Abstract
Objective
To evaluate the long‐term efficacy of Bryan cervical disc arthroplasty in the treatment of myelopathy patients compared with radiculopathy patients.
Methods
This study is a prospective study. Sixty‐six patients (38 patients in myelopathy group and 28 patients in radiculopathy group) who were treated with Bryan cervical disc arthroplasty between 2004 and 2007 and followed for 10 years were included in this study. The Japanese Orthopaedic Association (JOA) score, neck disability index (NDI), and Odom's criteria were used to evaluate the clinical outcomes. X‐ray, computed tomography (CT), and magnetic resonance imaging (MRI) were used to evaluate the radiographic outcomes including the global range of motion (ROM), segmental ROM, and segment alignment before the surgery and at last follow‐up. The incidence of segmental kyphosis, segmental mobility lost, and the grade of paravertebral ossification (PO) were also evaluated at last follow‐up.
Results
The JOA score and NDI improved in both groups. Thirty‐three of 38 patients in myelopathy group and all patients in radiculopathy group reported good or excellent outcomes according to Odom's criteria. The segmental ROM was (9.5° ± 4.4°) before surgery and maintained at (9.0° ± 5.5°) at last follow‐up in myelopathy group. The segmental ROM was (9.5° ± 4.6°) and (9.0° ± 5.3°) before surgery and at last follow‐up in radiculopathy group, respectively. The Bryan prosthesis remained mobile at last follow‐up for 30 patients (78.9%) in the myelopathy group and 22 patients (78.6%) in the radiculopathy group. Of the patients in the myelopathy group, 21.1% developed segmental kyphosis, as did 21.4% of patients in the radiculopathy group. The incidence of PO and high‐grade PO was 92.1 and 28.9% in the myelopathy group, and was 92.9 and 32.1% in the radiculopathy group. There was no significant difference between both groups.
Conclusions
Bryan cervical disc arthroplasty was an effective and safe technique in treating patients with myelopathy. The clinical and radiographic outcomes in the myelopathy group were similar to those in the radiculopathy group at the 10‐year follow‐up.
Keywords: Bryan disc, Cervical disc arthroplasty, Long‐term follow‐up, Myelopathy, Radiculopathy
Introduction
In recent years, with changes in lifestyles and working environment, cervical degenerative diseases including radiculopathy and myelopathy caused by cervical disc herniation or cervical spondylosis have become one of the most prevalent diseases. The number of patients suffering from radiculopathy and myelopathy which required surgical treatment to resolve has increased rapidly1, 2. Over the past several decades, anterior cervical discectomy and fusion (ACDF) has been the golden standard surgical technique for cervical degenerative diseases3, 4. ACDF is an effective technique to directly decompress soft disc herniations and osteophytes which compressed spinal cord and nerve roots. ACDF could relieve the symptoms of radiculopathy and myelopathy effectively, and the fusion could also provide segmental stabilization, maintaining the alignment of the operation segment which could prevent kyphosis after the operation. However, with the wide application of ACDF, the concern about the complications of segment fusion is gradually increasing. This fusion can let the operation segment lose physiological mobility. Several previous biomechanical studies also demonstrated that the fusion of the operation segment could increase the intradiscal pressure or hypermobility in adjacent levels5, 6, 7. The pattern of intervertebral fusion made ACDF potentially accelerate the degeneration of adjacent segments and increase the incidence of adjacent segment disease (ASD), which many long‐term follow‐up studies also proved8, 9.
Due to the disadvantages mentioned above of ACDF, techniques designed to preserve the mobility of operated segments were being developed. The cervical artificial disc as a motion‐preserving prosthesis was used for cervical disc arthroplasty from the 1970s. Over the past 20 years, with the rapid development of materials science and cervical biomechanics research, many different designed types (unconstrained, semi‐constrained, and constrained) and different materials (metal to metal, metal to plastic) cervical artificial disc prosthesis have emerged10, 11, 12. Cervical disc arthroplasty could maintain the physiological mobility, anatomical disc space height and normal segmental alignment of the operated level. These advantages made cervical disc arthroplasty diminish the stress of the adjacent segment, which reduced or delayed the incidence of ASD compared with ACDF13, 14. Over the past decade, many clinical studies have demonstrated that cervical disc arthroplasty has been established as an alternative to ACDF for the treatment of symptomatic degenerative cervical disease15, 16, 17.
However, with the wild prevalent use of cervical disc arthroplasty, some controversy on the indication of cervical disc arthroplasty has been raised among surgeons. Cervical disc arthroplasty was initially used in patients with radiculopathy. There is still some controversy about whether cervical disc arthroplasty is suitable for patients with cervical spondylotic myelopathy (CSM). CSM is defined as impaired spinal cord function, including gait disturbance, difficulty with coordination and fine motor tasks, and other sensory and motor disturbance caused by cervical degenerative diseases leading to spinal cord compression1. There are some concerns about the motion‐preserving technique using in patients with CSM18, 19, 20. First, the spinal cord compression factors in patients with CSM include static compression factors and dynamic compression factors. The operation could decompress the static compression factors, but the dynamic compression factors might not be solved during the surgery. There has been a concern that the use of motion‐preserving techniques in patients with CSM could remain the dynamic compression factors which would maintain microtrauma to the compromised spinal cord, and thus lead to progression of myelopathy and adverse long‐term outcomes. Second, there was a concern that the occurrence of segmental kyphosis and paravertebral ossification (PO), which protrude to the spinal canal direction after cervical disc arthroplasty, might compress the spinal cord, and thus could result in recurrence or worsening of myelopathic symptoms.
Most previous clinical studies which evaluated the efficacy of cervical disc arthroplasty did not enroll the patients with CSM or enrolled a mixed cohort of patients with both myelopathy and radiculopathy8, 9, 13, 14, 15, 16. Only a few short‐ or mid‐term follow‐up studies demonstrated that cervical disc arthroplasty had satisfying short‐ to mid‐term outcomes in the treatment of patients with CSM21, 22, 23. Therefore, the long‐term efficacy of cervical disc arthroplasty for CSM still requires further patient outcomes to be reported.
The present study was thus designed to evaluate the long‐term efficacy of cervical disc arthroplasty for patients with CSM (myelopathy or radicumyelopathy) compared with efficacy for patients with radiculopathy. Therefore, we presented 10‐year follow‐up data of 8 patients with CSM and 28 patients with radiculopathy who underwent cervical disc arthroplasty. The main purpose of this study is to determine the long‐term outcomes of cervical disc arthroplasty in the treatment of CSM, as well as evaluating the long‐term complications and radiological outcomes of cervical disc arthroplasty for CSM.
Materials and Methods:
Inclusion and Exclusion Criteria
The inclusion criteria were as follows: (i) patients with myelopathy (symptoms of gait disturbance, loss of coordination, difficulty with fine motor task, etc.); (ii) patients with radiculopathy (symptoms of pain or/and sensory or motor deficit in upper extremities, etc.); (iii) patients with radicumyelopathy (symptoms of myelopathy and radiculopathy); (iv) the symptoms were caused by spinal cord and/or nerve root compression resulting from single‐level cervical degenerative diseases between the C3/ 4 and C6/ 7 level; (v) the symptoms of patients had not responded to conservative treatment; (vi) patients were treated by cervical disc arthroplasty; (vii) patients were willing to complete the follow‐up; and (viii) this is was a prospective, non‐randomized, comparative study to evaluate cervical disc arthroplasty for myelopathy patients compared with radiculopathy patients. All patients were followed up for 10 years.
The exclusion criteria were: (i) moderate or severe degeneration at the target level; (ii) instability or kyphosis; (iii) ossification of the posterior longitudinal ligament; (iv) previous cervical spine surgery and other surgical contraindications; and (v) spine disease that occurred after surgery in non‐surgical and non‐adjacent segment resulting in compression of spinal cord and/or nerve root which could influence the evaluation of efficacy of operation.
Patient Enrollment
This was a prospective, non‐randomized, comparative study of patients with myelopathy or radiculopathy who underwent Bryan (Medtronic Sofamor Danek, Memphis, TN) cervical disc arthroplasty in Beijing Jishuitan Hospital from March 2004 to December 2007. All the patients enrolled in the present study were treated by the same team, and all operations were performed by the same experienced group using the standard Bryan disc arthroplasty procedures.
A total of 66 patients that had completed clinical and radiographic follow‐up were included in this study. The mean follow‐up time was more than 10 years, and the follow‐up rate was 77.6%. The mean age of patients was 55.9 ± 7.9 years and consisted of 41 men (62.1%) and 25 women (37.9%). The index level included C3/4 (2 levels, 3.0%), C4/5 (13 levels, 19.7%), C5/6 (43 levels, 65.2%), and C6/7 (8 levels, 12.1%). According to the symptoms, patients were divided into a myelopathy group (total of 38 patients (57.6%), including 16 patients with myelopathy and 22 patients with myeloradiculopathy) and a radiculopathy group (28 patients, 42.4%).
Surgery Process
After general anesthesia, the patient was placed in a supine position and the neck was placed in a neutral position. The left‐side front transverse incision was taken for the C6/ 7 segment, the right‐side front transverse incision was taken for the other segments. The Smith‐Robinson approach was used to separate to the anterior vertebrae and insert a marker needle into the target intervertebral space. After confirming the operated segment by intraoperative fluoroscopy, the Bryan artificial disc operating system was placed at the target segment. The intervertebral disc was removed, the endplate was polished, and the osteophytes of posterior vertebral body and the posterior longitudinal ligament were removed. After the decompression of the spinal cord and nerve roots were satisfactory, the proper size Bryan artificial disc was placed. Intraoperative fluoroscopy was used to determine whether the position of the Bryan artificial disc was satisfactory. The drainage was placed, and the incision was closed layer by layer.
Clinical Evaluation
Japanese Orthopaedic Association (JOA) score 24
JOA was used to evaluate the spinal cord function, which was assessed at preoperative and at last follow‐up. The total score of the JOA was 17 points, including upper limb motor function (four points), lower limb motor function (four points), upper limb sensory function (two points), trunk sensory function (two points), lower limb sensory function (two points), and bladder function (two points). The better the function (three points). JOA improvement rate = [(follow‐up JOA score−preoperative JOA score)/(17−preoperative JOA score)] × 100%. JOA score improvement rate > 85% is considered an excellent score, 60%–84% is good, 25%–59% is fair, 0%–24% or if JOA score is lower than preoperative is poor.
Neck Disability Index (NDI) 25
NDI was used to evaluate neck pain and disability; NDI was assessed at preoperative and at last follow‐up. NDI contains 10 self‐reported items, including: pain intensity, personal care, lifting, reading, headache, concentration, working, sleeping, driving, and entertainment. Each item is scored from zero to five. The final score was presented as the percentage of the maximal score. Final NDI score is calculated as (total score/ (five × number of questions answered)) × 100%. Zero per cent to 20% is considered mild dysfunction, 21%–40% is moderate dysfunction, 41%–60% is severe dysfunction, and 61%–80% is considered as disability. Eighty‐one percent to 100% is either long‐term bedridden or exaggerating the impact of pain on their life.
Odom's Criteria
Odom's criteria were used to evaluate the overall efficacy at last follow‐up. Odom's criteria contain four levels. Excellent: all preoperative symptoms are completely relieved. Good: preoperative symptoms are relieved, and daily activities and work are not affected. Fair: preoperative symptoms are partially relieved, but daily activities are significantly limited. Poor: preoperative symptoms have no change or get worse.
Radiographic Evaluation
Radiographic evaluation included lateral neutral and dynamic (flexion‐extension) cervical radiographs, computed tomography (CT), and magnetic resonance imaging (MRI).
Range of Motion (ROM)
The ROM of the overall cervical spine (C2–C7) and index level (functional spinal unit) was measured by the Cobb angle method on lateral dynamic radiographs. The ROM of overall cervical spine and index level were measured preoperatively and at last follow‐up. The ROM at an index level of less than 2° was defined as mobility lost26.
Segmental Alignment
The segmental alignment was determined by the angle of the functional spinal unit (FSU) on lateral neutral radiographs. The segmental alignment was measured at preoperative and at last follow‐up. A negative FSU angle donated segmental kyphosis.
Paravertebral Ossification (PO)
PO was classified as five grades. Grade zero is no ossification. Grade I is ossification not invasive into intervertebral space. Grade II is ossification invasive into intervertebral space. Grade III is ossification form bridging bone between adjacent vertebral bodies, and the ROM of index level is affected; Grade IV is complete fusion, and the ROM of index level is less than 3°.
Statistical Analysis
The normally distributed data is given as the mean ± standard deviation, and the non‐normally distributed data is given as the median (interquartile). The independent sample t‐test was used to compare normally distributed data, and the Mann–Whitney u‐test was used to compare non‐normally distributed data, or ordinal data, between both groups. The Chi‐Square test was used to compare categorical data between both groups. Statistical significance was defined and accepted as P < 0.05. All statistical analyses were performed using IBM SPSS Statistics 20.0 (SPSS, Chicago, IL, USA).
Results
General Results
From the 66 patients, 38 (57.6%) patients were in the myelopathy group, and 28 (42.4%) patients were in the radiculopathy group. The mean age of patients in the radiculopathy group (54.4 ± 7.6 years) was younger than the patients in myelopathy group (57.0 ± 8.0 years); however, the difference was not significant. The proportional sex compositions in both groups were similar (68.4% of men in the myelopathy group vs. 53.6% of men in the radiculopathy group). The primary cause factor (36.8% disc herniation in the myelopathy group vs. 50% disc herniation in the radiculopathy group), follow‐up time (124 months in the myelopathy group vs. 129 months in radiculopathy group), and the distribution of index levels were similar in both groups. There was no significant difference in baseline data between the two groups (Table 1).
Table 1.
Baseline characteristics between two groups
| Variable | Myelopathy | Radiculopathy | P value | Text value |
|---|---|---|---|---|
| Age (years) | 57.0 ± 8.0 | 54.4 ± 7.6 | 0.175 | 1.371 |
| Gender | 0.219 | 1.511 | ||
| Male | 26 (68.4%) | 15 (53.6%) | ||
| Female | 12 (31.6%) | 13 (46.4%) | ||
| Primary cause | 0.285 | 1.143 | ||
| Disc herniation | 14 (36.8%) | 14 (50.0%) | ||
| Spondylosis | 24 (63.2%) | 14 (50.0%) | ||
| Follow‐up time (months) | 124.0 (17.0) | 129.0 (26.5) | 0.715 | 0.365 |
| Operated level | 0.389 | 3.015 | ||
| C3/ 4 | 0 | 2 (7.1%) | ||
| C4/ 5 | 7 (18.4%) | 6 (21.4%) | ||
| C5/ 6 | 26 (68.4%) | 17 (60.7%) | ||
| C6/ 7 | 5 (13.2%) | 3 (10.7%) |
Clinical Outcomes
JOA
The JOA score showed great improvement at the last follow‐up compared with preoperative scores in both groups. The preoperative and last follow‐up JOA score in the radiculopathy group was higher than those in the myelopathy group (P < 0.001) (Table 2).
Table 2.
Clinical outcomes between two groups
| Variable | Myelopathy | Radiculopathy | P value | Text value |
|---|---|---|---|---|
| Pre JOA | 12.0 (3.5) | 15.0 (1.5) | <0.001 | 5.963 |
| Last FU JOA | 15.5 (1.5) | 17.0 (0.5) | <0.001 | 3.846 |
| Pre NDI | 28.0 (14.5) | 26.0 (8.0) | 0.218 | 1.231 |
| Last FU NDI | 14.0 (12.0) | 12.0 (7.5) | 0.127 | 1.526 |
| Odom criteria | 0.060 | 1.884 | ||
| Excellent | 17 (44.7%) | 18 (64.3%) | ||
| Good | 16 (42.1%) | 10 (35.7%) | ||
| Fair | 5 (13.2%) | 0 | ||
| Poor | 0 | 0 |
FU, follow‐up; JOA, Japanese Orthopedic Association score; NDI, neck disability index; Pre, preoperative.
NDI
The NDI declined at last follow‐up in both groups, and there was no significant difference in NDI between both groups (Table 2).
Odom's Criteria
Using Odem's criteria, 86.8% of patients in the myelopathy group and 100% of the patients in the radiculopathy group reached a good or excellent outcome, and there was no significant difference between the two groups (Table 2). Up to the last 10 year follow‐up, there was no infection, migration of Bryan prosthesis, revision surgery in operated levels, or neurological deterioration in either group.
Radiographic Outcomes
ROM
The ROM of the index level and overall cervical spine were well maintained from pre‐operation to the last follow‐up in both groups (Table 3). At last follow‐up, eight patients (21.1%) in the myelopathy group and six patients (21.4%) in radiculopathy group occurred segmental mobility lost. The global ROM and segmental ROM at preoperative and last follow‐up had no significant difference in the two groups (Table 3).
Table 3.
Radiographic outcomes between two groups
| Variable | Myelopathy | Radiculopathy | P value | Text value |
|---|---|---|---|---|
| Pre global ROM | 45.5° ± 15.1° | 45.8° ± 15.7° | 0.930 | 0.089 |
| Last FU global ROM | 45.6° ± 13.1° | 48.8° ± 11.0° | 0.302 | 1.041 |
| Pre segmental ROM | 9.5° ± 4.4° | 9.5° ± 4.6° | 0.988 | 0.014 |
| Last FU segmental ROM | 9.0° ± 5.5° | 9.0° ± 5.3° | 0.992 | 0.010 |
| Pre segmental alignment | 2.2° ± 1.2° | 2.0° ± 1.5° | 0.559 | 0.587 |
| Last FU segmental alignment | 1.4° ± 1.7° | 1.1° ± 2.1° | 0.435 | 0.785 |
| High grade PO (n) | 11 (28.9%) | 9 (32.1%) | 0.782 | 0.277 |
| Segmental kyphosis (n) | 8 (21.1%) | 6 (21.4%) | 0.971 | 0.037 |
| Mobility lost (n) | 8 (21.1%) | 6 (21.4%) | 0.971 | 0.037 |
FU, follow‐up; High grade PO, Grade III‐IV PO; Mobility lost, ROM < 2°; Pre, preoperative; ROM, range of motion.
Segmental Alignment
The segmental alignment decreased from 2.2° at baseline to 1.4° at last follow‐up in the myelopathy group and decreased from 2.0° at baseline to 1.1° at last follow‐up in the radiculopathy group. Eight patients (21.1%) in the myelopathy group and six patients (21.4%) in the radiculopathy group developed segmental kyphosis at their last follow‐up. The segmental alignment showed no significant difference between both groups (Table 3).
PO
Thirty‐five patients (92.1%) in the myelopathy group (12 cases of Grade I, 12 cases of Grade II, four cases of Grade III, seven cases of Grade IV), and 26 patients (92.9%) in radiculopathy group (four cases of Grade I, 13 cases of Grade II, four cases of Grade III, five cases of Grade IV) had developed PO at their last follow‐up. The incidence of PO and high‐grade PO had no significant difference between both groups (Table 3).
Discussion
Clinical Outcomes
The effectiveness of cervical disc arthroplasty to maintain a good clinical outcome and motion at the index level has been established in many previously published studies8, 9, 13, 14, 15, 16, 21, 22, 23. However, the majority of previous studies of cervical disc arthroplasty were based on a mixed cohort of patients with both myelopathy and radiculopathy8, 9, 13, 14, 15, 16. The long‐term effect of cervical disc arthroplasty in treating patients with myelopathy remains uncertain. There are concerns that cervical disc arthroplasty in the treatment of CSM could cause dynamic compression factors to remain which would result in the progression of neurologic injuries and negative impact on long‐term outcomes18. Hence, the cervical disc arthroplasty for patients with myelopathy will face more challenges over time.
Riew et al.21 performed a study of 199 patients with myelopathy and compared the results from single‐level treatments of cervical disc arthroplasty (n = 106) versus arthrodesis (n = 93) with a 2 years follow‐up. The results indicated that both groups showed great improvement in neurological status, and there was no difference between the two groups. Fay et al.22 reported a 3‐year follow‐up study of 72 myelopathy patients and 53 radiculopathy patients treated with cervical disc arthroplasty and concluded that the clinical and radiographic outcomes in patients with myelopathy were similar to patients with radiculopathy. Khong et al.23 investigated 46 patients treated with cervical disc arthroplasty and compared success rates in myelopathy patients versus radiculopathy patients and demonstrated that the success rate with cervical disc arthroplasty was similar in both groups up to 5‐year follow‐up. However, studies with at least 5 to 10 years of follow‐up are still limited, and the long‐term efficacy of cervical disc arthroplasty in the management of myelopathy has yet to be proven.
In this study, 38 patients with myelopathy and 28 patients with radiculopathy treated with Bryan cervical disc arthroplasty were followed up for 10 years. Both the JOA and NDI improved compared to preoperative scores in both myelopathy and radiculopathy patients. Patients in myelopathy group have myelopathic symptoms which caused the JOA before surgery and at last follow‐up were all lower than those in the radiculopathy group. All of the patients in the radiculopathy group and 33 of the 38 patients in the myelopathy group received excellent or good outcomes according to Odom's criteria. No patient had radiological evidence of recurrent compression at the index level and no patient needed revision surgery at last follow‐up (Fig. 1). Furthermore, we found that the spinal cord compression in the five patients with fair outcomes, according to Odom's criteria, were all caused by spondylosis. This may suggest that the primary cause (disc herniation or spondylosis) could affect the long‐term results in myelopathy patients treated with cervical disc arthroplasty. This inference still needs long‐term follow‐up and a specifically designed study to confirm.
Figure 1.
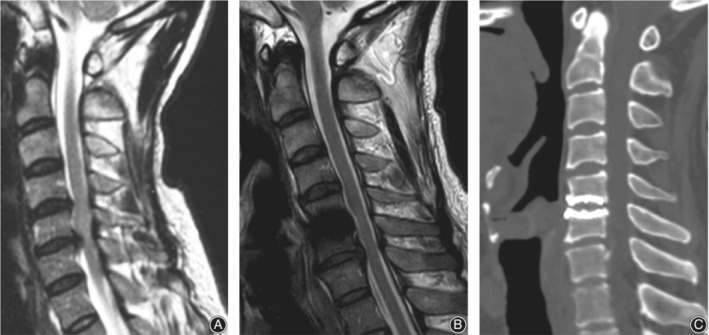
(A) Preoperative MRI showed spinal cord compression caused by disc herniation at C5/ 6 level. (B) MRI at 10‐year follow‐up showed spinal cord was decompressed. (C) CT at 10‐year follow‐up showed that Bryan disc was in good position.
Motion and Alignment
Cervical disc arthroplasty is designed to preserve motion at the index level. Quan et al.27 reported that 77.8% of Bryan prosthesis maintained mobility with a mean ROM of 8.4° in an 8‐year follow‐up study completed on 21 patients. Dejaegher et al.28 described the mean ROM of single‐level Bryan cervical disc arthroplasty as being at 8.6° at the 10‐year follow‐up, and 80.9% of prosthesis remained mobile. The results of this study were similar to the results of previous studies. Nearly 79% of prosthesis in both groups maintained mobility with a mean ROM of 9.0° at the 10‐year follow‐up.
As for sagittal alignment, Bryan disc has no ability to restore the local lordosis and tends to develop segmental kyphosis due to the structural absence of lordosis and lack of anterior column support27, 29. Several studies have documented the occurrence of segmental kyphosis after Bryan cervical disc arthroplasty; however, this was not related to clinical outcomes27, 30. In this study, we excluded patients with preoperative kyphosis. Approximately 20% of the patients developed segmental kyphosis in both groups at their last follow‐up. The occurrence of segmental kyphosis did not affect the clinical outcome (Fig. 2). Whether the kyphotic angle will continue to progress and lead to the recurrence of myelopathic symptoms still needs further follow up.
Figure 2.
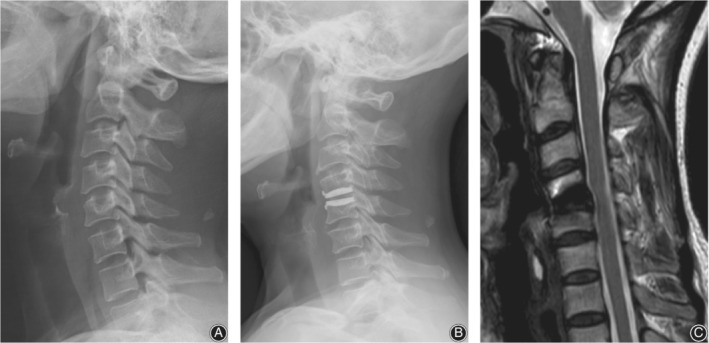
(A) Preoperative lateral X‐ray showed that lordosis existed at C4/ 5 level. (B) Lateral X‐ray at 10‐year follow‐up showed C4/ 5 level developed segmental kyphosis after. Bryan cervical disc arthroplasty. (C) MRI at 10‐year follow‐up showed that spinal cord was not compressed at operated level.
Paravertebral Ossification
PO is defined as bone formation in and around a disc replacement including heterotopic ossification and spondylotic osteophytes31, 32. The incidence of PO after cervical disc arthroplasty varied from 16.1% to 94.1%33. Many factors, including prosthesis types, follow‐up time, the primary cause (spondylosis or disc herniation) and evaluation methods, could affect the rate of PO occurrence31, 32, 34. Kong et al.34 conducted a meta‐analysis which showed that the prevalence of PO and high‐grade PO after cervical disc arthroplasty with 5 to 10 years of follow‐up was 53.6% and 47.5%. Zhao et al.35 reported the PO was present in 69.0% of patients after Bryan cervical disc arthroplasty at the 10‐year follow‐up. In this study, 61 of the 66 patients developed PO at their 10‐year follow‐up. The following reasons could account for the high incidence of PO in our study: (i) we used Tian's method based on both CT scan and dynamic radiograph to evaluate PO31, 32, which could provide more details about lateral PO and low grade PO which might not show on the X‐ray; (ii) patients with spondylosis were not excluded, which may increase the incidence of PO at the last follow‐up33; and (iii) patients were followed for 10 years, and the length of follow‐up would affect the results34. At the last follow‐up, the incidence of PO and high grade PO was similar in both groups, and the PO formation did not lead to recurrence or worsening of clinical symptoms in our study. However, further follow‐up is still required to access the progression of PO after cervical disc arthroplasty (Fig.3).
Figure 3.
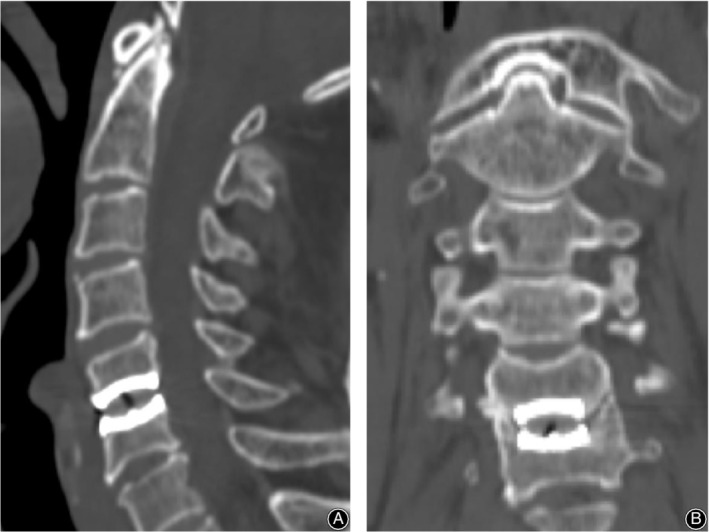
(A) Sagittal CT showed no paravertebral ossification (PO) at operated level. (B) Coronal CT showed GradIeV PO at operated level.
Limitation
There were some limitations to this study. First, the follow‐up rate was 77.6%, which was lower than the general validity follow‐up rate of 80%. However, due to the length of time and the difficulty of tracking patients for such a long duration, the follow‐up rate would be acceptable. Second, the outcomes of the present study did not compare with outcomes of fusion, and future research should focus on the comparison of ACDF versus cervical disc arthroplasty in the treatment of myelopathy and radiculopathy. Third, the present study only compared 10‐year follow‐up outcomes. There was a lack of different follow‐up time outcomes, so the dynamic changes could not be displayed. Finally, the patient sample of the present study is relatively small, and all patients were from one center. Larger‐scale and multi‐center clinical studies are still needed to evaluate the efficacy of cervical disc arthroplasty.
Conclusion
Bryan cervical disc arthroplasty was an effective and safe technique in treating patients with myelopathy. The clinical and radiographic outcomes in the myelopathy group were similar to those in the radiculopathy group at the 10‐year follow‐up. Segmental kyphosis and PO were detected in some patients at their last follow‐up. However, that did not affect clinical efficacy. Whether the segmental kyphosis and PO will progress and affect clinical efficacy still needs further follow‐up.
Acknowledgments
We thank the support of Beijing Jishuitan Hospital Nova Program (xkxx201614) and National Natural Science Foundation of China (11871459).
Reference
- 1. Wilson JR, Tetreault LA, Kim J, et al State of the art in degenerative cervical myelopathy: an update on current clinical evidence. Neurosurgery, 2017, 80: S33–S45. [DOI] [PubMed] [Google Scholar]
- 2. Badhiwala JH, Wilson JR. The natural history of degenerative cervical myelopathy. Neurosurg Clin N Am, 2018, 29: 21–32. [DOI] [PubMed] [Google Scholar]
- 3. Burkhardt BW, Brielmaier M, Schwerdtfeger K, Sharif S, Oertel JM. Smith‐Robinson procedure with an autologous iliac crest graft and Caspar plating: report of 65 patients with an average follow‐up of 22 years. World Neurosurg, 2016, 90: 244–250. [DOI] [PubMed] [Google Scholar]
- 4. Burkhardt BW, Brielmaier M, Schwerdtfeger K, Oertel JM. Clinical outcome following anterior cervical discectomy and fusion with and without anterior cervical plating for the treatment of cervical disc herniation‐a 25‐year follow‐up study. Neurosurg Rev, 2018, 41: 473–482. [DOI] [PubMed] [Google Scholar]
- 5. Liu N, Lu T, Wang Y, Sun Z, Li J, He X. Effects of new cage profiles on the improvement in biomechanical performance of multilevel anterior cervical Corpectomy and fusion: a finite element analysis. World Neurosurg, 2019; 129:e87–e96. [DOI] [PubMed] [Google Scholar]
- 6. Zhao X, Yuan W. Biomechanical analysis of cervical range of motion and facet contact force after a novel artificial cervical disc replacement. Am J Transl Res, 2019, 11: 3109–3115. [PMC free article] [PubMed] [Google Scholar]
- 7. Wu TK, Meng Y, Liu H, et al Biomechanical effects on the intermediate segment of noncontiguous hybrid surgery with cervical disc arthroplasty and anterior cervical discectomy and fusion: a finite element analysis. Spine J, 2019, 19: 1254–1263. [DOI] [PubMed] [Google Scholar]
- 8. Findlay C, Ayis S, Demetriades AK. Total disc replacement versus anterior cervical discectomy and fusion: a systematic review with meta‐analysis of data from a total of 3160 patients across 14 randomized controlled trials with both short‐ and medium‐ to long‐term outcomes. Bone Joint J, 2018, 100‐b: 991–1001. [DOI] [PubMed] [Google Scholar]
- 9. Chang SW, Bohl MA, Kelly BP, Wade C. The segmental distribution of cervical range of motion: a comparison of ACDF versus TDR‐C. J Clin Neurosci, 2018, 57: 185–193. [DOI] [PubMed] [Google Scholar]
- 10. Patwardhan AG, Havey RM. Prosthesis design influences segmental contribution to total cervical motion after cervical disc arthroplasty. Eur Spine J, 2019. 10.1007/s00586-019-06064-4. [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 11. Choi H, Baisden JL, Yoganandan N. A comparative in vivo study of semi‐constrained and unconstrained cervical artificial disc prosthesis. Mil Med, 2019, 184: 637–643. [DOI] [PubMed] [Google Scholar]
- 12. Turel MK, Kerolus MG, Adogwa O, Traynelis VC. Cervical arthroplasty: what does the labeling say? Neurosurg Focus, 2017, 42: E2. [DOI] [PubMed] [Google Scholar]
- 13. Xu S, Liang Y, Zhu Z, Qian Y, Liu H. Adjacent segment degeneration or disease after cervical total disc replacement: a meta‐analysis of randomized controlled trials. J Orthop Surg Res, 2018, 13: 244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Li J, Tong T, Niu R, Shen Y. A study on the clinical outcomes of patients with revision surgery for adjacent segment disease after 10‐year's anterior cervical spine surgery. J Orthop Surg Res, 2016, 11: 5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Zhu Y, Tian Z, Zhu B, Zhang W, Li Y, Zhu Q. Bryan cervical disc Arthroplasty versus anterior cervical discectomy and fusion for treatment of cervical disc diseases: a Meta‐analysis of prospective, randomized controlled trials. Spine (Phila Pa 1976), 2016, 41: E733–E741. [DOI] [PubMed] [Google Scholar]
- 16. Sasso WR, Smucker JD, Sasso MP, Sasso RC. Long‐term clinical outcomes of cervical disc Arthroplasty: a prospective, randomized, controlled trial. Spine (Phila Pa 1976), 2017, 42: 209–216. [DOI] [PubMed] [Google Scholar]
- 17. Lin GX, Rui G, Sharma S, Kotheeranurak V, Suen TK, Kim JS. Does the neck pain, function, or range of motion differ after anterior cervical fusion, cervical disc replacement, and posterior cervical foraminotomy?. World Neurosurg, 2019; 129:e485–e493. [DOI] [PubMed] [Google Scholar]
- 18. Sekhon LH. Cervical arthroplasty in the management of spondylotic myelopathy: 18‐month results. Neurosurg Focus, 2004, 17: E8. [DOI] [PubMed] [Google Scholar]
- 19. Park JH, Rhim SC, Roh SW. Mid‐term follow‐up of clinical and radiologic outcomes in cervical total disk replacement (Mobi‐C): incidence of heterotopic ossification and risk factors. J Spinal Disord Tech, 2013, 26: 141–145. [DOI] [PubMed] [Google Scholar]
- 20. Sasso RC, Smucker JD, Hacker RJ, Heller JG. Clinical outcomes of BRYAN cervical disc arthroplasty: a prospective, randomized, controlled, multicenter trial with 24‐month follow‐up. J Spinal Disord Tech, 2007, 20: 481–491. [DOI] [PubMed] [Google Scholar]
- 21. Riew KD, Buchowski JM, Sasso R, Zdeblick T, Metcalf NH, Anderson PA. Cervical disc arthroplasty compared with arthrodesis for the treatment of myelopathy. J Bone Joint Surg Am, 2008, 90: 2354–2364. [DOI] [PubMed] [Google Scholar]
- 22. Fay LY, Huang WC, Wu JC, et al Arthroplasty for cervical spondylotic myelopathy: similar results to patients with only radiculopathy at 3 years' follow‐up. J Neurosurg Spine, 2014, 21: 400–410. [DOI] [PubMed] [Google Scholar]
- 23. Khong P, Bogduk N, Ghahreman A, Davies M. Cervical disc arthroplasty for the treatment of spondylotic myelopathy and radiculopathy. J Clin Neurosci, 2013, 20: 1411–1416. [DOI] [PubMed] [Google Scholar]
- 24. Fukui M, Chiba K, Kawakami M, et al An outcome measure for patients with cervical myelopathy: Japanese orthopaedic association cervical myelopathy evaluation questionnaire (JOACMEQ): part 1. J Orthop Sci, 2007, 12: 227–240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Wu S, Ma C, Mai M, Li G. Translation and validation study of Chinese versions of the neck disability index and the neck pain and disability scale. Spine (Phila Pa 1976), 2010, 35: 1575–1579. [DOI] [PubMed] [Google Scholar]
- 26. Goffin J, Casey A, Kehr P, et al Preliminary clinical experience with the Bryan cervical disc prosthesis. Neurosurgery, 2002, 51: 840–845 discussion 845‐847. [DOI] [PubMed] [Google Scholar]
- 27. Quan GM, Vital JM, Hansen S, Pointillart V. Eight‐year clinical and radiological follow‐up of the Bryan cervical disc arthroplasty. Spine (Phila Pa 1976), 2011, 36: 639–646. [DOI] [PubMed] [Google Scholar]
- 28. Dejaegher J, Walraevens J, van Loon J, Van Calenbergh F, Demaerel P, Goffin J. 10‐year follow‐up after implantation of the Bryan cervical disc prosthesis. Eur Spine J, 2017, 26: 1191–1198. [DOI] [PubMed] [Google Scholar]
- 29. Fong SY, DuPlessis SJ, Casha S, Hurlbert RJ. Design limitations of Bryan disc arthroplasty. Spine J, 2006, 6: 233–241. [DOI] [PubMed] [Google Scholar]
- 30. Sasso RC, Metcalf NH, Hipp JA, Wharton ND, Anderson PA. Sagittal alignment after Bryan cervical arthroplasty. Spine (Phila Pa 1976), 2011, 36: 991–996. [DOI] [PubMed] [Google Scholar]
- 31. Tian W, Han X, Liu B, He D, Lv Y, Yue J. Generation and development of paravertebral ossification in cervical artificial disk replacement: a detailed analytic report using coronal reconstruction CT. Clin Spine Surg, 2017, 30: E179–e188. [DOI] [PubMed] [Google Scholar]
- 32. Tian W, Fan MX, Liu YJ, et al An analysis of paravertebral ossification in cervical artificial disc replacement: a novel classification based on computed tomography. Orthop Surg, 2016, 8: 440–446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Wu JC, Huang WC, Tu TH, et al Differences between soft‐disc herniation and spondylosis in cervical arthroplasty: CT‐documented heterotopic ossification with minimum 2 years of follow‐up. J Neurosurg Spine, 2012, 16: 163–171. [DOI] [PubMed] [Google Scholar]
- 34. Kong L, Ma Q, Meng F, Cao J, Yu K, Shen Y. The prevalence of heterotopic ossification among patients after cervical artificial disc replacement: a systematic review and meta‐analysis. Medicine (Baltimore), 2017, 96: e7163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Zhao Y, Zhang Y, Sun Y, Pan S, Zhou F, Liu Z. Application of cervical Arthroplasty with Bryan cervical disc: 10‐year follow‐up results in China. Spine (Phila Pa 1976), 2016, 41: 111–115. [DOI] [PubMed] [Google Scholar]


