Abstract
Background:
Biomechanical studies have shown double-bundle (DB) anterior cruciate ligament reconstruction (ACLR) to have increased anterior and rotational stability as compared with single-bundle ACLR. Various techniques exist to drill the femoral tunnel, such as anteromedial portal (AMP), outside-in (OI), and transtibial (TT) drilling. However, it is unclear whether one drilling technique is superior to others when a DB graft is used.
Purpose:
To systematically assess the outcomes and complications in patients undergoing DB ACLR through an AMP technique as compared with other femoral drilling techniques.
Study Design:
Systematic review; Level of evidence, 3.
Methods:
PubMed, Medline, and EMBASE databases were searched in April 2018. Nonrandomized studies were assessed with the MINORS (Methodological Index for Nonrandomized Studies), whereas randomized studies were assessed with the GRADE (Grading of Recommendations Assessment, Development and Evaluation) system.
Results:
Ten studies comprising 722 patients satisfied the inclusion criteria. A total of 351 patients underwent DB ACLR with AMP drilling (mean ± SD age, 32.7 ± 4.7 years); 318 patients had DB ACLR with OI drilling (age, 31.9 ± 4.1 years); and 53 received a DB ACLR with TT drilling (age, 26.5 ± 2.0 years). Graft types used included hamstring autograft (74.1%; n = 247), tibialis anterior autograft (6.0%; n = 20) and unspecified grafts (19.8%; n = 66). No significant difference in postoperative Tegner and Lysholm scores was found between the AMP and OI groups postoperatively. The AMP group had a lower anterior and posterior graft bending angle as compared with the OI group. Four patients (1.1%) in the AMP group had graft reruptures, as compared with 9 reruptures (2.8%) in the OI group. There were no reports of rerupture in the TT group.
Conclusion:
DB AMP ACLR results in significantly improved functional outcome scores postoperatively. AMP techniques yield similar functional outcomes to OI ACLR. No direct comparison in functional outcomes scores were available between the AMP and TT techniques. Low overall complication and revision rates were observed for patients undergoing DB AMP ACLR and were found to be similar to those of other femoral drilling techniques. Owing to a steeper graft bending angle in patients undergoing OI or TT ACLR relative to AMP ACLR, patients treated with OI or TT femoral drilling may have increased strain placed on the graft. Based on the various limitations in the available literature, it is not currently possible to make a definite conclusion of whether AMP is superior to non-AMP techniques in the setting of DB ACLR.
Keywords: double-bundle, anterior cruciate ligament, anteromedial portal, outside-in, knee
The anterior cruciate ligament (ACL) consists of 2 bundles, the anteromedial (AM) and posterolateral (PL) bundles, with the AM bundle acting as the primary restraint against anterior tibial translation whereas the PL bundle stabilizes the knee against rotatory forces.3,26 Rupturing the ACL is a devastating injury, as it can cause functional impairments6 and increase the lifetime risk of knee osteoarthritis.21 Recently, there has been a steady increase in popularity for anatomic ACL reconstructions (ACLRs) as an accurate way to restore native ACL positioning and biomechanical characteristics.11
Single-bundle (SB) and double-bundle (DB) ACLR techniques have been associated with positive functional outcomes.4,27 SB ACLRs aim to restore only the AM bundle of the ACLR, whereas DB ACLR uses 2 grafts to re-create the AM and PL bundles.36 Many biomechanical studies have indicated that DB ACLR has increased anterior and rotational stability as compared with SB ACLR.29 However, prognostic studies have shown that there are no significant differences in clinical outcomes between the reconstruction techniques.10
There are various options when considering how to drill the femoral tunnel during surgery. ACLR initially evolved from a 2-incision technique with an outside-in (OI) femoral drilling technique to a transtibial (TT) technique wherein the ACL femoral tunnel is drilled through a tibial tunnel.31 The OI technique is useful, especially in revision settings, as it may allow the creation of longer tunnels, oblique tunnels of a wider range of angles, more consistent femoral tunnel placement, and clearer fields of vision allowing for easier femoral drilling. However, the OI technique has been associated with more acute graft bending angles (GBAs) leading to potentially poorer graft healing and greater risk of rerupture.20 TT techniques are associated with less surgical pain and morbidity and reduced operative time.28 Some disadvantages of TT ACLR include increased interference screw bone divergence with damage to the graft during fixation.28 Newer techniques allow for independent drilling of the femoral tunnel through the AM portal (AMP).28 The AMP technique allows for a more accurate and anatomic placement of the ACL femoral tunnel, while theoretically improving anteroposterior and rotational stability.28 However, the drilling technique can be technically demanding for those not familiar with it and has an increased risk of injury to the common peroneal nerve.28
There has been extensive research comparing drilling techniques in SB ACLR. In a recent systematic review of 479 patients, the authors reported that SB ACLR with the AMP technique yields superior stability and improved postoperative functional outcomes as compared with TT techniques.5 In another meta-analysis, the SB ACLR AMP technique had better Lysholm scores and a larger proportion of knees with normal International Knee Documentation Committee (IKDC) grade as compared with patients treated with TT drilling.28 However, to date, there have been no systematic reviews that have critically compared various femoral drilling techniques in DB ACLR. Hence, the purpose of this study was to systematically assess the outcomes and complications in patients undergoing DB ACLR through the AMP as compared with other femoral drilling techniques. The hypothesis was that DP AMP ACLR would provide superior outcomes and lower rerupture rates to TT and OI in the same population.
Methods
Search Strategy
Three online databases (PubMed, Embase, and MEDLINE) were searched for studies comparing AMP femoral tunnel drilling with other non-AMP femoral drilling techniques for skeletally mature patients from data inception to April 24, 2018. The search terms included “anterior cruciate ligament,” “anterior cruciate ligament reconstruction,” “double-bundle,” “anteromedial portal,” and similar phrases (Appendix Table A1). The search terms were entered onto Google Scholar to ensure that articles were not missed. The research question and inclusion and exclusion criteria were established a priori. Inclusion criteria were (1) comparative studies (ie, AMP vs non-AMP drilling techniques; OI, TT, etc), (2) skeletally mature patients (ie, closed femoral and tibial physis), (3) DB reconstruction, (4) outcomes reported and stratified for population of interest, (5) human studies, and (6) English language. Exclusion criteria included (1) multiligament knee reconstruction, (2) partial tears treated with ACL augmentation, (3) review articles, (4) nonsurgical treatment studies (eg, conservative treatment, technique articles without outcomes), (5) case reports, (6) SB reconstruction, and (7) cadaveric/nonhuman studies.
Study Screening
A systematic screening approach in accordance with PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses)22 and R-AMSTAR (Revised Assessment of Multiple Systematic Reviews)15 was employed from the title to full-text screening stages in duplicate by 2 independent reviewers (T.T., A.G.). Discrepancies were discussed and resolved with input by a third reviewer. The references of included studies were also screened through the same systematic approach to capture any additional relevant articles.
Quality Assessment
Using the Journal of Bone & Joint Surgery classification system for literature in the field of orthopaedics, the level of evidence (1-4) for each study was determined by the 2 reviewers independently and in duplicate.35 The methodological quality of nonrandomized comparative studies was evaluated with the MINORS (Methodological Index for Nonrandomized Studies) checklist.30 A score of 0, 1, or 2 is given for each of the 12 items on the MINORS checklist, with a maximum score of 16 for noncomparative studies and 24 for comparative studies. Methodological quality was categorized a priori as follows for noncomparative and comparative studies, respectively: a score of 0-8 or 0-12 was considered poor quality; 9-12 or 13-18, fair quality; and 13-16 or 19-24, excellent quality.
Risk of bias in randomized controlled trials was assessed with the GRADE (Grading of Recommendations Assessment, Development and Evaluation) system.8 The GRADE tool begins its assessment by rating randomized controlled trials as high quality of evidence and observational studies as low quality. These studies are then evaluated via 5 factors associated with the quality of evidence: risk of bias, inconsistency, indirectness, imprecision, and publication bias.1,9
Data Abstraction
The 2 reviewers then independently abstracted relevant data from included articles and recorded the data onto a Google spreadsheet designed a priori. Demographic data included author, year of publication, sample size, study design and location, level of evidence, and patient demographics (eg, sex, age). Information was documented regarding rehabilitation protocols and postoperative outcomes (surgical and radiographic), including complications.
Statistical Analysis
Given the inconsistent reporting of outcomes, a meta-analysis could not be performed, and the results are summarized descriptively. Descriptive statistics, such as mean, range, and measures of variance (eg, standard deviations, 95% CIs), are presented where applicable. The intraclass correlation coefficient (ICC) was used to evaluate interreviewer agreement for the MINORS score. A kappa (κ) statistic was used to evaluate interreviewer agreement at all screening stages. Agreement was categorized a priori as follows: ICC/κ of 0.81-0.99 was considered almost perfect agreement; ICC/κ of 0.61-0.80, substantial agreement; ICC/κ of 0.41-0.60, moderate agreement; ICC/κ of 0.21-0.40, fair agreement; and a ICC/κ of ≤0.20 was considered slight agreement.17
Results
Study Characteristics
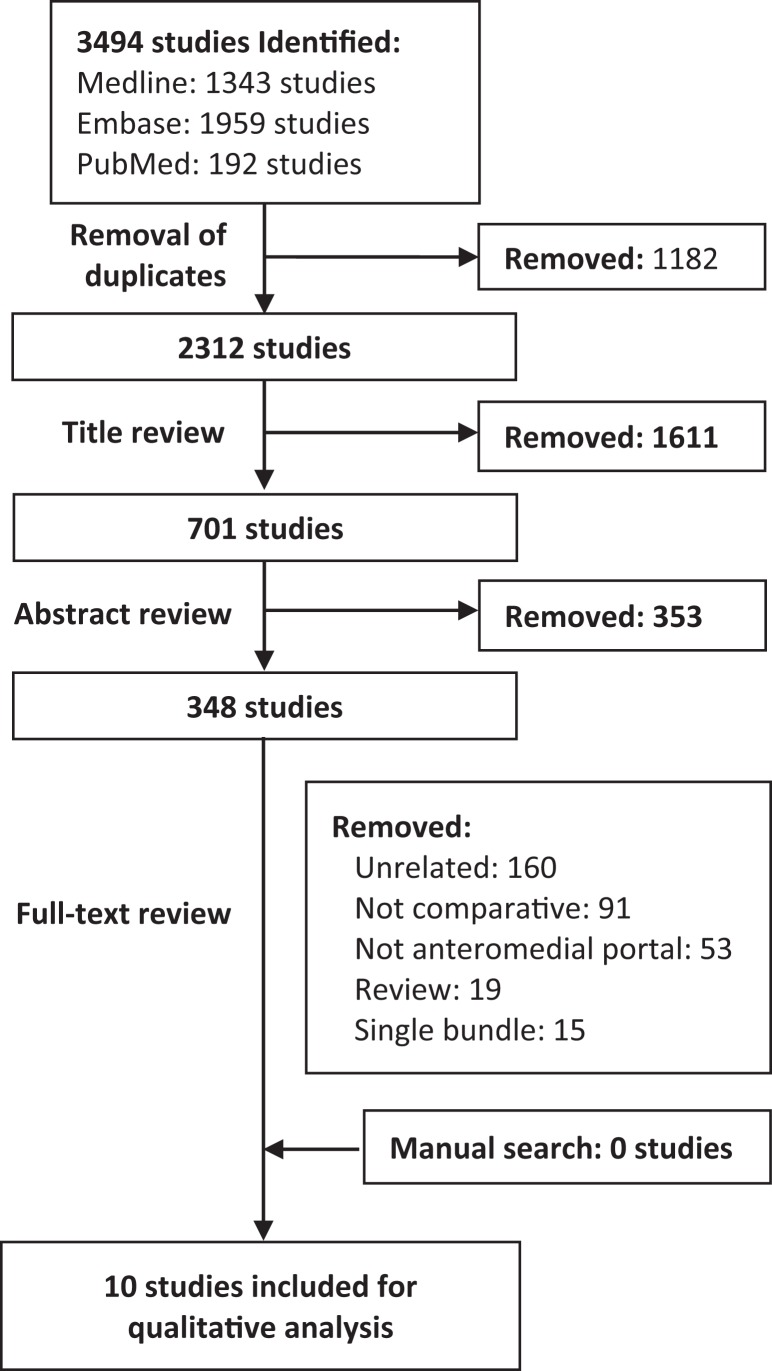
The initial search yielded a total of 3494 articles. After 1182 duplicates were excluded, a systematic screening process yielded 10 articles that met inclusion (Figure 1). There were no additional studies found upon reviewing references of included studies or a manual search through Google Scholar. Of the included studies, there was 6 randomized controlled trials, 2 prospective cohorts, and 2 retrospective cohorts. The included studies were conducted in South Korea (60%; n = 6) and Japan (40%; n = 4) (Table 1).
Figure 1.
PRISMA (Preferred Reporting Items for Systematic Meta-Analyses) flow diagram.
TABLE 1.
Study Characteristics and Methodological Qualitya
| Sample Size, n | AMP and Control, Mean ± SD (Range) | ||||||
|---|---|---|---|---|---|---|---|
| Lead Author (Year) | Study Design (LOE) | Total | Study (AMP), n | Control, n | Age, y | Follow-up | Study Qualityb |
| Kim (2018)11 | RCT (2) | 111 | 53 | 58 | GRADE: low | ||
| AMP | 36.4 ± 10.1 (20-60) | 34.9 ± 10.9 mo | |||||
| Control | 35.0 ± 10.1 (20-60) | 34.9 ± 10.9 mo | |||||
| Lee (2017)19 | RCT (1) | 80 | 40 | 40 | GRADE: moderate | ||
| AMP | 33.2 ± 8.3 | 29.5 mo | |||||
| Control | 35.4 ± 11.2 | 29.5 mo | |||||
| Kyung (2013)16 | RCT (2) | 76 | 38 | 38 | GRADE: low | ||
| AMP | 37.4 ± 11.4 | 2-6 d | |||||
| Control | 33.4 ± 10.6 | 2-6 d | |||||
| Kim (2012)13 | RCT (1) | 34 | 18 | 18 | GRADE: low | ||
| AMP | 36.7 ± 10.3 (18-47) | NR | |||||
| Control | 30.0 ± 12.2 (17-54) | NR | |||||
| Kim (2013)12 | RCT (1) | 80 | 40 | 40 | GRADE: low | ||
| AMP | 36.5 ± 10.1 (17-49) | 3 d | |||||
| Control | 31.0 ± 11.7 (18-54) | 3 d | |||||
| Lee (2015)18 | RCT (1) | 64 | 33 | 33 | GRADE: low | ||
| AMP | 32.0 ± 8.3 (20-45) | 3 d | |||||
| Control | 34.5 ± 11.0 (20-60) | 3 d | |||||
| Takeda (2013)32 | Prospective cohort (2) | 50 | 25 | 25 | MINORS: 19 of 24 | ||
| AMP | 27.7 (15-47) | 1 wk | |||||
| Control | 27.8 (15-48) | 1 wk | |||||
| Niki (2017)24 | Prospective cohort (3) | 64 | 32 | 32 | MINORS: 17 of 24 | ||
| AMP | 27.5 ± 6.3 | 2.5 y | |||||
| Control | 25.7 ± 10.9 | 3.3 y | |||||
| Nakamae (2012)23 | Retrospective cohort (3) | 50 | 28 | 22 | MINORS: 17 of 24 | ||
| AMP | 27.8 ± 12.1 | 26.1 ± 4.5 mo | |||||
| Control | 25.1 ± 9.6 | 26.1 ± 4.5 mo | |||||
| Tomihara (2014)34 | Retrospective cohort (3) | 55 | 25 | 30 | MINORS: 17 of 24 | ||
| AMP | 25.1 ± 9.8 | 1 wk | |||||
| Control | 25.1 ± 10.0 | 1 wk | |||||
aAMP, anteromedial portal; GRADE, Grading of Recommendations Assessment, Development and Evaluation; LOE, level of evidence; MINORS, Methodological Index for Non-Randomized Studies; NR, not reported; RCT, randomized controlled trial.
bThrough compiled MINORS rating, all nonrandomized comparative studies were scored from 0 to 24. Risk of bias in randomized studies was evaluated with the GRADE tool.
Study Quality
There was substantial agreement among reviewers at the title (κ = 0.865; 95% CI, 0.841-0.889) and abstract (κ = 0.650; 95% CI, 0.593-0.706) screening stages and almost perfect agreement after full-text screening (κ = 0.761; 95% CI, 0.685-0.837). The mean (± SD) MINORS score across all nonrandomized studies was 17.5 ± 1, indicating fair quality of evidence for nonrandomized studies. The risk of bias across all randomized studies was low to moderate (Appendix Table A2). There was almost perfect agreement among the reviewers for the quality assessment based on the MINORS criteria (weighted ICC = 0.953; 95% CI, 0.924-0.971) (Table 1).
Patient Characteristics
There were 722 patients in the included studies. Among the patients, 48.6% (n = 351) were enrolled in an AMP group, whereas 51.3% (n = 371) of patients were assigned to a non-AMP group. Of the 371 patients who underwent non-AMP ACLR, 85.7% (n = 318) received an OI technique, whereas only 14.3% (n = 53) received a TT technique. Furthermore, 73.1% (245 of 335) of patients in the AMP group were male, while 76.7% (247 of 322) of the patients in the non-AMP group were male. The mean age of the patients in the AMP group was 32.7 ± 4.7 years (range, 15-60 years) with a mean follow-up time of 39.1 months. The mean age of the patients in the OI group was 31.9 ± 4.1 years (range, 17-60 years) with a mean follow-up time of 42.9 months. The mean age of the patients in the TT group was 26.5 ± 2.0 years (range, 15-48 years) with a mean follow-up time of 22 months. Overall, 92.6% of patients (n = 669 of 722) were available at final follow-up (Table 1).
Surgical Technicalities
In this systematic review, all studies performed a DB-ACLR comparing AMP techniques with either OI ACLR or TT ACLR.
The graft choice for AMP ACLR included a 6-stranded (triple semitendinosus and triple gracilis) autograft (51.9%; n = 173), semitendinosus tendon autograft (13.2%; n = 44), unspecified hamstring autograft (9.0%; n = 30), and tibialis anterior allograft (6.0%; n = 20). Two studies (19.8%; n = 66) did not specify which type of graft was used.
The graft choice for OI ACLR included a 6-stranded (triple semitendinosus and triple gracilis) autograft (53.9%; n = 156), unspecified hamstring autograft (8.7%; n = 25), tibialis anterior allograft (6.9%; n = 20), and semitendinosus tendon autograft (6.2%; n = 18). Two studies (24.2%; n = 70) did not specify which type of graft was used.
The graft choice for TT ACLR included a 6-stranded (triple semitendinosus and triple gracilis) autograft (53.2%; n = 25) and semitendinosus tendon autografts (46.8%; n = 22) (Table 2).
TABLE 2.
Surgical Techniquesa
| Lead Author (Year): Drilling | Graft Choice | Graft Fixation | Tunnel Locations | |
|---|---|---|---|---|
| Femoral | Tibial | |||
| Kim (2018)11 | ||||
| AMP (n = 53) | Autograft hamstring tendon (n = 43), allograft tibialis anterior (n = 10) | Bioabsorbable interference screw | Bioabsorbable interference screw | Femoral: center of femoral insertion site (via accessory AMP). Tibial: remnant tibial insertion site |
| OI (n = 58) | Same as AMP | NR | NR | Femoral: same as AMP (except via central midpatellar portal). Tibial: same as AMP (except via central midpatellar portal) |
| Lee (2017)19 | ||||
| AMP (n = 40) | Autograft hamstring tendons, allograft tibialis anterior | NR | NR | Femoral: lateral cortex near lateral femoral condyle (via accessory AMP). Tibial: remnant tibial insertion site |
| OI (n = 40) | Same as AMP | NR | NR | Femoral: same as AMP (except via central midpatellar portal). Tibial: same as AMP (except via central midpatellar portal) |
| Kyung (2013)16 | ||||
| AMP (n = 38) |
Autograft hamstring tendon, allograft tibialis anterior | Cortical suspensory device | Bioabsorbable interference screw | Femoral: lateral cortex near lateral femoral condyle (via accessory AMP). Tibial: footprint defined by ACL remnant or bony landmarks |
| OI (n = 38) |
Same as AMP | Same as AMP | Same as AMP | Femoral: same as AMP (except via central midpatellar portal). Tibial: same as AMP (except via central midpatellar portal) |
| Kim (2012)13 | ||||
| AMP (n = 21) |
Autograft hamstring tendon, allograft tibialis anterior | Endobutton | Bioabsorbable interference screw | Femoral: lateral cortex near lateral femoral condyle (via accessory AMP). Tibial: remnant tibial insertion site |
| OI (n = 18) | Same as AMP | Retrobutton | Same as AMP | Femoral: same as AMP (except via central midpatellar portal). Tibial: same as AMP (except via central midpatellar portal) |
| Kim (2013)12 | ||||
| AMP (n = 40) |
Autograft hamstring tendon | NR | NR | Femoral: lateral cortex near lateral femoral condyle (via accessory AMP). Tibial: NR |
| OI (n = 40) | Same as AMP | NR | NR | Femoral: lateral cortex near lateral femoral condyle (via accessory AMP). Tibial: NR |
| Lee (2015)18 | ||||
| AMP (n = 31) |
Autograft hamstring tendon, allograft tibialis anterior | Cortical suspension system | Bioabsorbable interference screw | Femoral: 2 mm from posterior bony ridge of lateral femoral condyle and 3-4 mm posterior from PL corner of intercondylar notch (AM bundle) / 5 mm anterior to the joint cartilage on a line perpendicular to the tangent at the lowest point of the lateral femoral condyle (PL bundle) (both via accessory AMP). Tibial: remnant tibial insertion sites |
| OI (n = 33) | Same as AMP | Same as AMP | Same as AMP | Femoral: same as AMP (except via central midpatellar portal). Tibial: same as AMP |
| Takeda (2013)32 | ||||
| AMP (n = 25) |
Autogenous doubled semitendinosus, gracilis tendons. | Endobutton | Double-spike plate | Femoral: 6 mm anterior (high) to the posterior margin of the osteochondral junction at 90° of flexion to the lateral aspect of the thigh (PL bundle) / same as the PL bundle except drilled at “1:30” (vs “10:30”) with respect to resident’s ridge posterior cortex midpoint (AM bundle). Tibial: 8 mm anterior from retroeminence ridge (PL bundle) / 8 mm AM from retroeminence ridge (AM bundle) |
| TT (n = 25) | Same as AMP | Same as AMP | Same as AMP | Femoral: same as AMP except via PL bundle tibial tunnel (PL bundle) / same as AMP except via AM bundle tibial tunnel (AM bundle). Tibial: 1 cm anterior from anterior medial collateral ligament (PL bundle) / same as AMP AM bundle (AM bundle) |
| Niki (2017)24 | ||||
| AMP (n = 32) |
Semitendinosus tendon | Ligament tensioner | Double-spike plate | Femoral: posterior to intercondylar ridge to center of footprint (via AMP). Tibial: NR |
| OI (n = 32) | Same as AMP | Same as AMP | Same as AMP | Femoral: ACL set at insertion angle of 50° for AM bundle and 40° for PL bundle in relation to the joint line and drilled through lateral femoral cortex. Tibial: NR |
| Nakamae (2012)23 | ||||
| AMP (n = 28) |
Semitendinosus, gracilis tendons | Endobutton | Endobutton | Femoral: drilled through lateral femoral condyle (via far AMP). Tibial: NR |
| TT (n = 22) | Same as AMP | Same as AMP | Same as AMP | Femoral: posterior half of ACL insertion drilled via tibial tunnel. Tibial: posterior half of tibial attachment to ACL |
| Tomihara (2014)34 | ||||
| AMP (n = 25) |
Autogenous hamstring graft | Endobutton | Double-spike plate | Femur: above lateral meniscus (via far AMP). Tibial: anterior edge of medial collateral ligament to medial edge of tibial tubercle |
| OI (n = 30) | Same as AMP | Same as AMP | Same as AMP | Femur: lateral thigh to femoral lateral condyle. Tibial: Same as AMP |
aACL, anterior cruciate ligament; AM, anteromedial; AMP, anteromedial portal; NR, not reported; OI, outside-in; PL, posterolateral; TT, transtibial.
Graft Sizes
The mean overall graft length was 16.24 cm (n = 335).
Rehabilitation Protocol
Two studies reported rehabilitation protocols.11,19 One study reported partial weightbearing at 4 weeks with crutches and an increase in knee flexion range of motion to 120º at 4 weeks.11 At postoperative 6 weeks, patients were allowed full weightbearing with a brace.11 The other study reported use of an ACL limited-motion brace applied 4 to 5 days after surgery, and joint motion exercise was carried out at 15° increments per week.19 A pair of crutches was used to allow partial weightbearing from 3 days to 6 weeks after surgery. Patients were educated on performing proprioceptive balancing exercises at 3 months after surgery. Return to competitive sports involving jumping, pivoting, or sidestepping was prohibited until 6 months after the reconstruction.19
Functional Outcome Scores
The Tegner activity score was measured in 53 patients in the AMP group.11 A significant within-group increase in Tegner activity score was observed (P < .05). The Tegner activity score was measured in 58 patients in the OI group.11 A significant within-group increase in Tegner activity score was observed (P < .05). No significant differences in outcomes were noted between techniques. The Lysholm score was measured in 85 patients in the AMP group.11,19 A significant within-group increase in Lysholm score was observed in 1 study (P < .05). The Lysholm score was measured in 107 patients in the OI group.11,19 A significant within-group increase in Lysholm score was observed in 1 study (P < .05). No significant differences in outcomes were noted between techniques. No studies compared functional outcomes scores between AMP and TT.
Rotational Stability
Pivot shift was measured in 107 patients in the AMP group.11,23,24 The percentage of patients with pivot-shift results of glide or greater was 85.8% (n = 54) preoperatively and 12.1% (n = 13) postoperatively.
Pivot shift was measured in 3 studies (n = 90 patients) in the OI group.11,23,24 The percentage of patients with pivot-shift results of glide or greater was 91.4% (n = 53)4 preoperatively and 12.2% (n = 11) postoperatively.11,24 No studies reported postoperative pivot shift as an outcome in TT groups.
Radiographic Outcomes
The radiographic outcomes reported in the included studies are summarized in Appendix Table A3. In all cases, the GBA was measured by computed tomography. The AM GBA was found to decrease from 110.8º (95% CI, 110.2°-111.4°; n = 52) at 3 days postoperatively13,18 to 73.8º (SD, 11.2°; n = 32) 2 years postoperatively in patients who underwent ACLR with the AMP technique.24 This contrasts with patients who underwent ACLR with the OI technique, where it decreased from 101.3º (95% CI, 100.5°-102.1°; n = 51)13,18 at 3 days postoperatively to 90.7º (SD, 8.8°; n = 32) at 2 years postoperatively.24 No studies reported GBA measured by computed tomography as an outcome in TT.
Complications
The overall complication rate was 3.2% (n = 23). The following complications were reported in the AMP group (n = 351): 1.1% were reruptures (n = 4); 1.1% were gaps between the Endobutton and cortex (n = 4); and 0.5% were button slippages in the tunnel (n = 2).11,19
The following complications were reported in the OI group (n = 318): 2.8% were reruptures (n = 9); 0.3% was infection (n = 1); 0.003% were gaps between the button and cortex (n = 1); and 0.6% were button slippages in the tunnel (n = 2).11,19
No complications were reported in the TT group (n = 53), and the reoperation rate was 0%.
Discussion
The most important finding of this systematic review is that DB AMP ACLR has similar subjective and objective outcomes as well as a similar complication profile in comparison with non-AMP techniques. Furthermore, radiographic studies revealed a greater decrease in the GBA with time in the AMP group versus the OI group.
It has recently been proposed that a steep GBA may be a biomechanical factor that contributes to graft damage. In ACLR, sharp angulation of the graft at the tunnel aperture increases the local strain and abrasive forces, and repetitive bending may cause excessive stress on the bone-graft interface, slowing down the rate of graft healing.33 The generally more horizontal tunnels created in the OI ACLR technique create a steep angle, which may increase graft wear.28 In this systematic review, the GBA was reported only for patients who underwent OI drilling and AMP drilling. At 2 years postoperatively, the GBA for OI and AMP was 90.7º and 73.8º, respectively. In another study, the GBA in the TT technique was significantly larger than that of the AMP technique at low flexion angles when the graft was fully stretched.25 Anatomic ACLR leads to a more oblique femoral tunnel orientation, resulting in an ACL graft that bends at a less acute angle at the femoral tunnel aperture.33 However, the GBA is just one of many factors, such as tunnel positioning, the shape of the intercondylar fossa, graft selection, and graft tension, that likely plays a role in graft rupture. Unfortunately, the majority of the studies did not include information on these other possible confounders to allow us to comment on their impact on graft rupture rates with different drilling techniques.
AMP ACLR allows for a more anatomic graft position as compared with TT ACLR, which may play a role in decreasing rerupture rates. Femoral tunnels performed through the AMP are more precise and closer to the anatomic femoral ACL insertion as compared with the TT drilling, allowing for a more horizontal placement.7 It has been identified that in TT ACLR techniques, a vertical and anterior graft placement is required owing to drilling through the tibial tunnel, increasing biomechanical demand during rehabilitation.28
There were very few complications reported by the studies included in this systematic review, likely in large part because of the small sample sizes. For this reason, accurate comparison in rerupture rates and complication rates between the femoral tunnel drilling techniques was difficult. In general when using an AMP drilling technique, surgeons must be cognizant of the possibility of a short tunnel length.2 AMP ACLR techniques provide for a more oblique femoral tunnel position to improve the rotational stability. However, this more oblique tunnel position significantly decreases the femoral tunnel length and can cause difficulties such as the risk of unintentionally penetrating the outer cortex. Additionally, a number of studies have shown that the DB AMP technique can result in posterior-wall blowout and potential damage to the posterior articular cartilage.14 Complications involved in the TT drilling technique include interference screw–bone plug divergence in the femoral tunnel, damage to the graft during fixation, and graft-tunnel length mismatch.14 OI techniques have a greater risk of abrasion of the graft at the intra-articular edges of the tunnels.14
Strengths
The strengths of this systematic review stem from the rigorous methodology used. The use of multiple databases, a broad search strategy, and a duplicate systematic approach to reviewing the literature ensured that relevant articles were not overlooked. Excellent agreement at all screening stages and quality assessment were obtained.
Limitations
Despite the included studies being comparative in nature, their statistical and methodological heterogeneity (eg, follow-up period, outcome measures reported) precluded a meta-analysis. There is also a need for more consistent reporting in outcomes across studies of all drilling techniques to make more definitive analyses. The studies that were included in this review were also limited in their generalizability, as all of the patients were from Asia.
Future studies should use large prospective cohorts and randomized controlled trials with long-term follow-up to further assess the results presented in this review. Ideally, future studies would have more consistent reporting of important information, such as functional outcome scores, objective anterior and rotational stability testing, and tunnel positioning, which was found to be often lacking in the currently available literature.
Conclusion
DB AMP ACLR results in significantly improved functional outcome scores postoperatively. AMP techniques yield similar functional outcomes to OI ACLR. No direct comparison in functional outcomes scores was available between AMP and TT techniques. Low overall complication and revision rates were observed for patients undergoing DB AMP ACLR and were found to be similar to those of other femoral drilling techniques. Given a steeper GBA in patients undergoing OI or TT ACLR relative to AMP ACLR, patients treated with OI or TT femoral drilling may have increased strain placed on the graft. Based on the various limitations in the currently available literature, it was not possible to make a definitive conclusion on whether AMP is superior to non-AMP techniques in the setting of DB ACLR.
Appendix
TABLE A1.
Search Strategy
| Studies | ||
|---|---|---|
| MEDLINE (n = 1343) | Embase (n = 1959) | PubMed (n = 192) |
| Strategy: 1. anterior cruciate ligament.mp. or exp anterior cruciate ligament/ 2. anterior cruciate ligament reconstruction.mp. or exp anterior cruciate ligament reconstruction/ 3. double bundle.mp. 4. anteromedial portal.mp. 5. transportal.mp. 6. anatomic.mp. 7. 1 or 2 8. 3 or 4 or 5 or 6 9. 7 and 8 10. limit 9 to (human and English language) |
Strategy: 1. anterior cruciate ligament.mp. or exp anterior cruciate ligament/ 2. anterior cruciate ligament reconstruction.mp. or exp anterior cruciate ligament reconstruction/ 3. double bundle.mp. 4. anteromedial portal.mp. 5. transportal.mp. 6. anatomic.mp. 7. 1 or 2 8. 3 or 4 or 5 or 6 9. 7 and 8 10. limit 9 to (human and English language) |
Strategy: Search (((anterior cruciate ligament OR anterior cruciate ligament reconstruction)) AND (double bundle OR anteromedial portal OR anatomic or Transportal)) AND (“2017/04/24”[Date - Publication] : “3000”[Date - Publication]) |
TABLE A2.
Quality Assessment of Randomized Controlled Trials With the GRADE Toola
| Primary Author (Year) | Risk of Bias | Inconsistency | Indirectness | Imprecision | Publication Bias | Overall Score |
|---|---|---|---|---|---|---|
| Kim (2018)11 | 0 | 0 | 0 | 0 | 0 | Low |
| Lee (2017)19 | 0 | 0 | –1 | 0 | 0 | Moderate |
| Kyung (2013)16 | 0 | 0 | 0 | 0 | 0 | Low |
| Kim (2012)13 | 0 | 0 | 0 | 0 | 0 | Low |
| Kim (2013)12 | 0 | 0 | 0 | 0 | 0 | Low |
| Lee (2015)18 | 0 | 0 | 0 | 0 | 0 | Low |
a–2, very serious; –1, serious; 0, no risk of bias. GRADE, Grading of Recommendations Assessment, Development and Evaluation.
TABLE A3.
Radiographic Outcomesa
| AMP | OI | |||
|---|---|---|---|---|
| Anteromedial femoral graft bending angle (measured by CT) | ||||
| 3 d: 110.8º (95% CI, 110.2º-111.4º; n = 52) |
2 y: 73.8º (SD, 11.2º; n = 32) |
3 d: 101.3º (95% CI, 100.5º-102.1º; n = 51) |
2 y: 90.7º (SD, 8.8º; n = 32) |
|
| Posterolateral femoral graft bending angle (measured by CT) | ||||
| 3 d: 110.3º (95% CI, 110.2º-110.4º; n = 52) |
2 y: 65.2º (SD, 8.1º; n = 32) |
3 d: 101.5º (95% CI, 100.7º-102.4º; n = 51) |
2 y: 76.6º (SD, 5.5º; n = 32) |
|
| AM femoral tunnel length | ||||
| 3 d: 31.4 mm (95% CI, 31.3-31.5; n = 61) |
2 y: 32.9 mm (95% CI, 32.8-33.1; n = 54) |
3 d: 37.4 mm (95% CI, 36.9-38.0; n = 58) |
2 y: 37.2 mm (SD, 5.7; n = 32) |
|
| PL femoral tunnel length | ||||
| 3 d: 34.1 mm (95% CI, 34.1-34.2; n = 61) |
2 y: 30.4 mm (SD, 3.9; n = 32) |
3 d: 38.2 mm (95% CI, 37.7-38.6; n = 51) |
2 y: 32.8 mm (SD, 5.7; n = 32) |
|
| Tunnel divergent angle | ||||
| 3 d: 7.6º (95% CI, 6.7º-8.3º; n = 46) |
2 y: 11.4º (SD, 6.1º; n = 32) |
3 d: 7.4º (SD, 6.7º; n = 18) |
1 wk: 5.1º (range, 2.3º-8.1º; n = 30) |
2 y: 13.5º (SD, 6.7º; n = 32) |
| AM femoral tunnel (coronal) angle | ||||
| 3 d: 74.3º (SD, 5.1º; n = 38) |
2 y: 52.3º (95% CI, 48.3º-56.3º; n = 50) |
3 d: 73.3º (SD, 2.9º; n = 38) |
1 wk: 69.6º (range, 57.5º-81.8º; n = 30) |
|
| PL femoral tunnel (coronal) angle | ||||
| 3 d: 74.3º (SD, 5.1º; n = 38) |
2 y: 42.7º (95% CI, 38.5º-46.9º; n = 50) |
3 d: 65.8º (SD, 5.9º; n = 38) |
1 wk: 61.1º (range, 48.8º-78.4º; n = 30) |
|
| AM femoral tunnel (sagittal) angle | ||||
| 3 d: 55.0º (SD, 3.1º; n = 38) |
2 y: 43.6º (95% CI, 40.0º-47.1º; n = 50) |
3 d: 53.5º (SD, 4.0º; n = 38) |
1 wk: 55.1º (range, 45.2º-69.8º; n = 30) |
|
| PL femoral tunnel (sagittal) angle | ||||
| 3 d: 55.0º (SD, 3.1º; n = 38) |
2 y: 43.6º (95% CI, 40.0º-47.1º; n = 50) |
3 d: 53.3º (SD, 6.1º; n = 38) |
1 wk: 51.2º (range, 42.4º-68.4º; n = 30) |
|
aDays, weeks, and years are postoperative. AM, anteromedial; AMP, anteromedial portal; CT, computed tomography; OI, outside-in; PL, posterolateral.
Footnotes
One or more of the authors has declared the following potential conflict of interest or source of funding: O.R.A. has received educational consulting fees from Conmed and Smith & Nephew. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
References
- 1. Balshem H, Helfand M, Schünemann HJ, et al. GRADE guidelines: 3. Rating the quality of evidence. J Clin Epidemiol. 2011;64(4):401–406. [DOI] [PubMed] [Google Scholar]
- 2. Bedi A, Raphael B, Maderazo A, Pavlov H, Williams RJ. Transtibial versus anteromedial portal drilling for anterior cruciate ligament reconstruction: a cadaveric study of femoral tunnel length and obliquity. Arthroscopy. 2010;26:342–350. [DOI] [PubMed] [Google Scholar]
- 3. Benedetto PD, Benedetto ED, Fiocchi A, Beltrame A, Causero A. Causes of failure of anterior cruciate ligament reconstruction and revision surgical strategies. Knee Surg Relat Res. 2016;28:319–324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Chen G, Wang S. Comparison of single-bundle versus double-bundle anterior cruciate ligament reconstruction after a minimum of 3-year follow-up: a meta-analysis of randomized controlled trials. Int J Clin Exp Med. 2015;8(9):14604–14614. [PMC free article] [PubMed] [Google Scholar]
- 5. Chen H, Tie K, Qi Y, Li B, Chen B, Chen L. Anteromedial versus transtibial technique in single-bundle autologous hamstring ACL reconstruction: a meta-analysis of prospective randomized controlled trials. J Orthop Surg Res. 2017;12(1):167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Czuppon S, Racette BA, Klein SE, Harris-Hayes M. Variables associated with return to sport following anterior cruciate ligament reconstruction: a systematic review. Br J Sports Med. 2014;48(5):356–364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Gavriilidis I, Motsis EK, Pakos EE, Georgoulis AD, Mitsionis G, Xenakis TA. Transtibial versus anteromedial portal of the femoral tunnel in ACL reconstruction: a cadaveric study. Knee. 2008;15:364–367. [DOI] [PubMed] [Google Scholar]
- 8. Guyatt G, Oxman AD, Akl EA, et al. GRADE guidelines: 1. Introduction: GRADE evidence profiles and summary of findings tables. J Clin Epidemiol. 2011;64:383–394. [DOI] [PubMed] [Google Scholar]
- 9. Guyatt GH, Oxman AD, Vist G, et al. GRADE guidelines: 4. Rating the quality of evidence. Study limitations (risk of bias). J Clin Epidemiol. 2011;64(4):407–415. [DOI] [PubMed] [Google Scholar]
- 10. Ha J-K, Lee D-W, Kim J-G. Single-bundle versus double-bundle anterior cruciate ligament reconstruction: a comparative study with propensity score matching. Indian J Orthop. 2016;50:505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Kim JG, Kang SH, Kim JH, Lim CO, Wang JH. Comparison of clinical results, second-look arthroscopic findings, and MRI findings between the transportal and outside-in techniques for double-bundle anatomic anterior cruciate ligament reconstruction: a prospective, randomized controlled trial with a minimum 2-year follow-up. Am J Sports Med. 2018;46:544–556. [DOI] [PubMed] [Google Scholar]
- 12. Kim JG, Wang JH, Ahn JH, Kim HJ, Lim HC. Comparison of femoral tunnel length between transportal and retrograde reaming outside-in techniques in anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2013;21:830–838. [DOI] [PubMed] [Google Scholar]
- 13. Kim JG, Wang JH, Lim HC, Ahn JH. Femoral graft bending angle and femoral tunnel geometry of transportal and outside-in techniques in anterior cruciate ligament reconstruction: an in vivo 3-dimensional computed tomography analysis. Arthroscopy. 2012;28:1682–1694. [DOI] [PubMed] [Google Scholar]
- 14. Kim KI, Lee SH, Bae C, Bae SH. Three-dimensional reconstruction computed tomography evaluation of the tunnel location and angle in anatomic single-bundle anterior cruciate ligament reconstruction: a comparison of the anteromedial portal and outside-in techniques. Knee Surg Relat Res. 2017;29:11–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Kung J, Chiappelli F, Cajulis OO, et al. From systematic reviews to clinical recommendations for evidence-based health care: validation of Revised Assessment of Multiple Systematic Reviews (R-AMSTAR) for grading of clinical relevance. Open Dent J. 2010;4:84–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Kyung BS, Kim JG, Chang M, et al. Anatomic double-bundle reconstruction techniques result in graft obliquities that closely mimic the native anterior cruciate ligament anatomy. Am J Sports Med. 2013;41:1302–1309. [DOI] [PubMed] [Google Scholar]
- 17. Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33:159. [PubMed] [Google Scholar]
- 18. Lee BH, Bansal S, Park SH, Wang JH. Eccentric graft positioning within the femoral tunnel aperture in anatomic double-bundle anterior cruciate ligament reconstruction using the transportal and outside-in techniques. Am J Sports Med. 2015;43:1180–1188. [DOI] [PubMed] [Google Scholar]
- 19. Lee BH, Jangir R, Kim HY, et al. Comparison of anterior cruciate ligament volume after anatomic double-bundle anterior cruciate ligament reconstruction. Knee. 2017;24:580–587. [DOI] [PubMed] [Google Scholar]
- 20. Lee D, Kim J, Lee J, Park J, Kim D. Comparison of modified transtibial and outside-in techniques in anatomic single-bundle anterior cruciate ligament reconstruction. Arthroscopy. 2018;34:2857–2870. [DOI] [PubMed] [Google Scholar]
- 21. Mather RC, Koenig L, Kocher MS, et al. Societal and economic impact of anterior cruciate ligament tears. J Bone Joint Surg Am. 2013;95:1751–1759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Moher D, Shamseer L, Clarke M, et al. Preferred Reporting Items for Systematic Review and Meta-analysis Protocols (PRISMA-P) 2015 statement. Syst Rev. 2015;4:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Nakamae A, Ochi M, Adachi N, Deie M, Nakasa T. Clinical comparisons between the transtibial technique and the far anteromedial portal technique for posterolateral femoral tunnel drilling in anatomic double-bundle anterior cruciate ligament reconstruction. Arthroscopy. 2012;28:658–666. [DOI] [PubMed] [Google Scholar]
- 24. Niki Y, Nagai K, Harato K, Suda Y, Nakamura M, Matsumoto M. Effects of femoral bone tunnel characteristics on graft-bending angle in double-bundle anterior cruciate ligament reconstruction: a comparison of the outside-in and transportal techniques. Knee Surg Sports Traumatol Arthrosc. 2017;25:1191–1198. [DOI] [PubMed] [Google Scholar]
- 25. Nishimoto K, Kuroda R, Mizuno K, et al. Analysis of the graft bending angle at the femoral tunnel aperture in anatomic double bundle anterior cruciate ligament reconstruction: a comparison of the transtibial and the far anteromedial portal technique. Knee Surg Sports Traumatol Arthrosc. 2009;17(3):270–276. [DOI] [PubMed] [Google Scholar]
- 26. Petersen W, Zantop T. Anatomy of the anterior cruciate ligament with regard to its two bundles. Clin Orthop Relat Res. 2007;454:35–47. [DOI] [PubMed] [Google Scholar]
- 27. Ro KH, Kim HJ, Lee DH. The transportal technique shows better clinical results than the transtibial techniques for single-bundle anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2018;26:2371–2380. [DOI] [PubMed] [Google Scholar]
- 28. Robin BN, Jani SS, Marvil SC, Reid JB, Schillhammer CK, Lubowitz JH. Advantages and disadvantages of transtibial, anteromedial portal, and outside-in femoral tunnel drilling in single-bundle anterior cruciate ligament reconstruction: a systematic review. Arthroscopy. 2015;31(7):1412–1417. [DOI] [PubMed] [Google Scholar]
- 29. Seon JK, Gadikota HR, Wu J-L, Sutton K, Gill TJ, Li G. Comparison of single- and double-bundle anterior cruciate ligament reconstructions in restoration of knee kinematics and anterior cruciate ligament forces. Am J Sports Med. 2010;38:1359–1367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Slim K, Nini E, Forestier D, Kwiatkowski F, Panis Y, Chipponi J. Methodological index for non-randomized studies (MINORS): development and validation of a new instrument. ANZ J Surg. 2003;73:712–716. [DOI] [PubMed] [Google Scholar]
- 31. Sukur E, Akman YE, Senel A, Unkar EA, Topcu HN, Ozturkmen AY. Comparing transtibial and anteromedial drilling techniques for single-bundle anterior cruciate ligament reconstruction. Open Orthop J. 2016;10:481–489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Takeda Y, Iwame T, Takasago T, et al. Comparison of tunnel orientation between transtibial and anteromedial portal techniques for anatomic double-bundle anterior cruciate ligament reconstruction using 3-dimensional computed tomography. Arthroscopy. 2013;29:195–204. [DOI] [PubMed] [Google Scholar]
- 33. Tashiro Y, Gale T, Sundaram V, et al. The graft bending angle can affect early graft healing after anterior cruciate ligament reconstruction: in vivo analysis with 2 years’ follow-up. Am J Sports Med. 2017;45:1829–1836. [DOI] [PubMed] [Google Scholar]
- 34. Tomihara T, Yoshida G, Hara Y, Taniuchi M, Shimada N. Transparent 3-dimensional CT in evaluation of femoral bone tunnel communication after ACL double-bundle reconstruction: comparison between outside-in and transportal technique. Knee Surg Sports Traumatol Arthrosc. 2014;22:1563–1572. [DOI] [PubMed] [Google Scholar]
- 35. Wright JG, Swiontkowski MF, Heckman JD. Introducing levels of evidence to the journal. J Bone Joint Surg Am. 2003;85(1):1–3. [PubMed] [Google Scholar]
- 36. Zhang H, Qiu M, Zhou A, Zhang J, Jiang D. Anatomic anterolateral ligament reconstruction improves postoperative clinical outcomes combined with anatomic anterior cruciate ligament reconstruction. J Sports Sci Med. 2016;15:688–696. [PMC free article] [PubMed] [Google Scholar]