Abstract
Background. Safe opioid prescribing and effective pain care are particularly important issues in the United States, where decades of widespread opioid prescribing have contributed to high rates of opioid use disorder. Because of the importance of clinician-patient communication in effective pain care and recent initiatives to curb rising opioid overdose deaths, this study sought to understand how clinicians and patients communicate about the risks, benefits, and goals of opioid therapy during primary care visits. Methods. We recruited clinicians and patients from six primary care clinics across three health systems in the Midwest United States. We audio-recorded 30 unique patients currently receiving opioids for chronic noncancer pain from 12 clinicians. We systematically analyzed transcribed, clinic visits to identify emergent themes. Results. Twenty of the 30 patient participants were females. Several patients had multiple pain diagnoses, with the most common diagnoses being osteoarthritis (n = 10), spondylosis (n = 6), and low back pain (n = 5). We identified five themes: 1) communication about individual-level and population-level risks, 2) communication about policies or clinical guidelines related to opioids, 3) communication about the limited effectiveness of opioids for chronic pain conditions, 4) communication about nonopioid therapies for chronic pain, and 5) communication about the goal of the opioid tapering. Conclusions. Clinicians discuss opioid-related risks in varying ways during patient visits, which may differentially affect patient experiences. Our findings may inform the development and use of more standardized approaches to discussing opioids during primary care visits.
Keywords: chronic pain, clinical practice guidelines, opioid prescribing, risk communication
Chronic pain and opioid use disorder present enormous public health challenges to the US health care system. Estimates of chronic pain prevalence range from 25 to 100 million US adults.1,2 Pain contributes an estimated $600 billion in health care costs and lost worker productivity annually.2 Between 1999 and 2015, health care providers quadrupled their prescribing of opioid pain relievers, while overdose deaths increased dramatically.3 In 2017, over 47,000 people died in the United States from opioid overdoses.4 Importantly, primary care clinicians prescribe nearly half of all dispensed opioid prescriptions.5 To help combat opioid-related risks, the Centers for Disease Control and Prevention (CDC) published the 2016 Guideline for Prescribing Opioids for Chronic Pain that targets primary care treatment of chronic noncancer pain.6
Reflected in the CDC Guideline and other opioid prescribing best practices is the need for clinicians to regularly assess, and talk with their patients about, opioid-related risks, benefits, and treatment goals when considering or managing chronic opioid therapy. However, because primary care clinicians are often caring for multiple patient conditions during short clinic visits,7–9 it is unclear how accurately or comprehensively clinicians discuss opioid-related risks, benefits, and goals with their patients. At the same time, accurate and comprehensive communication is important to ensure that patients understand opioid-related health risks and benefits, and that clinicians and patients have a common understanding of appropriate treatment goals. Indeed, prior research has found that patients may have inaccurate perceptions of opioid-related risks and benefits,8,10 and patients and clinicians may not share the same outcome goals.11
Given the importance of effective primary care communication to achieve safe and guideline-concordant opioid prescribing, the purpose of this study was to describe how clinicians communicate about risks, benefits, and goals of opioid therapy during primary care visits. This knowledge may help identify communication deficits in patient-clinician interactions about opioid-related risks, benefits, and goals of opioid therapy. This knowledge may also aid in developing policy, education, and other interventions that increase safe and patient-centered pain care.
Methods
We conducted an observational study that analyzed audio recordings of clinic visits between primary care clinicians and patients with chronic noncancer musculoskeletal pain who were receiving opioids. This study, which focuses on patients receiving opioids, is part of a larger study to understand clinical decision making for chronic pain care, including care that does not involve opioids. We analyzed clinic visits occurring between May 2016 and May 2017. The Indiana University Institutional Review Board approved this study. A complete Consolidated Criteria for Reporting Qualitative Research checklist (COREQ) for our study can be found in Appendix 1.
Population and Sample
We recruited primary care clinicians from three health care systems in Indiana and Illinois. Eligible clinicians included physicians, physician assistants, and nurse practitioners who prescribe opioids. We purposefully recruited participants to obtain a sample that was diverse in practice type and location, clinician age, race/ethnicity, and sex. We also sought to have a diverse representation among the patients, including variations in age, race/ethnicity, sex, and complexity of pain condition. We recruited clinicians using e-mail invitations, in-person presentations at clinic staff meetings, and word-of-mouth. Next, we identified patient participants based on medical record review and recommendations from recruited clinicians. We deliberately sought patient diversity by recruiting from health clinics that serve diverse patient populations. Eligible patients were required to speak English, have a current chronic musculoskeletal pain condition, have no history of cancer in the 3 years before their visit, and currently receiving opioids. Because our larger study also recruited patients not currently receiving opioids, we identified patients with current opioid prescriptions by reviewing transcripts of their clinic visits.
Before we approached the patients, their primary care clinician confirmed their eligibility as a patient with chronic noncancer musculoskeletal pain. Both clinician and patient participants provided written informed consent to participate in the study. Patient participants were compensated with a $25 gift card for their time in the study.
Procedure
After notifying their primary care providers, a member of our research team approached eligible patients in clinic waiting areas or the exam room before scheduled visits. Patients were given sufficient time to read the consent form and ask any clarifying questions of the recruiter. After obtaining informed consent, the researcher placed an audio recorder in the exam room to capture all auditory interactions between the patient and primary care clinician. After the visit, the audio recorder was removed, and the audio file was transferred to a secure computer server. Next, a professional transcriptionist transcribed the audio recordings. Research team members de-identified each of the transcripts before analysis.
Analysis
We used a combination of deductive and inductive analytical approaches to explore patterns and themes related to clinicians’ descriptions of risks, benefits, and goals of opioid therapy during visits with patients.12,13 First, to ground our analysis in established clinical practice recommendations, we used a deductive or “top-down” approach to develop a codebook based on a subset of CDC Guideline recommendations that focus on communication about opioid-related risks, benefits, and goals of opioid therapy.6 Specifically, the Guideline recommends “. . . clinicians should establish treatment goals with all patients, including realistic goals for pain and function . . .” (Recommendation 1) and “. . . clinicians should discuss with patients known risks and realistic benefits of opioid therapy . . .” (Recommendation 2). The codebook included the following codes: 1 risks—utterances about current or potential for negative health effects of opioids; 2) benefits—utterances about current or potential positive health effects of opioids; and 3) goals—utterances about desired changes to pain therapy being utilized and/or utterances about the intended health effects of using opioids.
Second, two experienced and trained coders (ECD and OM) individually applied our initial codes to each clinic visit transcript in Dedoose qualitative analysis software Version 7.7.6.14 The coders then met to discuss the fit of the codebook and adjusted codes as needed, resulting in a revised coding template. During this process, we also used an inductive or “bottom-up” approach to describe new categories of meaningful data and make modifications to the codebook.12 For example, during this process, we divided the benefits code into two parts. The first code captured utterances about the positive health effects of opioids. The second code captured utterances about the lack of positive health effects of opioids.
Next, the two coders independently applied the codes from the modified codebook. The codes were applied at the utterance level, and codes were not mutually exclusive.15 The coders met after the first transcript and periodically thereafter to discuss coding differences and reach consensus. After coding all transcripts, each coder individually analyzed the coded text for patterns and themes, using the overarching research questions as a guide.16 During analysis, the coders met periodically to review emerging themes and reconcile any disagreements. We finished collecting and analyzing additional transcripts after two rounds of coding. Initially, we included and coded 24 transcripts. Next, we included six additional transcripts to determine whether any new themes emerged and if our emerging themes were consistent in the new transcripts. When no new themes emerged in the second round of coding, we concluded our data collection.
Finally, to ensure our analysis captured patients’ responses and interactions with their clinicians, we further examined the transcript excerpts within each theme. This process generated additional codes focused on patients’ responses. Two coders individually identified patient response–related codes, met to compare codes and reach consensus, and then applied these codes to all transcripts. The coders met and reviewed each excerpt until they reached consensus.
Throughout our data analysis we used several established qualitative methodology procedures to ensure rigor and validity of our findings. Specifically, we practiced reflexivity by continually questioning interpretations of data and becoming aware of one’s own preconceptions and biases. We also actively sought out the depth of description (seeking out rich, particular details of participants’ words) and searched for alternative explanations of the data.17–19
Results
Overview of Patients, Clinicians, and Visits
We analyzed 30 clinic visits across 3 health systems, 2 not-for-profit and 1 academic. The clinic visits took place across 6 clinics, with 21 visits at urban clinics and 9 at rural clinics. The clinic visits involved 11 physicians and 1 family nurse practitioner. Clinicians’ specialty included family medicine (n = 8), internal medicine (n = 3), and general medicine (n = 1). Clinicians’ experience ranged from 2 to 30 years of practice. Half of the clinicians were female; 9 identified as white, 2 identified as African American, and 1 identified as Asian.
Twenty of the 30 patient participants identified as female. Several patients had multiple pain diagnoses (as reported by their clinician following the visit), with the most common diagnoses being osteoarthritis (n = 10), spondylosis (n = 6), low back pain (n = 5), radiculopathy (n = 5), and spinal stenosis (n = 4). Additional information about study participants is located in Table 1.
Table 1.
Description of Clinician (n = 12) and Patient (n = 30) Samples
| Urban Clinics | Rural Clinics | |
|---|---|---|
| Clinicians, n (n = 12) | ||
| Sex | ||
| Female | 5 | 1 |
| Male | 4 | 2 |
| Race | ||
| White | 6 | 3 |
| African American | 2 | 0 |
| Asian | 1 | 0 |
| Specialty | ||
| Family medicine | 5 | 3 |
| Internal medicine | 3 | 0 |
| General Medicine | 1 | 0 |
| Years of practice | ||
| <10 | 2 | 2 |
| 10–20 | 6 | 0 |
| >20 | 1 | 1 |
| System type | ||
| Not-for-profit | 8 | 3 |
| Academic | 1 | 0 |
| Patients, n (n = 30) | ||
| Sex | ||
| Female | 17 | 3 |
| Male | 4 | 6 |
| Race | ||
| White | 13 | 9 |
| African American | 8 | 0 |
| Age, years | ||
| 18–30 | 0 | 1 |
| 31–40 | 4 | 1 |
| 41–50 | 3 | 0 |
| 51–60 | 6 | 4 |
| 61–70 | 6 | 2 |
| 71+ | 2 | 1 |
| Paina | ||
| Diagnoses | ||
| Osteoarthritis | 7 | 3 |
| Spondylosis | 6 | 0 |
| Low back pain | 2 | 3 |
| Radiculopathy | 2 | 3 |
| Spinal Stenosis | 4 | 0 |
| Fibromyalgia | 2 | 1 |
| Rheumatoid arthritis | 2 | 0 |
| Location(s) | ||
| Spine | 16 | 2 |
| Knee | 6 | 1 |
| Shoulder | 2 | 2 |
| Hip | 2 | 1 |
Some patients had multiple pain diagnoses and pain locations. As a result, totals shown are more than the number of patients.
Nearly all clinicians had discussions related to risk, benefits, or goals of opioid therapy. Discussions included five themes in clinician communication about risks, benefits, and goals of chronic opioid therapy. Patient responses to clinician utterances generally fell into three main categories: listening, agreeing, and providing or asking for more information about a topic.
Communication About Individual-Level and Population-Level Risks
Clinicians varied in their opioid-related risk utterances, sometimes describing individual (i.e., patient-specific) risk factors and/or sometimes describing population-level risk statistics. A few clinicians described individual-level risk factors and negative outcomes associated with opioid use (e.g., comorbid disease or fall risk) specific to the patient. In some instances, clinicians described individual-level risk factors as rationale for recommending reduction or discontinuation of opioids. In this example, a clinician described how a patient’s comorbid condition, chronic obstructive pulmonary disease (COPD), when combined with opioids, may increase the severity of respiratory suppression:
Clinician 3: . . . we do not want you on the narcotics a long time. The thing that you are getting is one of the side effects is that it can suppress breathing. So you already have COPD you have enough trouble breathing just with your COPD.
Patient 5: I breathe a lot better now that I quit smoking though.
Some clinicians also described opioid-related risks at the population level. For example, clinicians referenced current rates of opioid addiction or overdose. These risks referred to someone other than the patient. For example, this clinician communicated opioid-related mortality statistics:
Clinician 6: . . . when people are on long-term pain medicine, and things are getting tighter and tighter as you know, it is hard because people are dying. We have almost 100 people a day dying of narcotic overdose every day. It is actually, I have not been able to talk to _____ at the school today . . . for years and years, the number one cause of death in teenagers has always been car crashes. In the last 6 years, opioid overdose. So teenagers in America today are more likely to die of an opioid overdose than a car crash.
Patient 18: I do understand that.
In response to individual and population-level risk comments, some patients listened to the information provided through short responses to the clinician, similar to the quote above. We also saw some patients agreeing and/or requesting additional information about the risks as well as providing some of their own information to the risk discussion like Patient 5 who has COPD. Patient 5 provides more information about how her recent lifestyle change has made it easier for her to breathe.
Communication About Policies or New Practices Related to Opioids
Some clinicians also described current opioid policies or changes to prescribing to their patients. Most of these clinicians worked in the same health care system. In nearly all cases, this discussion occurred in the context of opioid dose reduction or discontinuation. For example, this clinician described the CDC Guideline for Prescribing Opioids for Chronic Pain and suggested that the patient’s current dose was too high6:
Clinician 6: . . . Cause we’re kind of . . . I think I showed you before, the CDC came out with some guidelines and we’re kind of exceeding those. We’ve got dose . . . of course you’re a big guy and everything like that.
Another clinician described her health system’s policy that recommends limiting opioid prescriptions:
Clinician 3: Now at HEALTH SYSTEM really doesn’t want us writing more than 2 pain pills a day. If we said we were going to reduce these from 4 to 3, do you think you would still manage or how would that be for you?
Patient 5: No that wouldn’t work. That just wouldn’t work. I know we talked about that last time.
In most circumstances, clinicians referenced policies or changes in common practice to introduce the topic of tapering or as support for the decision to taper. Many patients listened to clinicians’ explanations about opioid policies and practices and were occasionally not given a chance to respond or confirmed with short responses, such as “I’m listening” and “I understand.”
Communication About the Limited Effectiveness of Opioids for Chronic Pain Conditions
Some clinicians described opioids as medications that can reduce pain in the short-term but not provide long-term benefit for patients’ underlying pain conditions. These utterances often occurred in the context of discussion about nonopioid treatment options and/or about identifying the underlying cause of the patients’ pain. For example,
Clinician 5: The challenge here is making sure we are treating your pain with the right medication. Yea the Norco (hydrocodone and paracetamol) will make the pain go away, but it will not necessarily treat the cause of the pain, and if we treat the cause of the pain then maybe long term you will not have to take [opioids] . . .
Patient 17: Well I’m thinking I might have hurt it lifting her. I still do a lot of lifting and she’s [granddaughter] gotten heavier . . .
Similarly, another clinician focused on the importance of understanding the underlying cause of pain rather than relying on opioids:
Clinician 7: You know as far as the pain medication. We need to figure out what’s going on. That way we can kind of get at the root cause and you know just throwing pills at you is not a good, long-term plan here . . .
Most patients listened or agreed with clinicians’ discussions of limited benefits from opioids and in a couple instances mentioned their acceptance that their pain may always linger.
Clinician 8: There’s certain things I’m just not going to be able to fix for you and I’m glad that you have that, you know, mind set about it, it certainly makes our job a lot easier.
Patient 20: Especially I have a lot of arthritis all over my body and that’s the same thing with the fibromyalgia, you just have a lot of pain. I’ve had it for 17 years. I guess I just learned to deal with it and pray that I can at least stay on the tramadol to help my legs.
Communication About Nonopioid Treatment Options for Chronic Pain
Many clinicians discussed using nonopioid therapies (e.g., nonsteroidal anti-inflammatory drugs, topical lidocaine, or physical therapy) as potentially better approaches to treating patients’ pain. In the example below, one clinician suggested several non-opioid treatment options in addition to not increasing the opioid dose:
Clinician 7: Instead of just upping what we are already doing actually keeping the Norco (hydrocodone and paracetamol) where we are but help attack the pain in another way. . . . Lyrica (pregabalin) and gabapentin. Physical therapy would be great . . .
Some clinicians also suggested additional assessments and consultations to identify the root cause of the patients’ pain condition (e.g., imaging or referral to surgery).
The majority of the patients agreed with or discussed additional information during nonopioid treatment discussions. Patients were often onboard with trying new medications to treat the pain and sometimes wanted clarification of medication administration, logistic information about tapering/receiving these new treatments such as transportation, or to share other relevant information. For example, Patient 26 agrees with the new treatment plan with the expectation that it will better control her pain.
Clinician 10: I would be interested to see how a combination of the Cymbalta and low dose Lyrica help with things and if that allows us to continue our efforts and kind of wean down that Oxycodone.
Patient 26: Yeah, if I can have an alternative that worked better, hey I’m in.
In the context of a couple physical therapy discussions, clinicians emphasized the importance of pursuing physical therapy to avoid falls and improve physical function. Beyond these, functional discussions varied from a short statement at the beginning or end of a visit to patients setting goals such as playing with grandkids or going upstairs.
Communication About the Goal of the Opioid Tapering
Some of the clinicians had discussions about tapering the opioid medications that patients were currently taking. Tapering-related utterances ranged from clinicians expressing discomfort with a current opioid dose to clinicians directly recommending dose reduction. Some of these communications were suggestive of ongoing discussions about opioid tapering across several visits. For example, one clinician responded to a patient’s request for an increase in an opioid dose by suggesting opioid tapering and her discomfort with the current dose:
Patient 1: Really I need something better for pain. I really do. If you could up my milligram.
Clinician 1: I won’t be able to do that, actually we’re working on decreasing it, because you’re on more than I’m really comfortable prescribing.
In this example, the clinician recommended nonopioids for pain in support of the tapering process:
Patient 26, Clinician 10: I would be interested to see how a combination of the Cymbalta (duloxetine) and low dose Lyrica (pregabalin) help with things and if that allows us to continue our efforts and kind of wean down that oxycodone.
Most patients agreed with tapering discussions while a couple requested more information about the tapering process such as how much they would be going down.
Clinician 5: So instead of like taking away the 7s and going straight to the 5s you take them away incrementally.
Patient 11: What are you thinking of this?
Clinician 5: It is a little bit slower, but I think you will feel less of a change.
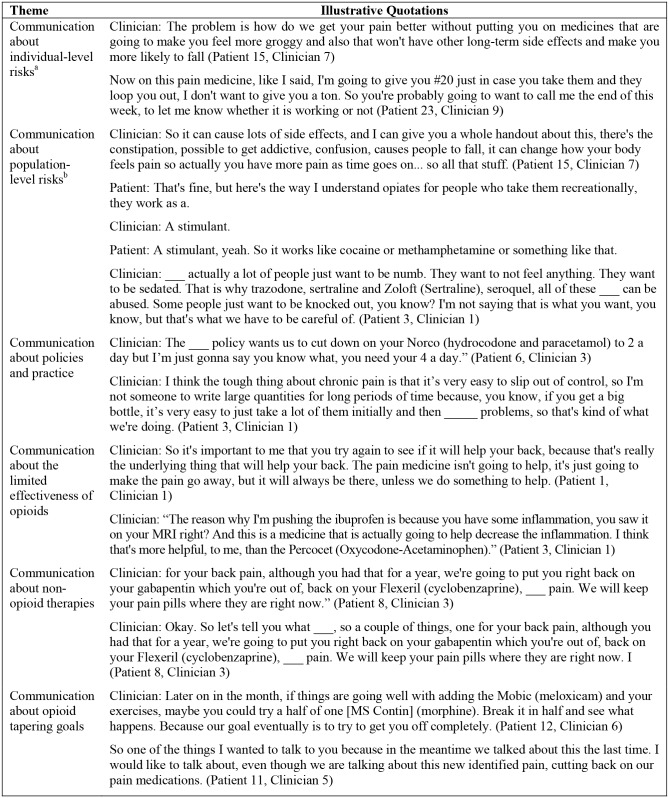
Additional illustrative quotes related to each of the five themes can be found in Figure 1.
Figure 1.
Emergent themes with illustrative quotes.
aIndividualized risk discussions occur when a clinician addresses risks specific to that patient.
bPopulation risk discussions occur when a clinician addresses risks about the general population rather than the patient.
Discussion
Currently, the United States is facing a public health crisis related to opioid use disorder and overdose deaths.20,21 A significant driver of this crisis has been widespread opioid prescribing for pain, a prevalent symptom that affects millions of Americans. Primary care clinicians prescribe more opioids than any other provider type.5 Yet primary care clinicians are time constrained during visits7,9 and report limited pain management knowledge.22 Therefore, this study aimed to describe how primary care clinicians communicate with patients about opioid-related risks, benefits, and goals. This is an important step in ensuring clinician communication is consistent with current clinical guidelines, and in supporting safe prescribing and effective clinician-patient relationships.
The primary finding of this study is that clinicians actively communicated about opioid-related risks in multiple ways. We observed clinicians explaining to patients that increased opioid doses could cause sedation and other adverse effects.23,24 In some cases, clinicians articulated these risks in terms of individual risk factors, such as increased risk of respiratory problems in a patient with COPD.25 More often, clinicians described population-level risk information, such as opioid-related mortality statistics. Clinicians also referenced policies or current practices that recommended caution in opioid dosing, which could be interpreted as indirect discussions about risks. Similar to prior research, we found that clinicians referenced policies as a facilitator in tapering discussions to avoid blame and discomfort when communicating with the patient.26 Given that clinical guidelines recommend clinicians actively assess and discuss risks, this finding is generally encouraging; however, with recent attention to guideline misapplication, this discussion type may be a concern for patients whose risks do not outweigh the benefits.27,28 At the same time, it is unclear if and how different approaches to communicating opioid-related risks differentially affect patients. The use of different risk communication approaches may have implications for clinician satisfaction as well as patient satisfaction, treatment adherence, and health behavior.29,30 Evidence shows that clinicians who tailor their risk communication to a specific patient’s case might better inform patients.29–32 For example, a recent study revealed that patients preferred to know how opioids may affect their health based on their unique medical history, as opposed to population-level concerns.29 Furthermore, more accurate patient risk perceptions may aid conversations about therapy changes, such as opioid tapering.29 At the same time, when discussing concerns about risks and aiming to reduce opioids, a conversation that can be fraught,30,33–36 clinicians may feel more comfortable deferring to a third-party policy or rule, which cannot be directly negotiated.
When examining utterances about opioid-related risks from the patient perspective, we observed that most of the patients listened to clinicians discussing risks without commenting. Some of the patients wanted to have clarifying discussions about risks of opioids. Thus, similar to prior research our findings suggest that patients may not fully understand or agree that opioid-related risks apply to them.29 Additional research is needed to identify barriers that preclude patients from being more actively engaged in communication about opioid-related risks with their primary care provider.
We also found that clinicians communicated about the limited effectiveness of opioids in treating chronic noncancer pain, especially for improving general outcomes like physical function.23,37 Such discussions are encouraging given the limited evidence for the benefit of long-term opioids in treating chronic noncancer pain.38
We also found that many clinicians discussed the use of nonopioid therapies for patients’ pain. In some cases, using nonopioid therapies was described in the context of clinicians’ goals to maintain or decrease patients’ opioid doses. While we saw patients often agree or listen to the proposed changes to their treatment plan, previous literature suggests patients are not confident about managing pain without opioid medication.8 This incongruence between patient preferences and utterances during clinic visits has the potential to harm patient-clinician relationship and should be explored further.
Our study has a number of strengths. By collecting direct observations of clinical visits, we obtained a rich understanding of how chronic pain care is delivered in an era of increased concern about the risks and potential benefits of opioid prescribing. Moreover, we observed a diverse group of clinicians and patients that spanned rural and urban areas and multiple health systems. Also, by using a mixed inductive and deductive thematic analysis approach, we were able to gain a more thorough understanding of how opioids are discussed during healthcare encounters. Still, our study is not without limitations. Although we reached thematic saturation in our analysis, having a larger and/or more diverse sample of clinicians might have elicited a wider range of communication themes. It is also plausible that patients or clinicians who declined to participate may engage in different discussions about opioids than those who volunteered to be observed; consequently, we may have missed some aspects of clinical communication and perspectives related to risks, benefits, and goals of opioid therapy. Additionally, we did not assess the dose, type, duration of opioid therapy, or history of substance use disorder, all of which might influence communication about opioid therapy. Also, our study occurred in the Midwestern United States, and results may not be transferable to other settings. With that said, this region of the country has been particularly affected by opioid use disorder, making it an important area to study. We also recognized that clinician discussions could have been affected by being audio recorded. However, we believe that by using a discreetly placed audio-only recorder, such effects were minimal. Finally, because we captured a single visit in an ongoing patient-clinician relationship, we may have missed other relevant communication about risks, benefits, and goals of opioid therapy. With that said, given the risks and regulations currently surrounding chronic opioid therapy, we believe it is reasonable to expect that some meaningful opioid-related communication occurs at all primary care visits.
In conclusion, this study provides timely understanding of how clinicians communicate with patients about common chronic pain conditions and the medications often used in their treatment. Our findings add to recent literature that aims to conceptually describe factors affecting patient-clinician interactions39 and clinical decision making for chronic pain care.40 Building on our work, future studies might examine larger samples of patients and clinicians to estimate the prevalence of the types of communication we observed as well as the relative effectiveness of different communication strategies. Finally, educational efforts and decision support tools could be designed to help clinicians communicate with patients in ways that support safe and guideline-concordant opioid prescribing while minimizing poor patient experiences.
Supplemental Material
Supplemental material, RBG_Themes_MDM_Policy_and_Practice_Second_Review_Final_clean_doc.rjf_online_supp for An Analysis of Primary Care Clinician Communication About Risk, Benefits, and Goals Related to Chronic Opioid Therapy by Elizabeth C. Danielson, Olena Mazurenko, Barbara T. Andraka-Christou, Julie DiIulio, Sarah M. Downs, Robert W. Hurley and Christopher A. Harle in MDM Policy & Practice
Acknowledgments
The authors acknowledge Laura Militello, MS (Applied Decision Science), and Robert Cook, MD, MPH (University of Florida), for their input into the study design, data collection, and analysis. Each author listed significantly contributed to the work presented in this article.
Footnotes
The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: BTA has received past grant funding from Alkermes, Inc. CAH has received past grant funding from Pfizer, Inc., Impact Education as a speaker honorarium, and the International Olympic Committee for travel. Authors ECD, OM, JD, SMD, and RWH declare that they have no competing interests.
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Financial support for this study was provided entirely by Grant Number R01HS023306 from the Agency for Healthcare Research and Quality. The funding agreement ensured the authors’ independence in designing the study, interpreting the data, writing, and publishing the report.
Authors’ Note: Preliminary analysis for this article was represented at the American Pain Society Conference in 2017 and AcademyHealth Annual Research Meeting in 2018.
ORCID iD: Christopher A. Harle  https://orcid.org/0000-0002-4803-3632
https://orcid.org/0000-0002-4803-3632
Supplemental Material: Supplementary material for this article is available on the Medical Decision Making Policy & Practice website at http://journals.sagepub.com/home/mpp.
Contributor Information
Elizabeth C. Danielson, Department of Health Policy and Management, Indiana University Richard M. Fairbanks School of Public Health, Indianapolis, Indiana
Olena Mazurenko, Department of Health Policy and Management, Indiana University Richard M. Fairbanks School of Public Health, Indianapolis, Indiana.
Barbara T. Andraka-Christou, College of Health & Public Affairs, University of Central Florida, Orlando, Florida
Julie DiIulio, Applied Decision Science, LLC, Dayton, Ohio.
Sarah M. Downs, Department of Health Policy and Management, Indiana University Richard M. Fairbanks School of Public Health, Indianapolis, Indiana
Robert W. Hurley, Wake Forest University School of Medicine, Winston Salem, North Carolina
Christopher A. Harle, Department of Health Policy and Management, Indiana University Richard M. Fairbanks School of Public Health, Indianapolis, Indiana; Regenstrief Institute Center for Biomedical Informatics, Indianapolis, IN.
References
- 1. Nahin RL. Estimates of pain prevalence and severity in adults: United States, 2012. J Pain. 2015;16(8):769–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Gaskin DJ, Richard P. The economic costs of pain in the United States. J Pain. 2012;13(8):715–24. [DOI] [PubMed] [Google Scholar]
- 3. Rudd RA, Aleshire N, Zibbell JE, Gladden RM. Increases in drug and opioid overdose deaths—United States, 2000–2014. MMWR Morb Mortal Wkly Rep. 2016;64(50–51):1378–82. [DOI] [PubMed] [Google Scholar]
- 4. Seth P, Scholl L, Rudd RA, Bacon S. Overdose deaths involving opioids, cocaine, and psychostimulants—United States, 2015–2016. MMWR Morb Mortal Wkly Rep. 2018;67(12):349–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Levy B, Paulozzi L, Mack KA, Jones CM. Trends in opioid analgesic-prescribing rates by specialty, US, 2007–2012. Am J Prev Med. 2015;49(3):409–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Dowell D, Haegerich TM, Chou R. CDC guideline for prescribing opioids for chronic pain—United States, 2016. JAMA. 2016;315(15):1624–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Tai-Seale M, McGuire TG, Zhang W. Time allocation in primary care office visits. Health Serv Res. 2007;42(5):1871–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Frank JW, Levy C, Matlock DD, et al. Patients’ perspectives on tapering of chronic opioid therapy: a qualitative study. Pain Med. 2016;17(10):1838–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Østbye T, Yarnall KS, Krause KM, Pollak KI, Gradison M, Michener JL. Is there time for management of patients with chronic diseases in primary care? Ann Fam Med. 2005;3(3):209–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Goesling J, Moser SE, Lin LA, Hassett AL, Wasserman RA, Brummett CM. Discrepancies between perceived benefit of opioids and self-reported patient outcomes. Pain Med. 2016;19(2):297–306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Henry SG, Bell RA, Fenton JJ, Kravitz RL. Goals of chronic pain management: do patients and primary care physicians agree and does it matter? Clin J Pain. 2017;33(11):955–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Fereday J, Muir-Cochrane E. Demonstrating rigor using thematic analysis: a hybrid approach of inductive and deductive coding and theme development. Int J Qual Methods. 2006;5(1):80–92. [Google Scholar]
- 13. Cho JY, Lee EH. Reducing confusion about grounded theory and qualitative content analysis: Similarities and differences. Qual Rep. 2014;19(32):1–20. [Google Scholar]
- 14. SocioCultural Research Consultants. Dedoose Version 7.7.6, Web Application for Managing, Analyzing, and Presenting Qualitative and Mixed Method Research Data. Los Angeles: SocioCultural Research Consultants; 2017. [Google Scholar]
- 15. Heigham J, Croker R. Qualitative Research in Applied Linguistics: A Practical Introduction. London: Palgrave Macmillan; 2009. [Google Scholar]
- 16. Crabtree BF, Miller WL. Doing Qualitative Research. Thousand Oaks, CA: SAGE Publishing; 1999. [Google Scholar]
- 17. Borkan J. Immersion/crystallization. In: Crabtree BF, Miller WL, eds. Doing Qualitative Research. Thousand Oaks: Sage; 1999. p 179–94. [Google Scholar]
- 18. Charmaz K. Constructing Grounded Theory: A Practical Guide Through Qualitative Analysis. Thousand Oaks: Sage; 2006. [Google Scholar]
- 19. Davies D, Dodd J. Qualitative research and the question of rigor. Qual Health Res. 2002;12(2):279–89. [DOI] [PubMed] [Google Scholar]
- 20. Rudd RA, Seth P, David F, Scholl L. Increases in drug and opioid-involved overdose deaths—United States, 2010–2015. MMWR Morb Mortal Wkly Rep. 2016;65(50–51):1445–52. [DOI] [PubMed] [Google Scholar]
- 21. Hedegaard H, Warner M, Miniño AM. Drug Overdose Deaths in the United States, 1999–2016. NCHS Data Brief, No. 294. Hyattsville: National Center for Health Statistics; 2017. [Google Scholar]
- 22. Upshur CC, Luckmann RS, Savageau JA. Primary care provider concerns about management of chronic pain in community clinic populations. J Gen Intern Med. 2006;21(6):652–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Chou R, Turner JA, Devine EB, et al. The effectiveness and risks of long-term opioid therapy for chronic pain: a systematic review for a National Institutes of Health Pathways to Prevention Workshop. Ann Intern Med. 2015;162(4):276–86. [DOI] [PubMed] [Google Scholar]
- 24. Birke H, Ekholm O, Sjøgren P, Kurita GP, Højsted J. Long-term opioid therapy in Denmark: a disappointing journey. Eur J Pain. 2017;21(9):1516–27. [DOI] [PubMed] [Google Scholar]
- 25. Levine M. In older adults with COPD, new opioid use was linked to increased risk for respiratory and all-cause mortality. Ann Intern Med. 2017;166(2):JC11. [DOI] [PubMed] [Google Scholar]
- 26. Kennedy LC, Binswanger IA, Mueller SR, et al. “Those conversations in my experience don’t go well”: a qualitative study of primary care provider experiences tapering long-term opioid medications. Pain Med. 2017;19(11):2201–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Kroenke K, Alford DP, Argoff C, et al. Challenges with implementing the centers for disease control and prevention opioid guideline: a consensus panel report. Pain Med. 2019;20(4):724–35. [DOI] [PubMed] [Google Scholar]
- 28. Centers for Disease Control and Prevention. CDC advises against misapplication of the Guideline for Prescribing Opioids for Chronic Pain [cited November 21, 2019]. https://www.cdc.gov/media/releases/2019/s0424-advises-misapplication-guideline-prescribing-opioids.html
- 29. Matthias MS, Johnson NL, Shields CG, et al. “I’m not gonna pull the rug out from under you”: patient-provider communication about opioid tapering. J Pain. 2017;18(11):1365–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Esquibel AY, Borkan J. Doctors and patients in pain: conflict and collaboration in opioid prescription in primary care. Pain. 2014;155(12):2575–82. [DOI] [PubMed] [Google Scholar]
- 31. Fagerlin A, Zikmund-Fisher BJ, Ubel PA. Helping patients decide: ten steps to better risk communication. J Natl Cancer Inst. 2011;103(19):1436–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Kreuter MW, Wray RJ. Tailored and targeted health communication: strategies for enhancing information relevance. Am J Health Behav. 2003;27(Suppl. 3):S227–S232. [DOI] [PubMed] [Google Scholar]
- 33. Matthias MS, Parpart AL, Nyland KA, et al. The patient-provider relationship in chronic pain care: providers’ perspectives. Pain Med. 2010;11(11):1688–97. [DOI] [PubMed] [Google Scholar]
- 34. Dobscha SK, Corson K, Flores JA, Tansill EC, Gerrity MS. Veterans affairs primary care clinicians’ attitudes toward chronic pain and correlates of opioid prescribing rates. Pain Med. 2008;9(5):564–71. [DOI] [PubMed] [Google Scholar]
- 35. Frantsve LME, Kerns RD. Patient-provider interactions in the management of chronic pain: current findings within the context of shared medical decision making. Pain Med. 2007;8(1):25–35. [DOI] [PubMed] [Google Scholar]
- 36. Henry SG, Bell RA, Fenton JJ, Kravitz RL. Communication about chronic pain and opioids in primary care: Impact on patient and physician visit experience. Pain. 2018;159(2):371–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Noble M, Tregear SJ, Treadwell JR, Schoelles K. Long-term opioid therapy for chronic noncancer pain: a systematic review and meta-analysis of efficacy and safety. J Pain Symptom Manage. 2008;35(2):214–28. [DOI] [PubMed] [Google Scholar]
- 38. Krebs EE, Gravely A, Nugent S, et al. Effect of opioid vs nonopioid medications on pain-related function in patients with chronic back pain or hip or knee osteoarthritis pain: the SPACE randomized clinical trial. JAMA. 2018;319(9):872–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Henry SG, Matthias MS. Patient-clinician communication about pain: a conceptual model and narrative review. Pain Med. 2018;19(11):2154–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Militello LG, Anders S, Downs SM, et al. Understanding how primary care clinicians make sense of chronic pain. Cogn Technol Work. 2018;20(4):575–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, RBG_Themes_MDM_Policy_and_Practice_Second_Review_Final_clean_doc.rjf_online_supp for An Analysis of Primary Care Clinician Communication About Risk, Benefits, and Goals Related to Chronic Opioid Therapy by Elizabeth C. Danielson, Olena Mazurenko, Barbara T. Andraka-Christou, Julie DiIulio, Sarah M. Downs, Robert W. Hurley and Christopher A. Harle in MDM Policy & Practice