Abstract
Heterotopic ossification (HO) is a debilitating condition characterized by the pathologic formation of ectopic bone. HO occurs commonly following orthopedic surgeries, burns, and neurologic injuries. While surgical excision may provide palliation, the procedure is often burdened with significant intra-operative blood loss due to a more robust contribution of blood supply to the pathologic bone than to native bone. Based on these clinical observations, we set out to examine the role of vascular signaling in HO. Vascular endothelial growth factor A (VEGFA) has previously been shown to be a crucial pro-angiogenic and pro-osteogenic cue during normal bone development and homeostasis. Our findings, using a validated mouse model of HO, demonstrate that HO lesions are highly vascular, and that VEGFA is critical to ectopic bone formation, despite lacking a contribution of endothelial cells within the developing anlagen.
Subject terms: Bone, Pathogenesis
Introduction
Pathology from excess ectopic bone formation following musculoskeletal injury, or trauma-induced heterotopic ossification (HO), presents a substantial barrier to recovery in 20% of patients with hip replacements, musculoskeletal trauma, neurologic injury, and blast/burn injuries.1,2 Patients with HO experience substantive morbidity including chronic pain, restricted joint function, and open wounds. Effective therapeutics are lacking in contemporary medicine aside from surgical excision. However, these procedures can fail to completely reverse the joint contractures and restricted range of motion.3 Furthermore, even after a successful excision procedure, recurrence may occur via similar cellular mechanisms as observed in HO from the incident trauma.4–6
While the etiologies of HO are diverse, it often follows a predictable progression of endochondral ossification7–10 after acute inflammatory insult with proliferation of progenitor populations of multipotent mesenchymal stromal cells (MSCs),11–13 chondrogenesis, angiogenesis, and ossification7 resulting in highly vascular regions surrounding the HO.14 These observations parallel programming seen in normal developing bone and fracture healing, suggesting overlapping pathways between developing bone and posttraumatic HO such as the intimate coupling of vascular invasion and osteogenesis.15 Previous studies have further demonstrated MSCs differentiating into a cartilaginous scaffold and supportive matrix,16 forming a hypoxic environment responsible for the upregulation of HIF1a and VEGFA.17–19 During normal bone formation, VEGFA facilitates co-invasion of this anlagen by neovasculature and Osterix(Osx)-expressing osteoblast precursors,16 with increased delivery of oxygen to support growing metabolic activity.20 Similar migratory behavior to primary ossification centers by osteoblast precursors was observed in response to VEGFA secreted by chondrocytes.21 Disruption of these processes lead to impaired endochondral ossification.8,22 Notably, mice with conditional deletion of VEGFA in Col2a expressing cells demonstrate aberrations in cartilage development and increased chondrocyte apoptosis.13,23 The role of VEGFA as a pro-angiogenic/osteogenic signal24–26 fundamental to bone development and homeostasis27 highlights a promising candidate for uncoupling acute injury and ectopic bone formation. Though previous studies have demonstrated the role of endothelial progenitors and VEGFA28 in bone development and in a nontraumatic HO model, previous work did not identify the role of mesenchymal-derived VEGFA in traumatic HO.
Acute posttraumatic inflammation stimulates local13,29 and recruited MSCs to secrete a collection of soluble factors30,31 including VEGFA.32 However, MSCs have been well demonstrated to be a heterogeneous population13 and thus the true lineage and source of these progenitor cells have remained unclear. Various origins have been proposed for the progenitor cells responsible for HO including Tie2/vWF/VeCadherin-positive endothelium,33 Prx1/Mx-1/PDGFRα-positive muscle interstitial fibro-adipogenic progenitors,34–36 scleraxis (Scx) lineage tendon derived stem cells37 and a myriad of other identifying markers.13,38–41 Further illustrating the vast heterogeneity of involved cell lineages, additional peripheral progenitor niches such as those marked by odd-skipped related (Osr1, Osr2) genes42 and engrailed1 (En1)43 may also be involved although not yet implicated with HO.
Given the role of VEGFA during normal bone development and the infiltration of mesenchymal stem cells throughout the formation of HO, we hypothesized that interruption of progenitor-cell-derived VEGFA would lead to a reduction in posttraumatic HO formation. We demonstrate that mesenchymal progenitors are a significant source of VEGFA important for ectopic bone formation and cell-specific inhibition of this signal significantly reduces posttraumatic HO.
Results
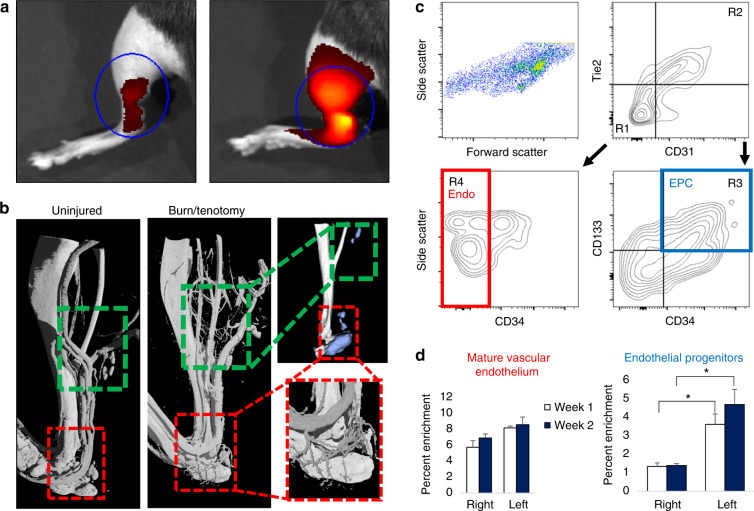
Extremity trauma and inflammation induces a pro-angiogenic environment characterized by an increase in total endothelial structures
Previous studies have demonstrated the upregulation of vascular signaling prior to pre-HO chondrogenesis.28 However, high-resolution imaging of the actual vessels have not been obtained in relation to HO after trauma. To do this, we performed multiple modalities to corroborate the increase in vascular density at multiple timepoints across the progression of endochondral ossification, including the acute phase after injury (20 h) and plateau of ossification (9 weeks). First, we used near infrared in vivo interrogation using Angiosense 750EX to image the mouse hindlimb and demonstrate a robust increase in blood flow (Fig. 1a). Next, to obtain a high resolution and anatomic assessment of the vascular network implicated with HO formation, we performed microfil injection and nano-CT imaging. We visualized two distinct regions of increased vascular growth around the calcaneus in the distal hindlimb (Fig. 1b, red inset) and proximal to the tibial/fibular fuse point in the injured leg. HO formed in close proximity to corresponding vascular beds at 9 weeks (as demonstrated by microCT analyzed at density thresholds above the intravascular polymer) leading us to conclude that there was indeed involvement of vasculature following the peripheral injury with both increased blood flow and angiogenesis at the injury site. To further characterize the cell surface markers of the infiltrating cells at the HO site at more subacute timepoints, we performed flow cytometry of the injured tissue, specifically interrogating two specific cell types: potentially increasing endothelium per microfil imaging and a progenitor niche capable of undergoing transition to connective tissues44 to contribute to the HO anlagen. FACS analysis of the injury site highlighted a significant enrichment of CD31− Tie2− CD34+ CD133+ 45–47 (Fig. 1c) endothelial progenitor cells (EPCs) in burn/tenotomy mice at 1 and 2 weeks (2.70 and 3.36-fold increases compared with uninjured contralateral leg, P = 0.032 and 0.002, respectively). There was not similar enrichment of mature endothelium at the 1 or 2 week timepoints (Fig. 1d). Given previous literature demonstrating the autocrine nature of VEGFA in vascular homeostasis,48 this cellular enrichment of EPCs is consistent with a robust induction of neovasculature and also suggest these progenitor cells as a possible source for VEGFA signaling involved in the angiogenesis associated with HO development consistent with previously described nontrauma HO models.28 Thus, we demonstrate using several different modalities that during HO formation, a rich, patent vascular network intimately surrounds the bone, is more prominent than in the uninjured extremity, and likely a facilitative influence in the progression of ectopic of endochondral ossification.
Fig. 1.
Focal injury superimposed upon systemic inflammation induces robust local angiogenesis and produces enrichment of endothelial progenitors at the injury site. a Angiosense IVIS demonstrates increased perfusion to injured hindlimb at 20 h post surgery (representative images from n = 3 per group). b MICROFIL perfusion nano-CT images and micro-CT of mature mice show networks of nascent vessel outgrowth in regions of subsequent HO formation following burn tenotomy (green inset) at 9 weeks. Vessels in the distal hindlimb exhibit dense vascular infiltration (red inset). c FACS gating schema of injury site 2 weeks after burn tenotomy. CD31− Tie2− CD34+ CD133+ endothelial progenitor cells (EPC, blue) identified via R1 + R3. CD31+ Tie2+ CD34− mature endothelial cells (red) identified via R2 + R4. Remaining live events were collected by surface marker depletion. d Proportion of gated EPC and mature endothelium from all live cells as assessed by flow cytometry was quantified at 1 week and 2 weeks post burn tenotomy
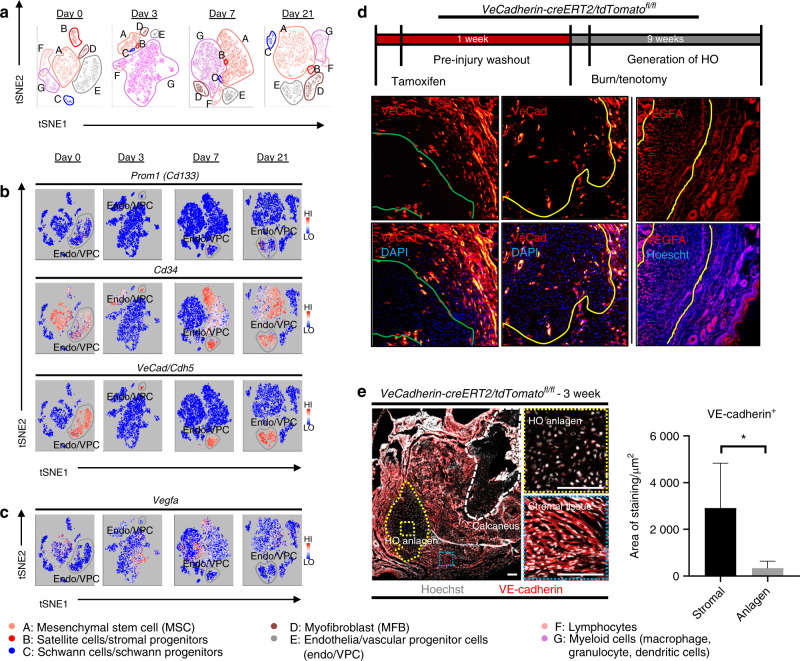
Vascular progenitors are not the contributing source for VEGFA at the burn/tenotomy injury site
Given the enrichment of EPCs demonstrated by flow cytometry, we performed a directed single-cell RNA sequencing experiment in order to characterize transcriptome-level expression of Vegfa and the cellular subpopulations producing these transcripts at baseline preinjury (day 0), and days 3, 7, and 21 postinductive burn/tenotomy. Clustering analysis was performed by blinded biostatistician. In order to characterize the perturbation from baseline caused by inductive burn/tenotomy, clusters were first preliminarily generated unsupervised, and subsequently rank correlated by centroids. This allowed to consolidate clusters into seven cell families, and subsequently compare them across replicates both within a single timepoint and across all timepoints. Clusters show high intra-timepoint stability, as demonstrated by the red diagonals in rank correlation heatmaps for each timepoint and PCA plots. The only notable exception to correlation with self was cluster A that showed a reciprocal minor correlation with cluster D. Based on this high fidelity, replicates within timepoints were pooled for subsequent analysis, with proportional contribution to each cluster from all replicates confirmed by PCA plots (Supplemental Figs. 1–12). The resulting seven clusters (Fig. 2a) were identified via gene ontology terms and KEGG pathway analyses (Tables 1–7) in addition to characteristic gene expression (Supplemental Figs. 13–15): mesenchymal stem cells (Pdgfra), satellite cells with putative stromal progenitors (Pax7), Schwann cells/neural progenitors (Plp1, Cnp, Dhh), myofibroblasts (MFB) encompassing pericytes and smooth muscle cells (Acta2, Mylk), endothelia/vascular progenitor cells (Cdh5, Pecam, Cd34), lymphocytes (Ms4a1), and myeloid cells including macrophages (Ccr2, Mrc1, Fcgr1), granulocyte (Ccr1, S100a9), dendritic cells (Cd209a). Fold change and adjusted P values for genes of interest are included in Table 8. Notably, the endothelial/vascular progenitors cluster (D) demonstrated expression of both Prom1(Cd133) and Cd34 (Fig. 2b, top/middle), corresponding to the EPC subpopulation identified in flow cytometry (Fig. 1c, d). This cluster also demonstrated high expression of mature endothelium genes (Supplemental Fig. 1) suggesting a mixed phenotype of the EPC and endothelium identified earlier in the flow cytometry. VeCadherin/Cdh5 (Fig. 2b, bottom) also robustly marked this cellular subpopulation. However, this cluster did not exhibit high Vegfa expression levels (Fig. 2c) across any timepoints, suggesting these cells actually were not the likely source for VEGFA signal. To verify these findings, we looked to reconcile data from previous studies that have identified cells of the endothelial lineage to serve as potential HO progenitor cells using a Tie-Cre33 marker. These models, however, did not use inducible systems which allow for adult labeling of cells, which is necessary to assess the true contribution of adult endothelial cells to posttraumatic HO. To address this limitation, inducible tdTomato reporter mice expressing creERT driven by the Cdh5 promoter were treated with tamoxifen with washout prior to burn/tenotomy to interrogate the spatial arrangement of early cells of endothelial lineage. Histological analysis demonstrated Cdh5+ cells spatially peripheral to the forming HO lesion but a distinct absence of Cdh5+ cells in the inflamed soft tissue deep to the cutaneous/stromal layers at 1 week (Fig. 2d, green). These cells remained a minor population in the progressing HO anlagen even at the 3 week timepoint (Fig. 2d, yellow), in stark contrast to the copious number of VEGFA-expressing cells seen in the same region (Fig. 2d, right). With the observation of Cdh5 enrichment in the periphery of pre-HO anlagen, we corroborated the significant enrichment in the surrounding stroma compared with pre-HO tissue via thresholded quantification of endogenous reporter micrographs (Fig. 2e). Thus, we verified that progenitors from endothelial lineages were not likely candidate precursors to the formation of HO, nor sources for VEGFA within the HO niche. The relatively few numbers of Cdh5+ cells within the HO analgen is consistent with previous studies showing that mesenchymal cells of nonendothelial lineage (i.e. Prx+, Mx1+, or Scx+) are the traumatic HO progenitors.34,36,37,49 Having demonstrated that HO lesions are highly vascular but that cells of endothelial origin do not densely populate the interior of the HO anlagen, we next examined whether VEGFA expression spatially correlated with other cellular subpopulations.
Table 2.
Cluster B: Top 10 upregulated terms from KEGG and Gene Ontology Domains
| ID | Name | Concept | #Genes | FDR |
|---|---|---|---|---|
| mmu03010 | Ribosome | KEGG | 68 | 2.00E−19 |
| mmu05412 | Arrhythmogenic right ventricular cardiomyopathy (ARVC) | KEGG | 71 | 0.000 437 49 |
| mmu04080 | Neuroactive ligand-receptor interaction | KEGG | 154 | 0.017 800 51 |
| mmu04740 | Olfactory transduction | KEGG | 21 | 0.028 569 4 |
| mmu05410 | Hypertrophic cardiomyopathy (HCM) | KEGG | 77 | 0.093 835 47 |
| mmu05414 | Dilated cardiomyopathy | KEGG | 80 | 0.106 303 39 |
| mmu04020 | Calcium signaling pathway | KEGG | 143 | 0.159 608 01 |
| mmu04260 | Cardiac muscle contraction | KEGG | 59 | 0.179 346 27 |
| mmu04960 | Aldosterone-regulated sodium reabsorption | KEGG | 35 | 0.185 410 25 |
| mmu04340 | Hedgehog signaling pathway | KEGG | 45 | 0.230 030 64 |
| GO:0022626 | Cytosolic ribosome | GOCC | 80 | 1.22E−38 |
| GO:0044391 | Ribosomal subunit | GOCC | 131 | 5.61E−31 |
| GO:0022625 | Cytosolic large ribosomal subunit | GOCC | 43 | 5.86E−28 |
| GO:0044445 | Cytosolic part | GOCC | 163 | 3.82E−27 |
| GO:0005840 | Ribosome | GOCC | 180 | 3.30E−26 |
| GO:0015934 | Large ribosomal subunit | GOCC | 76 | 2.36E−21 |
| GO:0030016 | Myofibril | GOCC | 167 | 7.33E−21 |
| GO:0043292 | Contractile fiber | GOCC | 180 | 8.64E−19 |
| GO:0030017 | Sarcomere | GOCC | 148 | 1.09E−18 |
| GO:0044449 | Contractile fiber part | GOCC | 161 | 1.68E−18 |
| GO:0003735 | Structural constituent of ribosome | GOMF | 151 | 3.61E−26 |
| GO:0019843 | rRNA binding | GOMF | 57 | 2.47E−14 |
| GO:0005198 | Structural molecule activity | GOMF | 432 | 1.66E−13 |
| GO:0000981 | RNA polymerase II transcription factor activity, sequence-specific DNA binding | GOMF | 503 | 7.69E−09 |
| GO:0001071 | Nucleic acid binding transcription factor activity | GOMF | 804 | 1.48E−07 |
| GO:0003700 | Transcription factor activity, sequence-specific DNA binding | GOMF | 804 | 1.48E−07 |
| GO:0030552 | cAMP binding | GOMF | 21 | 1.60E−07 |
| GO:0001228 | Transcriptional activator activity, RNA polymerase II transcription regulatory region sequence-specific binding | GOMF | 263 | 7.22E−06 |
| GO:0043565 | Sequence-specific DNA binding | GOMF | 769 | 7.64E−06 |
| GO:0030551 | Cyclic nucleotide binding | GOMF | 31 | 8.48E−06 |
| GO:0007517 | Muscle organ development | GOBP | 307 | 1.56E−22 |
| GO:0007519 | Skeletal Muscle tissue development | GOBP | 149 | 2.23E−21 |
| GO:0060538 | Skeletal muscle organ development | GOBP | 153 | 3.10E−21 |
| GO:0014706 | Striated muscle tissue development | GOBP | 329 | 1.84E−20 |
| GO:0060537 | Muscle tissue development | GOBP | 344 | 4.68E−20 |
| GO:0061061 | Muscle structure development | GOBP | 527 | 1.75E−18 |
| GO:0035914 | Skeletal muscle cell differentiation | GOBP | 66 | 8.23E−18 |
| GO:0060415 | Muscle tissue morphogenesis | GOBP | 66 | 1.76E−15 |
| GO:0055001 | Muscle cell development | GOBP | 149 | 3.30E−15 |
| GO:0006936 | Muscle contraction | GOBP | 226 | 7.59E−15 |
Table 3.
Cluster C: Top 10 upregulated terms from KEGG and Gene Ontology Domains
| ID | Name | Concept type | X.Genes | FDR |
|---|---|---|---|---|
| mmu04514 | Cell adhesion molecules (CAMs) | KEGG | 108 | 4.99E−07 |
| mmu04360 | Axon guidance | KEGG | 123 | 7.75E−06 |
| mmu05412 | Arrhythmogenic right ventricular cardiomyopathy (ARVC) | KEGG | 69 | 0.003 312 12 |
| mmu04530 | Tight junction | KEGG | 107 | 0.005 248 1 |
| mmu04971 | Gastric acid secretion | KEGG | 59 | 0.027 180 8 |
| mmu04012 | ErbB signaling pathway | KEGG | 84 | 0.040 082 96 |
| mmu04512 | ECM-receptor interaction | KEGG | 81 | 0.048 468 92 |
| mmu05414 | Dilated cardiomyopathy | KEGG | 78 | 0.048 468 92 |
| mmu05410 | Hypertrophic cardiomyopathy (HCM) | KEGG | 74 | 0.081 685 01 |
| mmu04540 | Gap junction | KEGG | 75 | 0.081 685 01 |
| GO:0030424 | Axon | GOCC | 435 | 2.03E−23 |
| GO:0097458 | Neuron Part | GOCC | 1 223 | 8.88E−20 |
| GO:0043005 | Neuron projection | GOCC | 963 | 4.47E−18 |
| GO:0043209 | Myelin sheath | GOCC | 195 | 7.26E−18 |
| GO:0045202 | Synapse | GOCC | 678 | 2.59E−14 |
| GO:0033267 | Axon part | GOCC | 232 | 1.12E−13 |
| GO:0044304 | Main axon | GOCC | 65 | 2.20E−12 |
| GO:0036477 | Somatodendritic compartment | GOCC | 700 | 3.91E−11 |
| GO:0044456 | Synapse part | GOCC | 510 | 3.91E−11 |
| GO:0043218 | Compact myelin | GOCC | 19 | 5.42E−11 |
| GO:0005249 | Voltage-gated potassium channel activity | GOMF | 55 | 2.78E−07 |
| GO:0005267 | Potassium channel activity | GOMF | 80 | 2.36E−06 |
| GO:0008092 | Cytoskeletal protein binding | GOMF | 711 | 4.23E−06 |
| GO:0015079 | Potassium ion transmembrane transporter activity | GOMF | 107 | 4.23E−06 |
| GO:0005200 | Structural constituent of cytoskeleton | GOMF | 60 | 1.22E−05 |
| GO:0015267 | Channel activity | GOMF | 293 | 1.24E−05 |
| GO:0022803 | Passive transmembrane transporter activity | GOMF | 293 | 1.24E−05 |
| GO:0005251 | Delayed rectifier potassium channel activity | GOMF | 23 | 4.27E−05 |
| GO:0022836 | Gated channel activity | GOMF | 199 | 0.000 110 22 |
| GO:0005216 | Ion Channel activity | GOMF | 264 | 0.000 123 54 |
| GO:0010001 | Glial Cell differentiation | GOBP | 174 | 1.23E−33 |
| GO:0007272 | Ensheathment of neurons | GOBP | 108 | 2.31E−30 |
| GO:0008366 | Axon ensheathment | GOBP | 108 | 2.31E−30 |
| GO:0042552 | Myelination | GOBP | 106 | 6.00E−30 |
| GO:0042063 | Gliogenesis | GOBP | 232 | 2.94E−28 |
| GO:0022008 | Neurogenesis | GOBP | 1 289 | 6.92E−23 |
| GO:0021782 | Glial Cell development | GOBP | 75 | 4.85E−17 |
| GO:0048699 | Generation of neurons | GOBP | 1 198 | 2.86E−16 |
| GO:0014037 | Schwann cell differentiation | GOBP | 32 | 4.24E−16 |
| GO:0007422 | Peripheral nervous system development | GOBP | 63 | 1.41E−15 |
Table 4.
Cluster D: Top 10 upregulated terms from KEGG and Gene Ontology Domains
| ID | Name | Concept type | X.Genes | FDR |
|---|---|---|---|---|
| mmu04270 | Vascular smooth muscle contraction | KEGG | 91 | 6.51E−17 |
| mmu05412 | Arrhythmogenic right ventricular cardiomyopathy (ARVC) | KEGG | 70 | 7.57E−11 |
| mmu04510 | Focal adhesion | KEGG | 192 | 6.84E−10 |
| mmu05414 | Dilated cardiomyopathy | KEGG | 79 | 1.51E−09 |
| mmu05410 | Hypertrophic cardiomyopathy (HCM) | KEGG | 75 | 2.08E−08 |
| mmu04260 | Cardiac muscle contraction | KEGG | 58 | 2.13E−07 |
| mmu04020 | Calcium signaling pathway | KEGG | 145 | 7.88E−07 |
| mmu04512 | ECM-receptor interaction | KEGG | 81 | 6.03E−06 |
| mmu05012 | Parkinson's disease | KEGG | 102 | 1.53E−05 |
| mmu04970 | Salivary secretion | KEGG | 57 | 0.000 526 44 |
| GO:0043292 | Contractile fiber | GOCC | 178 | 2.54E−24 |
| GO:0030016 | Myofibril | GOCC | 165 | 6.97E−24 |
| GO:0044449 | Contractile fiber part | GOCC | 159 | 6.97E−24 |
| GO:0042383 | Sarcolemma | GOCC | 124 | 8.03E−24 |
| GO:0030018 | Z disc | GOCC | 89 | 1.06E−22 |
| GO:0030017 | Sarcomere | GOCC | 146 | 1.29E−21 |
| GO:0031674 | I band | GOCC | 101 | 9.96E−21 |
| GO:0032432 | Actin filament bundle | GOCC | 57 | 7.27E−17 |
| GO:0030055 | Cell-substrate junction | GOCC | 342 | 2.42E−15 |
| GO:0005924 | Cell-substrate adherens junction | GOCC | 338 | 1.18E−14 |
| GO:0005261 | Cation channel activity | GOMF | 204 | 1.07E−07 |
| GO:0008324 | Cation transmembrane transporter activity | GOMF | 416 | 1.72E−07 |
| GO:0022890 | inorganic cation transmembrane transporter activity | GOMF | 362 | 1.83E−07 |
| GO:0003779 | Actin binding | GOMF | 326 | 4.05E−07 |
| GO:0046873 | Metal ion transmembrane transporter activity | GOMF | 296 | 1.05E−06 |
| GO:0022836 | Gated channel activity | GOMF | 205 | 5.27E−06 |
| GO:0005216 | Ion Channel activity | GOMF | 272 | 5.35E−06 |
| GO:0030551 | Cyclic nucleotide binding | GOMF | 32 | 6.42E−06 |
| GO:0015075 | Ion transmembrane transporter activity | GOMF | 538 | 8.49E−06 |
| GO:0008092 | Cytoskeletal protein binding | GOMF | 714 | 1.18E−05 |
| GO:0003012 | Muscle system process | GOBP | 293 | 5.28E−32 |
| GO:0006936 | Muscle contraction | GOBP | 224 | 5.28E−32 |
| GO:1903522 | Regulation of blood circulation | GOBP | 190 | 2.05E−24 |
| GO:0008015 | Blood circulation | GOBP | 347 | 1.16E−21 |
| GO:0003013 | Circulatory system process | GOBP | 351 | 1.99E−21 |
| GO:0008016 | Regulation of heart contraction | GOBP | 125 | 2.07E−21 |
| GO:0061061 | Muscle structure development | GOBP | 527 | 1.46E−20 |
| GO:0003008 | System process | GOBP | 1 104 | 2.91E−20 |
| GO:0044057 | Regulation of system process | GOBP | 382 | 7.31E−20 |
| GO:0006939 | Smooth muscle contraction | GOBP | 88 | 2.35E−18 |
Table 5.
Cluster E: Top 10 upregulated terms from KEGG and Gene Ontology Domains
| ID | Name | Concept | #Genes | FDR |
|---|---|---|---|---|
| mmu04360 | Axon guidance | KEGG | 122 | 1.99E−10 |
| mmu04530 | Tight junction | KEGG | 108 | 4.12E−08 |
| mmu04670 | Leukocyte transendothelial migration | KEGG | 100 | 3.37E−05 |
| mmu04270 | Vascular smooth muscle contraction | KEGG | 91 | 0.001 949 41 |
| mmu04070 | Phosphatidylinositol signaling system | KEGG | 70 | 0.002 174 78 |
| mmu05216 | Thyroid cancer | KEGG | 29 | 0.004 564 17 |
| mmu04520 | Adherens junction | KEGG | 67 | 0.005 146 28 |
| mmu04720 | Long-term potentiation | KEGG | 62 | 0.011 450 77 |
| mmu05100 | Bacterial invasion of epithelial cells | KEGG | 68 | 0.012 868 56 |
| mmu04330 | Notch signaling pathway | KEGG | 46 | 0.013 308 21 |
| GO:0030054 | Cell Junction | GOCC | 1 174 | 5.40E−17 |
| GO:0005911 | Cell–cell junction | GOCC | 570 | 1.39E−15 |
| GO:0070161 | Anchoring junction | GOCC | 609 | 1.84E−13 |
| GO:0005912 | Adherens junction | GOCC | 596 | 1.94E−13 |
| GO:0005913 | Cell–cell adherens junction | GOCC | 302 | 3.22E−11 |
| GO:0042641 | Actomyosin | GOCC | 61 | 1.16E−09 |
| GO:0030027 | Lamellipodium | GOCC | 136 | 2.50E−09 |
| GO:0098590 | Plasma Membrane region | GOCC | 698 | 5.05E−09 |
| GO:0001725 | Stress fiber | GOCC | 52 | 5.68E−09 |
| GO:0032432 | Actin Filament bundle | GOCC | 57 | 5.68E−09 |
| GO:0045296 | Cadherin binding | GOMF | 281 | 5.00E−10 |
| GO:0098641 | Cadherin binding involved in cell-cell adhesion | GOMF | 262 | 5.71E−08 |
| GO:0098631 | Protein binding involved in cell adhesion | GOMF | 274 | 6.95E−08 |
| GO:0098632 | Protein binding involved in cell-cell adhesion | GOMF | 269 | 8.48E−08 |
| GO:0050839 | Cell Adhesion molecule binding | GOMF | 395 | 4.10E−07 |
| GO:0005088 | Ras guanyl-nucleotide exchange factor activity | GOMF | 107 | 5.84E−06 |
| GO:0005112 | Notch binding | GOMF | 16 | 1.49E−05 |
| GO:0019904 | Protein domain specific binding | GOMF | 599 | 4.60E−05 |
| GO:0005085 | Guanyl-nucleotide exchange factor activity | GOMF | 169 | 5.78E−05 |
| GO:0001071 | Nucleic acid binding transcription factor activity | GOMF | 806 | 0.000 465 87 |
| GO:0003158 | Endothelium development | GOBP | 99 | 1.22E−20 |
| GO:0045446 | Endothelial cell differentiation | GOBP | 85 | 1.06E−19 |
| GO:0001525 | Angiogenesis | GOBP | 386 | 4.52E−17 |
| GO:0001667 | Ameboidal-type cell migration | GOBP | 306 | 1.39E−16 |
| GO:0043542 | Endothelial cell migration | GOBP | 137 | 4.28E−16 |
| GO:0048514 | Blood Vessel morphogenesis | GOBP | 467 | 4.29E−16 |
| GO:0072358 | Cardiovascular system development | GOBP | 587 | 1.10E−15 |
| GO:0001944 | Vasculature development | GOBP | 576 | 2.60E−15 |
| GO:0001568 | Blood vessel development | GOBP | 552 | 3.65E−15 |
| GO:0001885 | Endothelial cell development | GOBP | 53 | 5.44E−15 |
Table 6.
Cluster F: Top 10 upregulated terms from KEGG and Gene Ontology Domains
| ID | Name | Concept | #Genes | FDR |
|---|---|---|---|---|
| mmu03010 | Ribosome | KEGG | 68 | 3.07E−25 |
| mmu05340 | Primary immunodeficiency | KEGG | 31 | 3.98E−19 |
| mmu04660 | T-cell receptor signaling pathway | KEGG | 105 | 1.28E−16 |
| mmu05332 | Graft-versus-host disease | KEGG | 28 | 4.22E−15 |
| mmu05320 | Autoimmune thyroid disease | KEGG | 29 | 4.18E−14 |
| mmu05330 | Allograft rejection | KEGG | 30 | 1.33E−13 |
| mmu04650 | Natural killer cell mediated cytotoxicity | KEGG | 92 | 2.20E−13 |
| mmu04940 | Type I diabetes mellitus | KEGG | 33 | 3.65E−11 |
| mmu04640 | Hematopoietic cell lineage | KEGG | 71 | 1.84E−10 |
| mmu04060 | Cytokine-cytokine receptor interaction | KEGG | 199 | 8.44E−10 |
| GO:0022626 | Cytosolic Ribosome | GOCC | 80 | 2.70E−31 |
| GO:0009897 | External side of plasma membrane | GOCC | 228 | 1.65E−28 |
| GO:0098552 | Side of membrane | GOCC | 391 | 1.20E−27 |
| GO:0044391 | Ribosomal subunit | GOCC | 131 | 1.01E−22 |
| GO:0001772 | Immunological synapse | GOCC | 32 | 2.26E−21 |
| GO:0044445 | Cytosolic part | GOCC | 163 | 1.36E−20 |
| GO:0022625 | Cytosolic large ribosomal subunit | GOCC | 43 | 9.01E−20 |
| GO:0005840 | Ribosome | GOCC | 179 | 1.35E−17 |
| GO:0022627 | Cytosolic small ribosomal subunit | GOCC | 30 | 1.19E−15 |
| GO:0015934 | Large ribosomal subunit | GOCC | 76 | 1.88E−13 |
| GO:0003735 | Structural constituent of ribosome | GOMF | 151 | 3.26E−19 |
| GO:0005070 | SH3/SH2 adapter activity | GOMF | 23 | 3.78E−12 |
| GO:0003823 | Antigen binding | GOMF | 51 | 4.75E−12 |
| GO:0004896 | Cytokine receptor activity | GOMF | 80 | 9.70E−12 |
| GO:0004872 | Receptor activity | GOMF | 772 | 3.96E−11 |
| GO:0004888 | Transmembrane signaling receptor activity | GOMF | 545 | 3.96E−11 |
| GO:0038023 | Signaling receptor activity | GOMF | 626 | 3.96E−11 |
| GO:0060089 | Molecular transducer activity | GOMF | 772 | 3.96E−11 |
| GO:0099600 | Transmembrane receptor activity | GOMF | 568 | 5.16E−11 |
| GO:0019843 | rRNA binding | GOMF | 57 | 3.40E−10 |
| GO:0046649 | Lymphocyte activation | GOBP | 538 | 5.60E−48 |
| GO:0045321 | Leukocyte activation | GOBP | 629 | 6.12E−44 |
| GO:0042110 | T-cell activation | GOBP | 381 | 1.97E−42 |
| GO:0070489 | T-cell aggregation | GOBP | 381 | 1.97E−42 |
| GO:0071593 | Lymphocyte aggregation | GOBP | 382 | 1.97E−42 |
| GO:0070486 | Leukocyte aggregation | GOBP | 388 | 5.58E−42 |
| GO:0007159 | Leukocyte cell-cell adhesion | GOBP | 414 | 1.40E−41 |
| GO:0030098 | Lymphocyte differentiation | GOBP | 294 | 9.69E−38 |
| GO:0001775 | Cell activation | GOBP | 726 | 5.47E−37 |
| GO:0030217 | T-cell differentiation | GOBP | 218 | 2.00E−36 |
Fig. 2.
Vascular progenitors are not the source for VEGFA in HO formation. a Resultant seven clusters identifying cellular subpopulations within HO anlagen at respective timepoints. b Expression profiles for vascular progenitor genes Prom1 (Cd133), CD34, and Vecad/Cdh5. c Expression profile for Vegfa d Schematic for induction protocol of endogenous reporter mice. VeCadherin-creERT2/tdTomatofl/fl identify cells with endothelial programming within outlined regions. Sections taken from distal hindlimb of injury. Right: Sections of injury site from wild-type 3 week burn/tenotomy mice labeled for VEGFA. e Tiled immunofluorescent micrograph of 3 week burn/tenotomy injury site in endogenous VeCadherin reporters. Quantifications for thresholded total positive area (FIJI/ImageJ) were performed across biological triplicate, with 2 hpf per specimen for both HO anlagen site vs. surrounding stroma (n = 6/group)
Table 1.
Cluster A: Top 10 upregulated terms from KEGG and Gene Ontology Domains
| ID | Name | Concept | #Genes | FDR |
|---|---|---|---|---|
| mmu04141 | Protein processing in endoplasmic reticulum | KEGG | 156 | 5.56E−10 |
| mmu00510 | N-Glycan biosynthesis | KEGG | 43 | 1.79E−06 |
| mmu04512 | ECM-receptor interaction | KEGG | 82 | 1.95E−05 |
| mmu03060 | Protein export | KEGG | 22 | 7.76E−05 |
| mmu04310 | Wnt signaling pathway | KEGG | 137 | 0.000 162 |
| mmu00532 | Glycosaminoglycan biosynthesis - chondroitin sulfate/dermatan sulfate | KEGG | 21 | 0.000 213 33 |
| mmu00534 | Glycosaminoglycan biosynthesis - heparan sulfate/heparin | KEGG | 22 | 0.000 468 57 |
| mmu04120 | Ubiquitin mediated proteolysis | KEGG | 127 | 0.001 014 98 |
| mmu05217 | Basal cell carcinoma | KEGG | 50 | 0.001 937 43 |
| mmu04350 | TGF-beta signaling pathway | KEGG | 78 | 0.005 932 52 |
| GO:0005578 | Proteinaceous extracellular matrix | GOCC | 284 | 2.14E−36 |
| GO:0031012 | Extracellular matrix | GOCC | 410 | 1.73E−27 |
| GO:0044420 | Extracellular matrix component | GOCC | 121 | 9.66E−17 |
| GO:0005783 | Endoplasmic reticulum | GOCC | 1 234 | 1.58E−13 |
| GO:0005794 | Golgi apparatus | GOCC | 1 113 | 1.57E−12 |
| GO:0005604 | Basement membrane | GOCC | 93 | 3.48E−09 |
| GO:0044432 | Endoplasmic reticulum part | GOCC | 423 | 2.29E−07 |
| GO:0005793 | Endoplasmic reticulum-Golgi intermediate compartment | GOCC | 53 | 3.12E−07 |
| GO:0005581 | Collagen trimer | GOCC | 71 | 4.70E−06 |
| GO:0005801 | Cis-golgi network | GOCC | 32 | 4.70E−06 |
| GO:0005201 | Extracellular matrix structural constituent | GOMF | 35 | 5.06E−07 |
| GO:0005539 | Glycosaminoglycan binding | GOMF | 157 | 1.17E−06 |
| GO:0008201 | Heparin Binding | GOMF | 120 | 1.25E−06 |
| GO:0016758 | Transferase activity, transferring hexosyl groups | GOMF | 149 | 2.51E−06 |
| GO:1901681 | Sulfur compound binding | GOMF | 183 | 5.05E−05 |
| GO:0019838 | Growth factor binding | GOMF | 116 | 0.000 216 25 |
| GO:0016757 | Transferase activity, transferring glycosyl groups | GOMF | 229 | 0.000 429 31 |
| GO:0017147 | Wnt-protein binding | GOMF | 30 | 0.000 451 6 |
| GO:0004576 | Oligosaccharyl transferase activity | GOMF | 57 | 0.000 524 88 |
| GO:0001968 | Fibronectin binding | GOMF | 27 | 0.000 738 19 |
| GO:0001501 | Skeletal system development | GOBP | 412 | 3.26E−15 |
| GO:0051216 | Cartilage development | GOBP | 151 | 1.10E−14 |
| GO:0061448 | Connective tissue development | GOBP | 205 | 4.24E−14 |
| GO:0030198 | Extracellular matrix organization | GOBP | 189 | 1.43E−12 |
| GO:0043062 | Extracellular structure organization | GOBP | 190 | 1.94E−12 |
| GO:0009100 | Glycoprotein metabolic process | GOBP | 265 | 8.91E−12 |
| GO:0048736 | Appendage development | GOBP | 160 | 2.40E−11 |
| GO:0060173 | Limb development | GOBP | 160 | 2.40E−11 |
| GO:0035107 | Appendage morphogenesis | GOBP | 142 | 7.77E−11 |
| GO:0035108 | Limb morphogenesis | GOBP | 142 | 7.77E−11 |
Table 7.
Cluster G: Top 10 upregulated terms from KEGG and Gene Ontology Domains
| ID | Name | Concept | #Genes | FDR |
|---|---|---|---|---|
| mmu04142 | Lysosome | KEGG | 119 | 5.08E−14 |
| mmu04145 | Phagosome | KEGG | 128 | 6.29E−13 |
| mmu05140 | Leishmaniasis | KEGG | 63 | 6.29E−13 |
| mmu05150 | Staphylococcus aureus infection | KEGG | 42 | 7.05E−10 |
| mmu05323 | Rheumatoid arthritis | KEGG | 74 | 6.01E−09 |
| mmu04062 | Chemokine signaling pathway | KEGG | 164 | 1.71E−08 |
| mmu04380 | Osteoclast differentiation | KEGG | 111 | 3.92E−08 |
| mmu00190 | Oxidative phosphorylation | KEGG | 107 | 5.01E−08 |
| mmu04612 | Antigen processing and presentation | KEGG | 53 | 5.60E−08 |
| mmu04620 | Toll-like receptor signaling pathway | KEGG | 86 | 6.44E−08 |
| GO:0000323 | Lytic Vacuole | GOCC | 383 | 2.20E−27 |
| GO:0005764 | Lysosome | GOCC | 383 | 2.20E−27 |
| GO:0005773 | Vacuole | GOCC | 910 | 2.20E−16 |
| GO:0098552 | Side of membrane | GOCC | 396 | 1.39E−11 |
| GO:0045335 | Phagocytic vesicle | GOCC | 46 | 3.58E−11 |
| GO:0016469 | Proton-transporting two-sector ATPase complex | GOCC | 35 | 1.78E−10 |
| GO:0098796 | Membrane protein complex | GOCC | 803 | 1.78E−10 |
| GO:0044437 | Vacuolar part | GOCC | 317 | 2.82E−10 |
| GO:0005774 | Vacuolar membrane | GOCC | 303 | 5.79E−10 |
| GO:0009897 | External side of plasma membrane | GOCC | 232 | 5.79E−10 |
| GO:0015078 | Hydrogen ion transmembrane transporter activity | GOMF | 77 | 3.46E−09 |
| GO:0004896 | Cytokine receptor activity | GOMF | 82 | 1.57E−08 |
| GO:0036442 | Hydrogen-exporting ATPase activity | GOMF | 24 | 3.01E−08 |
| GO:0019829 | Cation-transporting ATPase activity | GOMF | 52 | 4.24E−07 |
| GO:0035586 | Purinergic receptor activity | GOMF | 21 | 6.63E−07 |
| GO:0042625 | ATPase coupled ion transmembrane transporter activity | GOMF | 53 | 1.00E−06 |
| GO:0003823 | Antigen binding | GOMF | 51 | 1.14E−06 |
| GO:0016820 | Hydrolase activity, acting on acid anhydrides, catalyzing transmembrane movement of substances | GOMF | 86 | 1.21E−06 |
| GO:0015077 | Monovalent inorganic cation transmembrane transporter activity | GOMF | 241 | 2.68E−06 |
| GO:0001614 | Purinergic nucleotide receptor activity | GOMF | 17 | 3.11E−06 |
| GO:0006955 | immune response | GOBP | 875 | 1.04E−69 |
| GO:0050776 | Regulation of immune response | GOBP | 472 | 1.26E−44 |
| GO:0006952 | Defense response | GOBP | 1 014 | 1.28E−44 |
| GO:0002252 | Immune effector process | GOBP | 566 | 1.08E−41 |
| GO:0002250 | Adaptive immune response | GOBP | 275 | 8.39E−40 |
| GO:0045321 | Leukocyte activation | GOBP | 630 | 2.17E−39 |
| GO:0002682 | Regulation of immune system process | GOBP | 987 | 4.64E−39 |
| GO:0045087 | Innate Immune response | GOBP | 430 | 2.15E−37 |
| GO:0002443 | Leukocyte mediated immunity | GOBP | 242 | 1.29E−36 |
| GO:0001775 | Cell activation | GOBP | 729 | 4.04E−36 |
Table 8.
Cluster identities—characteristic genes
| Gene | Fold change | Adj. P-value |
|---|---|---|
| A. Mesenchymal stem cells | ||
| Pdgfra | 2.535 350 835 | 0 |
| Prrx1 | 2.107 476 632 | 0 |
| B. Satellite cells/stromal progenitors | ||
| Pax7 | 2.874 586 669 | 0 |
| C. Schwann cells/neural progenitors | ||
| Plp1 | 22.637 784 39 | 0 |
| Cnp | 12.449 861 55 | 0 |
| Dhh | 2.683 388 559 | 0 |
| D. Myofibroblasts | ||
| Acta2 (aSMA) | 24.233 088 11 | 0 |
| Mylk | 10.489 084 02 | 0 |
| E. Endothelial/vascular progenitor cells | ||
| Cdh5 (VeCadherin) | 11.049 161 63 | 0 |
| Pecam1 | 10.105 707 91 | 0 |
| Cd34 | 2.496 854 666 | 0 |
| F. Lymphocytes | ||
| Ms4a1 | 6.438 651 332 | 0 |
| G. Myeloid cells | ||
| Ccr2 | 4.634 343 897 | 0 |
| Mrc1 | 4.064 399 087 | 0 |
| Fcgr1 | 2.972 696 05 | 0 |
| Ccr1 | 2.366 385 493 | 0 |
| S100a9 | 7.099 537 959 | 0 |
| Cd209a | 1.899 307 918 | 1.11E−228 |
Mesenchymal progenitor cells, instead of endothelial lineage cells, comprise the majority of cells within traumatic HO lesions
Unsupervised clustering yielded seven unique clusters (Fig. 2c), representing clusters of infiltrating inflammatory cells including macrophages, dendritic cells, and granulocytes, lymphocytes, endothelial cells/vascular progenitors, satellite cells with putative stromal progenitors, and progenitor subpopulations including mesenchymal stem cells, stromal progenitors, neural progenitors, and vascular progenitors. The mesenchymal stem cell population (cluster A) exhibited a remarkably constrained expression of Pdgfra, Osr2, and En1 (Fig. 3a), all markers for a variety of progenitor populations reported in existing literature. Vegfa expression was indeed found in the Pdgfra expressing population across all timepoints (Fig. 3b). Interestingly, Vegfa expression was also found in macrophage populations after injury (Fig. 3c). Visualized as a timecourse, the mesenchymal stem cell cluster seems to become more heterogenous as a function of time, differentiating into a population with diluted enrichment in Pdgfra, Prrx1, and Vegfa, along with the expected expression of chondrogenic (Sox9) and preosteoblast (Runx2) markers (Fig. 3d, top). This expression profile is starkly contrasted by robust downregulation in chondrogenic and osteoblastic genes in the vascular cluster (Fig. 3d, bottom), further corroborating that these cells are not the progenitors for HO formation, nor do they produce VEGFA. Simultaneously referencing the expression profiles (Fig. 3a, b), Vegfa seems to correspond strongly with a subpopulation of the mesenchymal stem cell cluster strongly expressing Pdgfra. Immunofluorescent histology confirmed robust synthesis of VEGFA at the injury site, colocalizing with PDGFRα positive cells (Fig. 3e), with significant increases in both signals compared with contralateral control and a direct correlation between PDGFRα and VEGFA signal (Fig. 3f).
Fig. 3.
Mesenchymal progenitor cells comprise the majority of VEGFA expressing cells within HO lesions. Clusters from 10× RNA sequencing across days 0, 3, 7, and 21 timepoints. Expression profiles corresponding to a mesenchymal progenitor cells: Pdgfra, Osr2, and En1; b Vegfa; c and macrophages: Mrc1 and Adgre1. d Expression heatmap delineating timecourse for log-fold changes in expression for genes of interest within (Top) mesenchymal stem cell cluster A and (Bottom) endothelial cells/vascular progenitor cells cluster E. Red and blue signify upregulation and downregulation respectively. e Representative immunolabeling from burn/tenotomy on wild-type mice 1 week after injury. n = 3/group. Color dotted squares designate magnified regions. White dotted lines circumscribe residual bellies of Achilles tendon. Dash dot lines outline reference native bone (calcaneus). Scalebars represent 100 μm. f Quantifications for relative signal in 1-week injury site (left leg) vs. uninjured contralateral limb (right leg) following automated thresholding (Yen). Linear regression of PDGFRα vs. VEGFA demonstrates significant correlation
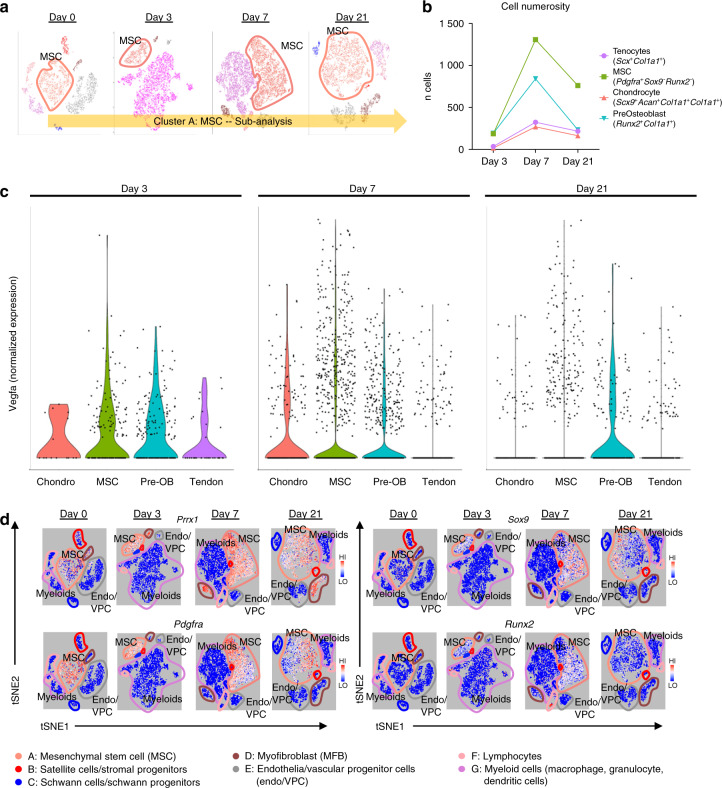
Vegfa is variably expressed across MSC progenitors and their differentiated progeny
In order to characterize the MSC cluster with more granularity, we performed a subanalysis on the interesting MSC cluster (Fig. 4a) in light of the suggestive expression profiles pointing to differentiating/differentiated cells like chondrocytes (Sox9) and preosteoblasts (Runx2) (Fig. 3d). Transcripts profiling tenocytes (Scx+Col1a1+), MSC (Pdgfra+Sox9-Runx2-), chondrocytes (Sox9+Acan+Col1a1+Col3a1+), and preosteoblasts (Runx2+Col1a1+) were used to stratify subgroups within the MSC cluster ‘A.’ These cells were observed to peak In number at day 7, with MSCs (day 7: 1 309 MSCs vs. 269 chondrocytes, 842 preosteoblasts, and 324 tenocytes) the dominant subpopulation comprising this MSC cluster and were subsequently analyzed for their level of Vegfa expression as shown in resulting violin plots (Fig. 4c). Vegfa was found in low levels within residual tendon that was attenuated by day 7. Conversely, at day 3, MSCs along with chondrocytes, and preosteoblasts to a lesser degree were found to be enriched in Vegfa. This transiently dissipated for both MSCs and chondroblasts by day 7. However, more terminally differentiating cells, pre-osteoblasts were found to propagate this Vegfa signal even into day 21. With this sustained signaling from MSCs through more differentiated progeny, we investigated a suitable candidate driver that could simultaneously attenuate Vegfa expression across the predominant MSCs, but also the spectrum of their differentiation following musculoskeletal polytrauma. We observed Prrx1 to overlap robustly with not only Pdgfra cells, but also Sox9 and Runx2 subpopulations as well (Fig. 4d). Given confirmation of transcriptional and translational expression of Vegfa from mesenchymal stem cells and their progeny in the injury niche, we hypothesized that conditional knockout in these cells would produce a reduction in posttraumatic HO.
Fig. 4.
Vegfa is variably expressed amongst MSC progenitors and their differentiated progeny. a Schematic of cluster subanalysis of MSC cells from single-cell RNA sequencing. b Discrete counts of cell types and classification criteria. c Expression levels of Vegfa across all indicated cell types. d Expression profiles of characteristic markers Prrx1; mesenchymal progenitors: Pdgfra; chondrocytes: Sox9; and preosteoblasts: Runx2
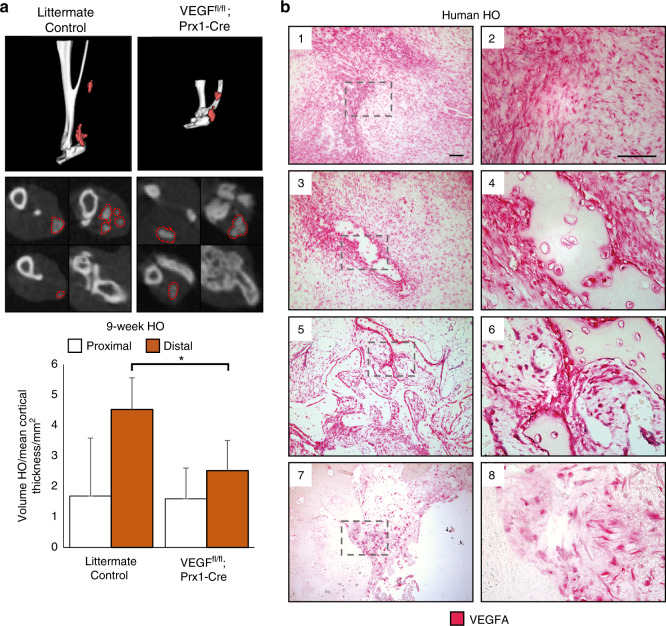
Conditional genetic deletion of VEGFA from Prx1 lineage cells decreases posttraumatic extremity HO
Having identified an increase in vascularity at a traumatic HO site and characterized a potential source for vascular signal, we next set out to assess the role of Prx1+ lineage cell derived VEGFA. Our single-cell RNA sequencing data reaffirm co-expression of Pdgfra and Prrx1 (Fig. 4d), corroborating our previously demonstrated work showing cells of the Prx1+ lineage define the HO progenitor cells.34 In addition, VEGFA has been shown to be produced by osteoprogenitor cells and to drive bone development.50 Recent studies also demonstrate that VEGFA from cells marked by Col2CreER-mediated recombination, but not vascular cell lineage (Flt1) functions as a survival and differentiation factor for chondrocytes.51 Thus, to evaluate the role of VEGFA on ectopic cartilage formation, we deleted VEGFA from cells of the Prx1+ lineage. Following VEGF deletion from Prx1+ MSCs via Prx1-cre/Vegffl/fl, these mutant mice produced significantly less HO in the distal hindlimb (44% relative reduction, P = 0.036 after normalization by cortical thickness due to stunted limb phenotype) when induced by burn/tenotomy (Fig. 5a). Given the density of PDGFRα+ cells observed with histology, the reduction in ectopic bone formation following selective gene knockout, implicates VEGFA expression and production by MSCs as a major niche in the acute inflammatory response after burn/tenotomy. Additional histological analyses of injury sites of Prx1-cre/Vegffl/fl 9 weeks post injury exhibit a profound absence i.e. significant ablation of VEGFA signaling in the deletion mice compared with littermate controls, despite comparable levels of PDGFRα+ cells (Supplemental Fig. 2) validating the degree of gene ablation.
Fig. 5.
VEGFA knockout and molecular inhibition attenuates formation of HO in the distal hindlimb. Following 9 weeks burn tenotomy, a Prx-Cre;Vegffl/fl; treated WT mice exhibit lower volumes of heterotopic ossification than their corresponding controls at 800 HU. Prx-Cre HO volumes normalized by mean cortical thickness (mm) due to congenital phenotype. n = 4–9/group. Bars represent means and SD. *P < 0.05 vs. Control by Student’s t test. b Magnified images of human HO samples immunolabeled for VEGFA: (1,2) pre-HO stroma, (3,4) early HO formation with surrounding stromal fibroblasts, (5,6) intermediate HO, and (7,8) mature HO with terminal ossification. VEGFA indicated by red, scalebar indicates 100 μm
Finally, histology was obtained from human HO specimens with diverse morphologies that reflect the full histologic spectrum of human disease (Fig. 5b, n = 10 human specimens). VEGFA immunostaining was performed, which paralleled our findings from mouse tissues. In early spindle cell lesions before frank ossification (Fig. 5b1,2), a high density of VEGF immunoreactive cells were present. In other areas with early and inconscipuous amounts of woven bone, noticeably stronger VEGF immunoreactivity was present within bone-lining cells (Fig. 5b3,4). These findings were consistent across specimens and in areas of more conspicuous lamellar bone (Fig. 5b5,6), in which bone-lining cells were the again prominently VEGF immunoreactive. In samples with HO of a thicker, more ‘cortical’ appearance (Fig. 5b7,8) bone-lining cells continued to show VEGF immunoreactivity while osteocytes within thicker bone fragments showed little staining. Thus, and across human samples, VEGF highlights similar populations of HO stromal progenitor cells and osteoblasts as in our mouse models, suggesting a potentially similar pathophysiology and disease course.
Discussion
HO is the formation of ectopic bone highly reliant on angiogenesis to progress through endochondral ossification to mature into its mineralized, final form. VEGFA is regulated by many transcription factors including HIF1a which is thought to be a major stimulus in cancer, bone development, and bone pathology.19,34,50,52 Having identified the central role of HIF1a in traumatic HO, we set out to determine whether VEGFA, a downstream signaling mediator of HIF1a, is involved in HO formation.
Previous studies have shown that VEGFA orchestrates ossification during normal bone development.53 Furthermore, elegant studies have demonstrated that VEGFA produced by cells of Osx-Cre lineage regulate blood vessel recruitment and early osteoblast differentiation21 and that VEGFA produced by Col2-Cre-marked cells is necessary for chondrocyte survival.51 We chose to target VEGFA in cells of the Prx1-Cre lineage as we were the first to identify these cells as the HO progenitor cells,34 a decision further supported by our transcriptomic and histologic data correlating Prrx1 and Pdgfra expression. Notably, in our model, chondrocytes provided limited contribution to Vegfa expression levels. However, preosteoblasts were found to be the responsible cell population for Vegfa expression at later timepoints (D21), demonstrating that in addition to recruited MSCs, their differentiating progeny propagated the robust expression Vegfa. While MSCs were the dominant source for Vegfa expression both in magnitude and volume (Fig. 4), the heterogeneity of Vegfa also deriving from chondroblasts and preosteoblasts further reinforced our strategy in producing VEGFA knockout via a Prx1 driver. Of particular note from a bioinformatics perspective, while the overwhelming majority of clusters demonstrated high specificity in alignment, two clusters A and D showed moderate levels of correspondence to each other following the initial pseudo clustering (Fig. 2a). These clusters correspond to related progenitor cells, both expressing a common ancestry given their prrx1 enrichment. However, the musculoskeletal mesenchymal progenitor population (D) exhibited sparse VEGFA signaling, essentially rendering this an inert subpopulation. Here we show that genetic loss of VEGFA from the mesenchymal stem cell population (along with some chondrocyte and preosteoblasts) is sufficient to significantly reduce HO volume. VEGFA inhibition in cells of the Prx-Cre lineage did not, however, completely mitigate all HO formation likely due to alternative sources for VEGFA as demonstrated in our single-cell RNA sequencing, namely inflammatory cells.51,54,55 Despite previous literature implicating vascular sources of VEGFA secreted in a cell autonomous manner,48 our sequencing data concretely demonstrated a notable absence of Vegfa transcripts. In addition, these cells did not express common markers of chondrogenic and osteoblastic differentiation, cementing their supportive role in the periphery of the developing ectopic bone.
Histological analysis of our acute injury model demonstrated a lack of spatial proximity between Cdh5-creERT2 cells and VEGFA within the HO region when activated just prior to injury. Cells positive for Cdh5, however, were present in a large amount surrounding the mesenchymal condensation that underwent endochondral ossification corroborating our sequencing results and the Cdh5+ cell’s important supportive role to the HO niche. This presence of Cdh5+ cells also corresponded with an increase in blood flow as well as blood vessels likely derived from the identified EPCs, which is consistent with the rubor and swelling seen at a joint predisposed to HO prior to radiographic evidence.
Two pathways could explain our observed phenotype of HO inhibition following loss of mesenchymal-derived VEGFA: decreased angiogenesis secondary to loss of the trophic signal leading to an indirect deleterious effect on endochondral ossification or direct phenotypic changes to the mesenchymal cells themselves. Interestingly, our mesenchymal stem cell population did not exhibit upregulation of any VEGF receptors, including Flt1/VEGFR1, Kdr/VEGFR2, or Flt4/VEGFR3 (data not shown) rendering them unresponsive to VEGFA. This is largely concordant with previous literature characterizing VEGFA activity in fetal tissues.23 Given the large influx of inflammatory cells including VEGFA expressing macrophages, one could presume that there should be enough residual VEGFA at the locus of injury to rescue the loss of mesenchymal-derived VEGFA, especially with the former pathway. Given our observed reduction in HO, it seems the latter pathway is more likely. Indeed, previous work by Zelzer et al. 23 demonstrated that VEGFA loss from mesenchymal stem cells leads to aberrant growth plate development despite no changes to surrounding vasculature, instead pointing to transcriptional changes within the differentiated mesenchymal cells and chondroblasts themselves. Furthermore, in this paradigm, the partial bone phenotype is unsurprising as Pdgfra/Prrx1 cells highly expressing VEGFA were a subpopulation of a larger pool of progenitors. Nevertheless, the targeted ablation of VEGFA was observed to produce marked, clinically-relevant reductions of posttraumatic HO. As such, future work could involve utilization of selective, deliverable next-generational inhibitors such as siRNAs for cell-specific knockdowns to attenuate HO formation.
This work is also the first to our knowledge to further characterize the role for novel progenitor-cell populations rapidly expanding in the literature. Subpopulations characterized as dermal lineage progenitors like engrailed1 (En1)56 and fibro-adipogenic progenitors like odd-skipped related-1/2 (Osr1/2)57 were found in the larger Pdgfra cluster, implicating En1 and Osr1/2 expressing cells as subsets of a larger progenitor population involved with HO formation. These cells appear transcriptionally distinct from Vegfa expressing progenitors, suggesting next steps that will be necessary to further characterize the differentiation capacity of these cells in the HO niche and to what degree they differ in the disease course. In addition, given previous work demonstrating the spatial variation of different lineages i.e. concentration of Prx-positive cells in the distal hindlimb, these separate cells with progenitor phenotypes may perhaps mark more proximal contributing cells to HO formation. Downstream high-throughput analyses facilitated by Next-Gen sequencing modalities as performed in this work will offer additional insights into important phenotypes and candidate targets.
This study has several notable limitations. Our RNA-sequencing results did not offer substantial resolution between mature endothelium (Supplemental Fig. 1) and EPCs. However, the flow cytometry did mark this separation well. Furthermore, this data would suggest that analysis of VeCadherin endogenous reporters would be likely indicating both mature endothelium in addition to the EPCs on histology. Thus, a complete absence of signal necessarily still validates an absence of EPCs. We chose to use Prx-Cre which will mark all cells from embryonic and postnatal development rather than an inducible Cre given our previous studies that demonstrate their central role in HO using this model.34 In addition, we do not delineate whether VEGF stimulates MSC differentiation58 or just promotes chondrocyte survival. In addition, because of our approach to characterize perturbations of cellular populations found at baseline, these constraints limited are ability to characterize the cell populations with further granularity i.e. myeloid cells vs. individual clusters for macrophages, granulocytes, and dendritic cells. This leaves us potentially susceptible to artifacts in results specifically due to dilution of clusters (as seen in the Vegfa expression patterns in the mesenchymal stem cells.
Notwithstanding these limitations, our findings demonstrate that mesenchymal-derived VEGFA is a crucially expressed signal in the genesis of HO, suggesting that therapies targeting VEGFA may present a reasonable option for reducing this debilitating disease and expanding the repertoire for its prevention. Subsequent studies are required to determine the efficacy and safety profile of targeted siRNA delivery systems and existing systemic anti-VEGFA antibodies such as bevacizumab in more directed wound healing models for HO patients.
Materials and methods
Ethics statement
All animal experiments described were approved by the University Committee on Use and Care of Animals at the University of Michigan, Ann Arbor (Protocols: #05909 and 07930). This study was carried out in strict accordance with the recommendations in the Guide for the Care and Use of Laboratory Animals of the National Institutes of Health.59 All animal procedures were carried out in accordance with the guidelines provided in the Guide for the Use and Care of Laboratory Animals: Eighth Edition from the Institute for Laboratory Animal Research.60
Animals
Mice evaluated for ectopic bone were wild-type C57BL/6J (Jackson Laboratories), Cdh5-Cre/tdTomatofl/fl 61, VeCadherin(Cdh5)-creERT2/tdTomatofl/fl 62 (a gift from Dr Luisa Iruela Arispe, UCLA), Prx1-cre34/Vegfafl/fl, or Prx1-cre/Vegfafl/fl littermate controls. All breeding was performed at the University of Michigan in facilities managed by the Unit for Laboratory Animal Medicine. CreERT reporters were induced with two doses of 1 mg tamoxifen in mice one week prior to burn/tenotomy for adequate washout by the time of injury.
Injury models
All mice received presurgical analgesia consisting of 0.06 mg·kg−1 buprenorphine for 48 h, followed by anesthesia with inhaled isoflurane, and close postoperative monitoring with analgesic administration.
Mice received 30% total body surface area partial-thickness burn on a shaved dorsum followed by transection of the left Achilles tendon. Dorsal burn was induced using a metal block heated to 60 °C in a water bath and applied to the dorsum for 18 s continuously. HO anlagen was observed by week 3 with mature bone formation visible by microCT by 9 weeks.
In vivo imaging system
Mice were anesthetized via inhaled isoflurane and depilated with Nair. Specimens were imaged before injection for baseline fluorescence levels at 770-nm wavelength using an IVIS Spectrum system (PerkinElmer 124262). Per manufacturer’s instructions, 100 μL of 20 μmol·L−1 AngioSense 750EX (PerkinElmer NEV10011EX) solution was injected into the tail vein followed by re-imaging 24 h post injection at excitation/emission of 750/800 nm. AngioSense protocol was performed 20 h post burn/tenotomy (n = 3/group).
10× Single-cell RNA sequencing
Baseline uninjured tendon (day 0) and post surgery day 3, 7, and 21 harvested tissue samples were digested for 45 min in 0.3% Type 1 Collagenase and 0.4% Dispase II (Gibco) in Roswell Park Memorial Institute (RPMI) medium at 37 °C under constant agitation at 120 r·min−1. Digestions were subsequently quenched with 10% FBS RPMI and filtered through 40 μm sterile strainers. Cells were then washed in PBS with 0.04% BSA, counted and resuspended at a concentration of ~1 000 cells per μL. Cell viability was assessed with Trypan blue exclusion on a Countess II (Thermo Fisher Scientific) automated counter and only samples with >85% viability were processed for further sequencing.
Single-cell 3′ library generation was performed on the 10× Genomics Chromium Controller following the manufacturer’s protocol for the v2 reagent kit (10× Genomics, Pleasanton, CA, USA). Following generation of single-cell gel bead-in-emulsions (GEMs), reverse transcription was performed and the resulting Post GEM-RT product was cleaned up using DynaBeads MyOne Silane beads (ThermoFisher Scientific, Waltham, MA, USA). The cDNA was amplified, SPRIselect (Beckman Coulter, Brea, CA, USA) cleaned and quantified then enzymatically fragmented and size selected using SPRIselect beads to optimize the cDNA amplicon size prior to library construction. An additional round of double-sided SPRI bead cleanup is performed after end repair and A-tailing. Another single-sided cleanup is done after adapter ligation. Indexes were added during PCR amplification and a final double-sided SPRI cleanup was performed. Libraries were quantified by Kapa qPCR for Illumina Adapters (Roche) and size was determined by Agilent tapestation D1000 tapes. Read 1 primer sequence are added to the molecules during GEM incubation. P5, P7 and sample index and read 2 primer sequence are added during library construction via end repair, A-tailing, adapter ligation and PCR. Libraries were generated with unique sample indices for each sample. Libraries were sequenced on a HiSeq 4000, (Illumina, San Diego, CA, USA) using a HiSeq 4000 PE Cluster Kit (PN PE-410-1001) with HiSeq 4000 SBS Kit (100 cycles, PN FC-410-1002) reagents, loaded at 200 pmol·L−1 following Illumina’s denaturing and dilution recommendations. The run configuration was 26 × 8 × 98 cycles for Read 1, Index, and Read 2, respectively. Cell Ranger Single Cell Software Suite 1.3 was used to perform sample de-multiplexing, barcode processing, and single-cell gene counting (Alignment, Barcoding and UMI Count) at the University of Michigan Biomedical Core Facilities DNA Sequencing Core.
A total of ~200-500 million reads were generated from the 10× Genomics sequencing analysis for each replicate. The sequencing data were first preprocessed using the 10× Genomics software Cell Ranger (10× Genomics Inc., Pleasanton, CA, USA) and aligned to mm10 genome (deposited to the Gene Expression Omnibus database: GSE126060). Downstream analysis steps were performed using Seurat. Cells with fewer than 500 genes, more than 10% of reads mapping to the mitochondrial genome, or more than 60 000 UMIs; and genes expressed in fewer than 10 cells per replicate, were filtered for quality control. The downstream analysis steps for each sample type include normalization, scaling, dimensionality reduction (PCA, t-SNE, and UMAP), unsupervised clustering, and the discovery of differentially expressed cell-type specific markers. We verified the absence of the within-time-point batch effect by visual inspection of the per-sample contribution in the per-day merged set, once we pooled together samples from each timepoint (Fig. 2b). In order to characterize the induced changes in cellular populations following burn/tenotomy injury, provisional clusters were identified unsupervised clustering followed by centroid rank correlation comparison within and between timepoints (days 0, 3, 7, and 21). Provisional clusters that failed to align across these comparisons were discarded, leaving behind cells and clusters that were identified in the steady state (day 0) timepoint and subsequently perturbed across days 3, 7, and 21. Final clusters were refined by pooling cells from all the timepoints to create a merged set; correcting for batch effect of the merged set; and performing a supplemental unsupervised clustering. Expression profiles of known markers, GO term and KEGG pathway analysis, along with characteristic expression profiles were utilized to identify the cell types of each cluster. FDR adjustments were performed to determine statistical significance of gene expression fold changes within a cluster vs. all other clusters within the merged set. Enrichment was performed with LRPath. The whole Bioinformatics analysis summarized here is detailed in the supplementary material (Figs. S3–15).
Histology and immunofluorescence
Histologic evaluation was performed at indicated timepoints in wild-type C57BL/6J and tdTomato endogenous reporter mutants following burn/tenotomy. TdTomato and wild-type hindlimbs were fixed at 4 °C in 4% paraformaldehyde or 10% neutral-buffered formalin. Specimens were subsequently decalcified in 14% (m/v) EDTA solution for 4–6 weeks at 4 °C until deformable manually. Hindlimbs were cryo- or paraffin-embedded and 8 μm–10 μm sections were cut and mounted on Superfrost plus slides (Fisher) and stored at −20 °C.
Paraffin sections were consistently selected from similar regions defined by talus as the anatomical landmark, rehydrated, processed for antigen retrieval in citrate buffer for 20 min at 95 °C–100 °C and blocked with 2% serum, 1% BSA, and 0.1% fish skin gelatin. Human sections were separately treated with trypsin enzymatic antigen retrieval solution (Abcam) for 10 min at 37 °C and blocked with 3% hydrogen peroxide (20 min, RT) and 5% goat serum (1 h, RT). Immunostaining of HO anlagen was performed on paraffin sections with the following antibodies: goat anti-mPDGFR-alpha (R&D Systems, AF1062) and rabbit anti-mouse VEGFA (EMD Millipore, ABS82). Secondary antibodies consisted of donkey anti-rabbit or anti-goat Alexafluor-488 or −594 (Invitrogen). Primary and fluorophore conjugated secondary antibodies were diluted 1:50–100 (2–4 μg·mL−1) and 1:200, respectively. Nuclear counterstain was performed with Hoechst 33342 (Life Technologies). Immunostaining of human HO was performed on paraffin sections with polyclonal rabbit anti-mouse VEGFA (Santa Cruz, Cat No. sc-152). Slides were subsequently blocked with BLOXALL solution (Vector) and 2.5% normal horse serum, and incubated with second primary antibody, IMPRESS-AP reagent (Vector) with development and counterstain via Alkaline Phosphatase Substrate and hematoxylin (Vector). Appropriate primary antibody negative controls were run simultaneously with each tested sample.
Microscopy
Cryosections of tdTomato endogenous reporter mice were imaged with a Zeiss LSM 510-META Laser Scanning Confocal Microscope equipped with a helium neon 1 laser (AF594, RFP). Cryosections for immunolabeled samples were performed on a Leica TCS SP8 Laser Scanning Confocal Microscope with tunable laser whose excitation and emission parameters were set to fluorophore manufacturer’s instructions. Antibody labeled paraffin sections were imaged with epifluorescent upright scope (Olympus BX-51) equipped with DAPI and dual-cube 488 nm/TRITC filters attached to an Olympus DP-70 high-resolution digital camera. Each site was imaged in all channels and were overlaid in Olympus DPViewer or Photoshop before examination and quantifications in ImageJ. Images were adjusted linearly only in brightness and contrast identically across comparison groups for clarity where necessary.
For quantification of positively fluorescence, images were automatically thresholded via Yen method, and then measured across 1–3 separate hpf per biologic specimen (ImageJ, n = 1–3/specimen, N = 3 specimens/treatment group). Images were then analyzed for area via the standard ImageJ measurement panel.
Flow cytometry
FACS analysis was performed on the injury site after harvesting the soft tissue of the posterior compartment between the muscular attachment of the Achilles tendon and the calcaneal insertion. Correlating soft tissue was also harvested from the contralateral uninjured leg. Tissue was digested for 60 min in 0.3% Type I Collagenase and 0.4% Dispase II (Gibco) in RPMI at 37 °C under constant agitation. Digestions were quenched with RPMI supplemented with 10% FBS and filtered using a 70-μm sterile strainer, transferred to 15 mL conical tubes, and centrifuged at 300 × g for 5 min. Tubes were decanted and washed in PBS three times. Digested specimens were blocked for Fc receptors with anti-mouse CD16/32 for 15 min at 4 °C, and subsequently stained with the following antibodies: Tie2-PE (12-5987-83, eBioscience), CD31-APC (551262, BD Pharmingen), CD133-AF488 (11–1331–82, eBioscience), and CD34-eFluor450 (48–0341–82, eBioscience). Following 30 min of incubation at 4 °C, samples were washed, filtered through a 35 μm mesh strainer, incubated with propidium iodide, and run on a FACSAria II (BD Biosciences) Cell Sorter at the University of Michigan Flow Cytometry Core in the Biomedical Science Research Center. For sorting, after appropriate FSC/SSC, singlets, and viable cells were gated, the CD31 and Tie2 double-negative subpopulation was enriched for CD34 positive EPCs. Tie2 and CD31 double positive subpopulations were further refined for CD133 and CD34 double-negative mature endothelium. Event counts were normalized to total viable cells to control for possible differences in the amount of tissue harvested. Data were then analyzed using FlowJo software.
MICROFIL imaging
In vivo collateral vessel formation was assessed using MICROFIL. At 9 weeks after burn/tenotomy, wild-type mice were euthanized with cannulation of descending thoracic aorta and venting of inferior vena cava. Mice were perfused with MICROFIL (MV120-blue; Flow Tech Inc.) which was allowed to polymerize overnight at 4 °C and subsequently imaged with μCT (n = 2/group).
MicroCT analysis
Mouse hind limbs were imaged with μCT at 9 weeks post injury (Bruker, 35 μm resolution and 357 μA/70 kV beam). Images were reconstructed and ectopic bone volume formation calculated with Microview (GE Healthcare v2.2, Parallax rc16). All scans were analyzed with threshold Hounsfield units (HU) of 800, 1 250, or 1 800 to determine the gross volume of mineralized tissues. Additional analyses delineated ectopic bone proximal to the tibial-fibular confluence from bone distal to this landmark and were defined as proximal and distal HO respectively.
Statistical analysis
Primary outcome of interest for a priori power analysis is volume of mature ectopic bone formation. To detect 50% decrease from 7.5 mm3 in untreated mice at significance level of 0.05 and power of 0.80, three mice were required per group. Means and SD were calculated from numerical data, as presented in text, figures, and figure legends. Bar graphs represent means with error bars specifying one SD. Sample groups were confirmed to be homoscedastic via Levene’s test. Pairwise comparisons were conducted with Student’s t test after confirmation for homoscedasticity via F-test. P values are included in figure legends.
Supplementary information
Acknowledgements
We would like to thank Christopher Breuler, Caitlin Priest, Serra Ucer, and the University of Michigan Orthopaedic Research Laboratories for their technical assistance. We also thank the Department of Radiology at The University of Michigan for the use of The Center for Molecular Imaging and The Preclinical Imaging & Computational Analysis Shared Resource which are supported in part by Comprehensive Cancer Center NIH grant P30 CA046592. We also thank to the University of Michigan Biomedical Research Core Facilities and the DNA sequencing core.
Funding
B.L.: Supported by funding from NIH/National Institute of Arthritis and Musculoskeletal and Skin Diseases NIH1R01AR071379 and American College of Surgeons Clowes Award. D.M.S.: Supported by Plastic Surgery Foundation Resident Research Award. M.S.: Supported by Plastic Surgery Foundation National Endowment Award. C.H.: Supported by Howard Hughes Medical Institute Medical Research Fellowship. J.L.: Supported by Vascular Surgery T32 5-T32-HL-076123–14. A.W.J.: Supported by the NIH/NIAMS (R01 AR070773, K08 AR068316, S10OD016374), the Orthopedic Research and Education Foundation with funding provided by the Maryland Stem Cell Research Foundation, and the Musculoskeletal Transplant Foundation. P.B.Y.: Supported by funding from NIH/NIAMS R01 AR057374 and NHLBI R01 HL131910. Y.M.: Supported by funding from NIH/NIDCR R01 DE020843 and DE027662
Author contributions
C.H., S.M., A.K.H., D.M.S., M.S., S.Loder, C.A.P., John Li, N.D.V., K.V., M.A.G., S.Li., C.Y.H., J.X., A.W.J., S.A., Jun Li, and B.L. conceived and/or designed the work that led to the submission, acquired data, and/or played an important role in interpreting the results. C.H., S.M., M.S., P.B.Y., A.W.J., Jun Li, Y.M., S.A., and B.L. drafted or revised paper. All listed authors approved the final version.
Competing interests
A.W.J. serves on the scientific advisory board for Novadip LLC and also receives laboratory financial support from MTF Biologics for research unrelated to the current project. All other authors declare no competing interests..
Supplementary information
The online version of this article (10.1038/s41413-019-0075-6) contains supplementary material, which is available to authorized users.
References
- 1.Ranganathan K, et al. Heterotopic ossification: basic-science principles and clinical correlates. J. Bone Jt. Surg. Am. 2015;97:1101–1111. doi: 10.2106/JBJS.N.01056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Potter BK, Burns TC, Lacap AP, Granville RR, Gajewski DA. Heterotopic ossification following traumatic and combat-related amputations. Prevalence, risk factors, and preliminary results of excision. J. Bone Jt. Surg. Am. 2007;89:476–486. doi: 10.2106/00004623-200703000-00003. [DOI] [PubMed] [Google Scholar]
- 3.Ring D, Jupiter JB. Excision of heterotopic bone around the elbow. Tech. Hand Up. Extrem Surg. 2004;8:25–33. doi: 10.1097/00130911-200403000-00007. [DOI] [PubMed] [Google Scholar]
- 4.Pavey GJ, et al. What risk factors predict recurrence of heterotopic ossification after excision in combat-related amputations? Clin. Orthop. Relat. Res. 2015;473:2814–2824. doi: 10.1007/s11999-015-4266-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Genet F, et al. The impact of preoperative hip heterotopic ossification extent on recurrence in patients with head and spinal cord injury: a case control study. PloS ONE. 2011;6:e23129. doi: 10.1371/journal.pone.0023129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Agarwal S, et al. Surgical excision of heterotopic ossification leads to re-emergence of mesenchymal stem cell populations responsible for recurrence. Stem Cells Transl. Med. 2017;6:799–806. doi: 10.5966/sctm.2015-0365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kaplan FS, et al. The histopathology of fibrodysplasia ossificans progressiva. An endochondral process. J. Bone Jt. Surg. Am. 1993;75:220–230. doi: 10.2106/00004623-199302000-00009. [DOI] [PubMed] [Google Scholar]
- 8.Tannous O, et al. Heterotopic bone formation about the hip undergoes endochondral ossification: a rabbit model. Clin. Orthop. Relat. Res. 2013;471:1584–1592. doi: 10.1007/s11999-013-2801-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Shore EM, Kaplan FS. Inherited human diseases of heterotopic bone formation. Nat. Rev. Rheumatol. 2010;6:518–527. doi: 10.1038/nrrheum.2010.122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dey D, et al. The traumatic bone: trauma-induced heterotopic ossification. Transl. Res. 2017;186:95–111. doi: 10.1016/j.trsl.2017.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lounev VY, et al. Identification of progenitor cells that contribute to heterotopic skeletogenesis. J. Bone Jt. Surg. Am. 2009;91:652–663. doi: 10.2106/JBJS.H.01177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Reichel LM, Salisbury E, Moustoukas MJ, Davis AR, Olmsted-Davis E. Molecular mechanisms of heterotopic ossification. J. Hand Surg. Am. 2014;39:563–566. doi: 10.1016/j.jhsa.2013.09.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kan L, Kessler JA. Evaluation of the cellular origins of heterotopic ossification. Orthopedics. 2014;37:329–340. doi: 10.3928/01477447-20140430-07. [DOI] [PubMed] [Google Scholar]
- 14.Cocks M, et al. Vascular patterning in human heterotopic ossification. Hum. Pathol. 2017;63:165–170. doi: 10.1016/j.humpath.2017.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kusumbe AP, Ramasamy SK, Adams RH. Coupling of angiogenesis and osteogenesis by a specific vessel subtype in bone. Nature. 2014;507:323–328. doi: 10.1038/nature13145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Maes C, et al. Osteoblast precursors, but not mature osteoblasts, move into developing and fractured bones along with invading blood vessels. Dev. Cell. 2010;19:329–344. doi: 10.1016/j.devcel.2010.07.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Schipani E. Hypoxia and HIF-1 alpha in chondrogenesis. Semin Cell Dev. Biol. 2005;16:539–546. doi: 10.1016/j.semcdb.2005.03.003. [DOI] [PubMed] [Google Scholar]
- 18.Forsythe JA, et al. Activation of vascular endothelial growth factor gene transcription by hypoxia-inducible factor 1. Mol. Cell Biol. 1996;16:4604–4613. doi: 10.1128/MCB.16.9.4604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Krock BL, Skuli N, Simon MC. Hypoxia-induced angiogenesis: good and evil. Genes Cancer. 2011;2:1117–1133. doi: 10.1177/1947601911423654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rankin EB, Giaccia AJ, Schipani E. A central role for hypoxic signaling in cartilage, bone, and hematopoiesis. Curr. Osteoporos. Rep. 2011;9:46–52. doi: 10.1007/s11914-011-0047-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Duan X, et al. Vegfa regulates perichondrial vascularity and osteoblast differentiation in bone development. Development. 2015;142:1984–1991. doi: 10.1242/dev.117952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Zhou Z, et al. Impaired endochondral ossification and angiogenesis in mice deficient in membrane-type matrix metalloproteinase I. Proc. Natl Acad. Sci. USA. 2000;97:4052–4057. doi: 10.1073/pnas.060037197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Zelzer E, et al. VEGFA is necessary for chondrocyte survival during bone development. Development. 2004;131:2161–2171. doi: 10.1242/dev.01053. [DOI] [PubMed] [Google Scholar]
- 24.Hoeben A, et al. Vascular endothelial growth factor and angiogenesis. Pharmacol. Rev. 2004;56:549–580. doi: 10.1124/pr.56.4.3. [DOI] [PubMed] [Google Scholar]
- 25.Shweiki D, Itin A, Soffer D, Keshet E. Vascular endothelial growth factor induced by hypoxia may mediate hypoxia-initiated angiogenesis. Nature. 1992;359:843–845. doi: 10.1038/359843a0. [DOI] [PubMed] [Google Scholar]
- 26.Shibuya M. Vascular endothelial growth factor (VEGF) and its receptor (VEGFR) signaling in angiogenesis: a crucial target for anti- and pro-angiogenic therapies. Genes Cancer. 2011;2:1097–1105. doi: 10.1177/1947601911423031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Maes C, et al. Soluble VEGF isoforms are essential for establishing epiphyseal vascularization and regulating chondrocyte development and survival. J. Clin. Invest. 2004;113:188–199. doi: 10.1172/JCI200419383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Dilling CF, et al. Vessel formation is induced prior to the appearance of cartilage in BMP-2-mediated heterotopic ossification. J. Bone Min. Res. 2010;25:1147–1156. doi: 10.1359/jbmr.091031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kan Chen, Chen Lijun, Hu Yangyang, Ding Na, Li Yuyun, McGuire Tammy L., Lu Haimei, Kessler John A., Kan Lixin. Gli1-labeled adult mesenchymal stem/progenitor cells and hedgehog signaling contribute to endochondral heterotopic ossification. Bone. 2018;109:71–79. doi: 10.1016/j.bone.2017.06.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lozito TP, Jackson WM, Nesti LJ, Tuan RS. Human mesenchymal stem cells generate a distinct pericellular zone of MMP activities via binding of MMPs and secretion of high levels of TIMPs. Matrix Biol. 2014;34:132–143. doi: 10.1016/j.matbio.2013.10.003. [DOI] [PubMed] [Google Scholar]
- 31.Hengartner NE, Fiedler J, Schrezenmeier H, Huber-Lang M, Brenner RE. Crucial role of IL1beta and C3a in the in vitro-response of multipotent mesenchymal stromal cells to inflammatory mediators of polytrauma. PloS ONE. 2015;10:e0116772. doi: 10.1371/journal.pone.0116772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Chang YS, et al. Critical role of vascular endothelial growth factor secreted by mesenchymal stem cells in hyperoxic lung injury. Am. J. Respir. Cell Mol. Biol. 2014;51:391–399. doi: 10.1165/rcmb.2013-0385OC. [DOI] [PubMed] [Google Scholar]
- 33.Medici D, et al. Conversion of vascular endothelial cells into multipotent stem-like cells. Nat. Med. 2010;16:1400–1406. doi: 10.1038/nm.2252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Agarwal S, et al. Inhibition of Hif1alpha prevents both trauma-induced and genetic heterotopic ossification. Proc. Natl Acad. Sci. USA. 2016;113:E338–E347. doi: 10.1073/pnas.1515397113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Wosczyna MN, Biswas AA, Cogswell CA, Goldhamer DJ. Multipotent progenitors resident in the skeletal muscle interstitium exhibit robust BMP-dependent osteogenic activity and mediate heterotopic ossification. J. Bone Min. Res. 2012;27:1004–1017. doi: 10.1002/jbmr.1562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Dey D, et al. Two tissue-resident progenitor lineages drive distinct phenotypes of heterotopic ossification. Sci. Transl. Med. 2016;8:366ra163. doi: 10.1126/scitranslmed.aaf1090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Agarwal Shailesh, Loder Shawn J., Cholok David, Peterson Joshua, Li John, Breuler Christopher, Cameron Brownley R., Hsin Sung Hsiao, Chung Michael T., Kamiya Nobuhiro, Li Shuli, Zhao Bin, Kaartinen Vesa, Davis Thomas A., Qureshi Ammar T., Schipani Ernestina, Mishina Yuji, Levi Benjamin. Scleraxis-Lineage Cells Contribute to Ectopic Bone Formation in Muscle and Tendon. STEM CELLS. 2016;35(3):705–710. doi: 10.1002/stem.2515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kan L, Peng CY, McGuire TL, Kessler JA. Glast-expressing progenitor cells contribute to heterotopic ossification. Bone. 2013;53:194–203. doi: 10.1016/j.bone.2012.12.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Li Y, et al. The role of scleraxis in fate determination of mesenchymal stem cells for tenocyte differentiation. Sci. Rep. 2015;5:13149. doi: 10.1038/srep13149. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 40.Agarwal Shailesh, Loder Shawn J., Brownley Cameron, Eboda Oluwatobi, Peterson Jonathan R., Hayano Satoru, Wu Bingrou, Zhao Bin, Kaartinen Vesa, Wong Victor C., Mishina Yuji, Levi Benjamin. BMP signaling mediated by constitutively active Activin type 1 receptor (ACVR1) results in ectopic bone formation localized to distal extremity joints. Developmental Biology. 2015;400(2):202–209. doi: 10.1016/j.ydbio.2015.02.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Cholok David, Chung Michael T., Ranganathan Kavitha, Ucer Serra, Day Devaveena, Davis Thomas A., Mishina Yuji, Levi Benjamin. Heterotopic ossification and the elucidation of pathologic differentiation. Bone. 2018;109:12–21. doi: 10.1016/j.bone.2017.09.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Stricker S, et al. Odd-skipped related genes regulate differentiation of embryonic limb mesenchyme and bone marrow mesenchymal stromal cells. Stem Cells Dev. 2012;21:623–633. doi: 10.1089/scd.2011.0154. [DOI] [PubMed] [Google Scholar]
- 43.Moore, A. L. et al. Doxycycline reduces scar thickness and improves collagen architecture. Ann Surg. Epub ahead of print (2018). [DOI] [PMC free article] [PubMed]
- 44.Agarwal S, et al. Local and circulating endothelial cells undergo endothelial to mesenchymal transition (EndMT) in response to musculoskeletal injury. Sci. Rep. 2016;6:32514. doi: 10.1038/srep32514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Yang J, et al. CD34+ cells represent highly functional endothelial progenitor cells in murine bone marrow. PloS ONE. 2011;6:e20219. doi: 10.1371/journal.pone.0020219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Fritzenwanger M, et al. Differential number of CD34+, CD133+ and CD34+/CD133+ cells in peripheral blood of patients with congestive heart failure. Eur. J. Med. Res. 2009;14:113–117. doi: 10.1186/2047-783X-14-3-113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Massa M, et al. Circulating CD34+, CD133+, and vascular endothelial growth factor receptor 2-positive endothelial progenitor cells in myelofibrosis with myeloid metaplasia. J. Clin. Oncol. 2005;23:5688–5695. doi: 10.1200/JCO.2005.09.021. [DOI] [PubMed] [Google Scholar]
- 48.Lee S, et al. Autocrine VEGF signaling is required for vascular homeostasis. Cell. 2007;130:691–703. doi: 10.1016/j.cell.2007.06.054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Lees-Shepard JB, et al. Activin-dependent signaling in fibro/adipogenic progenitors causes fibrodysplasia ossificans progressiva. Nat. Commun. 2018;9:471. doi: 10.1038/s41467-018-02872-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Hu K, Olsen BR. Osteoblast-derived VEGF regulates osteoblast differentiation and bone formation during bone repair. J. Clin. Investig. 2016;126:509–526. doi: 10.1172/JCI82585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Nagao M, et al. Vascular endothelial growth factor in cartilage development and osteoarthritis. Sci. Rep. 2017;7:13027. doi: 10.1038/s41598-017-13417-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Shen X, et al. Prolyl hydroxylase inhibitors increase neoangiogenesis and callus formation following femur fracture in mice. J. Orthop. Res. 2009;27:1298–1305. doi: 10.1002/jor.20886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Ramasamy SK, et al. Blood flow controls bone vascular function and osteogenesis. Nat. Commun. 2016;7:13601. doi: 10.1038/ncomms13601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Sunderkotter C, Goebeler M, Schulze-Osthoff K, Bhardwaj R, Sorg C. Macrophage-derived angiogenesis factors. Pharmcol. Ther. 1991;51:195–216. doi: 10.1016/0163-7258(91)90077-Y. [DOI] [PubMed] [Google Scholar]
- 55.Leek RD, et al. Macrophage infiltration is associated with VEGF and EGFR expression in breast cancer. J. Pathol. 2000;190:430–436. doi: 10.1002/(SICI)1096-9896(200003)190:4<430::AID-PATH538>3.0.CO;2-6. [DOI] [PubMed] [Google Scholar]
- 56.Rinkevich Y, et al. Skin fibrosis. Identification and isolation of a dermal lineage with intrinsic fibrogenic potential. Science. 2015;348:aaa2151. doi: 10.1126/science.aaa2151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Vallecillo-Garcia P, et al. Odd skipped-related 1 identifies a population of embryonic fibro-adipogenic progenitors regulating myogenesis during limb development. Nat. Commun. 2017;8:1218. doi: 10.1038/s41467-017-01120-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Hu DP, et al. Cartilage to bone transformation during fracture healing is coordinated by the invading vasculature and induction of the core pluripotency genes. Development. 2017;144:221–234. doi: 10.1242/dev.130807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Council, N. R. Committee for the Update of the Guide for the Care and Use of Laboratory Animals. Guide for the Care and Use ofLaboratory Animals. 8th edn. Washington (DC): National Academies Press (US). (2011).
- 60.Ferrara N, Hillan KJ, Novotny W. Bevacizumab (Avastin), a humanized anti-VEGF monoclonal antibody for cancer therapy. Biochem. Biophys. Res. Commun. 2005;333:328–335. doi: 10.1016/j.bbrc.2005.05.132. [DOI] [PubMed] [Google Scholar]
- 61.Alva JA, et al. VE-Cadherin-Cre-recombinase transgenic mouse: a tool for lineage analysis and gene deletion in endothelial cells. Dev. Dyn. 2006;235:759–767. doi: 10.1002/dvdy.20643. [DOI] [PubMed] [Google Scholar]
- 62.Monvoisin A, et al. VE-cadherin-CreERT2 transgenic mouse: a model for inducible recombination in the endothelium. Dev. Dyn. 2006;235:3413–3422. doi: 10.1002/dvdy.20982. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.