, Thorne-Lyman Andrew L, Thrift Amanda G, Touvier Mathilde, Tran Bach Xuan, Tyrovolas Stefanos, Ukwaja Kingsley Nnanna, Ullah Irfan, Uthman Olalekan A, Vaezghasemi Masoud, Vasankari Tommi Juhani, Vollset Stein Emil, Vos Theo, Vu Giang Thu, Vu Linh Gia, Weiderpass Elisabete, Werdecker Andrea, Wijeratne Tissa, Willett Walter C, Wu Jason H, Xu Gelin, Yonemoto Naohiro, Yu Chuanhua, Murray Christopher J L. Health effects of dietary risks in 195 countries, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. The Lancet. 2019;393(10184):1958–1972. doi: 10.1016/S0140-6736(19)30041-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gakidou E, Afshin A, Abajobir AA, et al. Global, regional, and national comparative risk assessment of 84 behavioural, environmental and occupational, and metabolic risks or clusters of risks, 1990-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet. 2017;390(10100):1345–1422. doi: 10.1016/S0140-6736(17)32366-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.United Nations General Assembly. United Nations Decade of Action on Nutrition. Seventieth Session of the United Nations General Assembly, New York, 15–28 September 2015. Agenda Item 15 (A70/L.42). New York: United Nations General Assembly; 2016. http://www.un.org/ga/search/view_doc.asp?symbol = A/70/L.42.
- 4.Lytle LA, Sokol RL. Measures of the food environment: a systematic review of the field, 2007-2015. Health Place. 2017;44(C):18–34. doi: 10.1016/j.healthplace.2016.12.007. [DOI] [PubMed] [Google Scholar]
- 5.Caspi CE, Sorensen G, Subramanian SV, Kawachi I. The local food environment and diet: a systematic review. Health Place. 2012;18(5):1172–1187. doi: 10.1016/j.healthplace.2012.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lang T, Heasman M. Food Wars: the Global Battle for Mouths. Earthscan: Minds and Markets; 2004. [Google Scholar]
- 7.Engler-Stringer R, Le H, Gerrard A, Muhajarine N. The community and consumer food environment and children’s diet: a systematic review. BMC Public Health. 2014;14(1):522. doi: 10.1186/1471-2458-14-522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Glanz K. Measuring Food Environments. Am J Prev Med. 2009;36(4):S93–S98. doi: 10.1016/j.amepre.2009.01.010. [DOI] [PubMed] [Google Scholar]
- 9.Cummins S, Macintyre S. Food environments and obesity-neighbourhood or nation? Int J Epidemiol. 2006;35(1):100–104. doi: 10.1093/ije/dyi276. [DOI] [PubMed] [Google Scholar]
- 10.Swinburn B, Egger G, Raza F. Dissecting obesogenic environments: the development and application of a framework for identifying and prioritizing environmental interventions for obesity. Prev Med. 1999;29(6):563–570. doi: 10.1006/pmed.1999.0585. [DOI] [PubMed] [Google Scholar]
- 11.Peeters A. Obesity and the future of food policies that promote healthy diets. Nat Rev Endocrinol. 2018;14(7):430–437. doi: 10.1038/s41574-018-0026-0. [DOI] [PubMed] [Google Scholar]
- 12.Hawkes C, Jewell J, Allen K. A food policy package for healthy diets and the prevention of obesity and diet-related non-communicable diseases: the NOURISHING framework. Obes Rev. 2013;14:159–168. doi: 10.1111/obr.12098. [DOI] [PubMed] [Google Scholar]
- 13.Adam A, Jensen JD. What is the effectiveness of obesity related interventions at retail grocery stores and supermarkets?—a systematic review. BMC Public Health. 2016;16:1–18. doi: 10.1186/s12889-016-3985-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cameron Adrian J., Charlton Emma, Ngan Winsfred W., Sacks Gary. A Systematic Review of the Effectiveness of Supermarket-Based Interventions Involving Product, Promotion, or Place on the Healthiness of Consumer Purchases. Current Nutrition Reports. 2016;5(3):129–138. doi: 10.1007/s13668-016-0172-8. [DOI] [Google Scholar]
- 15.Escaron AL, Meinen AM, Nitzke SA, Martínez-Donate AP. Supermarket and grocery store–based interventions to promote healthful food choices and eating practices: a systematic review. Prev Chronic Dis. 2013;10:120156–120120. doi: 10.5888/pcd10.120156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gittelsohn J, Rowan M, Gadhoke P. Interventions in small food stores to change the food environment, improve diet, and reduce risk of chronic disease. Prev Chronic Dis. 2012;9:110015. doi: 10.5888/pcd9.110015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Glanz K, Bader MDM, Iyer S. Retail grocery store marketing strategies and obesity. Am J Prev Med. 2012;42(5):503–512. doi: 10.1016/j.amepre.2012.01.013. [DOI] [PubMed] [Google Scholar]
- 18.Hartmann-Boyce Jamie, Bianchi Filippo, Piernas Carmen, Riches Sarah Payne, Frie Kerstin, Nourse Rebecca, Jebb Susan A. Grocery store interventions to change food purchasing behaviors: a systematic review of randomized controlled trials. The American Journal of Clinical Nutrition. 2018;107(6):1004–1016. doi: 10.1093/ajcn/nqy045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hasanthi Abeykoon A, Engler-Stringer R, Muhajarine N. Health-related outcomes of new grocery store interventions: a systematic review. Public Health Nutr. 2017;20(12):2236–2248. doi: 10.1017/S1368980017000933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Liberato SC, Bailie R, Brimblecombe J. Nutrition interventions at point-of-sale to encourage healthier food purchasing: a systematic review. BMC Public Health. 2014;14(1):919–914. doi: 10.1186/1471-2458-14-919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Pinard CA, Shanks CB, Harden SM, Yaroch AL. An integrative literature review of small food store research across urban and rural communities in the U.S. Prev Med Rep. 2016;3:324–332. doi: 10.1016/j.pmedr.2016.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.van’t Riet J. Sales effects of product health information at points of purchase: a systematic review. Public Health Nutr. 2012;16(3):418–429. doi: 10.1017/S1368980012001103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Woodruff RC, Raskind IG, Harris DM, Gazmararian JA, Kramer M, Haardörfer R, Kegler MC. The dietary impact of introducing new retailers of fruits and vegetables into a community: results from a systematic review. Public Health Nutr. 2017;21(5):981–991. doi: 10.1017/S1368980017003226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Afshin A, Penalvo J, Del Gobbo L, et al. CVD prevention through policy: a review of mass media, food/menu labeling, taxation/subsidies, built environment, school procurement, worksite wellness, and marketing standards to improve diet. Curr Cardiol Rep. 2015;17(11):2224–2212. doi: 10.1007/s11886-015-0658-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Allender S, Gleeson E, Crammond B, et al. Policy change to create supportive environments for physical activity and healthy eating: which options are the most realistic for local government? Health Promot Int. 2012;27(2):261–274. doi: 10.1093/heapro/dar018. [DOI] [PubMed] [Google Scholar]
- 26.Thow AM, Downs S, Jan S. A systematic review of the effectiveness of food taxes and subsidies to improve diets: understanding the recent evidence. Nutr Rev. 2014;72(9):551–565. doi: 10.1111/nure.12123. [DOI] [PubMed] [Google Scholar]
- 27.World Health Organization. Adelaide Recommendations on Healthy Public Policy. Second International Conference on Health Promotion, Adelaide, South Australia, 5-9 April 1988. Adelaide: World Health Organization; 1988. https://www.who.int/healthpromotion/conferences/previous/adelaide/en/.
- 28.Glanz K, Johnson L, Yaroch A, Phillips M, Ayala GX, Davis EL. Measures of retail food store environments and sales: review and implications for healthy eating initiatives. J Nutr Educ Behav. 2016;48(4):280–288.e281. doi: 10.1016/j.jneb.2016.02.003. [DOI] [PubMed] [Google Scholar]
- 29.Berning JP, Chouinard HH, McCluskey JJ. Do positive nutrition shelf labels affect consumer behavior? Findings from a field experiment with scanner data. Am J Agric Econ. 2010;22(3):25–26. doi: 10.1093/ajae/aaq104. [DOI] [Google Scholar]
- 30.Bernales-Korins M, Ang IYH, Khan S, Geliebter A. Psychosocial influences on fruit and vegetable intake following a NYC supermarket discount. Obesity. 2017;25(8):1321–1328. doi: 10.1002/oby.21876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ni Mhurchu C, Blakely T, Jiang Y, Eyles HC, Rodgers A. Effects of price discounts and tailored nutrition education on supermarket purchases: a randomized controlled trial. Am J Clin Nutr. 2010;91(3):736–747. doi: 10.3945/ajcn.2009.28742. [DOI] [PubMed] [Google Scholar]
- 32.Ball K, McNaughton SA, Le HN, et al. Influence of price discounts and skill-building strategies on purchase and consumption of healthy food and beverages: outcomes of the Supermarket Healthy Eating for Life randomized controlled trial. Am J Clin Nutr. 2015;101(5):1055–1064. doi: 10.3945/ajcn.114.096735. [DOI] [PubMed] [Google Scholar]
- 33.Jensen JD, Sommer I. Reducing calorie sales from supermarkets – “silent” reformulation of retailer-brand food products. Int J Behav Nutr Phys Act. 2017;14(1):325–314. doi: 10.1186/s12966-017-0559-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Blake MR, Lancsar E, Peeters A, Backholer K. The effect of sugar-sweetened beverage price increases and educational messages on beverage purchasing behavior among adults. Appetite. 2018;126:156–162. doi: 10.1016/j.appet.2018.03.012. [DOI] [PubMed] [Google Scholar]
- 35.Michie S, van Stralen MM, West R. The behaviour change wheel: a new method for characterising and designing behaviour change interventions. Implement Sci. 2011;6:42. doi: 10.1186/1748-5908-6-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Michie S, Richardson M, Johnston M, et al. The behavior change technique taxonomy (v1) of 93 hierarchically clustered techniques: building an international consensus for the reporting of behavior change interventions. Ann Behav Med. 2013;46(1):81–95. doi: 10.1007/s12160-013-9486-6. [DOI] [PubMed] [Google Scholar]
- 37.Effective Public Health Practice Project . Effective Public Health Practice Project (EPHPP) Quality Assessment Tool for Quantitative Studies. Hamilton: Effective Public Health Practice Project; 1998. [Google Scholar]
- 38.de Wijk René A., Maaskant Anna J., Polet Ilse A., Holthuysen Nancy T. E., van Kleef Ellen, Vingerhoeds Monique H. An In-Store Experiment on the Effect of Accessibility on Sales of Wholegrain and White Bread in Supermarkets. PLOS ONE. 2016;11(3):e0151915. doi: 10.1371/journal.pone.0151915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Papies EK, Potjes I, Keesman M, Schwinghammer S, van Koningsbruggen GM. Using health primes to reduce unhealthy snack purchases among overweight consumers in a grocery store. Int J Obes. 2014;38(4):597–602. doi: 10.1038/ijo.2013.136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Steenhuis I, van Assema P, van Breukelen G, Glanz K. The effectiveness of nutrition education and labeling in Dutch supermarkets. Am J Health Promot. 2004;18(3):221–224. doi: 10.4278/0890-1171-18.3.221. [DOI] [PubMed] [Google Scholar]
- 41.Waterlander WE, de Boer MR, Schuit AJ, Seidell JC, Steenhuis IH. Price discounts significantly enhance fruit and vegetable purchases when combined with nutrition education: a randomized controlled supermarket trial. Am J Clin Nutr. 2013;97(4):886–895. doi: 10.3945/ajcn.112.041632. [DOI] [PubMed] [Google Scholar]
- 42.Salmon SJ, De Vet E, Adriaanse MA, Fennis BM, Veltkamp M, De Ridder DTD. Social proof in the supermarket: promoting healthy choices under low self-control conditions. Food Qual Prefer. 2015;45(C):113–120. doi: 10.1016/j.foodqual.2015.06.004. [DOI] [Google Scholar]
- 43.Walmsley R, Jenkinson D, Saunders I, Howard T, Oyebode O. Choice architecture modifies fruit and vegetable purchasing in a university campus grocery store: time series modelling of a natural experiment. BMC Public Health. 2018;18(1):1–9. doi: 10.1186/s12889-018-6063-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Cummins S, Findlay A, Higgins C, Petticrew M, Sparks L, Thomson H. Reducing inequalities in health and diet: findings from a study on the impact of a food retail development. Environ Plann A. 2008;40(2):402–422. doi: 10.1068/a38371. [DOI] [Google Scholar]
- 45.Cummins S, Findlay A, Petticrew M, Sparks L. Retail-led regeneration and store-switching behaviour. J Retail Consum Serv. 2008;15(4):288–295. doi: 10.1016/j.jretconser.2007.06.002. [DOI] [Google Scholar]
- 46.Wrigley N, Warm D, Margetts B. Deprivation, diet, and food-retail access: findings from the Leeds ‘Food Deserts’ Study. Environ Plann A. 2003;35(1):151–188. doi: 10.1068/a35150. [DOI] [Google Scholar]
- 47.Gill L, Rudkin S. Deconstructing supermarket intervention effects on fruit and vegetable consumption in areas of limited retail access: evidence from the Seacroft Study. Environ Plann A. 2014;46(3):649–665. doi: 10.1068/a45675. [DOI] [Google Scholar]
- 48.Blake MR, Peeters A, Lancsar E, et al. Retailer-led sugar-sweetened beverage price increase reduces purchases in a hospital convenience store in Melbourne, Australia: a mixed methods evaluation. J Acad Nutr Diet. 2018;118(6):1027–1036.e1028. doi: 10.1016/j.jand.2017.06.367. [DOI] [PubMed] [Google Scholar]
- 49.Brimblecombe J, Ferguson M, Chatfield MD, Liberato SC, Gunther A, Ball K, Moodie M, Miles E, Magnus A, Mhurchu CN, Leach AJ, Bailie R, SHOP@RIC research collaborative Effect of a price discount and consumer education strategy on food and beverage purchases in remote Indigenous Australia: a stepped-wedge randomised controlled trial. Lancet Public Health. 2017;2(2):e82–e95. doi: 10.1016/S2468-2667(16)30043-3. [DOI] [PubMed] [Google Scholar]
- 50.Scott JA, Begley AM, Miller MR, Binns CW. Nutrition education in supermarkets: the Lifestyle 2000 experience. Aust J Public Health. 1991;15(1):49–55. doi: 10.1111/j.1753-6405.1991.tb00010.x. [DOI] [PubMed] [Google Scholar]
- 51.Ferguson M, O’Dea K, Holden S, Miles E, Brimblecombe J. Food and beverage price discounts to improve health in remote Aboriginal communities: mixed method evaluation of a natural experiment. Aust N Z J Public Health. 2017;41(1):32–37. doi: 10.1111/1753-6405.12616. [DOI] [PubMed] [Google Scholar]
- 52.Crawford SM, Kalina L. The Shop Smart tour. J Nutr Educ. 1993;25(2):100B. doi: 10.1016/S0022-3182(12)80996-4. [DOI] [Google Scholar]
- 53.Hobin E, Bollinger B, Sacco J, et al. Consumers’ response to an on-shelf nutrition labelling system in supermarkets: evidence to inform policy and practice. The Milbank Quarterly. 2017;95(3):494–534. doi: 10.1111/1468-0009.12277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Fuller D, Engler-Stringer R, Muhajarine N. Examining food purchasing patterns from sales data at a full-service grocery store intervention in a former food desert. Prev Med Rep. 2015;2(C):164–169. doi: 10.1016/j.pmedr.2015.02.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Minaker LM, Lynch M, Cook B, Mah CL. Exploring sales data during a healthy corner store intervention in Toronto: The Food Retail Environments Shaping Health (FRESH) project. Health Promot Chronic Dis Prev Can. 2017;37(10):294–301. doi: 10.24095/hpcdp.37.10.04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Winkler LL, Christensen U, Glümer C, Bloch P, Mikkelsen BE, Wansink B, Toft U. Substituting sugar confectionery with fruit and healthy snacks at checkout – a win-win strategy for consumers and food stores? A study on consumer attitudes and sales effects of a healthy supermarket intervention. BMC Public Health. 2016;16(1):1–12. doi: 10.1186/s12889-016-3849-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Adam A, Jensen JD, Sommer I, Hansen GL. Does shelf space management intervention have an effect on calorie turnover at supermarkets? J Retail Consum Serv. 2016;34(C):311–318. doi: 10.1016/j.jretconser.2016.07.007. [DOI] [Google Scholar]
- 58.Toft U, Winkler LL, Mikkelsen BE, Bloch P. mer CGU. Discounts on fruit and vegetables combined with a space management intervention increased sales in supermarkets. Eur J Clin Nutr. 2017;71(4):476–480. doi: 10.1038/ejcn.2016.272. [DOI] [PubMed] [Google Scholar]
- 59.Närhinen M, Nissinen A, Puska P. Changes in supermarket sales during and after a staged health promotion campaign. Br Food J. 2000;102(4):308–319. doi: 10.1108/00070700010327733. [DOI] [Google Scholar]
- 60.Närhinen M, Nissinen A, Puska P. Healthier choices in a supermarket: the municipal food control can promote health. Br Food J. 1999;101(2):99–108. doi: 10.1108/00070709910261909. [DOI] [Google Scholar]
- 61.Vandenbroele J, Slabbinck H, Van Kerckhove A, Vermeir I. Curbing portion size effects by adding smaller portions at the point of purchase. Food Qual Prefer. 2018;64:82–87. doi: 10.1016/j.foodqual.2017.10.015. [DOI] [Google Scholar]
- 62.Ogawa Y, Tanabe N, Honda A, Azuma T, Seki N, Suzuki T, Suzuki H. Point-of-purchase health information encourages customers to purchase vegetables: objective analysis by using a point-of-sales system. Environ Health Prev Med. 2010;16(4):239–246. doi: 10.1007/s12199-010-0192-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Sigurdsson V, Larsen NM, Gunnarsson D. An in-store experimental analysis of consumers' selection of fruits and vegetables. Serv Ind J. 2011;31(15):2587–2602. doi: 10.1080/02642069.2011.531126. [DOI] [Google Scholar]
- 64.Curhan RC. The effects of merchandising and temporary promotional activities on the sales of fresh fruits and vegetables in supermarkets. J Mark Res. 1974;11(3):286–294. doi: 10.1177/002224377401100307. [DOI] [Google Scholar]
- 65.Jeffery RW, Pirie PL, Rosenthal BS, Gerber WM, Murray DM. Nutrition education in supermarkets: an unsuccessful attempt to influence knowledge and product sales. J Behav Med. 1982;5(2):189–200. doi: 10.1007/BF00844808. [DOI] [PubMed] [Google Scholar]
- 66.Levy AS, Mathews O, Stephenson M, Tenney JE, Schucker RE. The impact of a nutrition information program on food purchases. J Public Policy Mark. 1985;4:1–13. doi: 10.1177/074391568500400101. [DOI] [Google Scholar]
- 67.Ernst ND, Wu M, Frommer P, Katz E, Matthews O, Moskowitz J, Pinsky JL, Pohl S, Schreiber GB, Sondik E. Nutrition education at the point of purchase: the Foods for Health project evaluated. Prev Med. 1986;15(1):60–73. doi: 10.1016/0091-7435(86)90036-8. [DOI] [PubMed] [Google Scholar]
- 68.Russo JE, Staelin R, Nolan CA, Russell GJ, Metcalf BL. Nutrition information in the supermarket. J Consum Res. 1986;13(1):48–70. doi: 10.1086/209047. [DOI] [Google Scholar]
- 69.Achabal DD, McIntyre SH, Bell CH, Tucker N. The effect of nutrition POP signs on consumer attitudes and behavior. J Retail. 1987;63(1):9–24. [Google Scholar]
- 70.Dougherty MF, Wittsten AB, Guarino MA. Promoting low-fat foods in the supermarket using various methods, including videocassettes. J Am Diet Assoc. 1990;90(8):1106–1108. [PubMed] [Google Scholar]
- 71.Winett RA, Moore JF, Wagner JL, Hite LA, Leahy M, Neubauer TE, Walberg JL, Walker WB, Lombard D, Geller ES. Altering shoppers’ supermarket purchases to fit nutritional guidelines: an interactive information system. J Appl Behav Anal. 1991;24(1):95–105. doi: 10.1901/jaba.1991.24-95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Winett RA, Wagner JL, Moore JF, Walker WB. An experimental evaluation of a prototype public access nutrition information system for supermarkets. Health Psychol. 1991;10(1):75–78. doi: 10.1037/0278-6133.10.1.75. [DOI] [PubMed] [Google Scholar]
- 73.Patterson BH, Kessler LG, Wax Y, et al. Evaluation of a supermarket intervention: the NCI-Giant Food Eat for Health study. Eval Rev. 1992;16(5):464–490. doi: 10.1177/0193841X9201600502. [DOI] [Google Scholar]
- 74.Rodgers AB, Kessler LG, Portnoy B, et al. “Eat for Health”: a supermarket intervention for nutrition and cancer risk reduction. Am J Public Health. 1994;84(1):72–76. doi: 10.2105/AJPH.84.1.72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Paine-Andrews A, Francisco VT, Fawcett SB, Johnston J, Coen S. Health marketing in the supermarket: using prompting, product sampling, and price reduction to increase customer purchases of lower-fat items. Health Mark Q. 1996;14(2):85–99. doi: 10.1300/J026v14n02_08. [DOI] [PubMed] [Google Scholar]
- 76.Anderson ES, Winett RA, Bickley PG, Walberg-Rankin J, Moore JF, Leahy M, Harris CE, Gerkin RE. The effects of a multimedia system in supermarkets to alter shoppers’ food purchases: nutritional outcomes and caveats. J Health Psychol. 1997;2(2):209–223. doi: 10.1177/135910539700200217. [DOI] [PubMed] [Google Scholar]
- 77.Kristal AR, Goldenhar L, Muldoon J, Morton RF. Evaluation of a supermarket intervention to increase consumption of fruits and vegetables. 1997;11(6):422-425. [DOI] [PubMed]
- 78.Teisl MF, Levy AS. Does nutrition labeling lead to healthier eating? Journal of Food Distribution Research. 1997;28(3):18–27. [Google Scholar]
- 79.Winett RA, Anderson ES, Bickley PG, et al. Nutrition for a lifetime system: a multimedia system for altering food supermarket shoppers' purchases to meet nutritional guidelines. Comput Hum Behav. 1997;13(3):371–392. doi: 10.1016/S0747-5632(97)00015-0. [DOI] [Google Scholar]
- 80.Connell D, Goldberg JP, Folta SC. An intervention to increase fruit and vegetable consumption using audio communications: in-store public service announcements and audiotapes. J Health Commun. 2001;6(1):31–43. doi: 10.1080/10810730150501396. [DOI] [PubMed] [Google Scholar]
- 81.Weinehall L, Hellsten G, Bowman K, Hallmans G. Prevention of cardiovascular disease in Sweden: The Norsjoe community intervention programme-Motives, methods and intervention components. Scandinavian Journal of Public Health. 2011;29(suppl 56):13–20. [PubMed] [Google Scholar]
- 82.Wang MC, MacLeod KE, Steadman C, et al. Is the opening of a neighborhood full-service grocery store followed by a change in the food behavior of residents? Journal of Hunger & Environmental Nutrition. 2007;2(1):3–18. doi: 10.1080/19320240802077789. [DOI] [Google Scholar]
- 83.Song H-J, Gittelsohn J, Kim M, Suratkar S, Sharma S, Anliker J. A corner store intervention in a low-income urban community is associated with increased availability and sales of some healthy foods. Public Health Nutr. 2009;12(11):2060–2067. doi: 10.1017/S1368980009005242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Freedman MR, Connors R. Point-of-purchase nutrition information influences food-purchasing behaviors of college students: a pilot study. J Am Diet Assoc. 2010;110(8):1222–1226. doi: 10.1016/j.jada.2010.05.002. [DOI] [PubMed] [Google Scholar]
- 85.Gittelsohn J, Vijayadeva V, Davison N, et al. A food store intervention trial improves caregiver psychosocial factors and children’s dietary intake in Hawaii. Obesity. 2010;18(n1s):S84–S90. doi: 10.1038/oby.2009.436. [DOI] [PubMed] [Google Scholar]
- 86.Gittelsohn J, Song H-J, Suratkar S, et al. An urban food store intervention positively affects food-related psychosocial variables and food behaviors. Health Educ Behav. 2010;37(3):390–402. doi: 10.1177/1090198109343886. [DOI] [PubMed] [Google Scholar]
- 87.Jetter KM, Cassady DL. Increasing fresh fruit and vegetable availability in a low-income neighborhood convenience store: a pilot study. Health Promot Pract. 2010;11(5):694–702. doi: 10.1177/1524839908330808. [DOI] [PubMed] [Google Scholar]
- 88.Sutherland LA, Kaley LA, Fischer L. Guiding Stars: the effect of a nutrition navigation program on consumer purchases at the supermarket. Am J Clin Nutr. 2010;91(4):1090S–1094S. doi: 10.3945/ajcn.2010.28450C. [DOI] [PubMed] [Google Scholar]
- 89.Dannefer R, Williams DA, Baronberg S, Silver L. Healthy Bodegas: increasing and promoting healthy foods at corner stores in New York City. Am J Public Health. 2012;102(10):e27–e31. doi: 10.2105/AJPH.2011.300615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Holmes AS, Estabrooks PA, Davis GC, Serrano EL. Effect of a grocery store intervention on sales of nutritious foods to youth and their families. J Acad Nutr Diet. 2012;112(6):897–901. doi: 10.1016/j.jand.2012.01.012. [DOI] [PubMed] [Google Scholar]
- 91.Milliron B-JM, Woolf KWP, Appelhans BMA. A point-of-purchase intervention featuring in-person supermarket education affects healthful food purchases. J Nutr Educ Behav. 2012;44(3):225–232. doi: 10.1016/j.jneb.2011.05.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Ayala GX, Baquero B, Laraia BA, Ji M, Linnan L. Efficacy of a store-based environmental change intervention compared with a delayed treatment control condition on store customers’ intake of fruits and vegetables. Public Health Nutr. 2013;16(11):1953–1960. doi: 10.1017/S1368980013000955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Geliebter A, Ang IYH, Bernales-Korins M, Hernandez D, Ochner CN, Ungredda T, Miller R, Kolbe L. Supermarket discounts of low-energy density foods: effects on purchasing, food intake, and body weight. Obesity. 2013;21(12):E542–E548. doi: 10.1002/oby.20484. [DOI] [PubMed] [Google Scholar]
- 94.Gittelsohn J, Kim EM, He S, Pardilla M. A food store–based environmental intervention is associated with reduced BMI and improved psychosocial factors and food-related behaviors on the Navajo Nation. J Nutr. 2013;143(9):1494–1500. doi: 10.3945/jn.112.165266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Sadler R, Gilliland J, Arku G. A food retail-based intervention on food security and consumption. IJERPH. 2013;10(8):3325–3346. doi: 10.3390/ijerph10083325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Bangia DB, Palmer-Keenan DMP-K. Grocery store podcast about omega-3 fatty acids influences shopping behaviors: a pilot study. J Nutr Educ Behav. 2014;46(6):616–620. doi: 10.1016/j.jneb.2014.06.007. [DOI] [PubMed] [Google Scholar]
- 97.Cawley J, Sweeney MJ, Sobal J, Just DR, Kaiser HM, Schulze WD, Wethington E, Wansink B. The impact of a supermarket nutrition rating system on purchases of nutritious and less nutritious foods. Public Health Nutr. 2014;18(1):8–14. doi: 10.1017/S1368980014001529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Cummins S, Flint E, Matthews SA. New neighborhood grocery store increased awareness of food access but did not alter dietary habits or obesity. Health Aff. 2014;33(2):283–291. doi: 10.1377/hlthaff.2013.0512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Foster GD, Karpyn A, Wojtanowski AC, Davis E, Weiss S, Brensinger C, Tierney A, Guo W, Brown J, Spross C, Leuchten D, Burns PJ, Glanz K. Placement and promotion strategies to increase sales of healthier products in supermarkets in low-income, ethnically diverse neighborhoods: a randomized controlled trial. Am J Clin Nutr. 2014;99(6):1359–1368. doi: 10.3945/ajcn.113.075572. [DOI] [PubMed] [Google Scholar]
- 100.Paek H-J, Oh HJ, Jung Y, et al. Assessment of a Healthy Corner Store Program (FIT Store) in low-income, urban, and ethnically diverse neighborhoods in Michigan. Family & Community Health 2014:1-14. doi:10.1097/FCH.0000000000000014. [DOI] [PubMed]
- 101.Dubowitz T, Ghosh-Dastidar M, Cohen DA, et al. Diet and perceptions change with supermarket introduction in a food desert, but not because of supermarket use. Health Aff. 2015;34(11):1158–1168. doi: 10.1377/hlthaff.2015.0667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Elbel B, Moran A, Dixon LB, Kiszko K, Cantor J, Abrams C, Mijanovich T. Assessment of a government-subsidized supermarket in a high-need area on household food availability and children’s dietary intakes. Public Health Nutr. 2015;18(15):2881–2890. doi: 10.1017/S1368980015000282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Nikolova HD, Inman JJ. Healthy choice: the effect of simplified point-of-sale nutritional information on consumer food choice behavior. J Mark Res. 2015;52(6):817–835. doi: 10.1509/jmr.13.0270. [DOI] [Google Scholar]
- 104.Payne CR, Niculescu M, Just DR, Kelly MP. Shopper marketing nutrition interventions: social norms on grocery carts increase produce spending without increasing shopper budgets. PMEDR. 2015;2(C):287–291. doi: 10.1016/j.pmedr.2015.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Taillie LS, Ng SW, Popkin BM. Gains made by Walmart’s Healthier Food Initiative mirror preexisting trends. Health Aff (Millwood) 2015;34(11):1869–1876. doi: 10.1377/hlthaff.2015.0072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Ortega AN, Albert SL, Chan-Golston AM, Langellier BA, Glik DC, Belin TR, Garcia RE, Brookmeyer R, Sharif MZ, Prelip ML. Substantial improvements not seen in health behaviors following corner store conversions in two Latino food swamps. BMC Public Health. 2016;16(1):1–10. doi: 10.1186/s12889-016-3074-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Payne CRP, Niculescu MN, Just DRJ, Kelly MPK. This way to produce: strategic use of arrows on grocery floors facilitate produce spending without increasing shopper budgets. J Nutr Educ Behav. 2016;48(7):512–513.e1. doi: 10.1016/j.jneb.2016.05.001. [DOI] [PubMed] [Google Scholar]
- 108.Schultz J, Litchfield R. Evaluation of traditional and technology-based grocery store nutrition education. Am J Health Educ. 2016;47(6):355–364. doi: 10.1080/19325037.2016.1219286. [DOI] [Google Scholar]
- 109.Surkan PJS, Tabrizi MJ, Lee RM, Palmer AM, Frick KD. Eat right-live well! Supermarket intervention impact on sales of healthy foods in a low-income neighborhood. J Nutr Educ Behav. 2016;48(2):112–121.e1. doi: 10.1016/j.jneb.2015.09.004. [DOI] [PubMed] [Google Scholar]
- 110.Adjoian T, Dannefer R, Willingham C, Brathwaite C, Franklin S. Healthy checkout lines: a study in urban supermarkets. J Nutr Educ Behav. 2017;49(8):615–622.e1. doi: 10.1016/j.jneb.2017.02.004. [DOI] [PubMed] [Google Scholar]
- 111.Albert SL, Langellier BA, Sharif MZ, Chan-Golston AM, Prelip ML, Elena Garcia R, Glik DC, Belin TR, Brookmeyer R, Ortega AN. A corner store intervention to improve access to fruits and vegetables in two Latino communities. Public Health Nutr. 2017;20(12):2249–2259. doi: 10.1017/S1368980017001008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Bangia DB, Shaffner DWS, Palmer-Keenan DMP-K. A point-of-purchase intervention using grocery store tour podcasts about omega-3 s increases long-term purchases of omega-3-rich food items. J Nutr Educ Behav. 2017;49(6):475–480.e1. doi: 10.1016/j.jneb.2017.02.008. [DOI] [PubMed] [Google Scholar]
- 113.Budd N, Jeffries JK, Jones-Smith J, Kharmats A, McDermott AY, Gittelsohn J. Store-directed price promotions and communications strategies improve healthier food supply and demand: impact results from a randomized controlled, Baltimore City store-intervention trial. Public Health Nutr. 2017;20(18):3349–3359. doi: 10.1017/S1368980017000064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Elbel B, Mijanovich T, Kiszko K, Abrams C, Cantor J, Dixon LB. The introduction of a supermarket via tax-credits in a low-income area: the influence on purchasing and consumption. Am J Health Promot. 2017;31(1):59–66. doi: 10.4278/ajhp.150217-QUAN-733. [DOI] [PubMed] [Google Scholar]
- 115.Gittelsohn J, Trude A, Poirier L, Ross A, Ruggiero C, Schwendler T, Anderson Steeves E. The impact of a multi-level multi-component childhood obesity prevention intervention on healthy food availability, sales, and purchasing in a low-income urban area. IJERPH. 2017;14(11):1371–1315. doi: 10.3390/ijerph14111371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Liu E, Stephenson T, Houlihan J, Gustafson A. Marketing strategies to encourage rural residents of high-obesity counties to buy fruits and vegetables in grocery stores. Prev Chronic Dis. 2017;14:170109–170106. doi: 10.5888/pcd14.170109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Rushakoff JA, Zoughbie DE, Bui N, DeVito K, Makarechi L, Kubo H. Evaluation of Healthy2Go: a country store transformation project to improve the food environment and consumer choices in Appalachian Kentucky. Prev Med Rep. 2017;7(C):187–192. doi: 10.1016/j.pmedr.2017.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Franckle RL, Levy DE, Macias-Navarro L, Rimm EB, Thorndike AN. Traffic-light labels and financial incentives to reduce sugar-sweetened beverage purchases by low-income Latino families: a randomized controlled trial. Public Health Nutr. 2018;21(8):1426–1434. doi: 10.1017/S1368980018000319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Jilcott Pitts SB, Wu Q, McGuirt J, Sharpe PA, Rafferty AP. Impact on dietary choices after discount supermarket opens in low-income community. J Nutr Educ Behav. 2018;50(7):729–735. doi: 10.1016/j.jneb.2018.03.002. [DOI] [PubMed] [Google Scholar]
- 120.Payne C, Niculescu M. Can healthy checkout end-caps improve targeted fruit and vegetable purchases? Evidence from grocery and SNAP participant purchases. Food Policy. 2018;79:318–323. doi: 10.1016/j.foodpol.2018.03.002. [DOI] [Google Scholar]
- 121.Polascek M, Moran A, Thorndike AN, et al. A supermarket double-dollar incentive program increases purchases of fresh fruits and vegetables among low-income families with children: the Healthy Double Study. J Nutr Educ Behav. 2018;50(3):217–228. doi: 10.1016/j.jneb.2017.09.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Rogus S, Athens J, Cantor J, Elbel B. Measuring micro-level effects of a new supermarket: do residents within 0.5 mile have improved dietary behaviors? J Acad Nutr Diet. 2018;118(6):1037–1046. doi: 10.1016/j.jand.2017.06.360. [DOI] [PubMed] [Google Scholar]
- 123.Freedman DA, Bell BA. Access to healthful foods among an urban food insecure population: perceptions versus reality. J Urban Health. 2009;86(6):825–838. doi: 10.1007/s11524-009-9408-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Cummins S, Clary C, Shareck M. Enduring challenges in estimating the effect of the food environment on obesity. Am J Clin Nutr. 2017;106(2):445–446. doi: 10.3945/ajcn.117.161547. [DOI] [PubMed] [Google Scholar]
- 125.Kirkpatrick SI, Reedy J, Butler EN, et al. Dietary assessment in food environment research: a systematic review. Am J Prev Med. 2014;46(1):94–102. doi: 10.1016/j.amepre.2013.08.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Mah CL, Cook B, Rideout K, Minaker LM. Policy options for healthier retail food environments in city-regions. Can J Public Health. 2016;107(Suppl 1):eS64–eS67. doi: 10.17269/cjph.107.5343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Mah CL, Hasdell R, Minaker LM, Soo S, Cook BE, Demaio AR. Entrepreneurialism and health-promoting retail food environments in Canadian city-regions. Health Promot Int. 2018;33(6):1055–1065. doi: 10.1093/heapro/dax049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Hawe P, Shiell A, Riley T. Complex interventions: how “out of control” can a randomised controlled trial be? BMJ. 2004;328(7455):1561–1563. doi: 10.1136/bmj.328.7455.1561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Hawe P, Shiell A, Riley T, Gold L. Methods for exploring implementation variation and local context within a cluster randomised community intervention trial. J Epidemiol Community Health. 2004;58(9):788–793. doi: 10.1136/jech.2003.014415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Ayala GX, D'Angelo H, Gittelsohn J, Horton L, Ribisl K, Sindberg LS, Olson C, Kharmats A, Laska MN. Who is behind the stocking of energy-dense foods and beverages in small stores? The importance of food and beverage distributors. Public Health Nutr. 2017;20(18):3333–3342. doi: 10.1017/S1368980016003621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Andreyeva T, Middleton AE, Long MW, Luedicke J, Schwartz MB. Food retailer practices, attitudes and beliefs about the supply of healthy foods. Public Health Nutr. 2011;14(06):1024–1031. doi: 10.1017/S1368980011000061. [DOI] [PubMed] [Google Scholar]
- 132.Caspi CE, Pelletier JE, Harnack L, Erickson DJ, Laska MN. Differences in healthy food supply and stocking practices between small grocery stores, gas-marts, pharmacies and dollar stores. Public Health Nutr. 2015;19(03):540–547. doi: 10.1017/S1368980015002724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Kim M, Budd N, Batorsky B, et al. Barriers to and facilitators of stocking healthy food options: viewpoints of Baltimore City small storeowners. Ecology of Food and Nutrition. 2016;56(1):17–30. doi: 10.1080/03670244.2016.1246361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Minaker LM, Olstad DL, MacKenzie G, et al. An evaluation of the impact of a restrictive retail food environment intervention in a rural community pharmacy setting. BMC Public Health. 2016;16:586. doi: 10.1186/s12889-016-3281-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Brimblecombe J, Ferguson M, McMahon E, Peeters A, Miles E, Wycherley T, Minaker LM, de Silva K, Greenacre L, Mah C. Reducing retail merchandising of discretionary food and beverages in remote indigenous community stores: protocol for a randomized controlled trial. JMIR Res Protoc. 2019;8(3):e12646–e12612. doi: 10.2196/12646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Milio N. Promoting Health Through Public Policy. Philadephia: FA Davis; 1981. [Google Scholar]
- 137.Milio N. Making healthy public policy; developing the science by learning the art: an ecological framework for policy studies. Health Promot Int. 1987;2(3):263–274. doi: 10.1093/heapro/2.3.263. [DOI] [PubMed] [Google Scholar]
- 138.Dunaway LF, Mundorf AR, Rose D. Fresh fruit and vegetable profitability: insights from a corner store intervention in New Orleans, Louisiana. Journal of Hunger & Environmental Nutrition. 2017;12(3):352–361. doi: 10.1080/19320248.2016.1227746. [DOI] [Google Scholar]
- 139.Dooris M. Healthy settings: challenges to generating evidence of effectiveness. Health Promot Int. 2005;21(1):55–65. doi: 10.1093/heapro/dai030. [DOI] [PubMed] [Google Scholar]
- 140.Poland B, Krupa G, McCall D. Settings for health promotion: an analytic framework to guide intervention design and implementation. Health Promot Pract. 2009;10(4):505–516. doi: 10.1177/1524839909341025. [DOI] [PubMed] [Google Scholar]
- 141.Peeters A, et al. Creating food retail environments for health. Medical Journal of Australia Insight + 2018, https://insightplus.mja.com.au/2018/34/creating-food-retail-environments-for-health/