Abstract
With an incidence of less than 1%, paraduodenal hernias are very rare but account for ~0.2–5.8% of mechanical small bowel obstruction and carry a mortality rate of 20–50%. Right-sided paraduodenal hernias are three times less frequent than left-sided paraduodenal hernias. We report the case of a 37-year-old man who suffered from colicky abdominal pain accompanied by vomiting. The computed tomography scan showed a mechanical ileus, caused by a presumed paraduodenal hernia, and we chose an elective laparoscopic surgical approach. The patient recovered quickly and was discharged on the second postoperative day. Paraduodenal hernias are a diagnostic challenge as they are typically characterized by long-term non-specific abdominal symptoms and are only detected in the event of acute intestinal obstruction. Until now, laparoscopic therapy has only been described in eight case reports and we review this rare condition and the surgical options.
Keywords: internal hernia, paraduodenal hernia, laparoscopy, malrotation
INTRODUCTION
The incidence of internal hernias is less than 1%, of which congenital paraduodenal hernias account for 53%. Left-sided hernias occur three times more frequently than right-sided paraduodenal hernias [1]. A review of the literature revealed only 15 cases of right-sided hernias in adults. While left-sided paraduodenal hernias occur with equal frequency in men and women, right-sided paraduodenal hernias arise three times more frequently in men [1]. Internal hernias are reported to cause 0.2–5.8% of all cases of small bowel obstruction [2]. Paraduodenal hernias occur due to an error in the reduction and rotation of the midgut during embryonic development [3, 4]. The mesentery of the ascending colon to the right side of the superior mesenteric artery fails to merge with the retroperitoneum and forms a defect called Waldeyer’s fossa [3, 5, 6]. The small bowel, which subsequently herniates into the fossa, is typically located behind the ascending colon [5].
CASE
A 37-year-old patient presented with acute abdominal pain which was colicky in nature and accompanied by nausea and repeated vomiting. Physical examination showed tenderness in the right lower abdomen and guarding in all four quadrants. There was no history of previous abdominal surgery. A computed tomography (CT) scan revealed the mechanical obstruction of the small bowel and the suspicion of a pre-existing paraduodenal hernia in the right upper abdomen (Figs 1 and 2). Fortunately, the patient’s condition improved significantly following the administration of analgesia, and the initial conservative treatment was continued. An X-ray with oral contrast agent enhanced the suspicion of a right-sided paraduodenal hernia. As the patient was now pain free, we scheduled an elective diagnostic laparoscopy 3 weeks later.
Figure 1.
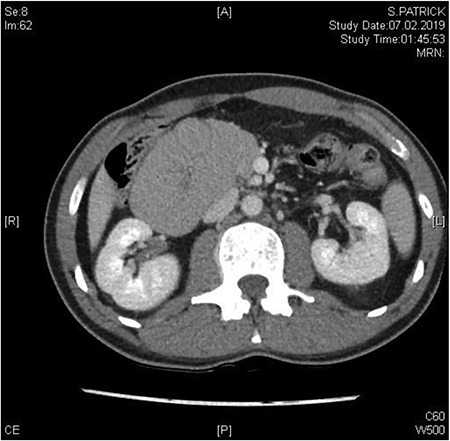
Between the head of pancreas and the lower edge of the liver, an oval-shaped, clearly defined convolution of small intestine loops measuring ~9.5 x 6.5 cm was visible. The duodenum could not be followed as expected—there is no duodenal part crossing the vessels to the left
Figure 2.
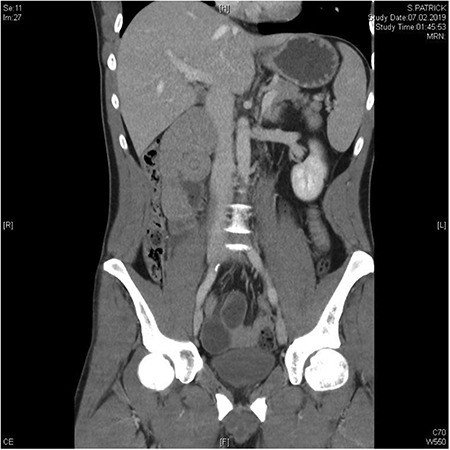
In the coronal plane, in addition to the suspicion of an internal hernia, a short intussusception was also suspected. Furthermore, this level shows that the herniating small intestine is located on the right, while the left side of abdomen appears empty
The patient was positioned supine. We used a 12-mm umbilical camera port, and 5-mm trocars were placed in the left and right middle abdomen. Laparoscopic inspection revealed a hernia aperture below the terminal ileum, behind which we found the hernia sac where the small intestine had become entangled 3 weeks previously (Fig. 3). The subsequent small bowel revision was uneventful. In the area of Treitz’s ligament, the vessels were on the right side with no herniation on the left side (Fig. 4). At this point, we decided to enlarge the hernia aperture by mobilizing the cecum. The ureter and the testicular vessels were identified. Finally, the hernia sac was widened, to prevent future entrapment of the small intestine. (Fig. 5) The postoperative course was uneventful and the patient was discharged 2 days later.
Figure 3.
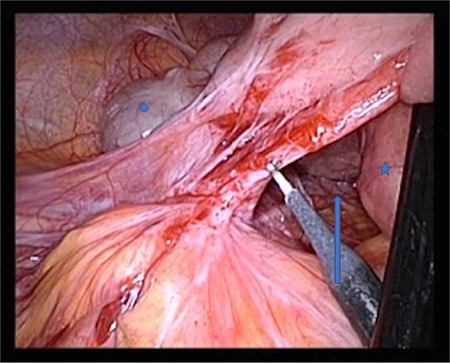
Star: duodenum, circle: cecum, arrow: Waldeyer’s fossa
Figure 4.

Star: transverse colon under the greater omentum, arrow: vessel axis, circle: proximal jejunum. The ligament of Treitz is not shown
Figure 5.
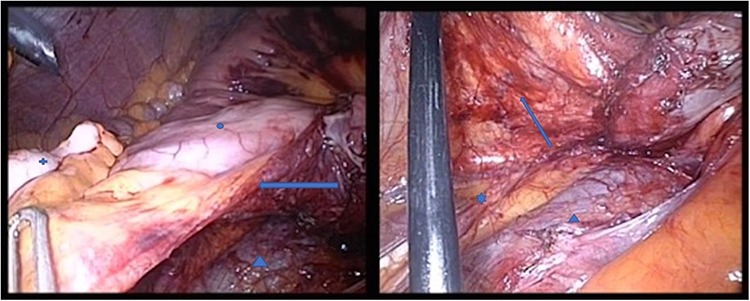
Both pictures display the hernia sac; in the right panel, the hernia sac has been elevated. Circle: terminal ileum, cross: appendix, star: ureter, triangle: V. cava, arrow: hernia sac, which has been opened
DISCUSSION AND REVIEW
Paraduodenal hernias develop from embryonic anomalies of the peritoneum and are associated with malrotation of the small intestine [6–8]. The diagnostic workup usually consists of a CT scan of the abdomen and/or an abdominal X-ray. The typical finding of a paraduodenal hernia shows an accumulation of small intestine loops lateral under the second part of the duodenum, behind the ascending colon [3]. The superior mesenteric vein is commonly rotated anteriorly to the left [1, 9]. An indicator of malrotation is the absence of the horizontal duodenum [1]; however, it is characteristic that the cecum is in its anatomically correct position. These diagnostic features were also apparent in our patient.
The published literature pertaining to right-sided paraduodenal hernias is sparse and consists mostly of case reports, of which we only found in total 15 patients. Seven of these patients received an exploratory laparotomy due to an acute mechanical obstruction. In only eight patients, a primary laparoscopic approach was chosen, and two cases required conversion to an open laparotomy due to surgical complexity [4, 7].
There are two surgical options. The first is to open the hernial sac with a lateral approach, reduction of the intestinal contents and subsequent complete excision of the hernial sac. As a consequence, the anatomical conditions automatically re-establish themselves [4].
The second option is to dissect and remove Ladd’s bands which extend from the large intestine to the duodenum and result from embryonic maldevelopment. The cecum is then mobilized, and the pre- and postarterial segments of the intestine are returned to their anatomical positions [8, 10].
The first option is the most frequently used according to published reports. While Ladd’s procedure is very commonly used for children, we only found two cases where Ladd bands were described intraoperatively in adults. Manipadem et al. observed that these correlated with a higher degree of incomplete rotation and that these patients usually describe a history of chronic abdominal pain since childhood.
Our patient, as well as most of the adult patients reported in the literature, developed intestinal symptoms at an older age, which suggested a less severe form of malrotation. This correlated with the intraoperative findings and the lack of a Ladd band. Therefore, opening the hernial sac in such cases is usually sufficient [10]. In accordance with other reports in the literature, the laparoscopic method is recommended as it yields the best postoperative outcome [8].
Paraduodenal hernias remain a diagnostic difficulty due to their rarity and their unspecific clinical symptoms. In case of unclear or chronic abdominal pain, an internal hernia should be in the differential diagnosis.
References
- 1. Martin LC, Merkle EM, Thompson WM. Review of internal hernias: radiographic and clinical findings. Am J Roentgenol 2006;186:703–17. [DOI] [PubMed] [Google Scholar]
- 2. Bittner JG, Edwards MA, Harrison SJ, Li K, Karmin PN, Mellinger JD, Mellinger JD. Laparoscopic repair of a right paraduodenal hernia. JSLS 2009;13:242–9. http://www.ncbi.nlm.nih.gov/pubmed/19660226 (1 July 2019, date last accessed]. [PMC free article] [PubMed] [Google Scholar]
- 3. Gupta RK, Kothari P, Gupta A, Ranjan R, Kesan KK, Mudkhedkar K, Karkare P, Mohammed N. Laparoscopic management of right paraduodenal hernia along with the correction of malrotation in a pediatric patient: a case report. Ann Pediatr Surg 2013;9:90–92. https://www.ajol.info/index.php/aps/article/viewFile/118653/108144 (23 July 23 2019, date last accessed). [Google Scholar]
- 4. Mehra R, Pujahari AK. Right paraduodenal hernia: report of two cases and review of literature. Gastroenterol Rep 2016;4:168–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Licciardello A, Rapisarda C, Conti P, Trombatore G. Small bowel obstruction caused by an unusual variant of paraduodenal hernia. The “middle congenital mesocolic hernia”: case report. J Gastrointest Surg 2014;18:1514–7. [DOI] [PubMed] [Google Scholar]
- 6. Manfredelli S, Andrea Z, Stefano P, Giovanni L, Maria M, Angelo F, et al. Rare small bowel obstruction: right paraduodenal hernia. Case report. Int J Surg Case Rep 2013;4:412–5. doi: 10.1016/j.ijscr.2012.11.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Shadhu K, Ramlagun D, Ping X. Para-duodenal hernia: a report of five cases and review of literature. BMC Surg 2018;18:1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Takagishi T, Niimi Y, Matsuki G, Nagano S, Hinami J, Kajiwara M, et al. Laparoscopic repair of right paraduodenal hernia in adult patients: case report and literature review. Case Rep Surg 2018;2018:1–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Blachar A, Federle MP. Internal hernia: an increasingly common cause of small bowel obstruction. Semin Ultrasound CT MR 2002;23:174–83. [DOI] [PubMed] [Google Scholar]
- 10. Manipadam JM, Lekha V, Syamprasad V, Ramesh H. Laparoscopic repair of a right paraduodenal hernia. Surg J (NY) 2018;4:e129–32. http://www.ncbi.nlm.nih.gov/pubmed/30038962 (23 July 2019, date last accesed). [DOI] [PMC free article] [PubMed] [Google Scholar]


