Abstract
Optimal management of concomitant coronary artery disease and carotid artery stenosis remains unknown. Current treatment strategies for patients with significant dual disease burden include simultaneous carotid endarterectomy and coronary artery bypass grafting (CABG) or staged carotid endarterectomy and CABG. Herein we present the case of a patient with severe coronary artery disease and carotid artery stenosis and discuss a novel hybrid approach to management of concomitant coronary and carotid disease using transcarotid artery revascularization with flow reversal before CABG.
Keywords: Carotid artery stenosis, Transcarotid artery revascularization (TCAR), Combined coronary artery disease
Postoperative stroke is one of the most dreaded complications after coronary artery bypass grafting (CABG). The frequency of post-CABG stroke is 0.5% to 7%.1,2 The etiology of post-CABG stroke is multifactorial. Carotid atherosclerotic disease is a known independent predicator of perioperative stroke after coronary revascularization.3,4 Despite numerous studies, the optimal management of concomitant coronary artery disease and carotid artery stenosis remains unknown. Current treatment strategies include simultaneous carotid endarterectomy (CEA) and CABG, staged CEA followed by CABG, staged CABG followed by CEA, staged transfemoral carotid artery stenting (TF-CAS) and CABG, and simultaneous TF-CAS and CABG. None of these therapeutic approaches have been uniformly accepted by the cardiovascular community. Herein we present the case of a patient with severe coronary artery disease and carotid artery stenosis and discuss a novel hybrid approach to the management of concomitant coronary and carotid disease. The patient has been adequately informed and consented to publication of this case report.
Case report
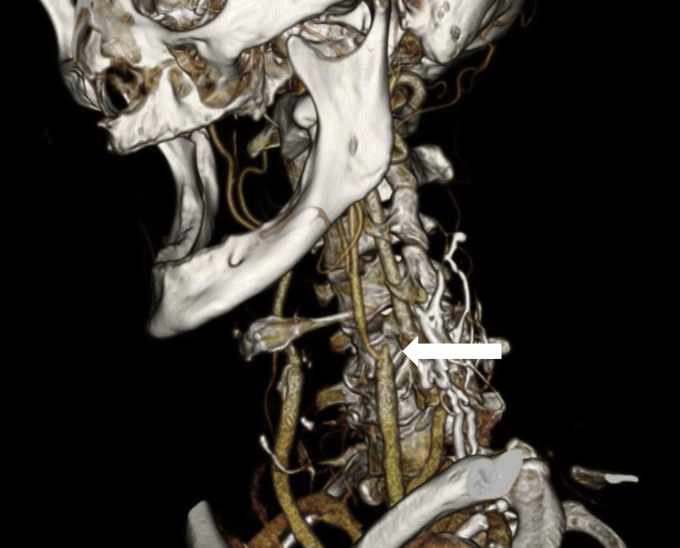
A 63-year-old man with a history of coronary artery disease, hyperlipidemia, hypertension, and tobacco abuse presented with acute onset of right hemiparesis and aphasia. Computed tomography angiography demonstrated a right internal carotid artery (ICA) occlusion and a left ICA string sign (Fig 1). During the course of the next few days, the patient recovered from a neurologic standpoint and was offered a left CEA. An electrocardiogram obtained as part of his preoperative workup showed new T-wave inversions. A subsequent echocardiogram demonstrated moderate left ventricular dysfunction with an ejection fraction of 35%. These new cardiac findings along with the patient's history of a myocardial infarction prompted a coronary catheterization, which demonstrated severe three-vessel coronary disease. Given the severity of the patient's coronary and carotid disease, he was offered a simultaneous transcarotid stent with the ENROUTE Transcarotid Neuroprotection and Stent System (Silk Road Medical, Sunnyvale, Calif) and CABG.
Fig 1.
Three-dimensional reconstruction of computed tomography angiography image demonstrating an apparent left internal carotid artery (ICA) occlusion due to trickle flow in ICA. The left ICA stump is marked by the arrow.
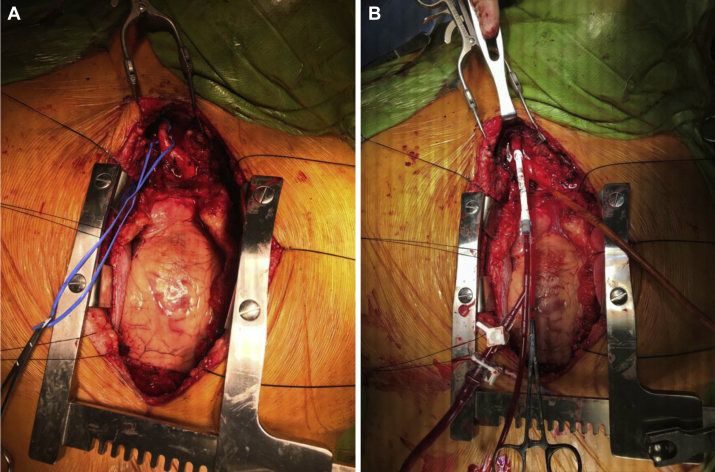
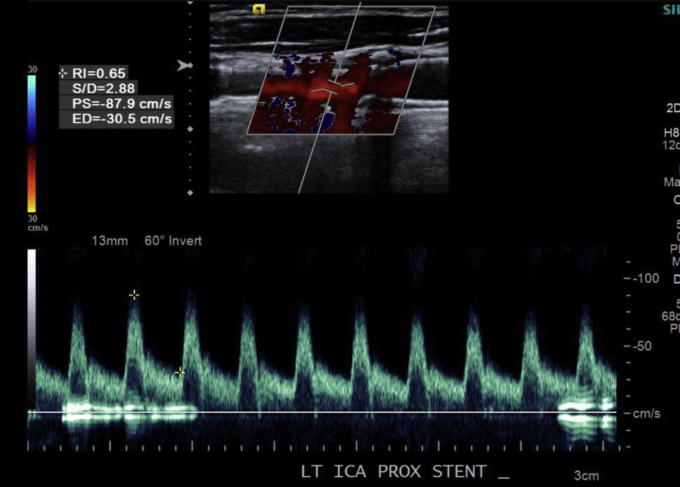
A sternotomy was performed, and the left internal mammary artery was harvested. Proximal control of the left common carotid artery (CCA) was obtained through the sternotomy incision (Fig 2, A). The right common femoral vein was accessed with a micropuncture kit under ultrasound guidance. The venous sheath was placed in the right femoral vein. The patient was heparinized to obtain an activated clotting time of >250 seconds. A purse-string suture was placed in the CCA, and the CCA was then accessed with a micropuncture kit. The arterial sheath was placed in the CCA (Fig 2, B). Intraoperative arteriography demonstrated severe stenosis in the proximal ICA (Fig 3, A). The flow controller was first connected to the arterial sheath, then the venous sheath. Active flow reversal was achieved by occluding the CCA proximal to the arteriotomy with an atraumatic vascular clamp. The lesion was crossed with a 0.014-inch wire and predilated, and a 7- × 30-mm self-expanding stent was deployed. A completion arteriogram was obtained postprocedurally and demonstrated a patent stent with no residual stenosis (Fig 3, B). The arterial sheath was removed and the arteriotomy was closed. The cardiac surgery team next performed a three-vessel CABG. After administration of protamine and chest closure, 300 mg of clopidogrel was given in the operating room through a nasogastric tube. Postoperatively, the patient was receiving dual antiplatelet therapy. The patient's postoperative course was complicated by atrial fibrillation; he was discharged home on postoperative day 9. There were no perioperative neurologic sequelae. A surveillance duplex ultrasound examination 1 month after transcarotid stent placement demonstrated a patent stent with no evidence of stenosis (Fig 4).
Fig 2.
A, Intraoperative view of proximal control of the common carotid artery (CCA) through median sternotomy. B, Intraoperative view of ENROUTE Transcarotid Neuroprotection and Stent System in place with arterial sheath in CCA.
Fig 3.
A, Intraoperative arteriogram demonstrating a critical left internal carotid artery (ICA) stenosis. B, Completion arteriogram demonstrating excellent flow in left ICA.
Fig 4.
Surveillance duplex ultrasound image demonstrating a patent stent with no hemodynamically significant stenosis.
Discussion
Concomitant carotid and coronary artery occlusive disease is a common clinical entity encountered by vascular and cardiac surgeons. Approximately 28% of patients undergoing CEA have significant coronary disease requiring revascularization.5 Similarly, 12% of patients undergoing coronary revascularization have hemodynamically significant carotid disease.6,7 The presence of significant carotid disease increases the risk of stroke after CABG.8,9 There is no consensus on the optimal management of synchronous carotid and coronary disease, although numerous single-institution retrospective studies have attempted to answer this question. However, in many instances, there are conflicting conclusions. For example, a meta-analysis of 16 observational studies by Borger et al10 demonstrated a significantly higher mortality and stroke rate for combined CEA-CABG compared with a staged approach. The subsequent meta-analysis by Sharma et al11 of 12 observational studies, on the other hand, found no difference in mortality and stroke between combined CEA-CABG and staged CEA-CABG.
TF-CAS is a viable alternative to CEA in certain patients. However, TF-CAS has not been widely adopted because it has consistently demonstrated higher stroke rates compared with CEA.12 In fact, a meta-analysis of 31 studies by Paraskevas et al13 reported a perioperative stroke rate of 15% for patients with symptomatic carotid disease undergoing TF-CAS and CABG. Transcarotid artery revascularization (TCAR) with dynamic flow reversal is a new endovascular option for carotid revascularization. The initial results appear to be superior to those of TF-CAS.14,15
Given this patient's severe coronary and carotid disease, we believed that simultaneous coronary and carotid revascularization was the optimal strategy. TCAR through a median sternotomy provided the morbidity benefits of an endovascular approach while mitigating stroke risk by avoiding aortic arch manipulation. However, this hybrid strategy has its limitations. The primary limitation is a deviation from the standard dual antiplatelet regimen. Our patient was managed with aspirin preoperatively, anticoagulated with heparin intraoperatively, and loaded with clopidogrel at the completion of the procedure. The onset of action of clopidogrel is 2 hours; therefore, there is a period of time when the stent is unprotected. Kon et al16 demonstrated that this antiplatelet regimen was safe in a small series of patients undergoing hybrid coronary revascularization. Nevertheless, carotid artery stenting in this setting is high risk and should be cautiously considered on a case-by-case basis.
Conclusions
Simultaneous TCAR-CABG is a novel hybrid strategy for the management of patients with concomitant carotid and coronary disease. The optimal antiplatelet regimen is unknown. Further investigation is needed before this technique is widely adopted.
From the Society for Clinical Vascular Surgery
Footnotes
Author conflict of interest: none.
The editors and reviewers of this article have no relevant financial relationships to disclose per the Journal policy that requires reviewers to decline review of any manuscript for which they may have a conflict of interest.
References
- 1.Kougias P., Kappa J.R., Sewell D.H., Feit R.A., Michalik R.E., Imam M. Simultaneous carotid endarterectomy and coronary artery bypass grafting: results in specific patient groups. Ann Vasc Surg. 2007;21:408–414. doi: 10.1016/j.avsg.2006.12.007. [DOI] [PubMed] [Google Scholar]
- 2.Fukuda I., Gomi S., Watanabe K., Seita J. Carotid and aortic screening for coronary artery bypass grafting. Ann Thorac Surg. 2000;70:2034–2039. doi: 10.1016/s0003-4975(00)02132-9. [DOI] [PubMed] [Google Scholar]
- 3.Brown K.R., Kresowik T.F., Chin M.H., Kresowik R.A., Grund S.L., Hendel M.E. Multistate population-based outcomes of combined carotid endarterectomy and coronary artery bypass. J Vasc Surg. 2003;37:32–39. doi: 10.1067/mva.2003.60. [DOI] [PubMed] [Google Scholar]
- 4.Cambria R.P., Ivarsson B.L., Akins C.W., Moncure A.C., Brewster D.C., Abbott W.M. Simultaneous carotid and coronary disease: safety of the combined approach. J Vasc Surg. 1989;9:56–64. [PubMed] [Google Scholar]
- 5.Brown K.R. Treatment of concomitant carotid and coronary artery disease. Decision-making regarding surgical options. J Cardiovasc Surg. 2003;44:395–399. [PubMed] [Google Scholar]
- 6.Salasidis G.C., Latter D.A., Steinmetz O.K., Blair J.F., Graham A.M. Carotid artery duplex scanning in preoperative assessment for coronary artery revascularization: the association between peripheral vascular disease, carotid artery stenosis, and stroke. J Vasc Surg. 1995;21:154–162. doi: 10.1016/s0741-5214(95)70254-7. [DOI] [PubMed] [Google Scholar]
- 7.Hertzer N.R., Loop F.D., Taylor P.C., Beven E.G. Staged and combined surgical approach to simultaneous carotid and coronary vascular disease. Surgery. 1978;84:803–811. [PubMed] [Google Scholar]
- 8.Prasad S.M., Li S., Rankin J.S., O'Brien S.M., Gammie J.S., Puskas J.D. Current outcomes of simultaneous carotid endarterectomy and coronary artery bypass graft surgery in North America. World J Surg. 2010;34:2292–2298. doi: 10.1007/s00268-010-0506-4. [DOI] [PubMed] [Google Scholar]
- 9.Naylor A.R., Bown M.J. Stroke after cardiac surgery and its association with asymptomatic carotid disease: an updated systematic review and meta-analysis. Eur J Vasc Endovasc Surg. 2011;41:607–624. doi: 10.1016/j.ejvs.2011.02.016. [DOI] [PubMed] [Google Scholar]
- 10.Borger M.A., Fremes S.E., Weisel R.D., Cohen G., Rao V., Lindsay T.F. Coronary bypass and carotid endarterectomy: does a combined approach increase risk? A metaanalysis. Ann Thorac Surg. 1999;68:14–21. doi: 10.1016/s0003-4975(99)00474-9. [DOI] [PubMed] [Google Scholar]
- 11.Sharma V., Deo S.V., Park S.J., Joyce L.D. Meta-analysis of staged versus combined carotid endarterectomy and coronary artery bypass grafting. Ann Thorac Surg. 2014;97:102–109. doi: 10.1016/j.athoracsur.2013.07.091. [DOI] [PubMed] [Google Scholar]
- 12.Brott T.G., Voeks J.H., Howard V.J. Stenting versus surgery for carotid stenosis. N Engl J Med. 2016;375:604–605. doi: 10.1056/NEJMc1605166. [DOI] [PubMed] [Google Scholar]
- 13.Paraskevas K.I., Nduwayo S., Saratzis A.N., Naylor A.R. Carotid stenting prior to coronary bypass surgery: an updated systematic review and meta-analysis. Eur J Vasc Endovasc Surg. 2017;53:309–319. doi: 10.1016/j.ejvs.2016.12.019. [DOI] [PubMed] [Google Scholar]
- 14.Malas M.B., Dakour-Aridi H., Wang G.J., Kashyap V.S., Motaganahalli R.L., Eldrup-Jorgensen J. Transcarotid artery revascularization versus transfemoral carotid artery stenting in the Society for Vascular Surgery Vascular Quality Initiative. J Vasc Surg. 2019;69:92–103.e2. doi: 10.1016/j.jvs.2018.05.011. [DOI] [PubMed] [Google Scholar]
- 15.Kwolek C.J., Jaff M.R., Leal J.I., Hopkins L.N., Shah R.M., Hanover T.M. Results of the ROADSTER multicenter trial of transcarotid stenting with dynamic flow reversal. J Vasc Surg. 2015;62:1227–1234. doi: 10.1016/j.jvs.2015.04.460. [DOI] [PubMed] [Google Scholar]
- 16.Kon Z.N., Brown E.N., Tran R., Joshi A., Reicher B., Grant M.C. Simultaneous hybrid coronary revascularization reduces postoperative morbidity compared with results from conventional off-pump coronary artery bypass. J Thorac Cardiovasc Surg. 2008;135:367–375. doi: 10.1016/j.jtcvs.2007.09.025. [DOI] [PMC free article] [PubMed] [Google Scholar]