Abstract
Background.
Studies have shown that physical activity can reduce the risk of mortality for female breast cancer patients and improve quality of life, reduce weight, and alter circulating biomarker levels. We conducted a pilot trial to determine the feasibility of increasing physical activity through a cultural dance intervention to achieve similar benefits.
Methods.
Conducted a pilot trial implementing a cultural dance intervention to increase and sustain physical activity for breast cancer survivors, which consisted of a six-month group-based intervention of Hula Dance. Anthropometric measures, fasting blood draws, and self-reported questionnaires to assess physical activity, mood, and quality of life, were completed at baseline, at the end of the 6-month intervention (time point month-6), and at two additional post-intervention time points at month-12 and month-24 to assess sustainability.
Results.
A total of 11 women with a median age of 63 years were enrolled in the intervention trial. Eight of the 11 (73%) completed the trial to month-12 and demonstrated an overall significant increase in weekly moderate exercise. There were no significant changes in intra-individual body mass index (BMI). However, there was a sustained post-intervention reduction in waist circumference and significant changes in circulating biomarker levels. For the self-reported measures, there was a significant increase in vigor/activity (p<0.001; Profile of Mood States-Short Form).
Conclusion.
Our intervention pilot trial demonstrated that a cultural dance program could achieve a sustainable increase in physical activity for breast cancer survivors, with potential to improve quality of life, increase vigor, and decrease levels of circulating cytokines associated with obesity and inflammation.
Keywords: survivor, breast cancer, physical activity, Hula Dance, biomarker
Background
There are over 3 million female breast cancer survivors in the U.S., and the number of survivors continues to rise with improved prevention and treatment strategies (www.cancer.org; American Cancer Society. Cancer Facts and Figures 2018. Atlanta, GA: American Cancer Society; 2018.) In addition, there have been increasing efforts to reduce the risk of recurrence and improve the quality of life (QOL) for individuals following breast cancer diagnosis and treatment.
Multiple studies have established that physical activity can reduce the risk of mortality for female breast cancer patients 1–8. A meta-analysis reported that physical activity after diagnosis was associated with a 34% lower risk of breast cancer-specific mortality, 41% lower risk of all-cause mortality, and 24% lower risk of breast cancer recurrence for breast cancer survivors 9. The American College of Sports Medicine (ACSM) recommends that cancer survivors engage in MVPA for at least 150 min/wk 10, 11. However, only an estimated 35% of individuals with breast cancer are achieving this level of physical activity after their diagnosis 10–12. It is a critical challenge to provide support to breast cancer survivors to maintain, or adopt, a physically active lifestyle to meet these recommendations.
Exercise interventions to increase physical activity have been implemented with overall positive efficacy for breast cancer survivors 13–16. Some of the demonstrated benefits of physical activity interventions for breast cancer survivors include, a decrease in body weight and insulin resistance, improvements in physical function and QOL, and reduction of depression, anxiety, and fatigue 14, 17–24. In addition, studies have demonstrated that physical activity can prevent cognitive decline 25, 26, with dance having more cognitive impact than other forms of conventional physical activity regimens (e.g. walking, jogging, and gym-based exercise) 27, 28.
Increasing evidence indicates that obesity and inflammation have key roles in cancer biology 29–31. As obesity negatively influences disease prognosis for women with breast cancer 32–34, effective lifestyle modifications (e.g. increasing physical activity) to reduce the negative effects of obesity-related factors that contribute to mortality are critically needed for breast cancer patients. The beneficial effects of physical activity for cancer survival have been attributed to reducing systemic inflammation by altering circulating levels of inflammatory cytokines 15, 16, 35. In addition, physical activity can alter circulating levels of hormones (i.e. estrogen, androgen, leptin, adiponectin), insulin, insulin-like growth factors (IGF), and IGF binding proteins (IGFBP)) 14, 31, 36–41.
There have been a limited number of intervention studies involving non-conventional modes of physical activity that may be more culturally relevant to women of multiethnic populations 42–48. Efficacy has been observed in intervention studies involving non-conventional forms of physical activity such as Tai Chi Chuan, yoga, and dance 42, 43, 45–47, 49. In one study evaluating the effects of Tai Chi Chuan on breast cancer survivors, slow, fluid, weight-bearing movements combined with controlled breathing techniques resulted in changes in blood pressure, circulating levels of insulin, IGF-1, IGFBPs, inflammatory biomarkers (IL-6, IL-2, and IFN-γ), and cortisol 43, 45, 48. Two recent intervention studies among breast cancer survivors demonstrated that yoga led to a reduction of inflammatory signaling in survivors experiencing persistent fatigue 42 and improved cognitive function 44. In another study, breast cancer survivors who completed a 6 month intervention of Greek traditional dance had an increase in physical function, an increase in handgrip strength, a reduction in arm volume, and a decrease in depression 46. These findings support the efficacy of culture-based, non-conventional modalities of physical activity for cancer survivors.
We conducted a pilot aerobic dance intervention study with a group-based Hula Dance program to increase physical activity for sedentary breast cancer survivors. Since the dance movements of Hula are taught in a class-based environment and involve aerobic activity, whole-body movement (engaging hands, arms and shoulders), and cognitive tasks (asymmetrical arm and leg movements and dance step memorization), the intent for implementing Hula to increase physical activity was to provide multidimensional benefits that a multiethnic population of breast cancer survivors would find sustainable.
Methods
Study Participants
Participants were recruited at participating medical centers in the Hawaii Cancer Consortium, from local breast cancer survivor groups, and through self-referrals in response to media announcements. The criteria for enrollment were: residency on Oahu, HI; female 21 years of age or older; histologically-confirmed diagnosis of primary breast cancer, disease Stage I through III; 6-60 months post-treatment completion of initial regional and systemic treatment; no current chemo- or radio-therapy; current use of hormone therapy or trastuzumab was allowed; approval for participation in the trial by attending physician; currently less than 60 minutes per week of moderate to vigorous exercise (i.e., sedentary); and physically capable of doing the hula-based physical activity. Participants were screened to determine if they met the eligibility criteria. Informed consent was obtained from all individuals included in the study.
Study Design
The pilot study was designed as an intervention trial to support a health behavior change. The study was initiated to determine feasibility and acceptability of the intervention and to determine if a physical activity intervention with Hula Dance would be sustainable and result in changes in self-reported well-being, anthropometry, and circulating biomarker levels.
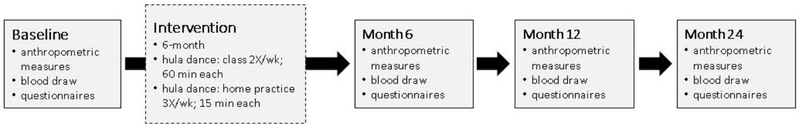
At the baseline visit, informed consent was obtained, questionnaires (QX) were reviewed for completeness, and a baseline blood draw and anthropometric measurements were taken. Blood draws, anthropometric measurements, and questionnaires were completed at four time points. The first time point was at baseline prior to the intervention program, then at three post-intervention time points, at month-6 (following the completion of the intervention), then at month-12 and 24. The protocol and informed consent were IRB-approved by the Western Institutional Review Board (WIRB) and the Clinical Trial was registered as a National Cancer Institute Clinical Trial (# ).
For a total of 6 months, participants attended a 60-minute supervised Hula Dance class twice a week and instructed to complete a 15-minute home-based Hula Dance practice three times per week with the goal of at least 150 minutes of moderate to vigorous physical activity per week. Each 60-minute Hula exercise class included a warm-up (10 minutes), conditioning (40 minutes), and cool-down (10 minutes) period. During the conditioning period a target heart rate of 50-70% of maximum heart rate (HRmax=220-age) for the intended moderate-intensity physical activity during the mid-conditioning period was the goal for participants 50. Heart rate was monitored by self-measures of the number of pulses per minute taken over the radial artery, on the inside of the wrist, for each participant. Heart rate was recorded at three time points during the 60-minute class (start of class, mid-conditioning; end of class). Every Hula class was conducted by the same Hula instructor; who has extensive experience in teaching Hula Dance and knowledge of the study guidelines. Hula is a Polynesian dance form that contains dance movements (whole body) and gestures that are in alignment to the meaning of the accompanied song. The instructor would teach the dance movements to each song in segments until the entire hula dance for each song has been memorized and can be danced in entirety. The hula dance accompanying each song would be practice multiple times through each session and throughout the six-month intervention. The physical activity dance program was designed to meet the abilities of the breast cancer survivors. An attendance log was kept to record each participant’s attendance. If the participant missed two consecutive Hula class meetings, the study coordinator contacted the participant with a reminder of the class schedule to encourage attendance.
For anthropometric assessments, a trained technician obtained participants’ height, weight, waist circumference and hip circumference measurements at each time point. Self-reported outcomes were assessed with the completion of questionnaires at each time point, with the exception of the individuals’ demographics, which was provided at the baseline visit only, e.g. information on socio-demographic and health characteristics included ethnicity, stage of breast cancer at diagnosis, treatment type, comorbidities and occupation, and family history of cancer. The Godin Exercise Questionnaire was used to assess minutes per week of exercise in the categories of light, moderate, and vigorous exercise 51. This questionnaire is a self-report measure asking participants to describe how many times they engage in strenuous, moderate, or mild physical activity during a typical 7-day period. The European Organization for Research and Treatment of Cancer Quality-of-Life Core Questionnaire (EORTC QLQ-C30) was used to assess the quality of life of cancer patient participants 52. It contains 30 items each scored on a 4 point response scale, with three categories: global health status, functional status (physical, role, emotional, cognitive, and social), and physical symptoms. The Brief Fatigue Inventory (BFI) is a 15 item measure (scored on a 11 point response scale), assessing for the severity and impact of fatigue on daily functioning during the last 24-hour period 53. The Centers for Epidemiological Studies Depression Scale (CES-D) was used to assess the presence of depression 54 with 20 items (scored on a 4 point scale) that include questions that fall into nine categories of depression (sadness, loss of interest, appetite, sleep, thinking/concentration, guilt, fatigue, movement, and suicidal ideation). The Profile of Mood States-Short Form (POMS-SF) questionnaire assessed affective states by asking participants to indicate how they have been feeling related to 65 adjectives rated on a 5-point scale 55. The 15-item, 5-point Social Constraints Scale (SCS) 56 was used to measure the degree to which participants feel their social relationships are strained due to experiencing cancer.
For circulating biomarker assessments, fasting (≥10 hours) blood was collected by a trained phlebotomist. One 10 ml EDTA collection tube was obtained at each blood draw. Whole blood was processed for plasma and buffy coat components, then aliquoted and stored at −80°C until the three time points (baseline, month- 6 and 12) could be analyzed, to minimize batch effects. Fevels of hormones, cytokines, and inflammatory markers were measured in the plasma component. To ensure reproducibility and reliability, a standard and quality control duplicates were also assayed. C-reactive protein (CRP) was assayed with the latex particle-enhanced immunoturbidimetric method using a kit (Pointe Scientific, Inc.) and a Cobas Mira Plus clinical autoanalyzer (Roche Diagnositcs); insulin, IGF-1, IGFBP3, adiponectin, and leptin were assessed by double-antibody enzyme-linked immunosorbent-assays (EFISA; R&D Systems) according to the manufacturer’s specifications; and biomarkers of inflammation (GM-CSF, IFN-Ɣ, IL-1β, IL-2, IL-4, IL-5, IL-6, IL-8, IL-10, TNF-α) were assayed with an immunoassay kit (Cytokine Human Magnetic 10-Plex Panel for the Luminex™ Instrument, ThermoFisher Scientific).
Statistical Analysis
To test for intra-individual differences in pre- and post-intervention for each of the self-reported assessments, least squares estimated (adjusted for covariates) means are shown. For the biomarker assessments, levels were adjusted for BMI at each time point. The mixed linear model (MIXED procedure; incorporating repeated measures) assessed the outcome changes over time, with a separate model run for each outcome 57. The SAS 9.4 software (SAS Institute Inc., Cary NC) performed all analyses.
Results
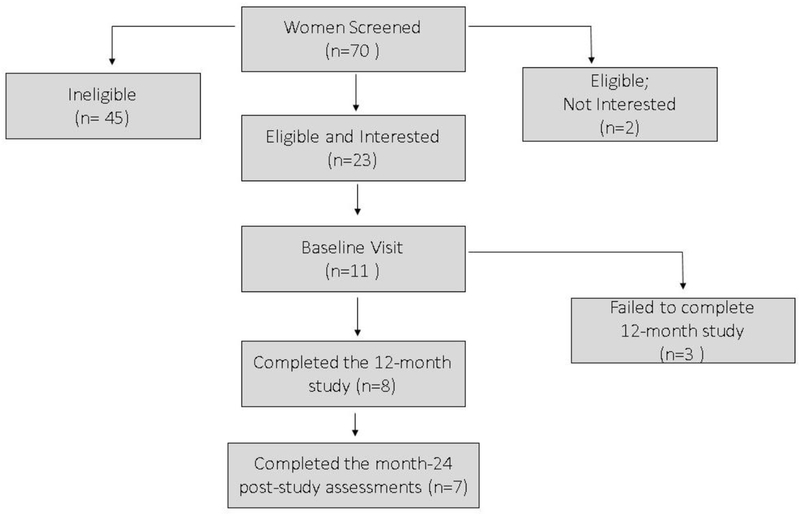
A total of 70 individuals inquired and were screened for eligibility; 45 were ineligible (generally because they were exercising more than 60 minutes per week), two were eligible but not interested after discussing the intervention parameters and requirements; 23 female breast cancer survivors were eligible and expressed an interest in participating (Figure 1). Of the 23 eligible individuals, 11 consented and completed their baseline assessments. The 11 participants had a median age of 63 years (SD=10.2 years), were diagnosed with early stage breast cancer (Stages I-II), and 2 years (median) post-diagnosis. Ten of the 11 (90%) participants self-reported as an ethnic minority (Asian/Pacific Islander).
Figure 1.
Flow chart of Hula Study participant recruitment and retention.
We assessed intra-individual changes pre-and post-intervention for anthropometry, self-reported psychosocial outcomes (questionnaires), and circulating plasma biomarkers, comparing baseline assessments to time points at months 6, 12, and 24 (Figure 2). The month-6 assessment was the assessment immediately following the intervention program, and the month-12 and 24 time points were included to assess the sustainability of the intervention, and changes associated with health-related outcomes 6 and 18 months following the end of the supervised Hula Dance program.
Figure 2.
Diagram of Hula Dance intervention time points and assessments.
To determine the feasibility of this study, we report that 9 of the 11 participants (82%) completed the Hula Dance program (0-6 months). The average attendance for the intervention phase of the nine participants was 84%. Eight of the 11 participants completed the study to the month-12 assessments and seven participants completed the month-24 assessments (anthropometric measures and self-report questionnaires). All seven participants who completed the month-24 assessments indicated that they continued to dance Hula regularly.
Anthropometric measures (weight, height, and waist and hip circumferences) were assessed. There was no significant change in body mass index (BMI) or hip circumference associated with the increased physical activity of the Hula intervention (Table 1), however there was a reduction in the waist circumference for the comparisons between the baseline and month-6, 12 and 24 time points. This reduction was statistically significant (p ≤ 0.05) for the baseline versus month-6 and month-24 time points. In addition, the reduction in the waist/hip circumference ratio for the baseline versus month-24 comparison was highly significant (p ≤ 0.001). These results suggest that the increased physical activity with the Hula Dance program led to a reduction primarily in the abdominal region, suggesting a decrease in central adiposity.
Table 1.
Intra-individual changes in anthropometry comparisons between baseline and post-intervention measures
| Anthropometric Measures | Mean Measures (n=8) | baseline vs. month 6 | Mean Measures (n=8) | baseline vs. month 12 | Mean Measures (n=7) | baseline vs. month 24 | |||
|---|---|---|---|---|---|---|---|---|---|
| baseline | month 6 | p-value | baseline | month 12 | p-value | baseline | month 24 | p-value | |
| Weight (lbs) | 134.5 | 132.0 | 0.21 | 134.5 | 134.3 | 0.90 | 127.7 | 128.5 | 0.73 |
| Height (inches) | 61.1 | 61.0 | -- | 61.1 | 60.8 | -- | 60.9 | 60.7 | -- |
| Waist Circumference (inches) | 37.6 | 36.2 | 0.05 | 37.6 | 36.9 | 0.30 | 36.3 | 34.1 | 0.006 |
| Hip Circumference (inches) | 38.4 | 38.1 | 0.28 | 38.4 | 38.0 | 0.15 | 37.5 | 37.7 | 0.63 |
| Waist / Hip Circumference Ratio | 0.98 | 0.95 | 0.07 | 0.98 | 0.97 | 0.51 | 0.97 | 0.90 | <0.001 |
| Body Mass Index (kg/m^2) | 25.3 | 24.9 | 0.31 | 25.3 | 25.5 | 0.70 | 24.2 | 24.6 | 0.45 |
Established questionnaires were used to assess self-reported outcome measures. The questionnaires were intended to identify changes in exercise levels, QOL, depression, and mood associated with participation in the Hula Dance intervention trial (Table 2). Based on the Godin Exercise Questionnaire results, participants significantly increased the amount of moderate exercise engaged in (increase in minutes of this type of intensity of exercise) during the supervised Hula intervention and sustained this increase for more than one year post-intervention (p ≤ 0.001). The majority of the measures from the EORTC QLQ-C30 assessment tool did not indicate statistically significant changes in QOL for the study participants. However, we did observe a trend of increasing global health status, although it was not statistically significant. There was also a sustained reduction in dyspnea and diarrhea (p=0.02), as measured by the self-reported EORTC scale. The POMS-SF questionnaire used to determine changes in mood associated with the intervention, there was a highly significant increase in vigor/activity (p<0.001), indicating an improvement in the participants’ mood or a decrease in mood disturbances 55. Interestingly, this questionnaire detected a marginally significant increase in the level of confusion/bewilderment in the comparison between baseline versus month-24.
Table 2.
Intra-individual changes in physical activity and psychosocial measures between baseline and post-intervention time points
| Physical Activity and Psychosocial Measures | mean measures (n=8) | baseline vs. month 6 | mean measures (n=8) | baseline vs. month 12 | mean measures (n=8) | baseline vs. month 24 | |||
|---|---|---|---|---|---|---|---|---|---|
| baseline | month 6 | p-value | baseline | month 12 | p-value | baseline | month 24 | p-value | |
| strenuous exercise (times per week) | 0.2 | 0.0 | 0.80 | 0.2 | 1.3 | 0.16 | 0.0 | 0.1 | 0.83 |
| moderate exercise (times per week) | 0.7 | 3.6 | <0.001 | 0.7 | 2.9 | 0.002 | 0.4 | 2.9 | <0.001 |
| mild exercise (times per week) | 4.6 | 3.3 | 0.18 | 4.6 | 3.1 | 0.10 | 4.8 | 2.7 | 0.01 |
| Godin Leisure-Time Exercise Questionnaire: Total Leisure Activity Score | 14.9 | 23.4 | 0.28 | 14.9 | 31.3 | 0.05 | 12.7 | 23.7 | 0.16 |
| EORTC QLQ-30 (v3): Global Health Status / QoL | 66.7 | 74.0 | 0.15 | 66.7 | 72.9 | 0.21 | 66.7 | 73.8 | 0.39 |
| EORTC QLQ-30 (v3): Physical Functioning | 86.7 | 87.9 | 0.73 | 86.7 | 85.8 | 0.82 | 85.7 | 83.8 | 0.56 |
| EORTC QLQ-30 (v3): Role Functioning | 85.4 | 83.3 | 0.75 | 85.4 | 87.5 | 0.75 | 83.3 | 88.1 | 0.48 |
| EORTC QLQ-30 (v3): Emotional Functioning | 78.1 | 84.4 | 0.08 | 78.1 | 82.3 | 0.23 | 76.2 | 78.6 | 0.50 |
| EORTC QLQ-30 (v3): Cognitive Functioning | 85.4 | 85.4 | 1.00 | 85.4 | 81.3 | 0.21 | 83.3 | 78.6 | 0.23 |
| EORTC QLQ-30 (v3): Social Functioning | 85.4 | 91.7 | 0.13 | 85.4 | 89.6 | 0.30 | 83.3 | 92.9 | 0.08 |
| EORTC QLQ-30 (v3): Fatigue | 22.2 | 20.8 | 0.79 | 22.2 | 25.0 | 0.60 | 22.2 | 25.4 | 0.55 |
| EORTC QLQ-30 (v3): Nausea and Vomiting | 2.1 | 0.0 | 0.37 | 2.1 | 2.1 | 1.00 | 2.4 | 0.0 | 0.29 |
| EORTC QLQ-30 (v3): Pain | 18.8 | 14.6 | 0.57 | 18.8 | 18.8 | 1.00 | 21.4 | 21.4 | 1.00 |
| EORTC QLQ-30 (v3): Dyspnoea | 12.5 | 4.2 | 0.27 | 12.5 | 4.2 | 0.27 | 14.3 | 0.0 | 0.07 |
| EORTC QLQ-30 (v3): Insomnia | 20.8 | 16.7 | 0.46 | 20.8 | 25.0 | 0.46 | 23.8 | 19.0 | 0.59 |
| EORTC QLQ-30 (v3): Appetite Loss | 4.2 | 0.0 | 0.21 | 4.2 | 0.0 | 0.21 | 4.8 | 0.0 | 0.14 |
| EORTC QLQ-30 (v3): Constipation | 16.7 | 8.3 | 0.15 | 16.7 | 12.5 | 0.46 | 14.3 | 4.8 | 0.16 |
| EORTC QLQ-30 (v3): Diarrhea | 16.7 | 12.5 | 0.52 | 16.7 | 0.0 | 0.02 | 19.0 | 9.5 | 0.28 |
| EORTC QLQ-30 (v3): Financial Difficulties | 20.8 | 16.7 | 0.58 | 20.8 | 12.5 | 0.27 | 23.8 | 14.3 | 0.23 |
| Center for Epidemiological Studies Depression (CESD): Total Score | 10.9 | 7.5 | 0.17 | 10.9 | 8.3 | 0.28 | 11.6 | 8.1 | 0.16 |
| Brief Fatigue Inventory: Index | 1.8 | 1.7 | 0.88 | 1.8 | 2.4 | 0.32 | 2.1 | 1.9 | 0.79 |
| POMS-SF: Tension/Anxiety | 2.0 | 2.9 | 0.27 | 2.0 | 2.5 | 0.52 | 2.1 | 5.1 | 0.09 |
| POMS-SF: Depression/Dejection | 2.0 | 2.3 | 0.78 | 2.0 | 1.8 | 0.84 | 2.3 | 5.3 | 0.08 |
| POMS-SF: Anger/Hostility | 1.5 | 2.9 | 0.20 | 1.5 | 2.4 | 0.42 | 1.3 | 5.1 | 0.11 |
| POMS-SF: Fatigue | 4.0 | 4.5 | 0.68 | 4.0 | 4.4 | 0.77 | 4.6 | 6.7 | 0.25 |
| POMS-SF: Confusion/Bewilderment | 1.8 | 2.9 | 0.09 | 1.8 | 2.8 | 0.12 | 2.0 | 4.3 | 0.05 |
| POMS-SF: Vigor/Activity | 10.5 | 14.1 | <0.001 | 10.5 | 13.0 | 0.008 | 10.6 | 14.9 | <0.001 |
| POMS-SF: Total Mood Disturbance | 0.7 | 1.4 | 0.88 | 0.7 | 0.8 | 0.99 | 1.7 | 11.7 | 0.23 |
| SCS: Most Important Person | 1.7 | 1.7 | 0.88 | 1.7 | 1.7 | 0.92 | 1.8 | 1.5 | 0.31 |
| SCS: Other People | 1.8 | 1.8 | 0.86 | 1.8 | 1.8 | 0.69 | 1.8 | 1.6 | 0.23 |
We also observed significant changes in the levels of circulating biomarkers associated with the Hula Dance intervention when we compared levels at baseline versus month- 6 and 12 (Table 3). Assays were not performed on the month-24 plasma samples, so there are no circulating biomarker data for this time point. A decrease in circulating IGFBP-3 levels was the only significant change observed for the baseline to month-6 comparison, and levels of IGFBP-3 were further reduced at the month-12 time point. There were multiple biomarkers with significant changes for the baseline versus month-12 comparison. In addition to IGFBP-3, we observed a reduction in the levels of IGF-1 as well as multiple inflammatory cytokines (IL-1B, IL-2, IL-4, IL-5, IL-6, IL-8, IL-10, GM-CSF, IFN-Ɣ, and TNF-α). These results support the observation that physiologic changes, as measured by changes in circulating IGF-1 and its binding protein, IGFBP-3, and biomarkers of inflammation, were associated with increased physical activity through participation in this cultural dance program.
Table 3.
Intra-individual changes in circulating biomarker levels between baseline and post-intervention time points
| Circulating Biomarker Levels* | mean measures (n=8) | baseline vs. month 6 | mean measures (n=8) | baseline vs. month 12 | ||
|---|---|---|---|---|---|---|
| baseline | month 6 | p-value* | baseline | month 12 | p-value* | |
| Adiponectin (ug/mL) | 8.7 | 9.9 | 0.09 | 8.7 | 9.6 | 0.19 |
| Cortisol (ng/mL) | 94.4 | 88.9 | 0.65 | 94.4 | 88.6 | 0.63 |
| IGF-1 (ng/mL) | 82.6 | 82.4 | 0.95 | 82.6 | 74.9 | 0.03 |
| IGFBP-3 (ug/mL) | 2.5 | 2.2 | 0.03 | 2.5 | 2.0 | 0.005 |
| Insulin (uU/mL) | 5.4 | 4.6 | 0.39 | 5.4 | 4.8 | 0.50 |
| Leptin (ng/mL) | 18.1 | 17.2 | 0.83 | 18.1 | 17.5 | 0.88 |
| Glucose (mg/dL) | 129.9 | 133.2 | 0.89 | 129.9 | 106.7 | 0.33 |
| CRP (mg/L) | 1.2 | 0.8 | 0.33 | 1.2 | 0.9 | 0.46 |
| IL-1B (pg/mL) | 26.3 | 28.0 | 0.46 | 26.3 | 20.8 | 0.02 |
| IL-2 (pg/mL) | 38.7 | 38.4 | 0.92 | 38.7 | 28.7 | 0.01 |
| IL-4 (pg/mL) | 33.6 | 36.5 | 0.37 | 33.6 | 26.5 | 0.03 |
| IL-5 (pg/mL) | 26.8 | 27.0 | 0.94 | 26.8 | 20.9 | 0.02 |
| IL-6 (pg/mL) | 58.2 | 60.8 | 0.93 | 58.2 | 77.1 | 0.54 |
| IL-8 (pg/mL) | 111.5 | 132.2 | 0.09 | 111.5 | 93.3 | 0.14 |
| IL-10 (pg/mL) | 57.6 | 58.4 | 0.90 | 57.6 | 40.7 | 0.03 |
| GM-CSF (pg/mL) | 32.7 | 35.4 | 0.39 | 32.7 | 26.1 | 0.05 |
| IFN-γ (pg/mL) | 44.0 | 49.3 | 0.15 | 44.0 | 36.3 | 0.05 |
| TNF-α (pg/mL) | 29.6 | 30.2 | 0.81 | 29.6 | 22.3 | 0.02 |
adjusted for BMI
Discussion
It is established that formalized exercise interventions to increase physical activity have been implemented with overall positive efficacy for breast cancer survivors. However, cancer survivors of minority populations were observed to be less likely to meet physical activity recommendations, more likely to be obese, and generally had poorer health-related QOF 12, 58–61. The poor breast cancer outcomes for some minority groups may be related to the lack of adherence to physical activity and weight control recommendations, highlighting a need for physical activity intervention strategies to increase interest and adherence for women of minority populations who are generally not meeting recommendations. Hawaii is one of the most racial and ethnically diverse places in the world, according to the U.S. Census Bureau, with approximately 75% of the population comprised of minorities. The racial/ethnic composition of our study participants reflected the high percentage of minorities in the population. In addition, breast cancer incidence is relatively high in Hawaii, ranking 6th in the nation (2018; statecancerprofiles.cancer.gov). Therefore, there was great motivation to initiate a study to increase physical activity through a modality that is culturally sensitive for a population with high breast cancer incidence.
Prior studies have demonstrated that increasing physical activity with a dance program has multiple benefits such as good adherence to physical activity, and improved QOL, vigor, and physical function 46, 62. Our pilot trial to examine the psychosocial and biological effects of increasing physical activity using a supervised six-month cultural dance intervention demonstrated that this approach has the potential to increase and sustain moderate physical activity for previously sedentary breast cancer survivors. The intra-individual levels of moderate physical activity increased significantly during the six-month intervention and were sustained for more than one year after the completion of the intervention. In addition, we observed multidimensional effects (e.g. anthropometric, circulating biomarker levels, physical functioning, and psychosocial) associated with the completion of the trial. To our knowledge, this is the first intervention study utilizing Hula Dance to increase physical activity and improve QOL for breast cancer survivors.
This pilot intervention trial demonstrated that a cultural dance program could be implemented to sustain moderate physical activity for the intervention period and even post-intervention. We were particularly encouraged because 7 of the 11 participants that started the trial continued to practice their Hula Dance well past (>1 year) the completion of the intervention portion of the trial. Maintaining healthy behavior changes is challenging, especially when there are many competing demands following diagnosis and treatment for cancer survivors. To facilitate sustaining the participants’ increased physical activity through Hula Dance, the Hula classes continued to be available to the participants following the intervention portion of the trial. Our study demonstrated that sedentary breast cancer survivors can increase their levels of physical activity and maintain a lifestyle change to include moderate-intensity physical activity. Additional studies with larger sample sizes will be important to confirm the efficacy in these findings.
While there are numerous effective physical activity interventions, long-term maintenance and follow-up is rarely conducted and assessed for many studies. For example, a report evaluating the maintenance of intervention outcomes, found that only 16% (10 of 63 trials) of physical activity and/or dietary interventions trials for breast cancer survivors did a post-intervention assessment (≥ 3 months) 63. Of the 10 trials, only four (40%) observed maintenance of the intervention outcomes. These results support the importance of post-intervention study follow-ups and a better understanding of the factors that contribute to a sustainable physical activity modality.
The self-report assessments indicated a significant increase in vigor during the intervention and post-intervention. This would be expected, as previous studies have demonstrated exercise and group support have been related to increased vigor 64–68. The Hula Dance intervention was conducted in a group-based setting, likely fostering social support among the participants. However, the increase in bewilderment and confusion for the baseline to months- 6, 12, and 24 time point comparisons was unexpected. It is possible that it reflects a change in the participants’ perception of cognitive functioning since the task of learning and memorizing the Hula Dance steps for each song may have been challenging. Because of the small sample size, we are limited in our interpretation and assessment of the impact of these differences.
Obesity is a risk factor of breast cancer 5, 69. Increased circulating levels of insulin and IGF-axis proteins are strongly associated with obesity and breast cancer 70–72. Insulin and IGFs are growth factors that can promote proliferation in mammary cells, potentially initiating breast cancer development and recurrence. Levels of biologically active IGFs are regulated by IGF-binding proteins; IGFBP-3 is the binding protein that regulates the bioavailability of IGF-1. Previous studies have examined the association between increasing physical activity and a reduction in circulating IGF-1 and IGFBP-3 levels, but the results were mixed. Irwin et al. found a significant decrease in insulin, IGF-1, and IGFBP-3 levels for postmenopausal breast cancer survivors participating in a six-month, moderate-intensity aerobic exercise intervention trial 14 However, McTieman et al. observed a marginal, non-significant decrease in IGF-1 and IGFBP-3 levels in a 12-month moderate-intensity exercise trial 73. A 12-week physical activity intervention with moderate intensity Tai Chi Chuan for breast cancer survivors did not result in a reduction of IGF-1 or IGFBP-3 45. In our study, we observed a statistically significant decrease in IGF-1 and IGFBP-3 levels associated with the Hula Dance program. Interestingly, IGF-1 levels demonstrated a decreasing trend from baseline to months- 6 and 12, with the most marked decrease by month-12. It is possible that sustained physical activity (≥6 months) is important for a significant decrease in IGF-1 levels. There was also a decreasing trend in IGFBP-3 levels, with the most significant change in month-12. Moreover, IGFBP-3 levels have been shown to be positively related to central adiposity 74; although there was not a significant reduction in weight for our study participants, we did observe a significant reduction in waist circumference and WHR. These results suggest that increasing moderate physical activity with the Hula Dance intervention resulted in a reduction in central adiposity and a concomitant decrease in circulating IGFBP-3 levels.
Inflammation plays a role in the development and progression of cancer 75. Elevated circulating levels of inflammatory cytokines (e.g. CRP, TNF-α, IL-6) have been observed in breast cancer patients 76, 77, and physical activity has been shown to modulate these levels 45, 78–80. However, results across studies have been inconsistent. Some studies have indicated significant changes in CRP, or TNF-α, IL-6 levels associated with exercise, and others have found no significant changes in these levels. Interestingly, CRP and IL-6 were two cytokines that did not significantly decrease with our physical activity intervention. In fact, IL-6, although not significant, demonstrated an increasing trend in levels between baseline and months-6 and 12. Janelsins et al. also observed an increase in IL-6 levels associated with their Tai Chi Chuan intervention 45. In our study, we observed a significant decrease in the circulating levels of multiple inflammatory cytokines at month-12 (IGF-1, IGFBP3, IL-1B, IL-2, IL-4, IL-5, IL-10, GM-CSF, IFN-Ɣ, and TNF-α). The majority of these cytokines were not significantly different at month-6, which is the time point at the completion of the intervention. It is possible that sustained physical activity (≥6 months) is important in significantly decreasing the levels of these inflammatory biomarkers. However, Schmidt et al. observed a decrease in the levels of inflammatory cytokines (IL-2, IL-4, IL-5, IL-10, IL-12, IL-13, GM-CSF, IFN-Ɣ and TNF-α) associated with increased physical activity (walking) for one week and the effects were more pronounced in obese participants 49.
Although this was a small pilot study and there are limitations in the conclusions that can be made from it, the study demonstrates the feasibility to increase physical activity with a cultural dance program. A larger wait-list controlled study should be implemented to confirm our findings, that the increased physical activity through the Hula Dance intervention can result in an improvement in the QOL, a reduction in waist circumference, as well as changes in the levels of circulating biomarkers associated with the IGF-axis and inflammation. Self-efficacy is important to continued maintenance of physical activity 81. Therefore, fostering dissemination of culturally relevant physical activity interventions is critically important, especially for minority populations that are generally not meeting the physical activity recommendations. In addition, sustainability of the increased physical activity is important for long-term impact of these types of interventions.
Highlights:
Physical activity can reduce risk of cancer recurrence, improve quality of life, lower body mass index, reduce inflammation, and alter levels of circulating biomarkers associated with obesity.
We demonstrate the feasibility of a cultural dance program to increase and sustain physical activity in previously sedentary breast cancer survivors.
We observed a significant reduction in waist circumference, changes in levels of circulating biomarkers of obesity and inflammation, and an increase in vigor/activity based on self-reported measures through questionnaires.
Acknowledgements.
The authors would like to thank all of the study participants for their participation in this trial. We would like to acknowledge support from the UHCC Analytical Biochemistry Shared Resource and Clinical Trials Office. The work was supported by pilot funding under the National Cancer Institute’s (NCI) award P30CA071789.
Funding
The work was supported by pilot funding under the National Cancer Institute’s (NCI) award P30CA071789.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of Interest
L. Loo declares that she has no conflicts of interest. K. Nishibun declares that she has no conflicts of interest. L. Welsh declares that she has no conflicts of interest. T. Makolo declares that she has no conflicts of interest. C. Chong declares that she has no conflicts of interest. I Pagano declares that she has no conflicts of interest. H. Yu declares that she has no conflicts of interest. E. Bantum declares that she has no conflicts of interest.
Ethical Approval
This article does not contain any studies with animals performed by any of the authors.
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individuals included in the study.
References:
- 1.McNeely ML, Campbell KL, Rowe BH, Klassen TP, Mackey JR, Courneya KS. Effects of exercise on breast cancer patients and survivors: a systematic review and meta-analysis. CMAJ. 2006;175(1): 34–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sternfeld B, Lee IM. Physical activity and cancer: the evidence, the issues and the challenges. New York: Oxford University Press; 2008. [Google Scholar]
- 3.Bianchini F, Kaaks R, Vainio H. Overweight, obesity, and cancer risk. Lancet Oncol. 2002;3(9): 565–574. [DOI] [PubMed] [Google Scholar]
- 4.Bianchini F, Kaaks R, Vainio H. Weight control and physical activity in cancer prevention. Obes Rev. 2002;3(1): 5–8. [DOI] [PubMed] [Google Scholar]
- 5.Ballard-Barbash R, Friedenreich CM, Courneya KS, Siddiqi SM, McTiernan A, Alfano CM. Physical activity, biomarkers, and disease outcomes in cancer survivors: a systematic review. J Natl Cancer Inst. 2012;104(11): 815–840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Holmes MD, Chen WY, Feskanich D, Kroenke CH, Colditz GA. Physical activity and survival after breast cancer diagnosis. JAMA. 2005;293(20): 2479–2486. [DOI] [PubMed] [Google Scholar]
- 7.Irwin ML, Smith AW, McTiernan A, et al. Influence of pre- and postdiagnosis physical activity on mortality in breast cancer survivors: the health, eating, activity, and lifestyle study. J Clin Oncol. 2008;26(24): 3958–3964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Irwin ML, McTiernan A, Manson JE, et al. Physical activity and survival in postmenopausal women with breast cancer: results from the women’s health initiative. Cancer Prev Res (Phila). 2011;4(4): 522–529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ibrahim EM, Al-Homaidh A. Physical activity and survival after breast cancer diagnosis: meta-analysis of published studies. Med Oncol. 2011. ;28(3): 753–765. [DOI] [PubMed] [Google Scholar]
- 10.Kushi LH, Doyle C, McCullough M, et al. American Cancer Society Guidelines on nutrition and physical activity for cancer prevention: reducing the risk of cancer with healthy food choices and physical activity. CA Cancer J Clin. 2012;62(1): 30–67. [DOI] [PubMed] [Google Scholar]
- 11.Rock CL, Doyle C, Demark-Wahnefried W, et al. Nutrition and physical activity guidelines for cancer survivors. CA Cancer J Clin. 2012;62(4): 243–274. [DOI] [PubMed] [Google Scholar]
- 12.Hair BY, Hayes S, Tse CK, Bell MB, Olshan AF. Racial differences in physical activity among breast cancer survivors: implications for breast cancer care. Cancer. 2014;120(14): 2174–2182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cadmus LA, Salovey P, Yu H, Chung G, Kasl S, Irwin ML. Exercise and quality of life during and after treatment for breast cancer: results of two randomized controlled trials. Psycho-oncology. 2009; 18(4): 343–352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Irwin ML, Varma K, Alvarez-Reeves M, et al. Randomized controlled trial of aerobic exercise on insulin and insulin-like growth factors in breast cancer survivors: the Yale Exercise and Survivorship study. Cancer Epidemiol Biomarkers Prev. 2009; 18(1): 306–313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kahn BB, Flier JS. Obesity and insulin resistance. J Clin Invest. 2000;106(4): 473–481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rose DP, Komninou D, Stephenson GD. Obesity, adipocytokines, and insulin resistance in breast cancer. Obes Rev. 2004;5(3): 153–165. [DOI] [PubMed] [Google Scholar]
- 17.Courneya KS, Mackey JR, Bell GJ, Jones LW, Field CJ, Fairey AS. Randomized controlled trial of exercise training in postmenopausal breast cancer survivors: cardiopulmonary and quality of life outcomes. J Clin Oncol. 2003;21(9): 1660–1668. [DOI] [PubMed] [Google Scholar]
- 18.Craft LL, Vaniterson EH, Helenowski IB, Rademaker AW, Courneya KS. Exercise effects on depressive symptoms in cancer survivors: a systematic review and meta-analysis. Cancer Epidemiol Biomarkers Prev. 2012;21(1): 3–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cramp F, Byron-Daniel J. Exercise for the management of cancer-related fatigue in adults. Cochrane Database Syst Rev. 2012;11: CD006145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Demark-Wahnefried W, Morey MC, Sloane R, et al. Reach out to enhance wellness home-based diet-exercise intervention promotes reproducible and sustainable long-term improvements in health behaviors, body weight, and physical functioning in older, overweight/obese cancer survivors. J Clin Oncol. 2012;30(19): 2354–2361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Demark-Wahnefried W, Platz EA, Ligibel JA, et al. The role of obesity in cancer survival and recurrence. Cancer Epidemiol Biomarkers Prev. 2012;21(8): 1244–1259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ligibel JA, Campbell N, Partridge A, et al. Impact of a mixed strength and endurance exercise intervention on insulin levels in breast cancer survivors. J Clin Oncol. 2008;26(6): 907–912. [DOI] [PubMed] [Google Scholar]
- 23.Payne JK, Held J, Thorpe J, Shaw H. Effect of exercise on biomarkers, fatigue, sleep disturbances, and depressive symptoms in older women with breast cancer receiving hormonal therapy. Oncology nursing forum. 2008;35(4): 635–642. [DOI] [PubMed] [Google Scholar]
- 24.Marinac CR, Godbole S, Kerr J, Natarajan L, Patterson RE, Hartman SJ. Objectively measured physical activity and cognitive functioning in breast cancer survivors. J Cancer Surviv. 2015;9(2): 230–238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Behrman S, Ebmeier KP. Can exercise prevent cognitive decline? Practitioner. 2014;258(1767): 17–21, 12–13. [PubMed] [Google Scholar]
- 26.Miller DI, Taler V, Davidson PS, Messier C. Measuring the impact of exercise on cognitive aging: methodological issues. Neurobiol Aging. 2012;33(3): 622 e629–643. [DOI] [PubMed] [Google Scholar]
- 27.Coubard OA, Duretz S, Lefebvre V, Lapalus P, Ferrufino L. Practice of contemporary dance improves cognitive flexibility in aging. Front Aging Neurosci. 2011;3: 13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kattenstroth JC, Kolankowska I, Kalisch T, Dinse HR. Superior sensory, motor, and cognitive performance in elderly individuals with multi-year dancing activities. Front Aging Neurosci. 2010;2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Crespi E, Bottai G, Santarpia L. Role of inflammation in obesity-related breast cancer. Curr Opin Pharmacol. 2016;31: 114–122. [DOI] [PubMed] [Google Scholar]
- 30.Crusz SM, Balkwill FR. Inflammation and cancer: advances and new agents. Nat Rev Clin Oncol. 2015; 12( 10): 584–596. [DOI] [PubMed] [Google Scholar]
- 31.Trompet S, de Craen AJ, Mooijaart S, et al. High Innate Production Capacity of Proinflammatory Cytokines Increases Risk for Death from Cancer: Results of the PROSPER Study. Clin Cancer Res. 2009;15(24): 7744–7748. [DOI] [PubMed] [Google Scholar]
- 32.Brown KA, Simpson ER. Obesity and breast cancer: progress to understanding the relationship. Cancer Res. 2010;70(1): 4–7. [DOI] [PubMed] [Google Scholar]
- 33.Calle EE, Rodriguez C, Walker-Thurmond K, Thun MJ. Overweight, obesity, and mortality from cancer in a prospectively studied cohort of U.S. adults. N Engl J Med. 2003;348(17): 1625–1638. [DOI] [PubMed] [Google Scholar]
- 34.Carmichael AR. Obesity and prognosis of breast cancer. Obes Rev. 2006;7(4): 333–340. [DOI] [PubMed] [Google Scholar]
- 35.Walter M, Liang S, Ghosh S, Hornsby PJ, Li R. Interleukin 6 secreted from adipose stromal cells promotes migration and invasion of breast cancer cells. Oncogene. 2009;28(30): 2745–2755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.McTiernan A, Tworoger SS, Rajan KB, et al. Effect of exercise on serum androgens in postmenopausal women: a 12-month randomized clinical trial. Cancer Epidemiol Biomarkers Prev. 2004;13(7): 1099–1105. [PubMed] [Google Scholar]
- 37.McTiernan A, Tworoger SS, Ulrich CM, et al. Effect of exercise on serum estrogens in postmenopausal women: a 12-month randomized clinical trial. Cancer Res. 2004;64(8): 2923–2928. [DOI] [PubMed] [Google Scholar]
- 38.Allin KH, Nordestgaard BG, Flyger H, Bojesen SE. Elevated pre-treatment levels of plasma C-reactive protein are associated with poor prognosis after breast cancer: a cohort study. Breast Cancer Res. 2011;13(3): R55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Duggan C, Irwin ML, Xiao L, et al. Associations of insulin resistance and adiponectin with mortality in women with breast cancer. J Clin Oncol. 2011;29(1): 32–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.McTiernan A Mechanisms linking physical activity with cancer. Nat Rev Cancer. 2008;8(3): 205–211. [DOI] [PubMed] [Google Scholar]
- 41.Ropelle ER, Flores MB, Cintra DE, et al. IL-6 and IL-10 anti-inflammatory activity links exercise to hypothalamic insulin and leptin sensitivity through IKKbeta and ER stress inhibition. PLoS Biol. 2010;8(8). [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 42.Bower JE, Greendale G, Crosswell AD, et al. Yoga reduces inflammatory signaling in fatigued breast cancer survivors: a randomized controlled trial. Psychoneuroendocrinology. 2014;43: 20–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Campo RA, Light KC, O’Connor K, et al. Blood pressure, salivary cortisol, and inflammatory cytokine outcomes in senior female cancer survivors enrolled in a tai chi chih randomized controlled trial. J Cancer Surviv. 2015;9(1): 115–125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Derry HM, Jaremka LM, Bennett JM, et al. Yoga and self-reported cognitive problems in breast cancer survivors: a randomized controlled trial. Psycho-oncology. 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Janelsins MC, Davis PG, Wideman L, et al. Effects of Tai Chi Chuan on insulin and cytokine levels in a randomized controlled pilot study on breast cancer survivors. Clin Breast Cancer. 2011;11(3): 161–170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Kaltsatou A, Mameletzi D, Douka S. Physical and psychological benefits of a 24-week traditional dance program in breast cancer survivors. J Bodyw Mov Ther. 2011; 15(2): 162–167. [DOI] [PubMed] [Google Scholar]
- 47.Larkey L, Huberty J, Pedersen M, Weihs K. Qigong/Tai Chi Easy for fatigue in breast cancer survivors: Rationale and design of a randomized clinical trial. Contemp Clin Trials. 2016;50: 222–228. [DOI] [PubMed] [Google Scholar]
- 48.Sprod LK, Janelsins MC, Palesh OG, et al. Health-related quality of life and biomarkers in breast cancer survivors participating in tai chi chuan. J Cancer Surviv. 2012;6(2): 146–154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Schmidt FM, Weschenfelder J, Sander C, et al. Inflammatory cytokines in general and central obesity and modulating effects of physical activity. PLoS One. 2015; 10(3): e0121971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Services USDoHaH. Physical Activity Guidelines for Americans. Washington, D.C.; 2008. [Google Scholar]
- 51.Godin G, Shephard RJ. A simple method to assess exercise behavior in the community. Can J Appl Sport Sci. 1985;10(3): 141–146. [PubMed] [Google Scholar]
- 52.Aaronson NK, Ahmedzai S, Bergman B, et al. The European Organization for Research and Treatment of Cancer QLQ-C30: a quality-of-life instrument for use in international clinical trials in oncology. J Natl Cancer Inst. 1993;85(5): 365–376. [DOI] [PubMed] [Google Scholar]
- 53.Mendoza TR, Wang XS, Cleeland CS, et al. The rapid assessment of fatigue severity in cancer patients: use of the Brief Fatigue Inventory. Cancer. 1999;85(5): 1186–1196. [DOI] [PubMed] [Google Scholar]
- 54.Radloff LS. The CES-D Scale: A self-report depression scale for research in the general population. Applied Psychological Measurement. 1977; 1(3): 285–401. [Google Scholar]
- 55.McNair DM, Lorr M, Droppleman LF. Manual for the Profile of Mood States. San Diego, CA: Educational and Industrial Testing Service; 1971. [Google Scholar]
- 56.Lepore SJ, Silver RC, Wortman CB, Wayment HA. Social constraints, intrusive thoughts, and depressive symptoms among bereaved mothers. J Pers Soc Psychol. 1996;70(2): 271–282. [DOI] [PubMed] [Google Scholar]
- 57.Singer JD, Willett JB. Applied Longitudinal Data Analysis: Modeling Change and Event Occurrence: Oxford University Press; 2003. [Google Scholar]
- 58.Spector D, Battaglini C, Groff D. Perceived exercise barriers and facilitators among ethnically diverse breast cancer survivors. Oncology nursing forum. 2013;40(5): 472–480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Spector D Few people living with and beyond cancer meet current exercise recommendations. Evid Based Nurs. 2014;17(4): 116. [DOI] [PubMed] [Google Scholar]
- 60.Paxton RJ, Phillips KL, Jones LA, et al. Associations among physical activity, body mass index, and health-related quality of life by race/ethnicity in a diverse sample of breast cancer survivors. Cancer. 2012;118(16): 4024–4031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Smith AW, Alfano CM, Reeve BB, et al. Race/ethnicity, physical activity, and quality of life in breast cancer survivors. Cancer Epidemiol Biomarkers Prev. 2009;18(2): 656–663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Bradt J, Shim M, Goodill SW. Dance/movement therapy for improving psychological and physical outcomes in cancer patients. Cochrane Database Syst Rev. 2015;1: CD007103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Spark LC, Reeves MM, Fjeldsoe BS, Eakin EG. Physical activity and/or dietary interventions in breast cancer survivors: a systematic review of the maintenance of outcomes. J Cancer Surviv. 2013;7(1): 74–82. [DOI] [PubMed] [Google Scholar]
- 64.Crush EA, Frith E, Loprinzi PD. Experimental effects of acute exercise duration and exercise recovery on mood state. J Affect Disord. 2018;229: 282–287. [DOI] [PubMed] [Google Scholar]
- 65.Halpern J, Cohen M, Kennedy G, Reece J, Cahan C, Baharav A. Yoga for improving sleep quality and quality of life for older adults. Altern Ther Health Med. 2014;20(3): 37–46. [PubMed] [Google Scholar]
- 66.Hsu CY, Moyle W, Cooke M, Jones C. Seated T’ai Chi in Older Taiwanese People Using Wheelchairs: A Randomized Controlled Trial Investigating Mood States and Self-Efficacy. J Altern Complement Med. 2016;22(12): 990–996. [DOI] [PubMed] [Google Scholar]
- 67.Osei-Tutu KB, Campagna PD. The effects of short- vs. long-bout exercise on mood, VO2max, and percent body fat. Prev Med. 2005;40(1): 92–98. [DOI] [PubMed] [Google Scholar]
- 68.Papastergiou D, Kokaridas D, Bonotis K, Diggelidis N, Patsiaouras A. Exercise, supportive group therapy, and mood profile of Greek cancer patients: intervention effect and related comparisons. Support Care Cancer. 2018;26(10): 3571–3578. [DOI] [PubMed] [Google Scholar]
- 69.Iyengar NM, Hudis CA, Dannenberg AJ. Obesity and inflammation: new insights into breast cancer development and progression. Am Soc Clin Oncol Educ Book. 2013: 46–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Bowers LW, Rossi EL, O’Flanagan CH, deGraffenried LA, Hursting SD. The Role of the Insulin/IGF System in Cancer: Lessons Learned from Clinical Trials and the Energy Balance-Cancer Link. Front Endocrinol (Lausanne). 2015;6: 77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Christopoulos PF, Msaouel P, Koutsilieris M. The role of the insulin-like growth factor-1 system in breast cancer. Mol Cancer. 2015;14: 43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.O’Flanagan CH, Bowers LW, Hursting SD. A weighty problem: metabolic perturbations and the obesity-cancer link. Horm Mol Biol Clin Investig. 2015;23(2): 47–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.McTiernan A, Sorensen B, Yasui Y, et al. No effect of exercise on insulin-like growth factor 1 and insulin-like growth factor binding protein 3 in postmenopausal women: a 12-month randomized clinical trial. Cancer Epidemiol Biomarkers Prev. 2005;14(4): 1020–1021. [DOI] [PubMed] [Google Scholar]
- 74.Gram IT, Norat T, Rinaldi S, et al. Body mass index, waist circumference and waist-hip ratio and serum levels of IGF-I and IGFBP-3 in European women. Int J Obes (Lond). 2006;30(11): 1623–1631. [DOI] [PubMed] [Google Scholar]
- 75.Grivennikov SI, Greten FR, Karin M. Immunity, inflammation, and cancer. Cell. 2010;140(6): 883–899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Heikkila K, Ebrahim S, Lawlor DA. A systematic review of the association between circulating concentrations of C reactive protein and cancer. J Epidemiol Community Health. 2007;61(9): 824–833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Pierce BL, Ballard-Barbash R, Bernstein L, et al. Elevated biomarkers of inflammation are associated with reduced survival among breast cancer patients. J Clin Oncol. 2009;27(21): 3437–3444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Fairey AS, Courneya KS, Field CJ, et al. Effect of exercise training on C-reactive protein in postmenopausal breast cancer survivors: a randomized controlled trial. Brain Behav Immun. 2005;19(5): 381–388. [DOI] [PubMed] [Google Scholar]
- 79.Friedenreich CM. Physical activity and breast cancer: review of the epidemiologic evidence and biologic mechanisms. Recent Results Cancer Res. 2011;188: 125–139. [DOI] [PubMed] [Google Scholar]
- 80.Gomez AM, Martinez C, Fiuza-Luces C, et al. Exercise training and cytokines in breast cancer survivors. Int J Sports Med. 2011;32(6): 461–467. [DOI] [PubMed] [Google Scholar]
- 81.Mosher CE, Lipkus I, Sloane R, Snyder DC, Lobach DF, Demark-Wahnefried W. Long-term outcomes of the FRESH START trial: exploring the role of self-efficacy in cancer survivors’ maintenance of dietary practices and physical activity. Psycho-oncology. 2013;22(4): 876–885. [DOI] [PMC free article] [PubMed] [Google Scholar]