Abstract
Peripartum cardiomyopathy (PPCM) can lead to long-term systolic dysfunction, especially among black women. Hypertensive disorders of pregnancy (HDP) are the strongest risk factor for PPCM, but controversy remains on whether HDP predict a favorable outcome. Women with HDP are also often diagnosed with PPCM earlier than those without HDP. Our objective is to determine recovery of systolic function in patients with PPCM stratified by HDP, timing of diagnosis, and race. We conducted a retrospective cohort study of 220 patients (55% black) diagnosed with PPCM. Patients with PPCM and HDP were diagnosed earlier postpartum than patients without HDP (p=0.013), an effect that was most pronounced in non-black patients. Rates of LVEF recovery were similar among PPCM patients with and without HDP (68.4% vs. 62.6%, p=0.425). In contrast, patients with PPCM diagnosed after 1 month postpartum had lower rates of LVEF recovery than patients diagnosed < 1 month postpartum (53.7% vs. 69.9%, p= 0.035). LVEF at time of diagnosis is a strong predictor of LVEF recovery, and patients with PPCM diagnosed after 1 month postpartum had lower baseline LVEF compared to patients presenting earlier (p = 0.041). The presence of HDP does not correlate with LVEF recovery in our racially diverse PPCM cohort. In contrast, early diagnosis portends a favorable outcome. Early diagnosis is associated with higher LVEF at presentation, likely explaining the improved outcomes in these women. These findings underscore the need for early monitoring and diagnosis, especially in at-risk and underserved populations.
Keywords: preeclampsia/pregnancy, cardiomyopathy, women, disparities, quality of care
Graphical Abstract
INTRODUCTION
Peripartum cardiomyopathy (PPCM) is an often severe form of cardiomyopathy diagnosed towards the end of pregnancy or in the months after delivery that affects at least 1 in 2,000 deliveries in the United States (U.S.).1,2 Recovery to normal systolic function occurs in 61-72% of patients in contemporary cohorts with approximately 13% of patients having persistent severe dysfunction or major adverse cardiovascular events such as left ventricular assist device (LVAD), heart transplant, or death.1,3,4
Preeclampsia and gestational hypertension are hypertensive disorders of pregnancy (HDP) that are more common in black women and strongly predispose to the development of peripartum cardiomyopathy (PPCM).1,5 At least 22% of patients with PPCM have preeclampsia and a third have any hypertension, including preeclampsia, gestational hypertension, or chronic hypertension.6 Preeclampsia and PPCM likely share pathophysiological mechanisms, including the upregulation of antiangiogenic and vasculotoxic hormones secreted by the placenta.1,7,8
In patients in whom HDPs contribute to the development of PPCM, resolution of postpartum hypertension and normalization of angiogenic imbalance may theoretically accelerate resolution of PPCM. Consistent with this notion, PPCM cohorts in Germany and Japan have demonstrated a higher likelihood of LV recovery among patients with HDP compared to patients without HDP.9,10 In contrast, however, several studies in the U.S. have demonstrated no such relationship3,11 or conflicting outcomes.12
Timing of diagnosis may confound the relationship between HDP and PPCM since women with HDP are often treated with antihypertensives postpartum and require close follow-up in the days to weeks after delivery. Early postpartum follow-up may facilitate the early diagnosis and treatment of PPCM in women at risk. The prospective PPCM cohort in the Investigations of Pregnancy-Associated Cardiomyopathy (IPAC) registry suggested that earlier diagnosis is a predictor of recovery of systolic function, but interaction with HDP was not probed, and this relationship has not been explored in other cohorts.11
Finally, we and others have shown that important racial disparities exist in PPCM outcomes in the U.S. and worldwide.4,11,13–16 In our cohort of 220 women with PPCM, black women were almost half as likely to recover and took twice as long to do so. Interestingly, we also noted that black women were diagnosed significantly later than non-black women, typically a month or more after delivery.4 Together, these observations raise the question of how race, HDP, and timing of diagnosis interplay, if at all, to impact prognosis in PPCM. Our objective was therefore to understand how HDP and timing of postpartum diagnosis impact PPCM outcomes in one of the largest and racially diverse PPCM cohorts in the U.S.
METHODS
We conducted a retrospective cohort study of women diagnosed with PPCM between 1986 until 2016 treated within the University of Pennsylvania Health System (UPHS). This study was approved by the University of Pennsylvania Institutional Review Board. To minimize the possibility of unintentionally sharing information that can be used to reidentify patients, a subset of the data that support the findings of this study are available from the corresponding author on reasonable request.
Cohort
We queried the UPHS clinical data warehouse, Penn Data Store (PDS), to identify all patients with a potential diagnosis of peripartum cardiomyopathy, based on ICD-9 (International Classification of Diseases, Ninth Revision) diagnosis code of 674.5 or the presence of an echocardiogram within 6 months of delivery. We manually reviewed medical records, including echocardiography reports, consultation notes, and discharge summaries of all potentially eligible women. We included patients 18 years or older if they were diagnosed with PPCM or heart failure towards the end of pregnancy or in the several months following delivery, and had no other identifiable cause for their heart failure.17 Inclusion criteria for PPCM diagnosis included: (1) systolic dysfunction as determined by left ventricular ejection fraction (LVEF) < 45% or fractional shortening (FS) < 30% on echocardiogram at time of diagnosis; (2) documentation of systolic dysfunction in clinical notes at time of diagnosis; or (3) ongoing systolic dysfunction documented by echocardiogram or clinical notes among women transferred to UPHS after diagnosis. Exclusion criteria included a history of congenital heart disease, significant valvular disease predating PPCM diagnosis, and a history of radiation or cardiotoxic chemotherapy.
Covariates
We extracted relevant demographic and clinical information from PDS including diagnosis details, past obstetric and medical history, and clinical outcomes. Race was self-reported as documented in PDS. We dichotomized race as black versus non-black as described previously4 and based upon reports that black women with PPCM have worse outcomes as described above. We included gestational hypertension, preeclampsia, and eclampsia as hypertensive disorders of pregnancy as diagnosed on retrospective chart review. Timing of PPCM diagnosis was recorded as a categorical variable in the original cohort and was dichotomized into early (< 1 month after delivery) versus late (≥ 1 month after delivery).
Outcomes
Our primary outcome was full recovery of LV function, defined as LVEF > 50%, consistent with other contemporary cohorts.3,4,11 Secondary outcomes included time to recovery (days) for patients with documented dates of diagnosis and follow-up echocardiograms and adverse cardiovascular events including left ventricular assist device (LVAD) placement, heart transplantation, or death. Patients without follow-up echocardiogram data were censored. Patients were followed for the duration of time that they received care at UPHS, through 2016. As LVEF at time of diagnosis is one of the strongest predictors of subsequent LVEF recovery, we compared differences in baseline LVEF at time of diagnosis stratified by HDP and timing of PPCM diagnosis among the cohort of patients with available baseline echocardiographic reports.
Statistical analysis
We presented continuous variables as mean with standard deviation (SD) and/or median with interquartile range. We assessed continuous variables using student t test and Wilcoxon rank sum tests as appropriate. Categorical variables are presented as counts and percentages and were compared utilizing Chi-square tests. We used Kaplan-Meier survival analysis for recovery time and group differences were compared using the Wilcoxon rank-sum test. We used logistic regression to analyze predictors of LVEF recovery. A p value <0.05 was considered significant. We performed the analysis using SAS version 9.4 software (SAS Institute Inc., Cary, North Carolina).
RESULTS
We identified 220 PPCM patients (121 black patients, 55%) between 1986 and 2016. We were able to ascertain HDP status in 180 patients (81.8%) and timing of diagnosis in 193 patients (87.7%). The median duration of follow-up was 42.6 months (intraquartile range 9.5 to 89.2 months).
Hypertensive disorders of pregnancy baseline characteristics
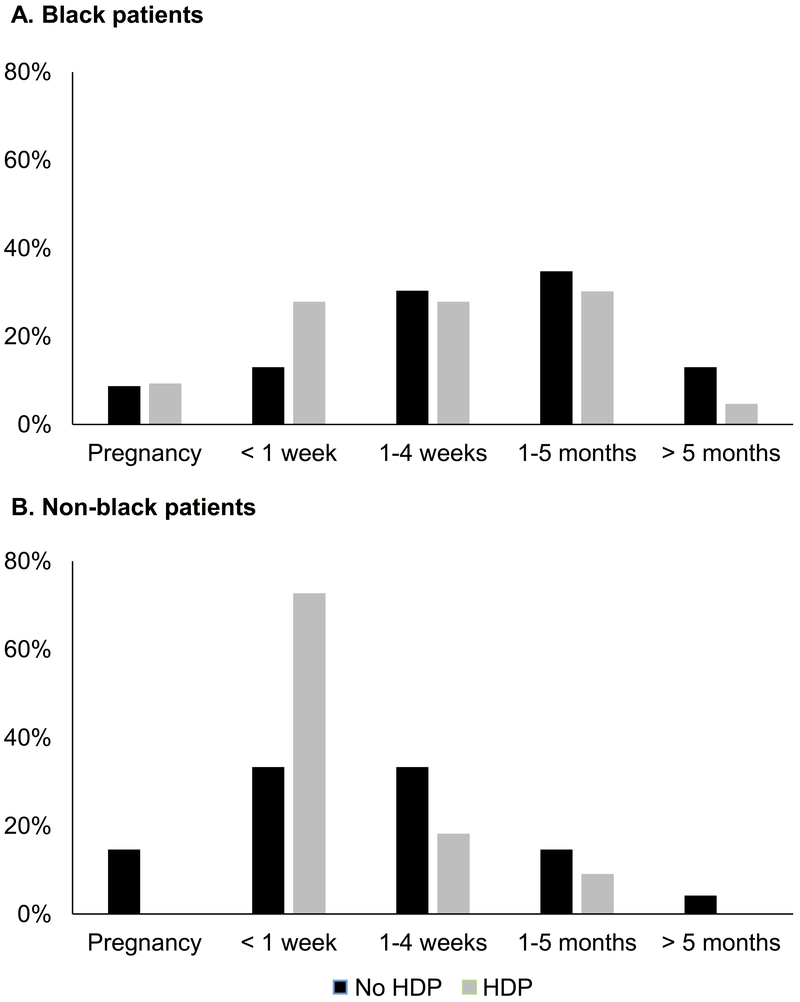
Baseline characteristics of patients with and without HDP stratified by race, are presented in Table 1. Patients with HDP are younger, more likely to be nulliparous, and have twin gestation (known risk factors for HDP). These differences were observed in both black and non-black patients although statistical significance was not reached in the stratified analysis. Chronic hypertension was similar between patients with and without HDP (9.1% vs. 8.2%, p=0.841) but was present almost exclusively in black patients. Both black and non-black patients with HDP were more than twice as likely to be diagnosed in the first week postpartum compared to patients without HDP, as demonstrated in Figure 1. This effect was particularly notable for non-black patients with HDP, among whom 72.7% presented in the first postpartum week. In comparison, only 27.9% of black patients with HDP were diagnosed in the first week after delivery (p=0.0001). There were no non-black patients with HDP diagnosed during pregnancy.
Table 1:
Baseline characteristics stratified by hypertensive disorder of pregnancy and race
| Entire cohort (N=180) | Blacks (N=96) | Non-blacks (N=84) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Characteristic | No HDP | HDP | p value | No HDP | HDP | p value | No HDP | HDP | p value |
| Mean age, years (SD) | 30.4 (5.8) | 28.0 (7.2) | 0.012 | 29.2 (5.5) | 26.0 (7.1) | 0.016 | 31.7 (5.8) | 30.6 (6.5) | 0.442 |
| Age > 30 years, no. (%) n=180 | 54 (54.0) | 28 (35.0) | 0.011 | 20 (40.0) | 11 (23.9) | 0.092 | 34 (68.0) | 17 (50.0) | 0.097 |
| Timing of diagnosis, no. (%) n=170 | |||||||||
| During pregnancy | 11 (11.7) | 4 (5.3) | 0.013 | 4 (8.7) | 4 (9.3) | 0.359 | 7 (14.6) | 0 (0) | 0.006 |
| < 1 week PP | 22 (23.4) | 36 (47.4) | 6 (13.0) | 12 (27.9) | 16 (33.3) | 24 (72.7) | |||
| ≥ 1 week and < 1 month PP | 30 (31.9) | 18 (23.7) | 14 (30.4) | 12 (27.9) | 16 (33.3) | 6 (18.2) | |||
| 1 – 5 months PP | 23 (24.5) | 16 (21.1) | 16 (34.8) | 13 (30.2) | 7 (14.6) | 3 (9.1) | |||
| > 5 months PP | 8 (8.5) | 2 (2.6) | 6 (13.0) | 2 (4.7) | 2 (4.2) | 0 (0) | |||
| Early diagnosis PP, no. (%) n=170 | 63 (67) | 58 (76.3) | 0.183 | 28 (65.1) | 24 (52.2) | 0.216 | 39 (81.3) | 30 (90.9) | 0.229 |
| Chronic hypertension, no. (%) n=172 | 9 (9.1) | 6 (8.2) | 0.841 | 8 (16.0) | 6 (14.3) | 0.820 | 1 (2.0) | 0 (0) | 0.424 |
| Nulliparous, no. (%) n=180 | 45 (45.0) | 48 (60.0) | 0.045 | 20 (40.0) | 25 (54.4) | 0.159 | 25 (50.0) | 23 (67.7) | 0.109 |
| Twin pregnancy, no. (%) n=180 | 8 (8.0) | 14 (17.5) | 0.053 | 2 (4.0) | 4 (8.7) | 0.342 | 6 (12.0) | 10 (29.4) | 0.046 |
| Cesarean delivery, no. (%) n=177 | 50 (51.2) | 50 (63.3) | 0.102 | 24 (49.0) | 25 (55.6) | 0.524 | 26 (53.1) | 25 (73.5) | 0.060 |
| Median EF at diagnosis, % (IQR) n=130 | 30 (15, 40) | 28.8 (21.3, 38.8) | 0.636 | 30 (15, 37.5) | 25 (15, 37.5) | 0.867 | 32.5 (15, 40) | 32.5 (25, 40) | 0.429 |
| EF at diagnosis < 30%, no. (%) n=130 | 34 (48.6) | 30 (50.0) | 0.871 | 16 (48.5) | 21 (63.6) | 0.215 | 18 (48.7) | 9 (33.3) | 0.221 |
Abbreviations: HDP, hypertensive disorder of pregnancy; PP, postpartum; EF, ejection fraction; IQR, intraquartile range
Figure 1:
Timing of diagnosis by hypertensive disorder of pregnancy and race. Timing refers to the postpartum period.
In the 130 patients with complete echocardiographic data at baseline, LVEF at time of diagnosis was similar between patients with and without HDP in the entire cohort (median LVEF 28.8% vs. 30%, p=0.636) with similar rates of EF < 30% documented in the two groups (see Table 1, Figure S1). Among black patients with HDP, 63.6% had a baseline LVEF < 30% whereas only 33.3% of non-black patients with HDP had an LVEF < 30%.
Time to diagnosis baseline characteristics
Patients diagnosed early (during pregnancy or within one month of delivery) trended towards being older and having higher rates of HDP, were more likely to have twin gestation and to undergo Cesarean delivery than women diagnosed later in the postpartum period (see Table 2). In contrast to comparisons based on HDP above, patients with early postpartum diagnosis had a higher median LVEF compared to patients diagnosed one month or later postpartum (30% vs. 22.5%, p=0.041) and more patients in the late diagnosis group had LVEF < 30% (63.2% vs. 44.8%, p=0.054), see Table 2 and Figure S1.
Table 2:
Baseline characteristics stratified by time to diagnosis and race
| Entire cohort (N=193) | Blacks (N=104) | Non-blacks (N=89) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Characteristic | Early | Late | p value | Early | Late | p value | Early | Late | p value |
| Mean age, years (SD) | 30.1 (6.8) | 28.2 (5.8) | 0.073 | 28.3 (6.8) | 27.5 (6.3) | 0.554 | 31.6 (6.5) | 30.5 (3.0) | 0.535 |
| Age > 30 years, no. (%) | 69 (50) | 19 (34.6) | 0.052 | 22 (35.5) | 12 (28.6) | 0.461 | 47 (61.8) | 7 (53.8) | 0.586 |
| Timing of diagnosis, no. (%) | |||||||||
| During pregnancy | 17 (12.3) | 0 | <.0001 | 10 (16.1) | 0 | <.0001 | 7 (9.2) | 0 | <.0001 |
| < 1 week PP | 66 (47.8) | 0 | 22 (35.5) | 0 | 44 (57.9) | 0 | |||
| ≥ 1 week and < 1 month PP | 55 (39.9) | 0 | 30 (48.4) | 0 | 25 (32.9) | 0 | |||
| 1 – 5 months PP | 0 | 44 (80.0) | 0 | 33 (78.6) | 0 | 11 (84.6) | |||
| > 5 months PP | 0 | 11 (20.0) | 0 | 9 (21.4) | 0 | 2 (15.4) | |||
| Hypertensive disorder of pregnancy n=170 | 58 (47.9) | 18 (36.7) | 0.183 | 28 (53.9) | 15 (40.5) | 0.216 | 30 (48.5) | 3 (25.0) | 0.229 |
| Chronic hypertension, no. (%) n=164 | 11 (9.4) | 3 (6.4) | 0.532 | 10 (19.6) | 3 (8.6) | 0.16 | 1 (1.5) | 0 | 0.668 |
| Nulliparous, no. (%) n=193 | 72 (52.2) | 25 (45.5) | 0.399 | 28 (45.2) | 17 (40.5) | 0.636 | 44 (57.9) | 8 (61.5) | 0.805 |
| Twin pregnancy, no. (%) n=192 | 22 (15.9) | 3 (5.6) | 0.054 | 5 (8.1) | 2 (4.9) | 0.529 | 17 (22.4) | 1 (7.7) | 0.224 |
| Cesarean delivery, no. (%) n=188 | 82 (60.3) | 21 (40.4) | 0.014 | 30 (49.2) | 16 (41.0) | 0.425 | 52 (69.3) | 5 (38.5) | 0.032 |
| Median EF at diagnosis, % (IQR) n=143 | 30 (20, 40) | 22.5 (12.5, 37.5) | 0.041 | 27.5 (18.8, 38.8) | 21.3 (12.5, 32.5) | 0.139 | 32.5 (20, 40) | 30 (15, 41.3) | 0.866 |
| EF at diagnosis < 30%, no. (%) n=143 | 47 (44.8) | 24 (63.2) | 0.052 | 24 (54.6) | 20 (66.7) | 0.297 | 23 (37.7) | 4 (50) | 0.503 |
Abbreviations: PP, postpartum; EF, ejection fraction; IQR, intraquartile range
PPCM outcomes
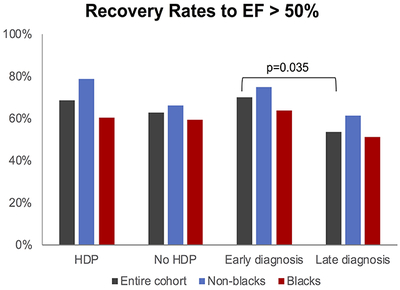
Patients with HDP had similar rates of recovery of LV function compared with patients without HDP (68.4% vs. 62.6%, p=0.425) (Table 3). Black patients demonstrated similar rates of recovery despite HDP status, whereas non-black patients with HDP trended towards having higher rates of recovery (78.8% vs. 66%, p=0.209). Among patients who recovered (n=114), 63.1% had documentation on time to recovery within two years of diagnosis. In this smaller subset, the variability of time to recovery was high and no significant difference existed between those with and without HDP. Rates of adverse outcomes (persistent dysfunction resulting in transplant, LVAD, or death) were low and similar in patients with and without HDP (4% vs. 7.1%, p=0.378).
Table 3:
Recovery outcomes stratified by postpartum time to diagnosis, hypertensive disorder of pregnancy, and race
| HDP (n=175) | Early diagnosis (n=187) | |||||
|---|---|---|---|---|---|---|
| Outcome | Yes | No | p value | Yes | No | p value |
| Recovery of EF ≥ 50%, no. (%) | ||||||
| Entire cohort | 52 (68.4) | 62 (62.6) | 0.425 | 93 (69.9) | 29 (53.7) | 0.035 |
| Blacks | 26 (60.5) | 29 (59.2) | 0.901 | 37 (63.8) | 21 (51.2) | 0.211 |
| Non-blacks | 26 (78.8) | 33 (66.0) | 0.209 | 56 (74.7) | 8 (61.5) | 0.327 |
| Time to Recovery, months (IQR)† | ||||||
| Entire cohort (n=72/114) | 3.5 (2.1, 11.4) | 4.5 (1.3, 9.4) | 0.918 | 4.0 (1.7, 9.6) | 7.0 (5.4, 17.1) | 0.047 |
| Blacks (n=23/55) | 2.9 (1.1, 14.3) | 7.3 (4.5, 10.2) | 0.379 | 4.3 (1.3, 9.3) | 15.7 (8.6, 17.5) | 0.013 |
| Non-blacks (n=49/59) | 3.8 (2.1, 9.8) | 4.0 (1.3, 9.1) | 0.599 | 4.0 (1.7, 9.7) | 5.4 (1.7, 7.0) | 0.886 |
| Transplant, LVAD, or death, no. (%) | ||||||
| Entire cohort | 3 (4.0) | 7 (7.1) | 0.378 | 13 (9.8) | 8 (14.8) | 0.323 |
| Blacks | 2 (4.7) | 3 (6.1) | 0.756 | 7 (12.1) | 6 (14.6) | 0.71 |
| Non-blacks | 1 (3.0) | 4 (8.0) | 0.352 | 6 (8.0) | 2 (15.4) | 0.393 |
Abbreviations: HDP, hypertensive disorder of pregnancy; IQR, interquartile range
Patients with early diagnosis (Table 3) had significantly higher rates of LV recovery (69.9% vs. 53.7%, p=0.035). This trend was consistent in the analysis stratified by race. Patients with early diagnosis had a shorter time to recovery compared to patients with late diagnosis (4 vs. 7 months, p=0.047). This result was driven by differences in time to recovery among black patients (4.3 vs. 15.7 months, p=0.013). Rates of adverse outcomes were similar in patients diagnosed early and late (9.8% vs. 14.8%, p=0.323). In univariate logistic regression analysis, non-black race and early diagnosis were associated with a two-fold increase in odds of LV recovery, whereas baseline LVEF ≥ 30% was associated with an almost 4-fold increase in odds of recovery (Table 4).
Table 4:
Characteristics associated with recovery of LV function
| Characteristic | OR (95% CI) | p value |
|---|---|---|
| Age > 30 years | 1.06 (0.60, 1.85) | 0.851 |
| Non-black race | 1.90 (1.07, 3.37) | 0.029 |
| Early diagnosis | 2.0 (1.05, 3.84) | 0.036 |
| Hypertensive disorder of pregnancy | 1.29 (0.69, 2.43) | 0.426 |
| Chronic hypertension | 0.75 (0.25, 2.22) | 0.604 |
| Nulliparous | 1.76 (1.0, 3.1) | 0.05 |
| Twin pregnancy | 1.79 (0.72, 4.46) | 0.21 |
| Cesarean delivery | 1.01 (0.57, 1.81) | 0.965 |
| Baseline EF ≥ 30% | 3.91 (1.88, 8.15) | 0.0003 |
We performed several sensitivity analyses to confirm the robustness of our findings. First, we repeat our analysis among women with documented preeclampsia and found similar trends. Second, given that our cohort spans 30 years, during which time the standard of heart failure care has evolved, we repeated the analysis stratified by date of diagnosis (diagnosis date prior to 2006 or 2006 and later). Rates of recovery were similar in both cohorts when stratified by HDP and timing of diagnosis.
DISCUSSION
We have made a number of clinically important observations in our analysis. First, women with hypertensive disorders of pregnancy are diagnosed with PPCM earlier in the postpartum period. This effect is largely driven by the very early presentation of nonblack patients. Second, early diagnosis (during or within one month of delivery) is strongly associated with recovery of LV function whereas HDP is not. Finally, early postpartum diagnosis is independently associated with higher baseline LV function, which may represent the mechanism by which early diagnosis mediates improved recovery.
Hypertensive disorders of pregnancy and PPCM outcomes
Prior studies exploring the prognostic impact of preeclampsia or any hypertensive disorder on PPCM outcomes have had mixed results (see Table S1). In a German cohort of 115 patients, HDP were highly prevalent and strongly associated with partial or full recovery of LV function compared to patients without HDP (49% vs. 7%, respectively, p=0.009).9 Similarly in a Japanese cohort of 102 patients, HDP were associated with shorter hospitalization at time of diagnosis and improved LV recovery.10 Studies evaluating black patients in Soweto, South Africa have demonstrated improved PPCM outcomes with higher blood pressure at time of diagnosis but notably these studies excluded women with high blood pressure.14,15
Race may mediate the relationship between preeclampsia and PPCM outcomes and explain why different outcomes are observed in cohorts based on geography and racial composition. In contrast to the German and Japanese cohorts, HDP have not been associated with favorable outcomes in the U.S.-based cohorts (see Table S1). The prospective IPAC cohort of 100 patients (30% black) demonstrated high rates of HDP but no association of HDP with recovery of LV function.11 Goland et al. reported no difference in LV recovery at up to 48 months of follow-up among 187 patients (24% black) with and without HDP.3 A small, predominately black cohort in St. Louis (39 patients, 77% black) found that women with preeclampsia had lower 1-year rates of event-free survival, although among survivors with complete echocardiographic follow-up, women with preeclampsia had significantly higher rates of LV recovery (80% vs. 25%).12
Our study here is one of the largest cohorts to date that addresses the question of how HDP impact outcomes and the first to evaluate the impact of race. We find that HDP are not associated with improved LV recovery. Moreover, this association was maintained in the analysis stratified by race. On the other hand, we observed a number of trends that should be further explored in future analyses with larger populations. Non-black women with HDP were more likely to present in the first week after delivery compared to black women with HDP. Non-black women with HDP also trended towards having higher baseline LV function, an important predictor of LV recovery, compared to women without HDP. Overall rates of LV recovery were similar between women with and without HDP, but recovery rates did trend towards being higher in those with HDP compared to those without among the 76 non-black women (79% vs. 66%, p=0.285), underscoring the notion that different outcomes observed in international cohorts among PPCM women with HDP may be related to differences in racial composition of those cohorts. It is possible that a potentially protective effect of preeclampsia in non-black populations is not present in black patients due to competing factors that adversely impact outcomes, perhaps related to socioeconomic or biological factors.
Time to diagnosis and PPCM outcomes
We have previously shown in this cohort that black women have lower rates of LV recovery and longer time to recovery compared to non-black women. Here, we demonstrated that delayed time to diagnosis postpartum is associated with lower rates of LV recovery. Moreover, this observation was maintained in both black and non-black women, and was independent of HDP status. Thus our study strongly suggests that timing of diagnosis is a key factor in overall outcome. Few studies have explored the relationship between timing of diagnosis and outcomes. In the IPAC cohort, black women were enrolled on average at 42 days postpartum, compared to 26 days for non-black women. Longer time to postpartum diagnosis was significantly associated with worse outcomes in univariate analysis.11 In the St. Louis cohort, Lindley et al demonstrated that none of the women diagnosed during pregnancy experienced LV recovery but did not evaluate timing of postpartum presentation.12
Delayed diagnosis may explain part of the striking differences between outcomes in black versus non-black women with PPCM. Socioeconomic factors can lead to the delayed recognition of heart failure symptoms by patients and/or physicians, leading to delays in the diagnosis and early treatment of PPCM. Adherence to evidence-based medications is lower in vulnerable patient populations and is associated with worse cardiovascular outcomes.18 The initiation of evidence-based therapies such as ACE inhibitors or beta blockers in non-ischemic cardiomyopathy is associated with LV reverse remodeling and even short-term changes in LVEF with medication are associated with prolonged survival.19,20 We previously demonstrated that prescription rates of angiotensin-converting enzymes inhibitors and beta blockers were similar between black and non-black patients in our cohort at time of diagnosis.4 We would expect that women with a delayed diagnosis would also have delayed initiation of these evidence-based therapies, leading to worse LV function at baseline and therefore lower likelihood of recovery. None of the patients in our cohort were treated with bromocriptine.
Limitations
Our study also has limitations. Retrospective cohort data spanning 30 years may have incomplete data capture as patients were treated according to clinician discretion and not all patients had continuous follow-up within the UPHS system. Differences in follow-up frequency between patient groups could contribute to differences in time to recovery. Although our cohort is among the largest in the U.S., our sample size limits our ability to interrogate subgroups for all clinically relevant variables that may impact recovery. Referral bias may be present as sicker patients are more likely to be referred to a major academic medical center. Preeclampsia diagnoses may be underreported and misclassified; for this reason, we used HDP diagnoses more broadly with the assumption that some cases of gestational hypertension may represent preeclampsia. We included patients with a diagnosis of PPCM and LV systolic dysfunction based on echocardiogram reports and documentation in clinical records, but had to exclude some patients due to inability to obtain full reports of all baseline and follow-up echocardiograms. Finally, although we have documentation of medication prescriptions at the time of diagnosis, we do not have more detailed data regarding the duration of treatment, dose titration, or adherence to medications, which may also impact recovery. Despite our study representing the largest clinical PPCM cohort reported in the U.S., we are limited by sample size to generalize potentially important trends observed in the stratified analysis by race. Moving forward, efforts to combine clinical cohorts and create a prospective, longitudinal, and adjudicated PPCM registry should be prioritized in order to better understand how patient characteristics impact prognosis.
CONCLUSION
In a racially diverse cohort of patients with PPCM, early postpartum presentation is strongly associated with recovery of LV function whereas hypertensive disorders of pregnancy are not. Later diagnosis is associated with lower EF at presentation, likely explaining the overall worse outcomes observed in black women. These findings underscore the need for early monitoring and diagnosis, especially in at-risk underserved populations.
PERSPECTIVES
The association between HDP and recovery of LV function in patients with PPCM is not clear. In this racially diverse cohort of women with PPCM, HDP were not associated with improved rates of LV recovery. Receiving a diagnosis of PPCM during pregnancy or within one month after delivery was associated with improved LV recovery compared to patients diagnosed later in the postpartum period. Early diagnosis was associated with higher LVEF, which likely mediates the relationship between late diagnosis and lower recovery rates. Black women are more likely to be diagnosed later in the postpartum period and have lower rates of recovery. Understanding and addressing factors that lead to later diagnosis in this population may lead to improved clinical outcomes.
Supplementary Material
NOVELTY AND SIGNIFICANCE.
What is New?
In a racially diverse cohort of women with peripartum cardiomyopathy (PPCM) living in the U.S., hypertensive disorders of pregnancy were not associated with improved recovery rates.
Early diagnosis (within one month postpartum) was significantly associated with improved recovery compared to late diagnosis. This trend was consistent among black and non-black patients.
Patients with late diagnosis had a lower ejection fraction (EF) at time of presentation, which likely mediates the relationship between late diagnosis and lower recovery rates.
What is Relevant?
Earlier diagnosis of PPCM in black women may prevent the worse clinical outcomes currently observed in this population. Cardiac symptoms in women with PPCM risk factors should lead to prompt evaluation.
Controversy exists in the literature about the association of HDP and PPCM recovery. Our study contributes to the growing literature in the U.S. demonstrating that women with PPCM do not experience improved recovery rates, differential effects based on race and geography may exist.
Summary
Recovery rates of PPCM in the U.S. are high but a significant proportion of women still develop severe cardiomyopathy or adverse outcomes. Black women are diagnosed significantly later than white women and have worse rates of recovery. Improving the early monitoring and diagnosis of PPCM in at-risk women may improve clinical outcomes in traditionally underserved populations.
Acknowledgments
Sources of Funding: This study was supported by the NIH CTSA SPIRIT award and grants K12HD085848 (Dr. Lewey) and R01HL126797 (Dr. Arany) from the National Institutes of Health.
Footnotes
Disclosures: No conflicts of interest to disclose
REFERENCES
- 1.Arany Z, Elkayam U. Peripartum Cardiomyopathy. Circulation. 2016. April 5;133(14):1397–1409. [DOI] [PubMed] [Google Scholar]
- 2.Gunderson EP, Croen LA, Chiang V, Yoshida CK, Walton D, Go AS. Epidemiology of peripartum cardiomyopathy: incidence, predictors, and outcomes. Obstet Gynecol. 2011. September;118(3):583–591. [DOI] [PubMed] [Google Scholar]
- 3.Goland S, Bitar F, Modi K, Safirstein J, Ro A, Mirocha J, Khatri N, Elkayam U. Evaluation of the clinical relevance of baseline left ventricular ejection fraction as a predictor of recovery or persistence of severe dysfunction in women in the United States with peripartum cardiomyopathy. J Card Fail. 2011. May;17(5):426–430. [DOI] [PubMed] [Google Scholar]
- 4.Irizarry OC, Levine LD, Lewey J, Boyer T, Riis V, Elovitz MA, Arany Z. Comparison of Clinical Characteristics and Outcomes of Peripartum Cardiomyopathy Between African American and Non-African American Women. JAMA Cardiol. 2017. November 1;2(11):1256–1260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Myatt L, Clifton RG, Roberts JM, Spong CY, Hauth JC, Varner MW, Thorp JM, Mercer BM, Peaceman AM, Ramin SM, Carpenter MW, Iams JD, Sciscione A, Harper M, Tolosa JE, Saade G, Sorokin Y, Anderson GD. First-Trimester Prediction of Preeclampsia in Low-Risk Nulliparous Women. Obstet Gynecol. 2012. June;119(6):1234–1242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bello N, Hurtado Rendon IS, Arany Z. The Relationship Between Preeclampsia and Peripartum Cardiomyopathy: A Systematic Review and Meta-Analysis. J Am Coll Cardiol. 2013. October 29;62(18):1715–1723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Patten IS, Rana S, Shahul S, Rowe GC, Jang C, Liu L, Hacker MR, Rhee JS, Mitchell J, Mahmood F, Hess P, Farrell C, Koulisis N, Khankin EV, Burke SD, Tudorache I, Bauersachs J, Monte F del, Hilfiker-Kleiner D, Karumanchi SA, Arany Z. Cardiac angiogenic imbalance leads to peripartum cardiomyopathy. Nature. 2012. May;485(7398):333–338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Powe CE, Levine RJ, Karumanchi SA. Preeclampsia, a disease of the maternal endothelium: the role of anti-angiogenic factors and implications for later cardiovascular disease. Circulation [Internet]. 2011. June 21 [cited 2018 Sep 10];123(24). Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3148781/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Haghikia A, Podewski E, Libhaber E, Labidi S, Fischer D, Roentgen P, Tsikas D, Jordan J, Lichtinghagen R, von Kaisenberg CS, Struman I, Bovy N, Sliwa K, Bauersachs J, Hilfiker-Kleiner D. Phenotyping and outcome on contemporary management in a German cohort of patients with peripartum cardiomyopathy. Basic Res Cardiol [Internet]. 2013. July [cited 2018 Aug 23];108(4). Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3709080/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kamiya CA, Kitakaze M, Ishibashi-Ueda H, Nakatani S, Murohara T, Tomoike H, Ikeda T. Different characteristics of peripartum cardiomyopathy between patients complicated with and without hypertensive disorders. -Results from the Japanese Nationwide survey of peripartum cardiomyopathy-. Circ J Off J Jpn Circ Soc. 2011;75(8):1975–1981. [DOI] [PubMed] [Google Scholar]
- 11.McNamara DM, Elkayam U, Alharethi R, Damp J, Hsich E, Ewald G, Modi K, Alexis JD, Ramani GV, Semigran MJ, Haythe J, Markham DW, Marek J, Gorcsan J, Wu W-C, Lin Y, Halder I, Pisarcik J, Cooper LT, Fett JD. Clinical Outcomes for Peripartum Cardiomyopathy in North America. J Am Coll Cardiol. 2015. August;66(8):905–914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lindley KJ, Conner SN, Cahill AG, Novak E, Mann DL. Impact of Pre-Eclampsia on Clinical and Functional Outcomes in Women with Peripartum Cardiomyopathy. Circ Heart Fail [Internet]. 2017. June [cited 2018 Aug 20];10(6). Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5520674/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Modi KA, Illum S, Jariatul K, Caldito G, Reddy PC. Poor outcome of indigent patients with peripartum cardiomyopathy in the United States. Am J Obstet Gynecol. 2009. August;201(2):171.e1–171.e5. [DOI] [PubMed] [Google Scholar]
- 14.Blauwet LA, Libhaber E, Forster O, Tibazarwa K, Mebazaa A, Hilfiker-Kleiner D, Sliwa K. Predictors of outcome in 176 South African patients with peripartum cardiomyopathy. Heart Br Card Soc. 2013. March;99(5):308–313. [DOI] [PubMed] [Google Scholar]
- 15.Sliwa K, Förster O, Libhaber E, Fett JD, Sundstrom JB, Hilfiker-Kleiner D, Ansari AA. Peripartum cardiomyopathy: inflammatory markers as predictors of outcome in 100 prospectively studied patients. Eur Heart J. 2006. February 1;27(4):441–446. [DOI] [PubMed] [Google Scholar]
- 16.Fett JD, Sannon H, Thélisma E, Sprunger T, Suresh V. Recovery from severe heart failure following peripartum cardiomyopathy. Int J Gynaecol Obstet Off Organ Int Fed Gynaecol Obstet. 2009. February;104(2):125–127. [DOI] [PubMed] [Google Scholar]
- 17.Sliwa K, Hilfiker-Kleiner D, Petrie MC, Mebazaa A, Pieske B, Buchmann E, Regitz-Zagrosek V, Schaufelberger M, Tavazzi L, van Veldhuisen DJ, Watkins H, Shah AJ, Seferovic PM, Elkayam U, Pankuweit S, Papp Z, Mouquet F, McMurray JJV, Heart Failure Association of the European Society of Cardiology Working Group on Peripartum Cardiomyopathy. Current state of knowledge on aetiology, diagnosis, management, and therapy of peripartum cardiomyopathy: a position statement from the Heart Failure Association of the European Society of Cardiology Working Group on peripartum cardiomyopathy. Eur J Heart Fail. 2010. August;12(8):767–778. [DOI] [PubMed] [Google Scholar]
- 18.Lewey J, Choudhry NK. The current state of ethnic and racial disparities in cardiovascular care: lessons from the past and opportunities for the future. Curr Cardiol Rep. 2014;16(10):530. [DOI] [PubMed] [Google Scholar]
- 19.Packer M, Bristow MR, Cohn JN, Colucci WS, Fowler MB, Gilbert EM, Shusterman NH. The Effect of Carvedilol on Morbidity and Mortality in Patients with Chronic Heart Failure. N Engl J Med. 1996. May 23;334(21):1349–1355. [DOI] [PubMed] [Google Scholar]
- 20.Kramer DG, Trikalinos TA, Kent DM, Antonopoulos GV, Konstam MA, Udelson JE. Quantitative evaluation of drug or device effects on ventricular remodeling as predictors of therapeutic effects on mortality in patients with heart failure and reduced ejection fraction: a meta-analytic approach. J Am Coll Cardiol. 2010. July 27;56(5):392–406. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.