The term “vital capacity” i.e., capacity for life, was coined by John Hutchinson, the inventor of spirometry, since the total volume of air exhaled from fully inflated lungs seemed inversely predictive of mortality. A century later, data from the Framingham cohort reaffirmed that forced vital capacity (FVC) normalized to height is a strong independent marker of all age cardiovascular risk, even accounting for traditional risk factors, including age, obesity, blood pressure, smoking, heart rate, serum cholesterol, and blood glucose. In other studies, FVC is also associated with early markers such as blood pressure variability, serum fibrinogen and C-reactive protein. The predictive power of a low FVC is independent of clinical airway obstruction, such that in the Atherosclerosis Risk In Communities (ARIC) study, restrictively low lung function (RLLF; low FVC, normal FEV1/FVC ratio) was associated with a 70% increase in mortality, including either or both of heart disease and diabetes; worse than the risks of GOLD 0 or 1 chronic obstructive pulmonary disease. The reduced FVC of RLLF is not typically due to gas trapping and corresponds to true reduction in lung volumes. Why FVC variations are informative about extrapulmonary health risks is unclear, but possible reasons are summarized in Figure 1.
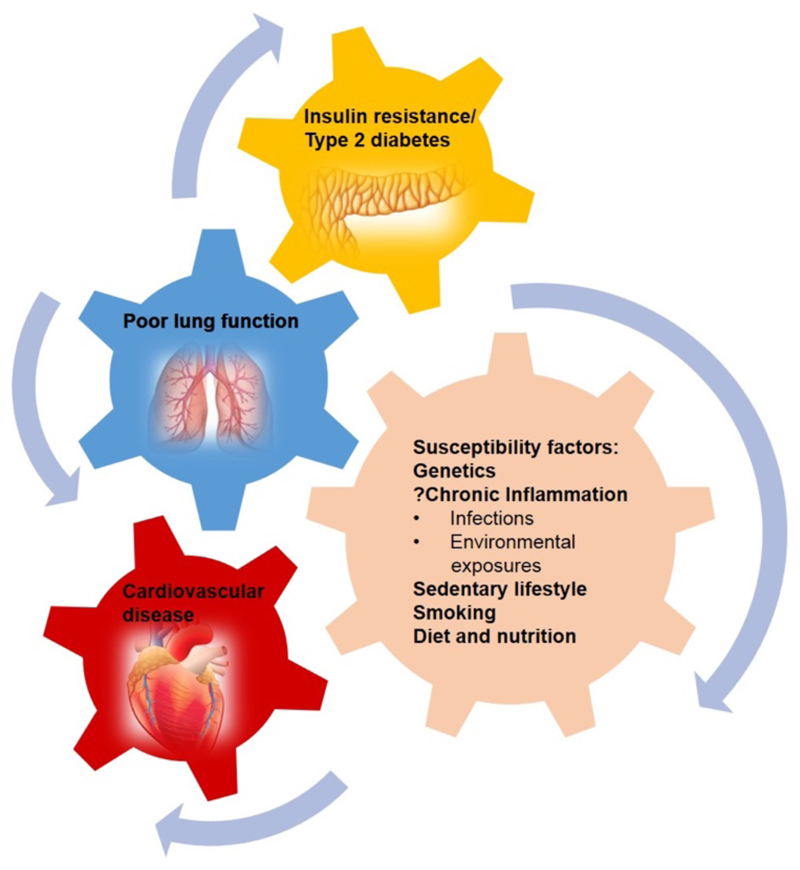
Figure 1.
Common origins of Lung, cardiovascular and metabolic disorder. Low lung function-cardiovascular disease-insulin resistance/type 2 diabetes epidemiologic triad are interrelated and may be driven by common underlying casual elements
FVC also varies across ethnic groups and geographical regions, even after adjusting for gender, height, weight and age. Even within a nation, there can be significant differences between ethnicities. In response to these differences, ethnic and geographic reference equations have been developed. This differs from the practice followed for other physiological parameters, notably blood pressure; it is accepted that some communities have a greater prevalence of hypertension, and different normal ranges for systolic and diastolic blood pressure are not applied. The logic of this approach for spirometry has been debated past; ethnically different normal ranges appear valid in some contexts, for example between genetically distinct populations with different body habitus. However, as shown by Burney and Hooper, a given FVC has the same prognostic significance for ‘normal’ African-American and White participants. Spirometry may thus be a proxy integrated index of early life exposures and development, which will be obscured by using of ethnic or regional norms. If so, the prevalent use of community-based normal lung function standards, while possibly useful for assessing lung disease, masks the potential of spirometry to assess cardiometabolic risk. India is an interesting case in point.
‘Healthy’ Indians have FVC values about a third lower than that of matched healthy white Americans or Europeans (PURE study). The use of global reference values would lead to 40-45% of Indians being categorized as RLLF. Further, India herself is not a single entity in terms of spirometry. Different reference equations have been published for North, South, East and West India to reflect regional differences. So what advice do we give to an Indian whose spirometry is 70% that of a gender, age and height matched white English control?
Three assumptions are made while generating normal ranges. First, that the local reference population is truly healthy. Second, variations across communities are reflective of innate differences related to genetics or body habitus. Third, these variations are not attributable to pathology and do not therefore mask pathophysiological differences. The definition of healthy is usually based on self-declaration, questionnaires and in some cases a normal chest radiograph and physical examination, with no prospective follow-up or laboratory investigations. Many were hospital based with relatives and attendants of patients recruited as ‘normal’; however, common environmental exposures may have affected these ‘normals’. Also, since poor lung function is related to insulin resistance and pre-diabetes, we need to have information about population prevalence. In independent studies, insulin resistance, pre-diabetes and undiagnosed asymptomatic cardiometabolic disease are much higher in India than in western populations, and variable between different sub-populations, raising concern about the first assumption of the local reference population being “similarly healthy”. The Indian Genome Variation study, as well as studies of human migration, shows North or West Indians are genetically similar to each other and to Caucasians. Even the South or East Indian populations are not very different; certainly, any differences are not comparable to differences between African and Caucasians. The actual differences in spirometry between sub-populations were complex, with directions reversing at different absolute value ranges i.e. one sub-population having lower lower-limits of normal, but higher upper-limits for FVC, when compared to another sub-population. Such differences may be due to greater heterogeneity, whether genetic or acquired, in the sub-population with a wider range. Many of these differences are readily understandable in the context of Indian socio-economic variations, with differences in shorter (with lower ranges of FVC) subjects being heavily influenced by the presence of stunting. Hypothetically, regions with lower economic development are likely to have lower pollution, more active lifestyles, but also a larger fraction of marginalized communities with stunting; thus, creating opposing effects upon lung function that would fit the complex differences discussed above. However, this has never been formally investigated.
In India, factors like low birth weight, short stature and high Cormic index (upper to lower body segment ratio) may indeed lead to systematic differences from predicted lung function, but this may also be a marker of adverse socioeconomic status (SES) with useful prognostic information. In fact, Cormic-index related variations in Indians would independently lead to falsely low FVC predictions from western equations (due to standing height underestimating upper body length). Thus, the lower than predicted FVC in Indians cannot be explained on basis of anthropometric differences such as longer legs, as in the case of Africans. This becomes clearer when we look at the effect of changed environment within the same genetic ancestry. Subjects of Indian subcontinent ethnicity, but born in America or Britain, have spirometry intermediate between indigenous Indians and white westerners. The differences are more pronounced for women. Even within India, a comparison of recent and older equations clearly shows that women have better lung function today than in previous decades. British-Indian and urban Indian children from affluent urban schools and from semi-rural or rural settings, have similar zFVC, greater than those from semi-rural or rural settings. Whether this relates to genetic, epigenetic or lifestyle differences is not apparent.
So how do we advise our hypothetical Indian with ‘normal’ spirometry which is worse than his white counterpart? There is little to no data on what it means to be ethnically normal, but globally abnormal. Clearly, telling our Indian that he is ‘normal’ because he is within the regional normal range may be at one level correct, but is actually deceptive since adverse SES influences may exist for the entire community. In fact, Indians (and other South Asians) have exceptionally high risk for development of cardiometabolic disease compared to white westerners. To some extent this Gordian knot can be cut by looking at second or third generation immigrants to an affluent society; if spirometry becomes the same as the affluent white, it is very clear that the ‘normal’ spirometry reported in the original habitat is no such thing, but likely carries the same bad prognostic implications as the same values would in a white counterpart. If it does not normalize, then the intriguing possibility is raised that ethnic genetic differences exist which lead to lower spirometry and the associated bad outcomes. Either way, the hypothetical Indian’s spirometry should be related not to that of his local counterparts, but to his relatives across the seas. As discussed above, the limited available information supports the contention that the differences transcend genes and likely reflect substantial environmental influences with prognostic significance. More work is needed and the widely spread Indian diaspora, with about 15 million non-resident Indians globally, is a good place to start. Such studies could define how to best use spirometry not only for respiratory disease diagnosis, but also as a health assessment tool accounting for true ethnic differences as well as meaningful environmental exposures.
In summary we spotlight the clear need for studies that systematically phenotype subjects with relevant physiological and biochemical parameters, including lung function, and nutritional and inflammatory markers. Given the importance of maternal, peri-natal influences, and birth weight in lung function, it would be important to conduct such studies as part of longitudinal birth cohorts. Such efforts would correctly place an individual at the centre of all stages of healthcare from clinical measurement to preventative and treatment strategies.
Funding
Wellcome Trust DBT India Alliance (AA, MA)
Footnotes
For more on spirometry and vital capacity as a predictor for CV risk see Trans Am Clin Climatol Assoc 1987; 98: 11-20
For the Framingha m study, see Am Heart J 1983; 105: 311–5 and for ARIC, see Thorax 2010; 65: 499–504
For more on FVC prognostic significance across ethnicity, see Int J Epidemiol 2012; 41: 782–90
For more on PURE Study see Lancet Respir Med 2013; 1: 599–609
For more on regional lung function variations in India see Indian J Chest Dis Allied Sci 2009; 51: 7–13.
For pulmonary function of immigrant vs US-born adults, see Chest 2010; 137: 1398–404.
For elevated cardiomet abolic disease risk of Indians, see the MASALA study, https://www.masalastudy.org