Abstract
BACKGROUND
Bouveret syndrome is a rare complication of cholelithiasis, with only 315 cases reported in the literature between 1967 and 2016. Delay in diagnosis is associated with a high mortality rate. Diagnosis is based upon clinical manifestations, gastroscopy, and imaging studies such as abdominal computed tomography and magnetic resonance cholan-giopancreatography. Endoscopic stone extraction or lithotripsy is the preferred choice for treatment as it is safe and minimally invasive with few complications. However, if endoscopy fails, surgery is required.
CASE SUMMARY
A 61-year-old female patient presented with recurrent epigastric pain for more than 6 mo. On endoscopy, a large amount of food residue was present in the stomach with multiple stones and ulcers in the antro-pyloric region. Based on these findings, a diagnosis of gastrolithiasis was made. However, computed tomography of the abdomen revealed the correct diagnosis of Bouveret syndrome. Initially, endoscopic treatment was attempted but it failed. Later, she was successfully managed by cholecystectomy with duodenal stone extraction and fistula repair (one-step method). At the last follow-up 6 mo after surgery, the patient was symptom-free.
CONCLUSION
Bouveret syndrome is a rare complication of gallstones that requires prompt endoscopic or surgical treatment to prevent mortality.
Keywords: Bouveret syndrome, Gallstones, Intestinal obstruction, Case report
Core tip: Bouveret syndrome is a rare clinical disease, with only 315 cases reported in the literature between 1967 and 2016. The disease is often misdiagnosed and has high mortality if diagnosis is delayed. Here, we describe a case of Bouveret syndrome, which was initially misdiagnosed as gastric calculus based on endoscopy but was later correctly diagnosed with Bouveret syndrome on computed tomography. The patient was successfully treated by surgery after failed endoscopic therapy.
INTRODUCTION
Bouveret syndrome is a rare clinical disease. Only 315 cases have been reported in the literature between 1967 and 2016. The disease is easy to get misdiagnosed and has high mortality if the diagnosis is delayed. Tools that have proven useful for diagnosing this disease include upper gastrointestinal endoscopy, computed tomography (CT) of the abdomen, and magnetic resonance cho-langiopancreatography (MRCP). Here, we describe a case of Bouveret syndrome, which was initially misdiagnosed as gastric calculus based on endoscopy but was later correctly diagnosed with the help of CT. The patient was successfully treated by surgery after failed endoscopic therapy.
CASE PRESENTATION
Chief complaints
A 61-year-old woman presented with recurrent epigastric pain for more than 6 mo. Her abdominal pain had worsened during a period of 4 days and was associated with vomiting and abdominal distention. She denied having a fever with chills or jaundice.
History of past illness
Her previous history included hypertension and diabetes.
Personal and family history
The family history was unremarkable.
Physical examination
On clinical examination, her abdomen was soft with mild epigastric tenderness and positive succussion splash.
Laboratory examinations
Blood examination showed a white blood cell count of 13.1 × 109/L with neutrophilia (75.7%), total bilirubin level of 28.7 mmol/L, direct bilirubin levels of 7.8 mmol/L, alanine aminotransferase level of 14 U/L, and aspartate aminotransferase level of 23 U/L.
Imaging examinations
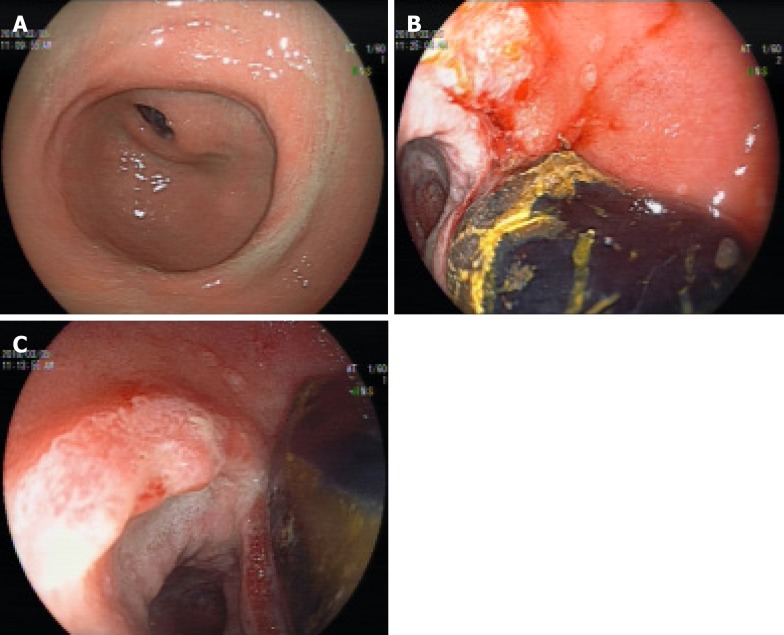
On gastroscopy, a large amount of food residue was present in the gastric fundus and body, and multiple stones and ulcers were found in the pyloric region and first part of the duodenum, causing gastric outlet obstruction (Figure 1). A provisional diagnosis of gastrolithiasis was made. Endoscopic extraction of the stones using a snare was attempted but was unsuccessful.
Figure 1.
Endoscopic findings. A: Deformed antrum; B and C: Duodenal bulbar stones and fistula that were misdiagnosed as gastric calculi and ulcers.
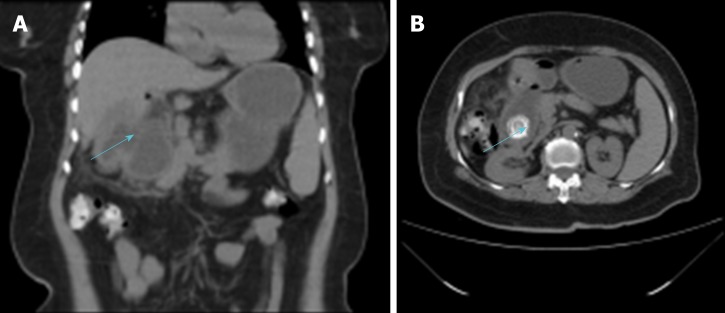
Abdominal ultrasonography showed a 6.4 cm × 3.6 cm heteroechoic lesion in the region of the junction between the pylorus and duodenum with a 4.9 cm stone located within. The gallbladder was shrunken and located close to the heteroechoic lesion. Abdominal CT showed chronic cholecystitis with a cholecystoduodenal fistula and the presence of an approximately 3.0 cm × 2.4 cm stone in the descending part of the duodenum (Figure 2). There was partial intrahepatic bile duct dilatation with pneumobilia.
Figure 2.
Computed tomography. A: Cholecystoduodenal fistula; B: The 3.0 cm x 2.4 cm stone in the descending part of the duodenum.
FINAL DIAGNOSIS
Based on the above findings, Bouveret syndrome was suspected.
TREATMENT
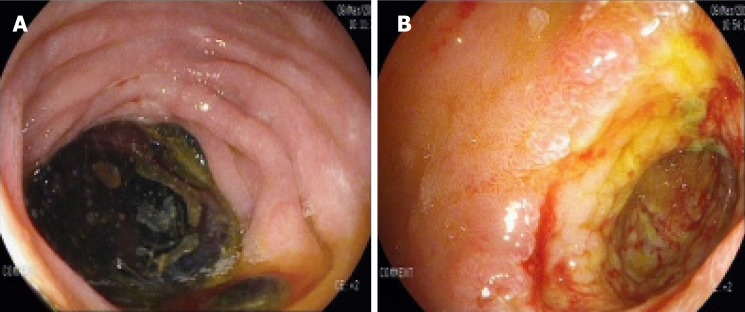
Repeat gastroscopy was performed, which showed a duodenal bulb stone with incarceration and a fistulous opening in the duodenal bulb (Figure 3). Due to the failure of multiple endoscopic stone extraction attempts, the patient had a hepatobiliary surgery consultation. Considering the patient’s long course of disease, CT findings of cholecystoduodenal fistula, and possibility of severe adhesions, open cholecystectomy with duodenal stone extraction and fistula repair were planned over laparoscopic treatment.
Figure 3.
Repeat gastroscopy. A: Stone incarceration in the duodenal bulb; B: The internal opening of the cholecystoduodenal fistula.
Intraoperatively, dense adhesions were present between the gallbladder and surrounding omentum tissue. The gallbladder was shrunken and thickened up to 1 cm with the presence of a cholecystoduodenal fistula of 2 cm. Calot’s triangle was frozen, making the dissection difficult. Upon opening the duodenum, an oval calculus about 4 cm x 6 cm in size was found in the descending duodenal segment. Cholecystectomy with duodenal stone extraction and fistula repair were performed.
OUTCOME AND FOLLOW-UP
The operation lasted 5 h and the intraoperative blood loss was 300 mL. The postoperative course was uneventful with a postoperative hospital stay of 7 d. At the last follow-up 6 mo after surgery, the patient was symptom-free.
DISCUSSION
Gallstones can migrate into the intestinal tract via the cholecysto- or choledochal-duodenal fistula and block the proximal duodenum or pylorus, causing gastric outlet obstruction, a condition known as Bouveret syndrome[1]. It is a rare complication of cholelithiasis. In the past 50 years from 1967 to 2016, only about 315 cases have been reported in the literature. The mortality rate of Bouveret syndrome is 12%–30% as it frequently occurs in elderly patients and is associated with many complications[2]. Fistula formation occurs due to pressure necrosis of the gallbladder wall and the adjacent organ (duodenum in this case) densely adhered to it. Other contributory factors include chronic inflammatory changes in the gallbladder wall and impaction of the stone in the gallbladder neck[3]. In the present case, the 6-mo history of epigastric pain was probably caused by calculous cholecystitis, and the calculi broke into the duodenal bulb after a long time.
Bouveret syndrome should be suspected in elderly patients with a previous history of chronic calculous cholecystitis, and sudden abdominal pain that is mainly in the right hypochondriac or epigastric region and is accompanied by nausea, vomiting, fever, and chills. Physical examination may reveal epigastric, subxiphoid, or right hypochondriac tenderness. Blood examination may show leukocytosis, deranged liver function tests, and elevation of inflammatory markers such as C-reactive protein. However, in rare cases it may show air-fluid levels suggestive of gastrointestinal obstruction, a high-density shadow in the right upper abdomen, and pneumobilia[4].
X-ray examination plays a limited role in diagnosing this disease. However, abdominal ultrasound is useful in determining the gallbladder wall thickening, gallbladder atrophy, and the presence or absence of gallstones. Moreover, in some cases, it can detect discontinuity in the gallbladder wall and the presence of gas in the gallbladder suggestive of internal fistula. Abdominal CT is an important tool for diagnosing this disease. The radiological triad of Rigler (small bowel obstruction, pneumobilia, and ectopic gallstone) is specific for its diagnosis[5,6]. The so-called “ectopic gallstone” is the stone shadow on the right side at the level of T12–L1 vertebrae. MRCP, especially contrast-enhanced MRCP, has high diagnostic value as it can detect the presence of fistula, as well as the size and location of the stone and its relationship with the fistula[7]. Upper gastrointestinal endoscopy is both diagnostic and therapeutic for this disease, as it can visualize the site and cause of upper gastrointestinal obstruction including the incarcerated stones. In about 31% of cases, the internal opening of the cholecystointestinal or choledochointestinal fistula can be detected[8]. Sometimes, the huge stone blocks the fistulous opening and also limits the endoscopic vision, leading to misdiagnosis as was seen in the current case.
Various treatments for Bouveret syndrome have been described in the literature, and can be broadly divided into non-surgical and surgical treatments. Non-surgical treatment has a low success rate about 9%[9]. However, with advances in endoscopic techniques, the success rate has greatly improved in the recent years. Common methods used to break the large stone into pieces include endoscopic lithotripsy, extracorporeal shock wave lithotripsy, electro-hydraulic lithotripsy, and endoscopic laser lithotripsy. The latter two technologies are simple, safe, and effective, with few complications, and are currently the most commonly used methods[10]. However, some scholars believe that endoscopic lithotomy increases the risk of esophageal injury, digestive tract perforation, and gastrointestinal bleeding. A study showed that 42% of patients failed to achieve stone removal by this technique[11]. Surgery is the mainstay of treatment and includes gastric or intestinal enterolithotomy with gallbladder duodenal fistula repair and cholecystectomy. It can be performed in a one or two-step method depending upon the patient’s age, physical condition, and disease characteristics. If the patient is in good general health, has a short history of symptoms, no major water, electrolyte imbalances, and no obvious inflammatory reaction at the site of choledocho- or cholecysto-intestinal fistula, one-stage operation can be considered[12]. The advantages of this method are that it prevents the need for a second operation and prevents the occurrence of retrograde biliary tract infection, gallbladder cancer, and recurrence of gallstone ileus. However, because the majority of patients with Bouveret syndrome are elderly, with a long history of systemic diseases, the incidence of postoperative complications and mortality of one-step surgery is relatively high. In such patients with higher risk of surgical complications, a two-step method is beneficial in which only the gastric or intestinal stones are removed in the first surgery to relieve the obstruction. After the patient’s physical condition improves, fistula repair and cholecystectomy can be performed in the second stage. Postoperative complications and mortality of the two-step method are significantly lower than those of the one-step method. Moreover, in some cases, a second surgery is not required as the diseased gallbladder is already shrunken and lacks stones due to the fistula. In addition, some scholars believe that in most patients, the biliary fistula closes spontaneously after the intestinal calculi are removed, making it unnecessary to repair the fistula. In such cases, biliary symptoms are often relieved or even disappear in the absence of stones, despite leaving the gallbladder in situ[13]. In recent years, with the extensive application of laparoscopy, laparoscopic surgery for Bouveret syndrome has become a safe and effective alternative to open surgery[14].
CONCLUSION
Bouveret syndrome is a rare clinical disease associated with high mortality, which requires a high index of clinical suspicion for timely diagnosis. CT, MRCP, and gastroscopy are the most useful tools for diagnosing this syndrome. Treatment should be individualized according to the patient’s age, physical condition, and disease characteristics. In view of the advantages of endoscopic lithotripsy or minimally invasive lithotripsy or lithotomy, it is recommended that endoscopic therapy be tried first; surgery can be performed if it fails[8]. For patients with multiple comorbidities and poor general condition, the two-step surgical method can significantly reduce mortality[15].
Footnotes
Informed consent statement: Written informed consent was obtained from the patient.
Conflict-of-interest statement: The authors declare that they have no conflict of interest.
CARE Checklist (2016) statement: The manuscript was prepared and revised according to the CARE Checklist (2016).
Manuscript source: Unsolicited manuscript
Peer-review started: August 19, 2019
First decision: September 10, 2019
Article in press: October 5, 2019
Specialty type: Medicine, Research and Experimental
Country of origin: China
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Iliescu L, Pan SM, Shabbir A S-Editor: Zhang L L-Editor: Wang TQ E-Editor: Liu MY
Contributor Information
Fei Wang, Department of Gastroenterology, People’s Hospital of Jianyang City, Jianyang 641400, Sichuan Province, China.
Zhi-Qiang Du, Department of Gastroenterology, People’s Hospital of Jianyang City, Jianyang 641400, Sichuan Province, China. 1028606063@qq.com.
Yi-Lan Chen, Department of Gastroenterology, People’s Hospital of Jianyang City, Jianyang 641400, Sichuan Province, China.
Tian-Ming Chen, Department of Gastroenterology, People’s Hospital of Jianyang City, Jianyang 641400, Sichuan Province, China.
Yue Wang, Department of Gastroenterology, People’s Hospital of Jianyang City, Jianyang 641400, Sichuan Province, China.
Xiang-Rong Zhou, Department of Gastroenterology, People’s Hospital of Jianyang City, Jianyang 641400, Sichuan Province, China.
References
- 1.Bhama JK, Ogren JW, Lee T, Fisher WE. Bouveret's syndrome. Surgery. 2002;132:104–105. doi: 10.1067/msy.2002.117196. [DOI] [PubMed] [Google Scholar]
- 2.Patel A, Agarwal S. The yellow brick road of Bouveret syndrome. Clin Gastroenterol Hepatol. 2014;12:A24. doi: 10.1016/j.cgh.2014.03.028. [DOI] [PubMed] [Google Scholar]
- 3.Mou XF, Tian LT, Zhou YX, X LL. Current status of diagnosis and treatment of Bouveret syndrome. Zhongguo Xiandai Putong Waike Jinzhan. 2013;16:484–485. [Google Scholar]
- 4.Lu DW, Li XP, Cai HP, Chen YX. Clinical analysis of 26 cases of Bouveret syndrome. Xiandai Shiyong Yixue. 2009;21:973–975. [Google Scholar]
- 5.Xia YP, Yu TF, Hu XY, Fang XM, Li D. Diagnostic value of CT plain scan for Bouveret syndrome. Linchuang Fangshexue Zazhi. 2012;31:588–590. [Google Scholar]
- 6.Chen LG, Ma J, Chen ZN, Hou LM. Progress in the diagnosis and treatment of Bouveret syndrome. Zhonghua Linchuang Yishi Zazhi. 2013;7:9576–9758 . [Google Scholar]
- 7.Algın O, Ozmen E, Metin MR, Ersoy PE, Karaoğlanoğlu M. Bouveret syndrome: evaluation with multidetector computed tomography and contrast-enhanced magnetic resonance cholangiopancreatography. Ulus Travma Acil Cerrahi Derg. 2013;19:375–379. doi: 10.5505/tjtes.2013.97254. [DOI] [PubMed] [Google Scholar]
- 8.Cappell MS, Davis M. Characterization of Bouveret's syndrome: a comprehensive review of 128 cases. Am J Gastroenterol. 2006;101:2139–2146. doi: 10.1111/j.1572-0241.2006.00645.x. [DOI] [PubMed] [Google Scholar]
- 9.Lowe AS, Stephenson S, Kay CL, May J. Duodenal obstruction by gallstones (Bouveret’s syndrome): a review of the literature. Endoscopy. 2005;37:82–87. doi: 10.1055/s-2004-826100. [DOI] [PubMed] [Google Scholar]
- 10.Sethi S, Kochar R, Kothari S, Thosani N, Banerjee S. Good Vibrations: Successful Endoscopic Electrohydraulic Lithotripsy for Bouveret's Syndrome. Dig Dis Sci. 2015;60:2264–2266. doi: 10.1007/s10620-014-3424-8. [DOI] [PubMed] [Google Scholar]
- 11.Mavroeidis VK, Matthioudakis DI, Economou NK, Karanikas ID. Bouveret syndrome-the rarest variant of gallstone ileus: a case report and literature review. Case Rep Surg. 2013;2013:839370. doi: 10.1155/2013/839370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Crespo Pérez L, Angueira Lapeña T, Defarges Pons V, Foruny Olcina JR, Cano Ruiz A, Benita León V, Gónzalez Martín JA, Boixeda de Miquel D, Milicua Salamero JM. [A rare cause of gastric outlet obstruction: Bouveret's syndrome] Gastroenterol Hepatol. 2008;31:646–651. doi: 10.1016/S0210-5705(08)75813-8. [DOI] [PubMed] [Google Scholar]
- 13.Stagnitti F, Mongardini M, Schillaci F, Dall’Olio D, De Pascalis M, Natalini E. Spontaneous biliodigestive fistulae. The clinical considerations, surgical treatment and complications. G Chir. 2000;21:110–117. [PubMed] [Google Scholar]
- 14.Narkhede RA, Bada VC, Kona LK. Laparoscopic Management of a Proximal Jejunal Gallstone with Patulous Ampulla and Choledochal Cyst-a Report of Unusual Presentation and a Review. Indian J Surg. 2017;79:51–57. doi: 10.1007/s12262-016-1575-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Corvera CU, Reza JA. In: Surgery of the Liver, Biliary Tract, and Pancreas. Philadelphia: Elsevier 2017; 2. Available from: https://www.sciencedirect.com/topics/medicine-and-dentistry/biliary-fistula. [Google Scholar]