Abstract
The iASSIST navigation system is a handheld accelerometer‐based navigation system that has been applied in clinical practice in recent five years. This meta‐analysis aimed to compare the radiographic and clinical outcomes of iASSIST navigation with conventional surgical techniques for patients undergoing total knee arthroplasty (TKA) and to compare the surgery time between an iASSIST group and a conventional treatment group. This systematic review and meta‐analysis included all comparative prospective and retrospective studies published in Pubmed, Embase, the Cochrane Central Register of Controlled Trials, the Web of Science and the CNKI databases over the past 20 years. Inclusion criteria were studies that compared the iASSIST navigation system with conventional TKA. The primary outcomes were mechanical axis (MA) and outliers, which means postoperative MA varus or valgus of more than 3°. Secondary outcomes were coronal femoral angle (CFA) and coronal tibial angle (CTA). Knee Society Score (KSS) was used to evaluate functional outcome. The Newcastle–Ottawa Scale (NOS) was used to assess the methodological quality of included studies. Eight studies involving 558 knees were included in this meta‐analysis. Of these, 275 patients used the iASSIST navigation system and 283 used conventional surgical techniques. A total of 5 studies were considered high quality and the other 3 were considered to be of moderate quality. The occurrence of malalignment of >3° in the iASSIST group was 13.3%, compared with 29.04% in the conventional group. Postoperative MA of the iASSIST group was significantly better than that of the conventional group (I 2 = 19%, OR = −0.92, 95% CI = −1.09 to −0.75, P < 0.00001). The iASSIST navigation system provided significantly increased accuracy in the coronal femoral angle (I 2 = 79%, OR = −0.88, 95% CI = −1.21 to −0.54, P < 0.00001) and the coronal tibial angle (I 2 = 34%, OR = 0.39, 95% CI = −0.48 to −0.30, P < 0.00001) compared with conventional techniques. However, the duration of surgery using the iASSIST procedure was longer and there was no significant difference in the short‐term KSS in the iASSIST group compared with the conventional group. We found that when pooling the data of included studies, the number of outliers was fewer in the iASSIST group, and compared with conventional TKA techniques, the iASSIST system significantly improved the accuracy of lower limb alignment but the duration of surgery was prolonged in addition to there being no apparent advantage in terms of short‐term functional score.
Keywords: Handheld navigation, Portable navigation, Surgical technique, Systematic review, Total knee arthroplasty
Introduction
As the incidence of knee osteoarthritis continues to increase, the number of patients requiring total knee arthroplasty (TKA) has risen1. TKA is regarded as an effective treatment for end‐stage osteoarthritis and rheumatic arthritis2. However, 20% of patients who undergo TKA are not satisfied with the results3, 4. The success of surgery depends on many factors, including soft tissue balancing, design of prostheses, and medical complications. Furthermore, surgical factors are critically important, such as the skill and experience of the surgeon, the precision of prosthesis implantation, and the duration of surgery.
Incorrect positioning of the prosthesis may result in unacceptable tibiofemoral tracking that could bring about additional stress at the loaded surfaces of the prosthesis leading to accelerated wear and component loosening5. Jeffery et al.6 suggest that aseptic loosening of implants in patients with alignment exceeding 3° of varus or valgus occurs at a rate of 24% compared with a rate of only 3% in patients whose alignment is within 3° of the neutral mechanical axis (MA). Malalignment may also increase wear on polyethylene tibial bearings7. Several studies have shown that postoperative MA of less than 3° may reduce the risk of future TKA failure8, 9, 10, 11, 12, 13. Thus, outliers of MA were defined as being outside a 3° divergence from the MA14.
An intramedullary guide is used for distal femoral resection and an extramedullary or intramedullary jig for tibial resection in conventional TKA surgery. This technique relies heavily on bone markers and the surgeonʼs experience, which have limited accuracy in terms of MA reconstruction and prosthesis implantation. Because of the relative stability of the osseous anatomy, computer‐assisted surgery (CAS) was introduced 30 years ago to aid surgeons in reducing surgical errors and ensuring precise prosthesis implantation15. In addition, CAS has been shown to improve the accuracy of prosthesis implantation and reduce the proportion of outliers for lower limb MA compared to conventional TKA16. The major shortcomings of CAS are a complicated registration process17, a steep learning curve, pin‐site‐related complications, and periprosthetic fractures of the tibia and femur18. However, a number of researchers argue that better lower limb alignment does not lead to better functional outcome19.
To avoid the shortcomings of CAS, navigation devices have been developed that use accelerometer‐based electronic components20, 21. They combine the alignment accuracy of CAS systems with the familiarity of conventional techniques while avoiding the preoperative imaging and large computer console required for registration and alignment feedback in the process of operating CAS22. The utility of the technique remains controversial, and its cost effectiveness remains unclear.
The iASSIST (Zimmer, Warsaw, IN, US) navigation device is a handheld computer‐assisted accelerometer‐based stereotaxic system that simplifies the registration process23. The iASSIST system is validated in cadavers and clinical studies by Scuderi et al.24, who use this unique technique to resolve issues of lower limb alignment reconstruction. To reduce operational complexity, the accelerometer, gyroscope, and wireless communication system are integrated into a small pod which attaches to the femoral and tibial resection jigs. After several simple registration steps, the pods display alignment information for the surgical field without altering the surgical steps, guiding femoral and tibial resection and providing the surgeon with the opportunity to verify bone resection steps and make further adjustments as necessary.
In the past 3 years, studies on the iASSIST system have gradually increased in number, with some researchers believing that it may improve the accuracy of lower limb alignment25, 26, 27, 28, 29, 30, although some have found no significant difference between the iASSIST and conventional techniques22, 23. The purpose of this meta‐analysis is to determine whether the iASSIST navigation system contributes to more accurate lower limb alignment, improving postoperative functional outcome, compared with conventional surgical techniques.
Materials and Methods
Study Selection
We conducted a comprehensive electronic search, in PubMed, Embase, Cochrane Central Register of Controlled Trials, Web of Science and CNKI databases, of literature published between 1 January 2000 and 1 October 2018, using the following terms: “iASSIST”, “Zimmer iASSIST”, “TKA”, and “MA.” This study was based on the Cochrane Review Methods, and reporting was carried out according to the Preferred Reporting Items for Systematic Reviews and Meta‐analyses (PRISMA). The review protocol has been registered in the International Prospective register of systematic reviews [CRD42019128880].
Both Chinese and English publications were included. Relevant studies were identified by reading the titles and abstracts of the manuscripts. If it was considered that the primary selection had yielded insufficient information, the full text was checked to confirm whether or not to include the article. Any disagreement was solved by discussion.
Eligibility Criteria
Studies were included if the following inclusion criteria were met:
The experimental group used iASSIST navigation in primary TKA.
The control group consisted of conventional primary TKA.
At least one outcome in our meta‐analysis was reported.
No infections were reported during the period of observation.
The studies were randomized controlled trials (RCT) or prospective and retrospective nonrandomized controlled trials (nRCT).
A study was excluded if any of the following applied:
It duplicated data from a study that was already included.
It did not stratify analysis between primary and revision TKA.
It was a systematic review.
Study Quality Assessment
All studies that were identified as satisfying these criteria were included in this meta‐analysis and independently evaluated by two reviewers. As recommended by the Cochrane Handbook for Systematic Reviews of Interventions, the Newcastle–Ottawa Scale (NOS; using the range 0–9)31 was used to assess studies that were included. The NOS evaluates the risk of bias for each study using three criteria: (i) selection of the exposed and unexposed study populations; (ii) comparability; and (iii) outcome measures. The maximum scores for these three factors are 4 stars, 2 stars, and 3 stars, respectively. Studies with a total score ≥7 were considered high quality; those scoring 6 were considered moderate quality and those that scored less than 6 stars were considered low quality. Any disagreements in the bias assessment were resolved by discussion.
Data Extraction
Two reviewers independently extracted data from each study included in the review. Extracted data comprised: first authorʼs name, publication year, study type, sample size, duration of follow up, measured parameters, and the NOS score. Patient information extracted from the studies included: age, gender, and body mass index (BMI). Primary outcomes were postoperative MA angle, having an ideal value of 0°, and outliers from the MA. The coronal angle of the femoral (CFA) or tibial component (CTA) in relation to the MA were regarded as secondary radiographic outcomes, with an ideal value of 90°. Duration of surgery was collected as a tertiary outcome. Knee Society Score (KSS) was used to assess short‐term clinical outcome. Data were extracted independently by two reviewers, with discrepancies in the extracted data resolved by discussion.
Statistical Methods
This meta‐analysis was performed using Cochrane Collaboration Review Manager 5.3 software. The mean difference (MD) and its corresponding 95% confidence interval (CI) for each measure were calculated for continuous measures; namely, the angles measured in each study. The odds ratio (OR) and its corresponding 95% CI were calculated for dichotomous measures, “yes” or “no” being the sole options. Heterogeneity was assessed using the I 2 statistic, the proportion of variation across studies occurring not as a result of chance. Significant heterogeneity was established for I 2 values >50% and P < 0.05. A fixed‐effects model was used for outcome data without significant heterogeneity; for those with significant heterogeneity, a random‐effects model was used. Values of P < 0.05 were considered statistically significant. In addition, where heterogeneity was significant, a sensitivity analysis was conducted by omitting studies individually in turn.
Results
Search
Figure 1 is a flow chart of the included and excluded studies. A total of 114 articles were identified for the meta‐analysis. Of these, 96 studies were duplications and 68 studies were excluded because the titles or abstracts did not meet the eligibility criteria. After reading full texts, 19 studies were excluded according to eligibility criteria. Finally, 8 studies were included in this review22, 23, 25, 26, 27, 28, 29, 30, of which 6 studies were in English and 2 in Chinese language.
Figure 1.
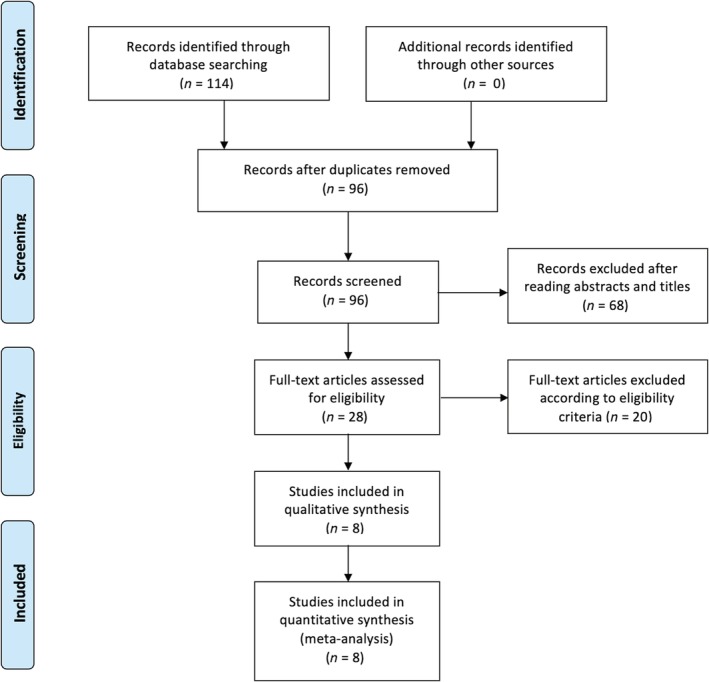
Flow chart.
Characteristics
The characteristics of each study included in this review are outlined in Table 1. A total of 5 RCT and 3 retrospective studies reported a total of 558 knee cases, of which 275 patients used the iASSIST navigation system and 283 underwent conventional surgery. All these studies used iASSIST navigation as navigation devices; 7 studies performed standard invasive TKA and 1 study conducted minimally invasive TKA. The average age of patients from the iASSIST and conventional groups was 66.5 and 66.4, respectively. The average BMI of patients from both groups was 27.1 and 27.0, respectively. The percentage of female patients from both groups was 70.2% and 71.7%, respectively. There were no significant differences between these two groups in terms of age, BMI, and gender. Of these, 8 studies evaluating mechanical alignment, the occurrence of malalignment (13.3%) in the conventional group was better than that (29.04%) in the iASSIST group in 3 studies, but no differences between these two groups in the other 5 studies were observed. Moreover, 3 articles reported that there were no significant differences in postoperative blood loss‐related indicators between these two groups; 2 articles reported that there was no significant difference in postoperative patient satisfaction between these two groups. All original data have been uploaded to the Open Science Framework (osf.io).
Table 1.
Characteristics of included studies
| Author | Year | Study design | iASSIST | CONV | Follow up | Results | P‐value | ||
|---|---|---|---|---|---|---|---|---|---|
| iASSIST | CONV | ||||||||
| Satit et al. | 2016 |
Mechanical axis (MA), Placement of components Surgical time |
40 | 40 | 6 weeks postoperative |
MA (°) MA outliers CFA (°) CTA (°) Surgical time (min) |
180.8 ± 2.1 3 90.3 ± 1.0 90.5 ± 1.8 96 ± 14.2 |
179.9 ± 3.2 10 90.7 ± 2.2 89.3 ± 1.9 94 ± 18.7 |
0.141 0.031 0.303 0.005 0.65 |
|
Tian et al. |
2017 |
MA, Placement of components KSS, VAS, surgical time |
20 | 20 | Immediate for radiological, 1 month for KSS and VAS |
MA shifting (°) CFA shifting (°) CTA shifting (°) Surgical time (min) KSS |
1.1 ± 1.1 0.9 ± 0.7 1.2 ± 0.9 80.9 ± 7.8 77.1 ± 8.6 |
2.9 ± 2.8 2.4 ± 0.9 2.2 ± 1.6 73.1 ± 9.1 70.2 ± 8.1 |
0.01 <0.01 <0.01 <0.01 <0.05 |
| Wei et al. | 2018 |
MA, Placement of components KSS, Hb loss, surgical time |
12 | 12 | 3 months postoperative for radiological and KSS |
MA shifting (°) CFA shifting (°) CTA shifting (°) Surgical time (min) KSS Hb loss (g/L) |
1.2 ± 0.45 0.86 ± 0.19 1.06 ± 0.26 67.4 ± 4.99 85.83 ± 4.3 10.42 ± 2.02 |
2.33 ± 0.62 2.01 ± 0.47 1.326 ± 0.23 63.3 ± 5.01 80.08 ± 5.18 19.08 ± 2.778 |
0.001 0.001 0.016 0.058 0.007 0.001 |
| Denti et al. |
2018 |
MA Tibial slope Range of motion Occasional pain |
10 | 10 | Immediate for radiological, 1 year for range of motion and occasional pain |
MA shifting (°) Tibial slope (°) Full ROM Occasional pain |
2.44 ± 2.01 1.94 ± 1.50 9 1 |
2.03 ± 1.15 3.04 ± 2.00 8 1 |
>0.05 >0.05 >0.05 >0.05 |
| Kinney et al. |
2018 |
MA, placement of components tourniquet time |
25 | 25 | 1 and 4 months postoperative |
MA shifting (°) CFA shifting (°) CTA shifting (°) Tourniquet time (min) |
1.92 ± 0.34 1.65 ± 0.17 1.28 ± 0.13 113.6 ± 2.5 |
2.83 ± 0.41 2.23 ± 0.33 1.71 ± 0.24 114.3 ± 3.2 |
0.09 0.12 0.12 0.86 |
| Liow et al. | 2016 | MA, placement of component, KSS, OKS, SF‐36 | 92 | 100 | 1 months for radiological; 6 months for KSS, OKS, and SF‐36 |
MA shifting (°) MA outliers CFA shifting (°) CTA shifting (°) KSS Surgical time (min) |
1.9 ± 1.4 8.7 1.6 ± 1.3 1.6 ± 1.2 71.7 ± 16.6 83.9 ± 21.8 |
2.8 ± 2.0 26 2.1 ± 1.5 2.1 ± 1.5 69.9 ± 16.4 72.5 ± 14.6 |
0.001 0.001 0.024 0.024 0.110 <0.001 |
| Moo et al. | 2018 | MA, placement of component, surgical time | 30 | 30 | Immediate postoperative |
MA (°) MA outliers (%) CFA (°) CTA (°) Surgical time (min) |
176.75 ± 0.75 43 91.75 ± 0.75 91.25 ± 0.75 96.25 ± 6.25 |
176.75 ± 0.75 36 92 ± 0.5 90 ± 0.5 90.62 ± 4.37 |
0.332 0.384 0.453 0.28 0.13 |
| Lo et al. | 2018 | MA, placement of component, surgical time | 46 | 46 | 6 months postoperative |
MA shifting (°) MA outliers CFA shifting (°) CTA shifting (°) Surgical time (min) |
0.19 ± 2.06 3 0.37 ± 1.36 0.24 ± 1.43 96 ± 14.2 |
0.69 ± 3.18 10 0.90 ± 2.21 0.25 ± 2.62 94 ± 18.7 |
0.372 0.045 0.172 0.972 0.613 |
The lower extremity mechanical axis (MA) is the angle formed by the MA of the femur (line between the center of the femoral head and the center of the knee) and the MA of the tibia (line between the center of the talus and the center of the knee or hip‐knee‐ankle angle); the coronal femoral‐component angle (CFA) is the angle formed by the femoral component and the MA of the femur; coronal tibia‐component angle (CTA) is the angle formed by the tibia base plate and the MA of the tibia; the accepted values used in study for normal alignment were: 3° varus/valgus for MA,the outlier were defined as cases in which the alignment error was >3° from the accepted values; KSS, Knee Society Score; VAS, visual analogue scale.
Quality
The methodological quality of each included study was assessed in accordance with the NOS. The NOS score of included studies ranged from 6 to 9, with an average score of 7.12. A total of 5 studies were high quality23, 25, 27, 29, 30, and the other 3 were moderate quality studies22, 26, 28.
Mechanical axis
5 studies provided MA outlier data, which indicated that there was a significant difference between the iASSIST and conventional groups (P = 0.009), with iASSIST reducing the proportion of such outliers (Fig. 2). The value of I 2 was >50%, signifying significant heterogeneity. The omission of 1 study22 changed the value of I 2 to 19%, suggesting that this article was the source of heterogeneity (Fig. 3).
Figure 2.
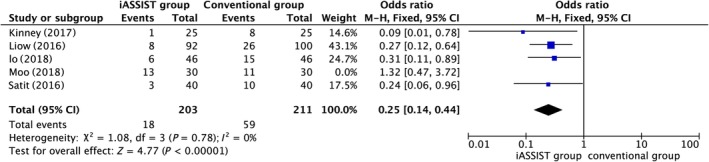
Postoperative mechanical axis (MA) outliers.
Figure 3.
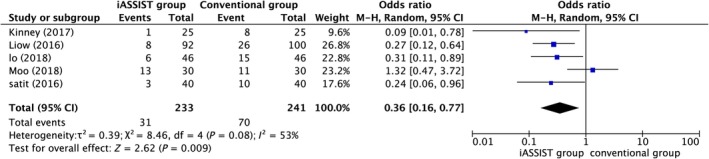
After omission of postoperative mechanical axis (MA) outliers.
Six studies provided data on MA, analysis of which demonstrated that highly significant differences were found between the iASSIST and conventional groups (P < 0.00001), indicating that iASSIST can significantly improve the accuracy of lower limb alignment compared to conventional treatment (Fig. 4).
Figure 4.
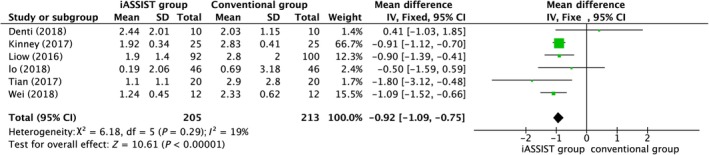
Postoperative mechanical axis (MA).
Coronal Prothesis Angle
Five articles measured the coronal femoral angle (CFA) and the coronal tibial angle (CTA). The meta‐analysis indicated that for both CFA and CTA, the iASSIST group was significantly different from the conventional group (P < 0.00001), indicating that iASSIST improved the accuracy of prosthesis placement of both components in the coronal plane (Figs. 5 and 6). However, with I 2 = 79%, the heterogeneity was considered significant for CFA. This value did not change greatly as articles were omitted in turn; thus, this result can be regarded as stable.
Figure 5.
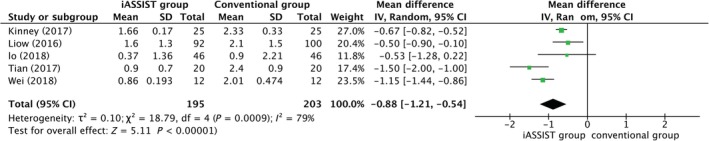
Postoperative coronal femoral angle (CFA).
Figure 6.
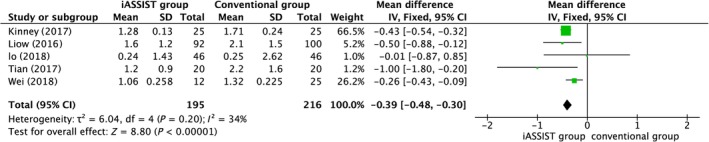
Postoperative coronal tibial angle (CTA).
Operation Time
Seven articles discussed duration of surgery. The mean duration of procedures using iASSIST compared to conventional surgery was 90.24 min versus 85.01 min, indicating that iASSIST was a significantly longer process (Fig. 7).
Figure 7.
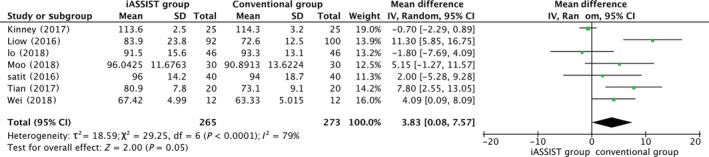
Duration of surgery.
Clinical Outcome
Postoperative KSS, a short‐term outcome measure, was featured in only 3 articles. The meta‐analysis indicated that there was no significant difference between iASSIST and conventional surgery in this regard (P = 0.86) (Fig. 8). Heterogeneity was significant. Omission of Liowʼs article27 resulted in the I 2 value falling to 0%, suggesting that this article was the source of heterogeneity (Fig. 9).
Figure 8.
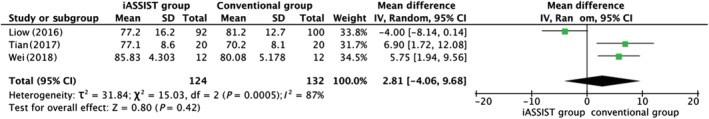
Postoperative Knee Society Score (KSS).
Figure 9.
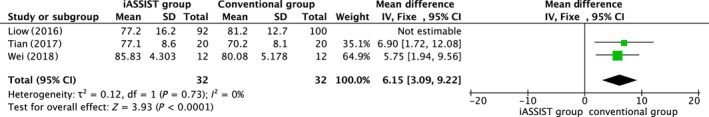
After omission of postoperative Knee Society Score (KSS).
Discussion
Total knee arthroplasty has proven to be a successful procedure, with approximately 250,000 operations performed in China annually, although TKA is not as satisfactory as total hip arthroplasty (THA). Approximately 20% of patients who have undergone TKA have been dissatisfied with their surgery, believed to be because of the surgeonʼs surgical technique. Conventional surgery relies on an intra‐medullary guiding system for cutting bones. Some factors may influence the application of such a system, including varus or valgus deformity, obesity, or a narrow canal. In addition, intra‐marrow penetration will lead to increased bleeding, leading to decreased hemoglobin levels and an increased risk of requiring blood transfusion. Clinicians have considered, therefore, various approaches to achieve a more satisfactory outcome, such as CAS or patient‐matched instrumentation (PMI). Previous studies found that CAS decreased the risk of malalignment to achieve superior short‐term functional outcome32. CAS has numerous limitations, such as complex landmark registration, pin complications, a steep learning curve, increased duration of surgery, and questionable cost effectiveness21, 33, 34, 35. PMI is an additional technique that assists surgeons in achieving improved lower limb alignment, but a 3D CT scan is required before surgery, and once osteotomy has been performed, the correction in alignment cannot be verified36. Conversely, the iASSIST system can verify alignment after osteotomy to ensure its accuracy. The authors of a recent study also noted that PMI was not able to reduce the number of outliers37. The iASSIST guidance system allows simple registration and displays alignment information for the surgical field without altering the actual surgical steps, thereby avoiding a number of pertinent complications caused by additional pinning, such as pin tract infections and pain. Therefore, the iASSIST system appears to circumvent the shortcomings of CAS and provides a more convenient and quicker surgical procedure27.
Results from this meta‐analysis indicate that the iASSIST navigation system offers a significant improvement in both MA and coronal prosthesis implantation compared with conventional techniques (P < 0.0001). Other articles comparing accelerator‐based navigation devices have come to similar conclusions, that such devices can improve the accuracy of lower limb alignment and, therefore, prosthesis implantation38, 39, 40. This meta‐analysis found that 89.1% of iASSIST surgeries, compared with 70.96% of conventional treatments, were within 3° of neutral MA, establishing that the iASSIST guidance system provides more accurate prosthesis implantation, which will reduce the risk of prosthesis loosening and early failure of TKA. We found that the studies from China all had positive results, probably because the Chinese patients had a smaller BMI, which results in fewer problems in surgery than in Western countries. However, due to the time required to register and install the navigation components, the duration of surgery of the iASSIST group was greater than conventional surgery. Contrary to some previous studies using CAS, there was no significant difference between the iASSIST system and conventional surgery in short‐term KSS. This may be due to the fact that the iASSIST system does not alter the actual surgical procedure used in conventional TKA to any significant degree as the principle is to provide accurate alignment information during surgery; studies that have much longer‐term follow up are required to establish its benefits.
Although we have presented here a high‐quality review of the iASSIST guidance system and compared it with conventional surgery, there are several limitations to the study. First, significant heterogeneity was observed, possibly because of differences in skill and experience of the various surgeons, different cutting guides in the conventional procedure, and the diversity of characteristics of patients from different countries and study type. In this article, 5 prospective RCT and 3 retrospective studies were included. There are currently 2 RCT underway that compare iASSIST with conventional surgical techniques. In general, conclusions are more convincing if only RCT are selected for a meta‐analysis, but the current state of the published literature suggests that to do so would result in too small a sample size to draw conclusions. In the future, a meta‐analysis including only RCT will provide additional evidence to guide clinical treatment, if necessary. Only coronal prosthesis angles were considered as the outcome measure, with no sagittal prosthesis angles included due to insufficient data. In addition, various studies have different follow‐up times, which may result in inconsistencies in the calculation of KSS. Measurement standards may vary from study to study, with errors in the recorded measurements. Thus, as a result of insufficient data, we were unable to analyze the complication rates, prothesis survival, and long‐term functional outcomes.
Unlike earlier research, recent studies have shown that a reduction in the numbers of MA outliers due to the use of CAS does not lead to better functional outcomes41, 42. Even the connection between MA and prosthesis survival may be overstated. Despite this debate, a neutral MA remains the “gold standard” for target alignment, supported by considerable quantities of data43. Therefore, more long‐term follow‐up studies are required to demonstrate the relationship between better postoperative lower limb alignment with postoperative functional outcome and prosthesis survival. However, high BMI and severe varus and valgus deformity may increase the deviation of lower limb alignment and the number of MA outliers5, 44, 45. Hence, subgroup meta‐analysis will be required to clarify the clinical significance of the iASSIST system when more detailed relevant literature becomes available.
In conclusion, the present systematic review and meta‐analysis demonstrates the superiority of the iASSIST navigation system, establishing that it provides improved alignment in lower limb reconstruction. However, the duration of surgery when using the iASSIST system is longer than for conventional techniques. Superior radiographic results are not associated with enhanced short‐term functional outcomes.
Acknowledgements
The authors of the original articles are gratefully acknowledged, as their articles facilitated this systematic review and meta‐analysis. In addition, we would like to thank all our coworkers from the First Hospital of China Medical Universities. The authors of this article did not accept funding from any organization.
Disclosure: The authors declare that they have no conflict of interest.
References
- 1. Kurtz SM, Lau E, Ong K, Zhao K, Kelly M, Bozic KJ. Future young patient demand for primary and revision joint replacement: national projections from 2010 to 2030. Clin Orthop Relat Res, 2009, 467: 2606–2612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Callahan CM, Drake BG, Heck DA, Dittus RS. Patient outcomes following tricompartmental total knee replacement. A meta‐analysis. JAMA, 1994, 271: 1349–1357. [PubMed] [Google Scholar]
- 3. Bourne RB, Chesworth BM, Davis AM, Mahomed NN, Charron KD. Patient satisfaction after total knee arthroplasty: who is satisfied and who is not?. Clin Orthop Relat Res, 2010, 468: 57–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Dossett HG, Swartz GJ, Estrada NA, LeFevre GW, Kwasman BG. Kinematically versus mechanically aligned total knee arthroplasty. Orthopedics, 2012, 35: e160–e169. [DOI] [PubMed] [Google Scholar]
- 5. Ritter MA, Davis KE, Meding JB, Pierson JL, Berend ME, Malinzak RA. The effect of alignment and BMI on failure of total knee replacement. J Bone Joint Surg Am, 2011, 93: 1588–1596. [DOI] [PubMed] [Google Scholar]
- 6. Jeffery RS, Morris RW, Denham RA. Coronal alignment after total knee replacement. J Bone Joint Surg Br, 1991, 73: 709–714. [DOI] [PubMed] [Google Scholar]
- 7. Collier MB, Engh CA Jr, McAuley JP, Engh GA. Factors associated with the loss of thickness of polyethylene tibial bearings after knee arthroplasty. J Bone Joint Surg Am, 2007, 89: 1306–1314. [DOI] [PubMed] [Google Scholar]
- 8. Bonutti PM, Dethmers D, Ulrich SD, Seyler TM, Mont MA. Computer navigation‐assisted versus minimally invasive TKA: benefits and drawbacks. Clin Orthop Relat Res, 2008, 466: 2756–2762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Ensini A, Catani F, Leardini A, Romagnoli M, Giannini S. Alignments and clinical results in conventional and navigated total knee arthroplasty. Clin Orthop Relat Res, 2007, 457: 156–162. [DOI] [PubMed] [Google Scholar]
- 10. Sikorski JM. Alignment in total knee replacement. J Bone Joint Surg Br, 2008, 90: 1121–1127. [DOI] [PubMed] [Google Scholar]
- 11. Kim YH, Park JW, Kim JS. Computer‐navigated versus conventional total knee arthroplasty a prospective randomized trial. J Bone Joint Surg Am, 2012, 94: 2017–2024. [DOI] [PubMed] [Google Scholar]
- 12. Fang DM, Ritter MA, Davis KE. Coronal alignment in total knee arthroplasty: just how important is it?. J Arthroplasty, 2009, 24: 39–43. [DOI] [PubMed] [Google Scholar]
- 13. Berend ME, Ritter MA, Meding JB, et al Tibial component failure mechanisms in total knee arthroplasty. Clin Orthop Relat Res, 2004, 428: 26–34. [DOI] [PubMed] [Google Scholar]
- 14. Abdel MP, Oussedik S, Parratte S, Lustig S, Haddad FS. Coronal alignment in total knee replacement: historical review, contemporary analysis, and future direction. Bone Joint J, 2014, 96: 857–862. [DOI] [PubMed] [Google Scholar]
- 15. Delp SL, Stulberg SD, Davies B, Picard F, Leitner F. Computer assisted knee replacement. Clin Orthop Relat Res, 1998, 354: 49–56. [DOI] [PubMed] [Google Scholar]
- 16. Rebal BA, Babatunde OM, Lee JH, Geller JA, Patrick DA Jr, Macaulay W. Imageless computer navigation in total knee arthroplasty provides superior short term functional outcomes: a meta‐analysis. J Arthroplasty, 2014, 29: 938–944. [DOI] [PubMed] [Google Scholar]
- 17. Bauwens K, Matthes G, Wich M, et al Navigated total knee replacement. A meta‐analysis. J Bone Joint Surg Am, 2007, 89: 261–269. [DOI] [PubMed] [Google Scholar]
- 18. Jung HJ, Jung YB, Song KS, Park SJ, Lee JS. Fractures associated with computer‐navigated total knee arthroplasty. A report of two cases. J Bone Joint Surg Am, 2007, 89: 2280–2284. [DOI] [PubMed] [Google Scholar]
- 19. Bonner TJ, Eardley WG, Patterson P, Gregg PJ. The effect of post‐operative mechanical axis alignment on the survival of primary total knee replacements after a follow‐up of 15 years. J Bone Joint Surg Br, 2011, 93: 1217–1222. [DOI] [PubMed] [Google Scholar]
- 20. Nam D, Cody EA, Nguyen JT, Figgie MP, Mayman DJ. Extramedullary guides versus portable, accelerometer‐based navigation for tibial alignment in total knee arthroplasty: a randomized, controlled trial: winner of the 2013 HAP PAUL award. J Arthroplasty, 2014, 29: 288–294. [DOI] [PubMed] [Google Scholar]
- 21. Nam D, Weeks KD, Reinhardt KR, Nawabi DH, Cross MB, Mayman DJ. Accelerometer‐based, portable navigation vs imageless, large‐console computer‐assisted navigation in total knee arthroplasty: a comparison of radiographic results. J Arthroplasty, 2013, 28: 255–261. [DOI] [PubMed] [Google Scholar]
- 22. Moo IH, Chen JYQ, Chau DHH, Tan SW, Lau ACK, Teo YS. Similar radiological results with accelerometer‐based navigation versus conventional technique in total knee arthroplasty. J Orthop Surg (Hong Kong), 2018, 26: 2309499018772374. [DOI] [PubMed] [Google Scholar]
- 23. Denti M, Soldati F, Bartolucci F, Morenghi E, De Girolamo L, Randelli P. Conventional versus smart wireless navigation in total knee replacement: similar outcomes in a randomized prospective study. Joints, 2018, 6: 90–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Scuderi GR, Fallaha M, Masse V, Lavigne P, Amiot LP, Berthiaume MJ. Total knee arthroplasty with a novel navigation system within the surgical field. Orthop Clin North Am, 2014, 45: 167–173. [DOI] [PubMed] [Google Scholar]
- 25. Kinney MC, Cidambi KR, Severns DL, Gonzales FB. Comparison of the iAssist handheld guidance system to conventional instruments for mechanical axis restoration in total knee arthroplasty. J Arthroplasty, 2018, 33: 61–66. [DOI] [PubMed] [Google Scholar]
- 26. Lo CK, Li HY, Wong YC, Wai YL. Total knee replacement with iASSIST navigation system. J Orthop Trauma Rehabil, 2018, 24: 29–33. [Google Scholar]
- 27. Liow MH, Goh GS, Pang HN, Tay DK, Lo NN, Yeo SJ. Computer‐assisted stereotaxic navigation improves the accuracy of mechanical alignment and component positioning in total knee arthroplasty. Arch Orthop Trauma Surg, 2016, 136: 1173–1180. [DOI] [PubMed] [Google Scholar]
- 28. Shuchang T, Qingqiang Y, Shuai L, et al Clinical application of iASSIST navigaiton system assisted total knee arthroplasty in the treatment of osteoarthritis. China Digital Med, 2017, 12: 26–34. [Google Scholar]
- 29. Wei H, Yang SH, Liu XZ. Application of computer‐assisted navigation (iASSIST technology) in total knee arthroplasty. Chin J Bone Jt, 2018, 7: 245–250. [Google Scholar]
- 30. Thiengwittayaporn S, Fusakul Y, Kangkano N, Jarupongprapa C, Charoenphandhu N. Hand‐held navigation may improve accuracy in minimally invasive total knee arthroplasty: a prospective randomized controlled trial. Int Orthop, 2016, 40: 51–57. [DOI] [PubMed] [Google Scholar]
- 31. Stang A. Critical evaluation of the Newcastle‐Ottawa scale for the assessment of the quality of nonrandomized studies in meta‐analyses. Eur J Epidemiol, 2010, 25: 603–605. [DOI] [PubMed] [Google Scholar]
- 32. Mason JB, Fehring TK, Estok R, Banel D, Fahrbach K. Meta‐analysis of alignment outcomes in computer‐assisted total knee arthroplasty surgery. J Arthroplasty, 2007, 22: 1097–1106. [DOI] [PubMed] [Google Scholar]
- 33. Blakeney WG, Khan RJ, Wall SJ. Computer‐assisted techniques versus conventional guides for component alignment in total knee arthroplasty: a randomized controlled trial. J Bone Joint Surg Am, 2011, 93: 1377–1384. [DOI] [PubMed] [Google Scholar]
- 34. Brin YS, Nikolaou VS, Joseph L, Zukor DJ, Antoniou J. Imageless computer assisted versus conventional total knee replacement. A Bayesian meta‐analysis of 23 comparative studies. Int Orthop, 2011, 35: 331–339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Zhang GQ, Chen JY, Chai W, Liu M, Wang Y. Comparison between computer‐assisted‐navigation and conventional total knee arthroplasties in patients undergoing simultaneous bilateral procedures: a randomized clinical trial. J Bone Joint Surg Am, 2011, 93: 1190–1196. [DOI] [PubMed] [Google Scholar]
- 36. Pourgiezis N, Reddy SP, Nankivell M, Morrison G, VanEssen J. Alignment and component position after patient‐matched instrumentation versus conventional total knee arthroplasty. J Orthop Surg (Hong Kong), 2016, 24: 170–174. [DOI] [PubMed] [Google Scholar]
- 37. Mannan A, Smith TO, Sagar C, London NJ, Molitor PJ. No demonstrable benefit for coronal alignment outcomes in PSI knee arthroplasty: a systematic review and meta‐analysis. Orthop Traumatol Surg Res, 2015, 101: 461–468. [DOI] [PubMed] [Google Scholar]
- 38. Bugbee WD, Kermanshahi AY, Munro MM, McCauley JC, Copp SN. Accuracy of a hand‐held surgical navigation system for tibial resection in total knee arthroplasty. Knee, 2014, 21: 1225–1228. [DOI] [PubMed] [Google Scholar]
- 39. Iorio R, Mazza D, Drogo P, et al Clinical and radiographic outcomes of an accelerometer‐based system for the tibial resection in total knee arthroplasty. Int Orthop, 2015, 39: 461–466. [DOI] [PubMed] [Google Scholar]
- 40. Wada K, Mikami H, Hamada D, Yonezu H, Oba K, Sairyo K. Measurement of rotational and coronal alignment in total knee arthroplasty using a navigation system is reproducible. Arch Orthop Trauma Surg, 2016, 136: 271–276. [DOI] [PubMed] [Google Scholar]
- 41. d'Amato M, Ensini A, Leardini A, Barbadoro P, Illuminati A, Belvedere C. Conventional versus computer‐assisted surgery in total knee arthroplasty: comparison at ten years follow‐up. Int Orthop, 2019, 43: 1355–1363. [DOI] [PubMed] [Google Scholar]
- 42. Goh GS, Liow MHL, Tay DK, Lo NN, Yeo SJ, Tan MH. Accelerometer‐based and computer‐assisted navigation in total knee arthroplasty: a reduction in mechanical axis outliers does not lead to improvement in functional outcomes or quality of life when compared to conventional total knee arthroplasty. J Arthroplasty, 2018, 33: 379–385. [DOI] [PubMed] [Google Scholar]
- 43. Donaldson J, Joyner J, Tudor F. Current controversies of alignment in total knee replacements. Open Orthop J, 2015, 9: 489–494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Tian F, Zang XH, Sun YS. Impact of knee varus and valgus deformity on alignment in lower extremities after total knee arthroplasty (TKA). Eur Rev Med Pharmacol Sci, 2018, 22: 83–89. [DOI] [PubMed] [Google Scholar]
- 45. Toivanen AT, Heliovaara M, Impivaara O, et al Obesity, physically demanding work and traumatic knee injury are major risk factors for knee osteoarthritis–a population‐based study with a follow‐up of 22 years. Rheumatology (Oxford), 2010, 49: 308–314. [DOI] [PubMed] [Google Scholar]


