Abstract
Objective:
Frey syndrome is a complication followed by parotidectomy which caused gustatory sweating and facial flush. There were several methods for the prevention of Frey syndrome, but most of them had no obvious effects. In this study, we compare the intra-auricular modification of facelift incision with the traditional lazy-S incision to see if it can decrease the risk of Frey syndrome.
Materials and Methods:
This is a retrospective study. From 2003 to 2009, a total of 61 patients with benign parotid tumor who received parotidectomy at Hualien Tzu Chi Hospital and were followed at outpatient department for at least 5 years were enrolled. Patients were divided into two groups according to the type of incisions during operation: (1) Group M: intra-auricular modification of facelift incision or (2) Group S: traditional lazy-S incision. All patients received the partial thickness sternocleidomastoid muscle flap. Clinical data including age, gender, pathologic result, presentation of Frey syndrome, size of tumor, length of operation, blood loss from surgery, length of placement of drain, total amount of drainage, and length of stay were collected and analyzed.
Results:
Sixty-one patients were enrolled. Eighteen patients were in Group M and forty-three were in Group S. There was no significant difference of age, gender, and size of tumor between the two groups. The pathologic results included parotitis, pleomorphic adenoma, Warthin's tumor, and others. No significant difference of pathologic results, blood loss from surgery, length of placement of drain, total amount of drainage, and length of stay between two groups was obtained. The length of operation was longer in Group M (P = 0.001) and the incidence of Frey syndrome was lower in Group M than Group S (P < 0.05).
Conclusions:
The use of intra-auricular modification of facelift incision can decrease the incidence of Frey syndrome.
KEYWORDS: Frey syndrome, Intra-auricular modification of facelift incision, Lazy-S incision, Sternocleidomastoid muscle flap
INTRODUCTION
Frey syndrome is a common complication after parotidectomy. The incidence of symptomatic Frey syndrome is around 12%–43% [1,2,3,4,5]. This is due to the aberrant reinnervation of parasympathetic nerves from auriculotemporal nerve to the sweat glands and vessels of the subcutaneous tissue in the preauricular and facial area [6,7]. Symptoms include flushing, sweating, burning, neuralgia, and itching in the preauricular and facial area [8,9,10]. There were many methods to decrease the incidence of Frey syndrome: fascia lata grafts, free dermal-fat-fascia grafts, dermal-fat grafts, platysma muscle flaps, temporoparietal fascia flaps, sternocleidomastoid muscle (SCM) flaps, superficial musculoaponeurotic system (SMAS) flaps, but they showed no good effectiveness [5]. This study compares the incidence of Frey syndrome between two incisions: lazy-S incision with SCM flap or intra-auricular modification of facelift incision with SCM flap and discusses why the former is a better way to prevent Frey syndrome.
MATERIALS AND METHODS
Patients
The study was conducted in accordance with the Declaration of Helsinki and was approved by the local ethics committee of the institute (IRB107-112-B). Informed written consent was waived because the study was a retrospective data analysis.
Between January 2003 and March 2009, 61 consecutive patients underwent parotidectomy for benign parotid tumor at Buddhist Tzu Chi General Hospital; 18 patients underwent intra-auricular modification of facelift incision (Group M) and 43 patients underwent lazy-S incision (Group S). All patients were older than 20 year and were followed at least 5 years. All patients received the partial-thickness SCM flap. Clinical data including age, gender, pathologic result, presentation of Frey syndrome, size of tumor, length of operation, blood loss from surgery, length of placement of drain, total amount of drainage, and length of stay were collected and analyzed.
Surgical procedures
All patients were in supine position with general anesthesia via orotracheal tube. The surgical pad was placed under shoulder and the neck was in extension with 45° to the horizontal plane. The facial nerve monitor was used. The surgical procedure was summarized as follows: The intra-auricular modification of facelift incision is different from the traditional incision which the preauricular incision was started from the posterior margin of tragus then through the intertragal notch to the crease between ear lobule and face. The incision then extends upward to the same level as the most superior part of external auditory canal and was parallel to the posterior auricular sulcus with distance about 2 mm to the auricle. Then, the incision was turned to the postauricular hairline and extended inferiorly with few mini-meters posterior to the hairline. The extent of inferior extension is depended on the size and location of the tumor [Figure 1]. If the tumor was located at the superior parotid part, the incision might be made longer along the hairline. After elevating the preauricular skin flap, we then identify the tragal cartilage. Then, the following procedure is the same in both the Group M and Group S: keep as much the great auricular nerve as possible; use the anterograde dissection and facial nerve monitor to identify the facial nerve. After removal of tumor, the depression of tumor bed was covered with one rotational flap developed from the superior part of the partial thickness SCM with base at the mastoid process. This flap was sutured to the posterior border of masseter fascia. The drainage tube was placed before the wound sutured. The antibiotics were used for 3 days after operation. Patients discharged from hospital the next day after the drainage was removed.
Figure 1.
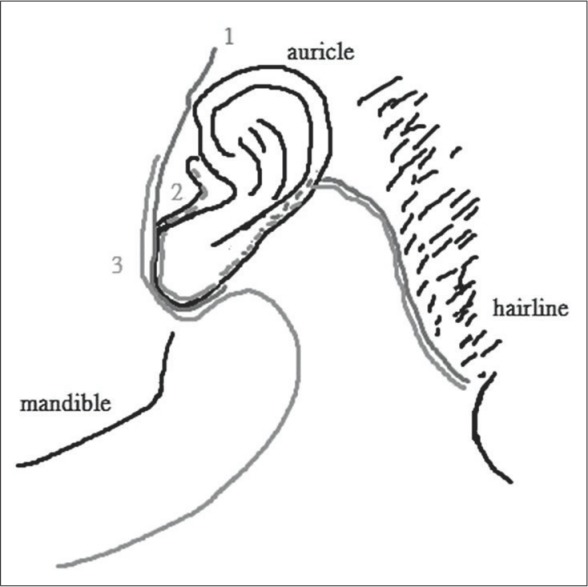
(1) for facelift incision, (2) for intra-auricular modification of facelift incision, and (3) for lazy-S incision
Evaluation of Frey syndrome
Each case was followed for at least 5 years and the charts were reviewed after operations to see if there are any records of Frey syndrome. Patient had either flushing or sweating while eating more than once a week was considered to have Frey syndrome.
Statistical analysis
The data were analyzed using the Statistical Package for the Social Sciences for Windows (version 22.0: SPSS Inc., Chicago, IL, USA). The median and the interquartile range were used for the presentation of data of two groups as “median (interquartile range).” We used the Wilcoxon rank-sum test to analyze the difference of median between the two groups. The Chi-Square test and the Fisher's exact test were used to compare the difference of ratio between two groups. P < 0.05 was considered statistically significant.
RESULTS
Demographic and clinical data findings
Eighteen patients were in Group M and received the intra-auricular modification of facelift incision with partial-thickness SCM rotational flap. Forty-three patients were in Group S and received the traditional lazy-S incision with partial-thickness SCM rotational flap. The results are shown in Table 1. There was no difference between the two groups in age (P = 0.331), gender (P = 0.151), or size of tumor (P = 0.588). The pathological results included parotitis, pleomorphic adenoma, Warthin tumor, and others (including two lymphoid hyperplasia and one each of cavernous hemangioma, sclerosing sialadenitis, hemangiolymphangioma, Kimura's disease, toxoplasmosis, atrophic gland, oncocytoma, and cat scratch disease). There was no difference between the two groups in pathological results (P = 0.907). There was also no difference between the two groups in blood loss from surgery (P = 0.217), length of placement of drain (P = 0.330), total amount of drainage (P = 0.401), and length of stay (P = 0.797). However, there was significant difference between two groups in length of operation (P = 0.001).
Table 1.
Demographics and results
| Item | Group M (n=18), n (%) | Group S (n=43), n (%) | Total (n=61), n (%) | P |
|---|---|---|---|---|
| Age (years) | 51.50 (31.00) | 49.00 (20.00) | 49.00 (24.00) | 0.331 |
| Gender (%) | ||||
| Female | 12 (66.7) | 20 (46.5) | 32 (52.5) | 0.151 |
| Male | 6 (33.3) | 23 (53.5) | 29 (47.5) | |
| Histology (%) | ||||
| Parotitis | 2 (11.1) | 5 (11.6) | 7 (11.5) | 0.907 |
| Pleomorphic adenoma | 9 (50.0) | 19 (44.2) | 28 (45.9) | |
| Warthin’s tumor | 5 (27.8) | 11 (25.6) | 16 (26.2) | |
| Others | 2 (11.1) | 8 (18.6) | 10 (16.4) | |
| Frey syndrome (%) | ||||
| No | 18 (100.0) | 34 (79.1) | 52 (85.2) | 0.047* |
| Yes | 0 | 9 (20.9) | 9 (14.8) | |
| Tumor size (cm2) | 8.50 (9.00) | 9.00 (6.00) | 9.00 (6.50) | 0.588 |
| Operation time (min) | 202.50 (81.25) | 140.00 (60.00) | 160.00 (82.50) | 0.001* |
| Blood loss (cc) | 10.00 (45.00) | 50.00 (40.00) | 10.00 (45.00) | 0.191 |
| Drain placement (days) | 3.00 (1.50) | 3.00 (2.00) | 3.00 (1.50) | 0.330 |
| Total drain amount (cc) | 55.50 (39.00) | 46.00 (36.00) | 46.00 (33.50) | 0.401 |
| Length of stay (days) | 7.00 (2.00) | 6.00 (3.00) | 6.00 (3.00) | 0.797 |
Data are presented as median (IQR) or count (%). *P<0.05 is considered statistically significant after test. Group M: Intra-auricular modification of facelift incision + SCM flap, Group S: Lazy-S incision + SCM flap. SCM: Sternocleidomastoid muscle, IQR: Interquartile range
Frey syndrome findings
There was significant difference between two groups in the presentation of Frey syndrome after parotidectomy (P = 0.047).
DISCUSSION
About 12%–43% of patients receiving parotidectomy would develop Frey syndrome 6–18 months after parotidectomy [1,2,3,4,5]. The cause of Frey syndrome is due to the aberrant reinnervation of the parasympathetic nerve fibers from auriculotemporal nerve to the sweat glands and blood vessels of the subcutaneous tissue [6,7]. When salivary glands were stimulated, such as eating or chewing, the acetylcholine was released by parasympathetic nerve endings to sweat glands and blood vessels in subcutaneous tissue, resulting in flushing, sweating, warmth, neuralgia, and itching at the preauricular region [8,9,10].
The diagnosis of Frey syndrome is mainly dependent on the clinical symptoms and signs [11].
The auriculotemporal nerve with parasympathetic postganglionic nerves is originated from the mandibular nerve in the infratemporal fossa and passes through the posterior mandible and terminates at the temporal region. The parotid branch is derived from auriculotemporal nerve or connective branch of auriculotemporal nerve and facial nerve and terminates at parotid gland [12].
According to the research of Iwanaga et al.[12], of the dissected seven cadavers with a total of 10 sides; in this study, all the parotid branches were originated from the main trunk of the auriculotemporal nerve when the nerve enters to the superficial temporal region; all the parotid branches enter into parotid gland at the superior border of the gland; the location which the parotid branches originated from the auriculotemporal nerve is at a vertical distance of 8.27 ± 4.67 mm from the midpoint of the tragus and at a horizontal distance of 7.90 ± 3.07 mm [Figure 2].
Figure 2.
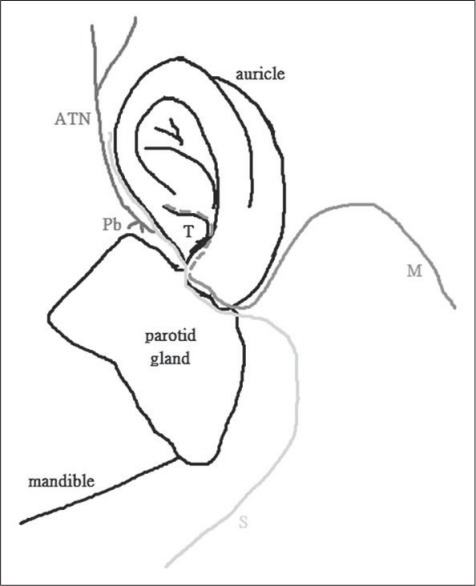
M for intra-auricular modification of facelift incision; S for lazy-S incision; ATN for auriculotemporal nerve; Pb for parotid gland; T for tragus
By blocking the passage of parasympathetic nerves in the parotid branch to sweat glands and blood vessels of subcutaneous tissue through the disconnection of the SMAS, the SCM flap can reduce the incidence of Frey syndrome [13].
In summary, the lower incidence of Frey syndrome of patients who received the intra-auricular modification of facelift incision might be presumed as followed: The parasympathetic postganglionic nerves of parotid branches must pass through the disconnection of SMAS which is consistent with the surgical incision to reach the sweat glands in the subcutaneous tissue. The intra-auricular modification of facelift incision does not extend to the cephalad, which can reduce the destruction of SMAS near parotid branch; its incision is on the hairline and is far from the parotid glands compared to the lazy-S incision. Besides, this method is started behind the tragus. Hence, it makes the aberrant reinnervation less likely to happen by the blockage of tragus cartilage.
The above reasons make the parasympathetic postganglionic nerves have to go farther to reach the incision and cross over the barrier of SMAS, thus reducing the incidence of Frey syndrome [Figure 2].
The use of facelift incision for parotidectomy results in good operative field [14] and can be used on the vast majority of benign parotid lesions even in the superior or anterior parotid lesions [15]; there is also a variety of modified incisions that can be used in different situations [16,17]. In most of the modified facelift incisions, the preauricular incision is extended upward to the auricular creases and even cephalad to the hairline of temporal region [16,17]. However, using the intra-auricular modification of facelift incision, the incision was begun behind the tragus, making the preauricular incision less obvious and less extended to the cephalad. Patients who receive facelift incisions also had better satisfaction with the postoperative appearance than the lazy-S incisions [18]. In addition, the complications (including wound hematoma, facial nerve damage, and flap necrosis) are similar to or even less than those of the lazy-S incision [19]. However, in this study, the operation time is longer with the intra-auricular modification of facelift incision, and this may be related to the surgical incision being farther away from the parotid gland.
CONCLUSIONS
From the anatomical viewpoint, the decreased incidence of Frey syndrome is attributed to (1) the preauricular incision is blocked by the tragal cartilage, (2) the preauricular SMAS is less damaged, and (3) the posterior incision was further away from the disconnection of SMAS. All the above makes the aberrant reinnervation of parasympathetic nerve to sweat gland more difficult.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Tuncel A, Karaman M, Sheidaei S, Tatlıpınar A, Esen E. A comparison of incidence of Frey's syndrome diagnosed based on clinical signs and minor's test after parotis surgery. Kulak Burun Bogaz Ihtis Derg. 2012;22:200–6. doi: 10.5606/kbbihtisas.2012.039. [DOI] [PubMed] [Google Scholar]
- 2.Freedberg AS, Shaw RS, McManus MJ. THE auriculotemporal syndrome. A clinical and pharmacologic study. J Clin Invest. 1948;27:669–76. doi: 10.1172/JCI102015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rustemeyer J, Eufinger H, Bremerich A. The incidence of Frey's syndrome. J Craniomaxillofac Surg. 2008;36:34–7. doi: 10.1016/j.jcms.2007.07.003. [DOI] [PubMed] [Google Scholar]
- 4.Neumann A, Rosenberger D, Vorsprach O, Dazert S. The incidence of Frey syndrome following parotidectomy: Results of a survey and follow-up. HNO. 2011;59:173–8. doi: 10.1007/s00106-010-2223-6. [DOI] [PubMed] [Google Scholar]
- 5.Nofal AA, Mohamed M. Sternocleidomastoid muscle flap after parotidectomy. Int Arch Otorhinolaryngol. 2015;19:319–24. doi: 10.1055/s-0035-1549155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Spiro RH, Martin H. Gustatory sweating following parotid surgery and radical neck dissection. Ann Surg. 1967;165:118–27. doi: 10.1097/00000658-196701000-00016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gardner WJ, Mccubbin JW. Auriculotemporal syndrome; gustatory sweating due to misdirection of regenerated nerve fibers. J Am Med Assoc. 1956;160:272–7. doi: 10.1001/jama.1956.02960390022007. [DOI] [PubMed] [Google Scholar]
- 8.de Bree R, van der Waal I, Leemans CR. Management of Frey syndrome. Head Neck. 2007;29:773–8. doi: 10.1002/hed.20568. [DOI] [PubMed] [Google Scholar]
- 9.Baek CH, Chung MK, Jeong HS, Son YI, Jung SC, Jeon HK, et al. Questionnaire evaluation of sequelae over 5 years after parotidectomy for benign diseases. J Plast Reconstr Aesthet Surg. 2009;62:633–8. doi: 10.1016/j.bjps.2007.08.034. [DOI] [PubMed] [Google Scholar]
- 10.Hartl DM, Julieron M, LeRidant AM, Janot F, Marandas P, Travagli JP. Botulinum toxin A for quality of life improvement in post-parotidectomy gustatory sweating (Frey's syndrome) J Laryngol Otol. 2008;122:1100–4. doi: 10.1017/S0022215108001771. [DOI] [PubMed] [Google Scholar]
- 11.Motz KM, Kim YJ. Auriculotemporal syndrome (Frey syndrome) Otolaryngol Clin North Am. 2016;49:501–9. doi: 10.1016/j.otc.2015.10.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Iwanaga J, Fisahn C, Watanabe K, Bobek SL, Ogata K, Tanoue R, et al. Parotid branches of the auriculotemporal nerve: An anatomical study with implications for Frey syndrome. J Craniofac Surg. 2017;28:262–4. doi: 10.1097/SCS.0000000000003260. [DOI] [PubMed] [Google Scholar]
- 13.Liu DY, Tian XJ, Li C, Sun SS, Xiong YH, Zeng XT, et al. The sternocleidomastoid muscle flap for the prevention of Frey syndrome and cosmetic deformity following parotidectomy: A systematic review and meta-analysis. Oncol Lett. 2013;5:1335–42. doi: 10.3892/ol.2013.1179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Upile T, Jerjes WK, Nouraei SA, Grant W, Singh S, Sudhoff H, et al. Further anatomical approaches to parotid surgery. Eur Arch Otorhinolaryngol. 2010;267:793–800. doi: 10.1007/s00405-009-1148-8. [DOI] [PubMed] [Google Scholar]
- 15.Lee SY, Koh YW, Kim BG, Hong HJ, Jeong JH, Choi EC. The extended indication of parotidectomy using the modified facelift incision in benign lesions: Retrospective analysis of a single institution. World J Surg. 2011;35:2228–37. doi: 10.1007/s00268-011-1209-1. [DOI] [PubMed] [Google Scholar]
- 16.Terris DJ, Tuffo KM, Fee WE., Jr Modified facelift incision for parotidectomy. J Laryngol Otol. 1994;108:574–8. doi: 10.1017/s002221510012746x. [DOI] [PubMed] [Google Scholar]
- 17.Hagan WE, Anderson JR. Rhytidectomy techniques utilized for benign parotid surgery. Laryngoscope. 1980;90:711–5. doi: 10.1288/00005537-198004000-00022. [DOI] [PubMed] [Google Scholar]
- 18.Bianchi B, Ferri A, Ferrari S, Copelli C, Sesenna E. Improving esthetic results in benign parotid surgery: Statistical evaluation of facelift approach, sternocleidomastoid flap, and superficial musculoaponeurotic system flap application. J Oral Maxillofac Surg. 2011;69:1235–41. doi: 10.1016/j.joms.2010.03.005. [DOI] [PubMed] [Google Scholar]
- 19.Grover N, D'Souza A. Facelift approach for parotidectomy: An evolving aesthetic technique. Otolaryngol Head Neck Surg. 2013;148:548–56. doi: 10.1177/0194599812475221. [DOI] [PubMed] [Google Scholar]


