Abstract
The current study aimed at investigating the association between Dietary Approach to Stop Hypertension (DASH) diet and odds of obesity phenotypes, is a cross sectional study conducted on 3218 Iranian overweight or obese participants (BMI >25 kg/m2), aged ≥20 years, who participated in the fourth phase (2009–2011) of the Tehran Lipid and Glucose Study. Using a valid and reliable food-frequency questionnaire, DASH diet scores between 8 and 40 points were determined. Obesity phenotypes including metabolic unhealthy obesity (MUHO) and metabolic healthy obesity (MHO) were defined using criteria of the Joint International statement(JIS) for metabolic syndrome. Multivariable logistic regression was used to determine the odds ratio (OR) for obesity phenotypes according to the tertiles of the DASH diet. Mean ± SD age of participants (43.5% male) was 39.2 ± 9.5 years and median (25–75 interquartile range) DASH diet score was 24 (21–27); percentages of MHO and MUHO subjects were 33.4 and 66.6%, respectively. In the multivariable adjusted model, after controlling for age, sex, BMI, physical activity, smoking status, socioeconomic status, and energy intake, participants in the highest tertile of DASH diet had lower odds of MUHO (OR:0.79;95%CI:0.64–0.98), in comparison to those in the lowest one (P for trend = 0.040). Our findings indicate that adherence to DASH diet may be favourable in prevention of metabolic abnormalities in overweight and obese individuals.
Subject terms: Obesity, Nutrition
Introduction
Obesity represents a rapidly growing public health problem worldwide over the last few decades1. Epidemiological studies have shown that combinations of obesity and metabolic abnormalities lead to increased risk of chronic diseses, such as diabetes, cardiovascular diseases (CVD), and all-cause mortality2,3. Recently, it has been shown that even individuals in the same body mass index category can have different levels of metabolic components, including lipid profiles, blood glucose, blood pressure, and waist circumference3. Among obese individuals, two phenotypes, including subjects with normal metabolic characteristics as the metabolically healthy obese (MHO) phenotype, and those with metabolically unhealthy status as the metabolically unhealthy obese (MUHO) phenotypes have been defined4,5, the long-term health outcomes of the MHO and MUHO phenotypes are still not fully understood6; one study reported that both metabolically healthy and unhealthy obese individuals are faced with increased risk of CVD and mortality7; however, the Hamer et al. study indicates that compared with the metabolically healthy nonobese participants, MHO was not associated with increased risk of CVD and all cause mortality8. Also, some evidence shows that the metabolically unhealthy obese phenotype had higher risk of chronic diseases, compared to the healthy one9.
Dietary patterns along with physical activity are important environmental factors that contribute to the progression of obesity and metabolic disorders10,11. Considering that meals, include a wide variety of foods with various mixtures of nutrients, which may have interactive effects, investigating dietary patterns is essential for providing valuable information, beyond individual nutrients or food groups12. The Dietary Approach to Stop Hypertension (DASH) diet, a dietary pattern, currently receiving much attention, was originally designed to reduce blood pressure13; this diet emphasizes intakes of fruits, vegetables, whole grains, nuts, legumes, moderate amounts of low-fat dairy; and underscores reduced intakes of red or processed meats, sodium, and sweetened beverages13.
Some studies with controversial results have explored the association between healthy diet indices such as DASH diet, Mediterranean diet, and food pyramid compliance with odds of obesity phenotypes14,15; although greater adherence to the Mediterranean was positively associated with MHO, compared to MUHO, and higher adherence to DASH diet score was related with lower odds of metabolically unhealthy normal weight phenotype in comparison to metabolically healthy normal weight younger adults, no significant association of Mediterranean diet and DASH index with obesity phenotypes was found in the elderly15. It has been reported that higher compliance to food pyramid recommendations but not DASH score is favorably related to MHO14. Since prevention of obesity-related cardiometabolic diseases is an enormous medical and socioeconomic task, and extremely important in terms of cost effectiveness16, the determination and assessment of enviromental factors such as dietary patterns which protect obese individuals against obesity-related metabolic diseases is vital. We therefore aim to investigate associations of higher adherence to the DASH diet with metabolically healthy and unhealthy obesity phenotypes among an Iranian population.
Materials and Methods
Subjects
The current study was conducted within the framework of the Tehran Lipid and Glucose Study (TLGS), a population-based prospective study, aimed at determining the risk factors for non-communicable diseases among a representative urban population of Tehran, including 15005 participants, aged ≥3 years. The first survey of TLGS began in 1999 and data collection, conducted at 3-year intervals, is ongoing. The baseline survey was a cross-sectional study, and surveys II, III, IV, and V were prospective follow-up surveys17,18.
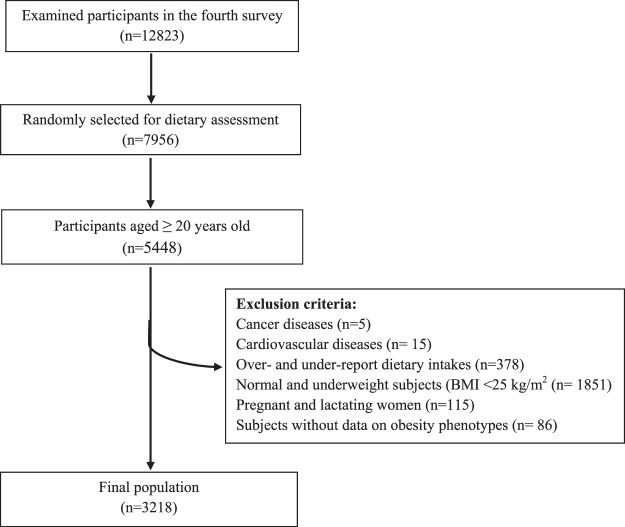
In the fourth survey of the TLGS (2009–2011), from among 12823 participants, 7956 randomly selected subjects, agreed to complete dietary assessment. For the present study, of 5448 individuals, aged ≥20 years, after exclusion of normal and underweight subjects (BMI <25 kg/m2; n = 1851), those with prevalent cancer (n = 5), cardiovascular diseases (n = 15), pregnant and lactating women (n = 115), participants with under- or over-reported dietary intakes below 800 kcal/d or above 4200 kcal/d, respectively (n = 378), and those without data on obesity phenotypes (n = 86), 3218 participants were finally enrolled in the study, some of whom fell into more than one category (Fig. 1).
Figure 1.
Flow chart of the Tehran Lipid and Glucose Study (TLGS) participants.
Written informed consents were obtained from all participants and the study protocol was reviewed and approved by the ethics research council of the Research Institute for Endocrine Sciences, Shahid Beheshti University of Medical Sciences. The study was performed in accordance with the Declaration of Helsinki as well as our institutional guidelines.
Measurements
Details of the study method and measurements have been reported previously18–21. Dietary data over the previous year were collected using a valid and reliable semi-quantitative food frequency questionnaire at baseline22. Trained dieticians asked participants to designate their consumption frequency for each food item during the previous year on a daily, weekly or monthly basis; portion sizes of consumed foods, reported in household measures, were then converted to grams21. DASH diet score in the Fung et al. study23 was determined based on eight components, i.e. higher intakes of whole grains, fruits, vegetables, legumes and nuts, and low-fat dairy and lower intakes of red or processed meats, sodium, and sweetened beverages. The intake of each food component was energy adjusted (g/1000 kcal) and then categorized into quintiles. Subject’s quintile rankings were used for whole grains, fruits, vegetables, legumes and nuts, and low-fat dairy to determine component scores, e.g. participants in the lowest quintile were recieved 1 point, and those in the highest one were recieved 5 points. For sodium, red and processed meats and sugar-sweetened beverages, those in the lowest quintile were assigned 5 points, and those in the highest one were assigned 1 point. We then summed up the scores for all the eight components to compute the DASH score. Thus, the total DASH score ranged from 8 (minimum adherence) to 40 (maximal adherence).
A trained interviewer used a pretested questionnaire to collect data on age, sex, medical history, medication use, and smoking habits. Smoking status was defined as nonsmoker and smoker (ex-smoker, current or occasionally). Education level was categorized based on years of education (≤12 years, >12 years). To collect physical activity, we used the Modifiable Activity Questionnaire (MAQ), which has been previously modified and validated among Iranians24. The participant’s weight, height, waist circumference (WC), systolic blood pressure (SBP), and diastolic blood pressure (DBP) were measured based on standard protocols as previously described19,21. Body mass index was computed as weight (kg) divided by height (m2). A blood sample was taken at the TLGS research laboratory in a sitting position after 12–14 h of overnight fasting according to the standard protocol to measure fasting plasma glucose (FPG), triglyceride (TG), total cholesterol (TC), high density lipoprotein cholesterol (HDL-C), and low density lipoprotein cholesterol (LDL-C)19,20.
Definitions
Obesity phenotypes, including MUHO and MHO were defined based on the Joint Interim Statement (JIS) criteria for metabolic syndrome (MetS)25. Participants were considered as having MUHO if they had ≥2 of the following: WC ≥ 91 cm in women and ≥89 cm in men26; FPG ≥ 100 mg/dl or drug treatment; fasting TGs ≥ 150 mg/dl or drug treatment; fasting HDL-C <50 mg/dl in women and <40 mg/dl in men or drug treatment; raised blood pressure defined as SBP ≥ 130 mmHg/DBP ≥ 85 mmHg or antihypertensive drug treatment. Those who had ≤1 component were categorized as MHO.
Statistical analyses
Data analysis was performed using the SPSS software (Statistical Package for the Social Sciences, version 15.0, SPSS Inc, Chicago, IL, USA). Distribution of variables was checked using histogram chart and the Kolmogorov-Smirnov’s test. Participants were categorized according to tertiles of DASH diet score cutoff points (≤22, 23–26, and ≥27). Baseline characteristics of participants are expressed as mean ± SD or median (25–75 interquartile range) for continuous variables, and percentages for categorical variables across tertiles of DASH score. We have used linear regression and Chi square to test the trend of continuous and dichotomous variables across tertiles of DASH score, respectively, and P for trend was reported. Odds of MUHO in comparison to reference category (MHO) across tertiles of DASH score was assessed using logistic regression models, adjusted for potential confounders including age, sex, BMI, physical activity, smoking status, dietary energy intake, and education level. We also analyzed the association of DASH score as a continuous variable with odds of MUHO in our population. Odds ratio (OR) and 95% confidence interval (CI) were reported, and P-values < 0.05 were considered statistically significant.
Results
The mean ± SD age of participants (43.5% male) was 39.2 ± 9.5 years and median (25–75 interquartile range) of the DASH diet score was 24 (21–27). Percentages of MHO and MUHO were 33.4 and 66.6%, respectively.
General characteristics of the study population across tertiles of DASH diet score are presented in Table 1. Participants in the highest DASH diet tertile were more likely to be female, older, have higher physical activaty and HDL-C concentration, and less likely to be smokers, compared to those in the lowest one (P < 0.05). There were no significant differences in any other demographic, anthropometric, and biochemical measures across tertiles of DASH diet scores.
Table 1.
Characteristics of participants across tertiles of DASH diet score in 3218 participants of the Tehran Lipid and Glucose Study.
| Characteristics | Tertiles of DASH score | P value* | ||
|---|---|---|---|---|
| Tertile 1 (n = 1220) | Tertile 2 (n = 1070) | Tertile 3 (n = 928) | ||
| Age (years) | 37.3 ± 9.0 | 39.6 ± 8.8 | 41.2 ± 8.9 | <0.001 |
| Men (%) | 50.7 | 44.1 | 33.4 | <0.001 |
| Body mass index (kg/m2) | 29.5 ± 3.7 | 29.5 ± 3.9 | 29.7 ± 3.7 | 0.139 |
| Smoking (%) | 15.4 | 10.5 | 8.8 | <0.001 |
| Physical activity (Met-h/day) | 74.8 (41.6–107.0) | 70.7 (38.7–99.8) | 62.7 (33.7–98.1) | <0.001 |
| Waist circumference (cm) | 97.4 ± 10.1 | 96.8 ± 9.9 | 96.7 ± 9.7 | 0.074 |
| Fasting blood glucose (mg/dl) | 96.2 ± 19.0 | 98.0 ± 22.5 | 98.0 ± 26.1 | 0.072 |
| Triglycerides (mg/dl) | 151.8 ± 87.9 | 161.0 ± 164.4 | 148.8 ± 87.9 | 0.573 |
| HDL- cholesterol (mg/dl) | 44.9 ± 10.6 | 45.8 ± 10.9 | 47.1 ± 11.4 | <0.001 |
| Systolic blood pressure (mmHg) | 113.7 ± 14.0 | 114.4 ± 14.1 | 113.4 ± 14.3 | 0.674 |
| Diastolic blood pressure (mmHg) | 77.4 ± 10.1 | 78.2 ± 10.9 | 77.1 ± 10.8 | 0.529 |
| Education level (>12 years) (%) | 27.7 | 29.3 | 28.7 | 0.351 |
Data are presented as mean ± standard deviation or median (interquartile range) and as percentage.
*Significant differences (p < 0.05) was obtained using chi square for categorical variables and linear regression for continuous variables.
Dietary intakes of participants according to DASH diet score are shown in Table 2; participants in the highest tertile of DASH diet score had higher intakes of vegetables, whole grain, fruits, nuts and legumes, and low-fat dairy, but lower intakes of sweetened beverages and red and processed meat. Dietary intakes of total energy, carbohydrates, proteins, fiber, folate, potassium, and calcium were significantly increased across DASH diet tertiles (P < 0.001), whereas intakes of total fat, saturated fat, monounsaturated fat, polyunsaturated fat, and sodium were decreased (P < 0.001).
Table 2.
Dietary nutrients and food group intake across tertiles of DASH diet score in 3218 participants of the Tehran Lipid and Glucose Study.
| Nutrient and food groups | Tertiles of DASH score | P for trend | ||
|---|---|---|---|---|
| Tertile 1 (n = 1220) | Tertile 2 (n = 1070) | Tertile 3 (n = 928) | ||
| DASH score (median) | 20.0 | 24.0 | 29.0 | |
| Vegetables (g/1000 Kcal) | 112.2 ± 60.0 | 147.1 ± 80.4 | 192.8 ± 108.9 | <0.001 |
| Fruits (g/1000 Kcal) | 117.5 ± 101.1 | 162.6 ± 114.7 | 229.3 ± 151.6 | <0.001 |
| Whole grains (g/1000 Kcal) | 52.3 ± 41.6 | 60.9 ± 41.4 | 62.7 ± 38.8 | <0.001 |
| Nuts and legumes (g/1000 Kcal) | 17.8 ± 13.2 | 21.7 ± 14.4 | 27.6 ± 18.6 | <0.001 |
| Low-fat dairy (g/1000 Kcal) | 83.7 ± 68.7 | 112.4 ± 81.1 | 132.6 ± 86.1 | <0.001 |
| sweetened beverages (g/1000 Kcal) | 19.3 (8.1–83.0) | 9.5 (3.5–19.8) | 4.1 (0.77–11.3) | <0.001 |
| Red and processed meat (g/1000 Kcal) | 12.2 ± 8.6 | 8.9 ± 6.3 | 6.8 ± 6.0 | <0.001 |
| Total energy (kcal/day) | 2292 ± 697 | 2430 ± 728 | 2585 ± 701 | <0.001 |
| Carbohydrates (% of energy) | 57.5 ± 6.6 | 58.3 ± 6.4 | 60.3 ± 12.8 | <0.001 |
| Proteins (% of energy) | 14.4 ± 3.1 | 15.0 ± 3.3 | 15.7 ± 12.9 | <0.001 |
| Fat (% of energy) | 30.8 ± 6.5 | 30.3 ± 5.9 | 29.0 ± 5.7 | <0.001 |
| Saturated fat (% of energy) | 10.0 ± 2.8 | 9.9 ± 2.5 | 9.4 ± 2.7 | <0.001 |
| Monounsaturated fat (% of energy) | 10.4 ± 3.0 | 10.1 ± 2.5 | 9.6 ± 3.1 | <0.001 |
| Polyunsaturated fat(% of energy) | 6.2 ± 2.0 | 6.0 ± 1.9 | 5.8 ± 2.4 | <0.001 |
| Dietary fiber (g/1000Kcal) | 18.1 ± 7.0 | 19.5 ± 6.3 | 21.4 ± 6.1 | <0.001 |
| Folate (µg/1000Kcal) | 245 ± 43 | 251 ± 40 | 259 ± 42 | <0.001 |
| Sodium (mg/1000Kcal) | 1559 ± 459 | 1525 ± 393 | 1430 ± 362 | <0.001 |
| Potassium (mg/1000 kcal) | 1677 ± 415 | 1977 ± 488 | 2265 ± 532 | <0.001 |
| Calcium (mg/1000Kcal) | 547 ± 167 | 637 ± 196 | 689 ± 204 | <0.001 |
Data values are mean ± SD or median (interquartile range).
The ORs (95% CI) of MUHO across tertile categories of DASH diet score are presented in Table 3. In the age and sex-adjusted model, the odds of MUHO in the third tertile of DASH diet score was 0.85 (95% CI: 0.69–1.04; P for trend = 0.128). After additional adjustment for energy intake, physical activity, smoking, BMI, and education level, the odds of MUHO in the highest, compared to the lowest DASH diet score category, decreased by 21% (OR: 0.79, 95% CI: 0.64–0.98; P for trend = 0.040). Also, we investigated the association of DASH score as a continuous variable with odds of obesity phenotypes in our population, and the statistical significance of findings was attenuated: the odds of MUHO, in comparison to MHO, based on one score change in the DASH diet was small (OR: 0.91, 95% CI: 0.85–1.01; P for trend = 0.100), (Table 4).
Table 3.
Multivariable-adjusted odds ratios (and 95% CIs) for obesity phenotype (MHO in comparison to MUHO) across tertiles of DASH score in 3218 participants of the Tehran Lipid and Glucose Study.
| Characteristics | Tertiles of DASH score | P trend | ||
|---|---|---|---|---|
| T1(lowest) | T2 | T3(highest) | ||
| MUHO/Total population | 815/1220 | 728/1070 | 599/928 | |
| Model 1* | 1.00 (Ref) | 0.86 (0.72–1.03) | 0.86 (0.72–1.03) | 0.119 |
| Model 2† | 1.00 (Ref) | 0.86 (0.70–1.04) | 0.85 (0.69–1.04) | 0.128 |
| Model 3‡ | 1.00 (Ref) | 0.86 (0.70–1.06) | 0.79 (0.64–0.98) | 0.040 |
*Crude model.
†Adjusted for age and sex.
‡Additionally adjusted for dietary energy intake, physical activity, smoking, body mass index, and education level.
MHO: Metabolically healthy obese; MUHO: Metabolically unhealthy obese
Table 4.
Multivariable-adjusted odds ratios (and 95% CIs) for obesity phenotype per each score increase in the DASH score in 3218 participants of the Tehran Lipid and Glucose Study.
| Characteristics | per each score increase in the DASH score | P value |
|---|---|---|
| OR (95% CI) | ||
| Model 1* | 0.97 (0.90–1.07) | 0.503 |
| Model 2† | 0.96 (0.88–1.04) | 0.347 |
| Model 3‡ | 0.91 (0.85–1.01) | 0.100 |
*Crude model.
†Adjusted for age and sex.
‡Additionally adjusted for dietary energy intake, physical activity, smoking, body mass index, and educational level.
Discussion
In this cross- sectional study, conducted on an adult Tehranian population, we found that, compared to MHO, greater adherence to the DASH diet was associated with 21% lower odds of MUHO, independent of age, sex, energy intake, physical activity, BMI, smoking, and educational level. Considering that the current study has been conducted on a large sample of Tehranian adults population, our findings on positive associaion of DASH diet with healthy metabolic status are potentially generalizable to the Iranian adult population.
In the current study, the association of DASH score as a continuous variable has been assessed with odds of obesity phenotypes in our population. Considering that the DASH score is a discrete variable with a narrow range between 8–40 (the range of this score in our population was from 9 to 37). When we analyzed the DASH score as a continuous variable, the statistical significance of findings was attenuated and our results no longer remained significant. It should be noted that in the epidemiological studies, variation in the exposure variable among the study population is so important and for simplicity of interpretation of results and their clinical applicability, studies mainly focus on high and poor quality diet, which can be attained by categorizing the exposure variable. Therefore, similar to more than 90% of other nutritional studies, we categorized DASH score in to tertiles in addition to the using it as a continuous variable. Categorizing DASH diet is helpful to determine more considerable associations with metabolic health status in obese participants.
Previously, the DASH-style diet, Mediterranean diet, healthy eating index (HEI), and food pyramid recommendation scores have been assessed with metabolic status in obese individuals and controversial findings were reported14,15,27. The Camhi et al. study indicates that HEI significantly differed between MHO and MUHO phenotypes among women aged 19–44 years; however, no significant difference was observed among men and elderly women27. Phillips et al. revealed that greater adherence to Irish food pyramid recommendations was positively related to metabolic health in MHO participants14; however, no significant association of DASH score with metabolic health was observed among obese participants15. Park et al. study15 indicate that greater adherence to DASH style diet plays favourable role in reducing metabolic abnormalities in normal weight individuals, findings observed among younger participants, not older ones; however, we found significant association between DASH diet and metabolic status in obese participants aged ≥ 20 years.
Although, limited studies have been conducted on the association of DASH diet with obesity or metabolic abnormalities, their results are in agreement to those of ours28,29. In the Saneei et al. study, adherence to the DASH diet was inversely related to metabolic abnormalities including central obesity, hypertriglyceridemia, high blood pressure, and low HDL-C concentration29. Similarly, Azadbakht et al. showed that higher adherence to the DASH diet was inversely associated with an unhealthy metabolic status28. It has been reported that obese individuals can have different levels of metabolic components, such as lipid profiles, glucose tolerance, blood pressure, and waist circumference3, heterogeneity in which various factors such as dietary patterns can play important role. Therefore, we examined participants in terms of metabolic disorders as well as overweight and obesity, based on a standard definition in two groups, the MHO and MUHO, and findings showed the DASH diet to be inversely associated with unhealthy metabolic status in overweight and obese individuals. The DASH style diet emphasizes increased intakes of fruits, vegetables, whole grains, nuts and legumes, low-fat dairy, and dietary fiber, and reduced intakes of red meat and sugar-sweetened beverages, all of which are closely associated with decrease in risk of metabolic abnormalities30–35. In the Yoo et al. study, individuals with higher intakes of fruit and vegetables had lower prevalence of MetS34. Similarly, it has been shown that higher intakes of whole grain, nuts, total fiber, fruit fiber, and legume fiber decreases the risk of metabolic abnormalities31,35. Furthermore, some studies have shown inverse associations of dairy products and calcium intakes with MetS30,33. Evidence shows the association of red meat and sugar-sweetened beverages with risk of metabolic abnormalities and inflammation36,37.
Although it is not clear how the DASH diet may modulate the odds of MHO, potential mechanisms linking DASH diet or its components with metabolic abnormalities have been previously reported30,38–40. It is suggested that high dietary fibre attenuates indicators of metabolic abnormalities such as FPG, TGs, BP and WC38; another mechanism suggested is the higher intakes of low-fat dairy via the effects of calcium on insulin sensitivity, WC, BP, and lipid profiles30,40. Also, the DASH dietry pattern contains high levels of potassium, magnesium, vitamin C, and phytochemicals, which reduce the risk of insulin resistance, obesity, and MetS39.
The current study has several strengths. This study is the first large size population-based study to examine the association between DASH diet and different phenotypes of obesity in the Middle East and North Africa (MENA) region. In the current study, we also used valid and reliable food-frequency and physical activity questionnaires for the population. However, our study does have some limitations. The cross-sectional nature of the study limited us from establishing a cause and effect relation between DASH diet and obesity phenotypes. Also, despite adjusting for the confounding role of various variables in our analysis, residual confounding due to unknown or unmeasured confounders, such as socioeconomic status cannot be excluded.
Our findings show that DASH diet score may be associated with decreased the odds of MUHO in overweight and obese individuals, indicating that greater adherence to the DASH-style dietary pattern was related to better metabolic profiles. However, to fully determine the association of DASH diet with obesity phenotype, further observational and interventional studies are needed to address the role of DASH-style diet in the development of obesity phenotypes and its potential mechanisms
Acknowledgements
This work was supported by a grant from the National Institute for Medical Research Development (NIMAD) (Project No. 963460), Tehran, Iran.We express our appreciation to the participants in the Tehran Lipid and Glucose Study for their enthusiastic support and to the staff of the Research Institute for Endocrine Sciences, Tehran Lipid and Glucose Study Unit for their valuable help. We also wish to acknowledge Ms Shiva for critical editing of the English grammar and syntax of the manuscript.
Author contributions
H.F., G.A. and F.T. contributed in conception, design, statistical analysis. H.F., M.D. and G.A. contributed in data collection and manuscript drafting. P.M. and F.A. supervised the study. All authors approved the final version of the manuscript.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Doustmohamadian S, et al. Risk of all-cause mortality in abdominal obesity phenotypes: Tehran Lipid and Glucose Study. Nutrition, Metabolism and Cardiovascular Diseases. 2017;27:241–248. doi: 10.1016/j.numecd.2016.11.123. [DOI] [PubMed] [Google Scholar]
- 2.Field AE, et al. Impact of overweight on the risk of developing common chronic diseases during a 10-year period. Archives of internal medicine. 2001;161:1581–1586. doi: 10.1001/archinte.161.13.1581. [DOI] [PubMed] [Google Scholar]
- 3.Kramer CK, Zinman B, Retnakaran R. Are metabolically healthy overweight and obesity benign conditions?: A systematic review and meta-analysis. Annals of internal medicine. 2013;159:758–769. doi: 10.7326/0003-4819-159-11-201312030-00008. [DOI] [PubMed] [Google Scholar]
- 4.Eftekharzadeh A, et al. Predictors of incident obesity phenotype in nonobese healthy adults. European Journal of Clinical Investigation. 2017;47:357–365. doi: 10.1111/eci.12743. [DOI] [PubMed] [Google Scholar]
- 5.Mirzaei B, et al. Cardiovascular risk in different obesity phenotypes over a decade follow-up: Tehran Lipid and Glucose Study. Atherosclerosis. 2017;258:65–71. doi: 10.1016/j.atherosclerosis.2017.02.002. [DOI] [PubMed] [Google Scholar]
- 6.Eckel N, Meidtner K, Kalle-Uhlmann T, Stefan N, Schulze MB. Metabolically healthy obesity and cardiovascular events: A systematic review and meta-analysis. European journal of preventive cardiology. 2016;23:956–966. doi: 10.1177/2047487315623884. [DOI] [PubMed] [Google Scholar]
- 7.Hinnouho G-M, et al. Metabolically healthy obesity and risk of mortality: does the definition of metabolic health matter? Diabetes care. 2013;36:2294–2300. doi: 10.2337/dc12-1654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hamer M, Stamatakis E. Metabolically healthy obesity and risk of all-cause and cardiovascular disease mortality. The Journal of clinical endocrinology and metabolism. 2012;97:2482–2488. doi: 10.1210/jc.2011-3475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rhee EJ, et al. Metabolic health is a more important determinant for diabetes development than simple obesity: a 4-year retrospective longitudinal study. PLoS One. 2014;9:e98369. doi: 10.1371/journal.pone.0098369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mirmiran P, et al. Low carbohydrate diet is associated with reduced risk of metabolic syndrome in Tehranian adults. International journal of food sciences and nutrition. 2017;68:358–365. doi: 10.1080/09637486.2016.1242119. [DOI] [PubMed] [Google Scholar]
- 11.Frank LD, Andresen MA, Schmid TL. Obesity relationships with community design, physical activity, and time spent in cars. American journal of preventive medicine. 2004;27:87–96. doi: 10.1016/j.amepre.2004.04.011. [DOI] [PubMed] [Google Scholar]
- 12.Hu FB. Dietary pattern analysis: a new direction in nutritional epidemiology. Current opinion in lipidology. 2002;13:3–9. doi: 10.1097/00041433-200202000-00002. [DOI] [PubMed] [Google Scholar]
- 13.Windhauser MM, et al. Translating the Dietary Approaches to Stop Hypertension diet from research to practice: dietary and behavior change techniques. Journal of the American Dietetic Association. 1999;99:S90–S95. doi: 10.1016/S0002-8223(99)00422-8. [DOI] [PubMed] [Google Scholar]
- 14.Phillips CM, et al. Defining metabolically healthy obesity: role of dietary and lifestyle factors. PLoS One. 2013;8:e76188–e76188. doi: 10.1371/journal.pone.0076188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Park Y-MM, et al. Mediterranean diet, Dietary Approaches to Stop Hypertension (DASH) style diet, and metabolic health in U.S. adults. Clinical Nutrition. 2017;36:1301–1309. doi: 10.1016/j.clnu.2016.08.018. [DOI] [PubMed] [Google Scholar]
- 16.Bluher M. Are there still healthy obese patients? Current opinion in endocrinology, diabetes, and obesity. 2012;19:341–346. doi: 10.1097/MED.0b013e328357f0a3. [DOI] [PubMed] [Google Scholar]
- 17.Azizi F, et al. Prevention of non-communicable disease in a population in nutrition transition: Tehran Lipid and Glucose Study phase II. Trials. 2009;10:5–5. doi: 10.1186/1745-6215-10-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Teymoori F, et al. Are dietary amino acids prospectively predicts changes in serum lipid profile? Diabetes & metabolic syndrome. 2019;13:1837–1843. doi: 10.1016/j.dsx.2019.04.013. [DOI] [PubMed] [Google Scholar]
- 19.Asghari G, et al. Adherence to the Mediterranean diet is associated with reduced risk of incident chronic kidney diseases among Tehranian adults. Hypertension research: official journal of the Japanese Society of Hypertension. 2017;40:96–102. doi: 10.1038/hr.2016.98. [DOI] [PubMed] [Google Scholar]
- 20.Farhadnejad H, Asghari G, Emamat H, Mirmiran P, Azizi F. Low-Carbohydrate High-Protein Diet is Associated With Increased Risk of Incident Chronic Kidney Diseases Among Tehranian Adults. Journal of renal nutrition: the official journal of the Council on Renal Nutrition of the National Kidney Foundation. 2019;29:343–349. doi: 10.1053/j.jrn.2018.10.007. [DOI] [PubMed] [Google Scholar]
- 21.Farhadnejad H, Asghari G, Mirmiran P, Azizi F. Dietary approach to stop hypertension diet and cardiovascular risk factors among 10- to 18-year-old individuals. Pediatric obesity. 2018;13:185–194. doi: 10.1111/ijpo.12268. [DOI] [PubMed] [Google Scholar]
- 22.Asghari G, et al. Reliability, comparative validity and stability of dietary patterns derived from an FFQ in the Tehran Lipid and Glucose Study. The British journal of nutrition. 2012;108:1109–1117. doi: 10.1017/s0007114511006313. [DOI] [PubMed] [Google Scholar]
- 23.Fung TT, et al. Adherence to a DASH-style diet and risk of coronary heart disease and stroke in women. Archives of internal medicine. 2008;168:713–720. doi: 10.1001/archinte.168.7.713. [DOI] [PubMed] [Google Scholar]
- 24.Momenan, A. A. et al. Reliability and validity of the Modifiable Activity Questionnaire (MAQ) in an Iranian urban adult population. Arch Iran Med15, 279–282, 012155/aim.007 (2012). [PubMed]
- 25.Alberti KG, et al. Harmonizing the metabolic syndrome: a joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation. 2009;120:1640–1645. doi: 10.1161/circulationaha.109.192644. [DOI] [PubMed] [Google Scholar]
- 26.Delavari A, Forouzanfar MH, Alikhani S, Sharifian A, Kelishadi R. First Nationwide Study of the Prevalence of the Metabolic Syndrome and Optimal Cutoff Points of Waist Circumference in the Middle East: The National Survey of Risk Factors for Noncommunicable Diseases of Iran. Diabetes Care. 2009;32:1092–1097. doi: 10.2337/dc08-1800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Camhi SM, Whitney Evans E, Hayman LL, Lichtenstein AH, Must A. Healthy eating index and metabolically healthy obesity in U.S. adolescents and adults. Preventive Medicine. 2015;77:23–27. doi: 10.1016/j.ypmed.2015.04.023. [DOI] [PubMed] [Google Scholar]
- 28.Azadbakht L, Mirmiran P, Esmaillzadeh A, Azizi T, Azizi F. Beneficial effects of a Dietary Approaches to Stop Hypertension eating plan on features of the metabolic syndrome. Diabetes care. 2005;28:2823–2831. doi: 10.2337/diacare.28.12.2823. [DOI] [PubMed] [Google Scholar]
- 29.Saneei P, et al. Adherence to the DASH diet and prevalence of the metabolic syndrome among Iranian women. European journal of nutrition. 2015;54:421–428. doi: 10.1007/s00394-014-0723-y. [DOI] [PubMed] [Google Scholar]
- 30.Azadbakht L, Mirmiran P, Esmaillzadeh A, Azizi F. Dairy consumption is inversely associated with the prevalence of the metabolic syndrome in Tehranian adults. The American journal of clinical nutrition. 2005;82:523–530. doi: 10.1093/ajcn.82.3.523. [DOI] [PubMed] [Google Scholar]
- 31.Hosseinpour-Niazi S, Mirmiran P, Sohrab G, Hosseini-Esfahani F, Azizi F. Inverse association between fruit, legume, and cereal fiber and the risk of metabolic syndrome: Tehran Lipid and Glucose Study. Diabetes research and clinical practice. 2011;94:276–283. doi: 10.1016/j.diabres.2011.07.020. [DOI] [PubMed] [Google Scholar]
- 32.Ibarrola-Jurado N, et al. Cross-sectional assessment of nut consumption and obesity, metabolic syndrome and other cardiometabolic risk factors: the PREDIMED study. PloS one. 2013;8:e57367. doi: 10.1371/journal.pone.0057367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Liu S, et al. Dietary calcium, vitamin D, and the prevalence of metabolic syndrome in middle-aged and older U.S. women. Diabetes care. 2005;28:2926–2932. doi: 10.2337/diacare.28.12.2926. [DOI] [PubMed] [Google Scholar]
- 34.Yoo S, et al. Comparison of dietary intakes associated with metabolic syndrome risk factors in young adults: the Bogalusa Heart Study. The American journal of clinical nutrition. 2004;80:841–848. doi: 10.1093/ajcn/80.4.841. [DOI] [PubMed] [Google Scholar]
- 35.Suliga E, Kozieł D, Cieśla E, Głuszek S. Association between dietary patterns and metabolic syndrome in individuals with normal weight: a cross-sectional study. Nutrition Journal. 2015;14:55. doi: 10.1186/s12937-015-0045-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Micha R, Wallace SK, Mozaffarian D. Red and processed meat consumption and risk of incident coronary heart disease, stroke, and diabetes mellitus: a systematic review and meta-analysis. Circulation. 2010;121:2271–2283. doi: 10.1161/CIRCULATIONAHA.109.924977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Malik, V. S. et al. Sugar sweetened beverages and risk of metabolic syndrome and type 2 diabetes: a meta-analysis. Diabetes care (2010). [DOI] [PMC free article] [PubMed]
- 38.Papathanasopoulos A, Camilleri M. Dietary fiber supplements: effects in obesity and metabolic syndrome and relationship to gastrointestinal functions. Gastroenterology. 2010;138(65-72):e61–62. doi: 10.1053/j.gastro.2009.11.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Most MM. Estimated phytochemical content of the dietary approaches to stop hypertension (DASH) diet is higher than in the Control Study Diet. Journal of the American Dietetic Association. 2004;104:1725–1727. doi: 10.1016/j.jada.2004.08.001. [DOI] [PubMed] [Google Scholar]
- 40.van Meijl LE, Vrolix R, Mensink RP. Dairy product consumption and the metabolic syndrome. Nutrition research reviews. 2008;21:148–157. doi: 10.1017/s0954422408116997. [DOI] [PubMed] [Google Scholar]