To the Editor:
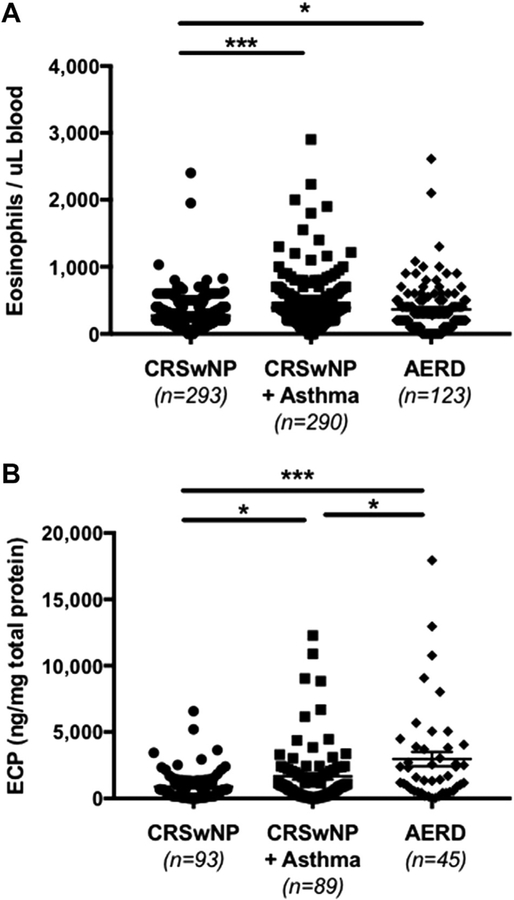
We thank Yılmaz et al1 for their insightful comments regarding our recent article investigating the clinical characteristics of patients with chronic rhinosinusitis with nasal polyps (CRSwNP), asthma, and aspirin exacerbated respiratory disease (AERD).2 We agree that these clinical conditions are traditionally characterized by an enhanced type 2 inflammatory environment, including eosinophils. Measuring eosinophil numbers within our clinical cohort could potentially be useful in determining if a specific clinical feature could be predicted by the number of eosinophils present. Unfortunately, our study was limited to a retrospective review of patient medical data and peripheral eosinophil counts could not be prospectively obtained. Additionally, not all study patients had a documented eosinophil count in their medical record, and among those that did, some had insufficient information regarding the presence of confounding factors (eg, whether the patient was taking systemic corticosteroids at the time of the blood draw). Because of these variables, we did not include an analysis of peripheral eosinophils in our original study. However, stimulated by the points raised by Yılmaz et al., we reviewed the available peripheral eosinophil counts in our cohort and found, on average, significantly elevated peripheral eosinophils in patients with CRSwNP+asthma (388 ± 21; P < .001) or with AERD (365 ± 33; P = .03) compared with patients with CRSwNP alone (272 ± 14) (Figure 1, A). Interestingly, there was no significant difference in peripheral eosinophil numbers between patients with CRSwNP+asthma and those with AERD (P = .56) (Figure 1, A), suggesting that, despite the limitations mentioned above, asthma may be a primary driving factor in elevated peripheral eosinophil levels in these patients.
FIGURE 1.
Assessment of eosinophilia among patients with chronic rhinosinusitis with nasal polyps (CRSwNP). (A) Numbers of eosinophils in peripheral blood and (B) levels of eosinophil cationic protein (ECP) in nasal polyp tissue were measured in patients with CRSwNP (circles), CRSwNP+asthma (squares), or aspirin exacerbated respiratory disease (AERD) (diamonds). Statistical significance was determined by the Kruskal-Wallis test with post hoc analysis using Dunn’s test for multiple comparison and *P < .05 and ***P < .001. Dot pots illustrate individual data points and solid lines represent the mean ± standard error of the mean.
The role eosinophils play in AERD pathogenesis as well as their utility in serving as a clinical biomarker of disease severity is not entirely clear. Our findings are consistent with some studies that have reported no difference in peripheral eosinophil numbers between patients with AERD and those with aspirin-tolerant asthma (with or without comorbid CRSwNP)3 or those with CRSwNP (with or without comorbid asthma).4 However, a recent report suggested that patients with CRSwNP with aspirin intolerance do have significantly higher numbers of peripheral eosinophils than patients with CRSwNP who tolerate aspirin.5 Among patients with AERD in particular, a latent class analysis identified 4 distinct subphenotypes including one consisting of patients with moderate asthma, severe upper airway symptoms, and blood eosinophilia greater than 400.6 However, in a separate study, the numbers of peripheral eosinophils did not significantly correlate with the level of asthma control (ie, controlled, partially controlled, or uncontrolled) in patients with AERD.7 In contrast, the Japanese Epidemiological Survey of Refractory Eosinophilic Chronic Rhinosinusitis (JESREC) study found that patients with CRSwNP with greater than 10% peripheral blood eosinophils had a significantly increased rate of sinus disease recurrence.8 Taken together, we agree with Yılmaz et al. that more in-depth investigations are warranted to determine if (and how) peripheral eosinophil levels in patients with CRSwNP (and AERD) could be reflective of certain clinical characteristics.
CRSwNP pathogenesis is thought in part to be driven by local, rather than systemic, inflammatory processes9 and several studies have examined eosinophils in sinonasal tissue. Patients with eosinophilic nasal polyps (defined as >10% eosinophils in the total cellular infiltrate per high-power field) were shown to have more severe upper and lower airway disease than patients with noneosinophilic nasal polyps.10 Interestingly, the number of eosinophils in nasal polyps of patients with AERD and CRSwNP was not found to be significantly different.11,12 In contrast, when assessing nasal polyps of patients who underwent sinus surgery at our institution between 2010 and 2014, we found patients with AERD, on average, had significantly elevated levels of eosinophil cationic protein (ECP) (2967 ng/mg total protein) compared with patients with CRSwNP+asthma (1671 ng/mg total protein, P = .03) or those with CRSwNP alone (890 ng/mg total protein, P < .001) (Figure 1, B). Additionally, patients with both CRSwNP and asthma had significantly more ECP than patients with CRSwNP alone (P = .03). Understanding the impact of asthma (and AERD) on ECP levels as well as why there is a discrepancy between eosinophil numbers and detectable levels of ECP in these diseases remains the focus of ongoing investigations. This discrepancy suggests caution against the sole use of eosinophil numbers in nasal polyps to distinguish between patients with AERD and those with CRSwNP.
Finally, we agree with Yılmaz et al1 that the 3 cardinal features of AERD (CRSwNP, asthma, and hypersensitivity to COX-1 inhibitors) typically develop at various stages over a period of time, as opposed to simultaneously. In our experience, we have not seen patients with AERD progress to develop eosinophilic pulmonary infiltrates or eosinophilic granulomatosis with polyangiitis. However, we look forward to learning about the results of the investigation by Yılmaz et al on eosinophilic pulmonary infiltrates in patients with AERD.
Acknowledgments
This work was supported by the Parker B. Francis Fellowship Program, the American Partnership for Eosinophilic Disorders/American Academy of Allergy, Asthma and Immunology HOPE Pilot Grant Award, the National Institutes of Health (grant nos. U19 AI106683-01 [Chronic Rhinosinusitis Integrative Studies Program], KL2TR001424, T32 AI083216, R37 HLO68546), and the Ernest Bazley Foundation.
Footnotes
Conflicts of interest: W. W. Stevens has received research support from Parker B. Francis Fellowship Program, the American Partnership for Eosinophilic Disorders/American Academy of Allergy, Asthma and Immunology HOPE Pilot Grant Award, and the National Institutes of Health’s National Center for Advancing Translational Sciences, KL2TR001424. A. T. Peters has received consultancy fees from Sanofi (advisory board membership). R. P. Schleimer has received research support from the National Institutes of Health; has received consultancy fees from Intersect ENT, GlaxoSmithKline, Allakos, Aurasense, Merck, BioMarck, Sanofi, AstraZeneca/MedImmune, Genentech, Exicure Inc., and Otsuka Inc,; and has stock in Allakos, Aurasense, BioMarck, and Exicure Inc.
REFERENCES
- 1.Yılmaz İ, Türk M, Bahçecioğlu SN. Eosinophilic asthma with nasal polyposis march: is aspirin-exacerbated respiratory disease the last station? J Allergy Clin Immunol Pract 2017;5:1807–8. [DOI] [PubMed] [Google Scholar]
- 2.Stevens WW, Peters AT, Hirsch AG, Nordberg CM, Schwartz BS, Mercer DG, et al. Clinical characteristics of patients with chronic rhinosinusitis with nasal polyps, asthma, and aspirin-exacerbated respiratory disease. J Allergy Clin Immunol Pract 2017;5:1061–70.e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mascia K, Borish L, Patrie J, Hunt J, Phillips CD, Steinke JW. Chronic hyper-plastic eosinophilic sinusitis as a predictor of aspirin-exacerbated respiratory disease. Ann Allergy Asthma Immunol 2005;94:652–7. [DOI] [PubMed] [Google Scholar]
- 4.Ikeda K, Shiozawa A, Ono N, Kusunoki T, Hirotsu M, Homma H, et al. Subclassification of chronic rhinosinusitis with nasal polyp based on eosinophil and neutrophil. Laryngoscope 2013;123:E1–9. [DOI] [PubMed] [Google Scholar]
- 5.Brescia G, Barion U, Zanotti C, Giacomelli L, Martini A, Marioni G. The prognostic role of serum eosinophil and basophil levels in sinonasal polyposis. Int Forum Allergy Rhinol 2017;7:261–7. [DOI] [PubMed] [Google Scholar]
- 6.Bochenek G, Kuschill-Dziurda J, Szafraniec K, Plutecka H, Szczeklik A, Nizankowska-Mogilnicka E. Certain subphenotypes of aspirin-exacerbated respiratory disease distinguished by latent class analysis. J Allergy Clin Immunol 2014;133: 98–103.e1–6. [DOI] [PubMed] [Google Scholar]
- 7.Bochenek G, Szafraniec K, Kuschill-Dziurda J, Nizankowska-Mogilnicka E. Factors associated with asthma control in patients with aspirin-exacerbated respiratory disease. Respir Med 2015;109:588–95. [DOI] [PubMed] [Google Scholar]
- 8.Tokunaga T, Sakashita M, Haruna T, Asaka D, Takeno S, Ikeda H, et al. Novel scoring system and algorithm for classifying chronic rhinosinusitis: the JESREC Study. Allergy 2015;70:995–1003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Schleimer RP. Immunopathogenesis of chronic rhinosinusitis and nasal polyposis. Annu Rev Pathol 2017;12:331–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wu D, Li L, Zhang M, Wang J, Wei Y. Two inflammatory phenotypes of nasal polyps and comorbid asthma. Ann Allergy Asthma Immunol 2017;118:318–25. [DOI] [PubMed] [Google Scholar]
- 11.Mahdavinia M, Carter RG, Ocampo CJ, Stevens W, Kato A, Tan BK, et al. Basophils are elevated in nasal polyps of patients with chronic rhinosinusitis without aspirin sensitivity. J Allergy Clin Immunol 2014;133:1759–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Stevens WW, Ocampo CJ, Berdnikovs S, Sakashita M, Mahdavinia M, Suh L, et al. Cytokines in chronic rhinosinusitis. Role in eosinophilia and aspirin-exacerbated respiratory disease. Am J Respir Crit Care Med 2015z;192:682–94. [DOI] [PMC free article] [PubMed] [Google Scholar]