Abstract
Newborn Screening (NBS) is a State-run program that mandates all newborns to be screened for a panel of medical conditions to reduce infant mortality and morbidity. Medicaid is a public health insurance program that expanded access to care for low-income infants. NBS mandates and Medicaid rolled out state-by-state in the 1960s, 70s, and 80s, which are considered significant programs that improved infant health in the latter half of the 20th Century. This article utilized variation in States’ timing of NBS mandates and Medicaid implementation to examine changes in infant mortality rates among white and African American infants associated with NBS, Medicaid, and their interaction. The analyses used data from birth and death certificates in the US Vital Statistics from 1959 to 1995. We find that the implementation of NBS mandates alone was not associated with significant declines in infant mortality and coincided with increases in within-state racial inequities. States experienced mortality declines and reduction in racial inequities after implementing Medicaid with NBS mandates.
Keywords: Newborn screening, Medicaid, Infant mortality, Race inequity
Highlights
-
•
Newborn screening (NBS) mandates was not linked to significant declines in infant mortality in states with no Medicaid.
-
•
NBS in non-Medicaid states initially increased racial inequities in infant mortality.
-
•
NBS was associated with improvements in infant mortality in states with Medicaid.
-
•
Racial inequities in infant mortality narrowed after NBS in Medicaid states.
1. Introduction
Newborn screening (NBS) is a state-run, public health program that screens 98% of approximately 4 million US newborns for a minimum of 29 genetic, endocrine, metabolic, and immune disorders not apparent at birth, resulting in approximately 12,000 diagnoses every year (Boyle, Bocchini, & Kelly, 2014). The Newborn Screening Saves Lives Act of 2007, and its successor Reauthorization Act of 2014, strengthened federal support for broad and comprehensive newborn screening (2014 federal [P.L 113–240] “Newborn Screening Saves Lives Reauthorization Act”). Advocates highlight the importance of early detection to initiate critical early intervention, reduce morbidity, and to prevent death (Urv & Parisi, 2017, pp. 323–346). NBS advocates and policymakers have also touted its universal coverage to claim that the program would reduce health disparities. However, little systematic research exists on the extent to which the NBS mandates affected disparities in infant mortality at the time (Brosco, Grosse, & Ross, 2015).
Using data from almost all US births since the late 1950s, we utilize the variation in States’ timing of NBS mandates between 1962 and 1984 to investigate the changes in population-level infant mortality associated with newborn screening. We also examine whether racial inequities in infant mortality narrowed or widened after NBS mandates. Lastly, we explore whether increased access to early-life care via the introduction of Medicaid strengthened the link between NBS mandates and mortality improvements.
Infant mortality is one of many deleterious health outcomes that NBS targets. We focused on infant mortality rate (IMR) in this article for two reasons. First, IMR is one of the primary indicators of a nation's health and reducing IMR is often an explicit goal for health policymakers (i.e., 2030 United Nations Sustainable Development Goals). Improving IMR and reducing inequities was a particularly salient national issue for the US in the 1950s and 1960s as mortality improvements began to lag compared to similarly developed nations (Singh & Yu, 1995). It was in this context that the US States began to introduce two major health policies targeting infant health: NBS mandates and Medicaid. Second, infant mortality is an extreme consequence of the medical conditions screened during NBS. While IMR alone would not be adequate in evaluating the efficacy of NBS per se, race-differences in IMR serve as useful indicators of how a program may be affecting different groups.
Race: Despite the near-universal reach of NBS via mandates, however, screening alone was likely insufficient to reduce infant mortality inequities. Early diagnosis through NBS may have only benefited those who were able to seek appropriate medical interventions, leaving others without the means to adequately change the progression of diseases (Hinton et al., 2016). Prior to Medicaid, African American infants had significant barriers—even more so than today—in accessing medical services (Institute of Medicine, 2003). Under these extreme unequal conditions, the introduction of NBS mandates may have disproportionately benefitted whites, further widening the racial infant mortality gap. While the unequal benefits of NBS may have occurred across other social strata such as income, our analyses focus on black-white differences as racial inequities in health and access to care has long been an issue of interest in US health policy (Goodman-Bacon, 2018). Furthermore, race2 is the best and likely the only proxy that measures access to care in public use US Vital Statistics Data spanning the entirety of the study period.
Medicaid: In 1965, Title XIX of the Social Security Act created Medicaid, a public means-tested insurance program, to expand access to predominantly low-income pregnant women and infants (Currie & Gruber, 1996; Goodman-Bacon, 2018). While the program fell short of leveling racial inequities in early-life care, Medicaid has been singled out as one of the most significant drivers of reducing infant mortality since its inception in the 1960s (Copeland & Meier, 1987; Corman & Grossman, 1985; Goodman-Bacon, 2018). Like NBS mandates, States had substantial leeway in joining the Medicaid program. The first States implemented Medicaid in 1966, and the last States joined in 1982 (Corman & Grossman, 1985). While States began to implement NBS mandates and Medicaid in the same 20-year period to reduce infant mortality, the timing of the two programs was not correlated. Some States began NBS mandates prior to Medicaid, and others joined Medicaid prior to implementing NBS mandates (Goodman-Bacon, 2018; Therrell & Adams, 2007). This sequence of events allows us to examine changes in infant mortality rates associated with two of the largest public health programs targeting infants in the latter half of the 20th Century.
The life-saving potential of NBS mandates may have been muted in disadvantaged populations exacerbating the inequity in infant mortality rates. Increased access to health care services to low-income infants after Medicaid would have improved the efficacy of NBS mandates among the disadvantaged group and narrowed the infant mortality disparity. We examine the intersection of screening mandates and access to medical care by answering the following research questions.
-
1.
Did infant mortality decrease in cohorts born after NBS mandates?
-
2.
Did the racial inequity in infant mortality change after NBS mandates?
-
3.
Did Medicaid reduce the racial gap associated with the introduction of NBS?
2. Data
We used the US Vital Statistics Natality and Mortality micro-data files to derive infant mortality rates by state, year, and race between 1959 and 1995. The Natality files recorded 50 percent of births prior to 1972 and almost all births thereafter. The Mortality files included almost all infant deaths occurring in the United States. The Vital Statistics may be the only dataset that is appropriate to study population-level changes associated with NBS mandates. The near-complete record of all infant deaths in the United States since the 1950s allows us to examine changes in infant mortality due to rare conditions that afflict a small percentage of the population.
Mortality data for New Jersey is missing for 1962 and 1963, and only 50% of deaths nationwide were recorded in 1972. We excluded New Jersey for the years 1962 and 1963 and multiplied deaths in 1972 by a factor of two. Also, we excluded data from Hawaii prior to 1968 from the analysis as its mortality data is incomplete between 1959 and 1967.
Our analyses examine infants born in the 50 States and the District of Columbia and do not include births to American citizens living outside the United States. In addition, we limit our analysis to white and African American infants. Prior to the 1970s, few births and deaths among other race groups produced unreliable estimates, and births among non-whites and non-African Americans rose rapidly after 1970, driven by immigration trends (Parrado, 2011). Changes in their infant mortality rates may reflect changes in composition rather than responses to policy changes. In addition, researchers have questioned the reliability of race reporting in death certificates among smaller race groups (Arias, Schauman, Eschbach, Sorlie, & Backlund, 2008). For these reasons, we limit both our national-level and race-specific analyses to white and African American infants.
3. Analytical strategy
Our analytical approach exploits the variation in the timing of States' adoption of NBS mandates and Medicaid to compare state-levels of infant mortality before and after each policy's implementation. Using the US natality and mortality files, we derived each year's infant mortality rate (IMR) for every state (1000*number of deaths under age one/number of births).
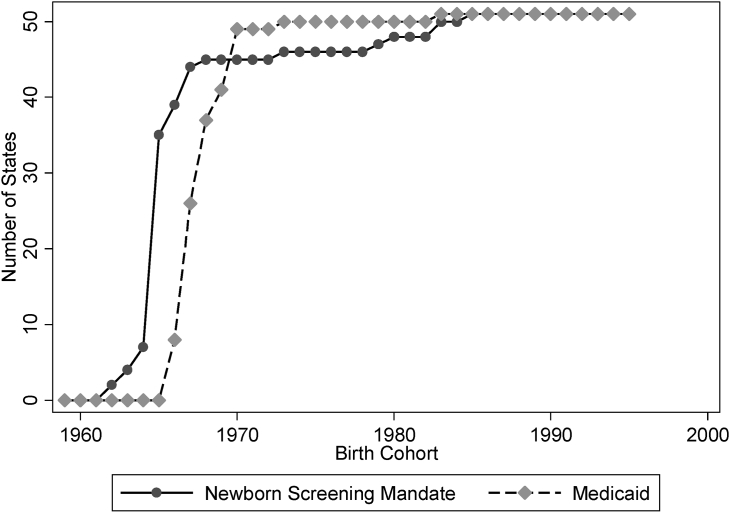
Exhibit 1 shows the timing of states’ implementation of NBS mandates and Medicaid. Our study period begins with a three-year period, during which no state had an NBS mandate or Medicaid. Delaware and Vermont first mandated NBS in 1962. The remaining States enforced NBS mandates between 1962 and 1984. North Carolina and Wyoming were the last to mandate NBS (Goodman-Bacon, 2018). The introduction of Medicaid also occurred throughout this period. The first states adopted Medicaid in 1966, and by 1983 all States had Medicaid.
Fig. 1.
Number of states that implemented Medicaid and Newborn Screening Mandates between 1959 and 1995. Sources: Therrell and Adams (2007), Table 1 and Sohn (2016). Notes: Includes 50 US States and the District of Columbia.
Our data represents approximately 25.5 million births prior to the start of both policies; 2.1 million births during the post-NBS mandate, pre-Medicaid period; 8.4 million births during the pre-NBS mandate, post-Medicaid period; and 97.5 million births after the implementation of both policies. During the study period from 1959 to 1995, the US Vital Statistics reported about 2.2 million infant deaths.
To examine the changes in infant mortality associated with NBS mandates and Medicaid, we regressed combined white and African American infant mortality on whether their state of birth had enforced an NBS mandate and whether it had adopted Medicaid. We also included an interaction term of these two policies. We examined the NBS mandate-Medicaid interaction term to determine whether Medicaid changed the association between NBS mandates and infant mortality rates.
Our second set of analyses examines the changes to the mortality gap between white and African American infants after NBS mandates and Medicaid were put in place. First, we estimated changes in infant mortality associated with NBS mandates, Medicaid, and their interaction separately for each race group. Then, we regressed changes to the mortality gap (difference in African American and white IMR) within each state and year on NBS mandates, Medicaid, and their interaction.
All our regressions are weighted by the number of births in each state and include state- and year-fixed effects to account for state-specific infant mortality levels and secular changes in infant mortality throughout the study period. All results correct for heteroscedasticity and panel-corrected standard errors. These adjustments to standard errors account for interdependent observations within states.
A limitation of this analytical approach is that it examines changes in all-cause infant mortality associated with introductions of NBS mandates and Medicaid rather than changes in deaths due to the specific diseases targeted by NBS. We have made the decision to examine all-cause mortality as cause-of-death on death certificates may have become more precise as a direct result of newborn screening technologies (Timmermans & Buchbinder, 2012).
The analyses use the state of residence at the time of birth and death to determine the State policy environment. While Medicaid eligibility and access to on-going care are determined by residence, the state in which the birth occurred would determine whether the newborn was subject to screening mandates. Over 97 percent of births and over 80 percent of infant deaths occurred in the mother's state of residence. If an infant were to move to another state after being born, their birth and death would be recorded in different states. This would underestimate the mortality rate in their birth state and overestimate the mortality in their death state. The Mortality Files in the Vital Statistics only recorded the state of birth between 1979 and 2004. During these years, about 95 percent of infants who died were living in the state that they were born in, and less than one percent of infant deaths were by infants born outside the 50 States and DC.
4. Results
NBS mandates alone were not associated with substantial declines in infant mortality rates (Exhibit 2). When Medicaid is accounted for, the NBS mandate is associated with an approximately 0.005 decline in infant deaths per 1000 births. This rate is equivalent to about 19 fewer deaths per year in a hypothetical birth cohort of four million. The 95 percent confidence interval ranges from 13 to 25 fewer infant deaths per year.
Table 1.
Change in IMR associated with newborn screening mandate interacted with Medicaid implementation.
| (in deaths per 1000 births) | Change in IMR | Std. Err | p-value | 95%CI of effect Size in No. of Birthsa |
|---|---|---|---|---|
| Medicaid | −1.036 | 0.003 | 0.000 | −4123 to −4164 |
| Newborn Screening | −0.005 | 0.001 | 0.000 | −13 to −25 |
| Medicaid + Newborn Screening | −0.094 | 0.001 | 0.000 | −370 to −386 |
Notes: State IMR is regressed on states' NBS and Medicaid implementation status. Regressions include fixed effects for birth year and state (r-squared = 0.955). Heteroskedastic panels corrected for standard errors. Analysis includes all years 1959-1995. Data for New Jersey is missing for 1962 and 1963. Data for Hawaii is missing prior to 1968. Adding state income growth rate (from the previous year) does not change results.
95% Confidence interval of the coefficient (change in IMR) is applied to a hypothetical birth cohort of 4 million. Negative values indicate declines in mortality.
Source: Authors' analysis of US Vital Statistics Data, 1958–1995
In contrast to the minimal change in IMR associated with NBS mandates alone, Exhibit 2 shows small but significant declines in IMR associated with NBS mandates when it is combined with Medicaid adoption. The 0.094 fewer deaths per 1000 births associated with the simultaneous implementation of both policies are equivalent to about 380 fewer deaths in a hypothetical birth cohort of four million.
Our second set of regression analyses focuses on racial differences in the relationship between NBS mandates, Medicaid, and infant mortality (Exhibit 3). NBS mandates, when adopted with Medicaid, are associated with significant declines in infant mortality among both white and African Americans infants. The change among African Americans, however, appears to be larger than among white infants. Infant mortality decreased by about 0.25 deaths per 1000 births among African Americans compared to about 0.096 deaths per 1000 births among white infants. These changes in IMR are equivalent to about 1000 and 380 fewer deaths in a hypothetical cohort of four million births respectively. Declines in IMR associated with NBS mandates alone were substantially smaller. NBS mandates alone were associated with 0.076 fewer deaths per 1000 births among whites and 0.054 more deaths per 1000 births among African Americans.
The third panel of Exhibit 3 explicitly regresses the within-state IMR differences between African American and white infants on NBS mandates, Medicaid, and their interaction term. NBS mandate alone is significantly associated with an increase in the IMR disparity. Excess infant mortality among African Americans increased by about 0.211 deaths per 1000 births when only NBS mandates were implemented in the state. When NBS mandates and Medicaid were implemented together, the white-black mortality gap decreased by about 0.067 deaths per 1000 births.
Table 2.
Change in IMR associated with newborn screening mandate interacted with Medicaid implementation separately by race.
| (in deaths per 1000 births) | Change in IMR | Std. Err | p-value | 95%CI of effect Size in No. of Birthsa |
|---|---|---|---|---|
| White | ||||
| Medicaid | −0.131 | 0.002 | 0.000 | −510 to −539 |
| Newborn Screening | −0.076 | 0.001 | 0.000 | −299 to −310 |
| Medicaid + Newborn Screening | −0.096 | 0.001 | 0.000 | −378 to −392 |
| African American | ||||
| Medicaid | −1.150 | 0.008 | 0.000 | −4537 to −4665 |
| Newborn Screening | 0.054 | 0.003 | 0.000 | 191 to 242 |
| Medicaid + Newborn Screening | −0.250 | 0.004 | 0.000 | −968 to −1031 |
| Within State Disparityb | ||||
| Medicaid | −1.145 | 0.008 | 0.000 | −4520 to −4643 |
| Newborn Screening | 0.211 | 0.003 | 0.000 | 821 to 871 |
| Medicaid + Newborn Screening | −0.067 | 0.004 | 0.000 | −238 to −299 |
Notes: State IMR is regressed on states' NBS and Medicaid implementation status separately by race. Regressions include fixed effects for birth year and state. Heteroskedastic panels corrected for standard errors. Analysis includes all years 1959-1995. Data for New Jersey is missing for 1962 and 1963. Data for Hawaii is missing prior to 1968. Adding state income growth rate (from the previous year) does not change results.
95% Confidence interval of the coefficient (change in IMR) is applied to a hypothetical birth cohort of 4 million. Negative values indicate declines in mortality.
Within state disparity is the difference in white IMR and African American IMR in each state and year. The difference is regressed on states' NBS and Medicaid status and includes fixed effects for birth year and state. Heteroskedastic panels are corrected for standard errors.
Source: Authors' analysis of US Vital Statistics Data, 1958–1995
5. Discussion
The CDC listed the expansion of the newborn screening program as one of the ten great public health achievements in the first decade of the 21st Century in the United States (Domestic Public Health Achievements Team, 2011). Unlike medical innovations such as magnetic resonance imaging (MRI) where unequal access created disparities in utilization of services and diagnosis of conditions (Weiss et al., 2018), all infants, regardless of race or socioeconomic status, born in mandate States underwent screening at birth. As one of the few quasi-universal public health requirements in the US, NBS mandates are expected to reduce health disparities (Brosco et al., 2015). Yet, while researchers have shown mixed results for the programs' ability to lower mortality of individual conditions, few empirical studies exist about the overall population health impact on infant mortality or about racial inequities. Existing studies on NBS's ability to prevent deaths focuses on newborns who were diagnosed with a specific disorder at screening. A class of studies links birth certificates of newborns who were diagnosed during NBS to death certificates to determine their mortality rates (Centers for Disease Control and Prevention (CDC, 1998); Vichinsky, Hurst, Earles, Kleman, & Lubin, 1988; Wang et al., 2015). More recently, prospective surveillance systems have tracked newborns in participating states (California, Iowa, New York, and Utah) with confirmed diagnoses and documented their follow-up care, health status, and early mortality (Hinton et al., 2014, 2016; Hoff, Ayoob, & Therrell, 2007). These patient-level studies conclude that long-term follow up is a critical component in any NBS program and must be aligned with other public health efforts to ensure diagnosed individuals receive appropriate care.
Our analysis of the Vital Statistics between 1959 and 1995 suggests that a universal screening program for rare inherited conditions may have had a limited impact on health inequities between white and African American infants. Only when expanded health care access via Medicaid is jointly implemented with NBS mandates did it show reductions in IMR disparities. Furthermore, overall mortality declines associated with NBS were far greater with Medicaid. Our estimates show very small mortality declines—approximately 20 in a hypothetical birth cohort of 4 million—associated with NBS mandates alone. When Medicaid is jointly implemented with NBS mandates, does it show a larger—in the order of 380 deaths in a hypothetical birth cohort of 4 million—reduction in infant mortality rates. These specific numbers should be interpreted with caution as they may be influenced by unobserved socioeconomic and behavioral changes throughout the decades. While infant mortality is only a partial picture of the public health impact of NBS and Medicaid, its responses to these programs are likely reflective of the broader health outcomes such as morbidity and later-life mortality.
Singh & Yu, 1995, States have expanded the conditions tested during NBS, keeping up with continued medical innovation (Benson & Therrell, 2010). Notably, the Recommended Uniform Screening Panel (RUSP) was determined in 2006 in an effort to standardize States’ NBS mandates and to inform health policy (Watson, Mann, Lloyd-Puryear, Rinaldo, & Howell, 2006). However, the economic, health and emotional cost of screening millions of newborns for rare genetic conditions each year is unlikely to yield substantial health improvements without access to follow-up care.
The widening of racial inequity in infant mortality in States with NBS but no Medicaid during the early years is an illustration of David Mechanic's prediction; “interventions that offer some of the largest possible gains for the disadvantaged may also increase disparities” (p. 48, Mechanic, 2002). Link and Phelan's notion of the fundamental causes of disease (Phelan, Link, & Tehranifar, 2010) —those with greater health capital, resources, knowledge, influence and social networks are more likely to benefit from health innovations—suggests that multiple mechanisms may link greater improvements in infant mortality among groups with more resources and social status as universal screening mandates are rolled out. The uneven history of NBS in the US indicates that (Wilson and Junger's, 1968) classic screening criteria remain blind to the reality of social inequities that make diagnosis and treatment more difficult for some people. These findings suggest caution for low- and middle-income countries considering newborn screening to reduce infant mortality disparities. Interventions that expand access to health care should be considered a critical and necessary component in mandating NBS.
This article is also consequential for renewed debate on the relationship between Medicaid expansion under the Affordable Care Act (ACA) and NBS mandates in the US (Costich & Durst, 2016). While the ACA requires most health plans to cover the federal RUSP during NBS, funding, and reimbursement mechanisms for follow-up care vary between States and complicates families’ access to medical services and treatment. To improve the efficacy of NBS, not only should provisions ensure health plans cover screening (Watson et al., 2006) but also follow-up care.
Declaration of competing interest
The authors do not have competing interests.
Footnotes
This research was supported by Binational Science Foundation grant 2010094. We thank participants at the 2019 UCLA Newborn Screening workshop for helpful comments. This project also benefited from facilities and resources provided by the California Center for Population Research at UCLA (CCPR), which receives core support (R24-HD041022) from the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD).
The US Vital Statistics changed the categories of race multiple times throughout the decades. To keep comparisons across years consistent and to reduce biases from immigration, we opted to focus on differences between White and African American births and mortality.
Contributor Information
Heeju Sohn, Email: hesohn@ucla.edu.
Stefan Timmermans, Email: stefan@soc.ucla.edu.
References
- Arias E., Schauman W.S., Eschbach K., Sorlie P.D., Backlund E. The validity of race and Hispanic origin reporting on death certificates in the United States. Vital and Health Statistics. Series 2, Data Evaluation and Methods Research. 2008;148:1–23. http://www.ncbi.nlm.nih.gov/pubmed/19024798 Retrieved from. [PubMed] [Google Scholar]
- Benson J.M., Therrell B.L. History and current status of newborn screening for hemoglobinopathies. Seminars in Perinatology. 2010;34(2):134–144. doi: 10.1053/j.semperi.2009.12.006. [DOI] [PubMed] [Google Scholar]
- Boyle C.A., Bocchini J.A., Kelly J. Reflections on 50 Years of newborn screening. Pediatrics. 2014;133(6):961–963. doi: 10.1542/peds.2013-3658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brosco J.P., Grosse S.D., Ross L.F. Universal state newborn screening programs can reduce health disparities. JAMA Pediatrics. 2015;169(1):7–8. doi: 10.1001/jamapediatrics.2014.2465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention (CDC) Mortality among children with sickle cell disease identified by newborn screening during 1990-1994--California, Illinois, and New York. MMWR. Morbidity and Mortality Weekly Report. 1998;47(9):169–172. http://www.ncbi.nlm.nih.gov/pubmed/9518280 Retrieved from. [PubMed] [Google Scholar]
- Copeland G.W., Meier K.J. Gaining ground. American Politics Quarterly. 1987;15(2):254–273. doi: 10.1177/004478087015002004. [DOI] [PubMed] [Google Scholar]
- Corman H., Grossman M. Determinants of neonatal mortality rates in the U.S. A reduced form model. Journal of Health Economics. 1985;4(3):213–236. doi: 10.1016/0167-6296(85)90030-x. [DOI] [PubMed] [Google Scholar]
- Costich J.F., Durst A.L. The Impact of the Affordable Care Act on Funding for Newborn Screening Services. Public Health Reports. 2016;131(1):160–166. doi: 10.1177/003335491613100123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Currie J., Gruber J. Health Insurance Eligibility, Utilization of Medical Care, and Child Health. Quarterly Journal of Economics. 1996;111(2):431–466. [Google Scholar]
- Domestic Public Health Achievements Team, C Ten Great Public Health Achievements --- United States, 2001--2010. 2011. https://www.cdc.gov/mmwr/preview/mmwrhtml/mm6019a5.htm Retrieved from. [PubMed]
- Goodman-Bacon A. Public Insurance and Mortality: Evidence from Medicaid Implementation. Journal of Political Economy. 2018;126(1):216–262. [Google Scholar]
- Hinton C.F., Homer C.J., Thompson A.A., Williams A., Hassell K.L., Feuchtbaum L., Follow-up and Treatment Sub-committee of the Advisory Committee on Heritable Disorders in Newborns and Children (ACHDNC) A framework for assessing outcomes from newborn screening: on the road to measuring its promise. Molecular Genetics and Metabolism. 2016;118(4):221–229. doi: 10.1016/j.ymgme.2016.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hinton C.F., Mai C.T., Nabukera S.K., Botto L.D., Feuchtbaum L., Romitti P.A. Developing a public health-tracking system for follow-up of newborn screening metabolic conditions: a four-state pilot project structure and initial findings. Genetics in Medicine. 2014;16(6):484–490. doi: 10.1038/gim.2013.177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoff T., Ayoob M., Therrell B.L. Long-term Follow-up Data Collection and Use in State Newborn Screening Programs. Archives of Pediatrics and Adolescent Medicine. 2007;161(10):994. doi: 10.1001/archpedi.161.10.994. [DOI] [PubMed] [Google Scholar]
- Institute of Medicine . National Academies Press (US); 2003. Unequal treatment: Confronting racial and ethnic disparities in health care. Unequal treatment: Confronting racial and ethnic disparities in health care. [PubMed] [Google Scholar]
- Mechanic D. Disadvantage, Inequality, And Social Policy. Health Affairs. 2002;21(2):48–59. doi: 10.1377/hlthaff.21.2.48. [DOI] [PubMed] [Google Scholar]
- Parrado E.A. How High is Hispanic/Mexican Fertility in the United States? Immigration and Tempo Considerations. Demography. 2011;48(3):1059–1080. doi: 10.1007/s13524-011-0045-0. [DOI] [PubMed] [Google Scholar]
- Phelan J.C., Link B.G., Tehranifar P. Social Conditions as Fundamental Causes of Health Inequalities: Theory, Evidence, and Policy Implications. Journal of Health and Social Behavior. 2010;51(1_suppl):S28–S40. doi: 10.1177/0022146510383498. [DOI] [PubMed] [Google Scholar]
- Singh G.K., Yu S.M. Infant Mortality in the United States: Trends, Differentials, and Projections, 1950 through 2010. 1995. https://ajph.aphapublications.org/doi/pdf/10.2105/AJPH.85.7.957 Retrieved from. [DOI] [PMC free article] [PubMed]
- Therrell B.L., Adams J. Newborn screening in North America. Journal of Inherited Metabolic Disease. 2007;30(4):447–465. doi: 10.1007/s10545-007-0690-z. [DOI] [PubMed] [Google Scholar]
- Timmermans S., Buchbinder M. University of Chicago Press; 2012. Saving babies?: The consequences of newborn genetic screening.https://books.google.com/books?id=k62nlCny8W8C Retrieved from. [Google Scholar]
- Urv T.K., Parisi M.A. Springer; Cham: 2017. Newborn screening: Beyond the spot; pp. 323–346. [DOI] [PubMed] [Google Scholar]
- Vichinsky E., Hurst D., Earles A., Kleman K., Lubin B. Newborn screening for sickle cell disease: effect on mortality. Pediatrics. 1988;81(6):749–755. http://www.ncbi.nlm.nih.gov/pubmed/3368274 Retrieved from. [PubMed] [Google Scholar]
- Wang Y., Liu G., Caggana M., Kennedy J., Zimmerman R., Oyeku S.O. Mortality of New York children with sickle cell disease identified through newborn screening. Genetics in Medicine. 2015;17(6):452–459. doi: 10.1038/gim.2014.123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watson M.S., Mann M.Y., Lloyd-Puryear M.A., Rinaldo P., Howell R.R. Newborn Screening: Toward a Uniform Screening Panel and System—Executive Summary. Pediatrics. 2006;117(Supplement 3):S296–S307. doi: 10.1542/peds.2005-2633I. [DOI] [PubMed] [Google Scholar]
- Weiss D., Rydland H.T., Øversveen E., Jensen M.R., Solhaug S., Krokstad S. Innovative technologies and social inequalities in health: A scoping review of the literature. PLoS One. 2018;13(4) doi: 10.1371/journal.pone.0195447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson J.M.G., Jungner G., World Health Organization . World Health Organization; 1968. Principles and practice of screening for disease. [Google Scholar]