Abstract
Objective
Investigation of the treatment of femur fractures and the type of femur fracture‐associated complications regarding timing of surgery and length of hospital stay.
Methods
In this retrospective cohort study, a total of 358 hip fractures were evaluated retrospectively from 1 January 2008 until 31 December 2010 at a level I trauma center in Germany. Inclusion criteria was age >18 years and a proximal femur fracture. Both sexes were evaluated. Mean age was 75.5 years, most patients were female (63.7%). Intervention was the operative treatment of proximal femur fracture. Outcome parameters were time until surgery, complications, reoperations, mortality, and length of hospital stay.
Results
Among the proximal femur fractures (n = 358), 46.6% were pertrochanteric, 11.2% subtrochanteric, and 42.2% femoral neck fractures. Operation upon hip fractures was managed regularly within 24 hours of injury (73%; mean for femoral neck: 28.3 hrs.; mean for pertrochanteric fractures: 21.4 hrs.; mean for subtrochanteric fractures: 19.5 hrs.). Delayed treatment, as well as implantation of hip total endoprosthesis (TEP), increased the overall length of hospital stay (15.4 vs 17.6 days; 18.1 vs 15.8 days). Accordingly, surgical procedures performed within 24 hours of injury resulted in a shorter hospital residence. Longest delay of operation was measured for hip fractures (28.3 hrs.).
In 351 patients, secondary injuries were detected in 94 individuals (26%), with fractures being the most common secondary injury (n = 40). We recorded postoperative complications of nonsurgical and surgical origin, and 33.6% of our patient cohort displayed complications. Complications were distributed among 118 patients. There was no significant difference in complications regarding the time of operation, with most nonsurgical and surgical complications appearing within 24 hours after operation (n = 110 vs n = 31). Nonsurgical complications, such as anemia (n = 49) and electrolyte imbalances (n = 30), were observed more frequently than surgical complications (n = 107 vs n = 34); however, these complications were reduced by delay in surgery (82.0% in 6–24 hrs. vs 74.2% in ≥24 hrs.). Anticoagulant therapy and age did not affect postoperative complications. The hospital mortality of patients was 6.2%. Follow‐up was restrained to ambulatory visits in the clinic.
Conclusions
Surgical management of hip fractures performed within 24 hours of injury minimizes hospital stay. We did not detect significant differences in the spectrum or number of complications regarding delay of surgery. Surgical complications mainly occur with rapid primary care, and medical complications can be reduced by more intensive preparation of patient and operation procedures.
Keywords: Age traumatology, Complications, Femoral neck fractures, Hip fractures; Pertrochanteric fracture
Abbreviations
- ASA
American Society of Anesthesiologists
- BMI
Body mass index
- DHS
dynamic hip screw
- HHA
hip hemi‐arthroplasty
- PFN
proximal femoral nail
- THP
total hip prosthesis
Introduction
In Germany, hip fractures represent a major health burden, with a prevalence of approximately 135,000 cases per year1, 2, 3. Since demographic change is associated with a high proportion of elderly clientele, an increase of fractures of the femoral neck by at least 40% is estimated to occur until 20304, 5, 6. The immense cost of €2–4 bn per year is mostly caused by age and prolonged release into the initial environment. One‐year mortality of hip fractures is alarmingly high at 20%–30%7, 8, 9.
Treatment of proximal femoral fracture is generally operative. An early operation leads to good results in femoral neck fractures due to reduced rates of head necrosis and 30‐day mortality10, 11, 12, 13. The ideal time for operation is controversially discussed, yet it is often shown to be less than 12 hours after the accident14, 15.
To prevent complications, such as ulcer, deep vein thrombosis, pulmonary embolism, and “surgical complications”, several organizations recommend an operation within 24–48 hours of injury for hip fractures16, 17, 18. A retrospective study was able to demonstrate a correlation between the number of days until operation and an elevated rate of total complications19. A Danish retrospective study showed that a delay of operation leads to increased 30‐ and 90‐day mortality after 12 and 24 hours respectively15, while an Italian study confirmed the 48‐hour limit for enhanced long‐term survival20.
The purpose of this study was to assess whether the time of operative treatment accounts for a particular spectrum of complications.
Additionally, we determined the average length of hospital stay and the underlying reasons.
Finally, we sought to investigate the treatment of femur fractures and which parameters lead to certain surgical complications, delayed operation, and reduced length of stay.
Methods
Population and Inquiry Period
All hip fractures (ICD‐10 S72.0, S72.1, S72.2) were retrospectively analyzed from 1 January 2008 until 31 December 2010 in a level I trauma center with a large sphere of referral in Germany. In this particular single center study, a consistent management throughout the 2 years with a simultaneously diverse operative repertory was performed.
A total of 351 patients with 358 proximal femoral fractures were included.
Inclusion criteria
Age >18 years
Proximal femur fracture.
Operative treatment of proximal femur fracture, including DHS, PFN, THP, HHA, Screw, and others.
No treatment (conservative fracture management).
Mortality, periods between accident/admission and operation, length of hospital stay, complications.
Retrospective cohort study.
Measured Parameters
Patient Characteristics
Age, sex, body mass index (BMI, kg/m2), American Society of Anesthesiologists (ASA)‐status22, concomitant injuries (other fractures, pneumonia, urinary tract infections), comorbidities (cardiological, nephrological, oncological etc.), medication and smoking status (yes/no) were collected at the entrance of hospital. Clinical significance of these parameters was whether they were linked to the time of operative care.
Time of Operation
The time of operation, the time between accident and operation, as well as the time between hospital admission and operating room were gathered for each patient retrospectively. A link between delay of operation and complication spectrum was sought.
Complications
Complications, reoperations, mortality and length of hospital stay (if deceased, the last day was considered) were assessed.
During the course of our study, nonsurgical and surgical complications were recorded. The complications were defined according to a selection of studies23, 24, 25, 26. Nonsurgical complications were defined as follows: anemia (hemoglobin <12.0 g/dL in women and <13.0 g/dL in men27), electrolyte imbalance28, symptomatic transitory psychotic syndrome29, cardiac or pulmonary complications [myocardial infarction30, pneumonia31], urinary tract infection32, renal dysfunction33, and thromboembolism28. Surgical complications included hematoma, mechanic malfunction [dislocations, cutting‐out, refracture], infections, necrosis, pseudarthrosis34, and healing in malposition according to the ICD‐10 in the patient's chart35.
Operative Procedure
The mechanism of injury, implant used (prosthesis, extra‐ or intramedullary implant), fracture classification (femoral head, pertrochanteric, subtrochanteric), postoperative course, rehabilitation, and living situation were also evaluated. We matched the applied implant and fracture type to the timing of operation and complications.
Statistics
Data was collected using Microsoft Excel® (Microsoft Corporation, Redmond, WA, USA), and statistical analyses were performed using GraphPad PRISM 5.0 (GraphPad Software 5.04, San Diego, CA, USA). Comparisons of groups were conducted using the one‐way analysis of variance (ANOVA) and Tukey's post hoc test (α = 0.05). The level of significance used was P < 0.05.
Results
Cohort Characteristics, Fractures, and Therapy
The average age of our 351 patients was 75.5 years (74.2–77.1), and the cohort consisted of 36.2% male and 63.7% female patients. Seven patients had both‐sided proximal femoral fractures. Predominant ASA‐status was II‐III, and, on average, 2.7 accompanying illnesses were recorded per individual.
Throughout the 358 proximal femoral fractures, 167 were pertrochanteric (46.6%), while 151 affected the femoral neck (42.2%). Subtrochanteric fracture occurred in 40 cases (11.2%) (Fig. 1A). Seven patients sustained simultaneous both‐sided hip fractures.
Figure 1.
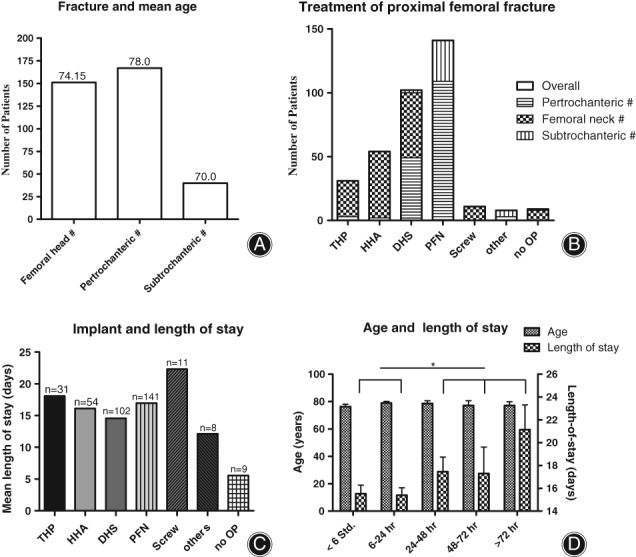
An early operative treatment reduced the duration of the hospital stay. (A) In this cohort, pertrochanteric femur fracture was the most common injury, followed by femoral neck fracture. (B) In hip fracture, PFN was used most frequently (40%), followed by DHS (28%). (C) Mean length of hospital stay for THP was 18.1 days (compared to all other with a mean of 15.8 days). (D) Mean age of patients operated on within the first 6 hours of injury was 74.1 years and did not differ significantly from the other groups. An early operation led to a length of stay of 15.5 days. The group of patients operated on either within or after 24 hours of injury differs significantly in length of stay (t‐test, P = 0.0374).
In femoral neck fractures, dual head prosthesis (34.4%) and dynamic hip screw (DHS, 29.3%) were commonly utilized, while total hip prosthesis (THP) (18.5%) was used least. In pertrochanteric fracture, pertrochanteric femoral nails (PFN, 65.3%) and DHS (29.3%) were utilized. In subtrochanteric fractures, 80% were operated on by using PFN (Fig. 1B).
Periods between Accident/Admission and Operation, Length of Stay
On average, 24 hours passed between a patient's admission and operation. Meanwhile, the time between a patient's accident and their hospital admission averaged 26.6 hours; however, with the exclusion of 10 outliers (125–672 hours) that average decreased to only 5.1 hours.
Patients with femoral neck fractures stayed 1 day less (15.4 days) compared to patients with pertrochanteric (16.6 days) or subtrochanteric (16.6 days) fractures. Between all types of implants used, no significant differences regarding length of stay were detected, with a median of 16.1 days in hospital (Fig. 1C).
Patients who underwent an operation within 6 hours of the accident stayed an average 15.5 days in the hospital, while operations within 6–24 hours and after 24 hours of injury were associated with stays of 15.4 and 17.6 days, respectively. Thus, surgeries performed after 1 day resulted in significantly longer stays (Fig. 1D).
The highest delay in operation was seen in relation to the usage of THP, while hip hemiarthroplasty (HHA) was regularly implanted within the first 6 hours of injury (Fig. 2A, B).
Figure 2.
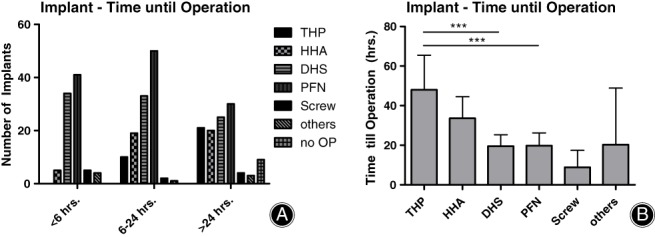
THP‐related procedures are associated with the longest delay until surgery. (A) While DHS and PFN were implanted regularly within 24 hours of injury, THP and HHA were regularly implanted >24 hours after the accident (THP vs PFN: *; HHA vs PFN *, PFN vs Screw: **, PFN vs others: **, PFN vs no OP: **; two‐way ANOVA, Bonferroni post‐test). (B) THP was implanted after an average of 48 hours, HHA after an average of 34 hours. Operation with DHS or PFN was significantly faster compared to THP (P = 0.0001 [***] and 0.0009 [***] respectively, One‐way ANOVA, Tukey's post hoc test 5% level of significance).
ASA‐Status, Anticoagulants, Timing of Operation
Subgroup analysis showed that ASA‐status did not differ significantly among the groups (Fig. 3A), while anticoagulants were used significantly less frequently in patients operated on within <6 hours of injury (Fig. 3A).
Figure 3.
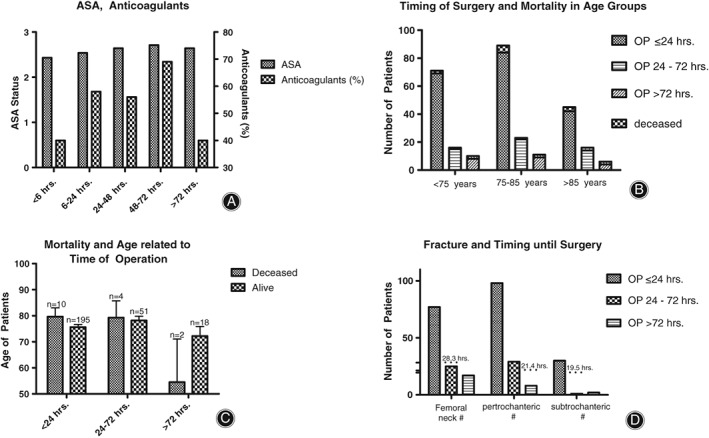
Based on ASA status and mortality, age did not affect the clinical outcome. (A) ASA‐status did not differ significantly among the groups. Anticoagulants were administered to more patients the longer their operation was delayed, while in the >72 hours group, only 40% were treated. Immediate operation was significantly rarer when anticoagulants were taken (Chi‐Square test with 5% level of significance, P = 0.0152). (B) Over all age groups, operation was mostly performed within 24 hours of injury (P = 0.0058 [**], two‐way ANOVA with 5% level of significance). The deceased patients were distributed equally among the age groups and there were no differences in mortality between the groups (P = 0.7486, one‐way ANOVA with Tukey's post hoc test and 5% level of significance). (C) The deceased patients that were operated on within 24 hours of injury were slightly older than those operated on after >72 hours. In the latter group, the survivors were older than the deceased patients, although this finding was not significant (P = 0.65; t‐test, unpaired, 5%‐level of significance). (D) Operation on femoral neck fractures took place an average of 28.3 hours after the time of injury, although most patients were operated within 24 hours of injury. Pertrochanteric fractures were regularly operated on within 24 hours of injury, with a mean time until operation of 21.4 hours.
Operation upon hip fractures was managed regularly within 24 hours of injury (Fig. 3B). Interestingly, patients who were operated on after 72 hours and survived were older than patients who were operated on after 72 hours and did not survive (Fig. 3C). Delay of operation was the longest for hip fractures, with 28.3 hours until operational treatment, and the shortest for pertrochanteric fractures (21.4 hours, Fig. 3D).
Secondary Injuries, Spectrum of Complications
In 351 patients, secondary injuries were detected in 94 individuals (26%), and the most common secondary injuries were fractures (Fig. 4A). We recorded postoperative complications of nonsurgical and surgical origin, and 33.6% of our patient cohort displayed complications. Complications were distributed among 118 patients, whereas surgical complications were most common in patients operated on within 6 hours of injury (Fig. 4B).
Figure 4.
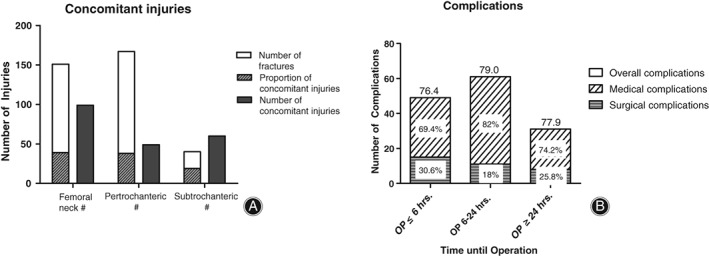
Hematoma and anemia were the most common complications. (A) Concomitant injuries occurred in 25.8% of femoral neck fractures, with 0.67 injuries on average per patient. Pertrochanteric fractures had 24.8% concomitant injuries, with 0.33 injuries per patient. Subtrochanteric fractures had the most concomitant injuries (46.5%), with 1.5 per patient on average. (B) Most complications were measured if the operation was performed within 6 to 24 hours of injury, while most surgical problems occurred within 6 hours of surgery. Age did not differ among the groups (P = 0.4195, one‐way ANOVA, Tukey's post hoc test, 5%‐level of significance).
Nonsurgical complications included anemia, electrolyte disturbances and transitory psychotic syndrome (Fig. 5A). Among surgical complications, mainly hematoma and mechanical complications such as dislocations, cutting‐out, or refracture were detected (Fig. 5B).
Figure 5.
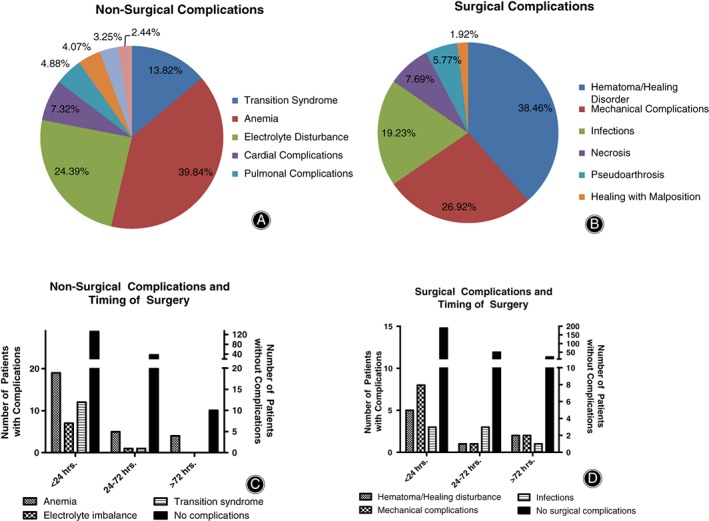
Non‐Surgical and surgical complications show a predominance if operation was performed within the first 24 hours of injury. (A) The relative frequency of nonsurgical complications shows anemia (37.7%), electrolyte imbalances and transition syndrome as the most common complications, while (B) frequency of surgical complications demonstrates that hematoma/healing disturbances were most common (38.5%). (C) When operations were performed within 24 hours of injury, anemia and transition syndrome were most common in patients; however, anemia became rare with a longer period before operation (without leading to significant differences, one‐way ANOVA with Tukey's post hoc test). (D) In most patients, no surgical complications were measured. When operations were performed within 24 hours, mechanical complications and hematoma/healing disturbances were most likely to occur in patients (no significant differences in one‐way ANOVA with Tukey's post hoc test).
There was no significant difference in complications regarding the time of operation, with most nonsurgical and surgical complications appearing within 24 hours after operation (Fig. 5C, D). Most complications occurred when using the PFN, while relative reflection depicts this implant as most secure (Table 1).
Table 1.
Relative complications divided into nonsurgical and surgical show THP as the implant with the lowest risk of surgical adverse events. THP leads to complications most commonly, while PFN und DHS – relatively considered – had the fewest complications. Regarding just surgical complications, THP was the lowest‐risk implant, followed by HHA and PFN
| THP | HHA | DHS | PFN | others | |
|---|---|---|---|---|---|
| Overall complications (Proportional to operations,%) | 61.23 | 55.54 | 48.03 | 46.09 | 84.21 |
| Non‐Surgical complications (%) | 54.81 | 44.44 | 31.38 | 32.62 | 47.37 |
| Surgical complications (%) | 6.46 | 11.11 | 16.67 | 13.48 | 36.84 |
| Number of patients | 31 | 54 | 102 | 141 | 19 |
Mortality
Twenty‐two patients died during their hospital stay (6.2%). These patients were older than the collective, although not significantly. Time until operation did not differ from the surviving collective.
Discussion
Studies addressing hip fractures report cohort characteristics comparable to those of our study36, 37, 38, 39, with a greater proportion of women40, 41 and a similar proportion of comorbidities42, 43.
Length of Hospital Stay
Regarding hip fractures, several studies reported an average stay in hospital of between 13 and 20 days when PFNs were implanted44, 45, 46, which is similar to our finding of 16.1 days. The longer hospital stay resulting from the usage of THP that we measured was confirmed by a German study, with 21.3 days of residence for prosthesis47. One possible explanation for the prolonged stay could be the longer time until operation. Shorter treatment times for patients with femoral neck fractures may be due to the earlier release of this cohort into a nursing home or short‐term care. The longer time until release shown for subtrochanteric fractures may underlie the greater force of impact for this kind of fracture, resulting in more concomitant injuries.
The minimization of time from patient admission to operation can reduce complications and shorten the length of their stay13. Length of hospitalization has tremendous financial implications since DRG‐implementation48, 49, 50. In this study, time until admission is significantly longer after exceeding the 24‐hour operation limit (17.6 vs 15.5 days). This time limit is confirmed by several studies51, 52, 53. Neither ASA‐status nor age of patients is significantly correlated to the timing of operation. Age of surviving patients is indeed correlated to the time of operation. Additionally, the intake of anticoagulants is correlated to the timing of operation, as we and several other studies were able to demonstrate54, 55, 56. An early operation may reduce mortality7, 57, which could not be proven by this study.
Spectrum of Complications
In this population, 33% of patients had complications, with 11.5% of them being surgical. Comparable studies show rates of 12.5%–40%46, 58, 59, 60, 61. Regarding nonsurgical complications, anemia and electrolyte imbalances were predominant, which confirms the rate of 6%–8% found in other studies43, 62.
We strictly separated hematoma from postoperative anemia in our population. While the latter accounted for the greatest part of nonsurgical complications in this study, other authors report up to 86% anemia after operations on hip fracture and tend to not list this as a complication63. In a Spanish analysis, a 24%–44% rate of anemia was described, which is close to our rate.
The time‐of‐operation and implant‐used variables show that nonsurgical complications (anemia and transitory psychotic syndrome) were mostly seen when the operation was performed in the first 24 hours; a longer preparation tends to reduce medical complications. An Israeli study shows that the positive effect of a fast operative procedure on mortality cannot be maintained for longer than 6 months64. Comorbidities especially seem to cause prolonged preparation for operative procedures65, 66, 67.
Surgical complications – especially hematoma and healing disorder with a frequency of 5.6% – were reported in this study, particularly after DHS and PFN, which is in accordance with the literature61, 68. A correlation between the intake of anticoagulants and either hematoma or risk of infection was not seen in this analysis. Infections were a rare complication (2.8%) and comparable to those rates previously reported (1.5%–3.8%43, 69, 70). A “collapse of osteosynthesis,” which the literature suggests can be expected in 3.4%–7.7% of patients39, 71, was seen in 3.9% of our study patients.
Femoral head necrosis has been detected in 1.1% of all fractures in the study; however, long‐term results remain to be collected, and the expected 11.8%34 suggests that the follow‐up was too short.
The fact that most surgical complications appeared within the first 24 hours after the operation could be due to the emergency aspect or lack of expertise of the primary operating surgeon, although the latter should not have any influence72, 73, 74. Referring to the implant used, no significant differences between DHS, THP, or PFN in surgical or nonsurgical complications were seen, which is confirmed by other surveys75.
Revisions were necessary in 11.5% of our patients because of surgical factors. Since similar studies report rates of 5.5 to 53%10, 46, 76, grading seems complicated.
Smektala et al.13 proclaimed that an early operation leads to reduced complications and higher survival rate. While an early operation seems to reduce the rate of complications77, 78, and a reduction of 36 to 24 hours before the operation raises the rate of survival7, we aimed to achieve an early treatment. Within 24 hours of injury, 58% of our patients were surgically supplied, which is close to comparable studies43, 46, 61. Primary THP was operated on after an average of 48.0 hours, while osteosynthesis was performed after a median of 15.4 hours, thereby demonstrating a significant difference. Clientele who are operated on within 6 hours of injury are marginally younger and have a lower ASA‐status than patients treated after the 6 hour period, which can be confirmed by the literature12, 61, 79. Patients older than 85 years are less frequently operated on within 24 hours of injury than are younger patients. A preoperative stabilization partly seems to provide survival benefits to patients80, which supports their supply in specialized age‐traumatology centers81, 82, 83.
Mortality
Hip fractures are associated with mortality rates of 5.4%–14.3% in the literature37, 39, 43; our rate of 6.2% lies within this range. The influence of age or sex could not be confirmed in our study84, 85, 86. Older patients seem to profit from a more intensive preparation for operation, which supports a collaboration between trauma surgery and geriatrics81, 82, 87; however, the operation threshold of 24 hours needs to be maintained and could be recently confirmed88, 89. A patient cutoff of 85 years of age is difficult to be determined, but in a recently published study with 2,000 patients an age of >82 years resulted in higher two‐year mortality89. The data seems to support a difference between the older and younger patients, but conducting a thorough physical examination, basic lab tests, and collecting the general health history and activity status of the patient needs to be the basis of making the decision about when to operate.
Limitations
The present study has been conducted retrospectively for 358 fractures. Incomplete patient records reduce the informative value of the inquiry. Follow‐up is restrained to ambulatory visits in the clinic and is therefore insufficient to detect long‐term complications, consolidation status, or long‐term results. An important bias could be that the patients operated on early were probably those in a better general condition, which could falsify the conclusion of these having better outcome parameters. Preoperative hemoglobin was not detected, and the definition of “anemia” is simply based on the postoperative hemoglobin value.
Regression analyses for potential confounders have not been fully performed, which is why some of the reported results may be due to confounding.
Conclusion
For hip fractures, surgical and nonsurgical complications arise in 33% of patients, with the former occurring more rarely at 11.5%. For the oldest patients, where comorbidity could an interfering factor, intensive preparation for operation seems to be beneficial, while delaying the operations longer than 24 hours increases the patient's length of stay in the hospital.
Declarations
Ethics Approval and Consent to Participate
Approval to analyze patient data was received on 6 January 2014 by the institutional review board (IRB) of the University Medical Center Göttingen (Ethikkommission der Universitätsmedizin Göttingen, Von‐Siebold‐Str.3, 37075 Göttingen). The patients' consent to participate was recorded in writing.
Consent for Publication
Not applicable.
Availability of Data and Material
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Competing Interests
The authors declare that they have no competing interests.
Funding
Not applicable.
Authors' Contributions
JR collected and interpreted the data. DS and JR analyzed and evaluated the data. DS wrote the first version of the manuscript. JR, JCA, DBH, and SS re‐wrote specific sections of the manuscript. All authors read and approved the final manuscript.
References
- 1. Böhm K, Tesch‐Römer C, Ziese T, eds. Gesundheit und Krankheit im Alter. Berlin: Robert Koch‐Inst, 2009. [Google Scholar]
- 2. Hoffmann F, Glaeske G. Incidence of hip fracture in Germany‐‐person‐related analysis of health insurance population. Gesundheitswesen, 2006, 68: 161–164. [DOI] [PubMed] [Google Scholar]
- 3. Minne HW, Pfeifer M, Wittenberg R, Würtz R. Schenkelhalsfrakturen in Deutschland: Prävention, Therapie, Inzidenz und sozioökonomische Bedeutung. Dtsch Arztebl, 2001, 98: 1751. [Google Scholar]
- 4. Beck A, Rüter A. Therapiekonzepte bei Schenkelhalsfrakturen. Teil 1. Der Chirurg, 2000, 71: 240–248. [DOI] [PubMed] [Google Scholar]
- 5. Icks A, Haastert B, Wildner M, Becker C, Meyer G. Trend of hip fracture incidence in Germany 1995‐2004: a population‐based study. Osteoporos Int, 2008, 19: 1139–1145. [DOI] [PubMed] [Google Scholar]
- 6. Bliemel C, Bieneck F, Riem S, et al Weiterbehandlung nach proximaler Femurfraktur ‐ Wer, wann, wohin? Eine deutschlandweite Statuserhebung mit Unterstützung der AG Alterstraumatologie der DGU. Z Orthop Unfall, 2012, 150: 210–217. [DOI] [PubMed] [Google Scholar]
- 7. Bohm E, Loucks L, Wittmeier K, Lix LM, Oppenheimer L. Reduced time to surgery improves mortality and length of stay following hip fracture: results from an intervention study in a Canadian health authority. Can J Surg, 2015, 58: 257–263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Karampampa K, Ahlbom A, Michaelsson K, Andersson T, Drefahl S, Modig K. Declining incidence trends for hip fractures have not been accompanied by improvements in lifetime risk or post‐fracture survival‐‐a nationwide study of the Swedish population 60 years and older. Bone, 2015, 78: 55–61. [DOI] [PubMed] [Google Scholar]
- 9. Omsland TK, Emaus N, Tell GS, et al Mortality following the first hip fracture in Norwegian women and men (1999‐2008). A NOREPOS study. Bone, 2014, 63: 81–86. [DOI] [PubMed] [Google Scholar]
- 10. Carretta E, Bochicchio V, Rucci P, Fabbri G, Laus M, Fantini MP. Hip fracture: effectiveness of early surgery to prevent 30‐day mortality. Int Orthop, 2011, 35: 419–424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Daugaard CL, Jorgensen HL, Riis T, Lauritzen JB, Duus BR, van der Mark S. Is mortality after hip fracture associated with surgical delay or admission during weekends and public holidays? A retrospective study of 38,020 patients. Acta Orthop, 2012, 83: 609–613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Manninger J, Kazar G, Fekete G, et al Significance of urgent (within 6h) internal fixation in the management of fractures of the neck of the femur. Injury, 1989, 20: 101–105. [DOI] [PubMed] [Google Scholar]
- 13. Smektala R, Hahn S, Schrader P, et al Medial hip neck fracture: influence of pre‐operative delay on the quality of outcome. Results of data from the external in‐hospital quality assurance within the framework of secondary data analysis. Unfallchirurg, 2010, 113: 287–292. [DOI] [PubMed] [Google Scholar]
- 14. Bretherton CP, Parker MJ. Early surgery for patients with a fracture of the hip decreases 30‐day mortality. Bone Joint J, 2015, 97: 104–108. [DOI] [PubMed] [Google Scholar]
- 15. Nyholm AM, Gromov K, Palm H, Brix M, Kallemose T, Troelsen A. Time to surgery is associated with thirty‐day and ninety‐day mortality after proximal femoral fracture: a retrospective observational study on prospectively collected data from the Danish fracture database collaborators. J Bone Joint Surg Am, 2015, 97: 1333–1339. [DOI] [PubMed] [Google Scholar]
- 16. Bonnaire W. S2e‐Leitlinie 012/001: Schenkelhalsfraktur des Erwachsenen. Available from: http://www.awmf.org/uploads/tx_szleitlinien/012-001l_S2e_Schenkelhalsfraktur_2015-10_01.pdf (accessed 17 November 2015).
- 17. National Institute for Health Care Excellence . NICE guideline: Hip fracture: management: Clinical guideline [CG124]. 2011. Available from: https://www.nice.org.uk/guidance/cg124/resources/hip-fracture-management-35109449902789 (accessed 12 Jan 2019). [PubMed]
- 18. Royal College of Physicians . Falls and Fragility Fracture Audit Programme (FFFAP): National Hip Fracture Database (NHFD) annual report 2014. 2014. Available from: http://www.nhfd.co.uk/20/hipfractureR.nsf/vwcontent/2014reportPDFs/$file/NHFD2014SummaryReport.pdf?OpenElement (accessed 20 Feb 2019).
- 19. Ryan DJ, Yoshihara H, Yoneoka D, Egol KA, Zuckerman JD. Delay in hip fracture surgery: an analysis of patient‐specific and hospital‐specific risk factors. J Orthop Trauma, 2015, 29: 343–348. [DOI] [PubMed] [Google Scholar]
- 20. Rosso F, Dettoni F, Bonasia DE, et al Prognostic factors for mortality after hip fracture: operation within 48 hours is mandatory. Injury, 2016, 47: S91–S97. [DOI] [PubMed] [Google Scholar]
- 21. Methley AM, Campbell S, Chew‐Graham C, McNally R, Cheraghi‐Sohi S. PICO, PICOS and SPIDER: a comparison study of specificity and sensitivity in three search tools for qualitative systematic reviews. BMC Health Serv Res, 2014, 14: 579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Saklad M. Grading of patients for surgical procedures. Anesthesiology, 1941, 2: 281–284. [Google Scholar]
- 23. Tosounidis TH, Castillo R, Kanakaris NK, Giannoudis PV. Common complications in hip fracture surgery: tips/tricks and solutions to avoid them. Injury, 2015, 46: S3–S11. [DOI] [PubMed] [Google Scholar]
- 24. Peeters CMM, Visser E, van de Ree CLP, Gosens T, Den Oudsten BL, de Vries J. Quality of life after hip fracture in the elderly: a systematic literature review. Injury, 2016, 47: 1369–1382. [DOI] [PubMed] [Google Scholar]
- 25. Muhm M, Hillenbrand H, Danko T, Weiss C, Ruffing T, Winkler H. Frühkomplikationsrate bei hüftgelenknahen Frakturen. Abhängigkeit von der Versorgung im Bereitschaftsdienst und von Nebenerkrankungen. Unfallchirurg, 2015, 118: 336–346. [DOI] [PubMed] [Google Scholar]
- 26. Flikweert ER, Wendt KW, Diercks RL, et al Complications after hip fracture surgery: are they preventable?. Eur J Trauma Emerg Surg, 2018, 44: 573–580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Beutler E, Waalen J. The definition of anemia: what is the lower limit of normal of the blood hemoglobin concentration?. Blood, 2006, 107: 1747–1750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Herold G, ed. Innere Medizin 2018: Eine vorlesungsorientierte Darstellung unter Berücksichtigung des Gegenstandskataloges für die Ärztliche Prüfung mit ICD 10‐Schlüssel im Text und Stichwortverzeichnis. Köln: Gerd Herold, 2018. [Google Scholar]
- 29. Dilling H, Mombour W, Schmidt MH, eds. Internationale Klassifikation psychischer Störungen: ICD‐10 Kapitel V (F) klinisch‐diagnostische Leitlinien. 10. Auflage, unter Berücksichtigung der Änderungen entsprechend ICD‐10‐GM 2015. Hogrefe Verlag: Bern, 2015. [Google Scholar]
- 30. Zipes DP, Braunwald E, eds. Braunwald's Heart Disease: A Textbook of Cardiovascular Medicine, 7th edn Philadelphia, PA: Elsevier Saunders, 2005. [Google Scholar]
- 31. Kasper DL, Fauci AS, Hauser SL, Longo DL, Jameson JL, Loscalzo J. Harrisons Innere Medizin. 19. Auflage, deutsche Ausgabe. New York, Berlin, Stuttgart: McGraw‐Hill Education; ABW Wissenschaftsverlag; Thieme, 2016. [Google Scholar]
- 32. McDougal W, Wein A, Kavoussi L, et al Campbell‐Walsh Urology 10th Edition Review. Philadelphia: Elsevie Saunders, 2012. [Google Scholar]
- 33. Moore EM, Bellomo R, Nichol AD. The meaning of acute kidney injury and its relevance to intensive care and anaesthesia. Anaesth Intensive Care, 2012, 40: 929–948. [DOI] [PubMed] [Google Scholar]
- 34. Haas NP, Krettek C. Tscherne Unfallchirurgie: Hüfte und Oberschenkel. Berlin, Heidelberg: Springer, 2011. [Google Scholar]
- 35. Graubner B, ed. ICD‐10‐GM 2018: Internationale statistische Klassifikation der Krankheiten und verwandter Gesundheitsprobleme 10. Revision ‐ German Modification. Köln: Deutscher Ärzteverlag; 2018. [Google Scholar]
- 36. Hongisto MT, Pihlajamaki H, Niemi S, Nuotio M, Kannus P, Mattila VM. Surgical procedures in femoral neck fractures in Finland: a nationwide study between 1998 and 2011. Int Orthop, 2014, 38: 1685–1690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Miedel R, Ponzer S, Törnkvist H, Söderqvist A, Tidermark J. The standard Gamma nail or the Medoff sliding plate for unstable trochanteric and subtrochanteric fractures. A randomised, controlled trial. J Bone Joint Surg Br, 2005, 87: 68–75 Available from: http://www.bjj.boneandjoint.org.uk/content/87-B/1/68.full. [PubMed] [Google Scholar]
- 38. Miller BJ, Callaghan JJ, Cram P, Karam M, Marsh JL, Noiseux NO. Changing trends in the treatment of femoral neck fractures: a review of the american board of orthopaedic surgery database. J Bone Joint Surg Am, 2014, 96: e149. [DOI] [PubMed] [Google Scholar]
- 39. Smektala R, Wenning M, Ekkernkamp A. Schenkelhalsfraktur: analyse der Ergebnisse externer Qualitätssicherung Ein Bericht über 22 556 Patienten. Der Chirurg, 1999, 70: 1330–1339. [DOI] [PubMed] [Google Scholar]
- 40. Lamb JN, Panteli M, Pneumaticos SG, Giannoudis PV. Epidemiology of pertrochanteric fractures: our institutional experience. Eur J Trauma Emerg Surg, 2014, 40: 225–232 Available from: http://link.springer.com.ezlib.ncifcrf.gov/article/10.1007/s00068-014-0375-x/fulltext.html. [DOI] [PubMed] [Google Scholar]
- 41. Muller‐Mai CM, Schulze Raestrup US, Kostuj T, Dahlhoff G, Gunster C, Smektala R. One‐year outcomes for proximal femoral fractures: posthospital analysis of mortality and care levels based on health insurance data. Unfallchirurg, 2015, 118: 780–794. [DOI] [PubMed] [Google Scholar]
- 42. Boy et al. Hüftgelenknahe Femurfraktur, BQS, 40472 Düsseldorf, 2008.
- 43. Kraus M, Krischak G, Wiedmann K, et al Clinical evaluation of PFNA(R) and relationship between the tip‐apex distance and mechanical failure. Unfallchirurg, 2011, 114: 470–478. [DOI] [PubMed] [Google Scholar]
- 44. Hohendorff B, Meyer P, Menezes D, Meier L, Elke R. Behandlungsergebnisse und Komplikationen nach PFN‐Osteosynthese. Der Unfallchirurg, 2005, 108: 938–953. [DOI] [PubMed] [Google Scholar]
- 45. Lenich A, Mayr E, Ruter A, Mockl C, Fuchtmeier B. First results with the trochanter fixation nail (TFN): a report on 120 cases. Arch Orthop Trauma Surg, 2006, 126: 706–712. [DOI] [PubMed] [Google Scholar]
- 46. Konig‐Leischnig A, Klewer J, Karich B, Richter K. Elderly trauma patients with proximal femur fractures: statistical evaluation of regular process data from a trauma center for the elderly. Unfallchirurg, 2017, 120: 667–674. [DOI] [PubMed] [Google Scholar]
- 47. Lohmann R, Frerichmann U, Stöckle U, Riegel T, Raschke MJ. Proximale Femurfrakturen im Alter. Der Unfallchirurg, 2007, 110: 603–609. [DOI] [PubMed] [Google Scholar]
- 48. Kurtz SM, Lau EC, Ong KL, Adler EM, Kolisek FR, Manley MT. Which clinical and patient factors influence the national economic burden of hospital readmissions after total joint arthroplasty?. Clin Orthop Relat Res, 2017, 475: 2926–2937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Shwartz M, Iezzoni LI, Ash AS, Mackiernan YD. Do severity measures explain differences in length of hospital stay? The case of hip fracture. Health Serv Res, 1996, 31: 365–385. [PMC free article] [PubMed] [Google Scholar]
- 50. Turner P, Cocks J, Cade R, Ewing H, Collopy B, Thompson G. Fractured neck of the femur (DRG 210/211): prospective outcome study. Aust N Z J Surg, 1997, 67: 126–130. [DOI] [PubMed] [Google Scholar]
- 51. Khan SK, Kalra S, Khanna A, Thiruvengada MM, Parker MJ. Timing of surgery for hip fractures: a systematic review of 52 published studies involving 291,413 patients. Injury, 2009, 40: 692–697. [DOI] [PubMed] [Google Scholar]
- 52. Lefaivre KA, MacAdam SA, Davidson DJ, Gandhi R, Chan H, Broekhuyse HM. Length of stay, mortality, morbidity and delay to surgery in hip fractures. Bone Joint J, 2009, 91: 922–927 Available from: http://www.bjj.boneandjoint.org.uk/content/jbjsbr/91-B/7/922.full.pdf. [DOI] [PubMed] [Google Scholar]
- 53. Uzoigwe CE, Burnand HGF, Cheesman CL, Aghedo DO, Faizi M, Middleton RG. Early and ultra‐early surgery in hip fracture patients improves survival. Injury, 2013, 44: 726–729. [DOI] [PubMed] [Google Scholar]
- 54. Eardley WGP, Macleod KE, Freeman H, Tate A. "Tiers of delay": warfarin, hip fractures, and target‐driven care. Geriatr Orthop Surg Rehabil, 2014, 5: 103–108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Ruffing T, Haunschild M, Egenolf M, et al Verzogerte Versorgung huftgelenknaher Femurfrakturen: Analyse des Strukturierten Dialogs Rheinland‐Pfalz. Der Unfallchirurg, 2016, 119: 936–942. [DOI] [PubMed] [Google Scholar]
- 56. Tran T, Delluc A, de Wit C, Petrcich W, Le Gal G, Carrier M. The impact of oral anticoagulation on time to surgery in patients hospitalized with hip fracture. Thromb Res, 2015, 136: 962–965. [DOI] [PubMed] [Google Scholar]
- 57. Accelerated care versus standard care among patients with hip fracture: the HIP ATTACK pilot trial. CMAJ, 2014, 186: 60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Belmont PJ, Garcia EJ, Romano D, Bader JO, Nelson KJ, Schoenfeld AJ. Risk factors for complications and in‐hospital mortality following hip fractures: a study using the National Trauma Data Bank. Arch Orthop Trauma Surg, 2014, 134: 597–604. [DOI] [PubMed] [Google Scholar]
- 59. Buecking B, Wack C, Oberkircher L, Ruchholtz S, Eschbach D. Do concomitant fractures with hip fractures influence complication rate and functional outcome?. Clin Orthop Relat Res, 2012, 470: 3596–3606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Burgers PT, Van Lieshout EM, Verhelst J, Dawson I, de Rijcke PA. Implementing a clinical pathway for hip fractures; effects on hospital length of stay and complication rates in five hundred and twenty six patients. Int Orthop, 2014, 38: 1045–1050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Müller‐Mai C, Schulze‐Raestrup U, Ekkernkamp A, Smektala R. Frühkomplikationen nach Versorgung der Schenkelhalsfraktur. Einfluss des Operationszeitpunktes ‐‐ Analyse von 30.254 Fällen der externen Qualitätssicherung in Westfalen‐Lippe. Chirurg, 2006, 77: 61–69. [DOI] [PubMed] [Google Scholar]
- 62. Saudan M, Lubbeke A, Sadowski C, Riand N, Stern R, Hoffmeyer P. Pertrochanteric fractures: is there an advantage to an intramedullary nail?: a randomized, prospective study of 206 patients comparing the dynamic hip screw and proximal femoral nail. J Orthop Trauma, 2002, 16: 386–393. [DOI] [PubMed] [Google Scholar]
- 63. Willems JM, de Craen AJM, Nelissen RGHH, van Luijt PA, Westendorp RGJ, Blauw GJ. Haemoglobin predicts length of hospital stay after hip fracture surgery in older patients. Maturitas, 2012, 72: 225–228. [DOI] [PubMed] [Google Scholar]
- 64. Peleg K, Rozenfeld M, Radomislensky I, Novikov I, Freedman LS, Israeli A. Policy encouraging earlier hip fracture surgery can decrease the long‐term mortality of elderly patients. Injury, 2014, 45: 1085–1090. [DOI] [PubMed] [Google Scholar]
- 65. Franzo A, Francescutti C, Simon G. Risk factors correlated with post‐operative mortality for hip fracture surgery in the elderly: a population‐based approach. Eur J Epidemiol, 2005, 20: 985–991. [DOI] [PubMed] [Google Scholar]
- 66. Librero J, Peiró S, Leutscher E, et al Timing of surgery for hip fracture and in‐hospital mortality: a retrospective population‐based cohort study in the Spanish National Health System. BMC Health Serv Res, 2012, 12: 1 Available from: http://bmchealthservres.biomedcentral.com/track/pdf/10.1186/1472-6963-12-15?site=http://bmchealthservres.biomedcentral.com. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Vidan MT, Sanchez E, Gracia Y, Maranon E, Vaquero J, Serra JA. Causes and effects of surgical delay in patients with hip fracture: a cohort study. Ann Intern Med, 2011, 155: 226–233. [DOI] [PubMed] [Google Scholar]
- 68. Gonschorek O, Verheyden AP, Tiemann A, Josten C. Komplikationen mit dem proximalen Femurnagel (PFN). Trauma Berufskrankh, 2003, 5: s171–s174. [Google Scholar]
- 69. Lee WT, Murphy D, Kagda FHY, Thambiah J. Proximal femoral locking compression plate for proximal femoral fractures. J Orthop Surg (Hong Kong), 2014, 22: 287–293. [DOI] [PubMed] [Google Scholar]
- 70. Hrubina M, Skotak M, Behounek SJ. DHS osteosynthesis for proximal femoral fractures: infectious complications. Acta Chir Orthop Traumatol Cech, 2013, 80: 351–355. [PubMed] [Google Scholar]
- 71. Fuchtmeier B, Gebhard F, Lenich A. Complications after pertrochanteric fractures. Unfallchirurg, 2011, 114: 479–484. [DOI] [PubMed] [Google Scholar]
- 72. Altintas B, Biber R, Bail HJ. The learning curve of proximal femoral nailing. Acta Orthop Traumatol Turc, 2014, 48: 396–400. [DOI] [PubMed] [Google Scholar]
- 73. Bliemel C, Oberkircher L, Eschbach D‐A, Struewer J, Ruchholtz S, Buecking B. Surgical treatment of proximal femoral fractures‐‐a training intervention?. Z Orthop Unfall, 2013, 151: 180–188. [DOI] [PubMed] [Google Scholar]
- 74. Prokop A, Dolezych R, Chmielnicki M. Pertrochanteric fracture ‐ operation for beginners?. Z Orthop Unfall, 2014, 152: 584–587. [DOI] [PubMed] [Google Scholar]
- 75. Bonnaire F, Lein T, Bula P. Implantatwahl am proximalen Femur. Trauma Berufskrankh, 2011, 13: 97–106. [Google Scholar]
- 76. Kurtinaitis J, Porvaneckas N, Kvederas G, Butenas T, Uvarovas V. Revision rates after surgical treatment for femoral neck fractures: results of 2‐year follow‐up. Medicina (Kaunas), 2013, 49: 138–142. [PubMed] [Google Scholar]
- 77. Bonnaire F, Strassberger C, Kieb M, Bula P. Osteoporotic fractures of the proximal femur. What's new?. Chirurg, 2012, 83: 882–891. [DOI] [PubMed] [Google Scholar]
- 78. Buecking B, Bohl K, Eschbach D, et al Factors influencing the progress of mobilization in hip fracture patients during the early postsurgical period?‐A prospective observational study. Arch Gerontol Geriatr, 2015, 60: 457–463. [DOI] [PubMed] [Google Scholar]
- 79. Bottle A, Aylin P. Mortality associated with delay in operation after hip fracture: observational study. BMJ, 2006, 332: 947–951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80. de Palma L, Torcianti M, Meco L, Catalani A, Marinelli M. Operative delay and mortality in elderly patients with hip fracture: an observational study. Eur J Orthop Surg Traumatol, 2014, 24: 783–788. [DOI] [PubMed] [Google Scholar]
- 81. Grund S, Roos M, Duchene W, Schuler M. Treatment in a center for geriatric traumatology. Dtsch Arztebl Int, 2015, 112: 113–119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82. Prestmo A, Hagen G, Sletvold O, et al Comprehensive geriatric care for patients with hip fractures: a prospective, randomised, controlled trial. The Lancet, 2015, 385: 1623–1633 Available from: http://www.thelancet.com/article/S0140673614624090/fulltext. [DOI] [PubMed] [Google Scholar]
- 83. Schoeneberg C, Hussmann B, Wesemann T, et al Herausforderung der Implementierung eines Alterstraumanetzwerks: Ein standortübergreifendes Verbundsystem. Der Unfallchirurg, 2018, 121: 313–320. [DOI] [PubMed] [Google Scholar]
- 84. Elliott J, Beringer T, Kee F, Marsh D, Willis C, Stevenson M. Predicting survival after treatment for fracture of the proximal femur and the effect of delays to surgery. J Clin Epidemiol, 2003, 56: 788–795. [DOI] [PubMed] [Google Scholar]
- 85. Frerichmann U, Raschke MJ, Stöckle U, Wöhrmann S, Lohmann R. Proximale Femurfrakturen im Alter. Der Unfallchirurg, 2007, 110: 610–616 Available from: http://link.springer.com.832-0.han.sub.uni-goettingen.de/article/10.1007/s00113-007-1258-y/fulltext.html. [DOI] [PubMed] [Google Scholar]
- 86. Geiger F, Schreiner K, Schneider S, Pauschert R, Thomsen M. Proximal fracture of the femur in elderly patients. The influence of surgical care and patient characteristics on post‐operative mortality. Orthopade, 2006, 35: 651–657. [DOI] [PubMed] [Google Scholar]
- 87. Kammerlander C, Roth T, Friedman SM, et al Ortho‐geriatric service‐‐a literature review comparing different models. Osteoporos Int, 2010, 21: S637–S646. [DOI] [PubMed] [Google Scholar]
- 88. Pincus D, Ravi B, Wasserstein D, et al Association between wait time and 30‐day mortality in adults undergoing hip fracture surgery. JAMA, 2017, 318: 1994–2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89. Müller F, Galler M, Kottmann T, Zellner M, Bäuml C, Füchtmeier B. Analyse von 2000 operativ versorgten proximalen Femurfrakturen: multiple Variablen beeinflussen die Mortalität. Der Unfallchirurg, 2018, 121: 550–559. [DOI] [PubMed] [Google Scholar]


