Abstract
Although air pollution is well known to be harmful to the lung and airways, it can also damage most other organ systems of the body. It is estimated that about 500,000 lung cancer deaths and 1.6 million COPD deaths can be attributed to air pollution, but air pollution may also account for 19% of all cardiovascular deaths and 21% of all stroke deaths. Air pollution has been linked to other malignancies, such as bladder cancer and childhood leukemia. Lung development in childhood is stymied with exposure to air pollutants, and poor lung development in children predicts lung impairment in adults. Air pollution is associated with reduced cognitive function and increased risk of dementia. Particulate matter in the air (particulate matter with an aerodynamic diameter < 2.5 μm) is associated with delayed psychomotor development and lower child intelligence. Studies link air pollution with diabetes mellitus prevalence, morbidity, and mortality. Pollution affects the immune system and is associated with allergic rhinitis, allergic sensitization, and autoimmunity. It is also associated with osteoporosis and bone fractures, conjunctivitis, dry eye disease, blepharitis, inflammatory bowel disease, increased intravascular coagulation, and decreased glomerular filtration rate. Atopic and urticarial skin disease, acne, and skin aging are linked to air pollution. Air pollution is controllable and, therefore, many of these adverse health effects can be prevented.
Key Words: air pollution, noncommunicable diseases, organ systems
Abbreviations: CO, carbon monoxide; NO2, nitrogen dioxide; O3, ozone; PM2.5, particulate matter with an aerodynamic diameter < 2.5 μm; PM10, particulate matter with an aerodynamic diameter < 10 μm; SO2, sulfur dioxide
FOR RELATED ARTICLE, SEE PAGE 409
Introduction
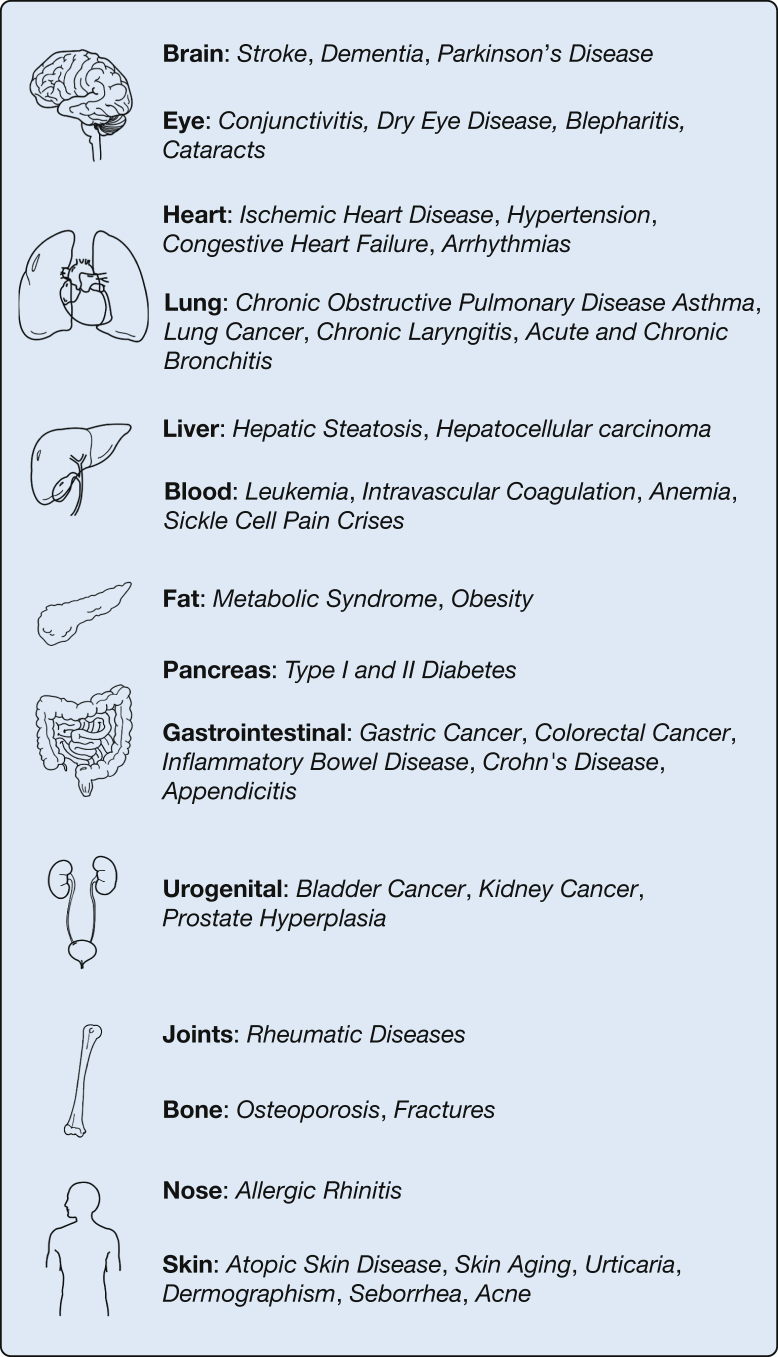
This second of a two-part report describes specific conditions associated with air pollution. The conditions are listed alphabetically. In addition to the text, Figure 1 presents associated organ systems, and Table 1 shows other effects of air pollution that are generally not associated with specific organs. It is important to note that for many of the diseases, the associations with exposures to air pollution in observational epidemiologic studies are not causal and may be subject to residual confounding due to other factors, such as smoking, lower socioeconomic status, and neighborhood factors. However, exposure dose and time relationships and animal studies corroborate and add strength to the conclusions from the epidemiologic studies.
Figure 1.
Many conditions are associated with air pollution. This figure lists diseases linked to air pollution according to organ systems.
Table 1.
Pollution Has Been Associated With These Pathobiologic Processes in Addition to the Effects in the Organ as shown in Figure 1
| Allergy: allergic sensitization |
| Blood and blood vessels: endothelial dysfunction, atherosclerosis, thrombosis, impaired hemoglobin formation; carboxyhemoglobinemia |
| Bone: bone demineralization |
| Brain: cognitive dysfunction; impaired psychomotor development and intelligence development; social stress; mood disorders; unfavorable emotional symptoms |
| Cancer: shortened telomere length; detrimental expression of genes involved in DNA damage and repair; inflammation; immune and oxidative stress response; epigenetic effects |
| Diabetes and metabolism: increased glycosylated hemoglobin, insulin resistance, leptin, and endothelin-1 levels; lower glucagon-like peptide-1, ghrelin, and glucagon levels |
| Eye: increased tearing (acutely) and drying (chronically) |
| Heart: changes in heart rate, BP, and vascular tone; reduced heart rate variability; conduction defects |
| Kidney: decreased glomerular filtration rate; increased mortality in patients undergoing dialysis |
| Respiratory tract: cough, phlegm, difficulty breathing, and bronchial hyperresponsiveness; exacerbations of many respiratory conditions; impeded lung development; transformation of asthma into COPD; decreased exercise performance; decreased spirometric measurements (lung function) |
| Reproductive: premature birth; low birth weight; poor sperm quality; impaired fetal growth; intrauterine inflammation; reduced fertility rates; increased risk of miscarriage, spontaneous abortions, premature rupture of membranes, and preeclampsia. Exposure during pregnancy is associated with childhood neoplasms and childhood asthma |
| Skin: aging |
| Sleep: associated with increased sleep apnea symptoms |
| Overall: shortened life expectancy, with additive or multiplicative effects in vulnerable persons |
Allergic and Immunologic Diseases
Allergic Sensitization and Rhinitis
It is well established that air pollution can exacerbate allergic responses in sensitized persons.1 Clinical epidemiologic studies show that ambient air pollution may also enhance allergic sensitization in children and increase IgE levels in the very young.2
There is considerable evidence that air pollution plays a role in both the development and the exacerbation of allergic rhinitis. A study of preschool-aged children found that exposure to traffic-related air pollution prenatally and in early life was associated with increased risk of allergic rhinitis.3 A study from China found a 10% and 11% increase in the incidence of medical utilization for allergic rhinitis among adults for each SD increase in particulate matter with an aerodynamic diameter < 2.5 μm (PM2.5) and nitrogen dioxide (NO2) levels, respectively.4
Autoimmune Disease
Environmental exposures may increase the risk of autoimmune diseases. The lung has an enormous surface area that comes into contact with a myriad of antigens. It has an efficient sensitization and antigen-presenting system that could make individuals prone to autoimmune disorders. Air pollution is a potential contributor to diseases such as rheumatoid arthritis and systemic lupus erythematosus.5, 6 A Canadian study found increased odds of having a diagnosis of a rheumatic disease with increased ambient PM2.5 exposure.7 Air pollutants have also been implicated in triggering or exacerbating juvenile idiopathic arthritis,5 but autoimmunity related to air pollution exposure has largely been understudied.
Bone Diseases
Environmental factors play a role in bone density and mineralization. To evaluate the effect of air pollution on bone structure and function, an analysis of > 9 million US Medicare enrollees found that osteoporosis-related bone fractures were statistically more common in areas of higher ambient PM2.5 concentrations. The effect was greater when only low-income communities were included in a sensitivity analysis.8
The same investigators studied 692 middle-aged men with low incomes from the Boston Area Community Health Bone Survey cohort and found that exposures to ambient black carbon and PM2.5 were associated with markers of increased bone turnover and bone mineral loss.8 The National Health Insurance Research Database of Taiwan and the Taiwan Environmental Protection Agency found an association between exposure to carbon monoxide (CO) and NO2 and osteoporosis.9 The Oslo Health Study found that long-term air pollution exposure (PM and NO2) was associated with a reduction in bone mineral density10 and fractures11 in elderly men.
Cancers
Outdoor air pollution has been classified as carcinogenic to humans by the International Agency for Research on Cancer based on evidence from epidemiologic and animal studies and mechanistic data.12 Many studies have shown an association between exposure to PM2.5 and particulate matter with an aerodynamic diameter < 10 μm (PM10) and risk of lung cancer.13 In addition, NO2 and ozone (O3) levels have been experimentally linked to cellular changes related to neoplasia: altered telomere length, expression of genes involved in DNA damage and repair, inflammation, immune and oxidative stress response, and epigenetic effects, such as DNA methylation.14 Diesel engine exhaust has been identified by the World Health Organization as a carcinogen based on evidence of a link with lung cancer.15, 16 Exposure to diesel exhaust or traffic pollution has also been associated with benign and malignant lung tumors in laboratory animals,16 colorectal cancer,17 and deaths from gastric cancer.18
Air pollution exposure is implicated in both the incidence and mortality of bladder cancer. A Spanish study reported an association between emissions of polycyclic aromatic hydrocarbons and diesel exhaust and bladder cancer in long-term residents of an industrially polluted area.19 Studies from Taiwan have shown an increased risk of bladder cancer deaths associated with ambient benzene and other hydrocarbons from evaporative losses of petroleum products and motor vehicle emissions.20 Another study from São Paulo, Brazil, found an association between PM10 exposure and risk of bladder cancer but not bladder cancer mortality.21 The American Cancer Society’s prospective Cancer Prevention Study II of 623,048 participants followed up for 22 years (1982-2004) found that PM2.5 was associated with death from cancers of the kidney and bladder and that NO2 levels were associated with colorectal cancer mortality.22
Benzene exposure from vehicular exhaust, especially during the prenatal period and in the early years of childhood, has been associated with the risk of childhood leukemia.23 Prenatal exposure to PM2.5 during pregnancy may increase a child’s risk of developing leukemia and astrocytomas.24
Cardiovascular Diseases
Particulate air pollution has been strongly associated with an increased risk of cardiovascular disease mortality, myocardial infarction, stroke, and hospital admission for congestive heart failure25 and has been estimated to account for 19% of all cardiovascular deaths, 23% of all ischemic heart disease deaths, and 21% of all stroke deaths.26 A 10 μg/m3 increase in PM2.5 in a 2-day period was associated with an approximately 2% increase in myocardial infarctions and hospital admissions for heart failure in a 26-city US survey.27 Other studies have found similar associations between acutely increased ambient PM2.5 and increases in mortality from myocardial infarction, stroke, heart failure, and hypertension.28 Mild increases in carboxyhemoglobin levels (in the 3%-6% range) can occur when individuals are exposed to traffic pollution and may trigger angina and arrhythmias in individuals with coronary heart disease.29 In Medicare recipients in nine US cities, PM concentrations during the 2 days prior to the event were associated with ischemic, but not hemorrhagic, stroke hospital admissions. This study also found a correlation between CO, NO2, and sulfur dioxide (SO2) levels and stroke.30 In a separate article, the increased risk of stroke was greatest within 12 to 14 h of exposure to PM2.5, and the relation held up even with PM2.5 levels below those considered safe by the US Environmental Protection Agency.31 These acute effects of PM exposure are likely mediated by autonomic dysregulation, endothelial dysfunction, or thrombosis or a combination of these factors.32 Many studies have found that cardiovascular parameters such as heart rate variability are associated with air pollution, especially exposure with PM2.5.33 A decrease in heart rate variability, as occurs with air pollution exposure, is associated with many poor health outcomes, such as an increased risk of adverse cardiovascular events and all-cause mortality in selected populations.34 Long-term effects of exposure to air pollution on the risk of cardiovascular diseases have been well documented.35, 36 These effects can shorten life expectancy even at relatively low PM levels.37 Studies have found a relationship between air pollution and atherosclerosis, which is a central mechanism for ischemic heart disease and stroke and may explain the long-term effects of pollution on risk of many cardiovascular diseases.25 The relationship of PM and ischemic mortality seems to vary with the composition and source of the PM2.5; the most damaging PM2.5 may come from coal combustion.38
Cognitive Function and Neurologic Diseases
Air pollution has deleterious effects on the CNS, including impairment of cognitive function and increased risk of dementia and stroke in older adults. A Canadian study of 4.4 million people showed that the risk of dementia was correlated in a “dose-dependent” manner with distance from a major roadway. People living within 50 meters had a hazard ratio of 1.07, whereas those living 50 to 100 meters away had a hazard ratio of 1.04, and those living 101 to 200 meters away had a hazard ratio of 1.02 compared with those living > 300 meters from a major roadway. Living near a busy roadway is a marker of air pollution exposure.39
Inflammation in the bloodstream in response to pollutants has been found to cause systemic vascular (including cerebral vascular) dysfunction.40 Studies in animals have shown that inhaled ultrafine particles can travel from the nose via the olfactory nerve directly into the brain, where they may cause inflammation and oxidative stress.41
Air pollution can damage the developing brain, which is especially concerning because this damage can impair cognitive function across the life span. Many studies have found that prenatal and early childhood exposure to PM2.5 is associated with delayed psychomotor development42 and lower child intelligence.43 A study in Mexico City found that children living in more polluted areas had worse cognitive performance and more prefrontal brain lesions on MRI. In the same article, the authors reported that dogs exposed to comparable levels of pollution had similar prefrontal lesions and deposits of ultrafine particles within those lesions.44
More than 1,000 articles have been written on air pollution and autism,45 which has been associated with exposure to polycyclic aromatic hydrocarbons, diesel exhaust, PM, CO, NO2, O3, and SO2 in prenatal or early life,46 and there are several animal studies to support these findings. However, many studies have not found associations, and there is a lack of consistency on the pollutant.47
Air pollution is also harmful to the aging brain. Older adults more heavily exposed to air pollution perform more poorly on cognitive testing and are at increased risk of dementia compared with less exposed adults.48 Long-term exposure to PM2.5 was associated with a smaller brain volume according to MRI (an indicator of brain aging) and higher odds of subclinical strokes among generally healthy adults.49 Short-term exposure to fine particles increased the risk of hospitalizations and all-cause mortality in Parkinson's disease.50
Diabetes, Obesity, and Endocrine Diseases
Evidence from several studies links air pollution and type 2 diabetes mellitus.51 PM2.5 and NO2 exposures are associated with prevalence of diabetes and increased glycosylated hemoglobin levels among both diabetic and nondiabetic individuals.52 There is also a higher morbidity and mortality related to ambient air pollution among patients with diabetes.53 Several studies have described increased risk for metabolic syndrome in adults exposed to high ambient PM10.54 It seems that air pollution affects accumulation of visceral adipose tissue55 or brown to white adipose tissue transition,56 which may worsen insulin resistance,57 oxidative stress, and systemic inflammation.
Several metabolic changes affecting fat deposition occur with exposure to air pollution. Children in Mexico City exposed to high PM2.5 levels had higher leptin and endothelin-1 levels and lower glucagon-like peptide-1, ghrelin, and glucagon levels compared with those living in low PM2.5 areas. Leptin was strongly correlated to PM2.5 cumulative exposures. Residing in a high PM2.5 and O3 environment was associated with 12-h fasting hyperleptinemia, altered appetite-regulating peptides, vitamin D deficiency, and increases in endothelin-1 in healthy children.58 Air pollution-associated glucose and lipid dysregulation seem to be mediated through pathways that increase insulin resistance.59 Children living in areas with more traffic-related air pollution have been found to have a higher BMI after adjusting for confounders,60 which may be a consequence of metabolic changes, including insulin resistance in response to pollution exposure.
Eye Diseases
Tearing and ocular irritation may occur as a reaction to visible haze, and this finding is often worse for contact lens wearers. Conjunctivitis is most associated with O3 and NO2 exposure, although PM10 and SO2 are also correlated.61 Cataract formation has been described in women exposed to household air pollution in low-income countries.62 O3 levels and decreased humidity have been associated with dry eye disease.63 Air pollution, specifically PM and CO, have been associated with acute worsening of blepharitis.64
GI Diseases
Although less investigated, air pollution has been linked to several GI conditions, including inflammatory bowel disease, enteritis, gastric ulcer, and appendicitis. A case-control study of chronic pollution exposure in the United Kingdom found that younger individuals were more likely to have Crohn's disease if they lived in areas with high NO2 or SO2 levels, although there was no overall association between exposure to air pollutants and risk of inflammatory bowel disease.65 Other studies, however, have suggested a possible link to inflammatory bowel disease.66
A small number of studies have found associations between short-term exposure to pollution and acute episodes of enteritis, gastric ulcer disease, and appendicitis. A Chinese study of > 12,000 hospital visits for enteritis found that PM10, PM2.5, NO2, SO2, and CO levels were significantly elevated on days of outpatient visits, whereas O3 was not. Lag models showed that the pollution association was most prominent on the day of admission.67 A study of elderly Hong Kong Chinese subjects found that long-term exposure to PM2.5 was associated with hospitalizations for gastric ulcer disease.68 A Canadian study of the 7-day accumulated average of ground level O3 showed a modest correlation with appendicitis and a stronger relationship with perforated appendicitis.69
Hematologic Diseases
It has been known since the 1970s that air pollution containing lead from gasoline causes anemia. Other pollutants released during fuel combustion may also contribute to hematologic disease, either by directly entering the bloodsteam following inhalation, or by activating inflammatory pathways in the lung that then result in intravascular inflammation. PM2.5 promotes an imbalanced coagulative state through platelet and endothelial activation by inflammatory cytokines.70 These increase the risk of thrombotic events, including myocardial infarction,71 stroke,30 and most likely DVT and pulmonary embolism.72
Exposure to lead in air pollution affects the formation of hemoglobin.73 Indoor air pollution has been shown to be a risk factor for anemia in young children74 as well as the elderly.75 Air pollution may increase hemoglobin distortion in sickle cell disease. The resulting microvascular obstruction leads to lack of oxygen and severe pain. Poor air quality, including increased O3 levels, has been correlated with ED visits for sickle cell pain crises.76
Liver Diseases
Living near a major roadway, which is associated with increased air pollution, is linked to an increased prevalence of hepatic steatosis.77 There are several potential reasons for this link as air pollution has many damaging effects on liver cells through inflammatory mediators, genotoxicity, mitochondrial damage, and damage to other organs, which affect the liver secondarily.78 The liver is the main detoxifying organ, and a variety of substances that enter the body, including toxic components on PM, are presented to the liver for catabolism.
A Taiwanese study of 23,820 persons followed up for a median of 16.9 years found that exposure to PM2.5 was associated with an increased risk of hepatocellular cancer.79 These investigators also recorded elevated alanine aminotransferase levels and hypothesized that carcinoma may result from chronic inflammation. A Chinese study found that high PM2.5 exposure following the diagnosis of hepatocellular carcinoma was associated with shortened survival in a dose-dependent manner.80
Alpha1-antitrypsin deficiency is a genetic disorder associated with decreased release from the liver of the enzyme that catabolizes the proteolytic enzyme products of inflammation. Persons with this disorder are more susceptible to the detrimental effects of inflammation. Exposure to O3 and PM10 was associated with a more rapid decline of lung function in the persons with the PiZZ variant of this disease.81
Renal Diseases
The kidney, a highly vascular organ, is vulnerable to both large and small vessel dysfunction and is therefore likely to be susceptible to the oxidative stress and systemic inflammatory effects of air pollution exposure. Animal models have shown that breathing diesel exhaust fumes exacerbates chronic renal failure by worsening renal oxidative stress, inflammation, and DNA damage.82 Living closer to a major highway has been found to be associated with a lower estimated glomerular filtration rate83; the association of decreased renal function with pollution was greater for exposure to PM.84
Respiratory Diseases
The respiratory tract is the main organ affected by air pollution and the most studied: there are more than 13,000 entries in PubMed for air pollution and respiratory disease. Ambient air pollution is estimated to cause the death of > 800,000 persons from COPD and 280,000 persons from lung cancer.85 Indoor air pollution is estimated to cause the death of > 750,000 persons from COPD and 300,000 persons from lung cancer,86, 87 making the toll for both forms of air pollution 1.6 million deaths for COPD and > 500,000 for lung cancer. There is overlap in the two forms of pollution and the two diseases.
Air pollution also causes breathlessness in most patients with severe chronic respiratory diseases. Air pollutants can affect all parts of the respiratory system and throughout a person’s life cycle. As discussed in Part 1 of this report,88 prenatal exposure to air pollutants is associated with wheezing and asthma in early childhood. The rate of lung function growth in childhood is decreased by exposure to pollutants89, 90 and is a predictor of adult lung disease. Among adults, long-term exposure to air pollution is a risk for accelerated lung function decline with aging.91 Childhood exposure to air pollution has been linked to the risk of asthma in many studies,92 and pollution exposure has also been found to increase the incidence of asthma in adults,93 although the evidence for this theory is less consistent.
In addition to asthma, air pollution is associated with the risk of COPD,94 lung cancer,95 and chronic laryngitis.96 It may be a factor in transforming asthma into COPD.97 Household air pollution may be more hazardous than outdoor air pollution because of the concentration and duration of exposure; it is a major risk factor for COPD and chronic bronchitis in low-income countries.98
Air pollutants are also well-known triggers of respiratory disease exacerbations. Many different pollutants, such as O3, PM, SO2, and NO2, have irritant effects that can induce cough, phlegm, and bronchial hyperresponsiveness. Increases in PM levels are associated with increased visits to the ED for asthma,99 COPD,100 and respiratory symptoms that are often attributed to respiratory infections.101
Skin Diseases
Several biologic parameters affecting skin quality are influenced by pollution, such as change in sebum excretion rate and composition, level of carbonylated proteins in the stratum corneum, and a higher erythematous index on the face of highly exposed subjects.102 The change in sebum may be a cause for increased acne occurring with air pollution.103
Several skin diseases have been associated with air pollution. A multicenter study found that air pollution was associated with a higher frequency of atopic and urticarial skin disease, dermographism, and seborrhea (but a lower frequency of dandruff).102 Urticaria is among the skin pathologies that have been associated with pollution. ED visits for urticaria have been correlated with poorer air quality over a 2- to 3-day lag.104 A number of studies have found positive associations between air pollution and prevalence and exacerbations of eczema, primarily in children with traffic-related exposures.105
Outdoor and indoor air pollution exposure has been associated with increased skin aging after controlling for sun exposure, smoking, and other confounders. Cooking with solid fuels was associated with 5% to 8% more severe wrinkle appearance on the face and a 74% increased risk of having fine wrinkles on the dorsal surface of hands independent of age and other influences on skin aging.106
The Role of the Health-Care Provider
Assessing exposure by primary care providers may be difficult because the source of air pollution varies between communities and within household situations. Studies on indoor air pollution use extensive surveys to report on smoke exposure, burning conditions, and symptoms during cooking and household work. Research on outdoor air pollution relies on monitoring of the individual pollutants by sophisticated means, including personal monitors. For primary care health-care providers, simply asking a few questions and documenting the answers in the medical record can help gauge the extent of exposure. For indoor air pollution, asking what type of fuel is used, how the home is ventilated, and how much time is spent around the fire may provide important information. For outdoor air pollution exposure, the questions should center around the proximity to sources of pollution (usually industrial and roadway) and exposure time.26
In advising patients, avoidance is the most important intervention; almost any means that reduce air pollution may be beneficial. Much international effort has gone into developing and deploying better household stoves.107 Reducing cookstove toxic emissions reduced BP in pregnant women at their regular prenatal visits. The reduction was greatest in those who had hypertension.108
Personal respirators (facemasks) can reduce inhaled particulates. Wearing personal respirators while being active in central Beijing reduced BP and heart rate variability, markers associated with cardiovascular morbidity.109 The beneficial effects of personal respirators extended to other cardiovascular markers and were almost immediate and lasted during the exposure time.110
Air purifiers also reduce PM. Air purification for just 48 h significantly decreased PM2.5 and reduced circulating inflammatory and thrombogenic biomarkers as well as systolic and diastolic BPs.111 In another study, air filtration improved endothelial function and decreased concentrations of inflammatory biomarkers but not markers of oxidative stress.112
Last, health-care workers are often influential members of communities, and it is their duty to advocate for clean air on behalf of their patients. Their influence can mobilize the attitudes of communities to cleaner and safer air.
Summary and Resolve
Air pollution is one of the most important avoidable risks to health globally. Air pollution has been termed the “silent killer” by the World Health Organization113 because its effects often go unnoticed or are not easily measured. Even when there is organ harm, it is usually attributed to an unknown or chance malfunction of that organ. Although the lungs have been the most studied organ, air pollution affects most systems. Many studies have found harmful effects of air pollution on a continuum of exposure that extends down into levels considered safe by national standards.
The good news is that the problem of air pollution can be addressed and ameliorated. Improving air quality may have almost immediate benefit, seen as increased infant birth weight with the 2008 Beijing Olympics,114 improved lung-function growth in children in the Children’s Health Study,90 and improved mortality seen in the Harvard Six Cities study.115 Improving air quality, then, may give us better and longer lives in a relatively short time.116
Acknowledgments
Financial/nonfinancial disclosures: None declared.
Other contributions: Laura Feldman, MPH, contributed content regarding maternal exposure to air pollution and adverse effects on fetal health.
Footnotes
FUNDING/SUPPORT: The contribution by G. D. T. was supported in part by a National Institute of Environmental Health Sciences Center grant [Grant E500260] to the New York University School of Medicine.
References
- 1.Majkowska-Wojciechowska B., Pelka J., Korzon L. Prevalence of allergy, patterns of allergic sensitization and allergy risk factors in rural and urban children. Allergy. 2007;62(9):1044–1050. doi: 10.1111/j.1398-9995.2007.01457.x. [DOI] [PubMed] [Google Scholar]
- 2.Patel M.M., Quinn J.W., Jung K.H. Traffic density and stationary sources of air pollution associated with wheeze, asthma, and immunoglobulin E from birth to age 5 years among New York City children. Environ Res. 2011;111(8):1222–1229. doi: 10.1016/j.envres.2011.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Deng Q., Lu C., Yu Y., Li Y., Sundell J., Norback D. Early life exposure to traffic-related air pollution and allergic rhinitis in preschool children. Respir Med. 2016;121:67–73. doi: 10.1016/j.rmed.2016.10.016. [DOI] [PubMed] [Google Scholar]
- 4.Teng B., Zhang X., Yi C. The association between ambient air pollution and allergic rhinitis: further epidemiological evidence from Changchun, Northeastern China. Int J Environ Res Public Health. 2017;14(3) doi: 10.3390/ijerph14030226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Farhat S.C., Silva C.A., Orione M.A., Campos L.M., Sallum A.M., Braga A.L. Air pollution in autoimmune rheumatic diseases: a review. Autoimmun Rev. 2011;11(1):14–21. doi: 10.1016/j.autrev.2011.06.008. [DOI] [PubMed] [Google Scholar]
- 6.Ritz S.A. Air pollution as a potential contributor to the ‘epidemic’ of autoimmune disease. Med Hypotheses. 2010;74(1):110–117. doi: 10.1016/j.mehy.2009.07.033. [DOI] [PubMed] [Google Scholar]
- 7.Bernatsky S., Smargiassi A., Barnabe C. Fine particulate air pollution and systemic autoimmune rheumatic disease in two Canadian provinces. Environ Res. 2016;146:85–91. doi: 10.1016/j.envres.2015.12.021. [DOI] [PubMed] [Google Scholar]
- 8.Prada D., Zhong J., Colicino E. Association of air particulate pollution with bone loss over time and bone fracture risk: analysis of data from two independent studies. Lancet Planet Health. 2017;1:e337–e347. doi: 10.1016/S2542-5196(17)30136-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chang K.H., Chang M.Y., Muo C.H. Exposure to air pollution increases the risk of osteoporosis: a nationwide longitudinal study. Medicine (Baltimore) 2015;94(17):e733. doi: 10.1097/MD.0000000000000733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Alvaer K., Meyer H.E., Falch J.A., Nafstad P., Sogaard A.J. Outdoor air pollution and bone mineral density in elderly men—the Oslo Health Study. Osteoporos Int. 2007;18(12):1669–1674. doi: 10.1007/s00198-007-0424-y. [DOI] [PubMed] [Google Scholar]
- 11.Alver K., Meyer H.E., Falch J.A., Sogaard A.J. Outdoor air pollution, bone density and self-reported forearm fracture: the Oslo Health Study. Osteoporos Int. 2010;21(10):1751–1760. doi: 10.1007/s00198-009-1130-8. [DOI] [PubMed] [Google Scholar]
- 12.International Agency for Research on Cancer . International Agency for Research on Cancer; Lyon, France: 2016. IARC Monographs on the Evaluation of Carcinogenic Risks to Humans. Outdoor Air Pollution. [Google Scholar]
- 13.Hamra G.B., Guha N., Cohen A. Outdoor particulate matter exposure and lung cancer: a systematic review and meta-analysis. Environ Health Perspect. 2014;122(9):906–911. doi: 10.1289/ehp/1408092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.DeMarini D.M. Genotoxicity biomarkers associated with exposure to traffic and near-road atmospheres: a review. Mutagenesis. 2013;28(5):485–505. doi: 10.1093/mutage/get042. [DOI] [PubMed] [Google Scholar]
- 15.Benbrahim-Tallaa L., Baan R.A., Grosse Y. Carcinogenicity of diesel-engine and gasoline-engine exhausts and some nitroarenes. Lancet Oncol. 2012;13(7):663–664. doi: 10.1016/s1470-2045(12)70280-2. [DOI] [PubMed] [Google Scholar]
- 16.International Agency for Research on Cancer . International Agency for Research on Cancer; Lyon, France: 2014. IARC Monographs on the Evaluation of Carcinogenic Risks to Humans, Diesel and Gasoline Engine Exhaust and Some Nitroarenes. [Google Scholar]
- 17.Kachuri L., Villeneuve P.J., Parent M.E. Workplace exposure to diesel and gasoline engine exhausts and the risk of colorectal cancer in Canadian men. Environ Health. 2016;15:4. doi: 10.1186/s12940-016-0088-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chiu H.F., Tsai S.S., Chen P.S. Traffic air pollution and risk of death from gastric cancer in Taiwan: petrol station density as an indicator of air pollutant exposure. J Toxicol Environ Health A. 2011;74(18):1215–1224. doi: 10.1080/15287394.2011.590100. [DOI] [PubMed] [Google Scholar]
- 19.Castano-Vinyals G., Cantor K.P., Malats N. Air pollution and risk of urinary bladder cancer in a case-control study in Spain. Occup Environ Med. 2008;65(1):56–60. doi: 10.1136/oem.2007.034348. [DOI] [PubMed] [Google Scholar]
- 20.Tsai S.S., Tiao M.M., Kuo H.W., Wu T.N., Yang C.Y. Association of bladder cancer with residential exposure to petrochemical air pollutant emissions in Taiwan. J Toxicol Environ Health A. 2009;72(2):53–59. doi: 10.1080/15287390802476934. [DOI] [PubMed] [Google Scholar]
- 21.Yanagi Y., Assuncao J.V., Barrozo L.V. The impact of atmospheric particulate matter on cancer incidence and mortality in the city of Sao Paulo, Brazil. Cad Saude Publica. 2012;28(9):1737–1748. doi: 10.1590/s0102-311x2012000900012. [DOI] [PubMed] [Google Scholar]
- 22.Turner M.C., Krewski D., Diver W.R. Ambient air pollution and cancer mortality in the Cancer Prevention Study II. Environ Health Perspect. 2017;125(8):087013. doi: 10.1289/EHP1249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Janitz A.E., Campbell J.E., Magzamen S., Pate A., Stoner J.A., Peck J.D. Benzene and childhood acute leukemia in Oklahoma. Environ Res. 2017;158:167–173. doi: 10.1016/j.envres.2017.06.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lavigne E., Belair M.A., Do M.T. Maternal exposure to ambient air pollution and risk of early childhood cancers: a population-based study in Ontario, Canada. Environ Int. 2017;100:139–147. doi: 10.1016/j.envint.2017.01.004. [DOI] [PubMed] [Google Scholar]
- 25.Brook R.D., Franklin B., Cascio W. Air pollution and cardiovascular disease: a statement for healthcare professionals from the Expert Panel on Population and Prevention Science of the American Heart Association. Circulation. 2004;109(21):2655–2671. doi: 10.1161/01.CIR.0000128587.30041.C8. [DOI] [PubMed] [Google Scholar]
- 26.Hadley M.B., Baumgartner J., Vedanthan R. Developing a clinical approach to air pollution and cardiovascular health. Circulation. 2018;137(7):725–742. doi: 10.1161/CIRCULATIONAHA.117.030377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Zanobetti A., Franklin M., Koutrakis P., Schwartz J. Fine particulate air pollution and its components in association with cause-specific emergency admissions. Environ Health. 2009;8:58. doi: 10.1186/1476-069X-8-58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.An Z., Jin Y., Li J., Li W., Wu W. Impact of particulate air pollution on cardiovascular health. Curr Allergy Asthma Rep. 2018;18(3):15. doi: 10.1007/s11882-018-0768-8. [DOI] [PubMed] [Google Scholar]
- 29.Aronow W.S., Isbell M.W. Carbon monoxide effect on exercise-induced angina pectoris. Ann Intern Med. 1973;79(3):392–395. doi: 10.7326/0003-4819-79-3-392. [DOI] [PubMed] [Google Scholar]
- 30.Wellenius G.A., Schwartz J., Mittleman M.A. Air pollution and hospital admissions for ischemic and hemorrhagic stroke among medicare beneficiaries. Stroke. 2005;36(12):2549–2553. doi: 10.1161/01.STR.0000189687.78760.47. [DOI] [PubMed] [Google Scholar]
- 31.Wellenius G.A., Burger M.R., Coull B.A. Ambient air pollution and the risk of acute ischemic stroke. Arch Intern Med. 2012;172(3):229–234. doi: 10.1001/archinternmed.2011.732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Franklin B.A., Brook R., Arden Pope C., III Air pollution and cardiovascular disease. Curr Probl Cardiol. 2015;40(5):207–238. doi: 10.1016/j.cpcardiol.2015.01.003. [DOI] [PubMed] [Google Scholar]
- 33.Vallejo M., Ruiz S., Hermosillo A.G., Borja-Aburto V.H., Cardenas M. Ambient fine particles modify heart rate variability in young healthy adults. J Expo Sci Environ Epidemiol. 2006;16(2):125–130. doi: 10.1038/sj.jea.7500447. [DOI] [PubMed] [Google Scholar]
- 34.Cheng Y.J., Lauer M.S., Earnest C.P. Heart rate recovery following maximal exercise testing as a predictor of cardiovascular disease and all-cause mortality in men with diabetes. Diabetes Care. 2003;26(7):2052–2057. doi: 10.2337/diacare.26.7.2052. [DOI] [PubMed] [Google Scholar]
- 35.Miller K.A., Siscovick D.S., Sheppard L. Long-term exposure to air pollution and incidence of cardiovascular events in women. N Engl J Med. 2007;356(5):447–458. doi: 10.1056/NEJMoa054409. [DOI] [PubMed] [Google Scholar]
- 36.Newby D.E., Mannucci P.M., Tell G.S. Expert position paper on air pollution and cardiovascular disease. Eur Heart J. 2015;36(2):83b–93b. doi: 10.1093/eurheartj/ehu458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Pope C.A., III, Burnett R.T., Thurston G.D. Cardiovascular mortality and long-term exposure to particulate air pollution: epidemiological evidence of general pathophysiological pathways of disease. Circulation. 2004;109(1):71–77. doi: 10.1161/01.CIR.0000108927.80044.7F. [DOI] [PubMed] [Google Scholar]
- 38.Thurston G.D., Burnett R.T., Turner M.C. Ischemic heart disease mortality and long-term exposure to source-related components of US fine particle air pollution. Environ Health Perspect. 2016;124(6):785–794. doi: 10.1289/ehp.1509777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Chen H., Kwong J.C., Copes R. Living near major roads and the incidence of dementia, Parkinson's disease, and multiple sclerosis: a population-based cohort study. Lancet. 2017;389(10070):718–726. doi: 10.1016/S0140-6736(16)32399-6. [DOI] [PubMed] [Google Scholar]
- 40.Tamagawa E., Bai N., Morimoto K. Particulate matter exposure induces persistent lung inflammation and endothelial dysfunction. Am J Physiol Lung Cell Mol Physiol. 2008;295(1):L79–L85. doi: 10.1152/ajplung.00048.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Elder A., Gelein R., Silva V. Translocation of inhaled ultrafine manganese oxide particles to the central nervous system. Environ Health Perspect. 2006;114(8):1172–1178. doi: 10.1289/ehp.9030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Guxens M., Garcia-Esteban R., Giorgis-Allemand L. Air pollution during pregnancy and childhood cognitive and psychomotor development: six European birth cohorts. Epidemiology. 2014;25(5):636–647. doi: 10.1097/EDE.0000000000000133. [DOI] [PubMed] [Google Scholar]
- 43.Jedrychowski W.A., Perera F.P., Camann D. Prenatal exposure to polycyclic aromatic hydrocarbons and cognitive dysfunction in children. Environ Sci Pollut Res Int. 2015;22(5):3631–3639. doi: 10.1007/s11356-014-3627-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Calderon-Garciduenas L., Mora-Tiscareno A., Ontiveros E. Air pollution, cognitive deficits and brain abnormalities: a pilot study with children and dogs. Brain Cogn. 2008;68(2):117–127. doi: 10.1016/j.bandc.2008.04.008. [DOI] [PubMed] [Google Scholar]
- 45.Lam J., Sutton P., Kalkbrenner A. A systematic review and meta-analysis of multiple airborne pollutants and autism spectrum disorder. PLoS One. 2016;11(9):e0161851. doi: 10.1371/journal.pone.0161851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Liu L., Zhang D., Rodzinka-Pasko J.K., Li Y.M. Environmental risk factors for autism spectrum disorders. Nervenarzt. 2016;87(suppl 2):55–61. doi: 10.1007/s00115-016-0172-3. [DOI] [PubMed] [Google Scholar]
- 47.Fordyce T.A., Leonhard M.J., Chang E.T. A critical review of developmental exposure to particulate matter, autism spectrum disorder, and attention deficit hyperactivity disorder. J Environ Sci Health A Tox Hazard Subst Environ Eng. 2018;53(2):174–204. doi: 10.1080/10934529.2017.1383121. [DOI] [PubMed] [Google Scholar]
- 48.Wellenius G.A., Boyle L.D., Coull B.A. Residential proximity to nearest major roadway and cognitive function in community-dwelling seniors: results from the MOBILIZE Boston Study. J Am Geriatr Soc. 2012;60(11):2075–2080. doi: 10.1111/j.1532-5415.2012.04195.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Wilker E.H., Preis S.R., Beiser A.S. Long-term exposure to fine particulate matter, residential proximity to major roads and measures of brain structure. Stroke. 2015;46(5):1161–1166. doi: 10.1161/STROKEAHA.114.008348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Zanobetti A., Dominici F., Wang Y., Schwartz J.D. A national case-crossover analysis of the short-term effect of PM2.5 on hospitalizations and mortality in subjects with diabetes and neurological disorders. Environ Health. 2014;13(1):38. doi: 10.1186/1476-069X-13-38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Eze I.C., Hemkens L.G., Bucher H.C. Association between ambient air pollution and diabetes mellitus in Europe and North America: systematic review and meta-analysis. Environ Health Perspect. 2015;123(5):381–389. doi: 10.1289/ehp.1307823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Honda T., Pun V.C., Manjourides J., Suh H. Associations between long-term exposure to air pollution, glycosylated hemoglobin and diabetes. Int J Hyg Environ Health. 2017;220(7):1124–1132. doi: 10.1016/j.ijheh.2017.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Raaschou-Nielsen O., Sorensen M., Ketzel M. Long-term exposure to traffic-related air pollution and diabetes-associated mortality: a cohort study. Diabetologia. 2013;56(1):36–46. doi: 10.1007/s00125-012-2698-7. [DOI] [PubMed] [Google Scholar]
- 54.Eze I.C., Schaffner E., Foraster M. Long-term exposure to ambient air pollution and metabolic syndrome in adults. PLoS One. 2015;10(6):e0130337. doi: 10.1371/journal.pone.0130337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Li W., Dorans K.S., Wilker E.H. Residential proximity to major roadways, fine particulate matter, and adiposity: the Framingham Heart Study. Obesity (Silver Spring) 2016;24(12):2593–2599. doi: 10.1002/oby.21630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Xu Z., Xu X., Zhong M. Ambient particulate air pollution induces oxidative stress and alterations of mitochondria and gene expression in brown and white adipose tissues. Part Fibre Toxicol. 2011;8:20. doi: 10.1186/1743-8977-8-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Alderete T.L., Habre R., Toledo-Corral C.M. Longitudinal associations between ambient air pollution with insulin sensitivity, beta-cell function, and adiposity in Los Angeles Latino children. Diabetes. 2017;66(7):1789–1796. doi: 10.2337/db16-1416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Calderon-Garciduenas L., Franco-Lira M., D'Angiulli A. Mexico City normal weight children exposed to high concentrations of ambient PM2.5 show high blood leptin and endothelin-1, vitamin D deficiency, and food reward hormone dysregulation versus low pollution controls. Relevance for obesity and Alzheimer disease. Environ Res. 2015;140:579–592. doi: 10.1016/j.envres.2015.05.012. [DOI] [PubMed] [Google Scholar]
- 59.Rao X., Patel P., Puett R., Rajagopalan S. Air pollution as a risk factor for type 2 diabetes. Toxicol Sci. 2015;143(2):231–241. doi: 10.1093/toxsci/kfu250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Jerrett M., McConnell R., Wolch J. Traffic-related air pollution and obesity formation in children: a longitudinal, multilevel analysis. Environ Health. 2014;13:49. doi: 10.1186/1476-069X-13-49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Chang C.J., Yang H.H., Chang C.A., Tsai H.Y. Relationship between air pollution and outpatient visits for nonspecific conjunctivitis. Invest Ophthalmol Vis Sci. 2012;53(1):429–433. doi: 10.1167/iovs.11-8253. [DOI] [PubMed] [Google Scholar]
- 62.Ravilla T.D., Gupta S., Ravindran R.D. Use of cooking fuels and cataract in a population-based study: the India Eye Disease Study. Environ Health Perspect. 2016;124(12):1857–1862. doi: 10.1289/EHP193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Hwang SH, Choi YH, Paik HJ, Wee WR, Kim MK, Kim DH. Potential importance of ozone in the association between outdoor air pollution and dry eye disease in South Korea [published online ahead of print March 10, 2016]. JAMA Ophthalmol. https://doi.org/10.1001/jamaophthalmol.2016.0139. [DOI] [PubMed]
- 64.Malerbi F.K., Martins L.C., Saldiva P.H., Braga A.L. Ambient levels of air pollution induce clinical worsening of blepharitis. Environ Res. 2012;112:199–203. doi: 10.1016/j.envres.2011.11.010. [DOI] [PubMed] [Google Scholar]
- 65.Kaplan G.G., Hubbard J., Korzenik J. The inflammatory bowel diseases and ambient air pollution: a novel association. Am J Gastroenterol. 2010;105(11):2412–2419. doi: 10.1038/ajg.2010.252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Opstelten J.L., Beelen R.M., Leenders M. Exposure to ambient air pollution and the risk of inflammatory bowel disease: a European nested case-control study. Dig Dis Sci. 2016;61(10):2963–2971. doi: 10.1007/s10620-016-4249-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Xu C., Kan H.D., Fan Y.N. Acute effects of air pollution on enteritis admissions in Xi'an, China. J Toxicol Environ Health A. 2016;79(24):1183–1189. doi: 10.1080/15287394.2016.1227006. [DOI] [PubMed] [Google Scholar]
- 68.Wong C.M., Tsang H., Lai H.K. STROBE—long-term exposure to ambient fine particulate air pollution and hospitalization due to peptic ulcers. Medicine (Baltimore) 2016;95(18):e3543. doi: 10.1097/MD.0000000000003543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Kaplan G.G., Tanyingoh D., Dixon E. Ambient ozone concentrations and the risk of perforated and nonperforated appendicitis: a multicity case-crossover study. Environ Health Perspect. 2013;121(8):939–943. doi: 10.1289/ehp.1206085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Robertson S., Miller M.R. Ambient air pollution and thrombosis. Part Fibre Toxicol. 2018;15(1):1. doi: 10.1186/s12989-017-0237-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Peters A., Dockery D.W., Muller J.E., Mittleman M.A. Increased particulate air pollution and the triggering of myocardial infarction. Circulation. 2001;103(23):2810–2815. doi: 10.1161/01.cir.103.23.2810. [DOI] [PubMed] [Google Scholar]
- 72.Franchini M., Mengoli C., Cruciani M., Bonfanti C., Mannucci P.M. Association between particulate air pollution and venous thromboembolism: a systematic literature review. Eur J Intern Med. 2016;27:10–13. doi: 10.1016/j.ejim.2015.11.012. [DOI] [PubMed] [Google Scholar]
- 73.Roels H., Bruaux P., Buchet J.P. Impact of air pollution by lead on the heme biosynthetic pathway in school-age children. Arch Environ Health. 1976;31(6):310–316. doi: 10.1080/00039896.1976.10667241. [DOI] [PubMed] [Google Scholar]
- 74.Accinelli R.A., Leon-Abarca J.A. Solid fuel use is associated with anemia in children. Environ Res. 2017;158:431–435. doi: 10.1016/j.envres.2017.06.032. [DOI] [PubMed] [Google Scholar]
- 75.Honda T., Pun V.C., Manjourides J., Suh H. Anemia prevalence and hemoglobin levels are associated with long-term exposure to air pollution in an older population. Environ Int. 2017;101:125–132. doi: 10.1016/j.envint.2017.01.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Yallop D., Duncan E.R., Norris E. The associations between air quality and the number of hospital admissions for acute pain and sickle-cell disease in an urban environment. Br J Haematol. 2007;136(6):844–848. doi: 10.1111/j.1365-2141.2007.06493.x. [DOI] [PubMed] [Google Scholar]
- 77.Li W., Dorans K.S., Wilker E.H. Residential proximity to major roadways, fine particulate matter, and hepatic steatosis: the Framingham Heart Study. Am J Epidemiol. 2017;186(7):857–865. doi: 10.1093/aje/kwx127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Kim J.W., Park S., Lim C.W., Lee K., Kim B. The role of air pollutants in initiating liver disease. Toxicol Res. 2014;30(2):65–70. doi: 10.5487/TR.2014.30.2.065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Pan W.C., Wu C.D., Chen M.J. Fine particle pollution, alanine transaminase, and liver cancer: a Taiwanese prospective cohort study (REVEAL-HBV) J Natl Cancer Inst. 2016;108(3) doi: 10.1093/jnci/djv341. [DOI] [PubMed] [Google Scholar]
- 80.Deng H., Eckel S.P., Liu L., Lurmann F.W., Cockburn M.G., Gilliland F.D. Particulate matter air pollution and liver cancer survival. Int J Cancer. 2017;141(4):744–749. doi: 10.1002/ijc.30779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Wood A.M., Harrison R.M., Semple S., Ayres J.G., Stockley R.A. Outdoor air pollution is associated with rapid decline of lung function in alpha-1-antitrypsin deficiency. Occup Environ Med. 2010;67(8):556–561. doi: 10.1136/oem.2009.047589. [DOI] [PubMed] [Google Scholar]
- 82.Nemmar A., Karaca T., Beegam S. Prolonged pulmonary exposure to diesel exhaust particles exacerbates renal oxidative stress, inflammation and DNA damage in mice with adenine-induced chronic renal failure. Cell Physiol Biochem. 2016;38(5):1703–1713. doi: 10.1159/000443109. [DOI] [PubMed] [Google Scholar]
- 83.Lue S.H., Wellenius G.A., Wilker E.H., Mostofsky E., Mittleman M.A. Residential proximity to major roadways and renal function. J Epidemiol Community Health. 2013;67(8):629–634. doi: 10.1136/jech-2012-202307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Yang Y.R., Chen Y.M., Chen S.Y., Chan C.C. Associations between long-term particulate matter exposure and adult renal function in the Taipei metropolis. Environ Health Perspect. 2017;125(4):602–607. doi: 10.1289/EHP302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Cohen A.J., Brauer M., Burnett R. Estimates and 25-year trends of the global burden of disease attributable to ambient air pollution: an analysis of data from the Global Burden of Diseases Study 2015. Lancet. 2017;389(10082):1907–1918. doi: 10.1016/S0140-6736(17)30505-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.World Health Organization . World Health Organization; Geneva, Switzerland: 2018. Household Air Pollution and Health. [Google Scholar]
- 87.Gordon S.B., Bruce N.G., Grigg J. Respiratory risks from household air pollution in low and middle income countries. Lancet Respir Med. 2014;2(10):823–860. doi: 10.1016/S2213-2600(14)70168-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Schraufnagel D.E., Balmes J.R., Cowl C.T. Air pollution and noncommunicable diseases: a review by the Forum of International Respiratory Societies’ Environmental Committee, Part 1: the damaging effects of air pollution. Chest. 2019;155(2):409–416. doi: 10.1016/j.chest.2018.10.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Rojas-Martinez R., Perez-Padilla R., Olaiz-Fernandez G. Lung function growth in children with long-term exposure to air pollutants in Mexico City. Am J Respir Crit Care Med. 2007;176(4):377–384. doi: 10.1164/rccm.200510-1678OC. [DOI] [PubMed] [Google Scholar]
- 90.Gauderman W.J., Urman R., Avol E. Association of improved air quality with lung development in children. N Engl J Med. 2015;372(10):905–913. doi: 10.1056/NEJMoa1414123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Lepeule J., Bind M.A., Baccarelli A.A. Epigenetic influences on associations between air pollutants and lung function in elderly men: the Normative Aging Study. Environ Health Perspect. 2014;122(6):566–572. doi: 10.1289/ehp.1206458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.McConnell R., Islam T., Shankardass K. Childhood incident asthma and traffic-related air pollution at home and school. Environ Health Perspect. 2010;118(7):1021–1026. doi: 10.1289/ehp.0901232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Young M.T., Sandler D.P., DeRoo L.A., Vedal S., Kaufman J.D., London S.J. Ambient air pollution exposure and incident adult asthma in a nationwide cohort of US women. Am J Respir Crit Care Med. 2014;190(8):914–921. doi: 10.1164/rccm.201403-0525OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Schikowski T., Adam M., Marcon A. Association of ambient air pollution with the prevalence and incidence of COPD. Eur Respir J. 2014;44(3):614–626. doi: 10.1183/09031936.00132213. [DOI] [PubMed] [Google Scholar]
- 95.Cui P., Huang Y., Han J., Song F., Chen K. Ambient particulate matter and lung cancer incidence and mortality: a meta-analysis of prospective studies. Eur J Public Health. 2015;25(2):324–329. doi: 10.1093/eurpub/cku145. [DOI] [PubMed] [Google Scholar]
- 96.Joo Y.H., Lee S.S., Han K.D., Park K.H. Association between chronic laryngitis and particulate matter based on the Korea National Health and Nutrition Examination Survey 2008-2012. PLoS One. 2015;10(7):e0133180. doi: 10.1371/journal.pone.0133180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.To T., Zhu J., Larsen K., Simatovic J., Feldman L., Ryckman K. Progression from asthma to chronic obstructive pulmonary disease. Is air pollution a risk factor? Am J Respir Crit Care Med. 2016;194(4):429–438. doi: 10.1164/rccm.201510-1932OC. [DOI] [PubMed] [Google Scholar]
- 98.Kurmi O.P., Semple S., Simkhada P., Smith W.C., Ayres J.G. COPD and chronic bronchitis risk of indoor air pollution from solid fuel: a systematic review and meta-analysis. Thorax. 2010;65(3):221–228. doi: 10.1136/thx.2009.124644. [DOI] [PubMed] [Google Scholar]
- 99.Sunyer J., Spix C., Quenel P., Ponce-de-Leon A., Ponka A., Barumandzadeh T. Urban air pollution and emergency admissions for asthma in four European cities: the APHEA Project. Thorax. 1997;52(9):760–765. doi: 10.1136/thx.52.9.760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Song Q., Christiani D.C., Xiaorong W., Ren J. The global contribution of outdoor air pollution to the incidence, prevalence, mortality and hospital admission for chronic obstructive pulmonary disease: a systematic review and meta-analysis. Int J Environ Res Public Health. 2014;11(11):11822–11832. doi: 10.3390/ijerph111111822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Darrow L.A., Klein M., Flanders W.D., Mulholland J.A., Tolbert P.E., Strickland M.J. Air pollution and acute respiratory infections among children 0-4 years of age: an 18-year time-series study. Am J Epidemiol. 2014;180(10):968–977. doi: 10.1093/aje/kwu234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Lefebvre M.A., Pham D.M., Boussouira B., Bernard D., Camus C., Nguyen Q.L. Evaluation of the impact of urban pollution on the quality of skin: a multicentre study in Mexico. Int J Cosmet Sci. 2015;37(3):329–338. doi: 10.1111/ics.12203. [DOI] [PubMed] [Google Scholar]
- 103.Liu W., Pan X., Vierkotter A. A time-series study of the effect of air pollution on outpatient visits for acne vulgaris in Beijing. Skin Pharmacol Physiol. 2018;31(2):107–113. doi: 10.1159/000484482. [DOI] [PubMed] [Google Scholar]
- 104.Kousha T., Valacchi G. The air quality health index and emergency department visits for urticaria in Windsor, Canada. J Toxicol Environ Health A. 2015;78(8):524–533. doi: 10.1080/15287394.2014.991053. [DOI] [PubMed] [Google Scholar]
- 105.Lee Y.L., Su H.J., Sheu H.M., Yu H.S., Guo Y.L. Traffic-related air pollution, climate, and prevalence of eczema in Taiwanese school children. J Invest Dermatol. 2008;128(10):2412–2420. doi: 10.1038/jid.2008.110. [DOI] [PubMed] [Google Scholar]
- 106.Li M., Vierkotter A., Schikowski T. Epidemiological evidence that indoor air pollution from cooking with solid fuels accelerates skin aging in Chinese women. J Dermatol Sci. 2015;79(2):148–154. doi: 10.1016/j.jdermsci.2015.04.001. [DOI] [PubMed] [Google Scholar]
- 107.World Health Organization . World Health Organization; Geneva, Switzerland: 2014. WHO Guidelines for Indoor Air Quality, Household Fuel Combustion. [Google Scholar]
- 108.Alexander D., Northcross A., Wilson N. Randomized controlled ethanol cookstove intervention and blood pressure in pregnant Nigerian women. Am J Respir Crit Care Med. 2017;195(12):1629–1639. doi: 10.1164/rccm.201606-1177OC. [DOI] [PubMed] [Google Scholar]
- 109.Langrish J.P., Mills N.L., Chan J.K. Beneficial cardiovascular effects of reducing exposure to particulate air pollution with a simple facemask. Part Fibre Toxicol. 2009;6:8. doi: 10.1186/1743-8977-6-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Yang X, Jia X, Dong W, et al. Cardiovascular benefits of reducing personal exposure to traffic-related noise and particulate air pollution: a randomized crossover study in the Beijing subway system [published online ahead of print June 13, 2018]. Indoor Air. 10.1111/ina.12485. [DOI] [PubMed]
- 111.Chen R., Zhao A., Chen H. Cardiopulmonary benefits of reducing indoor particles of outdoor origin: a randomized, double-blind crossover trial of air purifiers. J Am Coll Cardiol. 2015;65(21):2279–2287. doi: 10.1016/j.jacc.2015.03.553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Allen R.W., Carlsten C., Karlen B. An air filter intervention study of endothelial function among healthy adults in a woodsmoke-impacted community. Am J Respir Crit Care Med. 2011;183(9):1222–1230. doi: 10.1164/rccm.201010-1572OC. [DOI] [PubMed] [Google Scholar]
- 113.World Health Organization . World Health Organization; Geneva: 2018. Air pollution, the invisible killer. http://www.who.int/airpollution/en/. Accessed December 19, 2018. [Google Scholar]
- 114.Huang C., Nichols C., Liu Y. Ambient air pollution and adverse birth outcomes: a natural experiment study. Popul Health Metr. 2015;13:17. doi: 10.1186/s12963-015-0050-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Laden F., Schwartz J., Speizer F.E., Dockery D.W. Reduction in fine particulate air pollution and mortality: extended follow-up of the Harvard Six Cities study. Am J Respir Crit Care Med. 2006;173(6):667–672. doi: 10.1164/rccm.200503-443OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Pope C.A., III, Ezzati M., Dockery D.W. Fine-particulate air pollution and life expectancy in the United States. N Engl J Med. 2009;360(4):376–386. doi: 10.1056/NEJMsa0805646. [DOI] [PMC free article] [PubMed] [Google Scholar]