Abstract
Adverse pregnancy outcomes increase infants’ risk for mortality and future health problems. Neighborhood physical disorder may contribute to adverse pregnancy outcomes by increasing maternal chronic stress. Google Street View technology presents a novel method for assessing neighborhood physical disorder but has not been previously examined in the context of birth outcomes. In this cross-sectional study, trained raters used Google’s Street View imagery to virtually audit a randomly sampled block within each Chicago census tract (n = 809) for nine indicators of physical disorder. We used an item-response theory model and spatial interpolation to calculate tract-level neighborhood physical disorder scores across Chicago. We linked these data with geocoded electronic health record data from a large, academic women’s hospital in Chicago (2015–2017, n = 14,309 births). We used three-level hierarchical Poisson regression to estimate prevalence ratios for the associations of neighborhood physical disorder with preterm birth (overall and spontaneous), small for gestational age (SGA), and hypertensive disorder of pregnancy (HDP). After adjustment for maternal sociodemographics, multiparity, and season of birth, living in a neighborhood with high physical disorder was associated with higher prevalence of PTB, SGA, and HDP (prevalence ratios and 95% confidence intervals 1.21 (1.06, 1.39) for PTB, 1.13 (1.01, 1.37) for SGA, and 1.23 (1.07, 1.42) for HDP). Adjustment for neighborhood poverty and maternal health conditions (e.g., hypertension, diabetes, asthma, substance use) attenuated associations. Results suggest that an adverse neighborhood physical environment may contribute to adverse pregnancy outcomes. However, future work is needed to disentangle the unique contribution of physical disorder from other characteristics of disadvantaged neighborhoods.
Electronic supplementary material
The online version of this article (10.1007/s11524-019-00401-0) contains supplementary material, which is available to authorized users.
Keywords: Pregnancy outcomes, Premature birth, Electronic health records, Neighborhood physical disorder
Introduction
Adverse pregnancy outcomes increase the risk of infant mortality [1] and future health problems [2–4] and are also associated with future cardiovascular disease among mothers [5, 6]. According to multiple systematic reviews [7–9], women living in socioeconomically disadvantaged neighborhoods have worse pregnancy outcomes than those in more advantaged neighborhoods. One feature of disadvantaged neighborhoods that may adversely influence pregnancy outcomes is physical disorder, which includes physical signs of neighborhood deterioration or disinvestment (e.g., abandoned buildings, vacant lots, trash, and graffiti). Neighborhood physical disorder is hypothesized to reduce perceptions of safety and social cohesion among residents [10, 11] and has been associated with psychological distress [12, 13], depression [14], low physical activity [15, 16], and substance use [17]. Among pregnant women, neighborhood disorder has been linked with smoking [18] and low physical activity [19]. In addition, repeated exposure to psychosocial stress during pregnancy may lead to hormonal and neuroendocrine changes that may trigger spontaneous preterm birth or restrict fetal growth [20–22]. Thus, it is plausible that neighborhood physical disorder might influence pregnancy outcomes through maternal stress and health behaviors. However, relatively few studies have examined associations of neighborhood physical disorder with pregnancy outcomes [23].
Neighborhood physical disorder is often assessed through systematic social observation [24], which involves visually examining a street segment or city block and measuring multiple indicators of an underlying construct (e.g., recording the presence of graffiti, trash, and housing deterioration as indicators of neighborhood physical disorder). This approach has been used in several prior studies to estimate associations of neighborhood physical disorder with birth outcomes, including preterm birth, low birth weight, small for gestational age, and hypertensive disorders of pregnancy, with mixed findings [18, 25, 26]. Systematic social observation is complicated by the need to travel to different locations to complete in-person audits, which may be expensive. However, Google’s Street View imagery now enables researchers to conduct virtual neighborhood audits using readily available, high-resolution imagery [27, 28]. Street View audits are reliable and cost-effective for measuring neighborhood characteristics including physical disorder [27–34]. For example, Mooney et al. found that Google Street View-based audits required only 3% as much time as in-person audit while yielding similar results [35]. However, few studies have examined associations of Google Street View-derived measures of neighborhood physical disorder with health outcomes [31, 36], and to our knowledge no studies have used this approach in the context of pregnancy outcomes.
In this study, our objective was to examine associations of neighborhood physical disorder, measured via Google Street View virtual audits, with adverse pregnancy outcomes among women in Chicago using electronic health record (EHR) data. We hypothesized that women living in neighborhoods with higher levels of physical disorder would have higher odds of preterm birth, small for gestational age, and hypertensive disorder of pregnancy.
Methods
Study Population
We conducted a cross-sectional analysis using data from the Northwestern Medicine Enterprise Data Warehouse, an EHR repository. We extracted data for all singleton births occurring at Prentice Women’s Hospital in Chicago, Illinois, between January 1, 2015 and December 31, 2017 (n = 23,863 births). We used ArcMap version 10.5 (Environmental Systems Research Institute, Redlands, CA) to geocode mothers’ addresses during pregnancy. We restricted to births among women who lived in Chicago whose residence could be geocoded to a street address or address point (14,416 births to 13,755 mothers in 772 census tracts) to enable linkage of our physical disorder measure. We subsequently excluded 107 births for missing covariate data. The final study population included 14,309 births to 13,657 mothers in 772 census tracts. The Northwestern University Institutional Review Board approved this study.
Neighborhood Physical Disorder
We used Google Earth Pro’s Street View functionality (Google, Inc., Mountain View, CA) to virtually audit physical disorder. Street View is a free tool that provides panoramic, high-definition imagery at the street level captured using cameras mounted on cars. Overlapping pictures are taken by adjacent cameras, and images are stitched together to create a 360-degree panoramic view of the street. We assessed physical disorder using a previously described scale [36] based on validated measures [28, 37]. The scale includes nine indicators of physical disorder shown in Table 1 (e.g., trash, abandoned vehicles, graffiti, vacant lots). Audits were conducted by 12 trained raters who participated in a 2-h training session and completion of 10 practice blocks to establish coding consistency prior to the start of data collection.
Table 1.
Neighborhood physical disorder items and inter-rater reliability from block faces audited using Google Street View
| List of items | Categorization | Prevalence | % agreementa | Kappab |
|---|---|---|---|---|
| Trash/garbage | Heavy/moderate (1) versus light/none (0) | 21.8% | 85.2% | 0.53 |
| Abandoned vehicle | Yes (1) versus no (0) | 1.6% | 98.8% | – |
| Graffiti | Yes (1) versus no (0) | 13.0% | 91.4% | 0.56 |
| Graffiti scrubbed/painted over | Yes (1) versus no (0) | 13.9% | 86.4% | 0.50 |
| Other defaced property | Yes (1) versus no (0) | 26.8% | 76.7% | 0.44 |
| Bars on windows/doors | Yes (1) versus no (0) | 29.3% | 86.4% | 0.67 |
| Abandoned/boarded up buildings | Yes (1) versus no (0) | 8.3% | 92.6% | – |
| Building condition | More than half/all buildings in poor condition versus about half, less than half, none | 5.9% | 97.3% | – |
| Vacant lots | Yes (1) versus no (0) | 11.3% | 93.4% | 0.57 |
aTwo raters coded each block face (n = 257 block faces from 84 census blocks, reflecting a 10% sample of the full set of census blocks in the Chicago city limits)
bKappa statistics were not calculated for items with a prevalence below 10%
For this study, our goal was to create a physical disorder measure across the entire city of Chicago that could be linked to EHR data. We accomplished this by auditing one census block from each of the 810 census tracts that are wholly or partially within the Chicago city limits and using spatial interpolation methods, described below, to estimate physical disorder scores at unmeasured locations across the city. Census blocks are typically three to four-sided geographic areas bounded by streets or other physical features (e.g., bodies of water) and are the smallest units classified by the US Census Bureau. In prior work [36], we virtually audited neighborhood physical disorder from blocks in 242 Chicago census tracts using the scale described above (data collection completed between October 2017 and April 2018). For the current study, we first sampled one previously coded block from each of these tracts and then randomly sampled one block from each of the remaining 568 Chicago tracts. These additional 568 blocks were virtually audited between May and August of 2018. We excluded one block with no Google Earth imagery available, for a final total of 809 blocks. For each included block, raters assessed each “block face,” or single side of a street segment, with available imagery (range 3–7 block faces per block, median 4).
A 10% sample of blocks (n = 84) were coded by two raters in order to calculate inter-rater reliability. All other blocks were coded by a single rater. We calculated percent agreement between the two raters and calculated Cohen’s kappa statistics for physical disorder indicators with prevalence of ≥ 10% (for items with low prevalence, kappas are artificially low due to inflated expected chance agreement) [38].
As described previously [36, 37], we used an item response theory (IRT) model to combine physical disorder items into a summary score for each block face reflecting a latent level of physical disorder. Details on the IRT model are available in the Supplemental Appendix. We aggregated block face-level latent physical disorder scores to the block level by averaging the block face-level scores.
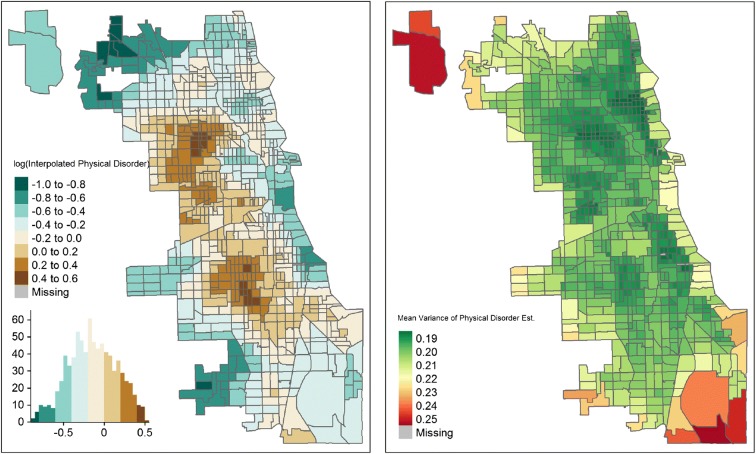
In order to interpolate levels of physical disorder throughout the entire city of Chicago, we used ordinary kriging, a spatial interpolation method that uses the spatial autocorrelation structure of observed locations to estimate values at non-observed locations [39]. Kriging, which has been used previously for Street View-derived physical disorder measures [32, 37], was accomplished using the “sp” package in R. First, we applied our block-level physical disorder scores to the latitude and longitude location of each block’s geographic centroid. Then, we built a semivariogram model, which estimated the degree of covariance between physical disorder measurements as a function of their distance apart. We modeled the semivariance (or the correlation between two values based on their distance) of the physical disorder score for each pair of census blocks in our dataset using the equation: γ(xi, xj) = 1/2[z(xi) − z(xj)]2 , where γ indicates the value of the semi-variance, xi and xj are two points in space, and z is the value of the physical disorder score measured at location x. We plotted an empirical variogram reflecting the average semivariance within 15 evenly spaced bins, or collections of data points within a certain distance. Based on this plot, we fit an exponential variogram model to obtain the interpolated physical disorder score at any point across a smooth raster surface reflecting the city of Chicago. Kriged physical disorder scores were log-transformed due to skewness, aggregated to the census tract level by averaging across all raster surface points falling within the tract (Fig. 1), and then linked to mothers based on their census tract of residence. Women were considered exposed to high neighborhood physical disorder if their home census tract was in the highest tertile of log-transformed physical disorder scores (range −0.13 to 0.52), while women in the bottom two tertiles (range − 0.86 to − 0.13) were considered exposed to low neighborhood physical disorder. This parameterization was chosen for ease of interpretation and due to non-linearity in the relationship between physical disorder score and adverse pregnancy outcomes.
Fig. 1.
Map of interpolated neighborhood physical disorder scores and variance. Physical disorder scores were interpolated throughout Chicago using ordinary kriging, a geospatial interpolation method that uses the spatial autocorrelation structure of observed locations to estimate values at non-observed locations. a, b show the mean and variance, respectively, of the log-transformed physical disorder score for each census tract. Higher positive values of log transformed physical disorder score indicate higher levels of neighborhood physical disorder
Outcomes
Pregnancy outcomes were defined using data extracted from the EHR on gestational age, birth weight, and problem lists/diagnostic codes. A prior study that compared extraction of birth outcomes from EHR versus manual extraction found differences to be small [40]. We excluded implausible values for gestational age (> 22 weeks or > 44 weeks) or birth weight (> 10 kg).
Our study outcomes included preterm birth (PTB), small for gestational age (SGA), and hypertensive disorder of pregnancy (HDP). PTB was defined as gestational age < 37 weeks. SGA was defined as birth weight below the 10th percentile for a given gestational age [41]. We focused on SGA rather than low birth weight in order to distinguish fetal growth restriction from low birth weight due to prematurity. HDP was defined using problem lists/diagnostic codes for gestational hypertension or preeclampsia during the current pregnancy. PTB was missing for 57 births and SGA for 76 births due to implausible values.
In a secondary analysis, we examined preterm birth in more detail by classifying preterm births as spontaneous and medically indicated. Spontaneous preterm birth was defined as birth following premature rupture of membranes or preterm labor, while medically indicated preterm birth was defined as birth after labor induction or cesarean section without labor for a medical complication (e.g., hypertensive disorder of pregnancy). We also examined very preterm birth, defined as gestational age < 32 weeks.
Covariates
Individual-level covariates were extracted from the EHR and included a priori selected factors hypothesized to confound associations between neighborhood physical disorder and adverse pregnancy outcomes: maternal age, race/ethnicity, insurance status (private, public, none), multiparity, and season of the birth. We included a quadratic term for maternal age to account for non-linearity in the relationship between maternal age and birth outcomes. Race/ethnicity categories included Black/African American, White, Hispanic/Latino, Asian/Pacific Islander, other race, and unknown race. We also extracted maternal health conditions which we considered potential mediators: gestational diabetes in the current pregnancy, prevalent diagnosis of hypertension or diabetes, history of asthma, history of a mental health issue, and history of substance use (including alcohol or tobacco use in current pregnancy). Neighborhood poverty was defined using the 2012–2016 American Communities Survey as the proportion of the mother’s census tract population with household incomes below the federally-defined poverty line.
Statistical Analysis
We examined the distribution of outcomes and covariates between mothers living in neighborhoods with high versus low physical disorder (defined as the top tertile versus the bottom two tertiles of the log-transformed latent physical disorder score). We also examined the distribution of covariates among women with and without each adverse pregnancy outcome. We then used three-level hierarchical models to estimate associations of neighborhood physical disorder with PTB, SGA, and HDP, with random effects to account for the nesting of births within mothers and mothers within census tracts. We used a Poisson distribution with robust variance estimates [42] in order to calculate prevalence ratios. We first ran an unconditional model to estimate the intraclass correlation coefficient, or proportion of the variance in each outcome attributable to differences across census tracts. Then, we added neighborhood physical disorder category to estimate unadjusted associations with birth outcomes (model 1). We then progressively adjusted for covariates as follow: model 2 adjusted for mother’s age, mothers age squared, race/ethnicity, insurance status, multiparity, and season; model 3 additionally adjusted for neighborhood poverty; and model 4 additionally adjusted for maternal health conditions (gestational diabetes, prevalent hypertension, prevalent diabetes, history of asthma, history of mental health issue, history of substance abuse). Finally, in a secondary analysis, we estimated associations of neighborhood physical disorder with spontaneous PTB, medically indicated PTB, and very PTB using the modeling approach described above.
Results
Google Street View imagery dates ranged from September 2007 to April 2018, with 94% of block faces having imagery captured in 2015–2017. Across blocks, the prevalence of the individual physical disorder items ranged from 1.6% for abandoned vehicles to 29.3% for bars on windows/doors (Table 1). Percent agreement for blocks coded by two raters ranged from 76.7 to 98.8%, and kappas ranged from 0.44 to 0.67 (reflecting moderate agreement). The internal consistency of the latent neighborhood physical disorder measure was 0.82, suggesting that the physical disorder items measure a consistent underlying construct. Item severities ranged from 1.17 (fairly common) for moderate/heavy trash to 4.55 (very rare) for abandoned vehicles. Item discriminations ranged from 0.54 (weak) for bars on windows to 1.76 (strong) for buildings in poor/deteriorated condition. The wide range of severities suggests that the physical disorder scale can pick up variation at a wide range of latent levels of physical disorder. Neighborhood physical disorder was moderately correlated with neighborhood poverty (Spearman correlation coefficient 0.46).
Of 14,309 births, 48% were among white women, 18% Hispanic/Latina, and 9% were among Black/African American women (Table 2). Participants living in neighborhoods in the highest disorder tertile were younger on average, more likely to be Hispanic/Latino or Black/African American, publicly insured, and multiparous than women in neighborhoods with lower disorder scores. They were more likely to have a history of asthma and substance use, prevalent hypertension, and gestational diabetes, and to live in higher-poverty neighborhoods. In addition, the prevalence of each adverse pregnancy outcome was highest among women in the neighborhoods with high physical disorder. All three adverse pregnancy outcomes were more common among women who were Black/African American, publicly insured, had a history of asthma or substance use, had prevalent hypertension, had gestational diabetes, or lived in higher-poverty neighborhoods (Table 3). Patterns varied for other covariates.
Table 2.
Characteristics of the study population by neighborhood physical disorder
| Overall | Low neighborhood physical disordera N (column %) |
High neighborhood physical disordera N (column %) |
|
|---|---|---|---|
| N | 14309 | 9547 | 4762 |
| Maternal age—mean (SD) | 31.7 (5.1) | 32.4 (4.6) | 30.2 (5.7) |
| Race | |||
| White | 6888 (48.1) | 5290 (55.4) | 1598 (33.5) |
| Hispanic/Latino | 2533 (17.7) | 1035 (10.8) | 1498 (31.5) |
| Black/African American | 1336 (9.3) | 653 (6.8) | 683 (14.3) |
| Asian/Pacific Islander | 1230 (8.6) | 998 (10.5) | 232 (4.9) |
| Other race | 1202 (8.4) | 793 (8.3) | 409 (8.6) |
| Unknown race | 1120 (7.8) | 778 (8.2) | 342 (7.2) |
| Insurance status | |||
| Private | 11331 (79.2) | 8420 (88.2) | 2911 (61.1) |
| Public | 2928 (20.5) | 1093 (11.4) | 1835 (38.5) |
| None | 50 (0.3) | 34 (0.4) | 16 (0.4) |
| Multiparous | 6559 (45.8) | 4065 (42.6) | 2494 (52.4) |
| History of asthma | 1370 (9.6) | 853 (8.9) | 517 (10.9) |
| History of mental health condition | 1403 (9.8) | 931 (9.8) | 472 (9.9) |
| History of substance use | 131 (0.9) | 68 (0.7) | 63 (1.3) |
| Prevalent hypertension | 199 (1.4) | 97 (1.0) | 102 (2.1) |
| Prevalent diabetes | 146 (1.0) | 84 (0.9) | 62 (1.3) |
| Gestational diabetes | 698 (4.9) | 403 (4.2) | 295 (6.2) |
| Infant sex | |||
| Male | 7301 (51.0) | 4878 (51.1) | 2423 (50.9) |
| Female | 7008 (49.0) | 4669 (48.9) | 2339 (49.1) |
| Percent of census tract below poverty level—mean (SD) | 15.9 (10.9) | 12.4 (8.4) | 23.0 (11.9) |
| Adverse pregnancy outcomesb | |||
| Preterm birth | 1082 (7.6) | 644 (6.8) | 438 (9.2) |
| Spontaneous preterm birth | 672 (4.7) | 398 (4.2) | 274 (5.8) |
| Induced preterm birth | 410 (2.9) | 246 (2.6) | 164 (3.4) |
| Very preterm birth | 267 (1.9) | 149 (1.6) | 118 (2.5) |
| Small for gestational age | 1469 (10.3) | 924 (9.7) | 545 (11.5) |
| Hypertensive disorder of pregnancy | 938 (6.6) | 572 (6.0) | 366 (7.7) |
aHigh neighborhood physical disorder was defined as living in a neighborhood in the highest tertile of log-transformed physical disorder scores (range − 0.13 to 0.52). Low neighborhood physical disorder was defined as living in a neighborhood in the lower two tertiles (range − 0.86 to − 0.13)
bMissing outcomes due to implausible values: preterm birth, n = 57; small for gestational age, n = 76
Table 3.
Characteristics of the study population by adverse pregnancy outcomes
| Preterm birtha | Small for gestational agea | Hypertensive disorder of pregnancy | ||||
|---|---|---|---|---|---|---|
| Yes N (column %) |
No N (column %) |
Yes N (column %) |
No N (column %) |
Yes N (column %) |
No N (column %) |
|
| N | 1082 | 13170 | 1469 | 12764 | 938 | 13371 |
| Maternal age—mean (SD) | 31.4 (5.5) | 31.7 (5.0) | 30.9 (5.5) | 31.8 (5.0) | 31.9 (5.5) | 31.6 (5.1) |
| Race | ||||||
| White | 441 (40.8) | 6419 (48.7) | 553 (37.6) | 6302 (49.4) | 434 (46.3) | 6454 (48.3) |
| Hispanic/Latino | 217 (20.1) | 2306 (17.5) | 248 (16.9) | 2273 (17.8) | 161 (17.1) | 2372 (17.7) |
| Black/African American | 158 (14.6) | 1173 (8.9) | 218 (14.9) | 1107 (8.7) | 149 (15.9) | 1187 (8.9) |
| Asian/Pacific Islander | 59 (5.4) | 1166 (8.9) | 196 (13.3) | 1029 (8.0) | 44 (4.7) | 1186 (8.9) |
| Other race | 111 (10.2) | 1089 (8.3) | 139 (9.5) | 1057 (8.3) | 71 (7.6) | 1131 (8.4) |
| Unknown race | 96 (8.9) | 1017 (7.7) | 115 (7.8) | 996 (7.8) | 79 (8.4) | 1041 (7.8) |
| Insurance status | ||||||
| Private | 775 (71.6) | 10511 (79.8) | 1094 (74.5) | 10181 (79.8) | 702 (74.8) | 10629 (79.5) |
| Public | 304 (28.1) | 2613 (19.8) | 370 (25.2) | 2539 (19.9) | 234 (25.0) | 2694 (20.1) |
| None | 3 (0.3) | 46 (0.4) | 5 (0.3) | 44 (0.3) | 2 (0.2) | 48 (0.4) |
| Multiparous | 473 (43.7) | 6063 (46.0) | 531 (36.2) | 5994 (47.0) | 352 (37.5) | 6207 (46.4) |
| History of asthma | 123 (11.4) | 1240 (9.4) | 154 (10.5) | 1208 (9.5) | 116 (12.4) | 1254 (9.4) |
| History of mental health condition | 142 (13.1) | 1253 (9.5) | 127 (8.7) | 1266 (9.9) | 115 (12.3) | 1288 (9.6) |
| History of substance use | 19 (1.8) | 111 (0.8) | 32 (2.2) | 95 (0.7) | 15 (1.6) | 116 (0.9) |
| Prevalent hypertension | 52 (4.8) | 147 (1.1) | 28 (1.9) | 169 (1.3) | 111 (11.8) | 88 (0.7) |
| Prevalent diabetes | 38 (3.5) | 106 (0.8) | 4 (0.3) | 140 (1.1) | 27 (2.9) | 119 (0.9) |
| Gestational diabetes | 91 (8.4) | 601 (4.6) | 77 (5.2) | 615 (4.8) | 92 (9.8) | 606 (4.5) |
| Infant sex | ||||||
| Male | 586 (54.2) | 6689 (50.8) | 750 (51.1) | 6518 (51.1) | 463 (49.4) | 6838 (51.1) |
| Female | 496 (45.8) | 6481 (49.2) | 719 (48.9) | 6246 (48.9) | 475 (50.6) | 6533 (48.9) |
| Proportion of tract below poverty level—mean (SD) | 18.2 (12.1) | 15.8 (10.8) | 17.7 (12.0) | 15.7 (10.8) | 17.6 (11.9) | 15.8 (10.8) |
aMissing outcomes due to implausible values: preterm birth: n = 57; small for gestational age: n = 76
Intraclass correlation coefficients for adverse pregnancy outcomes ranged from 2 to 4%. In unadjusted models, mothers living in neighborhoods in the highest tertile of physical disorder had higher prevalence of all three outcomes compared to mothers living in neighborhoods with lower levels of physical disorder (Table 4; prevalence ratios (PRs) as follows: PTB 1.37, 95% CI 1.20, 1.56; SGA 1.21, 95% CI 1.09, 1.35; HDP 1.28, 95% CI 1.12, 1.47). Adjustment for maternal age, race/ethnicity, insurance status, parity, and season of birth (model 2) reduced prevalence ratios to 1.21 (1.06, 1.39) for PTB, 1.13 (1.01, 1.37) for SGA, and 1.23 (1.07, 1.42) for HDP. After adjustment for neighborhood poverty (model 3), point estimates were further attenuated, and confidence intervals crossed the null for PTB and SGA, but not HDP (PRs and 95% CIs of 1.14 (0.99, 1.31), 1.08 (0.95, 1.23), and 1.18 (1.02, 1.37), respectively). Subsequent adjustment for maternal health conditions, which we conceived of as potential mediators, further attenuated estimates for PTB and HDP (Table 4). In a secondary analysis of preterm birth etiologies, patterns for spontaneous and medically indicated preterm births were similar to the associations estimated for any preterm birth (Table 5). Initial associations were attenuated with progressive covariate adjustment. Patterns were similar for the outcome of very preterm birth (< 32 weeks; Table 5).
Table 4.
Associations of neighborhood physical disorder with adverse pregnancy outcomes (n = 14,309 births)a,b
| Association of high versus low neighborhood physical disorder | Preterm birth—prevalence ratio (95% CI) | Small for gestational age—prevalence ratio (95% CI) | Hypertensive disorder of pregnancy—prevalence ratio (95% CI) |
|---|---|---|---|
| Model 1—unadjusted | 1.37 (1.20, 1.56) | 1.21 (1.09, 1.35) | 1.28 (1.12 1.47) |
| Model 2—adjusted for maternal confounders | 1.21 (1.06, 1.39) | 1.13 (1.01, 1.27) | 1.23 (1.07, 1.42) |
| Model 3—model 2 + neighborhood poverty | 1.14 (0.99, 1.31) | 1.08 (0.95, 1.23) | 1.18 (1.02, 1.37) |
| Model 4—model 3 + maternal health conditions | 1.11 (0.96, 1.28) | 1.08 (0.95, 1.22) | 1.09 (0.95, 1.26) |
aHigh neighborhood physical disorder was defined as living in a neighborhood in the highest tertile of log-transformed physical disorder scores (range − 0.13 to 0.52). Low neighborhood physical disorder was defined as living in a neighborhood in the lower two tertiles (range − 0.86 to − 0.13)
bModel 1: unadjusted. Model 2: adjusted for maternal age, maternal age squared, race/ethnicity, insurance status, multiparity, and season of birth. Model 3: adjusted for neighborhood poverty rate. Model 4: adjusted for maternal health conditions (gestational diabetes, prevalent hypertension, prevalent diabetes, history of asthma, history of mental health concern, history of substance use)
Table 5.
Associations of neighborhood physical disorder with preterm birth subtypes (n = 14,309 births)a,b
| Association of high versus low neighborhood physical disorder | Spontaneous preterm birth—prevalence ratio (95% CI) | Medically indicated preterm birth—prevalence ratio (95% CI) | Very preterm birthc—prevalence ratio (95% CI) |
|---|---|---|---|
| Model 1—unadjusted | 1.36 (1.11, 1.66) | 1.34 (1.10, 1.63) | 1.59 (1.22, 2.07) |
| Model 2—adjusted for maternal confounders | 1.23 (0.99, 1.53) | 1.21 (0.98, 1.51) | 1.24 (0.94, 1.64) |
| Model 3—model 2 + neighborhood poverty | 1.12 (0.98, 1.42) | 1.11 (0.88, 1.41) | 1.07 (0.80, 1.44) |
| Model 4—model 3 + maternal health conditions | 1.10 (0.87, 1.39) | 1.09 (0.86, 1.37) | 1.02 (0.76, 1.38) |
aHigh neighborhood physical disorder was defined as living in a neighborhood in the highest tertile of log-transformed physical disorder scores (range − 0.13 to 0.52). Low neighborhood physical disorder was defined as living in a neighborhood in the lower two tertiles (range − 0.86 to − 0.13)
bModel 1: unadjusted. Model 2: adjusted for maternal age, maternal age squared, race/ethnicity, insurance status, multiparity, and season of birth. Model 3: adjusted for neighborhood poverty rate. Model 4: adjusted for maternal health conditions (gestational diabetes, prevalent hypertension, prevalent diabetes, history of asthma, history of mental health concern, history of substance use)
cDefined as gestational age < 32 weeks
Discussion
In this analysis of EHR data from women in Chicago, we found that higher levels of neighborhood physical disorder (measured via virtual audit in Google Street View) were associated with higher prevalence of PTB, SGA, and HDP after adjusting for maternal characteristics and season of birth. After adjustment for neighborhood poverty, confidence intervals crossed the null for PTB and SGA but not for HDP.
Neighborhood physical disorder is hypothesized to increase the risk of adverse pregnancy outcomes through increasing psychological stress among pregnant women. Signs of physical disorder may cause residents to lose confidence in their neighborhood’s ability to intervene in threatening situations and prevent crime, which may increase stress and fear of crime [43]. Stress during pregnancy may result in neuroendocrine and inflammatory dysregulation that may trigger spontaneous PTB [20, 21, 44]. Stress is also linked to adverse coping mechanisms including smoking [18, 25] and unhealthy diet [45] among pregnant women. Finally, neighborhood physical disorder might discourage women from engaging in physical activity during pregnancy [19] which is associated with lower risk of adverse maternal outcomes like HDP [46, 47]. Our results provide some support for an association between neighborhood physical disorder and adverse pregnancy outcomes, although the magnitude of association was small.
Past findings regarding associations between neighborhood physical disorder and adverse pregnancy outcomes have been mixed. Although physical disorder has been measured in different ways, including using administrative data [12, 48–50] and participant perceptions [12], our findings can be most closely compared to other studies that used systematic social observation to assess indicators of physical disorder. For example, two prior studies in North Carolina used in-person systematic social observations to identify neighborhood “incivilities,” a similar construct incorporating features like litter, building condition, and presence of abandoned or boarded-up buildings. Physical incivilities were associated with pregnancy outcomes including HDP, PTB, and LBW among white women but not black women [18, 25], although in one study, associations varied across different geographical specifications of the neighborhood [25]. A third study, also in North Carolina, audited tax parcels for signs of housing damage (e.g., boarded up windows or doors) and signs of disorder (e.g., trash) in private and public spaces and found housing damage to be associated with SGA and LBW [26]. Our study differed from prior work in several ways. First, these prior studies using in-person systematic social observations did not adjust for neighborhood poverty, which attenuated associations for PTB and SGA in our study. Second, we used an IRT model to estimate physical disorder as a latent construct based on multiple measured indicators. This approach accounts for the complexity of neighborhood domains like physical disorder and the possibility that the presence of certain physical disorder indicators may indicate a greater degree of latent physical disorder than others [39] (e.g., abandoned buildings as opposed to litter). Finally, prior studies have typically used birth certificate data, which might underreport obstetric procedures and maternal and infant medical conditions [51–53]. EHR data, as used in our study, provides an alternative data source that might more reliably capture these measures, although it is not without limitations, as noted below.
Our finding that adjustment for neighborhood poverty attenuated associations between physical disorder and adverse pregnancy outcomes for PTB and SGA underscores the challenge of disentangling the effects of neighborhood poverty from more proximal neighborhood features. Neighborhood physical disorder and poverty were moderately correlated in our analysis and have been found to be correlated in past studies [18, 54]. Neighborhoods with higher poverty rates tend to have higher levels of physical disorder, and physical signs of disorder may also deter future investment in the neighborhood [55]. Disentangling complex neighborhood attributes is a challenging area that would benefit from future research. For example, positive neighborhood social attributes (e.g., social cohesion, social support, and participation in local organizations) have been found to have protective associations with pregnancy outcomes [56, 57] and might buffer harmful effects of neighborhood stressors, although this area remains understudied. We lacked information on these measures in the current study, so we were unable to examine how these factors may relate to physical disorder or pregnancy outcomes in our study population.
Our study is novel in using Google Street View and EHR data to examine associations of neighborhood physical disorder with adverse pregnancy outcomes. However, several limitations should be noted. First, we used census tracts to define neighborhoods, which may not accurately capture study participants’ own neighborhood definitions. We linked physical disorder scores based on women’s home addresses at the time of delivery but lacked information on neighborhoods where they worked or spent significant amounts of time away from home. We also lacked information on how long they had lived in their neighborhood and on their perceptions of neighborhood physical disorder, which may be more biologically proximal to pregnancy outcomes than objectively defined measures. Our use of Google Street View, while novel in the context of pregnancy outcomes, also has limitations. Physical disorder was assessed at only one time point for each census tract. In addition, we did not validate our virtual ratings against in-person ratings. However, a prior study that used a similar physical disorder scale to conduct both virtual and in-person audits found that the two approaches identified the same neighborhoods as having high physical disorder and concluded that Google Street View-based audits could substitute for in-person assessments with little loss of precision [35]. Finally, our approach of auditing one block per census tract may have resulted in misclassification of level of neighborhood physical disorder. However, the average area of Chicago census tracts is relatively small (0.8 km) and prior studies that used Google Street View audit paired with spatial interpolation have conducted audits on a similar scale (e.g., using a 1–2-km grid) [32, 37]. Our use of kriging allowed us to take spatial relationships into account when calculating census tract physical disorder scores, rather than simply assigning the value estimated based on the single audited block.
A strength of this study is the relatively large sample size available through EHR data. EHRs provide an opportunity for future longitudinal assessments that may strengthen causal inference by examining whether changes in adverse pregnancy outcomes follow changes in neighborhood physical disorder. Another benefit of EHR data is the availability of more granular data on maternal health conditions and etiology of preterm birth relative to the more commonly used birth certificates data. However, EHR systems are designed for patient care rather than research purposes and are also subject to limitations. Our EHR data did not contain information on diet or physical activity. Also, pre-pregnancy body mass index and gestational weight gain were captured inconsistently. We adjusted for reported history of substance abuse in our final models, but this variable did not distinguish between current or prior use, and may have been subject to recall or social desirability bias. In addition, our study population came from a single hospital in one city, which may limit the generalizability of findings. Finally, there may be residual confounding by unmeasured neighborhood-level variables (e.g., differences in neighborhood social norms or social cohesion that may buffer stress or support protective behaviors during pregnancy).
Conclusion
We found modest associations between neighborhood physical disorder and adverse pregnancy outcomes among women delivering at a large, academic women’s hospital in Chicago. Future work is needed to disentangle the unique contribution of physical disorder from other characteristics of disadvantaged neighborhoods.
Electronic supplementary material
(DOCX 14 kb)
Acknowledgments
We thank Allison Mo, Angelina Jose, Argie Claro, Hussain Ali, Jennifer Abel, Julia Davis, Lynn Vo, Meghan Murphy, and Simona Rachapalli for their assistance with conducting the neighborhood audits.
Funding information
This research was supported by an NHLBI Training Grant in Cardiovascular Epidemiology and Prevention (award number T32HL069771) and by the Northwestern Medicine Enterprise Data Warehouse Pilot Data Program from the Northwestern University Clinical and Translational Sciences Institute (NUCATS).
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Callaghan WM, MacDorman MF, Rasmussen SA, Qin C, Lackritz EM. The contribution of preterm birth to infant mortality rates in the United States. Pediatrics. 2006;118(4):1566–1573. doi: 10.1542/peds.2006-0860. [DOI] [PubMed] [Google Scholar]
- 2.Barker DJ, Eriksson JG, Forsen T, Osmond C. Fetal origins of adult disease: strength of effects and biological basis. Int J Epidemiol. 2002;31(6):1235–1239. doi: 10.1093/ije/31.6.1235. [DOI] [PubMed] [Google Scholar]
- 3.Rich-Edwards JW, Colditz GA, Stampfer MJ, et al. Birthweight and the risk for type 2 diabetes mellitus in adult women. Ann Intern Med. 1999;130(4 Pt 1):278–284. doi: 10.7326/0003-4819-130-4_part_1-199902160-00005. [DOI] [PubMed] [Google Scholar]
- 4.Stewart AL, Rifkin L, Amess PN, et al. Brain structure and neurocognitive and behavioural function in adolescents who were born very preterm. Lancet. 1999;353(9165):1653–1657. doi: 10.1016/s0140-6736(98)07130-x. [DOI] [PubMed] [Google Scholar]
- 5.Valdiviezo C, Garovic VD, Ouyang P. Preeclampsia and hypertensive disease in pregnancy: their contributions to cardiovascular risk. Clin Cardiol. 2012;35(3):160–165. doi: 10.1002/clc.21965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Catov JM, Wu CS, Olsen J, Sutton-Tyrrell K, Li J, Nohr EA. Early or recurrent preterm birth and maternal cardiovascular disease risk. Ann Epidemiol. 2010;20(8):604–609. doi: 10.1016/j.annepidem.2010.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ncube CN, Enquobahrie DA, Albert SM, Herrick AL, Burke JG. Association of neighborhood context with offspring risk of preterm birth and low birthweight: a systematic review and meta-analysis of population-based studies. Soc Sci Med. 2016;153:156–164. doi: 10.1016/j.socscimed.2016.02.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Metcalfe A, Lail P, Ghali WA, Sauve RS. The association between neighbourhoods and adverse birth outcomes: a systematic review and meta-analysis of multi-level studies. Paediatr Perinat Epidemiol. 2011;25(3):236–245. doi: 10.1111/j.1365-3016.2011.01192.x. [DOI] [PubMed] [Google Scholar]
- 9.Vos AA, Posthumus AG, Bonsel GJ, Steegers EA, Denktas S. Deprived neighborhoods and adverse perinatal outcome: a systematic review and meta-analysis. Acta Obstet Gynecol Scand. 2014;93(8):727–740. doi: 10.1111/aogs.12430. [DOI] [PubMed] [Google Scholar]
- 10.Cohen DA, Mason K, Bedimo A, Scribner R, Basolo V, Farley TA. Neighborhood physical conditions and health. Am J Public Health. 2003;93(3):467–471. doi: 10.2105/ajph.93.3.467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Franzini L, Elliott MN, Cuccaro P, et al. Influences of physical and social neighborhood environments on children’s physical activity and obesity. Am J Public Health. 2009;99(2):271–278. doi: 10.2105/AJPH.2007.128702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Giurgescu C, Zenk SN, Templin TN, Engeland CG, Kavanaugh K, Misra DP. The impact of neighborhood conditions and psychological distress on preterm birth in African-American women. Public Health Nurs. 2017;34(3):256–266. doi: 10.1111/phn.12305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cutrona CE, Russell DW, Hessling RM, Brown PA, Murry V. Direct and moderating effects of community context on the psychological well-being of African American women. J Pers Soc Psychol. 2000;79(6):1088–1101. doi: 10.1037//0022-3514.79.6.1088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ross CE. Neighborhood disadvantage and adult depression. J Health Soc Behav. 2000;41(2):177–187. [Google Scholar]
- 15.Mendes de Leon CF, Cagney KA, Bienias JL, et al. Neighborhood social cohesion and disorder in relation to walking in community-dwelling older adults: a multilevel analysis. J Aging Health. 2009;21(1):155–171. doi: 10.1177/0898264308328650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kwarteng JL, Schulz AJ, Mentz GB, Zenk SN, Opperman AA. Associations between observed neighborhood characteristics and physical activity: findings from a multiethnic urban community. J Public Health (Oxf) 2014;36(3):358–367. doi: 10.1093/pubmed/fdt099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Furr-Holden CD, Lee MH, Johnson R, et al. Neighborhood environment and marijuana use in urban young adults. Prev Sci. 2015;16(2):268–278. doi: 10.1007/s11121-014-0497-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Vinikoor-Imler LC, Messer LC, Evenson KR, Laraia BA. Neighborhood conditions are associated with maternal health behaviors and pregnancy outcomes. Soc Sci Med. 2011;73(9):1302–1311. doi: 10.1016/j.socscimed.2011.08.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Laraia B, Messer L, Evenson K, Kaufman JS. Neighborhood factors associated with physical activity and adequacy of weight gain during pregnancy. J Urban Health. 2007;84(6):793–806. doi: 10.1007/s11524-007-9217-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hobel C, Culhane J. Role of psychosocial and nutritional stress on poor pregnancy outcome. J Nutr. 2003;133(5 Suppl 2):1709s–1717s. doi: 10.1093/jn/133.5.1709S. [DOI] [PubMed] [Google Scholar]
- 21.Rich-Edwards JW, Grizzard TA. Psychosocial stress and neuroendocrine mechanisms in preterm delivery. Am J Obstet Gynecol. 2005;192(5 Suppl):S30–S35. doi: 10.1016/j.ajog.2005.01.072. [DOI] [PubMed] [Google Scholar]
- 22.Dunkel SC. Psychological science on pregnancy: stress processes, biopsychosocial models, and emerging research issues. Annu Rev Psychol. 2011;62:531–558. doi: 10.1146/annurev.psych.031809.130727. [DOI] [PubMed] [Google Scholar]
- 23.Nowak AL, Giurgescu C. The built environment and birth outcomes: a systematic review. MCN Am J Matern Child Nurs. 2017;42(1):14–20. doi: 10.1097/NMC.0000000000000299. [DOI] [PubMed] [Google Scholar]
- 24.Raudenbush SW, Sampson RJ. Ecometrics: toward a science of assessing ecological settings, with application to the systematic social observation of neighborhoods. Sociol Methodol. 1999;29:1–41. [Google Scholar]
- 25.Messer LC, Vinikoor-Imler LC, Laraia BA. Conceptualizing neighborhood space: consistency and variation of associations for neighborhood factors and pregnancy health across multiple neighborhood units. Health Place. 2012;18(4):805–813. doi: 10.1016/j.healthplace.2012.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Miranda ML, Messer LC, Kroeger GL. Associations between the quality of the residential built environment and pregnancy outcomes among women in North Carolina. Environ Health Perspect. 2012;120(3):471–477. doi: 10.1289/ehp.1103578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bader MD, Mooney SJ, Lee YJ, et al. Development and deployment of the Computer Assisted Neighborhood Visual Assessment System (CANVAS) to measure health-related neighborhood conditions. Health Place. 2015;31:163–172. doi: 10.1016/j.healthplace.2014.10.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Odgers CL, Caspi A, Bates CJ, Sampson RJ, Moffitt TE. Systematic social observation of children's neighborhoods using Google Street View: a reliable and cost-effective method. J Child Psychol Psychiatry. 2012;53(10):1009–1017. doi: 10.1111/j.1469-7610.2012.02565.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kepper MM, Sothern MS, Theall KP, et al. A reliable, feasible method to observe neighborhoods at high spatial resolution. Am J Prev Med. 2017;52(1S1):S20–S30. doi: 10.1016/j.amepre.2016.06.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Marco M, Gracia E, Martin-Fernandez M, Lopez-Quilez A. Validation of a Google Street View-based neighborhood disorder observational scale. J Urban Health. 2017;94(2):190–198. doi: 10.1007/s11524-017-0134-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Mooney SJ, Joshi S, Cerda M, Kennedy GJ, Beard JR, Rundle AG. Neighborhood disorder and physical activity among older adults: a longitudinal study. J Urban Health. 2017;94(1):30–42. doi: 10.1007/s11524-016-0125-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Quinn JW, Mooney SJ, Sheehan DM, et al. Neighborhood physical disorder in New York City. J Maps. 2016;12(1):53–60. doi: 10.1080/17445647.2014.978910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Rundle AG, Bader MD, Richards CA, Neckerman KM, Teitler JO. Using Google Street View to audit neighborhood environments. Am J Prev Med. 2011;40(1):94–100. doi: 10.1016/j.amepre.2010.09.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Wu YT, Nash P, Barnes LE, et al. Assessing environmental features related to mental health: a reliability study of visual streetscape images. BMC Public Health. 2014;14:1094. doi: 10.1186/1471-2458-14-1094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Mooney SJ, Bader MDM, Lovasi GS, et al. Street audits to measure neighborhood disorder: virtual or in-person? Am J Epidemiol. 2017;186(3):265–273. doi: 10.1093/aje/kwx004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Mayne Stephanie, Jose Angelina, Mo Allison, Vo Lynn, Rachapalli Simona, Ali Hussain, Davis Julia, Kershaw Kiarri. Neighborhood Disorder and Obesity-Related Outcomes among Women in Chicago. International Journal of Environmental Research and Public Health. 2018;15(7):1395. doi: 10.3390/ijerph15071395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Mooney SJ, Bader MD, Lovasi GS, Neckerman KM, Teitler JO, Rundle AG. Validity of an ecometric neighborhood physical disorder measure constructed by virtual street audit. Am J Epidemiol. 2014;180(6):626–635. doi: 10.1093/aje/kwu180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Feinstein AR, Cicchetti DV. High agreement but low kappa: I. The problems of two paradoxes. J Clin Epidemiol. 1990;43(6):543–549. doi: 10.1016/0895-4356(90)90158-l. [DOI] [PubMed] [Google Scholar]
- 39.Bader MDM, Ailshire JA. Creating measures of theoretically relevant neighborhood attributes at multiple spatial scales. Sociol Methodol. 2014;44:322–368. doi: 10.1177/0081175013516749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Knake LA, Ahuja M, McDonald EL, et al. Quality of EHR data extractions for studies of preterm birth in a tertiary care center: guidelines for obtaining reliable data. BMC Pediatr. 2016;16:59. doi: 10.1186/s12887-016-0592-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Duryea EL, Hawkins JS, McIntire DD, Casey BM, Leveno KJ. A revised birth weight reference for the United States. Obstet Gynecol. 2014;124(1):16–22. doi: 10.1097/AOG.0000000000000345. [DOI] [PubMed] [Google Scholar]
- 42.Zou G. A modified poisson regression approach to prospective studies with binary data. Am J Epidemiol. 2004;159(7):702–706. doi: 10.1093/aje/kwh090. [DOI] [PubMed] [Google Scholar]
- 43.Perkins DD, Meeks JW, Taylor RB. The physical-environment of street blocks and resident perceptions of crime and disorder - implications for theory and measurement. J Environ Psychol. 1992;12(1):21–34. [Google Scholar]
- 44.Culhane JF, Elo IT. Neighborhood context and reproductive health. Am J Obstet Gynecol. 2005;192(5 Suppl):S22–S29. doi: 10.1016/j.ajog.2005.01.071. [DOI] [PubMed] [Google Scholar]
- 45.Hurley KM, Caulfield LE, Sacco LM, Costigan KA, Dipietro JA. Psychosocial influences in dietary patterns during pregnancy. J Am Diet Assoc. 2005;105(6):963–966. doi: 10.1016/j.jada.2005.03.007. [DOI] [PubMed] [Google Scholar]
- 46.Saftlas AF, Logsden-Sackett N, Wang W, Woolson R, Bracken MB. Work, leisure-time physical activity, and risk of preeclampsia and gestational hypertension. Am J Epidemiol. 2004;160(8):758–765. doi: 10.1093/aje/kwh277. [DOI] [PubMed] [Google Scholar]
- 47.Sorensen TK, Williams MA, Lee IM, Dashow EE, Thompson ML, Luthy DA. Recreational physical activity during pregnancy and risk of preeclampsia. Hypertension. 2003;41(6):1273–1280. doi: 10.1161/01.HYP.0000072270.82815.91. [DOI] [PubMed] [Google Scholar]
- 48.Reagan PB, Salsberry PJ. Race and ethnic differences in determinants of preterm birth in the USA: broadening the social context. Soc Sci Med. 2005;60(10):2217–2228. doi: 10.1016/j.socscimed.2004.10.010. [DOI] [PubMed] [Google Scholar]
- 49.Farley TA, Mason K, Rice J, Habel JD, Scribner R, Cohen DA. The relationship between the neighbourhood environment and adverse birth outcomes. Paediatr Perinat Epidemiol. 2006;20(3):188–200. doi: 10.1111/j.1365-3016.2006.00719.x. [DOI] [PubMed] [Google Scholar]
- 50.Schempf A, Strobino D, O'Campo P. Neighborhood effects on birthweight: an exploration of psychosocial and behavioral pathways in Baltimore, 1995--1996. Soc Sci Med. 2009;68(1):100–110. doi: 10.1016/j.socscimed.2008.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Lydon-Rochelle MT, Holt VL, Cardenas V, et al. The reporting of pre-existing maternal medical conditions and complications of pregnancy on birth certificates and in hospital discharge data. Am J Obstet Gynecol. 2005;193(1):125–134. doi: 10.1016/j.ajog.2005.02.096. [DOI] [PubMed] [Google Scholar]
- 52.Schoendorf KC, Branum AM. The use of United States vital statistics in perinatal and obstetric research. Am J Obstet Gynecol. 2006;194(4):911–915. doi: 10.1016/j.ajog.2005.11.020. [DOI] [PubMed] [Google Scholar]
- 53.Zollinger TW, Przybylski MJ, Gamache RE. Reliability of Indiana birth certificate data compared to medical records. Ann Epidemiol. 2006;16(1):1–10. doi: 10.1016/j.annepidem.2005.03.005. [DOI] [PubMed] [Google Scholar]
- 54.Wei E, Hipwell A, Pardini D, Beyers JM, Loeber R. Block observations of neighbourhood physical disorder are associated with neighbourhood crime, firearm injuries and deaths, and teen births. J Epidemiol Community Health. 2005;59(10):904–908. doi: 10.1136/jech.2004.027060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Sampson RJ, Raudenbush SW. Systematic social observation of public spaces: a new look at disorder in urban neighborhoods. Am J Sociol. 1999;105(3):603–651. [Google Scholar]
- 56.Buka SL, Brennan RT, Rich-Edwards JW, Raudenbush SW, Earls F. Neighborhood support and the birth weight of urban infants. Am J Epidemiol. 2003;157(1):1–8. doi: 10.1093/aje/kwf170. [DOI] [PubMed] [Google Scholar]
- 57.Morenoff JD. Neighborhood mechanisms and the spatial dynamics of birth weight. Ajs. 2003;108(5):976–1017. doi: 10.1086/374405. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX 14 kb)